Abstract
Background
We aimed to examine the role of the rs6060566 polymorphism of the reactive oxygen species modulator 1 (ROMO1) gene in the development of myocardial infarction (MI) in Caucasians with type 2 diabetes (T2DM).
Methods
A total of 1072 subjects with T2DM were enrolled in this cross-sectional case–control study: 335 subjects with MI and 737 subjects without clinical signs of coronary artery disease (CAD). The genetic analysis of the rs6060566 polymorphism was performed in all subjects. To assess the degree of coronary artery obstruction, a subpopulation of 128 subjects with T2DM underwent coronary computed tomography angiography. Next, endarterectomy samples were obtained during myocardial revascularization from diffusely diseased coronary arteries in 40 cases, which were analysed for ROMO1 expression according to their genotype.
Results
There were no statistically significant associations between different genotypes or alleles of the rs6060566 polymorphism and MI in subjects with T2DM. The carriers of the C allele of the ROMO1 rs6060566 had a threefold increased likelihood of having 50–75% coronary artery stenosis (Adjusted OR = 3.27, 95% CI 1.16–9.20). Subjects with two affected coronary arteries had a 3.72 fold higher prevalence of MI (OR = 3.72, 95% CI 1.27–10.84). With CAD in LMCA or LAD, MI prevalence was about 3.5-fold higher (p = 0.07 for LMCA and p = 0.01 for LAD). Furthermore, the carriers of the rs6060566 C allele showed higher number of positive cells for ROMO1 expression in endarterectomy samples of coronary arteries.
Conclusions
According to our study, the rs6060566 polymorphism of the ROMO1 gene is not a risk factor for MI in Caucasians with T2DM. However, we found that subjects carrying the C allele were at a 3.27-fold increased risk of developing severe CAD compared with those who had non-obstructive CAD. Moreover, C allele carriers showed a statistically higher number of cells positive for ROMO1 compared with T allele carriers in coronary endarterectomy samples.
Similar content being viewed by others
Background
Type 2 diabetes mellitus (T2DM) is a heterogeneous group of metabolic disorders that affects around 8% of the world population and was thought to be responsible for 5 million deaths in 2015 worldwide [1]. In addition, it is one of the major risk factors for coronary artery disease (CAD), and more than 40% of patients with acute coronary syndrome (ACS) have DM [2]. CAD is characterized by atherosclerosis in epicardial coronary arteries and can be asymptomatic, whereas ACS usually presents with a symptom, such as unstable angina, and is frequently associated with myocardial infarction (MI) regardless of the presence of CAD [3]. Because of the proatherosclerotic, proinflammatory, and prothrombotic states associated with diabetes, diabetic patients with ACS are at high risk of subsequent cardiovascular events [4]. The 7-year risk of developing MI in diabetic patients was comparable to the risk of MI in non-diabetic patients with prior MI, which suggests that diabetes contributes significantly to the development of MI and can be considered as possible CAD risk equivalent [5].
In a physiological system, the imbalance between antioxidant defence mechanism and reactive oxygen species (ROS) production leads to oxidative stress and subsequent pathological conditions [6]. CAD occurs as a consequence of accelerated atherosclerosis, mainly driven by oxidative stress [7]. Numerous defence genes are involved in maintaining the balance between oxidant production and their removal by ROS-scavenger enzyme systems.
Reactive oxygen species modulator1 (ROMO1) gene is located in chromosome 20q11.22 [8] and produces a small transmembrane protein located in the inner mitochondrial membrane. It is a unique nonselective cation channel that is suggested to be regulated in response to fluctuation in free iron concentration and of its redox state [9]. Nevertheless, ROMO1 is vital for normal mitochondrial morphology and function [10], while its activation induces ROS production in the mitochondrial respiratory chain leading to oxidative stress and cell death [11]. Moreover, ROMO1 is involved in cell proliferation [12], cell apoptosis [13], it is thought to have a role in replicative senescence [14] as well as in carcinogenesis and tumour progression [15].
ROMO1 gene and its polymorphisms are relatively understudied. The role of ROMO1 in oxidative stress is well established. In addition, current knowledge on pathophysiology of CAD and MI sets oxidative stress as one of the key pathogenic mechanisms in its development [7] which is more prominent in T2DM subjects. Up until now, only one study has examined the relationship between ROMO1 polymorphism and vascular complications of T2DM [16]. Therefore, our study aimed to assess the potential role of the ROMO1 polymorphism rs6060566 in the development of MI in Slovenian subjects with T2DM. Furthermore, we also explored ROMO1 expression in coronary endarterectomy specimens with immunohistochemical staining.
Methods
Subjects
This retrospective cross‐sectional case–control study enrolled 1072 unrelated Caucasians with T2DM of at least 10 years’ duration. Participants were divided into two study groups: 335 subjects with MI and 737 subjects with no history of CAD, no signs of ischemic changes on electrocardiogram and no ischemic changes during submaximal stress testing; however, in these control subjects CAD could be clinically silent. Subjects were classified as having T2DM according to the current American Diabetes Association criteria [17]. The diagnosis of MI was made according to the established universal criteria [18]. Subjects with MI were included in the study 1–9 months after the acute event. Subjects without T2DM were not enrolled, because they have lower incidence of MI and lower levels of oxidative stress. Consequently, their inclusion would confound the presumed relation of MI to ROMO1 polymorphism.
