Abstract
Background
Oculocutaneous albinism (OCA) is an autosomal recessive disorder characterized by hypo-pigmentation of skin, hair, and eyes. The OCA clinical presentation is due to a deficiency of melanin biosynthesis. Intellectual disability (ID) in OCA cases is a rare clinical presentation and appropriate diagnosis of ID is challenging through clinical examination. We report an Indian family with a rare co-inheritance of OCA1B and ID due to a novel TYR gene variant and chromosomal copy number variations.
Methods
We have done a study on three siblings (2 males and 1 female) of a family where all of them presented with hypopigmented skin, hair and eyes. The male children and their father was affected with ID. Targeted exome sequencing and multiplex ligation-dependent probe amplification analysis were carried out to identify the OCA1B and ID associated genomic changes. Further Array-CGH was performed using SurePrint G3 Human CGH + SNP, 8*60 K array.
Results
A rare homozygous deletion of exon 3 in TYR gene causing OCA1B was identified in all three children. The parents were found to be heterozygous carriers. The Array-CGH analysis revealed paternally inherited heterozygous deletion (1.9 MB) of 15q11.1-> 15q11.2 region in all three children. Additionally, paternally inherited heterozygous deletion (2.6 MB) of 10q23.2-> 10q23.31 region was identified in the first male child; this may be associated with ID as the father and the child both presented with ID. While the 2nd male child had a denovo duplication of 13q31.1-> 13q31.3 chromosomal region.
Conclusion
A rare homozygous TYR gene exon 3 deletion in the present study is the cause of OCA1B in all three children, and the additional copy number variations are associated with the ID. The study highlights the importance of combinational genetic approaches for diagnosing two different co-inherited disorders (OCA and ID). Hence, OCA cases with additional clinical presentation need to be studied in-depth for the appropriate management of the disease.
Similar content being viewed by others
Background
Oculocutaneous albinism (OCA) is an autosomal recessive disorder that occurs due to deficiency of melanin biosynthesis resulting in generalized hypo-pigmentation of skin, eyes, and hair [1]. The incidence of OCA is not known; however, it varies in different regions of the world. Montoliu et al. reported the incidence of albinism is 1:17,000 in the Western population (North America & Europe). Federico et al. estimated the overall incidence of OCA was 1:17,000 to 1:20,000 [2, 3]. Based on the genetic etiology OCA (nonsyndromic) is classified into eight different subtypes (OCA1-7 and OA) [3–5]. The overlapping syndromic albinism such as Hermansky–Pudlak syndrome (HPS), Griscelli syndrome (GS), and Chediak–Higashi syndrome (CHS) have also been reported. Among all, OCA1 is the second most common sub-group of OCA categorized into two types; OCA1A (complete lack of Tyrosinase activity results in the absence of pigmentation in hair, skin, and eyes) and OCA1B (with residual Tyrosinase activity) [6]. OCA2 is commonly seen in African Americans, some Native American groups, and sub-Saharan Africans. The OCA type 3, specifically rufous Oculocutaneous albinism, is reported in Southern Africa [3]. The OCA type 4 is commonly reported in Japanese and Korean populations compared to other parts of the world [7].
The TYR gene is located on the 11q14 chromosome region, consisting of 5 exons encoding 529 amino acids of tyrosinase protein. This protein has dual enzymatic activity as it catalyzes the hydroxylation of tyrosine to dopaquinone in the melanin biosynthesis pathway and is also involved in the oxidation of L-DOPA [8]. The homozygous point mutation or large multiple exonic deletions in the TYR gene are responsible for OCA1 in humans and other mammals [9, 10].
Intellectual disability (ID) and psychotic illness in OCA1 is a rare occurrence; however, it is reported in a few cases of Cross-McKusick-Breen Syndrome (CMBS) [11]. Though the copy number changes are associated with developmental delay, the co-inheritance of ID and albinism has not been reported in the literature. Though the deletions of chromosome number 10 and 15 are reported in a few studies, none of these reports showed the involvement of the TYR gene [12–16]. This study describes a rare co-inheritance of OCA1B and ID in an Indian family, with a rare TYR gene variant and chromosomal copy number variations.
