Abstract
Background
Cervical cancer incidence is rising in Puerto Rico (PR). Whether the increase is real or reflective of increased diagnostic scrutiny remains unclear.
Methods
Using data from the PR Central Cancer Registry for 2001–2019, we estimated trends of hysterectomy-corrected cervical cancer incidence and mortality rates, overall, and by stage at diagnosis and age.
Results
Overall, cervical cancer incidence (per 100,000) increased 1.6%/year (95% CI, -0.5% to 3.8%) from 12.5 to 15.3, with a prominent increase in distant-stage disease (4.5%/year [95% CI, 1.6% to 8.0%]), particularly among screening age eligible (25–64-year-old) women (5.8%/year [95% CI, 2.1% to 10.6%]). Mortality rates in this age-group remained stable during the study period.
Conclusions
Increased occurrence of distant-stage disease among screening-eligible women is troubling and may reflect a real increase. Future research is needed to elucidate the factors underlying these trends. Improved prevention is also an urgent priority to reverse the rising cervical cancer incidence in PR.
Similar content being viewed by others
Background
Cervical cancer continues to be a major public health issue among the Hispanic population living in the United States (US) [1]. Unfortunately, in recent years, cervical cancer incidence has not decreased in the mainland US [2]. On the other hand, Puerto Rico (PR), a US territory that is home to nearly 2 million Hispanic or Latino population, is seeing a continued rise in cervical cancer incidence [3]. Timely follow-up care and treatment after an abnormal Pap result have been hampered due to repetated disaster events and the decreasing number of gynecologists on the island, where healthcare infrastructure is already inadequate [4]. As a result, cervical cancer incidence patterns, particularly stage at diagnosis, and mortality may have been influenced in recent years. In this study, we sought to evaluate trends of hysterectomy-corrected cervical cancer incidence and mortality rates in PR, overall and stratified by stage at diagnosis and age.
Methods
Incidence and mortality data were obtained from the PR Central Cancer Registry for 2001–2019, which collects sociodemographic and clinical information on all cancers diagnosed. We also used data from the 17-registries Surveillance, Epidemiology, and End Results (SEER) Program for 2001–2019, and evaluated incidence trends among Hispanic women in the mainland US. Cervical cancer cases were identified using the International Classification of Diseases for Oncology Third Edition site codes C53.0 to C53.9, and histology codes 8010 to 8671 and 8940 to 8941were used in order to focus on HPV-associated cases only. Hysterectomy information was obtained from the Behavioral Risk Factor Surveillance System (BRFSS) during the study period. Hysterectomy-corrected incidence and mortality rates were estimated following methods employed in similar studies [5, 6].
BRFSS is a nationally representative survey conducted by phone in the US and three territories (including PR) and collects information about health-related risk behaviors, health conditions, and the use of preventive services [7]. Logistic regression was used to calculate smoothed hysterectomy prevalence estimates considering age groups (18–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, and 80 + years), survey years, and an interaction term for age group and survey year. Age and year specific hysterectomy prevalence rates were used to estimate the corresponding population at-risk, by excluding the proportion of women with a history of hysterectomy from the denominators. After the corrections for hysterectomy prevalence were completed, incidence and mortality rates were standardized based on the age distribution of the 2000 US population.
Joinpoint Regression Program software (version 5.0.2) was used to estimate annual percent changes (APC) and average annual percent changes (AAPC) of trends, with their corresponding 95% confidence intervals (95% CI), which were calculated using the empirical quantile method. Incidence analysis was stratified by stage (localized, regional, and distant) and age (< 25 years, 25–64 years and ≥ 65 years), and mortality analysis was stratified by age (< 25 years, 25–64 years and ≥ 65 years). Since all the information evaluated in this study was de-identified, the University of Puerto Rico Comprehensive Cancer Center Institutional Review Board considered this study exempt.
Results
A total of 3,916 cervical cancer cases were diagnosed in PR during the study period. Trends of hysterectomy-corrected cervical cancer incidence rates are presented in Table 1. During 2001–2019, hysterectomy-corrected cervical cancer incidence in PR (per 100,000 person-years) increased from 12.5 to 15.3 (AAPC, 1.6% [95% CI, -0.5% to 3.8%]), largely driven by a marked rise during 2001–2010 (APC, 3.5% [95% CI, 1.3% to 26.6%]). In recent years (2010–2019), incidence moderated (APC, -0.3% [ 95% CI, -17.8% to 1.9%]).