Further, to assess the degree of coronary artery obstruction, a subpopulation of 128 subjects from both groups with T2DM underwent coronary computed tomography angiography (CTA) for diagnostic purposes at the International Centre for Cardiovascular Diseases MC Medicor, Izola, Slovenia. Subjects from the original control group (104 subjects) who were included in this substudy had normal echocardiography at rest and, therefore, low clinical likelihood of obstructive CAD according to 2019 European Society of Cardiology (ESC) guidelines for the diagnosis and management of chronic coronary syndromes. Subjects from original MI group (24 subjects) had coronary CTA prior to MI and, therefore, prior to the inclusion in this study. Non-invasive visualization of the epicardial coronary artery tree and the detection of stenosis were performed on dual source Dual energy CT scanner (Siemens, Germany). The acquisition and reading of the coronary CT angiograms were assessed by B.C., a senior expert cardiac radiologist. Normal coronary arteries were defined by the absence of obstructive or non-obstructive atherosclerotic plaque in the epicardial coronary tree. Non-obstructive CAD was defined by the presence of plaque occupying a cross-sectional area stenosis < 50%. The severity of CAD was classified by the degree of stenosis of the cross-sectional area (< 50%, ≥ 50—% ≤ 75% and > 75%) and by the number of diseased vessels (score from 0 to 3; as 0 for no vessel disease (VD), 1 for single VD, 2 for double VD and 3 for triple VD). Angiographically diagnosed diseased left main coronary artery (LMCA) was scored as 1 whilst ignoring stenosis of any of the two major branches: left anterior descending (LAD) or left circumflex (LCx). In addition, if LMCA was not affected by atherosclerosis, we assigned score 1 for each LAD or/and LCx, respectively. At last, diseased right coronary artery (RCA) was scored as 1.
All subjects enrolled in the study were of Caucasian ethnicity. After an informed consent for the participation in the study was obtained, a detailed interview (Additional file 1: The questionnaire) was made including active smoking status. For assessing the cardiovascular risk status of individual subject the Framingham equitation was used (Additional file 1: Cardiovascular risk assessment) and past or current comorbid conditions were taken into account (Additional file 1: Other comorbidities).
Furthermore, their blood was drawn for biochemical analysis and genotyping. Body mass index (BMI) was calculated as weight in kilograms divided by the height in meters square.
Biochemical analyses
Fasting glucose, high total cholesterol, low density lipoproteins (LDL), high density lipoproteins (HDL), and triglycerides were determined by standard colorimetric assays on an automated biochemistry analyser (Ektachem 250 Analyser, Eastman Kodak Company, Rochester, MN, USA). The serum level of low density lipoprotein (LDL)-cholesterol was calculated by the Friedewald formula (Friedewald et al. 1972). Hyperlipidaemia was defined as total cholesterol higher than 5 mmol/L and/or triglycerides higher than 2 mmol/L, or as a condition treated with hypolipidemic medications.
Glycated haemoglobin (HbA1c) values (non-diabetic reference range of 3.8–5.3%) were estimated by high-performance liquid chromatography. Three recent HbA1c levels were averaged for each subject. High sensitivity C-reactive protein (hsCRP) was measured using a latex enhanced immunonephelometric assay.
Moreover, we assessed oxidative stress in a subgroup of 115 subjects with T2DM with no experience of MI (23 with CAD (CAD+) and 92 without CAD (CAD−) by examining the serum levels of 8-hydroxy-2′-deoxygunosine (8-OHdG), a known marker for oxidative DNA damage. 8-OHdG levels were measured by commercially available enzyme-linked immunosorbent assay (ELISA) kit (IBL International GmbH, Hamburg, Germany) according to the manufacturer’s instructions. The ELISA kit uses a highly sensitive monoclonal antibody against 8-OHdG with an assay sensitivity of 0.5 ng/mL and intra- and interassay coefficients of variation of less than 10%.
Genotyping
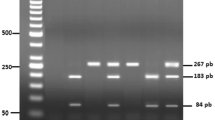
Genomic DNA was extracted from 100 μL of whole blood using a Qiagen isolation kit. The rs6060566 polymorphism of the ROMO1 gene was genotyped by KBioscience Ltd using their own novel fluorescence‐based competitive allele‐specific PCR (KASPar) assay. Details of the method used can be found at http://www.kbioscience.co.uk/.
Immunohistochemistry
In the second part of the study we included 40 subjects with T2DM with angina pectoris who had surgical myocardial revascularization. Coronary endarterectomy tissue samples were obtained during myocardial revascularization from diffusely diseased coronary arteries. With respect to different rs6060566 genotypes, relative expression for ROMO1 in resected tissue samples was analysed by immunohistochemistry.
Sections from formalin-fixed, paraffin-embedded tissue blocks of 40 coronary endarterectomy specimens were cut at a thickness of 5 µm. Immunohistochemistry was carried out using a VENTANA BenchMark Ultra Slide Staining System (Roche Diagnostics). Endarterectomy specimens were stained with antibody against ROMO1 (1:100, rabbit polyclonal, HPA012782, Sigma Prestige Antibodies, St. Louis U.S.A.). The detection of primary rabbit immunoglobulins was carried out with the NovoLink Max Polymer Detection System (Leica Biosystems Newcastle Ltd, United Kingdom) following the manufacturer’s instructions. The sections were further incubated with chromogen diamonobenzidine (DAB). Subsequently, reaction with the peroxidase produced a brown precipitate at the ROMO1 sites. Using a light microscope (Axio Scope 2, Zeiss Group, Germany), two researchers P.N. and D.P. independently evaluated the slides and manually counted ROMO1 positive cells at 400 × magnification. Numerical areal density of cells that were immunoreactive for ROMO1 was calculated (the number of positive cells per mm2) as described before [19].
