Abstract
Background
Sclerosing encapsulating peritonitis (SEP) is a rare clinical syndrome characterised by fibrosis and thickening of the peritoneum with massive adhesions of the abdominal organs. In humans, abdominal tumours, such as pancreatic adenocarcinoma, can be underlying diseases of SEP. This report describes a case of SEP in a dog with pancreatic ductal adenocarcinoma.
Case presentation
An 11-year-old male neutered French Bulldog presented with chronic vomiting. Ultrasonography revealed a mass in the centre of the abdomen. A small amount of ascites, interpreted as modified transudate, was present in the abdominal cavity. Computed tomography (CT) revealed peritoneal effusion with a thickened peritonium. Laparoscopy revealed a large nodular lesion occupying the central portion of the abdomen, continuous with the falciform ligament. Histological examination of the biopsy specimens of the mass, abdominal wall, and gastric peritoneum revealed marked fibroplasia with mild lymphoplasmacytic infiltrates. Based on these results, a tentative diagnosis of early stage sclerosing encapsulating peritonitis (SEP) was made. Prednisolone and tamoxifen were administered with the expectation of ameliorating SEP, however, the dog died 61 days post diagnosis. At autopsy, the intestinal loop and mesentery were encased in the fibrous membrane, which is a typical finding in SEP. Histopathology and immunohistochemistry of the samples obtained at autopsy supported the diagnosis of pancreatic ductal adenocarcinoma with peritoneal dissemination and distant metastasis with desmoplasia. The unexpectedly hardened skin, where previously laparoscopic ports were inserted, histologically contained the same carcinoma cells with desmoplasia.
Conclusions
To the best of our knowledge, this is the first report of canine SEP with pancreatic ductal adenocarcinoma that also caused metastasis to port insertion sites as well as distant organs.
Similar content being viewed by others
Background
Sclerosing encapsulating peritonitis (SEP) is a chronic form of peritonitis characterised by fibrosis and thickening of the visceral and parietal peritoneum with massive adhesions of the abdominal organs [1]. Peritoneal inflammation and intestinal adhesion cause clinical symptoms, such as abdominal pain, anorexia, and vomiting. In humans, the clinical features of SEP are well described, and the major underlying causes are peritoneal dialysis, abdominal surgery, drug administration, and abdominal tumours [2]. In contrast, it is an extremely rare condition in dogs, and the aetiology of SEP is not fully understood, but is thought to be multifactorial [3]. Most cases of canine SEP are diagnosed at the time of exploratory laparotomy or autopsy [1, 3,4,5]. Treatment protocols for SEP in dogs have not yet been established; therefore, SEP has a poor prognosis in most cases.
Pancreatic carcinoma arising from exocrine acinar cells or duct epithelial cells is rare in veterinary medicine [6]. Early diagnosis of this tumour in dogs is difficult, and a previous study reported that metastasis was observed in 78% of cases at the time of diagnosis [7]. Although pancreatic ductal carcinomas are a minority among canine pancreatic carcinomas, this type of carcinoma is consistently associated with abdominal or distant metastasis [6]. In humans, pancreatic ductal carcinomas cause prominent fibrosis of the pancreas, which may lead to SEP [8, 9]. This report describes a case of SEP associated with pancreatic ductal adenocarcinoma in a dog.
Case presentation
An 11-year-old male neutered French Bulldog with a history of chronic vomiting was referred to our hospital. A physical examination revealed abdominal pain and swelling. Blood analysis showed mild elevation of creatinine kinase (229 U/L; range 10–200 U/L). Abdominal radiography revealed a caudal displacement of the gastrointestinal tract by mixed fat and soft tissue opacity in the cranial to mid abdomen. No radiographic evidence of intestinal obstruction was noted. Ultrasonography revealed a mass with a mixed-echo pattern between the stomach and the intestinal tract, with a small amount of ascites (Fig. 1). Corrugation of the jejunum and ileum was observed. Cytological examination of the ascites revealed a modified transudate, mainly composed of neutrophils and macrophages (specific gravity, 1.020; total protein: 2.2 mg/dL). The bacterial culture of ascites was negative. Following these tests, CT and laparoscopy were performed under general anaesthesia.
