Abstract
Background
The low toxicity of perfluorocarbons (PFCs), their high affinity for respiratory gases and their compatibility with lung surfactant have made them useful candidates for treating respiratory diseases such as adult respiratory distress syndrome. We report results for treating acute allergic and non-allergic bronchoconstriction in sheep using S-1226 (a gas mixture containing carbon dioxide and small volumes of nebulized perflubron). The carbon dioxide, which is highly soluble in perflubron, was used to relax airway smooth muscle.
Methods
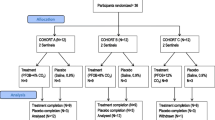
Sheep previously sensitized to house dust mite (HDM) were challenged with HDM aerosols to induce early asthmatic responses. At the maximal responses (characterised by an increase in lung resistance), the sheep were either not treated or treated with one of the following; nebulized S-1226 (perflubron + 12% CO2), nebulized perflubron + medical air, 12% CO2, salbutamol or medical air. Lung resistance was monitored for up to 20 minutes after cessation of treatment.
In additional naïve sheep, a segmental bronchus was pre-contracted with methacholine (MCh) and treated with nebulized S-1226 administered via a bronchoscope catheter. Subsequent bronchodilatation was monitored by real time digital video recording.
Results
Treatment with S-1226 for 2 minutes following HDM challenge resulted in a more rapid, more profound and more prolonged decline in lung resistance compared with the other treatment interventions. Video bronchoscopy showed an immediate and complete (within 5 seconds) re-opening of MCh-constricted airways following treatment with S-1226.
Conclusions
S-1226 is a potent and rapid formulation for re-opening constricted airways. Its mechanism(s) of action are unknown. The formulation has potential as a rescue treatment for acute severe asthma.
Similar content being viewed by others
Background
Asthma is a common chronic disorder characterized by airway hyper-responsiveness, bronchial smooth muscle hypertrophy, increased mucus secretion, and airway inflammation [1],[2] on a background of airway wall remodelling and mucous plugs [3],[4]. Asthma is triggered by many factors such as allergens (e.g., pollen, pet dander), irritants (e.g., smoke), drugs, cold, exercise [5], and upper respiratory tract infections [6]. Based on recent trends, the worldwide prevalence of asthma may increase from 300 million individuals currently to 400 million individuals by 2025 [7]. Healthcare costs of asthma are considered to be among the highest associated with chronic disease [8],[9]. In Canada, 59% of asthma patients treated in general practice are estimated to have uncontrolled disease [10]. Inhaled short acting β2-agonists represent the most common front-line emergency department treatment for acute exacerbations due to their well-known rapid bronchodilatory effect [11]–[13] β2-agonists, while generally considered safe may have significant side effects [14] and approximately one fifth to one third of patients do not respond to front-line treatment with short acting β2-agonists and ultimately require hospitalisation [15]. Furthermore, a clinically significant proportion of asthma patients are refractory to conventional treatments, posing a challenge for their management [16]. A new class of bronchodilators working through a different mechanism would be a useful addition for treating acute asthma.
In acute severe asthma, conventional treatment with inhaled β2 agonists may no longer be effective [11]–[13], as the therapeutic aerosol may be unable to penetrate airways obstructed by mucous plugs [4], increasing the risk of sudden death [17]. Emergency treatment for asthma includes mechanical ventilation [15] which may cause injury (barotrauma) to the ventilated segments of the lung [18]. Hence, a rapid non-invasive treatment for severe, life-threatening asthma is needed.
Inhaled carbon dioxide is a known bronchodilator for many mammalian species [19]. Hypercapnia has long been known to relax airway smooth muscle in vitro [20],[21], whereas hypocapnia causes airway smooth muscle contraction [22]. Hyperventilation is a well known trigger of asthma [23]. Studies by Fisher et al. [24] and Mc Fadden et al. [25] indicate that low alveolar PCO2 (PACO2) may be associated with an increase in airway tone in asthmatic patients. By contrast hypercapnia (induced by a short circuiting CO2 absorber) has been shown to reduce airway resistance in both healthy and asthmatic subjects [26]. Finally a study reported by Fisher and Hansen [27] showed that inhalation of 6% CO2 over 4–5 minutes relieved exercise induced airflow obstruction in young atopic asthmatics at rest and during exercise.
Perfluorooctylbromide (perflubron) is a chemically inert perfluorocarbon (PFC). It has a high solubility for respiratory gases such as CO2 and O2 and a low surface tension compatible with endogenous airway surfactant [28]–[30]. It has been used in total and partial liquid ventilation studies for treatment of ARDS [28]. In addition, perflubron has been shown to reduce pulmonary inflammation and injury through a variety of actions [28],[31]–[33]. The high density and low surface tension of perflubron should also facilitate the penetration of obstructed airways and re-expansion of collapsed lung [34].
There are no reported studies of PFC use in asthma. However, its properties of gas transport for CO2 and O2, low interfacial tension at the PFC-mucus interface, low toxicity and anti-inflammatory properties [31]–[33],[35] make it a good candidate as a rescue therapy in life threatening acute asthma. Recently perflubron aerosols have been used to successfully treat acute lung injury in an animal model [36],[37].
The major challenge for treating acute severe asthma is to open constricted airways rapidly enough to allow delivery of conventional medication to the diseased airways.