Statistical analysis
Normally distributed continuous variables were expressed as means ± standard deviations, and as median (interquartile range) when asymmetrically distributed. The normality of the continuous variables was examined by the Kolmogorov–Smirnov test. Normally distributed continuous variables were tested using an unpaired Student̕ s t test, and the Mann–Whitney U-test when asymmetrically distributed. Discrete variables were compared with Pearson χ2 test, which was also used to test whether the genotypes distribution departures form Hardy–Weinberg equilibrium. However, when in contingency table cells with expected frequencies < 5 were identified, the Fisher̕ s Exact test was used to determine if there is a significant relationship between two categorical variables.
Additionally, all variables that showed significant differences by univariate analysis were put into a stepwise multiple logistic regression.
The area-under-curve (AUC) of the receiver operating characteristic (ROC) curve for oxidative stress biomarker 8-OHdG was used to characterize utility for discriminating between CAD+ and CAD– among 115 subjects with T2DM and among 34 rs6060566 C allele carriers.
In order to provide the predictive power of the final multivariate logistic regression model, ROC curve analysis and the likelihood ratio test were applied.
A p value of < 0.05 was considered to be statistically significant. Statistical analysis was performed using the SPSS program version 19 (SPSS Inc. Chicago, IL).
Results
The clinical characteristics and biochemical parameters of the Slovenian subjects with T2DM are listed in Table 1. Cases (335 subjects with MI) had lower BMI, lesser waist circumference and better-controlled hypertension. Additionally, they had a higher total and LDL-cholesterol, triglycerides, and lower HDL-cholesterol. Moreover, cases had longer duration of T2DM. The two groups of subjects were well-matched with regard to age, gender, fasting glucose, HbA1c, hsCRP level and concomitant history of cerebrovascular insult (CVI) or transitory ischemic attack (TIA).
To address the issue of the oxidative stress status for CAD in subjects with T2DM without history of previous MI, the oxidative damage of DNA was evaluated by measuring the serum level of 8-OHdG. However, in the subgroup of 115 subjects with T2DM no significant difference in the median serum level was observed when 23 subjects with CAD (CAD+) and 92 subjects without CAD (CAD−) were compared [1.47 (range: 1.31–1.71) vs. 1.51 (1.3–1.73) ng/mL], respectively (p = 0.80, Mann–Whitney U-test). In addition, among the 34 rs6060566 C allele carriers, median serum level was higher in 9 CAD+ subjects when compared to 25 CAD− subjects [1.54 (range: 1.4–1.72) vs. 1.48 (1.33–1.69) ng/mL], respectively, but the difference was not statistically significant (p = 0.48, Mann–Whitney U-test).
Furthermore, the ROC curve analysis was used to evaluate if the serum level of 8-OHdG could serve as a biomarker for CAD. In neither of the examined groups, 8-OHdG had the ability to correctly classify subjects with T2DM as having CAD or not. Specifically, in each of the two groups, 8-OHdG yielded AUC values of 0.483 (95% CI 0.35–0.61) and 0.655 (95% CI 0.37–0.79), respectively, with p values far above the significance cutoff value (p = 0.05, ROC curve analysis).
Moreover, we found that oxidative stress in 34 C allele carriers (CC + CT genotypes) was not significantly different from the 81 TT carriers [1.49 (range: 1.36–1.71) vs. 1.51 (1.26–1.71) ng/mL], respectively (p = 0.70, Mann–Whitney U-test).
The genotype and allele frequencies of the ROMO1 rs6060566 polymorphism are shown in Table 2. Genotype distributions for both cases (subjects with MI) and controls (subjects without CAD) were in Hardy–Weinberg equilibrium (cases: p = 0.70; controls: p = 0.83, Pearson χ2 test; respectively). Moreover, in each of the studied groups, genotype (cases: p = 0.40 and controls: p = 0.21, Pearson χ2 test) and allele (cases: p = 0.24 and controls: p = 0.1, Pearson χ2 test) frequencies were not significantly different from those reported for the datasets in the 1000 Genomes Project Phase 3 European population.
Moreover, binary logistic regression analyses for different genetic models found no significant associations between different genotypes or alleles of the rs6060566 polymorphism and the risk of MI in Slovenian subjects with T2DM. Estimates of ORs were adjusted (adjusted ORs) (Table 3) for the variables (BMI, waist circumference, diastolic blood pressure, total cholesterol, HDL- and LDL-cholesterols, triglycerides, duration of DM in years) that were significant in the univariate analyses (Table 1).
Subjects who underwent coronary CTA did not show any significant differences in genotype and allele frequency distribution for the rs6060566 polymorphism (Table 4).
