Abstract
Background
Thousand and one amino-acid kinase 1 (TAOK1) encodes the MAP3K protein kinase TAO1, which has recently been displayed to be essential for neuronal maturation and cortical differentiation during early brain development. Heterozygous variants in TAOK1 have been reported in children with neurodevelopmental disorders, with or without macrocephaly, hypotonia and mild dysmorphic traits. Literature reports lack evidence of neuronal migration disorders in TAOK1 patients, although studies in animal models suggest this possibility.
Case presentation
We provide a clinical description of a child with a neurodevelopmental disorder due to a novel TAOK1 truncating variant, whose brain magnetic resonance imaging displays periventricular nodular heterotopia.
Conclusions
To our knowledge, this is the first report of a neuronal migration disorder in a patient with a TAOK1-related neurodevelopmental disorder, thus supporting the hypothesized pathogenic mechanisms of TAOK1 defects.
Similar content being viewed by others
Background
The advent of whole exome sequencing (WES) as a diagnostic tool has led to an overall diagnostic yield for unexplained neurodevelopmental disorders (NDDs) around 36%, and up to 53% for syndromic NDDs. WES has also led to a rapid increase in the identification of novel disease genes [1, 2].
The TAOK1 gene on chromosome 17 (OMIM * 610,266) encodes the “thousand and one amino acid kinase 1” (TAO1), a ubiquitous serine/threonine protein kinase with a high expression level in brain [3]. It is part of a family of three kinases, TAOKs1-3, which are implicated in critical processes during neurogenesis such as stress-activated MAPK pathway, DNA damage response and regulation of microtubule stability and cytoskeleton dynamics [3,4,5,6,7,8].
Although large–scale WES and array-CGH studies had already identified TAOK1 as a candidate gene for NDDs since 2011 [9, 10], the direct association has been confirmed only recently [11, 12]. Some of these studies clearly documented that defects in TAOK1 expression can affect neuronal maturation and cortical development both in vitro and in animal models [4, 11, 13, 14].
To date, a few case reports and case series present short clinical descriptions of a total of 37 children with NDDs due to heterozygous TAOK1 variants or genomic deletions encompassing the TAOK1 region [11,12,13,14,15,16]. The phenotype consists of a spectrum of nonspecific overlapping clinical features, mainly represented by variable developmental delay with or without macrocephaly, autism spectrum disorder (ASD), hypotonia and mild dysmorphic traits. Most variants occurred de novo, but some were inherited by an affected or mildly affected parent, showing intrafamilial variability [14, 16].
To date, the reported data on brain magnetic resonance imaging (MRI) findings in TAOK1-related patients are scarce and non-specific [11, 16,17,18].
Case presentation
The patient is a 5-year-old boy of Georgian origin, who was born at term by cesarean section (due to previous caesarean deliveries) from unrelated parents. Pregnancy and perinatal period were unremarkable. At birth, his weight was 4.185 g (+ 1.6 SD), length was 51 cm (-0.2 SD) and head circumference was 36 cm (+ 1 SD).
During infancy linear growth and weight gain were normal, while head circumference increased at an abnormal rate that resulted in acquired macrocephaly. At the age of five years, body weight was 21.5 Kg (0 SD), height was 112.5 cm (+ 0.7 SD) and head circumference was 57 cm (+ 4.2 SD). He showed mild dysmorphic traits: high forehead, long and pronounced philtrum, bulbous nose and uplifted earlobes. Acquired left-eye esophoria appeared at the age of four years [Fig. 1].
Early psychomotor development appeared normal until the age of 18 months, when language stagnation with poor communicative purpose and hyperactive behaviour emerged. He also displayed poor eye contact during social interactions and selective eating. At the age of two years ASD was suspected by clinicians. At the age of five years, his language consisted of fewer than 20 disyllabic words. Bowel and bladder control were acquired almost completely and his eating was still selective. Motor skills were achieved within the normal ranges. Neither paroxysmal events nor seizures were reported; awake and sleep electroencephalograms were unremarkable.