In this study we show that inhaled nebulized perflubron + CO2 (S-1226) rapidly opens constricted airways in an ovine model of allergic asthma using house dust mite as allergen [38],[39].
Methods
Experimental sheep
Female merino-cross farm-reared sheep aged 6 months were used in the experiments described here. After the sensitisation procedures (described below), sheep were transported to Animal House Facility at Veterinary Science, Parkville, Australia where they were kept in indoor pens for all the procedures described in this report. On arrival at the Animal House Facility all sheep were treated with an antihelminthic to ensure that they were parasite-free.
All experimental protocols used in this study were approved by the Animal Experimentation Ethics Committee at the University of Melbourne.
Drug source
Acetyl-β-methylcholine chloride (MCh) was from Sigma-Aldrich, Stenhein, Germany and salbutamol sulphate solution was purchased from GSK Pty Ltd Australia. Gas mixture (12% CO2 + 21% O2+ balance N2) was from CIG Pty Ltd Australia.
Characterization of nebulized perflubron
Characterization of perflubron delivered by the Sidestream nebulizer was conducted under cGMP conditions at SolAero Ltd laboratory. Methods to characterize perflubron aerosol were adapted from regulatory methods embodied in the European Nebulizer Standard [40]. The unique nature of perflubron required adaptation of methods including incorporation of trace quantities (5%) of a perflubron compatible non-volatile PFC which could be assayed gravimetrically to determine both aerosol output as well as particle size distributions. Aerosol output was determined using a breath simulation (500 mL at 15 cycles per minute) and collecting released aerosol representing the `inhaled aerosol’ on a pre-weighed 3M electrostatic filter, subsequently allowing volatile perflubron to dissipate and quantitatively weighing the non-volatile PFC component. The residual weight gain was then used to back calculate the original amount of deposited aerosol. Pre- and Post- weights of nebulizers provided the gross perflubron emitted, from which the analyzed aerosol proportion could be subtracted to estimate the proportion of perflubron in the vapor phase. Aerosol size was determined using a Marple 298X cascade impactor equipped with pre-weighed GF/A filters from which the non-volatile aerosol residue was similarly gravimetrically determined to quantify size fractions.
House dust mite (HDM) sensitization and airway challenges
Sheep 6 months of age were subcutaneously sensitized with 50 μg house dust mite (HDM) extract (Dermatophagoides pteronyssinus; CSL Ltd, Parkville, VIC, Australia) mixed 1:1 in aluminum hydroxide [Al(OH)3] adjuvant. Injections of 1 mL HDM / Al(OH)3 were given on three occasions at 2 week intervals [38]. Levels of HDM-specific IgE (IgE-HDM) were determined by enzyme-linked immunosorbent assay (ELISA) of serum samples obtained from animals immediately prior to, and 7 days after, HDM sensitization [38],[41]. Sheep were only selected for use in the study if they had increased levels of HDM-specific IgE (IgE-HDM) ≥2-fold above pre-sensitization values.
To induce pulmonary sensitization to HDM, all sheep were given three inhalation challenges of aerosolised HDM (1 mg/ml in 5 mL of phosphate buffered saline). Lung function was recorded for one hour directly after the aerosol HDM challenge. HDM aerosols were generated with a medical nebulizer (Vitalair RapidNeb, Allersearch, Vermont, Australia). The nebulizer was connected to a dosimeter system consisting of a solenoid valve and a source of compressed air (20 psi). The output of the nebulizers was directed into a T-piece with one arm connected to the inspiratory port of a mechanical ventilator (Intermed Bear 2 – Adult Volume Ventilator, Bear Medical Systems, Inc., Riverside, CA). HDM challenges were delivered at a tidal volume of 500 mL and a rate of 20 breaths per minute for 10 minutes.
Measurement of lung function
Data on lung function were obtained from all sheep using established techniques [42]. Briefly, pressures and flow were acquired from conscious unsedated sheep using a National Instruments Data Acquisition (DAQ) system with a Virtual Instrument programmed with Lab View® (National Instruments, Austin, USA). The sheep were restrained in a body sheath and head restraining harness tethered to a custom-made animal trolley. To measure oesophageal pressures, a balloon pressure catheter was advanced through one nostril into the lower esophagus. To assess tracheal pressures throughout the respiratory cycle a cuffed endotracheal tube was placed into the trachea and then a side-hole catheter was advanced 2 cm past the distal end of the endotracheal tube. The oesophageal and tracheal catheters were connected to differential transducers (Gaeltec 8 T, Gaeltec Ltd, Dunvegan, Scotland) to measure oesophageal pressure (Poes) and airway pressures (Paw) respectively. Transpulmonary pressure (Pl) was obtained from Poes with respect to Paw. Airflow was measured via a pneumotachograph (Hans Rudolph Inc, Kansas City, USA) attached to the proximal end of the endotracheal tube. Calibration and synchronization of the gas transducers and pneumotachograph were performed as described previously [43],[44]. Lung dynamics were determined by a modified Mead-Whittenberger method [45]. Breath by breath analysis of flow and pleural pressure (Ppl) was used to determine lung resistance (RL) from an average of five breaths. Data from breaths which differed by more than 20% in volume and more than 10% of the breathing rate were rejected. Acquisition and detailed analysis of pulmonary physiological data were performed on customized Lab View software developed by Koumoundouros et al. [42].
