Abstract
Rationale
Gastroesophageal reflux disease (GERD) is a common comorbidity in chronic obstructive pulmonary disease (COPD) and has been associated with increased risk of acute exacerbations, hospitalization, emergency room visits, costs, and quality-of-life impairment. However, it remains unclear whether GERD contributes to the progression of COPD as measured by lung function or computed tomography.
Objective
To determine the impact of GERD on longitudinal changes in lung function and radiographic lung disease in the COPDGene cohort.
Methods
We evaluated 5728 participants in the COPDGene cohort who completed Phase I (baseline) and Phase II (5-year follow-up) visits. GERD status was based on participant-reported physician diagnoses. We evaluated associations between GERD and annualized changes in lung function [forced expired volume in 1 s (FEV1) and forced vital capacity (FVC)] and quantitative computed tomography (QCT) metrics of airway disease and emphysema using multivariable regression models. These associations were further evaluated in the setting of GERD treatment with proton-pump inhibitors (PPI) and/or histamine-receptor 2 blockers (H2 blockers).
Results
GERD was reported by 2101 (36.7%) participants at either Phase I and/or Phase II. GERD was not associated with significant differences in slopes of FEV1 (difference of − 2.53 mL/year; 95% confidence interval (CI), − 5.43 to 0.37) or FVC (difference of − 3.05 mL/year; 95% CI, − 7.29 to 1.19), but the odds of rapid FEV1 decline of ≥40 mL/year was higher in those with GERD (adjusted odds ratio (OR) 1.20; 95%CI, 1.07 to 1.35). Participants with GERD had increased progression of QCT-measured air trapping (0.159%/year; 95% CI, 0.054 to 0.264), but not other QCT metrics such as airway wall area/thickness or emphysema. Among those with GERD, use of PPI and/or H2 blockers was associated with faster decline in FEV1 (difference of − 6.61 mL/year; 95% CI, − 11.9 to − 1.36) and FVC (difference of − 9.26 mL/year; 95% CI, − 17.2 to − 1.28).
Conclusions
GERD was associated with faster COPD disease progression as measured by rapid FEV1 decline and QCT-measured air trapping, but not by slopes of lung function. The magnitude of the differences was clinically small, but given the high prevalence of GERD, further investigation is warranted to understand the potential disease-modifying role of GERD in COPD pathogenesis and progression.
Clinical trials registration
Similar content being viewed by others
Introduction
Gastroesophageal reflux disease (GERD) is a common comorbidity in chronic obstructive pulmonary disease (COPD). The prevalence of self-reported GERD in those with COPD is reported to be between 17% [1] to 54% [2] while studies using 24-h pH probe and manometry report prevalence as high as 78% [3]. Pulmonary microaspiration and vagal-mediated reflex bronchoconstriction have been proposed as possible mechanisms by which GERD contributes to COPD outcomes [4, 5]. Cross-sectional studies have consistently shown that, compared to COPD patients without GERD, those with GERD experience more frequent acute exacerbations [6,7,8,9], more hospitalizations and emergency room visits [2, 10,11,12,13,14], higher healthcare costs [15], and worse quality-of-life [12, 16]. However, it remains unclear whether GERD contributes to COPD pathogenesis and progression as measured by lung function or quantitative computed tomography (QCT) [17].
Cross-sectional studies that evaluated the relationship between GERD and lung function have revealed conflicting results – some studies observed worse airflow obstruction [2, 18, 19] in those with GERD, while other studies showed no significant relationship between GERD and lung function [12, 20,21,22]. Due to the cross-sectional design of these studies, we cannot derive definitive conclusions about the causal associations between GERD and COPD disease progression. Therefore, to evaluate if GERD is associated with COPD disease progression as measured by lung function or quantitative chest imaging, we analyzed the data from a large, longitudinal, multicenter cohort study. To our knowledge, this is the first study to longitudinally assess both lung function and quantitative chest imaging over a five-year period to evaluate the association between GERD and COPD disease progression.