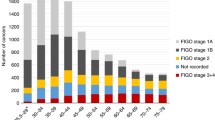
Trends in incidence according to stage at diagnosis are also presented in Table 1. Notably, distant stage cervical cancer incidence increased 4.5%/year (95% CI, 1.6% to 8.0%) during 2001–2019. Localized stage cervical cancer incidence increased, although not significantly, during 2001–2009 (APC, 4.5% [95% CI, -4.8% to 11.9%]), followed by a non-significant decrease during 2009–2013 (APC, -9.8% [95% CI, -18.6% to 10.9%]) and a recent non-significant increase during 2013–2019 (APC, 3.5% [95% CI, -3.3% to 22.4%]). Regional stage cervical cancer incidence increased during 2001–2017 (APC, 2.6% [95% CI, 1.7% to 4.8%]), followed by a decline in 2017–2019 (APC, -16.3% [95% CI, -25.3% to -0.3%]).
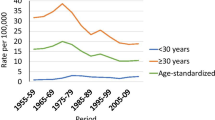
Trends of cervical cancer incidence comparing Puerto Rican and Hispanic women in the US are presented in Fig. 1. Contrary to PR, cervical cancer incidence among Hispanic women in the US is decreasing overall, and for localized and regional stages. For distant stage, we observed that US Hispanic women have a higher incidence. Despite of this, late-stage diagnoses among US Hispanic women have stabilized, while we observed an increase in PR.
In the analysis stratified by age, overall, non-significant changes in incidence rates were observed among the youngest (< 25 years) (APC, 1.2% [95% CI, -7.0% to 9.5%]) and oldest (≥ 65 years) (AAPC, -1.1% [95% CI, -3.3% to 1.2%]) age groups. Among 25–64-year-old group, incidence fluctuated during the study period, with a non-significant decrease during 2001–2005 (APC, -2.9% [95% CI, -12.9% to 3.4%]), followed by a significant increase during 2005–2009 (APC, 9.7% [95% CI, 2.6% to 17.0%]), and a recent stabilization during 2009–2019 (APC, 0.1% [95% CI, -2.3% to 1.7%]).
Trends of cervical cancer incidence rates by age and stage at diagnosis, reveal that in the 25–64-year-old group, localized tumors did not change during 2001–2019 (APC, 0.3% [95% CI, -1.5% to 2.0%]). Regional stage tumors had a significant increase during 2001–2017 (APC, 4.0% [95% CI, 9.0% to 38.8%]), followed by a recent non-significant decrease during 2017–2019 (APC, -16.2% [95% CI, -35.5% to 4.6%]). A significant increase of 5.8%/year (95% CI, 2.1% to 10.6%) occurred for distant stage cervical cancer. Among ≥ 65 years group, significant changes were observed during the study period, with an intial increase during 2001–2006 (APC, 14.0% [95% CI, 1.4% to 74.8%]), followed by a recent decrease in 2006–2019 (APC, -8.3% [95% CI, -15.2% to -5.5%]). A non-significant decrease was observed for regional stage tumors in the oldest group (APC, -2.8% [95% CI, -5.8% to 0.1%]).
Although hysterectomy-corrected mortality rates (per 100,000 person-years) increased from 2.5 in 2001 to 4.0 in 2019, no significant changes were observed overall (APC, -0.4% [95% CI, -2.3% to 1.6%]) nor in the 25–64-years age group (APC, 0.4% [95% CI, -1.8% to 2.7%]). Among the ≥ 65 years group, a non-significant initial increase in mortality rate was documented in 2001–2003 (APC, 48.9% [95% CI, -1.2% to 120.1%]), followed by a significant decrease during 2003–2019 (APC, -3.1% [95% CI, -15.1% to -0.9%]) (Table 2).
Discussion
In this population-based analysis of cervical cancer incidence and mortality patterns during 2001–2019 in PR, we observed that incidence rates increased among the screening age-eligible (25–64 years) group, while mortality rates remained stable. Increased occurrence of late-stage disease and no reductions in mortality suggest that the rising of cervical cancer incidence in PR may be real and not reflective of increased screening.
Similar to our findings, a recent US-based study also demonstrated that distant-stage cervical cancer incidence increased significantly at a similar rate (4.4%/year) among non-Hispanic White women living in low-income counties and a positive 1.5%/year change was also observed among Hispanic women [8]. Moreover, a study using data from the Texas Cancer Registry reported that non-Hispanic Black and Hispanic women had higher odds of late-stage cervical cancer diagnosis, primarily attributed to a higher neighborhood socioeconomic disadvantage among these populations [9]. While the reason for these patterns remains unclear, one may speculate that suboptimal screening behaviors and disruptions in follow-up care in low-resourced settings may be contributors. Future research is needed to explain these patterns among low-resourced US settings.
