Abstract
Background
Type 2 diabetes is associated with a variety of complications, including micro- and macrovascular complications, neurological manifestations and poor wound healing. Adhering to a Mediterranean Diet (MED) is generally considered an effective intervention in individuals at risk for type 2 diabetes mellitus (T2DM). However, little is known about its effect with respect to the different specific manifestations of T2DM. This prompted us to explore the effect of MED on the three most significant microvascular complications of T2DM: diabetic retinopathy (DR), diabetic kidney disease (DKD), and vascular diabetic neuropathies (DN).
Methods
We examined the association between the MED and the incidence of these microvascular complications in a prospective cohort of 33,441 participants with hyperglycemia free of microvascular complications at baseline, identified in the UK Biobank. For each individual, we calculated the Alternate Mediterranean Diet (AMED) score, which yields a semi-continuous measure of the extent to which an individual’s diet can be considered as MED. We used Cox proportional hazard models to analyze hazard ratios (HRs) and 95% confidence intervals (CIs), adjusting for demographics, lifestyle factors, medical histories and cardiovascular risk factors.
Results
Over a median of 12.3 years of follow-up, 3,392 cases of microvascular complications occurred, including 1,084 cases of diabetic retinopathy (DR), 2,184 cases of diabetic kidney disease (DKD), and 632 cases of diabetic neuropathies (DN), with some patients having 2 or 3 microvascular complications simultaneously. After adjusting for confounders, we observed that higher AMED scores offer protection against DKD among participants with hyperglycemia (comparing the highest AMED scores to the lowest yielded an HR of 0.79 [95% CIs: 0.67, 0.94]). Additionally, the protective effect of AMED against DKD was more evident in the hyperglycemic participants with T2DM (HR, 0.64; 95% CI: 0.50, 0.83). No such effect, however, was seen for DR or DN.
Conclusions
In this prospective cohort study, we have demonstrated that higher adherence to a MED is associated with a reduced risk of DKD among individuals with hyperglycemia. Our study emphasizes the necessity for continued research focusing on the benefits of the MED. Such efforts including the ongoing clinical trial will offer further insights into the role of MED in the clinical management of DKD.
Similar content being viewed by others
Background
Type 2 diabetes mellitus (T2DM) is associated with a variety of complications including micro- and macrovascular complications, neurological manifestations and poor wound healing. Diabetic retinopathy (DR), diabetic kidney disease (DKD), and vascular diabetic neuropathies (DN) are the three most significant microvascular complications and contribute significantly to morbidity and mortality worldwide [1]. Among these microvascular complications, DKD is highly prevalent and stands as the leading cause of kidney failure and end-stage kidney disease [2]. Notably, microvascular complications are also observed in patients with non-diabetic hyperglycemia, where glucose metabolism is abnormal but remains below the diagnostic criteria for T2DM [3].
Glucose-lowering agents such as metformin, sodium-glucose co-transporter-2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists, are generally recommended to ameliorate hyperglycemia [4]. However, these drugs may initially exacerbate DR and have been frequently associated with genitourinary infections, lactic acidosis and gastrointestinal side effects [5,6,7]. Antihypertensive drugs such as angiotensin-converting enzyme (ACE) inhibitors have been used for the treatment of DKD and DR; however, it is not well tolerated in some aged patients and may increase the risk of hyperkalemia when used in combination with angiotensin-receptor blockers (ARBs) [5]. In addition to drug treatment, diet therapy has been established as one of the most promising strategies for the management of hyperglycemia. The Mediterranean diet (MED) is a healthy dietary pattern that is characterized by increased consumption of legumes, vegetables, fruits, olive oil, whole-grain cereals and nuts. It also involves a moderate intake of fish and red wine, while limiting the consumption of red meat products and saturated fatty acids [8, 9]. In an umbrella review of meta-analyses, it has been revealed that higher adherence to the MED was associated with a 19% to 27% reduction in the risk of developing diabetes [10]. Furthermore, the MED was found to remarkably decrease the risk of T2DM in 8,291 Italian patients with a recent myocardial infarction [11] and 13,380 healthy Spanish university graduates [12].
Several systematic reviews have been conducted to investigate the impact of dietary interventions on microvascular complications. For instance, it has been shown that low-protein diets could significantly decrease urea levels in patients with DKD [13]. Additionally, adopting a vegetarian dietary pattern has been suggested to have a beneficial effect on DKD [14]. Furthermore, reducing salt intake among diabetic individuals has been found to slow the progression of DKD [15]. Previous systematic reviews have also revealed that higher adherence to the MED is associated with reduced risks of incident DR [16, 17]. However, it appears that adhering to the MED may have distinct effects on individual microvascular complications [18, 19]. Here, we sought to investigate the association between MED and the incidence of microvascular complications by performing a pooled analysis among participants with hyperglycemia. We have also investigated the effects of individual components of the MED on microvascular complications.
