Abstract
Background
To the best of our knowledge, no study has investigated the potential joint effect of large for gestational age (LGA) and assisted reproductive technology (ART) on the long-term health of children.
Methods
This was a prospective cohort study that recruited children whose parents had received ART treatment in the Center for Reproductive Medicine, Shandong Provincial Hospital, affiliated to Shandong University, between January 2006 and December 2017. Linear mixed model was used to compare the main outcomes. The mediation model was used to evaluate the intermediary effect of body mass index (BMI).
Results
4138 (29.5%) children born LGA and 9910 (70.5%) children born appropriate for gestational age (AGA) were included in the present study. The offspring ranged from 0.4 to 9.9 years. LGAs conceived through ART were shown to have higher BMI, blood pressure, fasting blood glucose, fasting insulin, and homeostatic model assessment of insulin resistance values, even after controlling for all covariates. The odds of overweight and insulin resistance are also higher in LGA subjects. After adjusting for all covariates, LGAs conceived through ART had BMI and BMI z-scores that were 0.48 kg/m2 and 0.34 units greater than those of AGAs, respectively. The effect of LGA on BMI was identified as early as infancy and remained consistently significant throughout pre-puberty.
Conclusions
Compared to AGA, LGA children conceived from ART were associated with increased cardiovascular-metabolic events, which appeared as early as infancy and with no recovery by pre-puberty.
Similar content being viewed by others
Background
The global prevalence of childhood obesity increased by 47.1% between 1980 and 2013 [1], and in 2015, a total of 107.7 million children were classified as obese [2]. Obesity during childhood is a medical disorder that leads to many comorbidities including obstructive sleep apnea syndrome, nonalcoholic fatty liver disease, polycystic ovary syndrome, impaired mobility, joint pain, depression, and anxiety disorders [3]. Furthermore, increasing evidence suggests that obese children are more likely to be classified as obese in adulthood compared to their counterparts with normal weight [4]. Childhood obesity has also been associated with cardiovascular disease and metabolic disorders throughout life [5].
Large for gestational age (LGA), a condition that affects 2.3% to 22.1% of Asian newborns, is generally defined as having a birth weight above the 90th percentile for gestational age [6]. Several factors determine the occurrence of LGA including genes [7], race [8], intrauterine malnutrition [9,10,11], and artificial intervention in gametes or embryos [12]. Although the long-term health consequences of LGAs were first reported in the 1990s, the condition had not attracted widespread attention until recently. Numerous studies have reported that LGA children (LGAs) have an elevated risk of obesity, hypertension, and metabolic disorders in both childhood and adulthood [13,14,15]. However, conflicting findings show that a high birth weight is not associated with future cardiovascular and metabolic health problems [16, 17]. Globally, over 8 million children have been conceived through assisted reproductive technology (ART) [18]. However, previous studies demonstrated that children conceived through ART were at a higher risk of developing cardiovascular metabolic challenges in childhood [19, 20]. Nonetheless, to the best of our knowledge, no study has investigated the potential joint effect of LGA and ART on the long-term health of children. Furthermore, little is known about the longitudinal changes associated with LGA, particularly regarding future cardiovascular metabolic health challenges or whether LGAs are able to compensate for the dysfunction over time.
In the present study, we explored the associations between LGA and cardiometabolic markers in the ART cohort. Additionally, we assessed the developmental stages at which the effects of LGA appeared and whether they were compensated for, over time. Furthermore, we examined the intermediary effect of later-life body mass index.
Methods
Study design and setting
This study was based on the ART cohort in the Center for Reproductive Medicine, Shandong Provincial Hospital, affiliated to Shandong University, which aimed to evaluate the growth and development of offspring conceived from assisted reproduction technology (ART). It was a prospective cohort that recruited children whose parents received ART treatment at the Center for Reproductive Medicine, Shandong Provincial Hospital Affiliated to Shandong University between January 2006 and December 2017. Recruitment into the study began in July 2014 and was still ongoing at the time of this publication.
