Abstract
Background
Renal outcomes in patients with type 2 diabetes following treatment with sodium–glucose co-transporter-2 inhibitors (SGLT2is) or glucagon-like peptide-1 receptor agonists (GLP1RAs) have not been directly compared. This study compared the impact of SGLT2i and GLP1RA therapy on renal function and metabolic parameters.
Methods
Patients with type 2 diabetes who initiated SGLT2i or GLP1RA therapy in a tertiary hospital between January 2009 and August 2023 were included to assess composite renal outcomes, such as a 40% decline in estimated glomerular filtration rate (eGFR), onset of end-stage renal disease, renal death, or new-onset macroalbuminuria. Alterations in blood pressure, glucose regulation parameters, lipid profile, and anthropometric parameters, including body fat and muscle masses, were examined over 4-years.
Results
A total of 2,112 patients were enrolled using a one-to-three propensity-score matching approach (528 patients for GLP1RAs, 1,584 patients for SGLT2i). SGLT2i treatment was favoured over GLP1RA treatment, though not significantly, for composite renal outcomes (hazard ratio [HR], 0.63; p = 0.097). SGLT2i therapy preserved renal function effectively than GLP1RAs (decrease in eGFR, ≥ 40%; HR, 0.46; p = 0.023), with improving albuminuria regression (HR, 1.72; p = 0.036). SGLT2i therapy decreased blood pressure and body weight to a greater extent. However, more patients attained HbA1c levels < 7.0% with GLP1RAs than with SGLT2is (40.6% vs 31.4%; p < 0.001). GLP1RA therapy enhanced β-cell function and decreased LDL-cholesterol levels below baseline values.
Conclusions
SGLT2is were superior for preserving renal function and reducing body weight, whereas GLP1RAs were better for managing glucose dysregulation and dyslipidaemia.
Similar content being viewed by others
Background
Type 2 diabetes is a multifactorial, chronic metabolic disorder that afflicts more than 600 million people worldwide, often leading to severe complications, including cardiovascular and renal diseases [1]. The therapeutic management of this complex disease provides an ongoing clinical challenge, necessitating the development of a diverse spectrum of pharmacological agents targeting various pathophysiological aspects. Among these, sodium–glucose co-transporter 2 inhibitors (SGLT2is) and glucagon-like peptide-1 receptor agonists (GLP1RAs) have emerged as two promising antidiabetic agents. Both have demonstrated efficacy in glycaemic control, cardiovascular risk mitigation, and improvement of renal outcomes in placebo-controlled randomized clinical trials (RCTs) [2, 3].
In addition to cardiovascular diseases (CVDs), diabetic nephropathy poses a significant clinical burden in type 2 diabetes and is a leading cause of mortality in affected patients [4]. Both SGLT2is and GLP1RAs have demonstrated favourable impacts on renal outcomes in RCTs [5, 6]. To the best of our knowledge, however, the impact of these two medication classes on renal outcomes has not yet been compared directly. Although there have been some meta-analyses comparing these effects [3, 7], such indirect comparisons are limited by inconsistent definitions of composite renal outcomes across the studies [8]. For example, several GLP1RA trials have included new-onset macroalbuminuria for defining composite renal outcomes [9, 10]. Conversely, SGLT2i trials have adopted different criteria for the albuminuria component. For example, development of albuminuria, regression from albuminuria to normal, or progression to overt proteinuria were used in respective studies [3, 11, 12]. Moreover, the criteria for diminished renal function have varied, with some trials depending on a percent decrease in estimated glomerular filtration rate (eGFR) [13] and others using a doubling of serum creatinine [14].
Few studies have specifically assessed the long-term differential impacts of SGLT2i and GLP1RA therapies on renal outcomes and related metabolic markers [15]. Our recent observations have revealed a potential association between renal function parameters, such as eGFR and albuminuria, and the variability in the effectiveness of these agents in averting cardiovascular events, thereby highlighting the crucial importance of renal management [5]. Definitive conclusions regarding renal outcomes have not been reached due to the limited number of studies designating them as primary endpoints. Against this background, the present study aimed to employ a real-world data approach to comprehensively compare the renal and metabolic consequences associated with SGLT2i and GLP1RA therapy in patients with type 2 diabetes.
Methods
Study design and population
We used a propensity-score matched cohort design that was approved by an independent Ethics Committee/Institutional Review Board (B-2103–675-103), with a waiver for patient-informed consent due to its retrospective nature. We included data from adult patients with type 2 diabetes who attended the diabetes clinic at Seoul National University Bundang Hospital, South Korea, between January 2009 and August 2023 and who satisfied the following inclusion criteria: (1) aged 19 years or older; (2) receiving a new prescription of SGLT2i or GLP1RA for a minimum of 90 days; and (3) with a documented baseline albuminuria status. Patients with medication adherence less than 70% to SGLT2i or GLP1RA therapy, or those who used both agents concomitantly, were excluded.
Over an up-to 4-year observation period, commencing from the date of prescription, evaluations were conducted at predefined intervals of 180, 365, 540, 730, 1,095, and 1,460 days. In addition, an exhaustive data collection was performed throughout this period to assess trends in clinical parameters. This investigation conformed to the STROBE statement for cohort studies.