Methods
Study design
The study was designed to understand OCA1B inheritance in three siblings and parents of the family. The NGS study was done to identify variants associated with the disease, and copy number variations were identified using array- comparative genomic hybridization (array-CGH).
Subjects and clinical description
The study was carried out in an Indian family with three children (2 males and 1 female) affected with albinism. The affected children were born of a consanguineous marriage. All the three siblings were presented with hypo-pigmentation of skin (few pigmented spots on hand and face), slight pigmentation on knee region, pigmented iris, brownish-red hair, and photophobia. The 1st child was an 11-year old male, and his clinical examination revealed developmental delay, facial dysmorphism (bulbous nose and wide ears), and ID. The 2nd child was an 8-year old female, had only albinism. She was intellectually normal. The 3rd child (5-year old, male) had ID along with Attention Deficit-Hyperactivity Disorder (ADHD) (hyperactivity, unable to sit still, aggressive) and showed mild facial dysmorphism with low set ears and mild hypertelorism. Both male children had severe speech retardation, and all the siblings had skin burns due to hypo-pigmentation of the skin. The complete blood count, liver and kidney function tests were found to be normal. Brainstem evoked response audiometry (BERA) examination revealed a normal hearing pattern. The father was 21-years old, while the mother was 18-years at the time of first pregnancy. The clinical evaluation of the parents revealed no bad obstetric history. The father had a history of poor social behavior with delayed development at childhood and is currently unable to perform complex routine activities, and the mother is intellectually normal.
Targeted exome sequencing (TES)
Peripheral blood samples were collected in EDTA vacutainers from all affected and non-affected family members. Genomic DNA was isolated from the peripheral blood leukocytes using a Qiagen Mini DNA isolation kit. The concentration was estimated using Qubit™. TES was performed with selective capture of the protein-coding regions of the genes responsible for OCA and other similar phenotype using Next Generation Sequencing (NGS). All the genes covered in the clinical exome assay have been screened for the given clinical indications. The libraries were sequenced to mean > 80-100X coverage on the Illumina sequencing platform.
Sanger sequencing and in-silico validation
The Sanger Sequencing was performed to confirm the variations identified through NGS. The analysis of TYR and RP1 genes variants were carried out by conventional PCR and Sanger Sequencing. The PCR reaction was carried out under the following conditions: Dream Taq Master Mix, 10 µM of primers, 100 ng of genomic DNA. Amplification was carried out in 25-μL volumes with initial denaturation of 95 °C for 2 min, 35 cycles: 95 °C for 30 s, annealing temperature for 30 s, and 72 °C for 45 s and final extension of 72 °C for 5 min (Table 1).
Direct sequencing was performed with the BigDye® terminator cycle sequencing ready reaction kit on an ABI prism 3730xl automated genetic analyzer. RP1 gene variant identified through NGS was confirmed with Sanger Sequencing. The PCR conditions were common for both the genes except annealing temperature (Table 1). The results obtained from Sanger Sequencing of genes were analyzed using BLASTN tools.
Multiplex ligation-dependent probe amplification (MLPA) assay
MLPA was performed using a commercially available kit (Cat. No. P325-A3 OCA2; MRC Holland) to identify the deletions in the TYR gene. A total of 5 µl DNA sample was heat-denatured for 5 min at 98 °C. Samples were cooled down to room temperature. The hybridization master mix (3 µl) was added to DNA and incubated for 1 min at 95 °C, and then the probes were hybridized for 16 h at 60 °C. Thermo cycler temperature was lowered to 54 °C, and a 32 µl ligase-65 master mix was added and incubated for 15 min at 54 °C for ligation of hybridized probes. The ligase enzyme was heat-inactivated at 98 °C for 5 min and cooled down to room temperature; a 10 µl polymerase master mix was added at room temperature to amplify ligated probes. PCR condition was for 35 cycles (95°c 30 s, 60°c 30 s, 72°c 60 s, 72°c 20 min, 15°c pause). Fragment separation by capillary electrophoresis was performed using an automated sequencer (ABI 3730xl). Results were analyzed using Coffalyser software. Each MLPA probe consisted of two hemi-probes that bind to adjacent sites on the target sequence. Upon ligation and subsequent PCR amplification, each distinct MLPA probe (specific to distinct target regions) generated an amplicon with a unique length, were separated and quantified by capillary electrophoresis. Heterozygous deletions within target sequences would prevent efficient probe binding and give a 35–50% reduced relative peak area of the amplification product specific to that probe set. The copy number differences of various exons between test and control DNA samples were detected by analyzing the MLPA peak patterns.