We performed multinomial logistic regression analyses to evaluate the association of the rs6060566 polymorphism with CAD in these subjects. Because of the low frequency of the minor C allele (Table 4) the analyses were performed assuming the dominant genetic model ([CC + CT] vs. TT). The final model is shown in Table 5. The dependent variables describing the severity of CAD were the number of diseased vessels and extent of stenosis (no diseased vessel and stenosis < 50% were used as references, respectively). Independent variables included in the model were dominant genetic model (TT genotype was used as reference), age, gender, lipid parameters and duration of T2DM in years. We did not observe any interactions between the dominant genetic model and CAD without adjustment for the possible confounders (Table 5). Nevertheless, when well-known CAD risk factors (age, gender, lipid parameters and duration of T2DM in years) were fixed in the model, the association between carriers of the [CC + CT] genotypes and ≥ 50% ≤ 75% cross-sectional area stenosis became statistically significant (p = 0.025, multinomial logistic regression). The carriers of the C allele of the ROMO1 rs6060566 had a threefold increased likelihood of having coronary artery stenosis (Adjusted OR = 3.27, 95% CI 1.16–9.20, Table 5). However, in a full fitted model, only dominant genetic model with CC + CT genotypes (Wald = 5.05, df = 1, p = 0.025, multinomial logistic regression) and triglycerides (Wald = 3.77, df = 1, p = 0.05, multinomial logistic regression) were independently associated with CAD in subjects who were diagnosed with ≥ 50%–≤ 75% stenosis. The model demonstrated the independent strength of the effect of the C allele; thus it appears that rs6060566 of the ROMO1 gene may contribute to CAD risk. Furthermore, the fit of the multivariate model was tested by ROC curve analysis. The predictive power of the final model, which included a dominant genetic model and additional risk factors—age, gender, lipid parameters and duration of T2DM—with the AUC of 0.729 (95% CI 0.61–0.85), was statistically significant (p < 0.001, ROC curve analysis). In addition, likelihood ratio test as a measure of the statistical significance of all predictors in the model showed a statistically significant score with the χ2 value of 27.62 (df = 16, p = 0.035, likelihood ratio test).
A total of 128 subjects with T2DM underwent coronary CTA (Fig. 1a–c). A single VD (1 VD) was observed in 22 (17%) subjects, two VD (2 VD) in 41 (32%) and three VD (3 VD) in 16 (13%) subjects. Moreover, in 49 (38%) subjects all major epicardial coronary arteries (LMCA, LAD, LCx and RCA) on CT angiograms (Fig. 1a) were normal. Moreover, 97 (76%) subjects had non-obstructive CAD (cross-sectional area stenosis of < 50%), in 28 (22%) subjects a cross-sectional area stenosis of ≥ 50%–≤ 75% was detected while only 3 subjects (2%) had stenosis of > 75% (Fig. 1a). As shown in Fig. 1a, subjects with 2 VD (14/41, 35%) and non-obstructive CAD (11/95, 11.3%) suffered from nonfatal MI more often than other subjects in both comparative groups (number of diseased vessels and percentage of cross-sectional area stenosis). Of note, there was a statistically significant difference (p = 0.0096, Pearson χ2 test) in the frequency distribution between subgroups with and without MI with regard to the extent of the CAD (Fig. 1a). In contrast, no difference (p = 0.283; Fisher’s Exact test) was observed between subgroups with regard to the coronary cross-sectional area stenosis (Fig. 1a). With regards to the number of the involved vessels, a significantly higher frequency (p = 0.013; Pearson χ2 test) of MI was found in subjects with 2 VD. Interestingly, subjects with two affected epicardial coronary arteries showed a 3.72-fold risk for MI (OR = 3.72, 95% CI 1.27–10.84, Fig. 1a).
Findings at coronary CTA. Distribution of Slovenian subjects with T2DM according to the extent and severity of CAD (a). Atherosclerotic burden in major coronary arteries (b). Relation between specific coronary artery and the risk of MI in subjects with CAD (CAD+) in comparison with subjects without CAD (CAD−) (c)
Coronary CTA revealed that more than 50% of the 128 subjects had developed CAD in LAD (Fig. 1b), while the remainder of the epicardial coronary arteries were spared of atherosclerotic disease more frequently. Atherosclerotic changes were noticed in LMCA in 39 subjects (30.6%), while a slightly higher percentage of atherosclerotic disease was seen in LCx and RCA (41%) (Fig. 1b). Furthermore, the relationship between the presence or absence of CAD with regards to coronary arteries was statistically significant (p = 0.055, Pearson χ2 test; Fig. 1b).
As depicted in Fig. 1c, subjects with CAD (CAD+) in LMCA or LAD had about 3.5-fold higher risk of experiencing MI (p = 0.07 for LMCA and p = 0.01 for LAD, Pearson χ2 test; respectively) compared with subjects without CAD (CAD−). However, in subjects with diseased LCx and RCA, MI occurred more frequently than in subjects with disease-free epicardial coronary arteries, although the difference was not statistically significant (p = 1.0 for LCx and p = 0.9 for RCA, Pearson χ2 test; respectively).
At the end of this study, the coronary artery segments, which were obtained by endarterectomy from subjects with advanced atherosclerosis, were examined with immunohistochemical staining. A statistically significantly higher numerical areal density of ROMO1 positive cells was found in 17 subjects with the C allele (Fig. 2) in comparison with 23 subjects with ROMO1 TT genotype (wild type) (835 ± 215/mm2 versus 412 ± 153/mm2; p < 0.001, Student̕ s t test).
