Abstract
Background
Mesenchymal stem cells (MSCs) have favorable characteristics that render them a potent therapeutic tool. We tested the characteristics of MSCs after temporal storage in various carrier solutions, such as 0.9% saline (saline), 5% dextrose solution (DS), heparin in saline, and Hartmann’s solution, all of which are approved by the U.S. Food and Drug Administration (FDA). Phosphate-buffered saline, which does not have FDA approval, was also used as a carrier solution. We aimed to examine the effects of these solutions on the viability and characteristics of MSCs to evaluate their suitability and efficacy for the storage of canine adipose-derived MSCs (cADMSCs).
Results
We stored the cADMSCs in the test carrier solutions in a time-dependent manner (1, 6, and 12 h) at 4 °C, and analyzed cell confluency, viability, proliferation, self-renewability, and chondrogenic differentiation. Cell confluency was significantly higher in 5% DS and lower in phosphate-buffered saline at 12 h compared to other solutions. cADMSCs stored in saline for 12 h showed the highest viability rate. However, at 12 h, the proliferation rate of cADMSCs was significantly higher after storage in 5% DS and significantly lower after storage in saline, compared to the other solutions. cADMSCs stored in heparin in saline showed superior chondrogenic capacities at 12 h compared to other carrier solutions. The expression levels of the stemness markers, Nanog and Sox2, as well as those of the MSC surface markers, CD90 and CD105, were also affected over time.
Conclusion
Our results suggest that MSCs should be stored in saline, 5% DS, heparin in saline, or Hartmann’s solution at 4 °C, all of which have FDA approval (preferable storage conditions: less than 6 h and no longer than 12 h), rather than storing them in phosphate-buffered saline to ensure high viability and efficacy.
Similar content being viewed by others
Background
Over the last two decades, stem cell transplantation has gained the attention of researchers due to its functional characteristics and therapeutic potential [1]. Mesenchymal stem cells (MSCs) or mesenchymal progenitor cells are recognized as the most broadly utilized stem cells in tissue engineering and regenerative medicine [2] because of their ability to treat different immune disorders [3] and their eminent multi-lineage differentiation potentiality [4]. They can be isolated from various sources, primarily from the bone marrow (BM), adipose tissue, umbilical cord blood, Wharton’s jelly, etc. [5]. Among these, AT is considered an abundant source of MSCs [6]. Furthermore, adipose-derived MSCs (ADMSCs) have shown therapeutic success in pre-clinical studies in various fields as they are more immune-privileged [7] and significantly more genetically stable for extended culture [7] compared to BM-derived MSCs (BMMSCs) [8]. Various pathologies are similar in canines and humans; canines thus portray an ideal model for replicating human conditions. They can also serve as a replacement for laboratory animals with artificially created diseases [9]. Consequently, canine ADMSCs (cADMSCs) can be considered a potential tool for stem cell-based therapy and as a model for human diseases.
Clinical applications of MSCs are determined by different factors such as the number of cells used [10], cell sources [11], culture conditions [12], cell collection processes [13], transplantation time [14], inter-individual variation [15], implementation methods [16], and cell quality before transplantation. Approval from the U.S. Food and Drug Administration (FDA) can also be a criterion for selecting carrier solutions before clinical therapy. Being fragile and extremely sensitive, MSCs require a strictly maintained environment to retain their quality and prevent deterioration. To minimize the decline in cell quality, it is advisable to transplant MSCs immediately after harvesting. However, time differences, ranging from a few hours to several days, between cell harvesting and transplantation are often unavoidable. Before clinical therapy, MSCs are stored in carrier solutions, followed by direct transplantation into the body. However, it is necessary to investigate the effects of the currently available carrier solutions on MSCs to determine which of these solutions best maintain cell viability and biological functions.
We selected five of the most commonly used carrier solutions in MSCs transplantation for clinical and experimental purposes, namely 0.9% saline (saline) [17], phosphate-buffered solution (PBS) [18], 5% dextrose solution (5% DS) [19], heparin in saline (Hepa-Sal) (1 IU/mL) [20], and Hartmann’s solution (HS) [21].
Saline is useful for maintaining cell viability and high proliferation ability [22], and 5% DS containing dextrose in saline for intravenous administration may contribute to hyperglycemia [23] and has a significantly negative effect on the cell metabolism and viability of MSCs in culture [24]. Hepa-Sal is composed of heparin, commonly used as an anticoagulant for the treatment of embolisms or thromboses [25], and saline. Heparin is also used in cell culture to boost the beneficial effects of extracellular supplements that are used; for instance, heparin does not affect the viability of human ADMSCs (hADMSCs) for at least 24 h [20], and it promotes cell proliferation [26, 27], cell viability [28], and differentiation of MSCs [29, 30]. A recent case of sudden death caused by hepatic embolism after infusion with MSCs attracted global attention to the acute toxicity of MSCs [31]. Li Liao et al. have suggested anticoagulation treatment with heparin for the efficient prevention of MSCs-induced coagulation and the adverse effect of high-dose MSCs infusion [32]. HS is an isotonic solution of several salts that are non-toxic to most cells [33], and it has more clinical benefits compared to those of physiologic saline [34]. Finally, unlike the aforementioned FDA-approved carrier solutions, PBS is applicable in laboratory protocols as additives in cell culture media [35]. Additionally, it is also used as the carrier solution of MSCs before transplantation for clinical or experimental purposes [36]. However, if PBS is used as a carrier, cell washing using FDA-approved solutions should be performed before transplantation.
In this study, we aimed to investigate the currently approved carrier solutions (saline, 5% DS, Hepa-Sal, and HS) as well as PBS in a time-dependent manner to determine the appropriateness and efficacy of these carrier solutions for the storage of ADMSCs at 4 °C.
Results
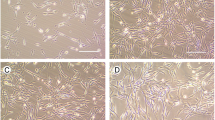
Effects of carrier solutions on cell morphology and proliferation
All the post-storage adherent cells had polymorphic and fibroblast-like morphology. They adhered to the plastic surface and expanded as a monolayer, which is characteristic of stem cells. No apparent morphological changes were observed among cADMSCs stored in the five different carrier solutions (Fig. 1A). cADMSCs significantly showed the highest and lowest confluency upon storage in 5% DS and PBS, respectively, for 12 h (Fig. 1B). cADMSCs stored for 1 h in saline, Hepa-Sal, and HS showed 27.61, 26.62, and 21.49% cell confluency, respectively. Storage in Hepa-Sal for 12 h showed 26.60% confluency, which is higher than that shown after storage in saline and HS for 12 h.
Morphology and confluency of post storage cADMSCs. A After storage in different carrier solutions at 4 °C in a time-dependent manner, cADMSCs at 24 h showed the typical fibroblast-like morphology (Scale bar = 50 μm). Cell confluency of cADMSCs was measured using ImageJ software. B cADMSCs stored in 5% DS showed the highest confluence until 12 h, whereas cells stored in PBS for 1, 6, and 12 h showed the lowest confluence at each time point compared with other solutions. Cells not stored in carrier solutions served as controls. cADMSCs - canine adipose-derived mesenchymal stem cells, Saline - 0.9% saline, PBS - Phosphate-buffered saline, 5% DS - 5% Dextrose solution, Hepa-Sal - Heparin in saline, HS - Hartmann’s solution
pH measurements
We aimed to measure the pH of the carrier solutions, as a pH that is different from the physiological pH can lead to unexpected effects on cell viability. There was an initial increase in the pH of fresh solutions when cADMSCs were stored in them, but this decreased over time. All solutions maintained a pH range of 5.45–7.56 (Table 1), which is acceptable for parenteral transplantation.