Methods
Patient selection
COPDGene (ClinicalTrials.gov Registration # NCT00608764) is an ongoing multicenter, longitudinal study designed to investigate the genetic and epidemiologic characteristics of smoking-related lung disease. A complete description of the protocol has been published previously [18]. Briefly, the primary inclusion criteria are: self-identified racial/ethnic category of non-Hispanic white or African-American, 45–80 years old, with a minimum of 10 pack-year smoking history (except for a small number of non-smoking controls). For the current analysis, we selected from the full cohort of 10,720 enrolled participants and included participants who were former or current smokers and completed both baseline (Phase I, 2008–2011) and 5-year follow-up (Phase II, 2012–2016) study visits. The research protocol was approved by the institutional review board at each participating institution and all participants provided written informed consent.
Diagnosis of GERD
Our primary predictor variable was the presence or absence of GERD. Standardized medical history and medication inventories were administered by research staff. GERD diagnosis was assessed by asking participants, “Have you ever been told by a physician that you have gastroesophageal reflux?” [16, 19]. To obtain an accurate medication list, participants were instructed to bring all current medications to the study visit. All medications were captured on the medications questionnaire, including GERD-related medications such as proton-pump inhibitors (PPI) and histamine receptor-2 blockers (H2 blockers).
Lung function
Our primary outcome variable was rate of lung function decline, as assessed by post-bronchodilator spirometry. Participants underwent spirometry (EasyOne™ spirometer; ndd, Andover, MA) before and after administration of 180 μg of albuterol (via Aerochamber Activis, Parsippany, NJ) at Phase I and Phase II. Percent predicted and lower limit of normal (LLN) values were obtained using National Health and Nutrition Examination III reference equations for spirometry [20]. COPD severity was assessed using spirometry criteria outlined by the Global Initiative for Obstructive Lung Disease (GOLD) guidelines [21]. GOLD 0, defined as forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) ≥0.7 and an FEV1 < 80% predicted in current or former smokers without COPD, is not currently included in the GOLD guidelines, but was used previously [22]. Preserved ratio and impaired spirometry (PRISm) was defined as a post-bronchodilator FEV1/FVC ≥0.7 and an FEV1 > 80% predicted in former or current smokers [23, 24]. Rates of FEV1 and FVC changes per year were calculated by dividing the differences between Phase I and Phase II by the number of years between visits.
Quantitative computed tomography (QCT) imaging measurements
Our secondary outcomes were QCT-based measures of lung disease. Participants included in this analysis had high-resolution CT scans at full inspiration at Phase I and Phase II to assess emphysema and airway disease. Quantitative imaging analysis were performed using VIDA (VIDA Diagnostics, Iowa City, IA; http://www.vidadiagnostics.com) software and Thirona (https://thirona.eu/) software. QCT outcomes included airway wall thickness (AWT)-Pi10 (square root of the wall area of a theoretical airway of 10 mm luminal perimeter), airway wall area (100 X wall area/total bronchial area), air trapping (percent of lung with attenuation values less than − 856 HU on expiratory CT) [25], emphysema (percent of voxels on inspiratory CT with attenuation values less than − 950 Hounsfield Units (HU), and Perc15 lung density (the 15th percentile point defined as the HU below which the 15% of voxels with the lowest density are distributed, adjusted for CT-based lung volumes) [26]. Rates of QCT imaging measurement changes per year were calculated by dividing the differences between Phase I and Phase II by the number of years between visits.
Statistical analysis
Demographic, clinical, and lung health characteristics were compared between those with and without GERD using descriptive statistics. GERD was assessed identically at the Phase I and Phase II visits, and in our primary analysis, we categorized those with GERD as reporting GERD at either visit and compared outcomes to those with no GERD at either visit. Associations between GERD and longitudinal changes in spirometry and QCT chest measurements were assessed using linear regression models with sandwich standard errors. We present the outcome data using three models: Model 1 is unadjusted; Model 2 covariates included age, sex, race, whether the patient smoked between Phase I and Phase II, body mass index (BMI), clinical center, and FEV1% predicted at Phase I; and Model 3 included covariates in Model 2 and whether or not the patient had ≥1 acute exacerbation of COPD between Phase I and Phase II.