Outcomes
The primary endpoint of this study comprised composite renal outcomes, which included a sustained reduction in eGFR of ≥ 40%, end-stage renal disease (ESRD), newly confirmed macroalbuminuria (evaluated by urinary albumin-to-creatinine ratio [ACR] assessment), and kidney-related mortality. Secondary outcomes comprised the risk assessment for each component of the primary outcome and the regression of albuminuria. Additionally, fractional excretion of glucose (FEglc), sodium (FENa), and potassium (FEK) were measured. Glycaemic control parameters (glycated haemoglobin [HbA1c], insulin, and glucagon), liver enzyme activities, and lipid profiles were also checked. Anthropometric parameters including body weight and blood pressure were monitored systematically. The specific definitions of these outcomes are detailed in Additional file 1: Table S1.
Data collection and measurements
Clinical data, including outpatient care details, admission records, laboratory values, anthropometric assessments, and prescription information, were extracted from the clinical database. Urinary albumin concentration was quantified using turbidimetry (502X; A&T, Tokyo, Japan) and urinary creatinine was evaluated using the Jaffe method (Hitachi 7170; Hitachi, Tokyo, Japan). Albuminuria was identified using the ratio of urinary ACR (mg/g). The eGFR was calculated using the Modification of Diet in Renal Disease (MDRD) equation, which was applied consistently throughout the study.
Composite urinary analyses in the study hospital routinely measure urinary glucose excretion and electrolytes, which enabled us to calculate the urinary fractional excretion of glucose, sodium, and potassium: FE-solute = (urine solute × serum creatinine)/(serum solute × urine creatinine). We calculated medication compliance as the medication possession ratio, defined by the number of days with medication prescribed within the visit time interval.
Anthropometric measurements, such as height and body weight, were collected using standardized protocols. Systolic (SBP) and diastolic blood pressure (DBP) were measured with the participant in a seated position using an electronic blood pressure meter (UA-1020 device; A&D, Tokyo, Japan).
Body composition, including muscle mass and fat mass, was assessed using bioelectrical impedance analysis (InBody720; InBody Co., Seoul, South Korea). Plasma glucose concentrations were ascertained using the glucose oxidase method (747 Clinical Chemistry Analyzer; Hitachi). To estimate pancreatic β-cell function and insulin resistance, the homeostasis model assessment of insulin resistance (HOMA-IR) and β-cell function (HOMA-β) indices were calculated [16]. Plasma HbA1c was measured using a Variant II Turbo HPLC Hemoglobin Testing System (Bio-Rad, Hercules, CA, USA). Total cholesterol, triglycerides, high-density lipoprotein (HDL)-cholesterol, and low-density lipoprotein (LDL)-cholesterol levels were measured using a 747 Clinical Chemistry Analyzer (Hitachi). Any values that were manifestly incorrect, presented in ambiguous ranges, or deemed physically implausible due to typographical errors, were omitted, as described previously [17].
Safety parameters
Safety assessments involved the monitoring of common adverse events, comprising gastrointestinal discomfort, urinary and genital infections, ketoacidosis, pancreatitis, malignancies, and hypoglycaemia. Hypoglycaemic incidents were recorded based on patient-reported symptoms and plasma glucose levels (< 70 mg/dL). Severe hypoglycaemic events are defined as plasma glucose levels (< 54 mg/dL) or hypoglycaemia requiring third-party assistance. Serious adverse events included death, hospitalization for any reason, and life-threatening events.
Statistical analysis
All data analyses were conducted using R software (version 4.1.0; The R Foundation for Statistical Computing, Vienna, Austria). Instances where the prescription or the follow-up observation terminated were treated as censored data. Continuous variables were expressed as mean ± standard deviation (SD), whereas categorical variables were delineated as counts and proportions of subjects. To account for differences in baseline characteristics, propensity-score matching was implemented at a 1:3 ratio through the ‘MatchIt’ package, adding a calliper set at 0.2 ratio, incorporating variables such as age, sex, duration of diabetes, body mass index (BMI), SBP, presence of hypertension, presence of dyslipidaemia, and background antidiabetic medications. Standardized mean difference (SMD) with ≤ 0.1 was considered well balanced after matching. Comparing characteristics after matching showed a balance between the groups, indicating a minimal impact on cohort selection.
Operating under the assumption that data were missing completely at random by Little’s test and were < 50% at each visit, a mixed model for repeated measures was used to evaluate continuous variables monitored longitudinally within the treatment groups, which comprised terms for treatment, visit, and the interaction between treatment and visit, with the baseline measurement included as a covariate. The incidence (per 1,000 person-years) for each outcome event in both the SGLT2i and GLP1RA groups was calculated.
Survival was analysed using a Kaplan–Meier method to estimate cumulative event-free survival rates over time, and the Cox proportional hazards regression model was applied to contrast hazard ratios between the treatment groups. Subgroup analyses were conducted stratified by sex (men vs women), age (< 65 years vs ≥ 65 years), eGFR (≥ 60 mL/min/1.72 m2 vs < 60 mL/min/1.72 m2), and albuminuria status (normoalbuminuria vs micro- and macroalbuminuria). Given that the initiation timelines for GLP1RAs and SGLT2is may differ, we further refined our matching criteria to include the year of medication commencement. This approach is aimed at mitigating any potential biases by aligning the follow-up durations and accounting for variations in comorbid illness patterns over time between the two medications.