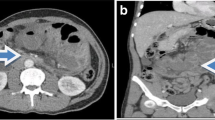
Pre- and post-intravenous contrast CT were reviewed by a ACVR board-certified radiologist (M.M.) which revealed a moderate amount of non-enhancing fluid attenuation in the peritoneal cavity surrounding and displacing the mesentery and omental fat from the abdominal wall (Fig. 2). In addition, there was mild thickening of the soft tissue attenuating and mildly contrast-enhancing rims of the mesentery, omental fat, and fat along the linea alba adjacent to the peritoneal effusion. The left limb of the pancreas was enlarged with an irregularly rounded margination and homogeneous parenchyma, which iso-attenuated to the rest of the pancreas.
Laparoscopy revealed a large nodular lesion occupying the central portion of the abdomen, with sanguineous abdominal fluid. The nodular lesion was continuous with the falciform ligament. The parietal peritoneal surface was diffusely white and rough (Fig. 3). Under laparoscopy, biopsies were obtained from the surface of the tumour, the abdominal wall around the tumour, and the serous membrane of the stomach. Histological examination of all samples showed proliferation of fibroconnective tissue with a chronic inflammatory reaction (Fig. 4). The fibroblasts in these tissues showed no atypia. Based on these findings, the dog was presumptively diagnosed with early phase SEP.
Laparoscopic views of the abdomen. Haemorrhagic ascites was observed in the caudal side of the spleen (A). Mass lesion was presented in the centre of the abdomen continuous to the hepatic falciform ligament (B, C). After excising the surface of the mass lesion, fatty or fat-like tissue emerged from the inside (D). The parietal peritoneal surface was diffusely white and rough (E). Samples were taken from parietal peritoneal surface (F). *indicates the mass lesion. †indicates the hepatic falciform ligament
Histopathological findings of biopsy specimen. Samples were taken from the surface of the mass lesion through laparoscopy and stained with haematoxylin-eosin (HE). Photomicrograph shows a thick layer of fibrous connective tissue covering mature adipose tissue. The mesothelial lining is lacking. A: low power field; B: high power field
Oral prednisolone (1 mg/kg, q24 h) was initiated to reduce fibroplasia and inflammation. Tramadol (5 mg/kg, iv, q12h) was used for pain management. Ascites was drained once per week (1000–1500 mL at each occasion). Two weeks after the initiation of these treatments, the dog exhibited decreased activity, anorexia, and weight loss. Physical examination revealed a marked swelling at the previous laparoscopic port insertion sites. The prednisolone dose was increased to 1.5 mg/kg q24 h. A week later, the dog showed a slight improvement in activity and appetite. Tamoxifen (1 mg/kg, PO, SID) was added to ameliorate peritoneal fibrosis in accordance with a previous report on canine SEP [4]. Despite these treatments, the dog’s condition progressively deteriorated, and the dog died 61 days post-diagnosis.
A full autopsy of the refrigerated carcass was performed 52 h post-mortem by an ACVP/JCVP board-certified anatomic pathologist (I.M.) with the consent of the owner of the dog. Turbid, 800 ml, dark brown ascites was present. Mildly turbid, orange thoracic fluid (180 mL) was observed. The parietal and visceral peritoneum was diffusely white to pale tan and severely thickened by up to 2 mm. This markedly thickened peritoneum encased the liver and small intestinal loop, resulting in immobilisation of these organs (Fig. 5). During autopsy, close evaluation of the pancreas was restricted by peritoneal fibrosis. The subcutaneous tissue at three previous laparoscopic ports insertion sites (right and left flank and left to the prepuce) was replaced with solid white tissue (Fig. 6A, B). The noncollapsing lung lobes were mottled orange, dark red, and rubbery on palpation. There was a cloudy red serous fluid discharge from the cut surfaces of the lung lobes. A small amount of similar fluid was present in the trachea.
