Abstract
Background
PKU is an autosomal recessive hereditary inborn error of metabolism caused by a lack of phenylalanine hydroxylase enzyme activity. Pegvaliase (PALYNZIQ®) treatment has been approved to reduce blood Phe concentrations in adult phenylketonuria patients with uncontrolled blood Phe concentrations greater than 600 micromol/L on current management. However, data regarding individuals under the age of 16 is still unavailable.
Case report
We report a 12-year-old Saudi girl who underwent pegvaliase therapy and was closely monitored for one year. Remarkably, a positive therapeutic response became apparent six months after commencing pegvaliase treatment. Phenylalanine (Phe) levels showed significant improvement, stabilising within the < 5 to 14 µmol/L range on a regular diet without any restriction. At her current age of 12, the patient maintains an unrestricted dietary regimen, consuming a diverse selection of foods, including poultry, meat, and protein sources, all while consistently maintaining normal Phe levels with no change in mental status after treatment. The parents gave their written, informed consent in allowing the research study to be carried out and clinical data to be published.
Conclusions
This report addresses the potential broader applications of Pegvaliase in children, as well as its safety and tolerability in this age group. However, larger sample sizes and robust methodologies are required to validate such findings.
Similar content being viewed by others
Introduction
Phenylketonuria (PKU) is an autosomal recessive hereditary metabolic disorder caused by a deficiency in the activity of phenylalanine hydroxylase (PAH; EC 1.14.16.1). This deficiency leads to an interruption in the enzymatic conversion of phenylalanine (Phe) into tyrosine (Tyr) within the liver, resulting in elevated Phe concentrations both systemically and in the brain [1,2,3].
The consequences of elevated blood Phe levels encompass deficits in executive cognitive functions, behavioral abnormalities, and psychiatric disturbances, including depression and anxiety. Furthermore, these effects extend to compromised quality of life (QoL), disrupted mood regulation, and impaired attention span [2, 4,5,6,7]. The clinical spectrum of PKU ranges from mild hyperphenylalaninemia, characterised by blood Phe levels predominantly below 360 µmol/L, to the more severe classical PKU phenotype where untreated Phe levels in the bloodstream exceed 1200 µmol/L [1].
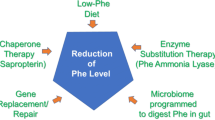
The timely management of blood Phe levels through dietary interventions has effectively reduced the occurrence of severe neurological complications during the critical phase of childhood brain development. However, significant medical challenges persist despite these advancements [8]. Sapropterin dihydrochloride (KUVAN®), a synthesised 6R-tetrahydrobiopterin (BH4) co-factor, historically represented the sole pharmacotherapeutic option for BH4-responsive PKU cases. This treatment primarily addresses milder phenotypic presentations characterised by residual PAH activity [9, 10]. A paradigmatic advance emerged in May 2018 with the FDA’s endorsement of pegvaliase (PALYNZIQ®, BioMarin Pharmaceutical Inc., Novato, CA, USA), a novel enzyme substitution therapy for adult PKU patients whose blood Phe concentration exceeds 600 µmol/L. In May 2019, the European Commission approved pegvaliase for PKU patients aged 16 years or older with inadequate blood Phe control [11]. The pegvaliase clinical trials signify significant progress in advancing the PKU therapeutic landscape [12,13,14,15,16,17,18]. Substantial reduction in blood Phe levels has exhibited correlations with sustained enhancements in neuropsychiatric outcomes, a phenomenon observed over the course of long-term pegvaliase treatment. The objective is for individuals undergoing pegvaliase treatment to attain consistent, lifelong control over blood Phe levels, thereby fostering cognitive and psychosocial improvement while consuming protein-unrestricted diets.
Evaluating adverse events (AEs) associated with pegvaliase treatment in PKU patients provides crucial insights into the therapy’s safety profile. Injection site reactions and arthralgia are the most common AEs, typically displaying a temporary course. Instances of anaphylaxis reactions, although infrequent, tend to be more prevalent within the initial six months of treatment initiation [17, 19].