Sensitivity analyses were undertaken for individuals who either continued or did not start the prescription of renin–angiotensin system (RAS) blockers, including angiotensin-converting enzyme inhibitors (ACEis) or angiotensin II receptor blockers (ARBs). This approach was designed to address potential bias in the Cox regression model, aiming to mitigate the confounding influence of RAS blocker usage, a factor intrinsically linked to renal outcomes. Furthermore, considering the impact of baseline renal function on the primary outcome, we categorized proteinuria and eGFR according to the Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group [18] and used the 'cmprsk' package for a multivariable competing risk regression with the Fine and Gray model to assess subdistribution hazard ratios (sHR) [19].
For parameters exhibiting substantial variability, such as ketone and glucagon levels, missing values were imputed using the last observation carried forward method, and log-transformed values were used for comparative analyses. The threshold for statistical significance was set at a two-sided p < 0.05, in accordance with conventional criteria for hypothesis testing.
Results
Patient characteristics
Before propensity-score matching, 11,728 patients with type 2 diabetes met the eligibility criteria. After 1:3 propensity-score matching, the analysis included data from 2,112 patients: 528 with GLP1RA therapy and 1,584 with SGLT2i therapy (Additional file 1: Fig. S1). Baseline characteristics were well balanced (Table 1). The mean age of patients in this cohort was 55.9 ± 13.5 years, and the mean BMI was 27.9 ± 4.3 kg/m2. Most patients (86.2%) had an eGFR ≥ 60 mL/min/1.73 m2, and over half (59.3%) were concurrently prescribed ACEis or ARBs. The most used agents were dapagliflozin (50.7%) or empagliflozin (45.7%) in the SGLT2i group and dulaglutide (65.5%) or liraglutide (26.1%) in the GLP1RA group (Additional file 1: Table S2).
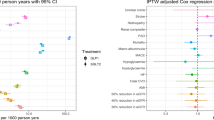
Primary endpoint: renal composite outcomes
Table 2 and Fig. 1 detail renal outcomes at a median follow-up of 731 days (interquartile range [IQR], 327–1,408). The primary composite renal outcomes occurred in 18 patients (3.4%) administered a GLP1RA and 42 patients (2.7%) administered an SGLT2i, corresponding to incidence rates of 16.9 and 9.4 per 1,000 person-years, respectively (Table 2), suggesting a trend toward risk reduction for composite renal outcomes with SGLT2i compared with GLP1RA (Fig. 1a). SGLT2i therapy significantly reduced the risk of a sustained eGFR decrease compared with GLP1RA (≥ 40% reduction in eGFR: HR, 0.46; 95% confidence interval [CI], 0.12–0.92) (Fig. 1b) and increased the likelihood of albuminuria regression (HR, 1.56; 95% CI, 1.03–2.38) (Fig. 1f). Subgroup analyses did not reveal any significant interactions stratified by age, sex, baseline eGFR, or albuminuria status (Additional file 1: Table S3).
Cumulative incidence of renal outcomes. a Composite renal outcomes, (b) sustained reduction in eGFR ³40%, (c) end-stage renal disease, (d) new-onset macroalbuminuria, (e) albuminuria progression, and (f) albuminuria regression. GLP1RA, glucagon-like peptide-1 receptor agonists; SGLT2i, sodium–glucose co-transporter-2 inhibitors. p values were calculated for the log-rank test conducted between the two groups
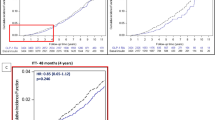
Changes in renal or metabolic measurements
Figure 2 and Additional file 1: Figs S2–S5 illustrate clinical parameters related to renal function, glycaemic metabolism, lipids, and anthropometry. Throughout the observation period, SGLT2i therapy consistently reduced urinary ACR and preserved eGFR levels (Fig. 2a and b). In contrast, eGFR levels decreased gradually in people with GLP1RA therapy, displaying a trend toward a group difference (p = 0.097).
Changes in clinical parameters related to renal function and glycaemic control: (a) albuminuria, (b) eGFR, (c) HbA1c, (d) FEglucose, (e) fasting glucose, (f) postprandial 2-h glucose, (g) HOMA-IR, and (h) HOMA-β. ACR, albumin-to-creatinine ratio; FE, fractional excretion. aSignificant change from baseline with GLP1RAs. bSignificant change from baseline with SGLT2is. *Significant difference between the two groups of changes from the baseline value by paired comparison. p values indicate the difference between the two groups by mixed-effect models for repeated measures (MMRM) by defined time point
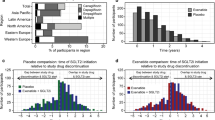
There were no significant differences in HbA1c and glucose levels between groups (Fig. 2c, e, and f). However, a greater proportion of patients reached the target HbA1c level (< 7%) with GLP1RA therapy than with SGLT2i therapy (40.6% vs 31.4%; p < 0.001). In the present study, urinary glucose excretions and electrolytes were measured in 60% of patients. SGLT2i therapy was associated with an increase to 33.6% in FEglc at 180 days, which was maintained within a range from 30.0% to 35.1% throughout the observation period (Fig. 2d). This increase was not observed with GLP1RA therapy. FENa increased with long-term GLP1RA therapy (Additional file 1: Fig. S2a). Overall, SGLT2i therapy decreased HOMA-IR, whereas GLP1RA therapy increased HOMA-β (Fig. 2g and h).