Methods
Study population
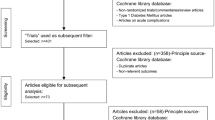
The UK Biobank cohort study recruited approximately 500,000 middle and aged adults across the UK from 2006 to 2010. We included hyperglycemic participants (defined as both fasting plasm glucose ≥ 5.56 mmol/L (100 mg/dL) and T2DM (self-reported or doctor-diagnosed, who were taking anti-hyperglycemic medications or insulin, or had glycosylated hemoglobin (HbA1c) levels > 48 mmol/mol)) and excluded those with a diagnosis of microvascular complications, incomplete dietary pattern information, or those who withdrew from the study (n=33441) based on previous criteria [20, 21]. The hyperglycemic participants include individuals with T2DM (n=7,969) and those without T2DM (n=25,472). The flowchart illustrating the inclusion of patients in our present study can be found in Fig. 1. The UK Biobank holds ethical approval from the North West Multi-Centre Research Ethics Committee and all participants provided informed consent. Our research protocol for this study has obtained approvals from the review committees associated with the UK Biobank.
Dietary assessment
The Alternate Mediterranean Diet (AMED) score was slightly modified from a traditional MED score [22,23,24]. Briefly, the AMED classifies various food items into nine distinct groups, which include vegetables, fruits, legumes, nuts, whole grains, fish, monounsaturated-to-saturated fat ratio (MUFA to SFA ratio), red and processed meats, and alcohol consumption. The total AMED score ranged from 0 to 9, with points assigned based on dietary habits. Points were assigned for higher consumption of fruits, vegetables, nuts, legumes, whole grains, fish, MUFA to SFA ratio, moderate consumption of alcohol, and lower consumption of red/processed meat. For each of these components, a score of 0 or 1 was assigned according to whether the participant was below or above the sex-specific median level of consumption in the study population and whether the component received points for lower or higher consumption (Additional file 1: Table S1) [25].
Assessment of main outcomes
Using the inclusion criteria provided in a recent study [21], we identified microvascular complications, including diabetic retinopathy (ICD-10: E113, E143, H280, H360), diabetic neuropathy (ICD-10: E114, E144, G590, G629, G632, G990), and diabetic kidney disease (ICD-10: E112, E142, N180, N181, N182, N183, N184, N185, N188, N189). To calculate the follow-up time, we measured the duration from the time of returning the baseline questionnaire to the occurrence of microvascular complications, the date of death, the date when a participant was lost to follow-up, or the end of the follow-up period, depending on which event occurred first.
Assessment of covariates
All participants completed touchscreen questionnaires, providing detailed information on socio-demographic factors such as age, gender, ethnicity, and the Index of Multiple Deprivation (IMD) [26]. They also reported their lifestyle habits, including dietary intake, physical activity levels, and alcohol consumption. Medical histories were documented as well. In addition to self-reported data, anthropometric measurements, such as height, body weight, and waist circumference (WC), were taken at the assessment center. Blood samples were collected from participants who had provided their consent at the time of recruitment. These samples were carefully stored at the UK Biobank under controlled conditions until they were later analyzed for various circulating biomarkers. In our analysis, several circulating biomarkers were considered to exhibit a positive correlation with an increased risk of DKD and thus treated as potential confounding factors. These biomarkers included glycated hemoglobin (HbA1c), insulin-like growth factor 1 (IGF), total cholesterol (TC), creatinine (CRT), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG).
Statistical analysis
The hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using Cox regression models. Two distinct models were constructed for this analysis. In model 1, we adjusted for age (continuous, years) and gender (men or women). In model 2, we additionally adjusted for ethnicity (white or other), index of multiple deprivations (a measure of socioeconomic status) [26], waist circumference (WC (continuous, centimeters)), alcohol consumption (categorized as never or special occasions only, one to three times a month, one to four times a week, daily or almost daily), physical activity (h/week), hypertension (yes or no), family history of diabetes (yes or no), family history of hypertension (yes or no), family history of heart disease (yes or no) and family history of stroke (yes or no), HbA1c (continuous, mmol/L), HDL-C (continuous, mmol/L), LDL-C (continuous, mmol/L), IGF (continuous, mmol/L), TG (continuous, mmol/L), CHOL (continuous, mmol/L), use of antihypertensive medication, use of cholesterol-lowering medication or use of diabetes medication (yes or no). Restricted cubic spline analysis was used to investigate the dose-response associations between the healthy lifestyle score and risks of microvascular complications. In the sensitivity analyses, we performed a lagged analysis of the exposure for 2 or 4 years, which could strengthen the temporality and allow a time window for the development of microvascular complications. The creatinine levels (continuous, µmol/L) and frequency of meat intake (times/week) were further adjusted for participants diagnosed with DKD. To investigate potential effect modifiers, we conducted stratified analyses according to age, gender, IMD, WC, alcohol intake, HbA1c, HDL-C, LDL-C, IGF, TG, TC, hypertension, physical activity, and use of antidiabetic medication, cholesterol-lowering medication and antihypertensive medication.