Effects of carrier solutions on cell proliferation
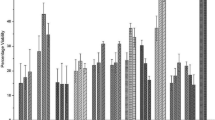
A high proliferation rate is a prerequisite for stem cells used in clinical applications. Cell counting kit-8 (CCK-8) assays showed that cADMSCs stored for 1 and 6 h in the five different carrier solutions showed a slight reduction or increase in proliferation, respectively (Fig. 2A). There was a significant decrease in the cell viability after proliferation at 12 h, with the highest and lowest proliferation observed in 5% DS and saline, respectively.
Post-storage proliferation and viability of cADMSCs. cADMSCs were suspended in different carrier solutions in a time-dependent manner at 4 °C. A Proliferation was determined by the cell counting kit-8 assay. cADMSCs showed no significant decrease in proliferation until 6 h of storage. However, there was significantly higher proliferation at 12 h of storage in 5% DS. B Viability was measured by the MTT assay. The viability of cADMSCs decreased significantly over time. Cells not stored in carrier solutions served as controls. The results are representative of three independent experiments. The bar graph represents the mean ± SD. cADMSCs - canine adipose-derived mesenchymal stem cells, Saline - 0.9% saline, MTT - 3,4,5 – dimethylthiazol-2-yl)-2–5-diphenyltetrazolium bromide, PBS - Phosphate-buffered saline, 5% DS - 5% Dextrose solution, Hepa-Sal - Heparin in saline, HS - Hartmann’s solution, SD - Standard deviation. (*P < 0.05, **P < 0.001, and ***P < 0.0001)
Effects of carrier solutions on the viability of cADMSCs
Generally, detachment of anchorage-dependent cells from the substrate culminates in apoptosis [37]. Although MSCs are known to be less responsive to this type of apoptosis, their viability can be affected when they are detached from a fixed surface in the absence of serum components [38]. Thus, for clinical trials, the effect of carrier solutions on cell viability should be examined. After storage for 1 h, cADMSCs in saline maintained > 86% cell viability, and other carrier solutions maintained approximately 70% cell viability. The viability of cADMSCs was higher in 5% DS and saline at 6 and 12 h, respectively, and decreased significantly in a time-dependent manner in other carrier solutions (Fig. 2B).
Effects of carrier solutions on colony-forming capacity
The colony-forming capacity (CFU) of cADMSCs stored in the different carrier solutions decreased over time. cADMSCs stored in saline and HS formed the highest number of colonies at 6 h (Fig. 3). After 12 h, cADMSCs in saline, 5% DS, and Hepa-Sal formed > 40 colonies, whereas approximately 34–38 colonies were formed in other solutions. There was no significant change in many colonies over time.
Post-storage colony-forming ability of cADMSCs. cADMSCs were suspended in various carrier solutions at 4 °C for different time points and formed colonies in all experimental groups. 1% crystal violet was used for staining and clusters with > 50 cells were considered colonies. Cells not stored in carrier solutions served as controls. The results are representative of three independent experiments. The bar graph represents the mean ± SD. cADMSCs - canine adipose-derived mesenchymal stem cells, Saline - 0.9% saline, PBS - Phosphate-buffered saline, 5% DS - 5% Dextrose solution, Hepa-Sal - Heparin in saline, HS - Hartmann’s solution
Effects of carrier solutions on the expression of stemness and cell surface markers
cADMSCs stored in various carrier solutions at different time points were evaluated for the gene expression, indicating stemness and other stem cell characteristics. The gene expression profiles of the housekeeping gene, Nanog, Sox2, cluster of differentiation (CD) 45, CD90, and CD105 are presented in Fig. 4A. cADMSCs stored in the different carrier solutions did not express the negative surface marker CD45. However, they expressed the positive markers CD90 and CD105, as well as the stemness markers Nanog and Sox2. Their expression was affected over time when stored in different carrier solutions.
Post-storage gene expression of stemness and surface markers of cADMSCs. A Gel results of genes. cADMSCs were suspended in various carrier solutions at 4 °C in a time-dependent manner and analyzed by RT-PCR for the expression of Nanog, Sox2, CD45, CD90, and CD105 followed by agarose gel electrophoresis. GAPDH was used as the housekeeping control gene. cADMSCs in all solutions did not express negative CD45. B, C, D, E Post-storage quantitative analysis of gene expression levels of cADMSCs. cADMSCs were suspended in various carrier solutions at 4 °C in a time-dependent manner. GAPDH was used as the housekeeping control gene. All mRNA data were normalized to the level of GAPDH and relative fold changes in expression level were measured. B The expression level of Nanog was significantly higher in HS at 1 h, which gradually decreased. Saline showed a significantly higher expression of Nanog at 12 h of storage. C A significantly high expression of Sox2 was found in 5% DS at 1 h and 12 h of storage. D The expression level of CD 90 up to 6 h was significantly higher in saline and PBS. E The expression level of CD105 at 12 h was significantly higher in PBS. Cells not stored in carrier solutions served as controls. The results are representative of three independent experiments. The bar graph represents the mean ± SD. cADMSCs - canine adipose-derived mesenchymal stem cells, GAPDH - Glyceraldehyde-3-Phosphate Dehydrogenase, Saline - 0.9% saline, PBS - Phosphate-buffered saline, 5% DS - 5% Dextrose solution, Hepa-Sal - Heparin in saline, HS - Hartmann’s solution, RT-PCR- Reverse transcription-polymerase chain reaction. SD - Standard deviation. (*P < 0.05, **P < 0.001, and ***P < 0.0001)
At 6 h, cADMSCs showed the highest expression of Nanog in PBS and the lowest expression in 5% DS (Fig. 4B). cADMSCs stored in PBS, 5% DS, Hepa-Sal, and HS showed a significantly low expression level of Nanog at 12 h. Even though the expression of Nanog decreased at 6 h in saline, its expression was the highest at 12 h. PBS, 5% DS, and Hepa-Sal revealed an almost similar level of expression of Sox2 at 6 h (Fig. 4C). Sox2 expression in HS decreased gradually until 6 h but we observed higher expression at 12 h. A significantly lower expression of Sox2 was found in PBS at 12 h, and an approximately similar level of expression was observed after storage in the other solutions. Hepa-Sal revealed the highest expression of CD90 at 1 h, and the expression level was significantly higher in 5% DS and saline at 6 h and HS at 12 h (Fig. 4D). The expression of CD105 was affected over time, as it was significantly lower in HS at 6 h and significantly higher in saline at 12 h. PBS showed the highest expression of CD105 at 12 h (Fig. 4E).
Effects of carrier solutions on chondrogenic differentiation
Quantitative reverse transcription-polymerase chain reaction (RT-qPCR) was performed to evaluate the expression of each target gene in the chondrogenic differentiation process. As shown in Fig. 5A and B, the chondrogenic differentiation potential of cADMSCs was affected over time in the different solutions compared with that of freshly harvested undifferentiated cADMSCs.