Regarding lipid profiles, GLP1RA therapy was more effective in reducing total cholesterol and LDL-cholesterol (Additional file 1: Fig. S3a and S3d), while SGLT2i therapy was better for controlling blood pressure and body weight (Additional file 1: Fig. S3e–S3h). Ketone levels increased with SGLT2i therapy, although the difference between the two groups was not statistically significant (Additional file 1: Fig. S4). SGLT2i therapy resulted in an increase in muscle percentage and a decrease in body fat percentage; however, no significant group differences were observed (Additional file 1: Fig. S5).
We examined the association between use of RAS blockers on albuminuria and renal function and the outcomes of the therapies (RAS blocker users: n = 1,129; RAS blocker nonusers: n = 788). Consistent use of RAS blockers tended to be associated with more favourable composite renal outcomes for patients administered a SGLT2i than for patients administered a GLP1RA (HR, 0.52; 95% CI, 0.26–1.00).
When matched further with the year of medication initiation (Additional file 1: Table S4), the results were similar to those from the original cohort and favoured SGLT2i over GLP1RA in terms of renal function deterioration and development of ESRD (significant) and albuminuria progression (trend).
Furthermore, a more advanced baseline kidney stage was correlated with an increased risk of primary composite renal outcomes, as shown in Additional file 1: Table S5. SGLT2is were found to significantly lower the sHR of composite renal outcomes compared to GLP1RAs in analyses utilizing multivariable risk regression models that included albuminuria and eGFR as variables.
Safety issues
A total of 743 patients (35.3%) reported one or more adverse events (GLP1RA group, n = 203 [38.4%]; SGLT2i group, n = 543 [34.3%]) (Additional file 1: Table S6). Overall, the incidence of adverse events was comparable between groups. The GLP1RA group experienced nausea and vomiting more frequently than the SGLT2i group (6.4% vs 0.6%; p < 0.001). The SGLT2i group tended to experience genitourinary infection more frequently than the GLP1RA group, but the difference was not significant (4.7% vs 3.8%; p = 0.394). For cardiovascular events, the HR was calculated (Additional file 1: Table S7) and was not significantly different between the two groups (HR, 1.84; 95% CI, 0.41–8.23). Serious adverse events were not significantly different between the two groups.
Discussion
In the present study of data from patients with type 2 diabetes, which employed 1:3 propensity-score matching (528 and 1,584 patients with GLP1RA and SGLT2i therapies, respectively), the incidence of primary composite renal outcomes for a ≤ 4-year follow-up were 16.9 and 9.4 per 1,000 person-years, respectively, with no significant difference found between the two agents. SGLT2i therapy significantly reduced the risk of a sustained eGFR decrease in individual components compared with GLP1RA, in either a ≥ 40% or ≥ 50% decrease in eGFR. Patients administered with SGLT2i also displayed a significantly increased likelihood of albuminuria regression than those administered with GLP1RA.
Notably, previous studies have provided mixed evidence concerning the relative effectiveness of SGLT2i and GLP1RA therapies on composite renal outcomes. A network analysis of 15 cardiovascular outcome trials (CVOTs) reported a 22% risk reduction in composite renal outcomes with SGLT2i compared to GLP1RA (relative risk [RR], 0.78; 95% CI, 0.65–0.93) [7]. In our recent network meta-analysis of 43 trials that compared nine types of glucose-lowering therapies [3], GLP1RA and SGLT2i therapies were associated with lower risks for composite renal outcome than placebo (22% and 34%, respectively), but no significant difference between GLP1RA and SGLT2i therapies was noted.
In a recent analysis using the Hong Kong Hospital Authority database involving 5,102 patients, SGLT2i users had a lower risk of composite renal outcomes than GLP1RA users (RR, 0.77; 95% CI, 0.62–0.96), mainly driven by a reduced development of ESRD (HR, 0.53; 95% CI, 0.33–0.86, p = 0.01) [20]. The beneficial impact of the use of SGLT2is in mitigating renal function decline observed in our study was not mirrored in the Hong Kong database study [20].
Of note, there are some differences between the two studies in their baseline characteristics. At baseline, the proportion of patients with normal eGFR levels or normoalbuminuria were higher in our cohort than in the Hong Kong study (86.9% vs 71.2% and 57.5% vs 44.1%, respectively). Additionally, we adopted a ≥ 40% eGFR reduction as the standard criterion for renal impairment, but the Hong Kong study adopted a ≥ 50% eGFR reduction.
In the most recent findings, the FLOW trial reported a 24% reduction in the progression of kidney disease and mortality associated with the administration of semaglutide 1.0 mg [21, 22]. It is crucial to acknowledge, however, that this trial was placebo-controlled and employed a GLP1RA, rather than an SGLT2i, in participants with type 2 diabetes and chronic kidney disease. These results underscore the necessity for direct comparative studies to more accurately determine the relative efficacy and safety of these treatments.