Array-comparative genomic hybridization (array-CGH)
Array-CGH was performed on DNA samples using SurePrint G3 Human CGH + SNP, 8*60 K array. The data was analyzed using CytoGenomics 5.0.0.38 (Agilent, Santa Clara, California, USA), and nomenclature of Copy Number Variations (CNVs) was done using ACMG guidelines [17]. All genomic positions were reported according to the human genome reference assembly (GRCh37).
Bioinformatics analysis
The sequences obtained from TES were aligned to the human reference genome (GRCh37/hg19) using the BWA program and analyzed using Picard and GATK version 3.6 to identify the variants relevant to the clinical indication. The GATK practices framework was followed for the identification of variants. The VEP program against Ensembl release 87 human gene model was used to perform Gene annotation of variants. Human Genome databases (ClinVar, OMIM, and HGMD) were used to annotate identified variants. The effects of these variants were calculated using Mutation Taster2.
In silico amino acid conservation site was analyzed using Multiple Amino Acid Sequence Alignment software (https://www.ebi.ac.uk/Tools/msa/clustalo). The protein sequences RP1 derived from humans, chimpanzees, rhesus monkeys, dogs, horses, murine, and cattle were compared. The RP1 protein functional analysis was done using online ScanPrositeExpasy software (https://prosite.expasy.org/scanprosite).
Results
We have studied the family having three children affected with albinism & subjected to NGS (Additional file 1: Table S1). The NGS analysis failed to cover the TYR gene exon 3 region of affected subjects, otherwise usually well covered in healthy individuals. After multiple attempts, amplification of the TYR gene exon 3 in all three children using conventional PCR was failed. Multiplex Ligation-dependent Probe Amplification (MLPA) analysis revealed a novel large homozygous deletion (Probe ratio 0.00) of exon 3 of TYR gene in all the three children (Fig. 1a). A heterozygous deletion of exon 3 of the TYR gene was identified in the mother (Probe ratio 0.47) and father (Probe ratio 0.49) (Fig. 1b). The novel deletion detected in the present study was submitted in the ClinVar database (Accession no: SCV001448215).
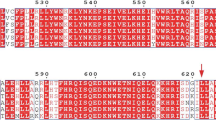
The further analysis through NGS revealed a novel heterozygous nonsense variation in exon 4 of the RP1 gene (chr8:55541078C > T; Depth: 55x) in the first child. Sanger Sequencing analysis confirmed the presence of RP1 gene variation (p.Gln1546Ter) in all the three children, mother, and maternal grandfather (Fig. 2a–c, e, f). The RP1 gene variant was absent in the father (Fig. 2d). The p.Gln1546Ter variation resulted in a stop codon and premature truncation of the protein at codon 1546 (p.Gln1546Ter; ENST00000220676.1). In silico prediction of the RP1 gene variant (p.Gln1546Ter) was disease-causing (probably deleterious) by MutationTaster2. The evolutionary conservation of RP1 variant p.Q1546Ter was determined by Multiple Amino Acid Sequence Alignment software. The RP1 protein sequences derived from human, chimpanzee, rhesus monkey, dog, horse, murine, and cattle showed that the residue-1546 was moderately conserved among all the primates (Fig. 2g, h).