Treatment delivery
Treatments with nebulized S-1226, nebulized perflubron and nebulized salbutamol were generated with a Sidestream® nebulizer (Philips Respironics). The nebulizer was connected to a dosimeter system consisting of a solenoid valve and a source of compressed (20 psi driving pressure) gas mixture (12% CO2, 21% O2 and 67% N2) for S-1226 or compressed medical air (21% O2 and 79% N2) for perflubron and salbutamol. Treatments were delivered at a tidal volume of 500 mL and a rate of 20 breaths per minute for 2 minutes. Treatments with CO2 alone and medical air were performed following the same protocol but with an empty nebulizer.
HDM challenge followed by treatment
Sheep (previously HDM sensitized) were challenged with HDM aerosols to induce early phase asthmatic responses. At the peak of these responses (characterised by an increase in lung resistance), the sheep were treated for two minutes with one of six treatment groups listed below. Lung resistance was monitored up to 20 minutes following cessation of treatment.
1- S-1226: Nebulized perfluorooctylbromide (perflubron) generated using a Sidestream® nebulizer (Philips Respironics) and driven by a compressed gas mixture containing 12% CO2, 21% O2 and balance N2.
2- CO2 alone: Inhalation of a gas mixture containing 12% CO2, 21% O2 and balance N2.
3- Perflubron: Nebulized perflubron driven by compressed medical air.
4- Salbutamol (1 mg/ml): Nebulized salbutamol driven by compressed medical air.
5- Medical air: Inhalation of medical air
6- No treatment: room air
Video bronchoscopy
An unsensitised sheep was used in separate experiments to visually assess the airway response to inhaled S-1226. Real time video recordings were taken with a bronchoscope digital camera following methacholine challenge. To insure that the same airway was recorded throughout the procedure, the upper region of the airway was tattooed by injecting tissue dye using a transbronchial needle. The airway was then pre-contracted with an aerosol of methacholine (MCh) delivered via a Trudell Ltd Pty bronchoscope catheter, inserted into the biopsy port of the bronchoscope. Doubling doses of methacholine were nebulized directly into the lung segment (0.009, 0.018, 0.037 w/v) for 30 seconds with a 2 minute interval between methacholine doses until the airway was maximally constricted. The airway was then treated with nebulized S-1226 delivered through a Trudell Pty Ltd bronchoscope catheter and the effects video recorded in real time. If the airway re-constricted, second and third treatments were administered.
Data analysis
In each experiment several intervals were analysed: Baseline, HDM-induced early phase response, and three post-treatment periods (immediately, 1–10 minute and 10 to 20 minutes after treatment cessation). Means were calculated for each interval and treatment effect was expressed as percent decline of lung resistance.
Analysis of variance (ANOVA) was performed over each time interval to determine if any of the treatment groups performed better than any other. A two tailed Dunnett’s post-hoc test was performed. This involved separate analyses addressing two distinct questions. The first: is S-1226 superior to no treatment, medical air (negative control) or salbutamol (positive control). Secondly to determine which component of S-1226, CO2 or perflubron contributed greater to its efficacy. Tests were performed using GraphPad Prism version 5.00 and R version 3.1.1 for windows. A p-value ≤ 0.05 was considered significant.
Results and discussion
Characterization of nebulized perflubron
Results from characterization of nebulized perflubron are summarized in Table 1. The mean rate of perflubron delivered was 598 mg/minute, of which some 203 mg/minute consisted of aerosol with the remaining 395 mg/minute was estimated to be in vapor form - thus the majority (approximately 2/3 of the nebulized perflubron) was delivered in vapor form. The perflubron which was delivered in aerosol form demonstrated a relatively small particle size distribution, with a Mass Median Aerodynamic Diameter (MMAD) of 1.1 um, with a Geometric Standard Deviation (GSD) of 2.5 (Table 1). The perflubron aerosol size distributions obtained from the Sidestream nebulizer are shown in Figure 1.
Sidestream nebulizer aerosol size distribution. Aerosol size is on the X-axis is plotted against the normative and cumulative underside aerosol distributions. The blue boxes profile the normative size distribution of nebulized perflubron, the near symmetry suggests a log-normal distribution of aerosol particles. The red squares plot the same data but as a cumulative size distribution of particle size against cumulative undersize %. The cumulative size distribution is used to interpolate the MMAD as the particle size at 50% of the cumulative mass – in this case the MMAD is 1.1 um. The Geometric Standard Deviation (GSD) of the MMAD is calculated using the intercepts at 15.8% and 84.1% (approximated by grey lines in Figure) using the formula GSD = sq rt (size 84.1um / size 15.8 um).
The characterization of nebulized perflubron demonstrated that the majority of the nebulized perflubron existed in the vapor form while the remaining proportion of aerosol existed as a relatively fine aerosol with an MMAD of 1.1 um. We infer that perflubron as vapor and aerosol, as well as CO2 gas component of inhaled S-1226, would rapidly distribute throughout the respiratory tract.
HDM challenge followed by treatment
Sensitized and HDM challenged sheep treated with S-1226 for 2 minutes during the peak of the early phase allergic response showed an immediate decline in lung resistance in all animals following HDM challenge (Figure 2).
Effect of S-1226 on lung resistance in the sheep model of asthma. Changes in lung resistance following treatment with S-1226 in 9 different sheep. The treatment was delivered for 2 minutes and lung resistance was measured immediately, and at 1–10 minutes and 10–20 minutes after treatment cessation. All nine sheep showed an immediate and sustained decline in lung resistance following S-1226 treatment given at the peak of the early phase response to inhaled allergen (HDM).