Results
The characteristics of study participants at baseline were listed according to their AMED scores. Among the 25,472 hyperglycemic participants without T2DM (48.9% men; mean age, 58.36 years), there were 2,495 (9.8%), 4,425 (17.4%), 5,176 (20.3%), 4,878 (19.2%), 4,194 (16.5%), 4,304 (16.9%) having 0-1, 2, 3, 4, 5, and 6-9 AMED score. Participants with higher AMED scores appear to be older, female and have lower levels of WC, IMD, and HbA1c. Additionally, they were less likely to use medications for hyperlipemia and hypertension (Table 1). Among the 7,969 hyperglycemic participants with T2DM (63.9% men; mean age, 60.28 years), there were 917 (11.5%), 1,573 (19.7%), 1,825 (22.9%), 1,464 (18.4%), 1,166 (14.6%), 1,024 (12.8%) having 0-1, 2, 3, 4, 5, and 6-9 AMED score. Participants with higher AMED scores also have lower levels of WC, IMD, and HbA1c (Table 2).
Among the total of 33,441 participants with hyperglycemia, there were 3,412 (10.2%), 5,998 (17.9%), 7,001 (20.9%), 6,342 (18.9%), 5,360 (16%), 5,328 (15.9%) having 0-1, 2, 3, 4, 5, and 6-9 AMED score (Table 3). During 404,918 person-years of follow-up (median 12.3 years), a total of 3,392 cases of composite microvascular complications were observed. These complications consisted of 1,084 cases of DR, 632 cases of DN, and 2,184 cases of DKD, with some patients being diagnosed with multiple microvascular complications simultaneously. After correcting for the confounding factors, the multivariable analyses showed that there were inverse associations between overall AMED scores and the risk of DKD; however, no such association was seen for DR and DN (Table 3 and Fig. 2). Moreover, comparing the highest AMED scores to the lowest yielded an HR of 0.79 [95% CIs: 0.67, 0.94] for DKD in participants with hyperglycemia (Table 3), indicating that higher AMED adherence protects DKD. Next, we conducted separate analyses for hyperglycemic participants with and without T2DM. The results revealed that adherence to AMED offers greater protection against DKD in the hyperglycemic participants with T2DM (HR, 0.64; 95% CI: 0.5, 0.83) (Table 4 and Fig. 3), whereas a reduced protective effect was observed in those without T2DM (Additional file 1: Table S2 and Additional file 1: Fig. S1).
Dose-response relationship of AMED with the risks of microvascular complications among total participants with hyperglycemia. The X-axis showed the numbers of AMED, and the y-axis showed the HRs of the composite microvascular complications (a), diabetic retinopathy (b), diabetic neuropathy (c), and diabetic kidney disease (d). Multivariable-adjusted models were adjusted for age (continuous, years) and gender (men or women), ethnicity (white or other), index of multiple deprivation (a measure of socioeconomic status), waist circumference (continuous, centimeters), alcohol consumption (categorized as never or special occasions only, one to three times a month, one to four times a week, daily or almost daily), physical activity (h/week), hypertension (yes or no), family history of diabetes (yes or no), family history of hypertension (yes or no), family history of heart disease(yes or no) and family history of stroke (yes or no), HbA1c (continuous, mmol/L), HDL-C (continuous, mmol/L), LDL-C (continuous, mmol/L), IGF (continuous, mmol/L), TG (continuous, mmol/L), CHOL (continuous, mmol/L), use of antihypertensive medication, cholesterol lowering medication and diabetes medication
Dose-response relationship of AMED with the risks of microvascular complications among hyperglycemic participants with T2DM. The X-axis showed the numbers of AMED, and the y-axis showed the HRs of the composite microvascular complications (a), diabetic retinopathy (b), diabetic neuropathy (c), and diabetic kidney disease (d). Multivariable-adjusted models were adjusted for age (continuous, years) and gender (men or women), ethnicity (white or other), index of multiple deprivation (a measure of socioeconomic status), waist circumference (continuous, centimeters), alcohol consumption (categorized as never or special occasions only, one to three times a month, one to four times a week, daily or almost daily), physical activity (h/week), hypertension (yes or no), family history of diabetes (yes or no), family history of hypertension (yes or no), family history of heart disease(yes or no) and family history of stroke (yes or no), HbA1c (continuous, mmol/L), HDL-C (continuous, mmol/L), LDL-C (continuous, mmol/L), IGF (continuous, mmol/L), TG (continuous, mmol/L), CHOL (continuous, mmol/L), use of antihypertensive medication, cholesterol lowering medication and diabetes medication
We further investigated the associations between individual components of AMED and the risks of DKD, DR or DN. For each incremental increase in the consumption of legumes, there was a potential 8% reduction in the risk of DKD among participants with hyperglycemia (HR, 0.92; 95% CI: 0.84, 1.01) (Fig. 4). This reduction was further strengthened among hyperglycemic participants with T2DM (HR, 0.89; 95% CI: 0.77, 0.99) (Fig. 5). In the case of the MUFA: SFA ratio, there was a 29% (HR, 0.71; 95% CI: 0.54-0.92) and a potential 23% (HR, 0.77; 95% CI: 0.58-1.03) decrease in the risk of DR among these two participant groups, respectively (Figs. 4 and 5). However, we did not observe a significant reduction in the risk associated with each incremental increase in the consumption of any AMED component about DN in both groups (Figs. 4 and 5). Interestingly, whole grains and fish appear to be the main components providing benefits in decreasing the risk of DKD among hyperglycemic participants without T2DM (Additional file 1: Fig. S2).