Secondary analyses compared changes in spirometry between [1] those with ‘persistent GERD’ (GERD at both Phase I and Phase II) vs. no GERD at either visit, [2] those with ‘incident GERD’ (no GERD at Phase I, but GERD at Phase II) vs. no GERD, and [3] those with ‘resolved GERD’ (GERD at Phase I, but not Phase II) vs. no GERD. Adjustments were made for the same covariates as Model 3 in the primary analyses. Additionally, logistic regression models were used to estimate the odds of having rapid FEV1 decline (defined as FEV1 decline of ≥40 mL/year) for those with vs. without GERD after adjustment for the same covariates. Lastly, we explored associations between GERD treatment (PPI and/or H2 blocker at Phase I and/or Phase II) and changes in lung function using linear regression models.
Results
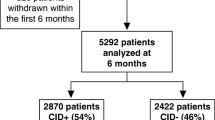
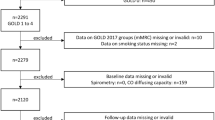
Data were available for 5728/10,720 (53.4%) participants who were former or current smokers and completed both Phase I (baseline, 2008–2011) and Phase II (5-year follow-up, 2012–2016) study visits (Supplemental Fig. 1S). Physician-diagnosed GERD was reported in 2101/5728 (36.7%) participants at either Phase I and/or Phase II (Table 1). Those with GERD were more frequently female (55.6% vs. 45.9%), GOLD stages ≥2 (38.0% vs. 28.3%), and prescribed inhaled therapies (43.5% vs. 26.1%). In addition, participants with GERD were more likely to have experienced acute exacerbations of COPD (26.8% vs. 13.8%) and severe exacerbations of COPD (12.1% vs. 6.9%), worse SGRQ total score (median of 25 vs. 14), and more dyspnea as assessed by mMRC score ≥ 2 (45.3% vs. 30.0%). Cohort characteristics at Phase I comparing those with (n = 4031) and without (n = 1697) available QCT measurements at both visits are provided in the Supplemental Table 1S.
Compared to participants without GERD, participants with GERD at Phase I and/or Phase II had faster decline in FEV1 (difference of − 3.64 mL/year, 95% confidence interval (CI), − 6.56 to − 0.73) and FVC (difference of − 4.26 mL/year; 95% CI, − 8.52 to − 0.004), after adjustment for age, sex, race, smoking, BMI, clinic center, and FEV1% predicted (Table 2). When additionally adjusted for acute exacerbations, the estimates were attenuated and no longer statistically significant, with 95% confidence interval bounds crossing zero. Participants with GERD showed faster progression of air trapping (difference of 0.159%/year; 95% CI, 0.054–0.264) on QCT. We observed no association between the rate of change of AWT-Pi10 (μm/year), airway wall area (%/year), emphysema (%/year), Perc15 lung density (HU/year), and GERD status.
In secondary analyses, ‘incident GERD’ (Phase I = ‘no’, Phase II = ‘yes’) was associated with faster decline in FEV1 and FVC compared to ‘any GERD’ (Phase I = ‘yes’ and/or Phase II = ‘yes’), ‘persistent GERD’ (Phase I = ‘yes’ and Phase II = ‘yes’), and ‘resolved GERD’ (Phase I = ‘yes’ and Phase II = ‘no’) (Table 3). The odds of rapid FEV1 decline (n = 2572) was significantly increased for those reporting ‘any GERD’ (adjusted odds ratio [aOR]: 1.20; 95% CI, 1.07 to 1.35), ‘persistent GERD’ (aOR: 1.23; 95% CI, 1.06 to 1.43), and ‘incident GERD’ (aOR: 1.33; 95% CI, 1.11 to 1.60); the only participants that did not have an increased odds of rapid decline was the ‘resolved GERD’ (aOR: 1.01; 95% CI, 0.82 to 1.26) group (Table 4).
Among our 5728 study participants, pharmacologic treatment with PPIs was reported by 990 (24%) and H2 blockers by 260 (6.5%), of whom most (81%) reported GERD at either visit, though 19% did not report GERD at either visit. Among those with GERD, treatment with PPI and/or H2 blocker at either Phase I and/or Phase II was associated with faster decline in lung function (Table 5). Among participants with GERD, the decline in both FEV1 (difference of − 6.61; 95% CI, − 11.9 to − 1.36) and FVC (difference of − 9.26; 95% CI, − 17.2 to − 1.28) were faster in those receiving PPI and/or H2 blocker compared to those who are not receiving either medication. Among those without GERD, PPI and/or H2 blocker treatment was not associated with lung function decline, though these estimates had less precision than in those with GERD due to the smaller sample.