Chromatogram showing heterozygous RP1 variation: (a) Mother (b) First child (c) Third child (d) Father (e) Second child (f) Maternal grandfather (g) Multiple amino acid sequence alignment analysis shows that the Amino acid p.Q1546 is moderately conserved among the primates (h) In silico RP1 protein functional analysis illustrating the functional domain, enzyme active site and the variation site
The array-CGH analysis revealed that the 1st child had paternally inherited 2.6 MB deletion in chromosome 10q23 region {arr[GRCh37] 10q23.2q23.31 (88816618_91483662) × 1} and 1.9 MB deletion in chromosome 15q11 region {arr[GRCh37] 15q11.1q11.2 (20575646_22509254) × 1} (Fig. 3a, b, d, g). However, the second child (female) was identified with only one paternally inherited CNVs (15q11.1-> 15q11.2) {arr[GRCh37] 15q11.1q11.2(20575646_22509254) × 1} (Fig. 3e, g).The 3rd child (male) was detected with paternally inherited CNVs (15q11.1-> 15q11.2) along with a denovo duplication (7.6 MB) of chromosome region 13q31.1-> 13q31.3 {arr[GRCh37] 13q31.1q31.3 (83199241_90822978) × 3} (Fig. 3c, f, g). Further, array CGH analysis in mother revealed no indication of CNVs.
Array- CGH karyogram showing: a, b Deletion of chromosomal region 10q23.2q23.31 in first child and father (Left to right) c Denovo duplication of chromosomal region 13q31.1q31.3 in the third child (male) d–g Deletion of chromosomal region 15q11.1q11.2 in first, the second and third child and father (Left to right)
The pedigree analysis revealed autosomal recessive inheritance of OCA1B from the parents to all three children (Fig. 4). The ID in the first-born male child was found to be associated with 10q23.2-> 23.31 deletion inherited from father, while in the 3rd child (male), ID was found to be associated with a denovo 13q31.1-> 13q31.3 duplication.
Discussion
OCA is a genetically heterogeneous congenital disorder characterized by low or absence of pigmentation in the hair, skin, and eyes. The OCA1B (OMIM# 606952) occurs due to autosomal recessive inheritance of a pathogenic mutation in the TYR gene [3]. So far, more than 320 TYR gene mutations and polymorphisms, including large multiple exon deletions have been reported in the Human Gene Mutation Database (https://www.hgmd.cf.ac.uk/ac/index.php/) provided in the public domain by the Institute of Medical Genetics, Cardiff, Wales, UK) and the Albinism Database (http://albinismdb.med.umn.edu/). The large deletion in the TYR gene was first reported by Schnur et al. in 1996 in an OCA1B patient who had compound heterozygous mutations of a TYR gene [18, 19]. Further, Sun et al. reported 12 TYR gene mutations in a total of 10 patients with OCA1. However, none of these studies have reported co-inheritance of OCA 1B and ID. In our study, we have identified a rare homozygous deletion of exon 3 in the TYR gene. To the best of our knowledge, this is the first case of large deletion of exon 3 in the TYR gene from the Indian population. This mutation has not been reported in any human mutation databases, including the albinism database so far. However, exon 3 deletion was first described by Mauri et al. in a single Turkish family affected with albinism [20]. The TYR gene exon 3 region encodes a copper B binding region bound by three conserved histidine residues, stimulating the tyrosinase enzyme activity. Tyrosinase protein encoded by the TYR gene is a copper monooxygenase that catalyzes the hydroxylation of tyrosine to dopaquinone in the melanin biosynthetic pathway and oxidation of L-DOPA [10]. In our case, reduced melanin synthesis is due to homozygous deletion of exon 3 of the TYR gene leading to inactivation of the tyrosinase enzyme. Blaszczyk et al. reported a case with exon 4 deletion in a non-human mammal, albino ferrets (Mustela Putorius Furo), which was similarly affected with hypo-pigmentation [21]. However, multiple exonic deletions have been reported in OCA1B subjects (http://albinismdb.med.umn.edu/). Our extensive literature search revealed that the different mutations within the tyrosinase-coding region causes OCA1 disorders of varying severity [22]. In the present study, whole exon 3 of the TYR gene is deleted in siblings inherited through autosomal recessive inheritance. Hence homozygous recessive genes transmitted through parental consanguinity have a high risk of developing genetic diseases.