The singleton children conceived from ART were eligible for inclusion in the study. However, children were excluded if they had congenital anomalies, kidney or cardiovascular diseases, or lacked anthropometry and cardiovascular metabolism data. In addition, children with a birth weight that was small for gestational age were excluded. Finally, 14,048 children were included in the study (Additional file 1: Fig. S1).
All parents provided signed informed consent and the study was approved by the ethics committee at the Center for Reproductive Medicine, Shandong Provincial Hospital affiliated to Shandong University.
Exposure assessment
The interest exposure is LGA, which represents a type of “intrauterine overgrowth” [21]. LGA is defined based on three factors: birth weight, gestational age (GA), and sex. Data on birth weight and sex were collected from medical records within 42 days of delivery. Gestational age was calculated using the birth and embryo transfer dates. GA-specific and sex-specific birth weight percentiles based on the Chinese population were used to categorize the GA groups [22]. Those infants exceeding the 90th percentile for a given gestational week are classified as LGA [21]. While infants with birth weight between 10th ~ 90th percentile were considered as appropriate for gestational age (AGA).
Covariates
Parental demographics, anthropometric data, medical history, and family socioeconomic status were collected before ART treatment. Information on mothers’ exposure to tobacco and alcohol during pregnancy was collected at 13–18 weeks of gestation. Moreover, data on neonatal anthropometry, congenital malformations and diseases, hypertensive disorders in pregnancy (HDP), gestational diabetes mellitus (GDM), and pregnancy anthropometry were collected within 42 days of delivery. The medical history of the parents was defined as whether the parents are diagnosed with hypertension or diabetes, and whether the mother has hyperlipidemia. Parental blood pressure, fasting blood glucose, and maternal lipid profile are routine screening in ART treatment. Exposure to tobacco during pregnancy not only included smoking pregnant women, but also their exposure from the surrounding environment. Family socio-economic status was defined as the parents’ highest socio-economic status. Education level was categorized as three years of college or above and high school or below. Occupation was categorized as student or unemployed, physical labor, and mental labor. Per capita monthly income was categorized as lower than ¥2999, ¥3000 ~ ¥4999, higher than ¥4999. Parity was categorized as first born, second born, and third born or late. The gestational age, children’s age, parents’ age, height, and BMI were adjusted as continuous variables. The categorical covariates such as sex, parity, GDM, HDP, education level, occupation, per capita monthly income, and medical history were converted into a dumbbell variable before adjusted in the models.
Outcomes
Follow-up visits with children occurred at infancy (0–0.9 years), toddler’s age (1–2.9 years), preschool (3–5.9 years), and school age (6–9.9 years). Children’s projects were determined by the age at visit. The outcomes we focus on include children’s height, BMI, blood pressure (BP), fasting blood glucose (FBG), fasting insulin (FIN), total cholesterol (TC), triacylglycerol (TG), high-density lipoprotein (HDL), and low-density lipoprotein (LDL). We included them as continuous variables and binary variables in the models, respectively.
Height (length) and weight were measured from 5 months. Briefly, height (accurate to 0.1 cm) and weight (accurate to 0.1 kg) were measured twice with a stadiometer and scaled. All children were required to wear light clothes. BMI was calculated as weight/height2. The sex-specific BMI z-score (z = (value-mean)/SD) was calculated based on the mean and the standard deviation (SD) of the 2006 WHO child growth standards. BMI z-score > 2 was classified as overweight.
BP was measured from the age of 2 and was estimated three times on the right arm while the child was sitting quietly, using a calibrated electronic BP monitor (Omron HEM-7012, Omron Healthcare, Japan). The mean from the last two BP readings was used for calculation. Sex-, age-, and height-specific BP z-score was calculated as (BP-expected BP)/σ. Because the mathematical formula for China’s expected blood pressure and σ cannot be obtained, we used the standard of the National High Blood Pressure Education Program (NHBPEP) [23]. In addition, in order to increase clinical relevancy, we divided blood pressure into SBP or DBP ≥ 95th percentiles of Chinese sex-, age-, and height-specific BP references and < 95th percentiles [24].