A limited number of patients aged 16 to 18 underwent pegvaliase treatment, with AEs resembling those observed in adult patients regarding both type and frequency. Conversely, data concerning individuals under the age of 16 remains unavailable. This article presents the first case report detailing a 12-year-old Saudi girl initiated on pegvaliase and closely observed over one year, yielding promising outcomes. This may underscore the rationale for exploring the potential benefits of pegvaliase in the pediatric age group. The reporting of this article aligns with the Case Report Guidelines (CARE) [20].
Case report
The index case was a 12-year-old Saudi girl, the offspring of healthy, non-consanguineous parents, and she had two elder healthy sisters. The pregnancy transpired without complications, with unremarkable findings during the antenatal ultrasounds. Her delivery occurred at full term (38 + 2 weeks) via cesarean section due to a history of a prior cesarean procedure. Her birth measurements fell within the normal range: length at 53 cm (90th percentile), weight at 3.66 kg (70th percentile), and head circumference at 34.5 cm (25th-50th percentile).
At eight months of age, the parents sought medical evaluation owing to concerns about her global developmental delay. She exhibited an inability to sit or crawl independently. The family pursued medical opinions from various centres. Yet, a definitive diagnosis remained elusive as the patient was born in Buraidah city (a small city in Saudi Arabia) with no neonatal screening program at the time of delivery. Correspondingly, the diagnosis was revealed at three years old when her parents consulted a pediatric neurologist, who observed that her developmental delay was accompanied by speech delay, hyperactivity, fair skin, blond hair, and hypotonia. An initial brain magnetic resonance imaging (MRI) did not reveal any abnormalities.
A comprehensive analysis of plasma amino acids indicated a notably elevated Phe level of 2116 µmol/l (reference range: 37–78 µmol/l) alongside a reduced Tyr level of 30 µmol/l (reference range: 40–92 µmol/l). Subsequently, she was referred to a different genetics institution and subsequent DNA molecular genetic testing uncovered a homozygous pathogenic missense mutation identified as NM_000277.3(PAH): c.754 C > T (p. Arg252Trp) in the PAH gene. Following diagnosis, the patient was promptly initiated on a Phe-restricted dietary regimen and prescribed KUVAN® (sapropterin dihydrochloride); however, this intervention did not achieve noticeable clinical improvement.
Referred to our care at the age of 9 years, the patient presented with mild intellectual disability and hyperactivity during her clinical assessment at that time. Regarding developmental milestones, she exhibited the capability to articulate coherent sentences, engage in writing activities, self-feed, and independently manage dressing tasks. Her overall developmental level was functioning at a level akin to a 5-year-old. This observation was corroborated by her assessed intelligence quotient (IQ) of 73, classifying her within the range of mild intellectual disability.
Upon physical examination, her height measured 142.3 cm (> 95th percentile). Her weight registered at 42 kg (90th -95th percentile) while her head circumference measured 52 cm (5th -10th percentile). Notably, the patient exhibited no discernible dysmorphic features, and her systemic examination yielded unremarkable findings. Although the patient exhibited good catch-up growth, it was evident that her learning capabilities and cognitive functions bore certain limitations. As a result, her educational pursuits were channeled into a specialized school environment. Throughout the course of her evaluation at our clinic, the patient remained under a regimen involving sapropterin dihydrochloride at a dosage of 20 mg/kg per day, complemented by a Phe-restricted dietary regimen.
Over the course of a one-year evaluation, the presented patient struggled with suboptimal control over Phe levels, which exhibited fluctuations ranging between 780 and 1116 µmol/L, (Fig. 1). Consequently, the parents approached us to inquire about the treatment and insisted to start even after we informed them that it was only approved for patients over the age of 16. The parents also asked to begin the treatment on a research basis. As a result, we included the patient in the study. The King Abdullah International Medical Research Centre (KAIMRC) in Riyadh, Saudi Arabia’s Institutional Review Boards (IRB) gave their approval for this study (Ref. RC19/120/R). The parents gave their written, informed consent in allowing the research study to be carried out and clinical data to be published.