The Retinitis Pigmentosa (RP) is a genetic disorder of the eye that leads to decreased peripheral vision where night blindness is caused by mutation in 50 genes including RP1 gene [23, 24]. In our study, a heterozygous RP1 gene variation (p.Gln1546Ter) was identified in all three children, mother and maternal grandfather. The RP1 gene variants identified in the family may not be associated with the phenotype due to the haploinsufficiency of the NDK isoenzyme [25]. However, follow-up of these patients is important to assess the future development of the RP.
The genetic basis of ID, multiple congenital anomalies (MCA), and an autism spectrum disorder (ASD) in children is not completely understood. However, CNVs identified by array-CGH have been reported in children affected with ID [26]. The co-occurrence of ID and OCA is a rare clinical presentation and diagnosis is challenging through clinical evaluation. We have studied CNVs in the affected siblings and their parents to understand the molecular basis of ID. The 10q23.2-> 10q23.31 deletion identified in our study is inherited by the 1st child from his father. Chromosome 10q23 contains more than five OMIM genes (PTEN, KLLN, ACTA2, FAS, LIPA, and SLC16A12). This chromosomal region is associated with several conditions, including ID (Additional file 1: Table S2). In the present study, the father and the child had a history of delayed development and poor social behavior, which may be associated with the deletion of chromosomal 10q23.2-> 10q23.31 region. According to the literature, the PTEN gene resides on 10q23.2-> 10q23.31 chromosomal region and is reported to be associated with neurological functions [27, 28]. The subjects with PTEN gene mutations have a high risk of autism spectrum disorder, macrocephaly, and cognitive deficits [29, 30]. The additional clinical presentation (ID) in the first child may be due to the loss of multiple genes, including the PTEN gene in the 10q23.2-> 10q23.31 region. The SLITRK1 and SLITRK6 genes located on 13q31.1-> 13q31.3 region are known to be associated with ID, ADHD, and facial dysmorphism [31]. Hence a denovo duplication (7.6 MB) of chromosome 13q31.1-> 13q31.3 region identified in the third child may be associated with ID. The duplication of 13q has also been reported in cases with autistic behavior, developmental delay, dysmorphism, including broad thumbs, strabismus, trigonocephaly (Additional file 1: Table S3).
The SLITRK1 gene is located in the 13q31.1 region and is associated with Gilles de la Tourette's syndrome (OMIM-137580). The individuals affected with these CNVs generally present with hyperactivity, impulsivity, repetitive movements [32]. However, more critical investigation of the genes involved in the duplication can provide precise genotype–phenotype correlation. Though paternally inherited deletion of 15q11.1-> 11.2(Chr coordinates: 20,575,646–22,784,582) present in all three siblings, the female sibling has no presentation of ID. Hence it indicates that 15q11.1-> 11.2 deletion may not be associated with ID. Genotype–phenotype correlation revealed that the exon3 deletion of the TYR gene is associated with the phenotype of OCA1B, and additional clinical presentation (ID) may be due to co-segregation of pathogenic CNVs in the family. Therefore, molecular evaluation is important for appropriate genetic counseling and management of the disease.
Conclusion
The OCA1B phenotype in children is due to the autosomal recessive inheritance of a rare exon 3 deletion of the TYR gene, which was identified through systemic molecular strategy. The additional clinical presentation (ID) may be due to the CNVs identified by array CGH. Therefore, a combination of genetic approaches is essential in cases with a complex phenotypic presentation for early diagnosis and better disease management.