Barriers to cervical cancer screening in PR include low educational attainment, low income, and lack of health insurance, smoking, morbid obesity, and high-risk sexual behaviors [10,11,12]. In addition, our research team documented that hurricanes Irma and Maria in 2017 and the COVID-19 pandemic in 2020 had an impact on cervical cancer screening uptake in the island [13]. Thus, our study findings together with documented barriers to screening in PR highlight the need for continued efforts to reduce these barriers and promote the prevention and early detection of cervical cancer in this population.
More research focused on assessing and addressing barriers to cervical cancer screening and timely follow-up and treatment is needed in this population. This will be essential to achieve the goal of cervical cancer elimination established by the World Health Organization (< 4 cases per 100,000 population) [14]. For cervical cancer screening, our research team documented that 70% of cervical cancer patients in PR diagnosed from 2011–2014 were screened within 3 years prior their diagnosis [15]. Among these, only 22% were also tested for HPV, showing lower utilization of HPV testing in this population in comparison to cervical Papanicolau. While future research should evaluate the impact of HPV testing uptake on disease trends in PR, our findings evidence significant increases in late stage and not early stage disease.
Unfortunately, similar to the US, strategies to enhance screening delivery (patient reminder, navigation) are not widely implemented in PR in the absence of evidence on their effectiveness and cost-effectiveness. A recently funded study (Grant: 1R01CA282424) will evaluate these interventions and HPV self-sampling approach with the goal to provide foundational data to ensure the wide implementation of these interventions.
Strengths of this study include the use of the PR Central Cancer Registry database, which allowed us to have population-based data from PR to describe the incidence and mortality rates in our analysis. Among limitations, we could not include individual information such as history of cervical cancer screening uptake and HPV infection and other information related to barriers to cervical cancer screening, follow-up, and access to treatment.
Conclusions
In summary, cervical cancer incidence in PR is increasing, especially distant-stage disease among screening eligible persons. Future research must elucidate the factors underlying these trends and the potential impact of the COVID-19 pandemic on future disease trends. Continued improvement in prevention is needed to mitigate the rising cervical cancer burden in PR.
Availability of data and materials
The data that supports the findings of this study came from the Puerto Rico Central Cancer Registry (PRCCR) database. Thus, data from this study is not publicly available because of the confidentiality agreement between PRCCR and the authors. Nevertheless, investigators could obtain the data through PRCCR following the confidentiality procedures. PRCCR data can be requested through the following site: https://rcpr.org/Datos-de-C%C3%A1ncer/Acceso-a-Datos.
Abbreviations
- AAPC:
-
Average annual percent change
- APC:
-
Annual percent change
- BRFSS:
-
Behavioral Risk Factor Surveillance System
- PR:
-
Puerto Rico
- US:
-
United States
References
Miller KD, Ortiz AP, Pinheiro PS, et al. Cancer statistics for the US Hispanic/Latino population, 2021. CA Cancer J Clin. 2021;71(6):466–87. https://doi.org/10.3322/caac.21695.
Deshmukh AA, Suk R, Shiels MS, et al. Incidence trends and burden of human papillomavirus-associated cancers among women in the United States, 2001–2017. JNCI J Natl Cancer Inst. 2021;113(6):792–6. https://doi.org/10.1093/jnci/djaa128.
Ortiz AP, Ortiz-Ortiz KJ, Colón-López V, et al. Incidence of cervical cancer in Puerto Rico, 2001–2017. JAMA Oncol. 2021;7(3):456. https://doi.org/10.1001/jamaoncol.2020.7488.
Perreira K, Peters R, Lallemand N, Zuckerman S. Puerto Rico Health Care Infrastructure Assessment. Site Visit Report. The Urban Institute. Published online January 2017. https://www.urban.org/sites/default/files/publication/87011/2001050-puerto-rico-health-care-infratructure-assessment-site-visit-report_1.pdf. Accessed 3 Feb 2024
Clarke MA, Devesa SS, Harvey SV, Wentzensen N. Hysterectomy-corrected uterine corpus cancer incidence trends and differences in relative survival reveal racial disparities and rising rates of nonendometrioid cancers. J Clin Oncol Off J Am Soc Clin Oncol. 2019;37(22):1895–908. https://doi.org/10.1200/JCO.19.00151.