Histology and immunohistochemistry for ROMO1 in endarterectomised tissue samples of coronary arteries (a–d) and positive controls (e–f): ROMO1 positive reaction in human kidney medulla (e) and testis (f). ROMO1 expression in representative tissue section in the C allele carrier of the rs6060566 polymorphism (a–c), c is a higher magnification of the square in b. A portion of the coronary artery (c) in which immunohistochemistry for ROMO1 reveals positive brown cells (arrows). No staining of cells in the coronary artery of the T allele carrier (d). Original magnification × 25 (a), × 100 (b, d, e) and × 400 (c, f)
Discussion
Our study investigated the role of oxidative stress ROMO1 gene polymorphism rs6060566 in Slovenian subjects with T2DM who experienced MI. We found no association of the rs6060566 polymorphism with MI. In contrast, we have identified a significant relationship between carriers of the [CC + CT] genotypes (under the assumption of the dominant genetic model) and ≥ 50%–≤ 75% cross-sectional area stenosis. Thus, we found that subjects carrying the C allele were at a 3.27-fold increased risk of developing severe CAD compared with those who had non-obstructive CAD. This contradiction in our results may be attributed to a slightly different pathophysiology of CAD and MI [7, 20]. CAD is a slowly progressive disease with inflammation and oxidative stress as main pathophysiologic factors, while MI is a complication of stable CAD caused by superficial plaque erosion, plaque rupture, erosion from calcium nodules or intraplaque haemorrhage. These triggers can be explained only in part by oxidative stress [20], and depend more on plaque vulnerability. Moreover, only 14% of occlusions leading to MI develop at sites of pre-existing high-grade stenosis (more than 70% in diameter) and more than two thirds of MIs occur on non-obstructive lesions (< 50% in diameter) [20].
To continue, a significantly higher frequency of MI was found in subjects with 2 VD as compared to the subjects in whom CAD was not detected by CTA. At first glance, it seems that the frequency of subjects with MI increased with the number of involved vessels. Our results are partly supported by in-depth study conducted on 12.594 diabetes patients by Gyldenkerne et al. [21] who found that the extent of CAD is a major risk factor for MI and death in patients with DM. We could not confirm this increased risk for MI in a group of subjects with 3 VD, most likely because of the small sample size. Another contributor could be our definition of the number of diseased vessels when LMCA was affected, which gave score of 1 disregarding LAD or LCX involvement. Although it is known that diabetic patients suffer from more extensive CAD and hence higher incidence of multi-vessel CAD than non-diabetic subjects [22], in our research, 3 VD was diagnosed only in 16 out of 128 subjects who underwent coronary CTA. It is important to note that all of them were diagnosed without atherosclerotic lesions in LMCA (due to the above-mentioned definition) and none of them has suffered a MI. Furthermore, all 16 subjects underwent either percutaneous coronary intervention (PCI) or coronary artery bypass grafting surgery (CABG). We may assume that appropriate myocardial revascularization strategy with optimal medical therapy led to reduced incidence of MI in this small group of Slovenian subjects with 3 VD. Recently, a large-scale meta-analysis based on 18.224 patients with DM undergoing PCI and CABG has demonstrated the superiority of CABG in reducing mortality, MI and the need for repeat revascularization in patients with DM and complex CAD (including LMCA and/or multivessel disease) [23]. However, our study did not examine clinical outcomes of PCI or CABG in subjects with complex CAD.
In our study, subjects with CAD localized in LMCA and LAD had a significantly higher occurrence of nonfatal MI compared to subjects without CAD in respective epicardial coronary arteries. In our study, they had about a 3.5-fold higher risk of MI. Our observations parallel with well-known facts that diabetes approximately doubles the risk of MI and death among patients with known CAD [24, 25]. On the other hand, the current study shows that MI is less frequent in subjects with disease-free epicardial coronary arteries. Thus, in the absence of angiographically significant CAD, patients with diabetes treated with contemporary prophylactic therapy have the same risk of cardiovascular events as patients without diabetes [26]. Therefore, optimal medical therapy and appropriate selection of myocardial revascularization strategy is critical for patients with DM [27].
T2DM patients are strongly prone to atherothrombotic complications in epicardial coronary arteries as well as in other macro- and microvasculature. One of the major contributors to susceptibility for atherothrombotic complications is genetic background [28]. Many studies [29, 30] have shown an association of different genetic loci and their polymorphisms with higher risk of atherosclerosis, CAD and MI. Numerous identified risk polymorphisms have no known pathophysiological function, but others are involved in inflammatory response, lipid function, transportation, endothelial dysfunction or oxidative stress regulation.
As oxidative stress is recognized as a central pathogenic process in accelerated atherosclerosis in T2DM, various studies [7] investigated the associations of oxidative stress genes (e.g. NADPH1 oxidase, Myeloperoxidase, Glutathione peroxidase 1, Glutathione S-transferase [31], NAD(P)H1: Quinone oxidoreductase, Superoxide dismutase 1 and 2 [32], Thioredoxin reductase 2 [33], Uncoupling protein 2 [34], etc.) with micro- and macrovascular complications in T2DM. In general, studies yielded conflicting results; some of these discrepancies could be attributed to different study populations, races, small sample sizes, study types (i.e. retrospective) and design. It should be noted that many association studies were conducted on one single common polymorphism and hence have not scanned for the gene–gene or gene-environment influences on the risk for MI.
Oxidative stress occurs when ROS production exceeds the elimination capacity of the antioxidant system. Most ROS are generated in the mitochondrial respiratory chain [35] and although by-products, they are vital for normal processes, such as the maintenance of the vascular tone, cell adhesion, immune responses and cellular growth [36]. Increased expression of ROMO1, firstly identified in tumour cells, increases ROS production [35], leading to oxidative stress and cell death [11]. The product encoded by ROMO1 is a small transmembrane protein located in the inner mitochondrial membrane that has been recently found to be a unique nonselective cation channel. Its function is suggested to be regulated in response to fluctuation of free iron concentration and redox state of iron [9]. It is proposed that ROMO1 activation causes the recruitment of B-cell lymphoma-extra-large (Bcl-xL) protein to the outer mitochondrial membrane that in turn reduces its membrane potential, resulting in ROS production [13].