Gross findings of abdominal organs at autopsy. The visceral peritoneum is diffusely thickened by fibrosis. Abdominal organs adhere to each other. Neoplastic nodule/mass is not grossly evident. D: diaphragm; F: fatty appendage of the falciform ligament. G: gallbladder; L: liver; Si: small intestine; Sp: spleen; St: stomach
Histopathologically, the intestinal loop was diffusely covered by up to 2-mm-thick dense fibrous connective tissue (desmoplasia), with scattered neoplastic foci (Fig. 7A-C). The neoplasm was characterised by haphazardly arranged ducts and tubules of atypical cuboidal to columnar epithelial cells, with secretion of periodic acid-Schiff (PAS)-positive mucus (Fig. 7D). Mitosis was 1 × 2.37 mm2 (10 HPFs). Similar neoplastic epithelial cells proliferated around the pancreatic ducts, with desmoplasia. Greater atypia and pleomorphism of the tumour cells were observed among neoplastic cells in the metastatic lesions, such as the lung, right periadrenal tissue, and subcutis of the previous laparoscopy ports insertion sites, than in the pancreatic and peritoneal regions (Fig. 7E). Tumour-associated desmoplasia was a consistent feature of this dog’s neoplasm. No inflammatory infiltrates were observed within or around the neoplasms. The differential diagnosis of this dog’s neoplasm included pancreatic ductal adenocarcinoma, pancreatic acinar cell carcinoma, pancreatic neuroendocrine tumour, and malignant mesothelioma. Advanced characterisation of the tumour cells was performed by a panel of immunohistochemistry (IHC) tests. Information on antibodies and immunohistochemistry results are summarised in Tables 1 and 2, respectively. Briefly, the tumour cells within the pancreas and peritoneum were reactive to CK, while they did not show reactivity to vimentin, CEA, WT1, CGA, or amylase (Table 2 and Fig. 7F-K). Based on these results, the dog was diagnosed with SEP secondary to pancreatic ductal adenocarcinoma. Septicaemia and pulmonary oedema were suspected to be the cause of death, possibly due to bacterial translocation through the small intestinal mucosa, for which peristalsis had most likely been hampered by SEP.
Histopathological and immunohistochemical findings of pancreatic ductal adenocarcinoma of a dog. A: Tumour cells proliferate around the pancreatic duct (asterisk). HE stain. (Bar = 400 μm). B: A magnified view of the rectangle in Fig. 6A. Tall columnar neoplastic epithelial cells proliferate forming irregular-shape ducts (HE stain; bar = 40 μm). C: Desmoplastic fibroplasia around tumour cells in the subserosa of the small intestine (Masson Trichrome stain; Bar = 200 μm). D: Mucus secreted by tumour cells is periodic acid-Schiff (PAS) reactive (PAS stain; Bar = 40 μm). E: Tumour cells in the laparoscopy port resemble those in other sites (HE stain; bar = 40 μm). F: Tumour cells in the subserosa are reactive to anti-pan-cytokeratin antibody. Immunohistochemistry (IHC; bar = 40 μm). G: Tumour cells in the subserosa are negative to anti-vimentin antibody (IHC; bar = 40 μm). H: Tumour cells in the subserosa are negative to anti-CEA antibody (IHC; bar = 40 μm). I: Tumour cells in the subserosa are negative to anti-amylase antibody (IHC; bar = 40 μm). J: Tumour cells in the subserosa are negative to anti-chromogranin-A antibody (IHC; bar = 40 μm). K. Tumour cells in the subserosa are negative to anti- Wilms tumour 1 (WT1) antibody; (IHC; bar = 40 μm)
Discussion and conclusions
SEP is a rare condition in veterinary medicine that manifests as severe peritonitis with encapsulation of abdominal organs by thick collagenous connective tissue. Thirteen cases of SEP have been reported in dogs [1, 3,4,5, 10,11,12,13,14,15]. Common clinical symptoms of SEP in dogs include vomiting, anorexia, abdominal pain, and weight loss. In human cases of SEP, gastrointestinal obstruction is a common complication and thought to be a major cause of gastrointestinal clinical signs and abdominal pain [2]. The incidence of gastrointestinal obstruction in canine SEP is lower than that in humans, and only one case of pyloric obstruction secondary to SEP has been reported [13]. In the present case, no gastrointestinal obstruction was observed during the first visit. The initial clinical symptoms observed in the dog may have been associated with peritonitis.
Canine SEP is commonly diagnosed during exploratory laparotomy [1, 3,4,5]. Image analysis is useful as an adjunct for the diagnosis of SEP. Peritoneal effusion, thickened peritoneal line, and intestinal encapsulation are common CT findings in canine SEP [4, 11, 12]. In our case, peritoneal effusion with a thickened peritoneal line was found on CT at the first visit. Although encapsulation of the abdominal organs was not detected by either CT or laparoscopy at this time, the histopathological findings of the gastric serosal biopsy were consistent with those of SEP. Based on the imaging analysis, we speculated that the abdominal mass was the omentum covered by fibrous connective tissue. By the time of death of the dog, however, peritoneal sclerosis had advanced to cover the entire abdominal organs. Although the final diagnosis of SEP was made at the time of autopsy, the initial SEP lesion was successfully detected using CT, laparoscopy, and peritoneal biopsy.