The underlying mechanisms by which SGLT2is and GLP1RAs manage glucose demonstrate clear distinctions. SGLT2i treatment improves glucose regulation primarily by augmenting glycosuria and attenuating insulin resistance [23]. By contrast, GLP1RAs mainly act on pancreatic β-cell function, systemic inflammation, and satiety neurons in the hypothalamus in the central nervous system [24]. While overall glucose regulation did not show significant disparities between the two therapeutic modalities, a more substantial fraction of patients treated with GLP1RA reached HbA1c values < 7% in the present study. This finding could be attributed to the fundamental pharmacological features of GLP1RA to enhance β-cell function and alleviate insulin resistance.
In the present study, GLP1RA therapy decreased total and LDL-cholesterol levels. It was reported that GLP1RA therapy is able to modulate lipogenesis and β-oxidation in liver [25] and to improve insulin sensitivity by promoting the degradation of apolipoprotein-B through phosphatidylinositol 3-kinase [26]. By contrast, it is noted that the reported impact of SGLT2is on cholesterol levels has not been consistent. A meta-analysis of 48 RCTs including 24,782 participants revealed increases in LDL- and HDL-cholesterol levels with SGLT2i therapy by 3.89 mg/dL (95% CI, 0.07–0.12) and by 2.33 mg/dL (95% CI, 0.05–0.08), respectively, compared to the control group [27]. Of note, the increase in HDL-cholesterol were more pronounced in Asians [27]. In the present study, SGLT2i therapy led to an increase in HDL-cholesterol, but a decrease in LDL-cholesterol. A recent meta-analysis reported that SGLT2i therapy increased LDL-cholesterol, but this effect was not observed with 10 mg of empagliflozin or dapagliflozin [28]. More than 95% of the cases in our study used these drugs at the same doses. Considering the lack of significant changes in lipid-lowering therapy in our study, the substantial improvement in insulin resistance and significant reduction in body weight by SGLT2i treatment might be attributable to LDL-cholesterol reduction [29].
In this study, the likelihood of achieving the target blood pressure was two-fold higher with SGLT2i therapy than with GLP1RA therapy. This result is in line with a previous study of Japanese subjects with type 2 diabetes [30].
We found that body weight was reduced more markedly with SGLT2i therapy than with GLP1RA therapy. In the large-scale RCTs with the medications used in our cohort, there was slightly greater weight loss with SGLT2i than GLP1RA (–2 kg for SGLT2i vs –1.5 kg for GLP1RA) (Additional file 1: Table S8) [9, 31,32,33,34,35,36]. Japanese studies showed similar findings [30, 37]. Notably, the GLP1RAs included in the current analysis were used at doses for diabetes management. Whereas GLP1RAs at higher doses were very effective for obesity management [38, 39]. Favourable effects of SGLT2i for lowering glucose [40] and heart failure and cardiovascular death were found more prominent in those with South Asian and East/Southeast Asian ancestry (defined as Asians) than in those with Western European ancestry in a meta-analysis [41]. The relatively lower body mass and high salt and high carbohydrate diet of Asian populations may be associated with these results [42].
In the present study, SGLT2i therapy increased ketone levels throughout the observation period, whereas GLP1RA therapy did not, which is consistent with previous studies [43, 44]. Ketone bodies are an ancillary fuel source substituting for glucose in the heart, and exhibit antioxidative and anti-inflammatory effects [45]. Ketone bodies require less oxygen to produce the same amount of energy than glucose, potentially improving organ function under conditions of stress [45]. An alteration of energy source by SGLT2i therapy can be linked to several advantages, including enhanced mitochondrial biogenesis and function, effective energy utilization, and increased erythropoiesis, all contributing to renal benefits [46].
In this study, there were no significant differences in overall adverse events between the two treatment groups. As anticipated, GLP1RA therapy was associated with gastrointestinal disturbances, including nausea and vomiting. SGLT2i therapy is typically linked with genital tract infections, but this was not observed in our present analysis, which might be due to the strict education regarding subjects maintaining hydration and good hygiene. In a recent large study (EMPA-KIDNEY), the use of empagliflozin did not increase the incidence of serious urinary tract infections, acute kidney injuries, symptomatic dehydration, or bone fractures [12].
Intriguingly, in the sensitivity analysis, the renoprotective effects of SGLT2i therapy were more pronounced with the simultaneous use of a RAS blocker. The renovascular benefits of RAS blockers for individuals with renal disease are well documented [47]. The combined use of a SGLT2i and RAS blocker curtails oxidative stress, as demonstrated by a decrease in the 8-isoprostane marker [48]. The recuperated tubuloglomerular feedback mechanisms are also associated with a decrease in the risk of cardiorenal complications [48].