ROMO1 is an essential protein involved in several cell functions. It is vital for maintaining mitochondrial cristae shape [10, 37] and its loss causes mitochondrial cytochrome c leakage, which is one of the key molecules involved in the intrinsic apoptotic pathway [37]. Its role in tumour necrosis factor (TNF)-alpha-induced apoptosis was furthermore confirmed by Kim et al. [13].
Hwang et al. [11] showed that enforced ROMO1 expression leads to massive cell death (necrosis) by excessive ROS production. It was shown that in physiological states ROMO1-derived ROS were indispensable for the proliferation of both normal and cancer cells, respectively [12]. Moreover, Chung el al [37] showed that ROMO1 might be a principal factor in the deregulation of nuclear factor-κB and related pathways that contribute to tumour cell proliferation and invasion. It is also thought to have a role in replicative senescence [14]. Lung, colorectal cancer and gliomas [38] have been linked to ROMO1. In non-small cell lung cancer ROMO1 can serve as disease biomarker and is a predictor of poor survival and malignant effusions in these patients [39, 40]. In colorectal cancer, ROMO1 expression predicts poor survival and higher invasiveness [15]. Its role is also being investigated concerning pulmonary and renal fibrosis [41], obstructive sleep apnoea syndrome [42] and Fanconi anaemia [43].
Furthermore, to our knowledge, this is the first study investigating the expression of the ROMO1 in coronary endarterectomy samples. The C allele carriers showed statistically higher number of cells positive for ROMO1 compared with T allele carriers. This result corroborates the findings by Petrovič et al. [16], in which greater ROMO1 expression was found in fibrovascular membranes of subjects with microvascular complication of T2DM, namely proliferative diabetic retinopathy. ROMO1 rs6060566 polymorphism is located in an intron region. Therefore, the exact mechanism on how rs6060566 polymorphism enhances the expression of this gene is not known. Several possible processes can be affected: transcription rate, nuclear export, transcript stability or, moreover, introns can also increase the efficiency of mRNA translation [44].
To continue, we assumed that ROMO1 rs6060566 polymorphism might be associated with MI. However, we failed to show the presumable association in Slovenian subjects with T2DM. One possible explanation for our results might be that some of the controls had clinically silent CAD that we did not detect with our inclusion criteria, or had other macro- or microvascular complications that could also be induced by oxidative stress. Not detecting clinically silent CAD is therefore a major limitation of our study. Otherwise, subjects with MI had a longer duration of DM and higher levels of HbA1c. It is generally believed that the relative risk for MI increases with any increase in glycaemia above the normal range [45]. On the other hand, blood pressure in cases was better managed, which is probably a consequence of a recent MI, thus recently optimized medical therapy and presumed better compliance.
Conclusions
In conclusion, in this study we did not observe any association between the rs6060566 polymorphism of the ROMO1 gene and the risk of MI in Caucasians with T2DM. However, we found that subjects carrying the C allele were at a 3.27-fold increased risk of developing severe CAD compared with those who had non-obstructive CAD. Moreover, C allele carriers showed a statistically higher number of cells positive for ROMO1 compared with T allele carriers in coronary endarterectomy samples. Furthermore, it seems likely that the extent of CAD was a risk factor for MI in a subgroup of subjects in whom 2 VD was diagnosed with coronary CTA.
In summary, our findings signal that 8-OHdG, a well-known oxidative stress marker, does not have the ability to discriminate between subjects with and without CAD. Association analyses in different ethnic populations are needed to confirm and validate our preliminary findings.
New opportunities for research activity are needed to explore the contribution of oxidative stress to the perpetuation of the atherosclerotic process in the coronary artery system in subjects with T2DM.
Availability of data and materials
The demographic, clinical, and genetic data that support the findings of this study are available under Additional file 2. The SNP data is available in European Variation Archive on https://www.ebi.ac.uk/eva/?eva-study=PRJEB41691.
Abbreviations
- ACS:
-
Acute coronary syndrome
- OR:
-
Odds ratio
- AUC:
-
Area-under-curve
- Bcl-xL:
-
B-cell lymphoma-extra-large
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass grafting surgery
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- CTA:
-
Computed tomography angiography
- CVI:
-
Cerebrovascular insult
- DAB:
-
Diamonobenzidine
- DM:
-
Diabetes mellitus
- 8-OHdG:
-
8-Hydroxy-2′-deoxygunosine
- ELISA:
-
Enzyme-linked immunosorbent assay
- ESC:
-
European society of cardiology
- HbA1c:
-
Glycated haemoglobin
- HDL:
-
High density lipoprotein
- hsCRP:
-
High sensitivity C-reactive protein
- HWE:
-
Hardy–Weinberg equilibrium
- KASP:
-
Competitive allele‐specific PCR
- LAD:
-
Left anterior descending
- LCx:
-
Left circumflex
- LMCA:
-
Left main coronary artery
- LDL:
-
Low density lipoprotein
- MAF:
-
Minor allele frequency
- MI:
-
Myocardial infarction
- NADP:
-
Nicotinamide adenine dinucleotide phosphate
- OR:
-
Odds ratio
- PCI:
-
Percutaneous coronary intervention
- RCA:
-
Right coronary artery
- ROC:
-
Receiver operating characteristic
- ROMO1:
-
Reactive oxygen species modulator 1
- ROS:
-
Reactive oxygen species
- TIA:
-
Transitory ischemic attack
- T2DM:
-
Type 2 diabetes mellitus
- TNF:
-
Tumour necrosis factor
- VD:
-
Vessel disease
References
Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98.
Tillin T, Hughes AD, Mayet J, Whincup P, Sattar N, Forouhi NG, et al. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians, and African Caribbeans: SABRE (Southall and Brent Revisited)—a prospective population-based study. J Am Coll Cardiol. 2013;61(17):1777–86.