The association between adherence to individual components of AMED and the risks of microvascular complications among total participants with hyperglycemia. One point was given for intakes above the median for fruit and vegetables, legumes and nuts, whole grains and fish. In addition, one point was given for intakes below the median of red and processed meat, for use of olive or rapeseed oil for cooking or as dressing and for moderate alcohol consumption with an average of 5–15 g of alcohol per day
The association between adherence to individual components of AMED and the risks of microvascular complications among hyperglycemic participants with T2DM. One point was given for intakes above the median for fruit and vegetables, legumes and nuts, whole grains and fish. In addition, one point was given for intakes below the median of red and processed meat, for use of olive or rapeseed oil for cooking or as dressing and for moderate alcohol consumption with an average of 5–15 g of alcohol per day
Next, we performed subgroup analyses. For participants with hyperglycemia, the results showed that the estimates for DKD, DR or DN did not differ by gender, IMD, WC, alcohol consumption, physical activity, hypertension, use of antihypertensive medication, cholesterol-lowering medication and diabetes medication, and levels of HbA1c, HDL-C, LDL-C, IGF, TG and TC. However, the risk of DKD was lower among participants with the age of ≤ 55 years (P = 0.001) (Additional file 1: Table S3). For hyperglycemic participants with T2DM, the risk of DKD was also lower among those aged ≤ 55 years (P = 0.006) (Additional file 1: Table S4). The risk estimates for DKD, DR, or DN remained consistent among hyperglycemic participants without T2DM, regardless of these confounding factors (Additional file 1: Table S5).
Next, we performed sensitivity analyses by excluding cases that occurred within 2 or 4 years of follow-up. We observed similar trends in the associations between AMED score and the risks of microvascular complications within both a single study group and across separate groups, after lagging the exposure for 2 or 4 years (Additional file 1: Table S6-S8). To further investigate potential confounding variables that might impact the development of DKD, we conducted additional adjustments for the frequency of meat intake and creatinine levels. Our analysis revealed that adjusting for these variables did not result in significant changes in the risk of DKD (Additional file 1: Table S9).
Discussion
Accumulating studies have evaluated the association of MED with the incidence of T2DM. For example, a recent systematic review and meta-analysis showed that adherence to the MED was significantly associated with a reduced risk of T2DM. Specifically, for each one-point increase in the MED score, there was a 3% decrease in the risk of T2DM [27]. In a three-arm randomized trial, it was also found that higher adherence to the MED was inversely associated with the risk of T2DM. Following a median follow-up of 4.0 years, the incidences of T2DM were 10.1% (95% CI: 5.1-15.1) in the MED group and 17.9% (95% CI: 11.4-24.4) in the control group [28]. Moreover, the ATTICA study, conducted among the residents of Greece's Attica province, has revealed that diabetic participants with higher MED scores had a 27% reduction in HOMA-IR, a key parameter used to assess insulin resistance [29]. Most recently, it has been reported that higher adherence to Mediterranean lifestyles could help prevent T2DM in the British adult population. This suggests a potential applicability of the MED to the non-Mediterranean populations [30].
Despite the potentially positive effect of MED in reducing the risk of T2DM, the influence of MED on microvascular complications remains inconclusive and warrants further investigation. A previous systematic review indicated that higher adherence to the MED was associated with a reduced risk of incident DR. However, the majority of the studies analyzed were cross-sectional [17]. Therefore, more longitudinal studies are needed to clarify this association. A longitudinal study conducted among 71,392 adults with diabetes in Iran showed a significant association between MED adherence and a decreased incidence of microvascular complications. However, this association was evaluated using pooled logistic regression models, which do not include time-to-event analysis [31]. A case-control study has revealed that T2DM patients consuming moderate or high MED had 62% or 86% lower risks of developing DKD compared to those with low adherence [32]. However, it is important to note that this study was exclusively conducted among women and the number of participants was relatively small, which might lead to a low statistical power. More importantly, some studies have even reported that the MED is not associated with DKD. A cross-sectional study showed that adherence to MED was not significantly associated with renal function among patients with DKD [33]. A post hoc analysis of a cohort of patients with T2DM has revealed that MED enriched with either olive oil or nuts did not exert a protective effect against DKD [18].
In this study, we demonstrated that adherence to the MED is associated with a lower risk of DKD. This aligns with previous evidence indicating that the MED can improve renal function. The Leontio Lyceum Albuminuria Study reported that adolescents with a higher adherence to MED showed decreased levels of albuminuria [34]. Additionally, a cross-sectional analysis conducted among a cohort of patients with T2DM in Taiwan demonstrated that a high intake of fish and vegetables, as opposed to the traditional Chinese snack dietary pattern, could improve clinical indicators of renal function [35].