No significant differences in the slopes of change of the QCT chest measures was found in those taking PPI and/or H2 blockers compared to those who were not taking medications (Supplemental Table 2S).
Discussion
Data from our large, multicenter, longitudinal cohort suggest that GERD may contribute to progressive loss of lung function and increases in air trapping over time. Although other studies have found cross-sectional associations between GERD and lung health, to our knowledge, our study is the first to use a longitudinal study design over a five-year period and assess both lung function and quantitative imaging measurements.
Despite several statistically significant associations between GERD and longitudinal changes in spirometry and QCT measures, we note that the magnitude of the effect sizes were clinically small, with point estimates of 2–5 mL/year faster FEV1 decline among those with GERD. Although this degree of faster lung function decline might not be expected to lead to significant clinical problems, we note that the effect size of cigarette smoking has been estimated at 4–27 mL/year faster decline, so an additional 2–5 mL/year might still contribute to disease progression, in combination with other factors that might contribute to lung function decline such as non-cigarette smoke exposures, respiratory infections, and abnormal inflammatory responses [27, 28]. Although we have little data to guide us in categorizing more significant rates of QCT changes over time, for spirometry, we applied a common definition of rapid FEV1 decline of ≥40 mL/year [29]. In this categorical logistic regression analysis, we saw that GERD was associated with a 20–33% increased odds of rapid decline. Although we must advise caution in interpreting this secondary analysis, these results suggest there might be a subgroup of persons more susceptible to pulmonary effects of GERD, but further research is needed to explore this hypothesis.
We included acute exacerbations as a covariate in our models as episodes of acute exacerbations have been known to accelerate lung function decline [30]. We found that rapid FEV1 decline and progression in QCT-measured air trapping were associated with GERD, but the estimates of slopes of FEV1 and FVC were attenuated compared to the model that did not include acute exacerbations as a covariate.
We evaluated loss of lung function both as continuous variables (mL/year) and as a categorical variable (FEV1 decline ≥40 mL, yes vs. no), then stratified GERD into ‘persistent’, ‘incident’, and ‘resolved.’ Rapid decline in FEV1 is a strong predictor of mortality and COPD-related hospitalization [31]. This current study suggests that GERD is an independent predictor of rapid FEV1 decline, using a multivariate logistic regression model controlling for age, sex, race, smoking status, BMI, FEV1% predicted at baseline, and acute exacerbations. Participants with ‘resolved GERD’ do not appear to have increased odds of rapid FEV1 decline raising the question about the potential role of GERD treatment in slowing lung function decline, which will need to be addressed in future clinical trials.
Smaller cross-sectional studies that have evaluated the relationship between lung function severity and GERD have shown mixed results. Mokhlesi et al. [32] found that symptomatic GERD was more prevalent in COPD patients with FEV1 ≤ 50% compared to those with FEV1 > 50% (23% vs. 9%, respectively; p = 0.08), while Rogha et al. [2] showed that patients with GERD have more severe COPD compared to those without GERD (GOLD stage ≥2 or higher: 88% vs. 67%, respectively; p = 0.005) supporting our findings. In contrast, several other studies found no association between lung function and GERD, possibly due to relatively small sample sizes [12, 33,34,35]. Our present study expands the literature on the relationship between lung function and GERD by adding temporal dimension and a larger sample size.