Strengths and limitations
The present study has several distinctive features. First, 20.7% of the study participants had a prevalence of pre-existing CVDs, which was lower than previous CVOTs ranging from 31.5–100% [5]. This result enhanced the possible insights. Second, unique to the present study were the comparisons between the two drug classes for specific in-hospital tests, such as FEglc, FENa, FEK, ketone levels, and body composition, which are not available in other large database studies [20]. Third, the observation period was relatively prolonged, with a median of 731 days (IQR, 327–1,408 days). However, there are several caveats for our analysis.
The first caveat is that the findings might not apply to other populations in the same way, as our data were derived from a cohort of East Asian ancestry. Second, the patients whose data were included in this study had a higher prevalence of diabetic kidney disease than adults with diabetes overall from Korean nationwide data (i.e. 36.6% vs 27.6%) [49]. However, the characteristics of the patients whose data were included in our study are similar to those of most patients with diabetes attending referral hospitals [50]. When we compared unmatched SGLT2i subjects with matched SGLT2i subjects, most characteristics were similar, except for slightly higher numbers of comorbidities and a lower BMI in the unmatched group. This difference means that SGLT2is were more prescribed for patients with more complications, particularly heart failure, whereas GLP1RAs were more prescribed for those with obesity. Third, we primarily investigated the class effects of SGLT2is and GLP1RAs, rather than the individual agents within the class.
Conclusions
In summary, SGLT2i therapy may offer more distinctive benefits in renal protection, particularly in the reduction in albuminuria and mitigation in eGFR decline, compared with GLP1RAs at doses prescribed for diabetes management. In contrast, GLP1RAs may emerge as a favourable choice for glucose regulation and dyslipidaemia management. Future head-to-head studies comparing the two agents or including recent potent GLP1RAs and GLP1/GIP co-agonists, to expand on the present observations, and thereby enhance tailored therapeutic approaches for managing type 2 diabetes are warranted.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACEi:
-
Angiotensin-converting enzyme inhibitor
- ACR:
-
Albumin-to-creatinine ratio
- ARB:
-
Angiotensin II receptor blocker
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- CVOT:
-
Cardiovascular outcome trial
- DBP:
-
Diastolic blood pressure
- eGFR:
-
Estimated glomerular filtration ratio
- ESRD:
-
End-stage renal disease
- FEglc:
-
Fraction excretion of glucose
- FEK:
-
Fraction excretion of potassium
- FENa:
-
Fraction excretion of sodium
- GLP1RA:
-
Glucagon-like peptide-1 receptor agonists
- HbA1c:
-
Glycated haemoglobin
- HDL-c:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostatic model assessment for insulin resistance
- HOMA-β:
-
Homeostatic model assessment for β-cell function
- HR:
-
Hazard ratio
- LDL-c:
-
Low-density lipoprotein cholesterol
- PP2:
-
Postprandial 2-h
- RAS:
-
Renin–angiotensin system
- RCT:
-
Randomized controlled trial
- SBP:
-
Systolic blood pressure
- SGLT2i:
-
Sodium–glucose co-transporter-2 inhibitors
- sHR:
-
Subdistribution hazard ratios
- SMD:
-
Standardized mean difference
- uACR:
-
Urinary albumin-creatinine-ratio
References
Ahmad E, Lim S, Lamptey R, Webb DR, Davies MJ. Type 2 diabetes. Lancet. 2022;400(10365):1803–20.
Brown E, Heerspink HJL, Cuthbertson DJ, Wilding JPH. SGLT2 inhibitors and GLP-1 receptor agonists: established and emerging indications. Lancet. 2021;398(10296):262–76.
Sohn M, Frias JP, Lim S. Cardiovascular efficacy and safety of antidiabetic agents: a network meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2023;25:3560–77.
Li S, Wang J, Zhang B, Li X, Liu Y. Diabetes mellitus and cause-specific mortality: a population-based study. Diabetes Metab J. 2019;43(3):319–41.
Sohn M, Dietrich JW, Nauck MA, Lim S. Characteristics predicting the efficacy of SGLT-2 inhibitors versus GLP-1 receptor agonists on major adverse cardiovascular events in type 2 diabetes mellitus: a meta-analysis study. Cardiovasc Diabetol. 2023;22(1):153.
Lim S, Eckel RH, Koh KK. Clinical implications of current cardiovascular outcome trials with sodium glucose cotransporter-2 (SGLT2) inhibitors. Atherosclerosis. 2018;272:33–40.
Lin DS, Lee JK, Hung CS, Chen WJ. The efficacy and safety of novel classes of glucose-lowering drugs for cardiovascular outcomes: a network meta-analysis of randomised clinical trials. Diabetologia. 2021;64(12):2676–86.
Patel RB, Ter Maaten JM, Ferreira JP, McCausland FR, Shah SJ, Rossignol P, Solomon SD, Vaduganathan M, Packer M, Thompson A, et al. Challenges of cardio-kidney composite outcomes in large-scale clinical trials. Circulation. 2021;143(9):949–58.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, Nissen SE, Pocock S, Poulter NR, Ravn LS, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, Lingvay I, Rosenstock J, Seufert J, Warren ML, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44.
Heerspink HJL, Stefansson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, Mann JFE, McMurray JJV, Lindberg M, Rossing P, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46.