Fasting blood samples were obtained from the age of 2. Nurses collected the fasting blood samples in the morning and stored them at – 80 ℃. The hexokinase method (Cobas c702 instrument; Roche Diagnostics, Mannheim, Germany) was used to determine FBG (mmol/L), while the Electrochemiluminescence immunoassay (Cobas e601 instrument; Roche Diagnostics) was utilized to measure serum insulin. Serum TC (mmol/L), TG (mmol/L), LDL (mmol/L), and HDL (mmol/L) were determined using a homogeneous assay (Cobas c702 instrument; Roche Diagnostics). The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as FIN(mIU/L) × FBG (mmol/L)/22.5. HOMA-IR was divided into ≥ 95th percentiles or < 95th percentiles based on the reference of healthy Chinese children [25]. We divided FBG into two groups based on the diagnostic criteria for impaired fasting glucose tolerance [26]: ≥ 5.6 mmol/L and < 5.6 mmol/L. Similarly, the classification of lipid profiles is also based on the diagnostic criteria for children with hyperlipidemia [27, 28].
Statistical analysis
Normally distributed data were expressed as means ± SD, skewed variables were presented as the median ± interquartile range, and categorical variables were expressed as numbers and percentages. The t-test and Wilcoxon rank sum test were used on continuous variables with normal and skewed distribution, respectively. The chi-square and Fisher’s exact tests were used to analyze categorical data. In addition, the quantile–quantile plot was employed to test for normality.
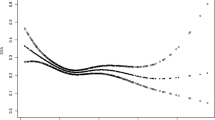
As this study was designed with repeated measurements, we used the linear mixed model to compare the main linear outcomes. The time-dependent and time-independent variables account for the random effects and fixed effects, respectively. The random effect included the unique offspring ID number. Other covariates were included in the fixed effects. When the outcome is analyzed as a binary variable, the generalized estimating equations (GEE) were applied. The confounding factors are determined through directed acyclic graphs (Additional file 2: Fig. S2). In Model 1, we adjusted for the children’s age and sex, while in Model 2, parity, gestational age, parental age at delivery, HDP, GDM, maternal pre-pregnancy BMI, and maternal tobacco and alcohol exposure during pregnancy, were adjusted. In Model 3, we further adjusted for genetic factors, including parents’ height, BMI, history of hypertension and diabetes, and maternal hyperlipidemia. In Model 4, variables from the above three models were considered along with socioeconomic factors. The number of follow-up visits was additionally adjusted for in each model. Moreover, a generalized additive model allowing for nonlinear correlation was used to describe the age-related trends in BMI, in the two groups.
Notably, a mediation model can separately evaluate the indirect effect of X (independent variable) on Y (dependent variable) through the mediator (M) and its direct effect on Y [29]. BMI was identified as a mediator when assessing the effect of LGA on other outcome variables (metabolic markers). The package of “mediation” was used for mediating effect analysis. Age-stratified analysis was based on developmental stages (toddler’s age: 1–2.9 years old; preschooler: 3–5.9 years; school age children: 6–9.9 years). At each developmental stage, the first follow-up data was used for analysis. The multiple linear models were applied for analysis. Children’s age, sex, parity, gestational age, parental age at delivery, HDP, GDM, maternal tobacco and alcohol exposure during pregnancy, parents’ BMI, parents’ history of hypertension and diabetes, maternal hyperlipidemia, and socioeconomic factors were added to the model.
To account for multiple testing, the Benjamini/Hochberg (B/H) method adjusted two-sided p values to control the false discovery rate (FDR). Statistical significance was based on a B/H-adjusted p value (q value) below 0.05, corresponding to an FDR of 5%. All analyses were conducted in R Version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Participant characteristics
The birth characteristics, parental characteristics, and socio-economic status in included and non-included children were shown in Additional file 3: Tab. S1. Overall, the included and non-included populations have similar birth information, parental characteristics, and socio-economic status. However, the included children tend to have slightly higher birth weight, are more likely to be the first child, have younger parents, and come from families with slightly lower socioeconomic status.