In addition to adding a temporal dimension in the assessment of the impact of GERD in lung function, we also evaluated whether GERD contributes to the progression of small airway disease and emphysema over time using QCT. Small airway obstruction and emphysematous lung destruction reflect abnormalities in lung function [36]. Airway changes using QCT in the context of aspiration have been evaluated previously [37,38,39,40,41,42], but these studies are also limited to small cross-sectional studies. Hiller et al. found that patients with recurrent aspiration of gastric contents had QCT evidence of bronchial wall thickening (95%) and air trapping (44%) [42]. Similarly, Cardasis et al. found increased airway wall thickening on QCT of patients with pathologically-confirmed chronic occult aspiration of whom 96% had diagnosis of GERD [41]. We found that the rate of air trapping progression over 5 years was faster in those with GERD compared to those without GERD. This could represent the development of distal small airway disease as a result of ongoing pulmonary micro-aspiration of refluxed gastric material and/or vagally-mediated reflex bronchoconstriction in GERD [4, 5]. However, the slopes of the other QCT measurements of small airway disease (AWT-Pi10 and airway wall area) and emphysema (% emphysema and Perc15 lung density) were not different between those with and without GERD. We hypothesize that air trapping in the setting of GERD is a possible early measurable imaging manifestation of small airway disease, possibly an imaging finding that can be seen prior to the other QCT measurements of small airway disease and emphysema. This hypothesis will need to be addressed in future longitudinal studies.
The association between GERD and lung health bring into question the role of anti-reflux treatment in management of COPD. We observed that pharmacologic treatment with PPI and/or H2 blocker among participants with GERD was associated with an accelerated decline in FEV1 and FVC. Using the same COPDGene cohort, Martinez et al. showed that the use of PPI was associated with improved SGRQ total score, but also increased exacerbations highlighting the possibility of confounding-by-indication [16]. The significant decline in lung function with PPI and/or H2 blocker use in this cohort is also likely due to confounding-by-indication. Xiong et al. suggested that treatment of GERD with PPI in patients with COPD is associated with delayed deterioration of FEV1 after 1-year follow-up [43]. However, several other studies evaluating the efficacy of anti-reflux medications in COPD did not report on the impact of these pharmacologic therapies on lung function [12, 32, 44,45,46]. A limitation to the pharmacologic treatment of GERD is that anti-reflux medications do not target nonacid reflux and weakly acidic reflux. Surgical intervention with fundoplication, on the contrary, impacts both acid and non-acid reflux. Most of the literature on anti-reflux surgery focuses on lung transplant. Although the evidence is conflicting, a systematic review by Robertson et al. suggested that anti-reflux surgery provided benefit in lung function among lung transplant patients [47]. We did not find studies specifically addressing anti-reflux surgery in COPD and lung function. The effects of anti-reflux therapies in COPD outcomes, specifically lung function, are unclear highlighting the need for carefully-designed clinical trials.
Our study has limitations. GERD was based on self-report of a physician diagnosis, not on validated reflux questionnaires, pH monitoring, or esophageal manometry. Therefore, GERD misclassification might have affected our results. Because this is an observational study, we cannot establish causal inferences.
Conclusion
GERD was associated with faster COPD disease progression as measured by rapid FEV1 decline and QCT-measured air trapping, but not by slopes of lung function. The magnitude of the differences was clinically small, but given the high prevalence of GERD, further investigation is warranted to understand the potential disease-modifying role of GERD in COPD pathogenesis and progression.
Availability of data and materials
The datasets used are available from the corresponding author on reasonable request.
References
Bor S, Kitapcioglu G, Solak ZA, Ertilav M, Erdinc M. Prevalence of gastroesophageal reflux disease in patients with asthma and chronic obstructive pulmonary disease. J Gastroenterol Hepatol. 2010;25:309–13.
Rogha M, Behravesh B, Pourmoghaddas Z. Association of gastroesophageal reflux disease symptoms with exacerbations of chronic obstructive pulmonary disease. J Gastrointestin Liver Dis. 2010;19:253–6.
Kamble NL, Khan NA, Kumar N, Nayak HK, Daga MK. Study of gastro-oesophageal reflux disease in patients with mild-to-moderate chronic obstructive pulmonary disease in India. Respirology. 2013;18:463–7.
Harding SM. Gastroesophageal reflux and asthma: insight into the association. J Allergy Clin Immunol. 1999;104:251–9.
Canning BJ, Mazzone SB. Reflex mechanisms in gastroesophageal reflux disease and asthma. Am J Med. 2003;115(Suppl 3A):45S–8S.
Sakae TM, Pizzichini MM, Teixeira PJ, Silva RM, Trevisol DJ, Pizzichini E. Exacerbations of COPD and symptoms of gastroesophageal reflux: a systematic review and meta-analysis. J Bras Pneumol. 2013;39:259–71.
Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, Tal-Singer R, Miller B, Lomas DA, Agusti A, Macnee W, Calverley P, Rennard S, Wouters EF, Wedzicha JA, Investigators ECLIPSEE. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363:1128–38.
Busch R, Han MK, Bowler RP, Dransfield MT, Wells JM, Regan EA, Hersh CP, Investigators C. Risk factors for COPD exacerbations in inhaled medication users: the COPDGene study biannual longitudinal follow-up prospective cohort. BMC Pulm Med. 2016;16:28.
Donaldson GC, Wedzicha JA. COPD exacerbations .1: Epidemiology. Thorax. 2006;61:164–8.
Terada K, Muro S, Sato S, Ohara T, Haruna A, Marumo S, Kinose D, Ogawa E, Hoshino Y, Niimi A, Terada T, Mishima M. Impact of gastro-oesophageal reflux disease symptoms on COPD exacerbation. Thorax. 2008;63:951–5.
Liang BM, Feng YL. Association of gastroesophageal reflux disease symptoms with stable chronic obstructive pulmonary disease. Lung. 2012;190:277–82.
Rascon-Aguilar IE, Pamer M, Wludyka P, Cury J, Coultas D, Lambiase LR, Nahman NS, Vega KJ. Role of gastroesophageal reflux symptoms in exacerbations of COPD. Chest. 2006;130:1096–101.
Takada K, Matsumoto S, Kojima E, Iwata S, Okachi S, Ninomiya K, Morioka H, Tanaka K, Enomoto Y. Prospective evaluation of the relationship between acute exacerbations of COPD and gastroesophageal reflux disease diagnosed by questionnaire. Respir Med. 2011;105:1531–6.
Shimizu Y, Dobashi K, Kusano M, Mori M. Different gastoroesophageal reflux symptoms of middle-aged to elderly asthma and chronic obstructive pulmonary disease (COPD) patients. J Clin Biochem Nutr. 2012;50:169–75.
Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235–45.
Martinez CH, Okajima Y, Murray S, Washko GR, Martinez FJ, Silverman EK, Lee JH, Regan EA, Crapo JD, Curtis JL, Hatabu H, Han MK, Investigators C. Impact of self-reported gastroesophageal reflux disease in subjects from COPDGene cohort. Respir Res. 2014;15:62.
Lee AL, Goldstein RS. Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis. 2015;10:1935–49.
Regan EA, Hokanson JE, Murphy JR, Make B, Lynch DA, Beaty TH, Curran-Everett D, Silverman EK, Crapo JD. Genetic epidemiology of COPD (COPDGene) study design. COPD. 2010;7:32–43.
Benson VS, Mullerova H, Vestbo J, Wedzicha JA, Patel A, Hurst JR. Associations between gastro-oesophageal reflux, its management and exacerbations of chronic obstructive pulmonary disease. Respir Med. 2015;109:1147–54.
Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87.
Soriano JB, Lamprecht B, Ramírez AS, Martinez-Camblor P, Kaiser B, Alfageme I, Almagro P, Casanova C, Esteban C, Soler-Cataluña JJ, de-Torres JP, Miravitlles M, Celli BR, Marin JM, Puhan MA, Sobradillo P, Lange P, Sternberg AL, Garcia-Aymerich J, Turner AM, Han MK, Langhammer A, Leivseth L, Bakke P, Johannessen A, Roche N, Sin DD. Mortality prediction in chronic obstructive pulmonary disease comparing the GOLD 2007 and 2011 staging systems: a pooled analysis of individual patient data. Lancet Respir Med. 2015;3:443–50.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS, Committee GS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO global initiative for chronic obstructive lung disease (GOLD) workshop summary. Am J Respir Crit Care Med. 2001;163:1256–76.
Wan ES, Castaldi PJ, Cho MH, Hokanson JE, Regan EA, Make BJ, Beaty TH, Han MK, Curtis JL, Curran-Everett D, Lynch DA, DeMeo DL, Crapo JD, Silverman EK, Investigators C. Epidemiology, genetics, and subtyping of preserved ratio impaired spirometry (PRISm) in COPDGene. Respir Res. 2014;15:89.