Canine pancreatic exocrine tumours, which commonly originate from the acinar and rarely from duct epithelial cells, show aggressive behaviour with frequent metastasis [7]. Common clinical signs of pancreatic exocrine tumours include lethargy, anorexia, vomiting, and abdominal pain. In humans, contrary to canine epidemiology, ductal carcinoma is far more common than its exocrine counterparts in pancreatic cancers [16]. This tumour carries poor prognosis (5-year survival rate is approximately 5%) because of the absence of effective methods for early diagnosis and the aggressive nature of this tumour in humans [16]. According to the literature, the key pathologic features of well and moderately differentiated pancreatic ductal adenocarcinomas are as follows:1) glandular and ductal structures with a haphazard proliferating pattern, 2) marked desmoplasia, and 3) production of sialo-type and sulphated acid mucins [16]. The histopathological features of neoplastic epithelial cells in the present report are consistent with the characteristics of human pancreatic ductal adenocarcinoma. There is no IHC panel to establish a diagnosis of pancreatic ductal adenocarcinoma in human medicine. We understood this restriction and applied IHC to our case to rule out a differential diagnosis. The possibility of pancreatic acinar cell carcinoma was eliminated based on a negative reaction to anti-amylase antibody, as well as the absence of zymogen-like granules in the cytoplasm of the neoplastic cells [17]. Pancreatic neuroendocrine tumours were ruled out due to a negative reaction to chromogranin A and the lack of a typical proliferating pattern of neuroendocrine tumours [18]. Another important differential diagnosis in the present case was sclerosing peritoneal mesothelioma (SPM). Mesothelioma generally originates from the mesothelial lining of the thoracic, abdominal, and pericardial cavities and vaginal tunics of the scrotum and typically proliferates in epithelioid, sarcomatoid, or biphasic patterns [19]. SPM is a very rare variant of mesothelioma, characterised by abundant background fibrous tissue, despite few neoplastic mesothelial cells [19]. According to previous reports, canine SPM never proliferated in a tubular pattern, unlike in our case, but proliferated in nests, clusters, or individualised patterns [20, 21]. IHC results, especially the lack of vimentin or WT1 immunophenotype, also precluded the diagnosis of SPM in our case, although the antibody to WT1 was not reactive to canine tissues in our experimental setting. However, it has been demonstrated that the antibody to WT1 can be a marker of canine mesotheliomas; therefore, our IHC results would be regarded as legitimate [22].
In the present case, all three previous laparoscopic skin ports insertion sites showed abnormal postsurgical swelling, which was histologically demonstrated to be metastasis of pancreatic ductal adenocarcinoma (Figs. 6, 7). In humans, postsurgical port-site metastasis of malignant tumours has been reported to occur in 1 to 2% of patients [23], especially in the field of urology [24]. To the best of our knowledge, there are no such reports in the veterinary literature. Malignant tumours such as pancreatic ductal adenocarcinoma may be a potential cause of laparoscopic port-site metastasis. There is a need to carefully prevent this type of dissemination or metastasis of malignant tumours by regular and careful employment of laparoscopic specimen retrieval bags and/or by adequate procedures to protect the surface of laparoscopic ports when dealing with cases of potential malignant neoplasms. In this case, no abnormalities were found in the pancreas on the CT scan. However, since histologic changes suggestive of SEP were detected in the biopsy specimen taken at the first visit, it is likely that the pancreatic lesion was subtle enough to escape CT scrutinisation. Metastasis of tumour cells in the laparoscopic skin ports suggests the onset of pancreatic ductal adenocarcinoma at the time of laparoscopy and CT.
In this case, pancreatic ductal adenocarcinoma was observed concurrently with SEP. The previously reported underlying causes of SEP in dogs include foreign body ingestion (e.g. fibreglass and stick), steatitis, leishmaniasis, abnormal liver development, and neoplasia [1, 3,4,5, 10,11,12,13,14,15]. Only one case of hepatocellular carcinoma has been reported as a tumour-related SEP in dogs [11]. In humans, abdominal tumours such as pancreatic adenocarcinoma, midgut neuroendocrine tumours, and gastric carcinoma have been reported as underlying diseases of SEP [8, 9, 25, 26]. In human pancreatic tumours, rupture of the pancreatic ductal tissue causes leakage of pancreatic enzymes, leading to peritoneal inflammation with a desmoplastic stromal reaction [9]. In particular, human pancreatic adenocarcinoma of ductal origin causes prominent fibrosis in the pancreas, which is associated with the prognosis of this tumour [27]. In this case, marked desmoplasia was observed with extensive peritoneal dissemination of tumour cells, which is consistent with the above-mentioned features of human pancreatic ductal adenocarcinoma. We believe that this is the first case of canine SEP with pancreatic ductal adenocarcinoma to the best of our knowledge.