Availability of data and materials
The human reference genome (GRCh37/hg19) (http://www.ensembl.org/) was used for the interpretation of genomic data. The project data is deposited under BioProject database with accession ID: PRJNA776081 (https://www.ncbi.nlm.nih.gov/bioproject/776081). Biosample IDs for all the participants are SAMN22713530, SAMN22713529, SAMN22713528, SAMN22713527, SAMN22713526, SAMN22705527, SAMN22696442 linked to BioProject PRJNA776081 (https://www.ncbi.nlm.nih.gov/bioproject/776081). The variants identified in TYR and RP1 gene are submitted to ClinVar under accession IDs SCV001448215 cited as “National Center for Biotechnology Information. ClinVar; [VCV000992661.1], https://www.ncbi.nlm.nih.gov/clinvar/variation/VCV000992661.1 (accessed Dec. 2, 2021)” and SCV002003955 cited as “National Center for Biotechnology Information. ClinVar; [VCV001315572.1], https://www.ncbi.nlm.nih.gov/clinvar/variation/VCV001315572.1 (accessed Dec. 2, 2021) respectively”. The details of NGS data is submitted to NCBI Sequence Read Archive under accession ID SRX13085209 (https://www.ncbi.nlm.nih.gov/sra?linkname=bioproject_sra_all&from_uid=776081) / SRP345279 (https://trace.ncbi.nlm.nih.gov/Traces/sra/?study=SRP345279) / SRR16892488 (https://trace.ncbi.nlm.nih.gov/Traces/sra/?run=SRR16892488). The RP1 gene sequences are submitted to GeneBank through BankIt under submission ID 2,515,543, the accession numbers are OL351360—https://www.ncbi.nlm.nih.gov/nuccore/OL351360. OL351361—https://www.ncbi.nlm.nih.gov/nuccore/OL351361. OL351362—https://www.ncbi.nlm.nih.gov/nuccore/OL351362. OL351363—https://www.ncbi.nlm.nih.gov/nuccore/OL351363. OL351364—https://www.ncbi.nlm.nih.gov/nuccore/OL351364. OL351365—https://www.ncbi.nlm.nih.gov/nuccore/OL351365. The array CGH data is submitted to GEO data base under project ID PRJNA785601 (https://www.ncbi.nlm.nih.gov/bioproject/PRJNA785601); with accession # GEO: GSE190026 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE190026).
Change history
18 January 2022
A Correction to this paper has been published: https://doi.org/10.1186/s12920-022-01159-2
Abbreviations
- TYR :
-
Tyrosinase
- RP1 :
-
Retinitis pigmentosa 1
- OCA 1:
-
Occulocuteneous albinism 1
- ID:
-
Intellectual disability
- MLPA:
-
Multiplex ligation-dependent probe amplification
- NGS:
-
Next-generation sequencing
- CNVs:
-
Copy number variations
- CGH:
-
Comparative genomic hybridization
- HPS:
-
Hermansky–Pudlak syndrome
- CHS:
-
Chediak–Higashi syndrome
- GS:
-
Griscelli syndrome
- CMBS:
-
Cross-McKusick-Breen syndrome
- ADHD:
-
Attention deficit-hyperactivity disorder
- BERA:
-
Brainstem evoked response audiometry
- TES:
-
Targeted exome sequencing
- SS:
-
Sanger sequencing
- OMIM:
-
Online mendelian inheritance in man
- PCR:
-
Polymerase chain reaction
- ACMG:
-
American College of Medical Genetics
- HGMD:
-
Human gene mutation database
- MCA:
-
Multiple congenital anomalies
- ASD:
-
Autism spectrum disorder
References
Spritz RA, Chiang PW, Oiso N, Alkhateeb A. Human and mouse disorders of pigmentation. Curr Opin Genet Dev. 2003;13(3):284–9.
Montoliu L, Grønskov K, Wei AH, Martínez-García M, Fernández A, Arveiler B, Morice-Picard F, Riazuddin S, Suzuki T, Ahmed ZM, Rosenberg T. Increasing the complexity: new genes and new types of albinism. Pigment Cell Melanoma Res. 2014;27(1):11–8.
Federico JR, Krishnamurthy K. Albinism. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020. PMID: 30085560.
Grønskov K, Dooley CM, Østergaard E, Kelsh RN, Hansen L, Levesque MP, Vilhelmsen K, Møllgård K, Stemple DL, Rosenberg T. Mutations in c10orf11, a melanocyte-differentiation gene, cause autosomal-recessive albinism. Am J Hum Genet. 2013;92(3):415–21.
Wei AH, Zang DJ, Zhang Z, Liu XZ, He X, Yang L, Wang Y, Zhou ZY, Zhang MR, Dai LL, Yang XM. Exome sequencing identifies SLC24A5 as a candidate gene for nonsyndromic oculocutaneous albinism. J Investig Dermatol. 2013;133(7):1834–40.