Wan ES, Hokanson JE, Murphy JR, Regan EA, Make BJ, Lynch DA, Crapo JD, Silverman EK, Investigators C. Clinical and radiographic predictors of GOLD-unclassified smokers in the COPDGene study. Am J Respir Crit Care Med. 2011;184:57–63.
Schroeder JD, McKenzie AS, Zach JA, Wilson CG, Curran-Everett D, Stinson DS, Newell JD, Lynch DA. Relationships between airflow obstruction and quantitative CT measurements of emphysema, air trapping, and Airways in Subjects with and without Chronic Obstructive Pulmonary Disease. AJR Am J Roentgenol. 2013;201:W460–70.
Parr DG, Dirksen A, Piitulainen E, Deng C, Wencker M, Stockley RA. Exploring the optimum approach to the use of CT densitometry in a randomised placebo-controlled study of augmentation therapy in alpha 1-antitrypsin deficiency. Respir Res. 2009;10:75.
Burrows B, Lebowitz MD, Camilli AE, Knudson RJ. Longitudinal changes in forced expiratory volume in one second in adults. Methodologic considerations and findings in healthy nonsmokers. Am Rev Respir Dis. 1986;133:974–80.
Xu X, Weiss ST, Rijcken B, Schouten JP. Smoking, changes in smoking habits, and rate of decline in FEV1: new insight into gender differences. Eur Respir J. 1994;7:1056–61.
Lange P, Groth S, Nyboe GJ, Mortensen J, Appleyard M, Jensen G, Schnohr P. Effects of smoking and changes in smoking habits on the decline of FEV1. Eur Respir J. 1989;2:811–6.
Dransfield MT, Kunisaki KM, Strand MJ, Anzueto A, Bhatt SP, Bowler RP, Criner GJ, Curtis JL, Hanania NA, Nath H, Putcha N, Roark SE, Wan ES, Washko GR, Wells JM, Wendt CH, Make BJ. Acute exacerbations and lung function loss in smokers with and without chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;195:324–30.
Mannino DM, Reichert MM, Davis KJ. Lung function decline and outcomes in an adult population. Am J Respir Crit Care Med. 2006;173:985–90.
Mokhlesi B, Morris AL, Huang CF, Curcio AJ, Barrett TA, Kamp DW. Increased prevalence of gastroesophageal reflux symptoms in patients with COPD. Chest. 2001;119:1043–8.
Ducoloné A, Vandevenne A, Jouin H, Grob JC, Coumaros D, Meyer C, Burghard G, Methlin G, Hollender L. Gastroesophageal reflux in patients with asthma and chronic bronchitis. Am Rev Respir Dis. 1987;135:327–32.
Lee AL, Button BM, Denehy L, Roberts SJ, Bamford TL, Ellis SJ, Mu FT, Heine RG, Stirling RG, Wilson JW. Proximal and distal gastro-oesophageal reflux in chronic obstructive pulmonary disease and bronchiectasis. Respirology. 2014;19:211–7.
Niklasson A, Strid H, Simrén M, Engström CP, Björnsson E. Prevalence of gastrointestinal symptoms in patients with chronic obstructive pulmonary disease. Eur J Gastroenterol Hepatol. 2008;20:335–41.
Hogg JC, Macklem PT, Thurlbeck WM. Site and nature of airway obstruction in chronic obstructive lung disease. N Engl J Med. 1968;278:1355–60.
Butler SG, Clark H, Baginski SG, Todd JT, Lintzenich C, Leng X. Computed tomography pulmonary findings in healthy older adult aspirators versus nonaspirators. Laryngoscope. 2014;124:494–7.
Scheeren B, Marchiori E, Pereira J, Meirelles G, Alves G, Hochhegger B. Pulmonary computed tomography findings in patients with chronic aspiration detected by videofluoroscopic swallowing study. Br J Radiol. 2016;89:20160004.
Makharia GK, Seith A, Sharma SK, Sinha A, Goswami P, Aggarwal A, Puri K, Sreenivas V. Structural and functional abnormalities in lungs in patients with achalasia. Neurogastroenterol Motil. 2009;21:603–8 e620.