The prognosis of SEP in dogs depends on the underlying disease but is generally considered to be poor. Previous reports have shown that 93% of SEP cases die within 13 months [1, 3,4,5, 10,11,12,13,14,15]. To date, treatment of SEP in dogs has not been established. Only one report has demonstrated successful treatment of SEP in a dog with traumatic abdominal penetration injury using methylprednisolone and tamoxifen [4]. Tamoxifen has a supportive effect on metalloproteinase synthesis, promotes mesothelial healing, and assists in preventing the formation of new fibrous adhesions in the visceral peritoneum [28]. In this case, no response was observed to prednisolone and tamoxifen treatment, and the patient died 61 days after the first visit. The poor prognosis in this case was most likely associated with the concurrent pancreatic ductal adenocarcinoma. In a retrospective study of 23 dogs with pancreatic exocrine tumours, the median survival time was 1 d. In this report, a large number of dogs were euthanised immediately after diagnosis because distant metastases were observed at the time of diagnosis [7]. Another retrospective study of dogs reported that all cases of pancreatic tumours of canine ductal origin had metastasis in abdominal organs such as the liver, spleen, and intestine, and were euthanised at the time of diagnosis [6].
This report describes a case of SEP with pancreatic ductal adenocarcinoma in a dog. The dog had a poor prognosis, and a definitive diagnosis was confirmed by autopsy. As both SEP and pancreatic ductal tumours are extremely rare in dogs, further studies are warranted to clarify the clinicopathological features of both diseases.
Availability of data and materials
All data generated during this study are included in this article.
Abbreviations
- SEP:
-
Sclerosing encapsulating peritonitis
- CT:
-
Computed tomography
- PAS:
-
Periodic acid-Schiff
- IHC:
-
Immunohistochemistry
- CK:
-
Cytokeratin
- CEA:
-
Carcinoembryonic Antigen
- CGA:
-
Chromogranin A
- SPM:
-
Sclerosing peritoneal mesothelioma
- WT1:
-
Wilms tumour 1
References
Hardie EM, Rottman JB, Levy JK. Sclerosing encapsulating peritonitis in four dogs and a cat. Vet Surg. 1994;23:107–14.
Danford CJ, Lin SC, Smith MP, Wolf JL. Encapsulating peritoneal sclerosis. World J Gastroenterol. 2018;24:3101–11.
Izawa T, Murai F, Akiyoshi H, Ohashi F, Yamate J, Kuwamura M. Encapsulating peritoneal sclerosis associated with abnormal liver development in a young dog. J Vet Med Sci. 2011;73:697–700.
Etchepareborde S, Heimann M, Cohen-Solal A, Hamaide A. Use of tamoxifen in a German shepherd dog with sclerosing encapsulating peritonitis. J Small Anim Pract. 2010;51:649–53.
Adamama-Moraitou KK, Prassinos NN, Patsikas MN, Psychas V, Tsioli B, Rallis TS. Sclerosing encapsulating peritonitis in a dog with leishmaniasis. J Small Anim Pract. 2004;45:117–21.
Aupperle-Lellbach H, Torner K, Staudacher M, Muller E, Steiger K, Klopfleisch R. Characterization of 22 canine pancreatic carcinomas and review of literature. J Comp Pathol. 2019;173:71–82.
Pinard CJ, Hocker SE, Weishaar KM. Clinical outcome in 23 dogs with exocrine pancreatic carcinoma. Vet Comp Oncol. 2021;19:109–14.
Tobioka N, Kataoka M, Hashimoto T, Naruse M, Sakakibara K, Kuroda T, et al. Chronic encapsulating fibrous peritonitis induced by carcinoma of the pancreas. Gan No Rinsho. 1983;29:1371–4.
Marusawa H, Katsurada A, Takaya H, Kumegawa Y, Kajimura K, Yamashita Y. A case of encapsulating peritonitis associated with pancreatic ascites induced by carcinoma of the pancreas. Nihon Shokakibyo Gakkai Zasshi. 1996;93:932–6.
Boothe HW, Lay JC, Moreland KJ. Sclerosing encapsulating peritonitis in three dogs. J Am Vet Med Assoc. 1991;198:267–70.