Lippi G, Sanchis-Gomar F, Cervellin G. Chest pain, dyspnea and other symptoms in patients with type 1 and 2 myocardial infarction. A literature review. Int J Cardiol. 2016;215:20–2.
Keller PF, Carballo D, Roffi M. Diabetes and acute coronary syndrome. Minerva Med. 2010;101(2):81–104.
Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339(4):229–34.
Heitzer T, Schlinzig T, Krohn K, Meinertz T, Münzel T. Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease [published correction appears in Circulation. 2003 Jul 29;108(4):500]. Circulation. 2001;104(22):2673–8.
Tibaut M, Petrovič D. Oxidative stress genes, antioxidants and coronary artery disease in type 2 diabetes mellitus. Cardiovasc Hematol Agents Med Chem. 2016;14(1):23–38.
Deloukas P, Matthews LH, Ashurst J, Burton J, Gilbert JG, Jones M, et al. The DNA sequence and comparative analysis of human chromosome 20. Nature. 2001;414(6866):865–71.
Lee GY, You D, Lee H-R, Hwang SW, Lee CJ, Yoo YD. Romo1 is a mitochondrial nonselective cation channel with viroporin-like characteristics. J Cell Biol. 2018;217(6):2059–71.
Norton M, Ng AC-H, Baird S, Dumoulin A, Shutt T, Mah N, et al. ROMO1 is an essential redox-dependent regulator of mitochondrial dynamics. Sci Signal. 2014;7(310):ra10.
Hwang IT, Chung YM, Kim JJ, Chung JS, Kim BS, Kim HJ, et al. Drug resistance to 5-FU linked to reactive oxygen species modulator 1. Biochem Biophys Res Commun. 2007;359(2):304–10.
Na AR, Chung YM, Lee SB, Park SH, Lee M-S, Yoo YD. A critical role for Romo1-derived ROS in cell proliferation. Biochem Biophys Res Commun. 2008;369(2):672–8.
Kim JJ, Lee SB, Park JK, Yoo YD. TNF-alpha-induced ROS production triggering apoptosis is directly linked to Romo1 and Bcl-X(L). Cell Death Differ. 2010;17(9):1420–34.
Chung YM, Lee SB, Kim HJ, Park SH, Kim JJ, Chung JS, et al. Replicative senescence induced by Romo1-derived reactive oxygen species. J Biol Chem. 2008;283(48):33763–71.
Kim HJ, Jo MJ, Kim BR, Kim JL, Jeong YA, Na YJ, et al. Reactive oxygen species modulator-1 (Romo1) predicts unfavorable prognosis in colorectal cancer patients. PLoS ONE. 2017;12(5):e0176834.
Petrovič MG, Kruzliak P, Petrovic D. The rs6060566 of the reactive oxygen species modulator 1 (Romo-1) gene affects Romo-1 expression and the development of diabetic retinopathy in Caucasians with type 2 diabetes. Acta Ophthalmol. 2015;93(8):e654-657.
Association AD. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Supplement 1):S13-27.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237–69.
Weibel ER. Stereological methods, vol. 1: practical methods for biological morphometry. Z Allg Mikrobiol. 1981;21(8):630–630.
Tibaut M, Petrovič D, Mekiš D. Pathophysiology of myocardial infarction and acute management strategies. Cardiovasc Hematol Agents Med Chem. 2016;14(3):150–9.
Gyldenkerne C, Olesen K, Madsen M, Thim T, Jensen LO, Raungaard B, et al. Extent of coronary artery disease is associated with myocardial infarction and mortality in patients with diabetes mellitus. Clin Epidemiol. 2019;11:419–28.
Waller BF, Palumbo PJ, Lie JT, Roberts WC. Status of the coronary arteries at necropsy in diabetes mellitus with onset after age 30 years. Analysis of 229 diabetic patients with and without clinical evidence of coronary heart disease and comparison to 183 control subjects. Am J Med. 1980;69(4):498–506.
Zhai C, Cong H, Hou K, Hu Y, Zhang J, Zhang Y. Clinical outcome comparison of percutaneous coronary intervention and bypass surgery in diabetic patients with coronary artery disease: a meta-analysis of randomized controlled trials and observational studies. Diabetol Metab Syndr. 2019;11:110.
Jensen LO, Thayssen P, Junker A, Maeng M, Tilsted HH, Kaltoft A, et al. Comparison of outcomes in patients with versus without diabetes mellitus after revascularization with everolimus- and sirolimus-eluting stents (from the SORT OUT IV trial). Am J Cardiol. 2012;110:1585–91.
Olesen KK, Tilsted HH, Jensen LO, Kaltoft A, Krusell LR, Ravkilde J, et al. Long-term outcome of sirolimus-eluting and zotarolimus-eluting coronary stent implantation in patients with and without diabetes mellitus (a Danish organization for randomized trials on clinical outcome III substudy). Am J Cardiol. 2015;115(3):298–302.
Olesen K, Madsen M, Egholm G, Thim T, Jensen LO, Raungaard B, et al. Patients with diabetes without significant angiographic coronary artery disease have the same risk of myocardial infarction as patients without diabetes in a real-world population receiving appropriate prophylactic treatment. Diabetes Care. 2017;40(8):1103–10.
Aronson D, Edelman ER. Coronary artery disease and diabetes mellitus. Cardiol Clin. 2014;32(3):439–55.