Treatment with S-1226 compared to the other arms of the study are shown in Figure 3. Lung resistance declined by 50.1% ± 5.5, 47.2% ± 6.2 and 51.8% ± 8.3 (mean ± SE) immediately, 1 to 10 minutes and 10 to 20 minutes after treatment with S-1226 respectively. Treatment with 12% CO2 resulted in declines in lung resistance of 36.9% ± 6.8, 20.6% ± 12.0 and 24.3% ± 28.4 (mean ± SE) immediately, 1 to 10 minutes and 10 to 20 minutes after treatment respectively. Treatment with perflubron + medical air resulted in declines in lung resistance of 24.8% ± 7.5, -1.3% ± 10.7 and -7.2% ± 5.1 (mean ± SE) immediately, 1 to 10 minutes and 10 to 20 minutes after treatment respectively. Treatment with salbutamol resulted in declines in lung resistance of 31.3% ± 6.8, 15.3% ± 7.1 and 14.3% ± 9.6 (mean ± SE) immediately, 1 to 10 minutes and 10 to 20 minutes after treatment respectively. Following inhalation of medical air, lung resistance declined by 23.1% ± 9.7, 16.0% ± 10.8 and 13.1% ± 17.5 (mean ± SE) immediately, 1 to 10 minutes and 10 to 20 minutes after treatment respectively. Lung resistance measured following HDM challenge with no treatment decreased by 1.9% ± 4.7, 24.4% ± 4.2 (mean ± SE) at 1 to 10 minutes and 10 to 20 minutes after treatment respectively.
Comparison between S-1226 and other bronchodilators in the sheep model of asthma. This figure shows the % decline in lung resistance following treatment with S-1226, 12% CO2, perflubron, salbutamol, medical air or no treatment in HDM challenged sheep. Measurements were taken immediately, 1–10 minutes and 10–20 minutes after treatment. Treatment with S-1226 showed significant and sustained declines in lung resistance compared to medical air or no treatment. In addition S-1226 showed a significantly greater decline in lung resistance compared to salbutamol. P-values show significant difference from S-1226; *p <0.05, # p ≤ 0.01.
Inhalation of nebulized S-1226 caused a rapid and sustained decrease in lung resistance during the early phase asthmatic response which was significantly greater than no treatment at 1–10 minutes (p = 0.002) and significantly greater than medical air immediately, 1–10 minutes and 10–20 minutes after treatment (p = 0.027, 0.018 and 0.039 respectively). The effect of S-1226 was significantly greater than salbutamol 1–10 minutes and 10–20 minutes after treatment (p = 0.025 and 0.046 respectively). S-1226 showed a significantly greater decline in lung resistance than perflubron alone immediately, 1–10 minutes and 10–20 minutes after treatment (p = 0.019, 0.002 and 0.012 respectively). Finally, the effect of S-1226 was stronger but not significantly different from CO2 alone immediately, 1–10 minutes and 10–20 minutes after treatment (p = 0.329, 0.124 and 0.319 respectively). The CO2 decline in lung resistance appeared shorter-lasting than the decline observed with S-1226.
Video-bronchoscopy of S-1226 treatment following MCh challenge
The rapidity of the effect was demonstrated by video-bronchoscopy. MCh challenge resulted in rapid constriction of the segmental and subsegmental bronchi. Without treatment the airway narrowing lasted for at least 20 minutes before a slow natural recovery. Following treatment with a spray of S-1226 there was an immediate re-opening (within 5 seconds) of the MCh-constricted airway (Figure 4). A video recording of this treatment effect can be viewed online under Additional file 1. The effect was sustained during the delivery of S-1226 and up to 1 minute after treatment cessation. After that the airway began to re-constrict. Second and third treatments with S-1226 had identical effects.
Video bronchoscopy of the effect of S-1226. Bronchoscopic still images of sheep airways pre and post MCh and seconds after initiating treatment with nebulized S-1226 (arrow heads indicate tissue dye). The video presentation is available online under Additional file 1.
Potential mechanisms of action
Our study did not attempt to determine the mechanism of action of S-1226. The bronchodilatory effect of CO2 has been demonstrated in many mammalian species including cats, rats dogs [19],[22] as well as sheep and humans However, the literature indicates that it might operate through several distinct mechanisms.
The first mechanism is through a direct physiologic relaxant effect of CO2 on airway smooth muscle [20]–[22]. The way(s) in which CO2 regulates bronchial smooth muscle tone is not fully understood. Recent in vitro data indicates that part of this effect is mediated by pH dependent and part by pH independent but epithelium dependent mechanisms [22]. Studies in vivo indicate the response (in rats) to inhaled CO2 does not require adrenergic pathways [46]. Fisher and Hansen [27] showed in their study of exercise induced asthma that cholinergic pathways were not involved in the bronchodilatory effects of inhaled CO2. Bronchodilator drugs that use β- adrenergic and cholinergic pathways form the current basis for treating obstructive lung disease.
Inhaled carbon dioxide (5, 10 and 15%) has been shown to reduce total lung resistance induced by intravenous histamine, acetylcholine and serotonin in dogs, cats and rats [19]. Inhaled CO2 has also been shown to reduce total lung resistance induced by pulmonary artery occlusion in cats and dogs [19]. All species studied responded to CO2 but there were small differences in response to the different broncho-constricting agents between species.