The E-KCG, Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, Emberson JR, Preiss D, Judge P, Mayne KJ, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023;388(2):117–27.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Mann JFE, Orsted DD, Brown-Frandsen K, Marso SP, Poulter NR, Rasmussen S, Tornoe K, Zinman B, Buse JB, Committee LS, et al. Liraglutide and renal outcomes in type 2 diabetes. N Engl J Med. 2017;377(9):839–48.
Hiramatsu T, Ito H, Okumura S, Asano Y, Iguchi D, Furuta S. Impact of glucagon like peptide-1 receptor agonist and sodium glucose cotransporter 2 inhibitors on type 2 diabetes patients with renal impairment. Diab Vasc Dis Res. 2020;17(6):1479164120971220.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Sohn M, Koo BK, Yoon HI, Song KH, Kim ES, Kim HB, Lim S. Impact of COVID-19 and associated preventive measures on cardiometabolic risk factors in South Korea. J Obes Metab Syndr. 2021;30(3):248–60.
Disease K. Improving global outcomes CKDWG: KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105(4S):S117–314.
Scrucca L, Santucci A, Aversa F. Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transplant. 2010;45(9):1388–95.
Lui DTW, Au ICH, Tang EHM, Cheung CL, Lee CH, Woo YC, Wu T, Tan KCB, Wong CKH. Kidney outcomes associated with sodium-glucose cotransporter 2 inhibitors versus glucagon-like peptide 1 receptor agonists: A real-world population-based analysis. EClinicalMedicine. 2022;50:101510.
Rossing P, Baeres FMM, Bakris G, Bosch-Traberg H, Gislum M, Gough SCL, Idorn T, Lawson J, Mahaffey KW, Mann JFE, et al. The rationale, design and baseline data of FLOW, a kidney outcomes trial with once-weekly semaglutide in people with type 2 diabetes and chronic kidney disease. Nephrol Dial Transplant. 2023;38(9):2041–51.
Gragnano F, De Sio V, Calabro P. FLOW trial stopped early due to evidence of renal protection with semaglutide. Eur Heart J Cardiovasc Pharmacother. 2024;10(1):7–9.
Cowie MR, Fisher M. SGLT2 inhibitors: mechanisms of cardiovascular benefit beyond glycaemic control. Nat Rev Cardiol. 2020;17(12):761–72.
Drucker DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 2018;27(4):740–56.
Patel VJ, Joharapurkar AA, Shah GB, Jain MR. Effect of GLP-1 based therapies on diabetic dyslipidemia. Curr Diabetes Rev. 2014;10(4):238–50.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuniga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
Sanchez-Garcia A, Simental-Mendia M, Millan-Alanis JM, Simental-Mendia LE. Effect of sodium-glucose co-transporter 2 inhibitors on lipid profile: A systematic review and meta-analysis of 48 randomized controlled trials. Pharmacol Res. 2020;160:105068.
Bechmann LE, Emanuelsson F, Nordestgaard BG, Benn M. SGLT2-inhibition increases total, LDL, and HDL cholesterol and lowers triglycerides: Meta-analyses of 60 randomized trials, overall and by dose, ethnicity, and drug type. Atherosclerosis. 2023;394:117236.
Gatti A, Maranghi M, Bacci S, Carallo C, Gnasso A, Mandosi E, Fallarino M, Morano S, Trischitta V, Filetti S. Poor glycemic control is an independent risk factor for low HDL cholesterol in patients with type 2 diabetes. Diabetes Care. 2009;32(8):1550–2.
Kobayashi K, Toyoda M, Hatori N, Sakai H, Furuki T, Sato K, Terauchi Y, Tamura K, Kanamori A. Comparison of the blood pressure management between sodium-glucose cotransporter 2 inhibitors and glucagon-like peptide 1 receptor agonists. Sci Rep. 2022;12(1):16106.
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, Probstfield J, Riesmeyer JS, Riddle MC, Ryden L, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–30.
Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, Buse JB, Chan JC, Choi J, Gustavson SM, Iqbal N, et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(13):1228–39.
Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Kober LV, Lawson FC, Ping L, Wei X, Lewis EF, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247–57.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, Charbonnel B, Frederich R, Gallo S, Cosentino F, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383(15):1425–35.
Kobayashi K, Toyoda M, Hatori N, Sakai H, Furuki T, Chin K, Kimura M, Saito N, Kanaoka T, Aoyama T, et al. Comparison of renal outcomes between sodium glucose co-transporter 2 inhibitors and glucagon-like peptide 1 receptor agonists. Diabetes Res Clin Pract. 2022;185:109231.
Kelly AS, Auerbach P, Barrientos-Perez M, Gies I, Hale PM, Marcus C, Mastrandrea LD, Prabhu N, Arslanian S, Investigators NNT. A Randomized, controlled trial of liraglutide for adolescents with obesity. N Engl J Med. 2020;382(22):2117–28.
Kadowaki T, Isendahl J, Khalid U, Lee SY, Nishida T, Ogawa W, Tobe K, Yamauchi T, Lim S. investigators S: Semaglutide once a week in adults with overweight or obesity, with or without type 2 diabetes in an east Asian population (STEP 6): a randomised, double-blind, double-dummy, placebo-controlled, phase 3a trial. Lancet Diabetes Endocrinol. 2022;10(3):193–206.