Post-storage differentiation ability of cADMSCs. cADMSCs were suspended in various carrier solutions at 4 °C for different time points. GAPDH was used as the housekeeping control gene. All mRNA data were normalized to the level of GAPDH and relative fold changes in expression level were measured. (A) The expression of COL2A was significantly higher in saline until 6 h and in Hepa-Sal at 12 h. PBS showed the lowest expression at 12 h of storage. (B) The expression of Sox9 of cADMSCs stored in HS was significantly higher at 1 and 6 h of storage. cADMSCs stored in Hepa-Sal at 12 h showed the highest expression of Sox9. Differentiated cells not stored in carrier solutions served as positive controls. The results are representative of three independent experiments. The bar graph represents the mean ± SD. cADMSCs - canine adipose-derived mesenchymal stem cells, GAPDH - Glyceraldehyde-3-Phosphate Dehydrogenase, COL2A - collagen type IIa, Saline - 0.9% saline, PBS - Phosphate-buffered saline, 5% DS - 5% Dextrose solution, Hepa-Sal - Heparin in saline, HS - Hartmann’s solution, NC - Negative control, SD - Standard deviation. (*P < 0.05), (**P < 0.001), (***P < 0.0001)
Compared to the other carrier solutions, the expression of collagen type IIa (COL2A) was significantly higher in cADMSCs stored in saline for 1 h and decreased over time, whereas Hepa-Sal showed opposite trends of increase in its expression from 1 h to 12 h (Fig. 5A). The lowest expression of COL2A was observed in PBS at 12 h. In Contrast, storage in HS at 1 and 6 h also showed higher expression of Sox9; however, it decreased drastically at 12 h, as it may have been affected by a longer period of storage (Fig. 5B). Hepa-Sal revealed the highest Sox9 expression, whereas its expression in cADMSCs stored in saline and 5% DS decreased over time (until 12 h).
Discussion
Stem cells are a useful tool in the field of regenerative medicine, and promising stem cell-based cellular strategies are actively being developed to treat degenerative and fatal diseases [39]. In clinical settings, cell type is a significant criterion for stem cell therapy; other factors to consider include cell dose, route of administration, and most importantly, storage time [40, 41]. For transplantation, ADMSCs must be detached from the cell culture expansion vessel and immediately preserved in a carrier solution before administration to the patient. In practice, the prompt transplantation of ADMSCs is not always feasible under clinical conditions. Many cell transplantations and surgical processes, as well as long-distance transportation of ADMSCs, may increase the waiting time before transfusion. Currently, traditional storage methods including cryopreservation cause cell destruction due to the use of cryoprotectants such as dimethyl sulfoxide, and they have been replaced by supercooling [42], vitrification [43], high-subzero preservation [44], and various other novel methods for the long-term (months to years) storage of MSCs.
Considering that a pH that differs from the physiological pH can cause an unfavorable impact on cell viability, we measured the pH of the carrier solutions and found that all the solutions maintained an acceptable pH for parenteral transplantation.
In clinical application, an extensive increase of MSCs in vitro is required to attain adequate cell numbers. Serigano et al. reported the importance of many factors including cell confluence as prerequisites in optimizing the expansion of BM-MSCs [10], which may affect the biological properties of BM-MSCs. In our evaluation, cADMSCs stored in 5% DS showed a constant level of highest confluence until 12 h. Contrastingly, cADMSCs stored in PBS for 1, 6, and 12 h showed the lowest confluence at each time point compared with the other solutions. Overall, all the storage solutions showed better confluency compared to control conditions, which reveals that they may have some specific mechanism that can improve the confluency of MSCs. However, the precise mechanism by which these solutions improve cell proliferation during storage is unclear and should be investigated in future studies.
In our study, the viability of cADMSCs decreased rapidly over a short duration of storage. Our results showed > 72% viability in all solutions except for Hepa-Sal (63%) at 6 h of storage. Similarly, Sohn et al. found that after 6 h, the viability of human BMMSCs (hBMMSCs) at 4 °C or room temperature (RT) was > 85% [38]. Moreover, Pal et al. found the viability of hBMMSCs in saline, 5% DS, and Dulbecco’s PBS for up to 6 h of storage at 4 °C was > 90%, which was slightly greater than the viability observed in our study [45]. Additionally, Veronesi et al. found that the viability of BMMSCs stored in physiologic saline for 18 h was 83% [46], whereas Ra et al. observed that the average viability of hADMSCs was 85.4% after 72 h of storage [47]. Yan Chen et al. showed that the storage of human umbilical cord blood-derived MSCs (hUCBMSCs) in normal saline for 6 h at 4 °C and RT exhibited maximum viability of 83 and 77%, respectively [48]. Stanislaus et al. [49] compared the efficacy of physiologic saline, PBS, and Dulbecco’s Modified Eagle Medium (DMEM)-high glucose as temporary storage solutions for MSCs. They found that hUCBMSCs showed > 70% viability after storage in physiological saline for 72 h. Elisa et al. [50] compared saline and DMEM as storage solutions for hADMSCs and reported that both storage solutions resulted in > 70% viability after 48 h. Their conclusion is following our result that cADMSCs stored in saline for up to 12 h showed the best viability. Regarding PBS, we found that cADMSCs stored in PBS for 12 h at 4 °C showed approximately 65% viability, whereas Muraki et al. [51] found that the viability of hBMMSCs stored in PBS at 4 °C for 24 h was 81%. Besides, Stanislaus et al. [49] also reported the viability of hUCBMSCs stored in PBS for 24 h to be > 70%.
In this study, the viability of cADMSCs stored in 5% DS decreased from 1 h and remained > 61% at 12 h, which is lower than the corresponding values in the study by Chen et al. [48] who reported the viability of hUCBMSCs stored in 5% DS for 6 h to be 80%. Moreover, Patricia et al. found that at 4 °C, the viability of hADMSCs stored in 5% DS and HS for 48 h was maintained at approximately 80% [52]. However, we observed > 74% viability when cADMSCs were stored in HS for 12 h at 4 °C.
Similar to normal saline, cADMSCs stored in Hepa-Sal at various time points showed a gradual reduction in cell viability. Regardless, cADMSCs maintained > 61% viability until 12 h of storage. We were unable to compare our results with those of other studies [53,54,55] because despite determining the effects of administration of MSCs suspended in the various storage solutions, their viability before transplantation was not recorded.
A key property of MSCs is their high proliferation rate [48]. In our study, we found that the ability of cADMSCs to proliferate steadily decreased gradually. Storage in saline and 5% DS revealed similar rates of MSC proliferation until 6 h, whereas storage in PBS revealed the highest proliferation of cADMSCs. The rates of proliferation continued to decrease significantly until 12 h of storage, and cADMSCs stored in 5% DS had a significantly higher proliferation rate compared to the other carrier solutions. Our findings conform with those of Pal et al. [45] that storing MSCs for < 8 h at 4 °C in 5% DS and up to 6 h at 4 °C in saline constituted permissible limits for clinical transplantation. In Contrast, Bronzini et al. [56] reported that cADMSC-treated cells showed less sensitivity to apoptotic stimuli than freshly isolated cells when maintained for 12 h in the PBS at RT.
Self-renewal is a common feature of stem cells. Thus, we investigated the effect of carrier solutions on the self-renewal ability of cADMSCs at different time points. Consistent with the results of Sohn et al. [38] that the CFU ability of hBMMSCs decreased by approximately 50% after 2 h of storage in saline, we found that cADMSCs formed approximately 40 colonies or more until 6 h in saline, PBS, Hepa-Sal, and HS. Additionally, cADMSCs in all the solutions continued to form more than 38 colonies at 12 h of storage.