Given the challenges in managing her Phe levels, the decision was made to propose the initiation of pegvaliase (PALYNZIQ®) in March 2020, when the patient was 9 years and 3 months old. The therapeutic approach involved a gradual escalation protocol, commencing with 2.5 mg once weekly for the initial month. Subsequently, the dosage was increased to 2.5 mg twice weekly, followed by further increments to 10 mg weekly, 10 mg twice weekly, 10 mg four times weekly, 10 mg daily, and ultimately reaching 20 mg daily.
Throughout this treatment course, consistent monitoring of Phe levels and the Phe to Tyr ratio was undertaken. Preceding the initiation of treatment, the patient’s guardians underwent comprehensive education regarding potential reported AEs and instructions regarding the proper administration of the medication. Emphasis was also placed on the periodic rotation of injection sites to ensure optimal outcomes.
Shortly after commencing treatment, the patient developed a generalised maculopapular skin rash on the third day (Fig. 2). In response, Betnovate Cream was initiated once daily while the treatment course was maintained. The patient did not experience itching, facial swelling, fever, or respiratory distress. The skin rash gradually resolved within 10 days following the initiation of pegvaliase and did not recur thereafter. Approximately six months after initiating pegvaliase treatment, the patient’s responsiveness became evident. The Phe levels showed notable improvement, stabilising within a range of < 5 to 14 µmol/L. Currently, at the age of 12, the patient enjoys an unrestricted diet, consuming various foods, including poultry, meat, and protein, all the while maintaining consistently normal Phe levels with no change in mental status or signs of hypophenylalaninemia.
Discussion
This article presents this compelling case of first successful usage of Pegvaliasein children, supported by promising outcomes. Despite the absence of prior utilisation of this therapy within this age group, the patient exhibited a remarkable reduction in Phe levels, which fell below 80 µmol/L. This decrease persisted even in instances of non-compliance with the Phe-restricted diet. The Phe levels went down and up after the initiation of our medication, however, after reaching the target of 20 mg/day, the patient consistently maintained Phe levels below 360 µmol/L, along with a favorable Phe/Tyr ratio of approximately one. These positive outcomes remained stable over the subsequent year, and no adverse events (AEs) were reported during this period.
The management approach for PKU revolves around a low-protein diet supplemented by Phe-restricted foods and/or adapted low-protein foods [21, 22]. Nonetheless, this regimen’s complexity challenges adherence and quality of life (QoL) [23]. Individuals with PKU desire innovative therapies to amplify natural protein consumption, diminish reliance on medical foods, bolster mental well-being, and effectively regulate blood Phe levels [24]. Although pegvaliase represents a pioneering treatment that has undergone rigorous clinical trials, none of these trials have encompassed the pediatric age group.
In the initial phase 1 open-label trial (PAL-001, NCT00634660), pegvaliase was evaluated among individuals aged over 18 with classic PKU, with an average baseline Phe concentration of 1310 µmol/L. Over a 42-day follow-up, those receiving the 0.1 mg/kg dose exhibited a noteworthy reduction in Phe levels, with a mean decrease of 48.3% by day six [18].
Pegvaliase dosing strategies were explored through three phase 2 studies. In PAL-002 (NCT00925054), involving 40 adult PKU patients, varied doses (0.001 to 0.1 mg/kg) inadequately controlled blood Phe levels. Similar outcomes emerged in PAL-004 (NCT01212744), a study with 16 adults receiving doses (0.06 to 0.8 mg/kg) five times weekly over 13 weeks. While the regimens in PAL-002 were generally well tolerated, higher doses in PAL-004 correlated with increased hypersensitivity reactions, necessitating dose reduction [25]. In response to these findings, phase 2 trial 165–205 (NCT01560286) was initiated, using an adaptable dosing approach. Twenty-four participants underwent a 4- to 8-week induction phase at 2.5 mg per week, followed by adaptable dose adjustments to maintain blood Phe concentration ≤ 600 µmol/L. After 24 weeks, mean blood Phe < 600 µmol/L by week 11 (56% ± 36% reduction from baseline) was detected. While by 24 weeks of treatment, all achieved < 120 µmol/L [14].