Studies by Ingram and colleagues [47] suggest that the bronchodilatory effect of CO2 may be independent of blood PCO2. They studied the effect of varying airway and arterial PCO2 on airway tone in dogs. They showed that low airway PCO2 combined with high arterial PCO2 resulted in a large increase in airway resistance [47]. These findings indicate that CO2 may have unique properties when delivered through the airways and supports the previously cited in vitro work that airway epithelium plays a part in the relaxant response [22]. Finally the rapidity of the response as seen in the sheep video indicates that neural mechanisms are involved. The non-adrenergic-non cholinergic (NANC) pathways are the best candidates for this effect. The NANC system has both broncho-constrictive and bronchodilator components [48]. CO2 alone or S-1226 may activate the bronchodilatory pathways or inhibit the broncho-constrictive pathways. Further work is required to address these questions.
The second mechanism may enhance delivery of CO2 to the airways. It could do this in several ways; first sustained release of CO2 dissolved in perflubron droplets as the droplets evaporate may explain the temporal synergism observed with the combination treatment. Second, because much of S-1226 is in gaseous form, it will be delivered rapidly into obstructed airways by diffusion and possibly through collateral ventilation.
The third mechanism whereby this combination treatment may work is by facilitating penetration and lubrication of mucus plugs, thus enhancing muco-ciliary clearance. We recently reported, using an in vitro system, that mucin plug clearance was significantly enhanced by perflubron [49].
S-1226 may also lower the surface tension in the inflamed airways. It has been shown that the normal airway is lined by a thin film of endogenous surfactant with a low surface tension [50]. This film is important for maintaining small airway patency at low lung volumes [51] and is abnormal in asthma [52],[53].
Finally, carbon dioxide and perfluorocarbons may also be beneficial for their anti-inflammatory properties. Perflubron given in vitro or during partial liquid ventilation exerts an anti-inflammatory effect on alveolar cells [54], decreases white blood cell counts, [54],[55] and the pro-inflammatory cytokines IL-1 and IL-6. Perflubron also increases release of the anti-inflammatory chemokine IL-10 [54].
Strengths and limitations of the animal model
Like with most experimental systems, large animal models of allergic airway disease have both strengths, and also limitations, which need to be recognised when evaluating new therapies for asthma [56]–[58]. For example, clinically efficacious anti-asthma drugs such as leukotriene LTE4 receptor antagonists, cromolyn and corticosteroids have all been successfully tested in the sheep model of asthma [59]. The success of these drugs is in contrast to the testing of platelet activated factor (PAF) antagonist therapies in sheep. PAF antagonists were shown to alleviate allergic airway responses in sheep [60], however the positive outcome with these treatments in sheep did not translate to humans giving negative results in clinical trials [61]. Nevertheless, sheep are an appropriate species to investigate the efficacy of the bronchodilator reported here for a number of important reasons. Firstly, the sheep respiratory system is at least comparable to the human system with respect to lung size, lung anatomy and morphology, and the pharmacological and physiological parameters of the ovine lung [57]–[59]. Pertinent to this study, as the mechanism of the bronchodilator most likely involves both the airway smooth muscle and the intact airway epithelium [22], is that the arrangement and morphology of ovine airway epithelium [62] and airway smooth muscle down the tracheo-bronchial tree [57] is functionally similar to that observed in human lungs. Thus, the bronchodilator interactions we report here for the sheep model could reasonably translate to the human lung. The other major asset of the sheep model for examining bronchodilator effectiveness relates to the docile nature of sheep, which allows experiments to be ethically conducted in unsedated and unanaesthetised animals [59],[63]. These anaesthetic and/or sedation agents, if administered as is necessary for behavioural reasons in most other animal species modeling asthma, may otherwise dampen, and thus mask, the bronchodilator responses.
In summary, we provide evidence that treatment with inhaled S-1226 delivered as an aerosol/gas mixture may play an important role in the treatment of acute asthma attacks. We show that perflubron combined with 12% CO2 is a potent airway smooth muscle relaxant in this ovine model of allergic asthma. The response to the combination treatment was rapid and exceeded treatment with medical air (negative control) and salbutamol (positive control) in both amplitude and temporal components. Further work is required to fully evaluate the mechanism(s) of action of this novel therapy.
Authors’ contributions
Conception and Design: TE, KS, FG, RL. Sheep experiments were conducted by TE, KS, PC, EK and JV. Data acquisition and analysis by EK, JV and GS. Aerosol characterization and delivery system design by CP and JD. Manuscript drafted by TE, revisions and additions by KS, JD, CP, FG, PC, RL, EK, JV, GS. All authors read and approved the final manuscript.
Additional file
References
Hamid Q: Pathogenesis of small airways in asthma. Respiration. 2012, 84: 4-11. 10.1159/000339550.
Sugita M, Kuribayashi K, Nakagomi T, Miyata S, Matsuyama T, Kitada O: Allergic bronchial asthma: airway inflammation and hyperresponsiveness. Intern Med. 2003, 42: 636-643. 10.2169/internalmedicine.42.636.