To determine whether pluripotency and surface markers of cADMSCs were affected by the carrier solutions, RT-PCR was performed, and the results were compared with untreated cells. At 1 h of storage, cADMSCs in 5% DS showed the highest expression of Nanog whereas cells in saline, PBS, Hepa-Sal, and HS showed an approximately similar expression of Nanog at 1 h. However, the expression level of Nanog at 12 h was significantly lower in all the solutions except saline. Sox2 is a pluripotency and self-renewal marker naturally expressed in MSCs at low levels in early passages and decreases with increasing passages [57]. The cADMSCs stored in saline and 5% DS for 1 h had the highest expression of Sox2. Similarly, Madonna et al. and Sujiwan et al. showed that a high concentration of dextrose upregulates the expression of Sox2 [58, 59]. Furthermore, cells stored in PBS for 12 h showed the lowest expression of Sox2 compared to that in cells stored in other solutions. The expression of positive MSC markers, CD90 and CD105, were also affected by carrier solutions. After 1 h of storage in Hepa-Sal, saline, and 5% DS, cADMSCs showed the highest expression of CD90 and had a moderate reduction in expression until 12 h, maintaining the highest expression in HS. Pal et al. found that MSCs expressed 99.5% positive CD90 when stored in 5% DS for 2 h [45]. Our results are similar to those of Ferda et al. who showed that human umbilical cord multipotent stromal cells showed a higher expression of CD90 until 36 h of storage in HS supplemented with 1% human serum albumin than in PBS [60]. Contrastingly, CD105 expression was higher in PBS than in any other solution at 12 h of storage.
To determine whether the biological function of cADMSCs was affected by the carrier solutions, the post-storage chondrogenic differentiation ability of cADMSCs in a time-dependent manner was investigated. Saline and HS showed a higher expression of COL2A and Sox9, respectively, at 6 h. The significant decrease of Sox9 expression in HS at 12 h can be a result of a longer duration of storage. cADMSCs stored in Hepa-Sal for 12 h showed the highest expression of both genes compared to other solutions. The higher chondrogenic ability of Hepa-Sal might be associated with the inherent nature of heparin as it ensures the secretion of endogenous growth factors such as transforming growth factor β1, vascular endothelial growth factor, and fibroblast growth factor from the cells, thereby promoting chondrogenesis [61, 62]. Besides, several studies have shown that the incorporation of heparin in hydrogel can improve the re-differentiation of differentiated chondrocytes and chondrocyte phenotypes [63, 64]. Chen et al. reported that when hUCBMSCs were stored in 0.9% saline, 5% DS, and other parenteral solutions for 6 h, MSCs from all solutions exhibited multi-differentiation (osteogenesis and adipogenesis) ability [48]. To date, there is no report conducted on the chondrogenic ability of MSCs on different storage solutions which remained unable to compare the results. Therefore, this subject needs to be uncovered in further study.
Using PBS or any other culture medium, such as DMEM, as a carrier solution is not approved by the FDA as they are suitable for in vitro use, not for transplantation [48]. There is evidence that the freshness and quality of hBMMSCs decrease after storage for 6 and 12 h in PBS [65]. Additionally, Boon et al. reported that a significant aggregation of hBMMSCs into cellular clumps when stored in PBS for 90 and 180 min at 0 °C may create an embolic hazard if delivered into blood vessels in cardiac applications and that it can block injection or infusion catheters applied for cell delivery during surgical operations, possibly affecting the overall effectiveness of transplantation therapy [66].
Exosomes are considered for the key paracrine factors that mediate the therapeutic activities of MSCs [67]. Ghadrdoost et al. transplanted MSCs combined with exogenous heparin in the treatment of cardiac infarction in rabbits; the efficacy of this treatment could be attributed to the heparin-mediated enhanced paracrine activity of MSCs [68]. Particularly, the exogenous heparin promoted the expression level of growth factors such as vascular endothelial growth factor. Accordingly, future studies should test the impact of our test carrier solutions on the yield and quality of MSC-derived exosomes for disease therapy. Furthermore, there is recent evidence of the protective use of various other solutions for the storage of MSCs such as University of Wisconsin (UW solution), Hank’s balanced salt solution (HBSS), and histidine-tryptophan-ketoglutarate (HTK) solution [69, 70]. A future comparative study of our selected short-term storage solutions with the hypothermic preservative solution (UW solution, HBSS, or HTK formulation) commonly implemented in solid organ transportation [71] will be appropriate for the study aims and clinical approaches.. However, UW solution and HTK solution are not appropriate to inject directly in the body whereas our selected carrier solutions can be applied for the cell transplantation what makes them a superior storage solution for having higher cell viability, reduced cost, and faster procedure.
Our results suggest that ADMSCs should be used within 6 h or not more than 12 h to ensure a high survival rate of cells and the efficacy of therapy. Moreover, an appropriate carrier solution should be selected based on the patient’s preexisting condition. For example, 5% DS should be avoided in patients with diabetes or hyperglycemia, and Hepa-Sal could be prioritized for cartilage regeneration and avoided in cases involving frequent bleeding tendency. Saline and HS can also be utilized as carrier solutions of ADMSCs depending on the necessity of the therapy. Notably, our study suggests that non-FDA-approved PBS should be replaced, preferably with Hepa-Sal to reduce the risk of embolisms, or any other FDA-approved solutions to increase cell viability. Further investigation on the effect of PBS on MSCs is warranted. Moreover, our findings need to be verified using in vivo models, and osteogenesis should also be examined.
Conclusion
The viability and efficacy of cADMSCs decreased over time when stored in different carrier solutions. Optimal storage is a requirement for the maximum utilization of their potential in clinical application. When storage is mandatory, ADMSCs can be stored in carrier solutions such as saline, 5% DS, Hepa-Sal, or HS at 4 °C, preferably for less than 6 h and no longer than 12 h. We also recommend replacing PBS with Hepa-Sal or any other FDA-approved carrier solution to ensure high cell viability, proliferation rates, differentiation ability, and native gene expression levels.
Methods
Isolation, culture, and expansion of ADMSCs
cADMSCs were isolated from the gluteal subcutaneous fat of a two-year-old Beagle that was primarily used for another objective in surgery research (Institutional Animal Care and Use approval number, KU18169–1). All the procedures were conducted according to the animal care and ethical guidelines of Konkuk University and Institutional Animal Care and Use guidelines for animal research. A previously described modified method was used to isolate the cells [72]. Briefly, the fat tissue was collected using the surgical procedure and washed thoroughly with PBS (Biowest, Seoul, South Korea). Then, the tissue was weighed (12 g) and digested with 0.1% collagenase type I (Worthington Biochemical Co., New Jersey, USA) prepared in sterile PBS and 1% penicillin-streptomycin (Gibco, New York, USA) for 1 h at 37 °C in a thermostatic water bath oscillator (Taitec Corporation, Saitama, Japan). The homogenate was centrifuged at 300×g for 10 min to distinguish the floating adipocytes from the stromal vascular fraction. Then, the supernatant was carefully discarded and the stromal vascular fraction was resuspended in DMEM-F12: (nutrient mixture) (Gibco), filtered with a 70-μm cell strainer (SPL Life Sciences, Gyeonggi-do, South Korea), and centrifuged at 150×g for 5 min to acquire a high-density cell pellet. The cells were plated at a density of 5 × 104 cells/cm2 in a T175 cm2 flask (SPL Life Sciences) and expanded in DMEM-F12supplemented with 10% fetal bovine serum (WELGENE Inc., Gyeongsangbuk-do, South Korea) and 1% penicillin-streptomycin in a humidified environment with 5% CO2 at 37 °C. The medium was replenished until 72 h, followed by a complete medium change on day 5 with the continuous microscopic observation of cell condition and attachment. We passaged the cells after reaching 80% confluence, cells were harvested and counted. Next, we suspended 5 × 105 -5 × 106 cADMSCs/vial (n = 10) containing 1 mL cell banker (Cell Banker 1, Nippon Zenyaku Kogyo Co., Ltd., Fukushima, Japan) at passage 1 for cryopreservation [73]. Cells from passage 2 were used for further studies [74].