Pegvaliase underwent assessment through a phase 3 study, PRISM-1 (NCT01819727) (17), with 261 participants with 20 mg/d a 40 mg/d group. Baseline Phe averaged 1232.7 µmol/L. Maintenance doses were achieved at around 11.5 weeks (20 mg/d) and 14 weeks (40 mg/d). Notably, Phe levels decreased significantly, by 51.1% at 12 months and 68.7% at 24 months, accompanied by improved inattention and mood scores. AEs were mostly mild to moderate (99%). Few discontinuations occurred due to anaphylaxis and arthralgia. PRISM-1 participants progressed to PRISM-2 (NCT01889862), demonstrating stable Phe levels in the active group, while the placebo group experienced an increase.
This study has limitations, involving a solitary case and a short follow-up duration, raising concerns about generalizability and long-term sustainability. While short-term effects are promising, uncertainties about long-term impact persist, warranting extended follow-up to evaluate its durability on Phe levels and overall well-being. Given PKU’s complexity, future research should explore combining pegvaliase with other therapies and individualised strategies based on precision medicine principles. Investigating these approaches in pediatric PKU patients would address these limitations and refine treatment strategies.
Conclusion
When considering PKU treatment, patient characteristics and preferences are pivotal considerations. Pegvaliase stands out by lowering blood Phe independently of PAH activity, setting it apart from existing therapeutic options. FDA approval for pegvaliase is exclusive to adults with uncontrolled blood Phe over 600 µmol/L. Across phases 1 to 3, pegvaliase significantly reduces Phe levels, improving inattention and mood; however, these benefits should be weighed against potential AEs. We presented a case of a 12-year-old girl on pegvaliase under close monitoring, showing positive outcomes and a good safety profile. This highlights broader pegvaliase applications, underscoring the need for ongoing research into its safety and efficacy in younger patients.
Data availability
The datasets will be available from the corresponding author upon reasonable request.
References
Blau N, van Spronsen FJ, Levy HL, Phenylketonuria. Lancet (London England). 2010;376(9750):1417–27.
Ten Hoedt AE, De Sonneville LMJ, Francois B, Ter Horst NM, Janssen MCH, Rubio-Gozalbo ME, et al. High phenylalanine levels directly affect mood and sustained attention in adults with phenylketonuria: a randomised, double-blind, placebo-controlled, crossover trial. J Inherit Metab Dis. 2011;34(1):165–71.
Williams RA, Mamotte CDS, Burnett JR. Phenylketonuria: an inborn error of phenylalanine metabolism. Clin Biochem Rev. 2008;29(1):31–41.
Moyle JJ, Fox AM, Arthur M, Bynevelt M, Burnett JR. Meta-analysis of neuropsychological symptoms of adolescents and adults with PKU. Neuropsychol Rev. 2007;17(2):91–101.
Smith I, Knowles J. Behaviour in early treated phenylketonuria: A systematic review. In: European Journal of Pediatrics, Supplement. 2000.
Gassió R, Campistol J, Vilaseca MA, Lambruschini N, Cambra FJ, Fusté E. Do adult patients with phenylketonuria improve their quality of life after introduction/resumption of a phenylalanine-restricted diet? Acta Paediatr Int J Paediatr. 2003;92(12):1474–8.
Weglage J, Fromm J, van Teeffelen-Heithoff A, Möller HE, Koletzko B, Marquardt T et al. Neurocognitive functioning in adults with phenylketonuria: results of a long term study. Mol Genet Metab. 2013;110(SUPPL.).
Blau N, Hennermann JB, Langenbeck U, Lichter-Konecki U. Diagnosis, classification, and genetics of phenylketonuria and tetrahydrobiopterin (BH4) deficiencies. Volume 104. Molecular Genetics and Metabolism; 2011.
Kuvan®. (Sapropterin Dihydrochloride) Tablets; Highlights of Prescribing Information. 2014.
European Medicines Agency. Kuvan: EPAR - Summary for the Public. 2007.
BioMarin Pharmaceutical Inc. European Commission Approves Palynziq® (Pegvaliase Injection) for Treatment of Phenylketonuria (PKU) in Patients Aged 16 Years or Older. 2019.
Longo N, Harding CO, Burton BK, Dorothy K, Vockley J, Wasserstein M, et al. Phase 1 trial of subcutaneous rAvPAL-PEG in subjects with phenylketonuria. PMC. 2015;384(9937):37–44.