At the age of four years, he underwent a comprehensive assessment with ADOS-2 Module 1 (Autism Diagnostic Observation Schedule-Second Edition), CARS-2 (Childhood Autism Rating Scale, 2nd Edition) and ADI-R (Autism Diagnostic Interview-Revised). He did not fully meet the criteria for autism diagnosis. His intelligence was in the normal range, with a nonverbal IQ of 98 (Leiter − 3 scale). Abdomen ultrasound and audiometry were unremarkable.
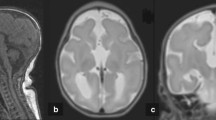
Brain MRI performed at 2y11m (last follow-up 6y11m) revealed two periventricular nodules, isointense to grey matter on all sequences, in the lateral wall of posterior horn and middle portion of the left lateral ventricle, suggestive of periventricular nodular heterotopia (PVNH) [Fig. 2a-b ]. A mild thinning of the corpus callosum (istmo) [Fig. 2c] and a left mesial temporal arachnoid cyst [Fig. 2d] were also present.
Brain MRI (6y 11 m), axial T1 (a-b), midline sagittal T1 (c) and axial T2 (d): periventricular nodular heterotopia in the posterior horn (a, black arrow) and middle portion (b, black arrow) of the left lateral ventricle, mild thinning of the corpus callosum istmo (c, white arrow), and arachnoid cyst in left mesial temporal lobe (d, arrowheads)
Array-CGH revealed a segmental duplication of 250Kb on the Y-chromosome: arr[GRCh37] Yq11.222(21058897_21311923)x2. The father was unavailable for segregation analysis.
WES revealed a novel heterozygous nonsense variant in the TAOK1 gene: NM_020791.4:c.[1414 C > T];[=], NP_065842.1:p.[(Arg472*)];[=]. The variant was absent in the mother, while the father was unavailable for testing.
Discussion and conclusions
We report a 5-year-old child with NDD, macrocephaly, mildly dysmorphic facial features and PVNH. WES identified the heterozygous nonsense variant NM_020791.4:c.1414 C > T in the TAOK1 gene, which has not been previously described in the literature or in databases (ClinVar, LOVD; accessed on 2023/09/14). The variant is absent in the reference population databases gnomAD v2.1.1/v3.1.2 and 1000 Genomes project (accessed on 2023/09/14). It generates a premature stop codon in exon 14 out of 20, which is expected to result in nonsense-mediated decay of the transcript, and haploinsufficiency is already known to be consistent with the molecular mechanism of the disease [11, 13]. We could not confirm whether it occurred de novo: the variant was not present in the mother, while the father was unavailable for testing and his clinical records were not accessible. However, inheritance from a mildly affected parent has been described in five cases [14, 16], suggesting the possibility of incomplete penetrance or variable expressivity. Based on the recommendations of the American College of Medical Genetics [19] and on the clinical similarities with published cases of TAOK1-related NDD [Table 1, Supplementary Materials], the variant was classified as likely pathogenic (criteria PVS1, PM2) and considered responsible for the proband’s phenotype. The 250Kb duplication detected in Yq11.222 occurs in a region that contains only a redundant paralogue of chromosome 6 gene CD24. The Database of Genomic Variants (DGV, accessed on 2023/09/14) contains a few duplications spanning or overlapping this region, while comparable and larger duplications are reported as benign/likely benign on ClinVar (accessed on 2023/09/14). Therefore, although the father was unavailable for segregation analysis, this variant was considered unrelated to the proband’s phenotype.
In order to better elucidate the phenotypic spectrum of TAOK1-related NDD, we have summarized the available data from 37 previously reported individuals with NDD [Table 1, Supplementary Materials] [11,12,13,14,15,16]. A few cases included in large cohort studies have insufficient clinical description and were not considered in this report [9, 10, 15, 20, 21]. A recent report of a de novo frameshift variant in a girl with isolated childhood-onset tremor was also excluded, because, based on the available clinical data, she did not properly fit into the definition of NDD [22]. Prenatal cases were also excluded [17, 18].