Cell morphology and proliferation
Cell morphology was investigated via monolayer culture as described previously [75]. Briefly, cryopreserved cells were thawed in a water bath at 37 °C and cultured in 6-well plates (SPL Life Sciences) at 2 × 104 cells/cm2. When cells reached 80–90% confluency, they were trypsinized by 0.25% trypsin (Gibco) and stored in tested carrier solutions, namely saline (Greenflex, Gyeonggi-do, South Korea), PBS, 5% DS (Greenflex), Hepa-Sal (JW Pharmaceutical, Seoul, South Korea), and HS (Safe-Flex Health Care, Seoul, South Korea) for 1, 6, and 12 h at 4 °C (Table 2). After the end of the storage period, the cells were re-seeded into the complete growth medium in a humidified environment with 5% CO2 at 37 °C, and the post-storage morphology and confluence of the attached cells at 24 h were observed using an inverted photomicroscope (Olympus Korea Co. Ltd., Seoul, South Korea). The obtained pictures were analyzed using ImageJ software (National Institutes of Health, USA). Untreated cells were used as controls. All experiments were performed in triplicates.
pH measurements
In this experiment, we aimed to measure the pH range of the tested carrier solutions after the storage of cADMSCs in a time-dependent manner. cADMSCs were dissociated by 0.25% trypsin and were washed twice with PBS followed by resuspension at a concentration of 1 × 106 cells/mL in selected carrier solutions for 1, 6, and 12 h at 4 °C. After storage, the supernatant was collected and pH was measured in triplicates using a pH meter (Mettler Toledo, Giessen, Germany). Fresh solutions without cells at time 0 were used as controls.
Proliferation assay
To assess the proliferation capacity of post-storage cADMSCs, a cell proliferation assay was conducted using CCK-8 (Dojindo Molecular Technologies, Maryland, USA) following the manufacturer’s instructions. Briefly, post-storage, 5 × 103 cells per well were seeded in 96-well plates (SPL Life Sciences) until they reached confluency. We set untreated cells as controls. The culture media was removed and 100 μL of fresh media containing 10 μL of CCK-8 was added to each well. The plate was then incubated for 3 h at 37 °C and 5% CO2, and the absorbance was measured at 450 nm using a spectrophotometer (SpectraMax, Molecular Devices, CA, USA). All experiments were performed in triplicates.
MTT assay
The viability of post storage cADMSCs was measured using the MTT (3,4,5 – dimethylthiazol-2-yl)-2–5-diphenyltetrazolium bromide) assay kit (Abcam cat. ab211019, Gyeonggi-do, South Korea) following the manufacturer’s protocol. Briefly, post-storage, 10 × 103 cells/well were seeded in 96-well plates (SPL Life Sciences) until they reached confluency. Untreated cells were used as controls in the interpretation of the data. Cells were incubated with the MTT solution for 3 h at 37 °C and 5% CO2, followed by the addition of MTT solvent for 15 min. Optical density was measured at 590 nm using a spectrophotometer. All experiments were performed in triplicates.
Colony-forming unit assay
We measured the CFU of cADMSCs at different time points by seeding 200 cells/100 mm dish (SPL Life Sciences) post-storage in triplicates according to the previously described method [72]. Cells were stained at day 14 with 1% crystal violet (Sigma-Aldrich, Missouri, USA) in methanol (Sigma-Aldrich), washed, and photographed. Then colonies, with ≥50 cells were counted manually.
Chondrogenic differentiation
For chondrogenic differentiation, 1 × 106 cells were cultured in 6-well plates (SPL Life Sciences) [76]. After reaching 60–80% confluency, the pellets were made by transferring cells into a 15-mL tube (SPL Life Sciences) followed by centrifugation at 1600 rpm for 5 min. The supernatant was discarded and replaced with 1 mL of chondrogenic differentiation medium (Cell Applications, Inc., CA, USA). The media were changed every alternative day for 14 days.
Gene expression analysis
After storage in carrier solutions, RT-PCR was performed as described previously [72]. The total RNA was extracted by TRI reagent® (Favorgen Biotech Corp., Kaohsiung, Taiwan) application according to the manufacturer’s protocol. The RNA concentration was measured using NanoDrop software (Thermo Fischer Scientific, Seoul, South Korea). Using 2 μg of the total RNA, the complementary deoxyribonucleic acid (cDNA) was synthesized using the 1st Strand cDNA Synthesis Kit (Takara, Shiga, Japan) following the manufacturer’s guidelines. Gene expression of the canine housekeeping gene glyceraldehyde 3-phosphate dehydrogenase (GAPDH) (Bioneer Corporation, Daejeon, Korea) [77], Nanog, Sox2 [72] and a cluster of differentiation molecules such as CD45, CD90, and CD105 (the most commonly found negative and positive markers respectively for cADMSCs [78]) were investigated. To prepare 20 μL of the total reaction volume, 17 μL of distilled water, 1 μL of cDNA, and 1 μL each of 10 pmol of reverse and forward primers were used. PCR amplification was performed with 35 cycles at 60 °C for 30 s using the GeneAmp® PCR system 9700 (Applied BioSystems, Foster City, CA, USA). The PCR products were marked by gel electrophoresis on 2% agarose (Duchefa Biochemie, Haarlem, Netherland) using a DNA ladder (Thermo Fischer Scientific). Images were digitally detected and recorded using Gel Doc (Sigma-Aldrich).
For the determination of chondrogenesis, the total RNA was isolated on day 14 from undifferentiated and differentiated cells and cDNA was synthesized. To determine the expression of Sox9 and COL2A, RT-qPCR was conducted using Power SYBR Green reagents in a 7500 RT-PCR System (Applied Biosystems, California, USA). Gene expression levels were calculated using the 2(−ΔCt) method relative to GAPDH as a reference gene [79]. The PCR primer sequences for differentiation are summarized in Table 3.