Kelly MM, O’Connor TM, Leigh R, Otis J, Gwozd C, Gauvreau GM, Gauldie J, O’Byrne PM: Effects of budesonide and formoterol on allergen-induced airway responses, inflammation, and airway remodeling in asthma. J Allergy Clin Immunol. 2010, 125: 349-356. 10.1016/j.jaci.2009.09.011.
Boser SR, Park H, Perry SF, Menache MG, Green FH: Fractal geometry of airway remodeling in human asthma. Am J Respir Crit Care Med. 2005, 172: 817-823. 10.1164/rccm.200411-1463OC.
Gotshall RW: Exercise-induced bronchoconstriction. Drugs. 2002, 62: 1725-1739. 10.2165/00003495-200262120-00003.
Tacon CE, Wiehler S, Holden NS, Newton R, Proud D, Leigh R: Human rhinovirus infection up-regulates MMP-9 production in airway epithelial cells via NF-{kappa}B. Am J Respir Cell Mol Biol. 2010, 43: 201-209. 10.1165/rcmb.2009-0216OC.
Masoli M, Fabian D, Holt S, Beasley R: The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004, 59: 469-478. 10.1111/j.1398-9995.2004.00526.x.
Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, FitzGerald JM: Economic burden of asthma: a systematic review. BMC Pulm Med. 2009, 9: 24-10.1186/1471-2466-9-24.
Ivanova JI, Bergman R, Birnbaum HG, Colice GL, Silverman RA, McLaurin K: Effect of asthma exacerbations on health care costs among asthmatic patients with moderate and severe persistent asthma. J Allergy Clin Immunol. 2012, 129: 1229-1235. 10.1016/j.jaci.2012.01.039.
Chapman KR, Boulet LP, Rea RM, Franssen E: Suboptimal asthma control: prevalence, detection and consequences in general practice. Eur Respir J. 2008, 31: 320-325. 10.1183/09031936.00039707.
Boulet LP, Becker A, Berube D, Beveridge R, Ernst P: Canadian Asthma Consensus Report, 1999. Canadian Asthma Consensus Group. CMAJ. 1999, 161: S1-S61.
Lougheed MD, Lemiere C, Dell SD, Ducharme FM, Fitzgerald JM, Leigh R, Licskai C, Rowe BH, Bowie D, Becker A, Boulet LP: Canadian Thoracic Society Asthma Management Continuum-2010 Consensus Summary for children six years of age and over, and adults. Can Respir J. 2010, 17: 15-24.
Rowe BH, Sevcik W, Villa-Roel C: Management of severe acute asthma in the emergency department. Curr Opin Crit Care. 2011, 17: 335-341. 10.1097/MCC.0b013e328348bf09.
Chowdhury BA, Dal PG: The FDA and safe use of long-acting beta-agonists in the treatment of asthma. N Engl J Med. 2010, 362: 1169-1171. 10.1056/NEJMp1002074.
McFadden ER: Acute severe asthma. Am J Respir Crit Care Med. 2003, 168: 740-759. 10.1164/rccm.200208-902SO.
Wener RR, Bel EH: Severe refractory asthma: an update. Eur Respir Rev. 2013, 22: 227-235. 10.1183/09059180.00001913.
Tough SC, Green FH, Paul JE, Wigle DT, Butt JC: Sudden death from asthma in 108 children and young adults. J Asthma. 1996, 33: 179-188. 10.3109/02770909609054550.
Oddo M, Feihl F, Schaller MD, Perret C: Management of mechanical ventilation in acute severe asthma: practical aspects. Intensive Care Med. 2006, 32: 501-510. 10.1007/s00134-005-0045-x.
Astin TW, Barer GR, Shaw JW, Warren PM: The action of carbon dioxide on constricted airways. J Physiol. 1973, 235: 607-623.
Duane SF, Weir EK, Stewart RM, Niewoehner DE: Distal airway responses to changes in oxygen and carbon dioxide tensions. Respir Physiol. 1979, 38: 303-311. 10.1016/0034-5687(79)90056-2.
Twort CH, Cameron IR: Effects of PCO2, pH and extracellular calcium on contraction of airway smooth muscle from rats. Respir Physiol. 1986, 66: 259-267. 10.1016/0034-5687(86)90078-2.
El Mays TY, Saifeddine M, Choudhury P, Hollenberg MD, Green FH: Carbon dioxide enhances substance P-induced epithelium-dependent bronchial smooth muscle relaxation in Sprague-Dawley rats. Can J Physiol Pharmacol. 2011, 89: 513-520. 10.1139/y11-052.
Thomas M, McKinley RK, Freeman E, Foy C: Prevalence of dysfunctional breathing in patients treated for asthma in primary care: cross sectional survey. BMJ. 2001, 322: 1098-1100. 10.1136/bmj.322.7294.1098.
Fisher HK, Holton P, Buxton RS, Nadel JA: Resistance to breathing during exercise-induced asthma attacks. Am Rev Respir Dis. 1970, 101: 885-896.
McFadden ER, Stearns DR, Ingram RH, Leith DE: Relative contributions of hypocarbia and hyperpnea as mechanisms in postexercise asthma. J Appl Physiol. 1977, 42: 22-27.
van den Elshout FJ, van Herwaarden CL, Folgering HT: Effects of hypercapnia and hypocapnia on respiratory resistance in normal and asthmatic subjects. Thorax. 1991, 46: 28-32. 10.1136/thx.46.1.28.