Gan S, Dawed AY, Donnelly LA, Nair ATN, Palmer CNA, Mohan V, Pearson ER. Efficacy of modern diabetes treatments DPP-4i, SGLT-2i, and GLP-1RA in white and asian patients with diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2020;43(8):1948–57.
Lee MMY, Ghouri N, McGuire DK, Rutter MK, Sattar N. Meta-analyses of results from randomized outcome trials comparing cardiovascular effects of SGLT2is and GLP-1RAs in Asian versus white patients with and without type 2 diabetes. Diabetes Care. 2021;44(5):1236–41.
Li X, Zhang Q, Zhou X, Guo S, Jiang S, Zhang Y, Zhang R, Dong J, Liao L. The different hypoglycemic effects between East Asian and non-Asian type 2 diabetes patients when treated with SGLT-2 inhibitors as an add-on treatment for metformin: a systematic review and meta-analysis of randomized controlled trials. Aging (Albany NY). 2021;13(9):12748–65.
Shin Y, Moon JH, Chin HJ, Ferrannini E, Lim S. Glycemic efficacy and metabolic consequences of an empagliflozin add-on versus conventional dose-increasing strategy in patients with type 2 diabetes inadequately controlled by Metformin and Sulfonylurea. Endocrinol Metab (Seoul). 2020;35(2):329–38.
Ferrannini E, Muscelli E, Frascerra S, Baldi S, Mari A, Heise T, Broedl UC, Woerle HJ. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124(2):499–508.
Lupsa BC, Kibbey RG, Inzucchi SE. Ketones: the double-edged sword of SGLT2 inhibitors? Diabetologia. 2023;66(1):23–32.
Ekanayake P, Mudaliar S. A novel hypothesis linking low-grade ketonaemia to cardio-renal benefits with sodium-glucose cotransporter-2 inhibitors. Diabetes Obes Metab. 2022;24(1):3–11.
Disease K. Improving global outcomes diabetes work G: KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2022;102(5S):S1–127.
Lytvyn Y, Kimura K, Peter N, Lai V, Tse J, Cham L, Perkins BA, Soleymanlou N, Cherney DZI. Renal and vascular effects of combined SGLT2 and angiotensin-converting enzyme inhibition. Circulation. 2022;146(6):450–62.
Diabetes & Complications in Korea. https://www.diabetes.or.kr/bbs/?code=fact_sheet&mode=view&number=1792&page=1&code=fact_sheet.
Lim S, Chung SH, Kim JH, Kim YH, Kim EJ, Joo HJ. Effects of metabolic parameters’ variability on cardiovascular outcomes in diabetic patients. Cardiovasc Diabetol. 2023;22(1):114.
Acknowledgements
Not applicable.
Funding
This study was supported by Daewoong Pharmaceutical company. The funder had no role in the research. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Concept and design: M.S. and S.L. Acquisition, analysis, or interpretation of data: M.S. and S.N. Drafting of the manuscript: M.S. and S.L. Critical revision of the manuscript for important intellectual content: M.S., M.A.N., and S.L. Statistical analysis: M.S. and S.L. Administrative, technical, or material support: M.S. and S.N. Supervision: S.L. S.L. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by an independent Ethics Committee/Institutional Review Board of the Seoul National University Bundang Hospital (B-2103–675-103). The requirement for informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12916_2024_3483_MOESM1_ESM.pdf
Additional file 1: Table S1. Definition of outcomes and diseases. Table S2. Types of SGLT2i or GLP1RA used in each cohort. Table S3. Incidence rate of composite renal outcome and its comparison between GLP1RA and SGLT2i users according to baseline characteristics. Table S4. Incidence rate of renal outcomes and comparison between GLP1RA and SGLT2i users in patients further matched with the year of medication start. Table S5. Multivariable competing risk regression estimates of subdistribution hazard ratio for the composite renal outcome with Fine and Gray Model. Table S6. Adverse events. Table S7. Incidence rate of cardiovascular outcomes and comparison between GLP1RA and SGLT2i users. Table S8. Weight changes after GLP1 receptor agonists and SGLT2 inhibitors therapy in major randomized controlled studies. Fig. S1. Study design flow chart. Fig. S2. Changes in clinical parameters related to renal function: (a) FENa, and (b) FEK. Fig. S3. Changes in clinical parameters of metabolic parameters: (a) total cholesterol, (b) triglycerides, (c) HDL-cholesterol, (d) LDL-cholesterol, (e) SBP, (f) DBP, (g, i) body weight, and (h, j) BMI. Fig. S4. Changes in glucagon and ketone bodies: (a) glucagon, (b) total ketone, (c) β-hydroxybutyrate, and (d) acetoacetate. Fig. S5. Changes in body composition: (a) whole body muscle mass, (b) whole body fat mass, (c) muscle percentage, and (d) fat percentage.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sohn, M., Nam, S., Nauck, M.A. et al. Long-term comparison of renal and metabolic outcomes after sodium–glucose co-transporter 2 inhibitor or glucagon-like peptide-1 receptor agonist therapy in type 2 diabetes. BMC Med 22, 273 (2024). https://doi.org/10.1186/s12916-024-03483-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03483-z