The main clinical features resulting from this review are developmental delay affecting speech and/or motor development, variable intellectual disability (ID), ASD, behavioral abnormalities, macrocephaly, hypotonia, joint hypermobility and dysmorphic facial traits (high forehead, downslanted palpebral fissures, low-set ears, bulbous nose and micrognathia). Less frequently reported are also feeding problems and limb undergrowth, and four patients had seizures [11, 12, 14, 16].
Our proband’s phenotype, characterized by severe language delay, poor communicative skills, acquired macrocephaly and mild dysmorphic facial features, is consistent with this clinical spectrum.
Neuroimaging data are available for only 22 patients with TAOK1-related NDDs [Dulovic-Mahlow et al., 2019; van Woerden et al., 2021; Hunter et al., 2022]. In 11 patients (50%) brain MRI was reported as normal, while the remaining had nonspecific, heterogeneous features, apparently not evocative of neuronal migration defects [Table 1, Supplementary Materials].
Our patient’s brain MRI displayed a mild thinning of the corpus callosum [Fig. 2c] and a left temporopolar arachnoid cyst [Fig. 2d]. Individually, similar nonspecific anomalies have already been observed [14, 16]. Interestingly, our patient also presented with PVNH in the left lateral ventricle [Fig. 2a-b].
PVNH is a congenital brain malformation of cortical development characterized by nodules of grey matter lining the ventricles, resulting from defects in the radial migration of cortical neurons along glial fibers during early brain development. It can be classified based on morphology, symmetry and location of heterotopic nodules along ventricle profiles on brain MRI images. Heterotopic nodules are highly epileptogenic, and may be isolated or associated with other brain abnormalities, variable intellectual disability and dysmorphic features [23, 24]. PVNH is also a genetically heterogeneous condition. Bilateral symmetrical multiple PVNH, often associated with cardiac malformations, is mostly related to defects in the FLNA gene (classical X-linked PVNH). Less typical PVNH forms, represented by bilateral asymmetrical and unilateral PVNH, may be caused by biallelic variants in ARFGEF2, DCHS1, MCPH1, INTS8, FAT4 or heterozygous defects in ERMARD, NEDD4L and MAP1B, as well as several chromosomal abnormalities. Most of these genes are involved in microtubule regulation, vesicle trafficking, cell-cell adhesion and cell polarity. A cumulative dosage effect of multiple genes in the pathogenesis of non-classical PVNH has been hypothesized [25,26,27].
Yu et al. recently reported one case of brain MRI abnormalities in a fetus with a de novo missense TAOK1 variant, in which bilateral polymicrogyria of the lateral fissure area could not be ruled out by the authors [18]. It would be interesting to know whether a postnatal MRI would confirm a malformation of cortical development.
The finding cortical migration defects such as of PVNH is highly consistent with the cellular and developmental role of TAOK1 in neuronal migration, as defined by previous functional studies both in vitro and in animal models [4, 11, 13, 14].
In the embryonic mouse brain, Van Woerden and colleagues [14] observed that reduced TAOK1 expression levels affected neural migration in vivo. Through in utero electroporation, they performed shRNA-mediated knockdown of Taok1 (Taok1kd) at embryonic day 14.5, a critical time for neurodevelopment, and observed a significant deficit in the migration of neurons derived from the transfected progenitors, at birth and at postnatal day 7.
Similarly, by comparing Taok1+/− (haploinsufficient) and WT mice, Wang et al. [13] detected a significant decrease in neuron density in the upper layer of the caudal cortex, confirming a defect in neuronal migration.
To the best of our knowledge, this is the first report of PVNH in an individual with TAOK1-related NDD, suggesting a possible expansion of the phenotype of TAOK1-of this condition.
Although further evidence is needed, this finding could represent a confirmation in humans of the essential role of TAOK1 in neuronal migration, as already indicated by functional studies in vitro and in vivo.
This work also highlights the importance of including brain MRI in the diagnostic workup of affected individuals, even in the absence of epilepsy or macrocephaly.
Data availability
Data and materials are available from the corresponding author upon reasonable request.