Barnes K. What is your diagnosis? Sclerosing encapsulating peritonitis. J Am Vet Med Assoc. 2015;247:43–5.
Veiga-Parga T, Hecht S, Craig L. Imaging Diagnosis-Sclerosing Encapsulating Peritonitis in a Dog. Vet Radiol Ultrasound. 2015;56:E65–9.
Carroll KA, Wallace ML, Hill TL, Bartges JW, Ruby JL, Mulder AT 2nd, et al. Pyloric outflow obstruction secondary to sclerosing encapsulating peritonitis in a dog. Aust Vet J. 2020;98:11–6.
Bellenger CR. Sclerosing encapsulating peritonitis in a dog. Aust Vet Pract. 1991;128:131–4.
Setoguchi AKT, Nishimura R, Sasaki N. Sclerosing encapsulating peritonitis in one dog and three cats. Jpn J Vet Anesth Surg. 1996;27:79–89.
Luchini C, Capelli P, Scarpa A. Pancreatic ductal adenocarcinoma and its variants. Surg Pathol Clin. 2016;9:547–60.
Hilmy AM, Kandeel KM, Selim NM. Pancreatic amylase as a tumour marker for pancreatic cancer. Arch Geschwulstforsch. 1984;54:475–82.
Marotta V, Zatelli MC, Sciammarella C, Ambrosio MR, Bondanelli M, Colao A, et al. Chromogranin a as circulating marker for diagnosis and management of neuroendocrine neoplasms: more flaws than fame. Endocr Relat Cancer. 2018;25:11–29.
Meuten D. Tumors in Domestic Animals, 5th ed; 2017.
Gumber S, Fowlkes N, Cho DY. Disseminated sclerosing peritoneal mesothelioma in a dog. J Vet Diagn Investig. 2011;23:1046–50.
Schoning P, Layton CE, Fortney WD, Willard LH, Cook JE. Sclerosing peritoneal mesothelioma in a dog evaluated by electron microscopy and immunoperoxidase techniques. J Vet Diagn Investig. 1992;4:217–20.
Milne EM, Piviani M, Hodgkiss-Geere HM, Piccinelli C, Cheeseman M, Cazzini P, et al. Comparison of effusion cell block and biopsy immunohistochemistry in mesothelial hyperplasia, mesothelioma, and carcinoma in dogs. Vet Clin Pathol. 2021;50:555–67.
Gamal EM, Szabo G, Nagy P, Brath E, Peto K, Olah A, et al. The role of pneumoperitoneum and the "chimney effect" on the development of port site metastasis. A new experimental animal model using Furka's spleen tissue suspension. Magy Seb. 2005;58:89–92.
Castillo OA, Vitagliano G. Port site metastasis and tumor seeding in oncologic laparoscopic urology. Urology. 2008;71:372–8.
Alshomimi S, Hassan A, Faisal Z, Mohammed A, Al Dandan O, Alsaif HS. Sclerosing encapsulating carcinomatous peritonitis: a case report. Saudi J Med Med Sci. 2021;9:63–6.
Wang YZ, King H, Diebold A. Cocoon formation in patients with midgut neuroendocrine tumors: a rare and unrecognized final pathway. Pancreas. 2013;42:944–8.
Korpela T, Ristimaki A, Udd M, Vuorela T, Mustonen H, Haglund C, et al. Pancreatic fibrosis, acinar atrophy and chronic inflammation in surgical specimens associated with survival in patients with resectable pancreatic ductal adenocarcinoma. BMC Cancer. 2022;22:23.
Moustafellos P, Hadjianastassiou V, Roy D, Velzeboer NE, Maniakyn N, Vaidya A, et al. Tamoxifen therapy in encapsulating sclerosing peritonitis in patients after kidney transplantation. Transplant Proc. 2006;38:2913–4.
Acknowledgements
The authors would like to thank Mr. Manabu Suzuki for histological examination of the biopsy specimens.
Funding
No specific funding has been received.
Author information
Authors and Affiliations
Contributions
YT is responsible clinician of this case. YP performed laparoscopy. IM performed autopsy and histopathological diagnosis. MM performed diagnostic imaging. AT drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written consent for publication was obtained from the patient’s owner.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tsukada, Y., Park, Y.T., Mitsui, I. et al. Sclerosing encapsulating peritonitis in a dog with pancreatic ductal adenocarcinoma. BMC Vet Res 18, 383 (2022). https://doi.org/10.1186/s12917-022-03485-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-022-03485-0