Tibaut M, Caprnda M, Kubatka P, Sinkovič A, Valentova V, Filipova S, et al. Markers of atherosclerosis: part 2—genetic and imaging markers. Heart Lung Circ. 2019;28(5):678–89.
Nikpay M, Goel A, Won H-H, Hall LM, Willenborg C, Kanoni S, et al. A comprehensive 1000 genomes–based genome-wide association meta-analysis of coronary artery disease. Nat Genet. 2015;47(10):1121–30.
Abraham G, Havulinna AS, Bhalala OG, Byars SG, de Livera AM, Yetukuri L, et al. Genomic prediction of coronary heart disease. Eur Heart J. 2016. https://doi.org/10.1101/041483.
Cilenšek I, Mankoč S, Petrovič MG, Petrovič D. GSTT1 null genotype is a risk factor for diabetic retinopathy in Caucasians with type 2 diabetes, whereas GSTM1 null genotype might confer protection against retinopathy. Dis Markers. 2012;32(2):93–9.
Kariž S, Nikolajević Starčević J, Petrovič D. Association of manganese superoxide dismutase and glutathione S-transferases genotypes with myocardial infarction in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2012;98(1):144–50.
Kariž S, Mankoč S, Petrovič D. Association of thioredoxin reductase 2 (TXNRD2) gene polymorphisms with myocardial infarction in Slovene patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2015;108(2):323–8.
Cheurfa N, Dubois-Laforgue D, Ferrarezi DAF, Reis AF, Brenner GM, Bouche C, et al. The common -866G>a variant in the promoter of UCP2 is associated with decreased risk of coronary artery disease in type 2 diabetic men. Diabetes. 2008;57(4):1063–8.
Chung YM, Kim JS, Yoo YD. A novel protein, Romo1, induces ROS production in the mitochondria. Biochem Biophys Res Commun. 2006;347(3):649–55.
D’Autréaux B, Toledano MB. ROS as signalling molecules: mechanisms that generate specificity in ROS homeostasis. Nat Rev Mol Cell Biol. 2007;8(10):813–24.
Semenzato M, Scorrano L. O ROM(e)O1, ROM(e)O1, wherefore art thou ROM(e)O1? Sci Signal. 2014;7(310):pe2.
Yu MO, Song N-H, Park K-J, Park D-H, Kim S-H, Chae Y-S, et al. Romo1 is associated with ROS production and cellular growth in human gliomas. J Neurooncol. 2015;121(1):73–81.
Lee SH, Lee JS, Lee EJ, Min KH, Hur GY, Lee SH, et al. Serum reactive oxygen species modulator 1 (Romo1) as a potential diagnostic biomarker for non-small cell lung cancer. Lung Cancer. 2014;85(2):175–81.
Lee SH, Park MJ, Choi SI, Lee EJ, Lee SY, In KH. Reactive oxygen species modulator 1 (Romo1) as a novel diagnostic marker for lung cancer-related malignant effusion. Medicine (Baltimore). 2017;96(4):e5975.
Liu D, Liu Y, Xia Z, Dong H, Yi Z. Reactive oxygen species modulator 1 regulates oxidative stress and induces renal and pulmonary fibrosis in a unilateral ureteral obstruction rat model and in HK-2 cells. Mol Med Rep. 2017;16(4):4855–62.
Ye L, Qian Y, Li Q, Fang S, Yang Z, Tan Y, et al. Serum Romo1 is significantly associated with disease severity in patients with obstructive sleep apnea syndrome. Sleep Breath. 2018;22(3):743–8.
Shyamsunder P, Verma RS, Lyakhovich A. ROMO1 regulates RedOx states and serves as an inducer of NF-κB-driven EMT factors in Fanconi anemia. Cancer Lett. 2015;361(1):33–8.
Shaul O. How introns enhance gene expression. Int J Biochem Cell Biol. 2017;91:145–55.
Balkau B, Shipley M, Jarrett RJ, Pyorala K, Pyorala M, et al. High blood glucose concentration is a risk factor for mortality in middle-aged nondiabetic men. Diabetes Care. 1998;21:360–7.
Acknowledgements
We thank Mrs. Petra Nussdorfer for her excellent technical assistance and expertise in immunohistochemistry of endarterectomised coronary artery tissue samples. We also thank Mrs. Visam Bajt for revising the English, and Mr. Miha Krkovič for his assistance in statistics.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
MT was a major contributor in writing the manuscript. SMR and DP concieved and designed the study. DP rceruited the participants. SMR analysed and interpreted the demographic, clinical and genetic data regarding CAD and 8-OHdG serum level. DP performed the histological examination of coronary endarterectomy tissue samples. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the National Medical Ethics Committee, Ministry of Health, Republic of Slovenia (“Komisija za medicinsko etiko”) (Number 0120-372/2017) and was performed in compliance with the Helsinki Declaration. Written informed consent was obtained from all participants before the start of the study. The aforementioned committee granted the permission to access the clinical and personal research subject’s data.
Consent for publication
Not applicable.
Competing interests
The authors affirm that they have no conflict of interest related to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The questionnaire, cardiovascular risk assessment Table S1 and information on other comorbidities Table S2.
Additional file 2.
Demographic, clinical and genetic data of Slovenian subjects with T2DM.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tibaut, M., Mankoč Ramuš, S. & Petrovič, D. The C allele of the reactive oxygen species modulator 1 (ROMO1) polymorphism rs6060566 is a biomarker predicting coronary artery stenosis in Slovenian subjects with type 2 diabetes mellitus. BMC Med Genomics 13, 184 (2020). https://doi.org/10.1186/s12920-020-00845-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-020-00845-3