Abbreviations
- ASD:
-
autism spectrum disorder
- MRI:
-
magnetic resonance imaging
- NDD/NDDs:
-
neurodevelopmental disorder/s
- PVNH:
-
periventricular nodular heterotopia
- TAOK1 :
-
Thousand and one aminoacid kinase 1
- WES:
-
whole exome sequencing
References
Maia N, Nabais Sá MJ, Melo-Pires M, De Brouwer APM, Jorge P. Intellectual disability genomics: current state, pitfalls and future challenges. BMC Genomics. 2021;22(1):909.
Srivastava S, Love-Nichols JA, Dies KA, Ledbetter DH, Martin CL, Chung WK, et al. Meta-analysis and multidisciplinary consensus statement: exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet Med. 2019;21(11):2413–21.
Hutchison M, Berman KS, Cobb MH. Isolation of TAO1, a protein kinase that activates MEKs in stress-activated protein kinase cascades. J Biol Chem. 1998;273(44):28625–32.
Beeman N, Sapre T, Ong SE, Yadav S. Neurodevelopmental disorder–associated mutations in TAOK1 reveal its function as a plasma membrane remodeling kinase. Sci Signal. 2023;16(766):eadd3269.
Drewes G, Ebneth A, Preuss U, Mandelkow EM, Mandelkow E. MARK, a Novel Family of protein kinases that Phosphorylate Microtubule-Associated proteins and trigger microtubule disruption. Cell. 1997;89(2):297–308.
Liu T, Rohn JL, Picone R, Kunda P, Baum B. Tao-1 is a negative regulator of microtubule plus-end growth. J Cell Sci. 2010;123(16):2708–16.
Pflanz R, Voigt A, Yakulov T, Jäckle H. Drosophila gene tao-1 encodes proteins with and without a Ste20 kinase domain that affect cytoskeletal architecture and cell migration differently. Open Biol. 2015;5(1):140161.
Zihni C, Mitsopoulos C, Tavares IA, Ridley AJ, Morris JDH. Prostate-derived sterile 20-like kinase 2 (PSK2) regulates apoptotic morphology via C-Jun N-terminal kinase and rho Kinase-1. J Biol Chem. 2006;281(11):7317–23.
Cooper GM, Coe BP, Girirajan S, Rosenfeld JA, Vu TH, Baker C, et al. A copy number variation morbidity map of developmental delay. Nat Genet. 2011;43(9):838–46.
Deciphering Developmental Disorders Study. Prevalence and architecture of de novo mutations in developmental disorders. Nature. 2017;542(7642):433–8.
Dulovic-Mahlow M, Trinh J, Kandaswamy KK, Braathen GJ, Di Donato N, Rahikkala E, et al. De Novo variants in TAOK1 cause Neurodevelopmental disorders. Am J Hum Genet. 2019;105(1):213–20.
Xie B, Fan X, Lei Y, Chen R, Wang J, Fu C, et al. A novel de novo microdeletion at 17q11.2 adjacent to NF1 gene associated with developmental delay, short stature, microcephaly and dysmorphic features. Mol Cytogenet. 2016;9(1):41.
Wang J, Li W, Li Z, Xue Z, Zhang Y, Yuan Y, et al. Taok1 haploinsufficiency leads to autistic-like behaviors in mice via the dorsal raphe nucleus. Cell Rep. 2023;42(9):113078.
Woerden GM, Bos M, Konink C, Distel B, Avagliano Trezza R, Shur NE, et al. TAOK1 is associated with neurodevelopmental disorder and essential for neuronal maturation and cortical development. Hum Mutat. 2021;42(4):445–59.
Basel-Salmon L, Ruhrman-Shahar N, Orenstein N, Goldberg Y, Gonzaga-Jauregui C, Shuldiner AR, et al. When phenotype does not match genotype: importance of real-time refining of phenotypic information for exome data interpretation. Genet Med. 2021;23(1):215–21.