Grønskov K, Ek J, Brondum-Nielsen K. Oculocutaneous albinism. Orphanet J Rare Dis. 2007;2(1):1–8.
Mohamed AF, El-Sayed NS, Seifeldin NS. Clinico-epidemiologic features of oculocutaneous albinism in northeast section of Cairo-Egypt. Egypt J Med Hum Genet. 2010;11(2):167–72.
Cooksey CJ, Garratt PJ, Land EJ, Pavel S, Ramsden CA, Riley PA, Smit NP. Evidence of the indirect formation of the catecholic intermediate substrate responsible for the autoactivation kinetics of tyrosinase. J Biol Chem. 1997;272(42):26226–35.
Fryer JP, Oetting WS, Brott MJ, King RA. Alternative splicing of the tyrosinase gene transcript in normal human melanocytes and lymphocytes. J Investig Dermatol. 2001;117(5):1261–5.
Aigner B, Besenfelder U, Müller M, Brem G. Tyrosinase gene variants in different rabbit strains. Mamm Genome. 2000;11(8):700–2.
Scheinfeld NS. Syndromic albinism: a review of genetics and phenotypes. Dermatol Online J. 2003. https://doi.org/10.5070/D30FB7F671.
Boissy RE. Dermatologic Manifestations of Albinism: Background, Pathophysiology, Etiology of Albinism, Epidemiology, Prognosis, Patient Education [Internet]. 2019 [cited 2021 May 13]. https://emedicine.medscape.com/article/1068184-overview
Chinagi DR, Patil LS, Giraddi T, Ugargol P. Scholars Journal of Medical Case Reports ISSN 2347-6559 (Online).
Arons B, Kosek JC, Forrest IS. Chlorpromazine therapy in a female albino mental patient: clinical, histochemical and biochemical observations. Life Sci. 1968;7(24):1273–80.
Rinchik EM, Bultman SJ, Horsthemke B, Lee ST, Strunk KM, Spritz RA, Avidano KM, Jong MT, Nicholls RD. A gene for the mouse pink-eyed dilution locus and for human type II oculocutaneous albinism. Nature. 1993;361(6407):72–6.
Lee ST, Nicholls RD, Bundey S, Laxova R, Musarella M, Spritz RA. Mutations of the P gene in oculocutaneous albinism, ocular albinism, and Prader-Willi syndrome plus albinism. N Engl J Med. 1994;330(8):529–34.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–23. https://doi.org/10.1038/gim.2015.30.
Sun W, Shen Y, Shan S, Han L, Li Y, Zhou Z, Zhong Z, Chen J. Identification of TYRmutations in patients with oculocutaneous albinism. Mol Med Rep. 2018;17(6):8409–13.
Schnur RE, Sellinger BT, Holmes SA, Wick PA, Tatsumura YO, Spritz RA. Type I oculocutaneous albinism associated with a full-length deletion of the tyrosinase gene. J Investig Dermatol. 1996;106(5):1137–40.
Shahzad M, Yousaf S, Waryah YM, Gul H, Kausar T, Tariq N, Mahmood U, Ali M, Khan MA, Waryah AM, Shaikh RS. Molecular outcomes, clinical consequences, and genetic diagnosis of Oculocutaneous Albinism in Pakistani population. Sci Rep. 2017;7(1):1–5.
Blaszczyk WM, Distler C, Dekomien G, Arning L, Hoffmann KP, Epplen JT. Identification of a tyrosinase (TYR) exon 4 deletion in albino ferrets (Mustela putorius furo). Anim Genet. 2007;38(4):421–3.
Opitz S, Käsmann-Kellner B, Kaufmann M, Schwinger E, Zühlke C. Detection of 53 novel DNA variations within the tyrosinase gene and accumulation of mutations in 17 patients with albinism. Hum Mutat. 2004;23(6):630–1.
Liu Q, Collin RWJ, Cremers FPM, den Hollander AI, van den Born LI, et al. Expression of wild-type Rp1 protein in Rp1 knock-in mice rescues the retinal degeneration phenotype. PLoS ONE. 2012;7(8):e43251.