Matsumoto H, Niimi A, Tabuena RP, Takemura M, Ueda T, Yamaguchi M, Matsuoka H, Jinnai M, Chin K, Mishima M. Airway wall thickening in patients with cough variant asthma and nonasthmatic chronic cough. Chest. 2007;131:1042–9.
Cardasis JJ, MacMahon H, Husain AN. The spectrum of lung disease due to chronic occult aspiration. Ann Am Thorac Soc. 2014;11:865–73.
Hiller N, Simanovsky N, Bahagon C, Bogot N, Maayan C. Chest computed tomography findings in familial dysautonomia patients: a model for aspiration. Isr Med Assoc J. 2009;11:393–7.
Xiong W, Zhang QS, Zhao W, Ding W, Liu JM, Zhao YF. A 12-month follow-up study on the preventive effect of oral lansoprazole on acute exacerbation of chronic obstructive pulmonary disease. Int J Exp Pathol. 2016;97:107–13.
Kempainen RR, Savik K, Whelan TP, Dunitz JM, Herrington CS, Billings JL. High prevalence of proximal and distal gastroesophageal reflux disease in advanced COPD. Chest. 2007;131:1666–71.
Eryuksel E, Dogan M, Olgun S, Kocak I, Celikel T. Incidence and treatment results of laryngopharyngeal reflux in chronic obstructive pulmonary disease. Eur Arch Otorhinolaryngol. 2009;266:1267–71.
Ingebrigtsen TS, Marott JL, Vestbo J, Nordestgaard BG, Hallas J, Lange P. Gastro-esophageal reflux disease and exacerbations in chronic obstructive pulmonary disease. Respirology. 2015;20:101–7.
Robertson AG, Ward C, Pearson JP, Corris PA, Dark JH, Griffin SM. Lung transplantation, gastroesophageal reflux, and fundoplication. Ann Thorac Surg. 2010;89:653–60.
Acknowledgements
We thank the participants and the investigators who have participated in the COPDGene study. We also thank Michael Jacobs, MD, PharmD and his Temple Pharmacy students for obtaining and organizing all the medications of the participants in the COPDGene. This material is the result of work supported by and conducted at the Minneapolis VA Health Care System.
Funding sources
This work was supported by NIH National Heart, Lung, and Blood Institute (NHLBI) grants U01 HL089897 and U01 HL089856, and NIH NCATS grant UL1TR002494. The COPDGene study (NCT00608764) is also supported by the COPD Foundation through contributions made to an Industry Advisory Committee comprised of AstraZeneca, Boehringer-Ingelheim, GlaxoSmithKline, Novartis, and Sunovion.
Disclaimer
The views expressed in this article are those of the authors and do not reflect the views of the United States Government, the Department of Veterans Affairs, the funders, the sponsors, or any of the author’s affiliated academic institution.
This research was also supported by the National Institutes of Health’s (NIH) National Center for Advancing Translational Sciences (NCATS), grant UL1TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH NCATS.
Author information
Authors and Affiliations
Consortia
Contributions
Designed the analysis: AKB, KMK, CHW, AP. Performed the statistical analysis: AP. Drafted the manuscript: AKB, KMK. Provided critical input and revised the manuscript for important intellectual content and approved the final manuscript: All. Take responsibility for the integrity of the data and the accuracy of the data analysis: All.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board (IRB) approval was obtained at each of the participating study centers prior to study initiation. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
Dr. Kunisaki has previously served as a consultant to GlaxoSmithKline in 2018. The other authors declare that they have no conflict of interests related to this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file: Supplemental Figure 1S.
Participant flow diagram. Supplemental Table 1S. Cohort characteristics at Phase I by availability of quantitative CT (QCT) measurements at both visits. Supplemental Table 2S. Multivariable linear regression models of the association between treatment with proton pump inhibitor (PPI) and/or H2 blocker (n = 960) and slopes of quantitative CT (QCT) measures of lung disease among those with gastroesophageal reflux disease (GERD).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baldomero, A.K., Wendt, C.H., Petersen, A. et al. Impact of gastroesophageal reflux on longitudinal lung function and quantitative computed tomography in the COPDGene cohort. Respir Res 21, 203 (2020). https://doi.org/10.1186/s12931-020-01469-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-020-01469-y