Hunter JM, Massingham LJ, Manickam K, Bartholomew D, Williamson RK, Schwab JL et al. Inherited and de novo variants extend the etiology of TAOK1-associated neurodevelopmental disorder. Mol Case Stud. 2022;mcs.a006180.
Liu CY, Yang YH, Li PS, Gan ML, Li DZ. Fetal macrocephaly in the third trimester: prenatal phenotype of TAOK1-associated neurodevelopmental disorder. Eur J Obstet Gynecol Reprod Biol. 2023;289:219–20.
Yu L, Yang C, Shang N, Ding H, Zhu J, Zhu Y, et al. Paternal De Novo variant of TAOK1 in a Fetus with Structural Brain abnormalities. Front Genet. 2022;13:836853.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Coe BP, Stessman HAF, Sulovari A, Geisheker MR, Bakken TE, Lake AM, et al. Neurodevelopmental disease genes implicated by de novo mutation and copy number variation morbidity. Nat Genet. 2019;51(1):106–16.
Satterstrom FK, Kosmicki JA, Wang J, Breen MS, De Rubeis S, An JY, et al. Large-scale exome sequencing study implicates both developmental and functional changes in the Neurobiology of Autism. Cell. 2020;180(3):568–584e23.
Blaschek A, Sitzberger A, Brugger M, Graf E, Berutti R, Zech M, et al. TAOK1-related neurodevelopmental disorder: a new differential diagnosis for childhood-onset tremor? Parkinsonism Relat Disord. 2023;109:105320.
Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns WB. A developmental and genetic classification for malformations of cortical development: update 2012. Brain. 2012;135(5):1348–69.
Battaglia G, Chiapparini L, Franceschetti S, Freri E, Tassi L, Bassanini S, et al. Periventricular Nodular Heterotopia: classification, epileptic history, and Genesis of Epileptic discharges. Epilepsia. 2006;47(1):86–97.
Cellini E, Vetro A, Conti V, Marini C, Doccini V, Clementella C, et al. Multiple genomic copy number variants associated with periventricular nodular heterotopia indicate extreme genetic heterogeneity. Eur J Hum Genet. 2019;27(6):909–18.
Liu W, Yan B, An D, Xiao J, Hu F, Zhou D. Sporadic periventricular nodular heterotopia: classification, phenotype and correlation with Filamin A mutations. Epilepsy Res. 2017;133:33–40.
Vriend I, Oegema R. Genetic causes underlying grey matter heterotopia. Eur J Paediatr Neurol. 2021;35:82–92.
Acknowledgements
The authors of this publication are members of the European Reference 299 Network on Rare Congenital Malformations and Rare Intellectual Disability ERN-ITHACA [EU 300 Framework Partnership Agreement ID: 3HP-HP-FPA ERN-01-2016/739516]. The study was funded by the unconditional support for medical writing received by Progetto Pulcino Onlus. We also thank family members for contributing the medical data necessary for this study.
Funding
None of the Authors have funding to declare.
Author information
Authors and Affiliations
Contributions
AC and SGC drafted the manuscript and retrieved the pertinent literature, SR participated in the proposal of the concept and retrieved the pertinent literature, GT performed genetic consultation and revised the manuscript, MN extracted MRI images and revised the manuscript, DF and CS revised the manuscript, LG and CF have supervised and substantively reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical review and approval were waived for this study because, according to the policy of “Azienda USL-IRCCS di Reggio Emilia” and the competent Ethics Committee of “Area Vasta Emilia Nord (AVEN)”, informed consent is considered sufficient for reports and case series of an observational nature. Written informed consent for publication was obtained from the participant’s parent/legal guardian.
Consent for publication
Written informed consent for publication of the patient’s clinical information, brain MRI images, photography and molecular data was obtained by the patient’s parent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cavalli, A., Caraffi, S.G., Rizzi, S. et al. Heterozygous truncating variant of TAOK1 in a boy with periventricular nodular heterotopia: a case report and literature review of TAOK1-related neurodevelopmental disorders. BMC Med Genomics 17, 68 (2024). https://doi.org/10.1186/s12920-024-01840-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-024-01840-8