Statistical analysis
The results were expressed as the mean ± standard deviation and analyzed by GraphPad Prism 6.0 (GraphPad Software, La Jolla, CA, USA) software, and the differences in mean number were determined by a student’s t-test. A probability level of *P < 0.05, ** P < 0.001, and ***P < 0.0001 was considered statistically significant.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADMSCs:
-
Adipose-derived mesenchymal stem cells
- BM:
-
Bone marrow
- BMMSCs:
-
Bone marrow-derived mesenchymal stem cells
- cADMSCs:
-
Canine ADMSCs
- CCK-8:
-
Cell Counting Kit-8
- CD:
-
Cluster of differentiation
- cDNA:
-
Complementary deoxyribonucleic acid
- CFU:
-
Colony-forming unit
- dH2O:
-
Deionized water
- 5% DS:
-
5% Dextrose solution
- DMEM-F12:
-
Dulbecco’s modified Eagle’s Medium: Nutrient Mixture
- F:
-
Forward
- FDA:
-
Food and Drug Administration
- GAPDH:
-
Glyceraldehyde 3- phosphate dehydrogenase
- Hepa-Sal:
-
Heparin in saline
- HS:
-
Hartmann’s solution
- HBSS:
-
Hank’s balanced salt solution
- HTK:
-
Histidine-tryptophan-ketoglutarate
- hADMSCs:
-
Human ADMSCs
- hBMMSCs:
-
Human BMMSCs
- hUCBMSCs:
-
Human umbilical cord blood-derived mesenchymal stem cells
- MSCs:
-
Mesenchymal stem cells
- MTT:
-
(3,4,5 – dimethylthiazol-2-yl)-2–5-diphenyltetrazolium bromide)
- PBS:
-
Phosphate-buffered saline
- RT:
-
Room temperature
- RT-PCR:
-
Reverse transcription-polymerase chain reaction
- R:
-
Reverse
- Saline:
-
0.9% saline
- UW solution:
-
University of Wisconsin solution
References
Collart-Dutilleul PY, Chaubron F, De Vos J, Cuisinier FJ. Allogenic banking of dental pulp stem cells for innovative therapeutics. World J Stem Cells. 2015;7(7):1010–21.
Caplan AI. Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. J Cell Physiol. 2007;213(2):341–7.
Le Blanc K, Frassoni F, Ball L, Locatelli F, Roelofs H, Lewis I, et al. Mesenchymal stem cells for treatment of steroid-resistant, severe, acute graft-versus-host disease: a phase II study. Lancet. 2008;371(9624):1579–86.
Jeong JA, Hong SH, Gang EJ, Ahn C, Hwang SH, Yang IH, et al. Differential gene expression profiling of human umbilical cord blood-derived mesenchymal stem cells by DNA microarray. Stem Cells. 2005;23(4):584–93.
Mohamadnejad M, Alimoghaddam K, Mohyeddin-Bonab M, Bagheri M, Bashtar M, Ghanaati H, et al. Phase 1 trial of autologous bone marrow mesenchymal stem cell transplantation in patients with decompensated liver cirrhosis. Arch Iran Med. 2007;10(4):459–66.
Zuk PA. Tissue engineering craniofacial defects with adult stem cells? Are we ready yet? Pharm Res. 2008;63(5):478–86.
Meza-Zepeda LA, Noer A, Dahl JA, Micci F, Myklebost O, Collas P. High-resolution analysis of genetic stability of human adipose tissue stem cells cultured to senescence. J Cell Mol Med. 2008;12(2):553–63.
Dahl JA, Duggal S, Coulston N, Millar D, Melki J, Shahdadfar A, et al. Genetic and epigenetic instability of human bone marrow mesenchymal stem cells expanded in autologous serum or fetal bovine serum. Int J Dev Biol. 2008;52(8):1033–42.
Schneider MR, Wolf E, Braun J, Kolb HJ, Adler H. Canine embryo-derived stem cells and models for human diseases. Hum Mol Genet. 2008;17(R1):R42–7.
Serigano K, Sakai D, Hiyama A, Tamura F, Tanaka M, Mochida J. Effect of cell number on mesenchymal stem cell transplantation in a canine disc degeneration model. J Orthop Res. 2010;28(10):1267–75.
Li G, Zhang XA, Wang H, Wang X, Meng CL, Chan CY, et al. Comparative proteomic analysis of mesenchymal stem cells derived from human bone marrow, umbilical cord, and placenta: implication in the migration. Proteomics. 2009;9(1):20–30.
Pal R, Hanwate M, Jan M, Totey S. Phenotypic and functional comparison of optimum culture conditions for upscaling of bone marrow-derived mesenchymal stem cells. Tissue Eng Regen Med. 2009;3(3):163–74.
Seeger FH, Tonn T, Krzossok N, Zeiher AM, Dimmeler S. Cell isolation procedures matter: a comparison of different isolation protocols of bone marrow mononuclear cells used for cell therapy in patients with acute myocardial infarction. Eur Heart J. 2007;28(6):766–72.
Park SS, Byeon YE, Ryu HH, Kang BJ, Kim Y, Kim WH, et al. Comparison of canine umbilical cord blood-derived mesenchymal stem cell transplantation times: involvement of astrogliosis, inflammation, intracellular actin cytoskeleton pathways, and neurotrophin-3. Cell Transplant. 2011;20(11–12):1867–80.
Hermann A, List C, Habisch HJ, Vukicevic V, Ehrhart-Bornstein M, Brenner R, et al. Age-dependent neuroectodermal differentiation capacity of human mesenchymal stromal cells: limitations for autologous cell replacement strategies. Cytotherapy. 2010;12(1):17–30.
Ikehara S. A new bone marrow transplantation method for stem cell disorders. Ann N Y Acad Sci. 2009;1173:774–80.
Guan Y, Li X, Yu W, Liang Z, Huang M, Zhao R, et al. Intravenous transplantation of Mesenchymal stem cells reduces the number of infiltrated Ly6C+ cells but enhances the proportions positive for BDNF, TNF-1α, and IL-1β in the infarct cortices of dMCAO rats. Stem Cells Int. 2018;2018:9207678.
Lin QM, Tang XH, Lin SR, Chen BD, Chen F. Bone marrow-derived mesenchymal stem cell transplantation attenuates overexpression of inflammatory mediators in rat brain after cardiopulmonary resuscitation. Neural Regen Res. 2020;15(2):324–31.
Jarocha D, Milczarek O, Wedrychowicz A, Kwiatkowski S, Majka M. Continuous improvement after multiple mesenchymal stem cell transplantations in a patient with complete spinal cord injury. Cell Transplant. 2015;24(4):661–72.
Yukawa H, Noguchi H, Oishi K, Takagi S, Hamaguchi M, Hamajima N, et al. Cell transplantation of adipose tissue-derived stem cells in combination with heparin attenuated acute liver failure in mice. Cell Transplant. 2009;18(5):611–8.
Ardanaz N, Vazquez FJ, Romero A, Remacha AR, Barrachina L, Sanz A, et al. Inflammatory response to the administration of mesenchymal stem cells in an equine experimental model: effect of autologous, and single and repeat doses of pooled allogeneic cells in healthy joints. BMC Vet Res. 2016;12(65):1–11.
Garvican ER, Cree S, Bull L, Smith RK, Dudhia J. Viability of equine mesenchymal stem cells during transport and implantation. Stem Cell Res Ther. 2014;5(4):94.
Strautz RL, Nelson JM, Meyer EA, Shulman IA. Compatibility of ADSOL-stored red cells with intravenous solutions. Am J Emerg Med. 1989;7(2):162–4.
Deorosan B, Nauman EA. The role of glucose, serum, and three-dimensional cell culture on the metabolism of bone marrow-derived mesenchymal stem cells. Stem Cells Int. 2011;2011:429187.