The positive effects of MED on renal function are likely attributed to the combined effects of its various components. The MED components, such as vegetables, fruits, and nuts are rich in vitamins C and E, α-tocopherol, β-carotene, selenium, and polyphenols. These ingredients could effectively reduce the oxidative damage to lipids and proteins associated with hyperfiltration [36, 37]. Furthermore, a high MUFA/SFA ratio, coupled with omega-3 fatty acid content in fish could improve hyperlipidemia, endothelial function and creatinine-clearance rate and reduce blood pressure [38, 39]. Interestingly, our findings indicated that legumes are a pivotal component of MED reducing the risk of DKD. We hypothesize that dietary fiber derived from legumes could delay the increase in postprandial glycaemia and mitigate the risk factors associated with DKD, such as low-grade inflammation, hypertension, and hyperlipidemia [40, 41].
The strengths of this study included the long period of follow-up and the large sample size. To our knowledge, this is the first prospective cohort study that has examined the relationship between a MED and the incidence of microvascular complications among individuals with hyperglycemia. Furthermore, the analysis effectively addressed potential confounding effects by adjusting for several well-established circulating biomarkers. This is crucial as these biomarkers are positively correlated with an increased risk of DKD [42]. We also acknowledge several limitations. First, the identification of microvascular complications relied on hospital inpatient records and death registries. This may potentially result in an underestimation of cases, especially given the unavailability of complete primary care data at present. Second, among the T2DM patients, some individuals have information available on their diabetes duration, while others do not. It is challenging to adjust for diabetes duration in all T2DM patients. However, we conducted a sensitivity analysis by including the available diabetes duration data for those participants with this information. Our analysis revealed that the inclusion of the diabetes duration did not impact the main outcomes (Additional file 1: Table S10). Third, AMED may be associated with improvements in healthy lifestyle behaviours during follow-up, leading to improvements in HbA1c levels, blood pressure, lipid profile, and other relevant circulating biomarkers. However, data on these factors were only collected at recruitment in the UK Biobank [21, 43,44,45], making it challenging to assess the impact of their dynamic changes on the outcomes. Moreover, the impact of changes in the use of medications for diabetes, hyperlipemia, or hypertension on the main outcomes cannot be assessed due to the absence of data on this information during the 12.3-year follow-up period. Future studies with more detailed information during follow-up are required to verify our findings. Fourth, our study indicates a slightly lower incidence of diabetic retinopathy (11.3%) compared to nephropathy (13.3%) among hyperglycemic participants with T2DM. This is inconsistent with a previous population-based cohort study [46]. In our study, the primary outcomes predominantly derive from the inpatient registration system, rather than universal screening. Therefore, it is possible that fewer individuals are registered for retinopathy compared to nephropathy. Finally, we utilized dietary data from a self-administered 24-hour recall method. As multiple 24-hour recalls are necessary to obtain a 'true' representation of habitual diet, and considering that many participants in the UK Biobank completed only one or two recalls, it's possible that the calculated MED scores may not comprehensively reflect the usual dietary intake of the participants [47, 48]. However, as evidenced by other studies, individuals generally maintain a relatively stable dietary intake over time [49, 50] and thus it is less likely that their diet categorization will remarkably change.
Conclusions
In this prospective cohort study, we have demonstrated that higher adherence to a MED is associated with a reduced risk of DKD among individuals with hyperglycemia. Our study emphasizes the necessity for continued research focusing on the benefits of the MED. Such efforts including the ongoing clinical trial will offer further insights into the role of MED in the clinical management of DKD.
Availability of data and materials
All data are available through request to the UK Biobank, and programs are available by contacting the corresponding author.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- AMED:
-
Alternate Mediterranean Diet
- ARBs:
-
Angiotensin-receptor blockers
- CIs:
-
Confidence intervals
- CRT:
-
Creatinine
- DKD:
-
Diabetic kidney disease
- DN:
-
Diabetic neuropathies
- DR:
-
Diabetic retinopathy
- eGFR:
-
Estimated glomerular filtration rate
- GFR:
-
Glomerular filtration rateGLP-1, glucagon-like peptide 1
- HbA1c:
-
Glycated hemoglobin
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostatic Model Assessment for insulin resistance
- HRs:
-
Hazard ratios
- IGF:
-
Insulin-like growth factor 1
- IMD:
-
Index of Multiple Deprivation
- LDL-C:
-
Low-density lipoprotein cholesterol
- MED:
-
Mediterranean Diet
- MUFA to SFA ratio:
-
Monounsaturated-to-saturated fat ratio
- MET:
-
Metabolic equivalent
- SGLT2:
-
Sodium-glucose co-transporter-2
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- T2DM:
-
Type 2 diabetes mellitus
- WC:
-
Waist circumference
References
Misra S, Ke C, Srinivasan S, Goyal A, Nyriyenda MJ, Florez JC, et al. Current insights and emerging trends in early-onset type 2 diabetes. Lancet Diabetes Endocrinol. 2023;11(10):768–82.