Fahim AT, Daiger SP, Weleber RG. Nonsyndromic retinitis pigmentosa overview. GeneReviews®[Internet]. 2017
Agarwal RP, Parks RE Jr. Erythrocytic nucleoside diphosphokinase: V. Some properties and behavior of the pi 7.3 isozyme. J Biol Chem. 1971;246(7):2258–64.
Miller DT, Adam MP, Aradhya S, Biesecker LG, Brothman AR, Carter NP, Church DM, Crolla JA, Eichler EE, Epstein CJ, Faucett WA. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet. 2010;86(5):749–64.
Lee SH, Ryoo E, Tchah H. Bannayan–Riley–Ruvalcaba syndrome in a patient with a PTEN mutation identified by chromosomal microarray analysis: a case report. Pediatr Gastroenterol Hepatol Nutr. 2017;20(1):65–70.
Bennett KL, Mester J, Eng C. Germline epigenetic regulation of KILLIN in Cowden and Cowden-like syndrome. JAMA. 2010;304(24):2724–31.
Waite KA, Eng C. Protean PTEN: form and function. Am J Hum Genet. 2002;70(4):829–44.
Varga EA, Pastore M, Prior T, Herman GE, McBride KL. The prevalence of PTEN mutations in a clinical pediatric cohort with autism spectrum disorders, developmental delay, and macrocephaly. Genet Med. 2009;11(2):111–7.
Quelin C, Spaggiari E, Khung-Savatovsky S, Dupont C, Pasquier L, Loeuillet L, Jaillard S, Lucas J, Marcorelles P, Journel H, Pluquailec-Bilavarn K. Inversion duplication deletions involving the long arm of chromosome 13: phenotypic description of additional three fetuses and genotype–phenotype correlation. Am J Med Genet A. 2014;164(10):2504–9.
Menten B, Maas N, Thienpont B, Buysse K, Vandesompele J, Melotte C, de Ravel T, Van Vooren S, Balikova I, Backx L, Janssens S. Emerging patterns of cryptic chromosomal imbalance in patients with idiopathic mental retardation and multiple congenital anomalies: a new series of 140 patients and review of published reports. J Med Genet. 2006;43(8):625–33.
Acknowledgements
We thank the family for their participation in the study.
Funding
Institutional core grant received from the Indian Council of Medical Research (ICMR) to carry out cytogenetic and molecular genetics research in the Cytogenetic department.
Author information
Authors and Affiliations
Contributions
SD, JG & JS collected family history and performed an evaluation. BRV, SD, JS contributed to the conception and designing of work. PP, AS & JG performed molecular work, genetic evaluation, acquisition, and data analysis. SD, PP & BRV reviewed the literature and drafted the manuscript. PP performed the In-silico analysis of variants identified. BRV, AS & JS performed substantive revision of the manuscript. BRV performed general supervision of the research work. JS & AS deposited all archiveable data to the respective repositories. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study protocols were approved by the “Institutional Ethics Committee on human subjects” of ICMR-National Institute of Immunohaematology. (Ethics approval number: NIIH/IEC/22–2019). Peripheral blood was collected for genetic analysis after a written and informed consent was obtained from the participants and the parents for minors.
Consent for publication
Written Informed consent was obtained from the family for the publication of anonymous clinical details. For all the three children (below 18 years) written informed consent was taken in from the mother.
Competing interests
All the authors declared no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: “Figure 1 has been updated and merged words have been corrected”
Supplementary Information
Additional file
1. Table S1: List of Genes associated with OCA and RP1 tested through NGS. Table S2: Clinical features of patients associated with deletion of chromosome 10q region. Table S3: Clinical features of patients associated with duplication of chromosome 13q region..
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dhangar, S., Panchal, P., Ghatanatti, J. et al. Novel deletion of exon 3 in TYR gene causing Oculocutaneous albinism 1B in an Indian family along with intellectual disability associated with chromosomal copy number variations. BMC Med Genomics 15, 2 (2022). https://doi.org/10.1186/s12920-021-01152-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-021-01152-1