Ling L, Camilleri ET, Helledie T, Samsonraj RM, Titmarsh DM, Chua RJ, et al. Effect of heparin on the biological properties and molecular signature of human mesenchymal stem cells. Gene. 2016;576(1 Pt 2):292–303.
Furue MK, Na J, Jackson JP, Okamoto T, Jones M, Baker D, et al. Heparin promotes the growth of human embryonic stem cells in a defined serum-free medium. Proc Natl Acad Sci U S A. 2008;105(36):13409–14.
Sasaki N, Okishio K, Ui-Tei K, Saigo K, Kinoshita-Toyoda A, Toyoda H, et al. Heparan sulfate regulates self-renewal and pluripotency of embryonic stem cells. J Biol Chem. 2008;283(6):3594–606.
Uygun BE, Stojsih SE, Matthew HW. Effects of immobilized glycosaminoglycans on the proliferation and differentiation of mesenchymal stem cells. Tissue Eng A. 2009;15(11):3499–512.
Ling L, Dombrowski C, Foong K, Haupt L, Stein G, Nurcombe V, et al. Synergism between Wnt3a and heparin enhances osteogenesis via a phosphoinositide 3-kinase/Akt/RUNX2 pathway. J Biol Chem. 2010;285(34):26233–44.
Benoit DS, Durney AR, Anseth KS. The effect of heparin-functionalized PEG hydrogels on three-dimensional human mesenchymal stem cell osteogenic differentiation. Biomaterials. 2007;28(1):66–77.
Cyranoski D. Korean deaths spark inquiry. Nature. 2010;468(7323):485.
Liao L, Shi B, Chang H, Su X, Zhang L, Bi C, et al. Heparin improves BMSC cell therapy: anticoagulant treatment by heparin improves the safety and therapeutic effect of bone marrow-derived mesenchymal stem cell cytotherapy. Theranostics. 2017;7(1):106–16.
Mizuno M, Katano H, Otabe K, Komori K, Kohno Y, Fujii S, et al. Complete human serum maintains viability and chondrogenic potential of human synovial stem cells: suitable conditions for transplantation. Stem Cell Res Ther. 2017;8(1):144.
Khajavi MR, Etezadi F, Moharari RS, Imani F, Meysamie AP, Khashayar P, et al. Effects of normal saline vs. lactated ringer's during renal transplantation. Ren Fail. 2008;30(5):535–9.
Lichtenauer M, Nickl S, Hoetzenecker K, Mangold A, Moser B, Zimmermann M, et al. Phosphate buffered saline containing calcium and magnesium elicits increased secretion of Interleukin-1 receptor antagonist. Lab Med. 2009;40(5):290–3.
Jeon SH, Shrestha KR, Kim RY, Jung AR, Park YH, Kwon O, et al. Combination Therapy Using Human Adipose-derived Stem Cells on the Cavernous Nerve and Low-energy Shockwaves on the Corpus Cavernosum in a Rat Model of Post-prostatectomy Erectile Dysfunction. Urology. 2016;88:226 e1–9.
Ruoslahti E, Reed JC. Anchorage dependence, integrins, and apoptosis. Cell. 1994;77(4):477–8.
Sohn HS, Heo JS, Kim HS, Choi Y, Kim HO. Duration of in vitro storage affects the key stem cell features of human bone marrow-derived mesenchymal stromal cells for clinical transplantation. Cytotherapy. 2013;15(4):460–6.
Bang OY, Lee JS, Lee PH, Lee G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol. 2005;57(6):874–82.
O'Donnell L, Turner L, Levine AD. Part 6: the role of communication in better understanding unproven cellular therapies. Cytotherapy. 2016;18(1):143–8.
Helledie T, Dombrowski C, Rai B, Lim ZX, Hin IL, Rider DA, et al. Heparan sulfate enhances the self-renewal and therapeutic potential of mesenchymal stem cells from human adult bone marrow. Stem Cells Dev. 2012;21(11):1897–910.
Sultana T, Lee JI, Park JH, Lee S. Supercooling storage for the transplantable sources from the rat and the rabbit: a preliminary report. Transpl Proceed. 2018;50(4):1178–82.
Bang S, Lee GK, Shin H, Suh CS, Lim HJ. Vitrification, in vitro fertilization, and development of Atg7 deficient mouse oocytes. Clin Experimental Reproduct Med. 2016;43(1):9–14.
Taylor MJ, Weegman BP, Baicu SC, Giwa SE. New approaches to cryopreservation of cells, tissues, and organs. Transfus Med Hemother. 2019;46(3):197–215.
Pal R, Hanwate M, Totey SM. Effect of holding time, temperature and different parenteral solutions on viability and functionality of adult bone marrow-derived mesenchymal stem cells before transplantation. Tissue Eng Regen Med. 2008;2(7):436–44.
Piccinno MS, Rasini V, Giordano R, Montemurro T, Bourin P, Sensebe L, et al. Transportation conditions for prompt use of ex vivo expanded and freshly harvested clinical-grade bone marrow mesenchymal stromal/stem cells for bone regeneration. Tissue Eng Part C. 2014;20(3):239–51.
Ra JC, Shin IS, Kim SH, Kang SK, Kang BC, Lee HY, et al. Safety of intravenous infusion of human adipose tissue-derived mesenchymal stem cells in animals and humans. Stem Cells Dev. 2011;20(8):1297–308.
Chen Y, Yu B, Xue G, Zhao J, Li RK, Liu Z, et al. Effects of storage solutions on the viability of human umbilical cord mesenchymal stem cells for transplantation. Cell Transplantion. 2013;22(6):1075–86.
Krishnanda SI, Agarwal R, Yausep OE, Rizkita M, Angraeni R, Pawitan JA. Comparison of various solutions for temporary storage of umbilical cord derived Mesenchymal stem cells. Annu Res Rev Biol. 2017;21(2):1–8.
Nofianti CE, Sari IN, Marlina, Novialdi, Pawitan JA Temporary storage solution for adipose derived mesenchymal stem cells. Stem Cell Investig 2018;5:19.
Muraki K, Hirose M, Kotobuki N, Kato Y, Machida H, Takakura Y, et al. Assessment of viability and osteogenic ability of human mesenchymal stem cells after being stored in suspension for clinical transplantation. Tissue Eng. 2006;12(6):1711–9.
Galvez-Martin P, Hmadcha A, Soria B, Calpena-Campmany AC, Clares-Naveros B. Study of the stability of packaging and storage conditions of human mesenchymal stem cell for intra-arterial clinical application in patient with critical limb ischemia. Eur J Pharm Biopharm. 2014;86(3):459–68.
Quimby JM, Webb TL, Habenicht LM, Dow SW. Safety and efficacy of intravenous infusion of allogeneic cryopreserved mesenchymal stem cells for treatment ofchronic kidney disease in cats: results of three sequential pilot studies. Stem Cell Res Ther. 2013;4:48.
Quimby JM, Webb TL, Randall E, Marolf A, Valdes-Martinez A, Dow SW. Assessment of intravenous adipose-derived allogeneic mesenchymal stem cells for the treatment of feline chronic kidney disease: a randomized, placebo-controlled clinical trial in eight cats. J Feline Med Surg. 2015;18(2):165–71.