Doshi SM, Friedman AN. Diagnosis and management of type 2 diabetic kidney disease. Clin J Am Soc Nephrol. 2017;12(8):1366–73.
Baranowska-Jurkun A, Matuszewski W, Bandurska-Stankiewicz E. Chronic microvascular complications in prediabetic states-an overview. J Clin Med. 2020;9(10):3289.
Brown E, Heerspink HJL, Cuthbertson DJ, Wilding JPH. SGLT2 inhibitors and GLP-1 receptor agonists: established and emerging indications. Lancet. 2021;398(10296):262–76.
Crasto W, Patel V, Davies MJ, Khunti K. Prevention of microvascular complications of diabetes. Endocrinol Metab Clin North Am. 2021;50(3):431–55.
Li C, Luo J, Jiang M, Wang K. The efficacy and safety of the combination therapy with GLP-1 receptor agonists and SGLT-2 inhibitors in type 2 diabetes mellitus: a systematic review and meta-analysis. Front Pharmacol. 2022;13:838277.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44.
Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6 Suppl):1402s–6s.
Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis. BMJ. 2008;337:a1344.
Galbete C, Schwingshackl L, Schwedhelm C, Boeing H, Schulze MB. Evaluating Mediterranean diet and risk of chronic disease in cohort studies: an umbrella review of meta-analyses. Eur J Epidemiol. 2018;33(10):909–31.
Mozaffarian D, Marfisi R, Levantesi G, Silletta MG, Tavazzi L, Tognoni G, et al. Incidence of new-onset diabetes and impaired fasting glucose in patients with recent myocardial infarction and the effect of clinical and lifestyle risk factors. Lancet. 2007;370(9588):667–75.
Martínez-González MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z, et al. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ. 2008;336(7657):1348–51.
Sohouli MH, Mirmiran P, Seraj SS, Kutbi E, Alkahmous HAM, Almuqayyid F, et al. Impact of low-protein diet on cardiovascular risk factors and kidney function in diabetic nephropathy: a systematic review and meta-analysis of randomized-controlled trials. Diabetes Res Clin Pract. 2022;191:110068.
Carvalho CM, Gross LA, de Azevedo MJ, Viana LV. Dietary fiber intake (Supplemental or dietary pattern rich in fiber) and diabetic kidney disease: a systematic review of clinical trials. Nutrients. 2019;11(2):347.
Suckling RJ, He FJ, Macgregor GA. Altered dietary salt intake for preventing and treating diabetic kidney disease. Cochrane Database Syst Rev. 2010;12:Cd006763.
Wu Y, Xie Y, Yuan Y, Xiong R, Hu Y, Ning K, et al. The Mediterranean diet and age-related eye diseases: a systematic review. Nutrients. 2023;15(9):2043.
Shah J, Cheong ZY, Tan B, Wong D, Liu X, Chua J. Dietary intake and diabetic retinopathy: a systematic review of the literature. Nutrients. 2022;14(23):5021.
Díaz-López A, Babio N, Martínez-González MA, Corella D, Amor AJ, Fitó M, et al. Mediterranean diet, retinopathy, nephropathy, and microvascular diabetes complications: a post hoc analysis of a randomized trial. Diabetes Care. 2015;38(11):2134–41.
Bryl A, Mrugacz M, Falkowski M, Zorena K. A Mediterranean diet may be protective in the development of diabetic retinopathy. Int J Mol Sci. 2023;24(13):11145.
Xia B, He Q, Pan Y, Gao F, Liu A, Tang Y, et al. Metabolic syndrome and risk of pancreatic cancer: a population-based prospective cohort study. Int J Cancer. 2020;147(12):3384–93.
Geng T, Zhu K, Lu Q, Wan Z, Chen X, Liu L, et al. Healthy lifestyle behaviors, mediating biomarkers, and risk of microvascular complications among individuals with type 2 diabetes: a cohort study. PLoS Med. 2023;20(1):e1004135.
Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119(8):1093–100.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608.
Ho FK, Gray SR, Welsh P, Petermann-Rocha F, Foster H, Waddell H, et al. Associations of fat and carbohydrate intake with cardiovascular disease and mortality: prospective cohort study of UK Biobank participants. BMJ. 2020;368:m688.
Hu EA, Steffen LM, Grams ME, Crews DC, Coresh J, Appel LJ, et al. Dietary patterns and risk of incident chronic kidney disease: the Atherosclerosis Risk in Communities study. Am J Clin Nutr. 2019;110(3):713–21.
He Q, Wu S, Zhou Y, Liu Y, Xia B, Li W, et al. Genetic factors, adherence to healthy lifestyle behaviors, and risk of bladder cancer. BMC Cancer. 2023;23(1):965.
Sarsangi P, Salehi-Abargouei A, Ebrahimpour-Koujan S, Esmaillzadeh A. Association between Adherence to the Mediterranean diet and risk of type 2 diabetes: an updated systematic review and dose-response meta-analysis of prospective cohort studies. Adv Nutr. 2022;13(5):1787–98.