Damgacioglu H, Burus T, Sonawane K, Hill E, Lang Kuhs KA, Deshmukh AA. County-level trends in cervical cancer incidence, stage at diagnosis, and mortality in kentucky. JAMA Netw Open. 2023;6(10):e2338333. https://doi.org/10.1001/jamanetworkopen.2023.38333.
Center for Disease Control and Prevention. About BRFSS. Published February 9, 2019. https://www.cdc.gov/brfss/about/index.htm. Accessed 18 Jan 2024.
Amboree TL, Damgacioglu H, Sonawane K, Adsul P, Montealegre JR, Deshmukh AA. Recent trends in cervical cancer incidence, stage at diagnosis, and mortality according to county-level income in the United States, 2000–2019. Int J Cancer. https://doi.org/10.1002/ijc.34860. Published online Jan 25, 2024.
Sokale IO, Oluyomi AO, Montealegre JR, Thrift AP. Racial/ethnic disparities in cervical cancer stage at diagnosis: mediating effects of neighborhood-level socioeconomic deprivation. Cancer Epidemiol Biomarkers Prev. 2023;32:818–24.
González D, Suárez EL, Ortiz AP. Cervical cancer screening and sexual risky behaviors among a population of hispanic origin. Womens Health Issues Off Publ Jacobs Inst Womens Health. 2015;25(3):254–61. https://doi.org/10.1016/j.whi.2015.01.002.
Pérez CM, González-Barrios D, Ramos-Cartagena JM, Ortiz AP. Association of body mass index with adherence to cervical cancer screening recommendations in hispanic women. J Low Genit Tract Dis. 2020;24(1):14–20. https://doi.org/10.1097/LGT.0000000000000504.
Gopalani SV, Soman A, Shapiro JA, et al. Breast, cervical, and colorectal cancer screening test use in the US territories of Guam, Puerto Rico, and the US Virgin Islands. Cancer Epidemiol. 2023;84:102371. https://doi.org/10.1016/j.canep.2023.102371.
Ortiz AP, Gierbolini-Bermúdez A, Ramos-Cartagena JM, et al. Cervical cancer screening among medicaid patients during natural disasters and the COVID-19 Pandemic in Puerto Rico, 2016 to 2020. JAMA Netw Open. 2021;4(10):e2128806. https://doi.org/10.1001/jamanetworkopen.2021.28806.
World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. 2020. Accessed February 7, 2024. https://www.who.int/publications-detail-redirect/9789240014107
Gómez-Vargas V, Ortiz-Ortiz KJ, Almodóvar-Rivera I, Torres-Cintrón CR, Deshmukh AA, Ortiz AP. Screening history and survival among women with cervical cancer in Puerto Rico. J Low Genit Tract Dis. 2023;27:19–23.
Acknowledgements
Not applicable.
Funding
This study was partially funded by the University of Puerto Rico and the University of Texas MD Anderson Cancer Center Partnership for Excellence in Cancer Research (NCI Grant 2U54CA096297 and Grant 2U54CA096300), by The effectiveness, cost-effectiveness, and budget impact of interventions to improve the delivery of cervical cancer screening in Puerto Rico study (NCI Grant 1R01CA282424) and by the National Program of Cancer Registries (NPCR) of the Centers for Disease Control and Prevention (CDC) (Grant NU58DP006318) to the Puerto Rico Central Cancer Registry (PRCCR). The funders did not play a role in the design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to this paper as follows: study conception and design: APO, CRT, EJS, JMR, HD, VC, KJO, AAD; data preparation and analysis: CRT, EJS, TSR; interpretation, and writing: APO, EJS, JMR, HD, AAD; supervision: APO, AAD; critical review and editing: all authors. All authors reviewed the results and approved the submitted manuscript.
Authors’ Twitter handles
@AnaPatriOrtiz (APO); @edusan218 (EJS); @ashish_deshmukh (AAD); @GroupHpv (HPV Interest Group led by research team).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The University of Puerto Rico Comprehensive Cancer Center Institutional Review Board considered this study exempt (number: 2019–09-11).
Consent for publication
Not applicable.
Competing interests
Dr. Deshmukh reported receiving consulting fees from Merck Inc and Value Analytics Lab outside the submitted work. Dr. Ortiz has been a consultant for Merck Inc and participates in an institutional grant funded by Merck Inc outside the submitted work. No additional competing interests were reported by the rest of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ortiz, A.P., Torres-Cintrón, C.R., Santiago-Rodríguez, E.J. et al. Recent cervical cancer incidence, stage at diagnosis, and mortality trends in Puerto Rico, 2001–2019. BMC Med 22, 327 (2024). https://doi.org/10.1186/s12916-024-03535-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03535-4