Fisher HK, Hansen TA: Site of action of inhaled 6 per cent carbon dioxide in the lungs of asthmatic subjects before and after exercise. Am Rev Respir Dis. 1976, 114: 861-870.
Wolfson MR, Shaffer TH: Pulmonary applications of perfluorochemical liquids: ventilation and beyond. Paediatr Respir Rev. 2005, 6: 117-127. 10.1016/j.prrv.2005.03.010.
Lehmler HJ, Bummer PM, Jay M: Liquid ventilation - a new way to deliver drugs to diseased lungs?. Chemtech. 1999, 29: 7-12.
Schürch S: Perfluorocarbon-surfactant interactions: biophysical aspects. Am Soc Artif Intern Organs. 2006, 52: 487-10.1097/00002480-200607000-00026.
Rotta AT, Gunnarsson B, Fuhrman BP, Wiryawan B, Hernan LJ, Steinhorn DM: Perfluorooctyl bromide (perflubron) attenuates oxidative injury to biological and nonbiological systems. Pediatr Crit Care Med. 2003, 4: 233-238. 10.1097/01.PCC.0000059729.21375.D0.
Smith TM, Steinhorn DM, Thusu K, Fuhrman BP, Dandona P: A liquid perfluorochemical decreases the in vitro production of reactive oxygen species by alveolar macrophages. Crit Care Med. 1995, 23: 1533-1539. 10.1097/00003246-199509000-00014.
Varani J, Hirschl RB, Dame M, Johnson K: Perfluorocarbon protects lung epithelial cells from neutrophil-mediated injury in an in vitro model of liquid ventilation therapy. Shock. 1996, 6: 339-344. 10.1097/00024382-199611000-00007.
Uchida T, Nakazawa K, Yokoyama K, Makita K, Amaha K: The combination of partial liquid ventilation and inhaled nitric oxide in the severe oleic acid lung injury model. Chest. 1998, 113: 1658-1666. 10.1378/chest.113.6.1658.
Shashikant BN, Miller TL, Jeng MJ, Davis J, Shaffer TH, Wolfson MR: Differential impact of perfluorochemical physical properties on the physiologic, histologic, and inflammatory profile in acute lung injury. Crit Care Med. 2005, 33: 1096-1103. 10.1097/01.CCM.0000163218.79770.29.
Kandler MA, von der Hardt K, Gericke N, Chada M, Dotsch J, Rascher W: Dose response to aerosolized perflubron in a neonatal swine model of lung injury. Pediatr Res. 2004, 56: 191-197. 10.1203/01.PDR.0000132667.47744.F4.
von der Hardt K, Kandler MA, Brenn G, Scheuerer K, Schoof E, Dotsch J, Rascher W: Comparison of aerosol therapy with different perfluorocarbons in surfactant-depleted animals. Crit Care Med. 2004, 32: 1200-1206. 10.1097/01.CCM.0000124876.31138.F6.
Bischof RJ, Snibson K, Shaw R, Meeusen EN: Induction of allergic inflammation in the lungs of sensitized sheep after local challenge with house dust mite. Clin Exp Allergy. 2003, 33: 367-375. 10.1046/j.1365-2222.2003.01534.x.
Snibson KJ, Bischof RJ, Slocombe RF, Meeusen EN: Airway remodelling and inflammation in sheep lungs after chronic airway challenge with house dust mite. Clin Exp Allergy. 2005, 35: 146-152. 10.1111/j.1365-2222.2005.02137.x.
Respiratory therapy equipment: Part 1-Nebulizing systems and their components. European Nebulizer Standard: EN 13544-1:2007+A1:2009. 2009, 1-43.
Shaw RJ, McNeill MM, Gatehouse TK, Douch PG: Quantification of total sheep IgE concentration using anti-ovine IgE monoclonal antibodies in an enzyme immunoassay. Vet Immunol Immunopathol. 1997, 57: 253-265. 10.1016/S0165-2427(97)00010-X.
Koumoundouros E, Snibson K, Mareels IY: Oesophageal techniques for deriving the lung dynamics of quietly breathing sheep. Conf Proc IEEE Eng Med Biol Soc. 2008, 2008: 2435-2438.
Abraham WM, Delehunt JC, Yerger L, Marchette B: Characterization of a late phase pulmonary response after antigen challenge in allergic sheep. Am Rev Respir Dis. 1983, 128: 839-844.
Rice AJ, Reynolds PN, Reynolds AM, Holmes MD, Scicchitano R: Tachykinin-induced bronchoconstriction in sheep is NK-1 receptor mediated and exhibits tachyphylaxis. Respirology. 2001, 6: 113-123. 10.1046/j.1440-1843.2001.00315.x.
Bijaoui E, Tuck SA, Remmers JE, Bates JH: Estimating respiratory mechanics in the presence of flow limitation. J Appl Physiol. 1999, 86: 418-426. 10.1063/1.370746.
Choudhury P, El Mays T, Snibson K, Wilson R, Leigh R, Dennis J, Nelson DE, Green FHY: Investigations of mechanisms of carbon dioxide-induced bronchial smooth muscle relaxation. Am J Respir Crit Care Med. 2012, 185: A2848-
Ingram RH: Effects of airway versus arterial CO2 changes on lung mechanics in dogs. J Appl Physiol. 1975, 38: 603-607.