Salas-Salvadó J, Bulló M, Babio N, Martínez-González M, Ibarrola-Jurado N, Basora J, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Car. 2011;34(1):14–9.
Panagiotakos DB, Tzima N, Pitsavos C, Chrysohoou C, Zampelas A, Toussoulis D, et al. The association between adherence to the Mediterranean diet and fasting indices of glucose homoeostasis: the ATTICA Study. J Am Coll Nutr. 2007;26(1):32–8.
Maroto-Rodriguez J, Ortolá R, Carballo-Casla A, Iriarte-Campo V, Salinero-Fort M, Rodríguez-Artalejo F, et al. Association between a mediterranean lifestyle and Type 2 diabetes incidence: a prospective UK biobank study. Cardiovasc Diabetol. 2023;22(1):271.
Ghaemi F, Firouzabadi FD, Moosaie F, Shadnoush M, Poopak A, Kermanchi J, et al. Effects of a Mediterranean diet on the development of diabetic complications: a longitudinal study from the nationwide diabetes report of the National Program for Prevention and Control of Diabetes (NPPCD 2016–2020). Maturitas. 2021;153:61–7.
Jayedi A, Mirzaei K, Rashidy-Pour A, Yekaninejad MS, Zargar MS, Akbari Eidgahi MR. Dietary approaches to stop hypertension, mediterranean dietary pattern, and diabetic nephropathy in women with type 2 diabetes: A case-control study. Clin Nutr ESPEN. 2019;33:164–70.
Moradi M, Daneshzad E, Najafabadi MM, Bellissimo N, Suitor K, Azadbakht L. Association between adherence to the Mediterranean diet and renal function biomarkers and cardiovascular risk factors among diabetic patients with nephropathy. Clin Nutr ESPEN. 2020;40:156–63.
Mazaraki A, Tsioufis C, Dimitriadis K, Tsiachris D, Stefanadi E, Zampelas A, et al. Adherence to the Mediterranean diet and albuminuria levels in Greek adolescents: data from the Leontio Lyceum ALbuminuria (3L study). Eur J Clin Nutr. 2011;65(2):219–25.
Hsu CC, Jhang HR, Chang WT, Lin CH, Shin SJ, Hwang SJ, et al. Associations between dietary patterns and kidney function indicators in type 2 diabetes. Clin Nutr. 2014;33(1):98–105.
Hernández-Marco R, Codoñer-Franch P, Pons Morales S, Del Castillo Villaescusa C, Boix García L, Valls Bellés V. Oxidant/antioxidant status and hyperfiltration in young patients with type 1 diabetes mellitus. Pediatr Nephrol. 2009;24(1):121–7.
Slavin JL, Lloyd B. Health benefits of fruits and vegetables. Adv Nutr. 2012;3(4):506–16.
Chrysohoou C, Pitsavos C, Panagiotakos D, Skoumas J, Lazaros G, Oikonomou E, et al. Long-term fish intake preserves kidney function in elderly individuals: the Ikaria study. J Ren Nutr. 2013;23(4):e75-82.
Rasmussen BM, Vessby B, Uusitupa M, Berglund L, Pedersen E, Riccardi G, et al. Effects of dietary saturated, monounsaturated, and n-3 fatty acids on blood pressure in healthy subjects. Am J Clin Nutr. 2006;83(2):221–6.
Trinidad TP, Mallillin AC, Loyola AS, Sagum RS, Encabo RR. The potential health benefits of legumes as a good source of dietary fibre. Br J Nutr. 2010;103(4):569–74.
Mirmiran P, Yuzbashian E, Asghari G, Sarverzadeh S, Azizi F. Dietary fibre intake in relation to the risk of incident chronic kidney disease. Br J Nutr. 2018;119(5):479–85.
Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005;28(1):164–76.
Zhao L, Clay-Gilmour A, Zhang J, Zhang X, Steck SE. Higher ultra-processed food intake is associated with adverse liver outcomes: a prospective cohort study of UK Biobank participants. Am J Clin Nutr. 2024;119(1):49–57.
Petermann-Rocha F, Carrasco-Marin F, Boonpor J, Parra-Soto S, Shannon O, Malcomson F, et al. Association of five diet scores with severe NAFLD incidence: a prospective study from UK Biobank. Diabetes Obes Metab. 2024;26(3):860–70.
Maroto-Rodriguez J, Delgado-Velandia M, Ortolá R, Perez-Cornago A, Kales SN, Rodríguez-Artalejo F, et al. Association of a Mediterranean lifestyle with all-cause and cause-specific mortality: a prospective study from the UK Biobank. Mayo Clin Proc. 2024;99(4):551–63.
Wei Y, Herzog K, Ahlqvist E, Andersson T, Nyström T, Zhan Y, et al. All-cause mortality and cardiovascular and microvascular diseases in latent autoimmune diabetes in adults. Diabetes Care. 2023;46(10):1857–65.