Longo N, Zori R, Wasserstein MP, Vockley J, Burton BK, Decker C et al. Long-term safety and efficacy of pegvaliase for the treatment of phenylketonuria in adults: combined phase 2 outcomes through PAL-003 extension study. Orphanet J Rare Dis. 2018;13(1).
Zori R, Thomas JA, Shur N, Rizzo WB, Decker C, Rosen O, et al. Induction, titration, and maintenance dosing regimen in a phase 2 study of pegvaliase for control of blood phenylalanine in adults with phenylketonuria. Mol Genet Metab. 2018;125(3):217–27.
Gupta S, Lau K, Harding CO, Shepherd G, Boyer R, Atkinson JP, et al. Association of immune response with efficacy and safety outcomes in adults with phenylketonuria administered pegvaliase in phase 3 clinical trials. EBioMedicine. 2018;37:366–73.
Harding CO, Amato RS, Stuy M, Longo N, Burton BK, Posner J, et al. Pegvaliase for the treatment of phenylketonuria: a pivotal, double-blind randomised discontinuation phase 3 clinical trial. Mol Genet Metab. 2018;124(1):20–6.
Thomas J, Levy H, Amato S, Vockley J, Zori R, Dimmock D, et al. Pegvaliase for the treatment of phenylketonuria: results of a long-term phase 3 clinical trial program (PRISM). Mol Genet Metab. 2018;124(1):27–38.
Longo N, Harding CO, Burton BK, Grange DK, Vockley J, Wasserstein M, et al. Single-dose, subcutaneous recombinant phenylalanine ammonia lyase conjugated with polyethylene glycol in adult patients with phenylketonuria: an open-label, multicentre, phase 1 dose-escalation trial. Lancet. 2014;384(9937):37–44.
Initial US, Approval. PALYNZIQ (pegvaliase-pqpz) injection, for subcutaneous use. 2018;1–38.
Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218–35.
Vockley J, Andersson HC, Antshel KM, Braverman NE, Burton BK, Frazier DM, et al. Phenylalanine hydroxylase deficiency: diagnosis and management guideline. Genet Med. 2014;16(2):188–200.
Singh RH, Cunningham AC, Mofidi S, Douglas TD, Frazier DM, Hook DG, et al. Updated, web-based nutrition management guideline for PKU: an evidence and consensus based approach. Mol Genet Metab. 2016;118(2):72–83.
Bosch AM, Burlina A, Cunningham A, Bettiol E, Moreau-Stucker F, Koledova E et al. Assessment of the impact of phenylketonuria and its treatment on quality of life of patients and parents from seven European countries. Orphanet J Rare Dis. 2015;10(1).
Brown CS, Lichter-Konecki U. Phenylketonuria (PKU): a problem solved? Mol Genet Metab Rep. 2016;6:8–12.
Thomas JA, Longo N, Zori R, Burton BK, Wasserstein M, Grange DK et al. Evaluation of multiple dosing regimens in phase 2 studies of rAvPAL-PEG (BMN 165, pegvaliase) for control of blood phenylalanine levels in adults with phenylketonuria [poster]. In: SIMD Annual Meeting. 2015.
Acknowledgements
We are grateful to patients and their families involved in this study.
Funding
Medical writing for this article was funded by BioMarin Pharmaceutical Inc which was not involved in study concept, data collection and analysis or manuscript development.
Author information
Authors and Affiliations
Contributions
M.A: Writing the manuscript, submitting, management and clinical diagnosis. R.A: collecting the data and follow up the patient. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board (IRB) of King Abdullah International Medical Research Centre (KAIMRC), Riyadh (Ref. RC19/120/R). In addition, written informed consent for the publication of genetic, molecular, and clinical data was obtained from the parents of the enrolled patients. The parents of the patient gave written informed consent in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent for the publication of related data was obtained from the parents of the enrolled patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alfadhel, M., Albarakati, R. First successful outcomes of pegvaliase (PALYNZIQ) in children. BMC Med Genomics 17, 76 (2024). https://doi.org/10.1186/s12920-024-01847-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-024-01847-1