Ten Berge RE, Weening EC, Roffel AF, Zaagsma J: Beta 2- but not beta 3-adrenoceptors mediate prejunctional inhibition of non-adrenergic non-cholinergic contraction of guinea pig main bronchi. Eur J Pharmacol. 1995, 275: 199-206. 10.1016/0014-2999(94)00771-X.
Al-Saiedy M, Nelson E, El Mays T, Amrein M, Green F: Perflubron enhances mucin plug clearance in vitro in the presence of natural surfactant. Eur Respir J. 2013, 42 (Suppl. 57): 124s-ERS International Congress, Barcelona, Spain. Ref Type: Abstract
Bachofen H, Schurch S: Alveolar surface forces and lung architecture. Comp Biochem Physiol A Mol Integr Physiol. 2001, 129: 183-193. 10.1016/S1095-6433(01)00315-4.
Schurch S, Bachofen H, Possmayer F: Surface activity in situ, in vivo, and in the captive bubble surfactometer. Comp Biochem Physiol A Mol Integr Physiol. 2001, 129: 195-207. 10.1016/S1095-6433(01)00316-6.
Cheng G, Ueda T, Sugiyama K, Toda M, Fukuda T: Compositional and functional changes of pulmonary surfactant in a guinea-pig model of chronic asthma. Respir Med. 2001, 95: 180-186. 10.1053/rmed.2000.1012.
Winkler C, Hohlfeld JM: Surfactant and allergic airway inflammation. Swiss Med Wkly. 2013, 143: w13818-
Croce MA, Fabian TC, Patton JH, Melton SM, Moore M, Trenthem LL: Partial liquid ventilation decreases the inflammatory response in the alveolar environment of trauma patients. J Trauma. 1998, 45: 273-280. 10.1097/00005373-199808000-00012.
Rotta AT, Steinhorn DM: Partial liquid ventilation reduces pulmonary neutrophil accumulation in an experimental model of systemic endotoxemia and acute lung injury. Crit Care Med. 1998, 26: 1707-1715. 10.1097/00003246-199810000-00026.
Kirschvink N, Reinhold P: Use of alternative animals as asthma models. Curr Drug Targets. 2008, 9: 470-484. 10.2174/138945008784533525.
Van der Velden J, Snibson KJ: Airway disease: the use of large animal models for drug discovery. Pulm Pharmacol Ther. 2011, 24: 525-532. 10.1016/j.pupt.2011.02.001.
Zosky GR, Sly PD: Animal models of asthma. Clin Exp Allergy. 2007, 37: 973-988. 10.1111/j.1365-2222.2007.02740.x.
Abraham WM: Modeling of asthma, COPD and cystic fibrosis in sheep. Pulm Pharmacol Ther. 2008, 21: 743-754. 10.1016/j.pupt.2008.01.010.
Tomioka K, Garrido R, Ahmed A, Stevenson JS, Abraham WM: YM461, a PAF antagonist, blocks antigen-induced late airway responses and airway hyperresponsiveness in allergic sheep. Eur J Pharmacol. 1989, 170: 209-215. 10.1016/0014-2999(89)90541-4.
Kasperska-Zajac A, Brzoza Z, Rogala B: Platelet-activating factor (PAF): a review of its role in asthma and clinical efficacy of PAF antagonists in the disease therapy. Recent Pat Inflamm Allergy Drug Discov. 2008, 2: 72-76. 10.2174/187221308783399306.
Mariassy AT, St George JA, Nishio SJ, Plopper CG: Tracheobronchial epithelium of the sheep: III. Carbohydrate histochemical and cytochemical characterization of secretory epithelial cells. Anat Rec. 1988, 221: 540-549. 10.1002/ar.1092210110.
Koumoundouros E, Bischof RJ, Meeusen EN, Mareels IM, Snibson KJ: Chronic airway disease: deteriorating pulmonary function in sheep associated with repeated challenges of house dust mite. Exp Lung Res. 2006, 32: 321-330. 10.1080/01902140600916960.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
SolAeroMed Inc is a small biotechnology company founded in partnership with the University of Calgary to develop a novel rescue drug for acute asthma (S-1226). This paper describes pre-clinical animal studies in the development of this drug.
- Dr Tamer El Mays is a co-founder, shareholder and was a temporary employee of SolAeroMed Inc.
- Dr Richard Leigh is a shareholder in SolAeroMed Inc.
- Dr Cora Pieron is a shareholder and part-time employee of SolAeroMed Inc.
- Dr Dennis is a director, co-founder and shareholder in SolAeroMed Inc.
- Dr Francis Green is a director, co-founder and shareholder in SolAeroMed Inc.
- Dr Ken Snibson is a shareholder in SolAeroMed Inc.
- All remaining authors have no competing interests to declare.
Electronic supplementary material
12931_2014_98_MOESM1_ESM.zip
Additional file 1: Video clip description: the black dot is the stain from the tissue dye. The partially occluded airway that is in the center of the screen begins to dilate immediately after the treatment starts (with the click sound on the video). Note that the adjacent smaller, completely occluded, airways also re-opened with treatment. (ZIP 5 MB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
El Mays, T.Y., Choudhury, P., Leigh, R. et al. Nebulized perflubron and carbon dioxide rapidly dilate constricted airways in an ovine model of allergic asthma. Respir Res 15, 98 (2014). https://doi.org/10.1186/s12931-014-0098-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-014-0098-x