Liu B, Young H, Crowe FL, Benson VS, Spencer EA, Key TJ, et al. Development and evaluation of the Oxford WebQ, a low-cost, web-based method for assessment of previous 24 h dietary intakes in large-scale prospective studies. Public Health Nutr. 2011;14(11):1998–2005.
Jackson KA, Byrne NM, Magarey AM, Hills AP. Minimizing random error in dietary intakes assessed by 24-h recall, in overweight and obese adults. Eur J Clin Nutr. 2008;62(4):537–43.
Wang DD, Leung CW, Li Y, Ding EL, Chiuve SE, Hu FB, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587–95.
Khalili H, Håkansson N, Chan SS, Chen Y, Lochhead P, Ludvigsson JF, et al. Adherence to a Mediterranean diet is associated with a lower risk of later-onset Crohn’s disease: results from two large prospective cohort studies. Gut. 2020;69(9):1637–44.
Acknowledgements
We thank all UK Biobank participants and staff.
Funding
Science and Technology Planning Project of Guangzhou (NO. 201903010044); Science and Technology Program of Shenzhen (NO. JCYJ20220530145017038); Basic and Applied Basic Research Program of Guangdong (NO. 2022A1515110850).
Author information
Authors and Affiliations
Contributions
C.Q., T.L., and J.Q.: designed research; C.Q., J.Z., J.L., X.W., Y.L., J.Y., and B.X.: analyzed data; C.Q.: wrote the paper; M.P.P., T.Z., N.W., P.H., and H.C.: critically reviewed the manuscript; M.P.P., C.Q., and B.X.: revised the manuscript; and all authors: approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The UK Biobank study was approved by the North West Multi-Center Research Ethics Committee (REC reference for UK Biobank 11/NW/0382), and written informed consent was provided prior to participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12916_2024_3455_MOESM1_ESM.zip
Additional file 1: Fig. S1. Dose-response relationship of AMED with the risks of microvascular complications among hyperglycemic participants without T2DM. The X-axis showed the numbers of AMED, and the y-axis showed the HRs of the composite microvascular complications (a), diabetic retinopathy (b), diabetic neuropathy (c), and diabetic kidney disease (d). Multivariable-adjusted models were adjusted for age (continuous, years) and gender (men or women), ethnicity (white or other), index of multiple deprivation (a measure of socioeconomic status), waist circumference (continuous, centimeters), alcohol consumption (categorized as never or special occasions only, one to three times a month, one to four times a week, daily or almost daily), physical activity (h/week), hypertension (yes or no), family history of diabetes (yes or no), family history of hypertension (yes or no), family history of heart disease (yes or no) and family history of stroke (yes or no), HbA1c (continuous, mmol/L), HDL-C (continuous, mmol/L), LDL-C (continuous, mmol/L), IGF (continuous, mmol/L), TG 30 (continuous, mmol/L), CHOL (continuous, mmol/L), use of antihypertensive medication and use of cholesterol lowering medication. Fig. S2. The association between adherence to individual components of AMED and the risks of microvascular complications among hyperglycemic participants without T2DM. One point was given for intakes above the median for fruit and vegetables, legumes and nuts, whole grains and fish. In addition, one point was given for intakes below the median of red and processed meat, for use of olive or rapeseed oil for cooking or as dressing and for moderate alcohol consumption with an average of 5–15 g of alcohol per day. Table S1. Components and scoring criteria of the Alternate Mediterranean Diet (AMED). Table S2. HRs (95% CIs) of microvascular complications according to the numbers of AMED among hyperglycemic participants without T2DM. Table S3. Stratified analyses of the associations of AMED with the risks of microvascular complications among total participants with hyperglycemia. Table S4. Stratified analyses of the associations of AMED with the risks of microvascular complications among hyperglycemic participants with T2DM. Table S5. Stratified analyses of the associations of AMED with the risks of microvascular complications among hyperglycemic participants without T2DM. Table S6. Sensitivity analyses of the associations between AMED scores and the risks of microvascular complications among total participants with hyperglycemia, after lagging the exposure for 2 or 4 years. Table S7. Sensitivity analyses of the associations between AMED scores and the risks of microvascular complications among hyperglycemic participants with T2DM, after lagging the exposure for 2 or 4 years. Table S8. Sensitivity analyses of the associations between AMED scores and the risks of microvascular complications among hyperglycemic participants without T2DM, after lagging the exposure for 2 or 4 years. Table S9. Sensitivity analyses of the associations between AMED scores and the risks of diabetic kidney disease (DKD) after including frequency of meat intake and creatinine as additional confounders in model 2 of DKD. Table S10. HRs (95% CIs) of microvascular complications according to the numbers of AMED among T2DM participants with available information on the diabetes duration.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qu, C., Zhao, J., Lai, J. et al. Adherence to a Mediterranean diet is associated with a lower risk of diabetic kidney disease among individuals with hyperglycemia: a prospective cohort study. BMC Med 22, 224 (2024). https://doi.org/10.1186/s12916-024-03455-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03455-3