Gotherstrom C, Westgren M, Shaw SW, Astrom E, Biswas A, Byers PH, et al. Pre- and postnatal transplantation of fetal mesenchymal stem cells in osteogenesis imperfecta: a two-center experience. Stem Cells Transl Med. 2014;3(2):255–64.
Bronzini I, Patruno M, Iacopetti I, Martinello T. Influence of temperature, time and different media on mesenchymal stromal cells shipped for clinical application. Vet J. 2012;194(1):121–3.
Han SM, Han SH, Coh YR, Jang G, Chan Ra J, Kang SK, et al. Enhanced proliferation and differentiation of Oct4- and Sox2-overexpressing human adipose tissue mesenchymal stem cells. Exp Mol Med. 2014;46:e101.
Seubbuk S, Sritanaudomchai H, Kasetsuwan J, Surarit R. High glucose promotes the osteogenic differentiation capability of human periodontal ligament fibroblasts. Mol Med Rep. 2017;15(5):2788–94.
Madonna R, Geng YJ, Shelat H, Ferdinandy P, De Caterina R. High glucose-induced hyperosmolarity impacts proliferation, cytoskeleton remodeling and migration of human induced pluripotent stem cells via aquaporin-1. Biochim Biophys Acta. 2014;1842(11):2266–75.
Celikkan FT, Mungan C, Sucu M, Ulus AT, Cinar O, Ili EG, et al. Optimizing the transport and storage conditions of current good manufacturing practice -grade human umbilical cord mesenchymal stromal cells for transplantation (HUC-HEART trial). Cytotherapy. 2019;21(1):64–75.
Noh YK, Du P, Dos Santos Da Costa A, Park K. Induction of chondrogenesis of human placenta-derived mesenchymal stem cells via heparin-grafted human fibroblast derived matrix. Biomaterials Research. 2018;22:12.
Chung HJ, Kim HK, Yoon JJ, Park TG. Heparin immobilized porous PLGA microspheres for angiogenic growth factor delivery. Pharm Res. 2006;23(8):1835–41.
Kim M, Kim SE, Kang SS, Kim YH, Tae G. The use of de-differentiated chondrocytes delivered by a heparin-based hydrogel to regenerate cartilage in partial-thickness defects. Biomaterials. 2011;32(31):7883–96.
Brown GCJ, Lim KS, Farrugia BL, Hooper GJ, Woodfield TBF. Covalent Incorporation of Heparin Improves Chondrogenesis in Photocurable Gelatin-Methacryloyl Hydrogels. Macromol Biosci. 2017;17(12).
Shin TH, Lee S, Choi KR, Lee DY, Kim Y, Paik MJ, et al. Quality and freshness of human bone marrow-derived mesenchymal stem cells decrease over time after trypsinization and storage in phosphate-buffered saline. Sci Rep. 2017;7(1):1106.
Heng BC, Cowan CM, Basu S. Temperature and calcium ions affect aggregation of mesenchymal stem cells in phosphate buffered saline. Cytotechnology. 2008;58(2):69–75.
Akyurekli C, Le Y, Richardson RB, Fergusson D, Tay J, Allan DS. A systematic review of preclinical studies on the therapeutic potential of mesenchymal stromal cell-derived microvesicles. Stem Cell Rev Rep. 2015;11(1):150–60.
Ghadrdoost B, Khoshravesh R, Aboutaleb N, Amirfarhangi A, Dashti S, Azizi Y. Heparin enhances the effects of Mesenchymal stem cell transplantation in a rabbit model of acute myocardial infarction. Nigerian J Physiol Sci. 2018;33(1):9–15.
Nahar S, Nakashima Y, Miyagi-Shiohira C, Kinjo T, Kobayashi N, Saitoh I, et al. A comparison of the preservation of mouse adipose tissue-derived mesenchymal stem cells using the University of Wisconsin solution and Hank’s balanced salt solution. Stem Cells Int. 2018;2018.
von Oppell UO, Pfeiffer S, Preiss P, Dunne T, Zilla P, Reichart B. Endothelial cell toxicity of solid-organ preservation solutions. Ann Thorac Surg. 1990;50(6):902–10.
Mangus RS, Tector AJ, Agarwal A, Vianna R, Murdock P, Fridell JA. Comparison of histidine-tryptophan-ketoglutarate solution (HTK) and University of Wisconsin solution (UW) in adult liver transplantation. Liver Transpl. 2006;12(2):226–30.
Neupane M, Chang CC, Kiupel M, Yuzbasiyan-Gurkan V. Isolation and characterization of canine adipose-derived mesenchymal stem cells. Tissue Eng Part A. 2008;14(6):1007–15.
Martinello T, Bronzini I, Maccatrozzo L, Mollo A, Sampaolesi M, Mascarello F, et al. Canine adipose-derived-mesenchymal stem cells do not lose stem features after a long-term cryopreservation. Res Vet Sci. 2011;91(1):18–24.
Bernardo ME, Zaffaroni N, Novara F, Cometa AM, Avanzini MA, Moretta A, et al. Human bone marrow derived mesenchymal stem cells do not undergo transformation after long-term in vitro culture and do not exhibit telomere maintenance mechanisms. Cancer Res. 2007;67(19):9142–9.
Kim AY, Kim Y, Lee SH, Yoon Y, Kim WH, Kweon OK. Effect of gelatin on Osteogenic cell sheet formation using canine adipose-derived Mesenchymal stem cells. Cell Transplant. 2017;26(1):115–23.
Sasaki A, Mizuno M, Ozeki N, Katano H, Otabe K, Tsuji K, et al. Canine mesenchymal stem cells from synovium have a higher chondrogenic potential than those from infrapatellar fat pad, adipose tissue, and bone marrow. PLoS One. 2018;13(8):e0202922.
Okui Y, Kano R, Maruyama H, Hasegawa A. Cloning of canine toll-like receptor 7 gene and its expression in dog tissues. Vet Immunol Immunopathol. 2008;121(1–2):156–60.
Mildmay-White A, Khan W. Cell surface markers on adipose-derived stem cells: a systematic review. Curr Stem Cell Res Therapy. 2017;12(6):484–92.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods. 2001;25(4):402–8.
Acknowledgments
The authors wish to thank Regeniks Co., Ltd., and veterinarian Muyoung Kim for helping us obtain the fat tissue. The authors also convey their gratitude to Umair Jan, Institute of Biomedical Science and Technology, Konkuk University for assisting in arranging references.
Funding
The present study was fully supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. NRF-2019R1F1A1047244). The funder had no role in the study design, data analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
T.S performed all the experiments, wrote the paper, and got assistance for statistical analysis from S.B.L. A.A.D helped with manuscript drafting, designing an experiment, and figure preparation. Finally, S.G.C contributed to the writing and final review of the manuscript. Funding management and conception were carried out by J.I.L. All authors reviewed and agreed on the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The adipose tissue collected from a beagle was primarily used for another objective in surgery research at Konkuk University (Institutional Animal Care and Use approval number KU18169–1). All the animal procedures undertaken had Institutional Animal Care and Use approval, and all the relevant institutional and national animal care and maintenance guidelines were followed.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sultana, T., Dayem, A.A., Lee, S.B. et al. Effects of carrier solutions on the viability and efficacy of canine adipose-derived mesenchymal stem cells. BMC Vet Res 18, 26 (2022). https://doi.org/10.1186/s12917-021-03120-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-021-03120-4