Overall, 9910 (70.5%) children were in the AGA group while 4138 (29.5%) were in the LGA category (Table 1, Additional file 1: Fig. S1). Table 1 gives a summary of the birth, parental, and socioeconomic characteristics of the study participants. The characteristics differed significantly between the two groups. For instance, children in the LGA group had a significantly higher length, birth weight/length (BW/L), birth weight/length2 (BW/L2), and birth weight/length3 (ponder index) (length: mean 51.08 vs. 50.02 cm; BW/L: mean 7.68 vs. 6.56 kg/m; BW/L2: mean 15.04 vs. 13.11 kg/m2; ponder index: mean 29.50 vs. 26.24 kg/m3, all P < 0.001). Compared to the AGA category, parents who gave birth to LGA infants were older (age: mother, mean 31.98 vs. 31.40 years; father, mean 32.73 vs. 32.23 years, both P < 0.001), higher (height: mother, mean 162.42 vs. 161.43 cm; father, mean 174.18 vs. 173.56 cm, both P < 0.001) and heavier (BMI: mother, mean 24.28 vs. 22.87 kg/m2; father, mean 25.98 vs. 25.58 kg/m2, both P < 0.001). Moreover, LGA children were more likely to be exposed to GDM, pre-pregnancy diabetes (GDM: 9.9% vs. 6.4%, pre-pregnancy diabetes: 1.0% vs. 0.2%, all P < 0.001).
Anthropometric measures and cardiometabolic makers
There were striking anthropometric differences between children in the LGA and AGA groups (Tables 2 and 3, Additional file 4: Tab. S2). Compared with AGA subjects, LGAs conceived from ART subjects had significantly higher odds of overweight (odds ratio (OR) = 1.59, 95% confidence interval (CI): 1.46–1.74; Table 2). LGAs conceived from ART had BMI and BMI z-scores that were 0.48 kg/m2 and 0.34 units greater than those of AGAs, respectively. Additionally, LGA children were about 1.09 cm taller in height and had 0.39 more height z-score units compared to those in the AGA group (height: mean 88.17 vs. 86.43 cm, height z-score: mean 1.10 vs. 0.65). At birth, length and Ponder index were higher in LGA newborns than in their AGA peers (both P < 0.001) (Table 1). Moreover, higher BMI and BMI z-scores were observed in the LGA group from infancy to pre-puberty, and after adjusting for confounders, the difference was still significant (BMI kg/m2: infancy, mean 18.68 vs. 18.13; toddler’s age, mean 16.94 vs. 16.44; preschooler, mean 16.44 vs. 15.83; school age children, mean 17.96 vs. 16.99; BMI z-score: infancy, mean 1.07 vs. 0.70, toddler’s age, mean 0.70 vs. 0.33, preschooler, mean 0.78 vs. 0.34, school age children, mean 1.37 vs. 0.79) (Table 4). The significantly higher BMI, BMI z-score, height, height z-score were observed in both male and female LGA children conceived through ART (Additional file 5: Tab. S3, Additional file 6: Fig. S3). Similarly, the significantly higher BMI, BMI z-score, height, height z-score were observed both in fresh embryo transfer and frozen embryo transfer (Additional file 7: Tab. S4).
LGAs conceived through ART had significantly higher systolic blood pressure (SBP) and diastolic blood pressure (DBP) values than the AGAs (SBP: mean 94.14 vs. 93.40 mmHg; DBP: mean 57.76 vs. 56.76) (Table 3, Additional file 4: Tab. S2). In addition, age-specific analysis revealed that LGAs conceived through ART were associated with a significantly higher BP at toddler’s age and pre-school age but not in school age subgroup children (SBP: toddler’s age, mean 89.86 vs. 89.40 mmHg, q = 0.014; preschooler, mean 95.70 vs. 94.94 mmHg, q = 0.047; school age children, mean 102.53 vs. 101.72 mmHg, q = 0.835; DBP: toddler’s age, mean 53.96 vs. 53.38 mmHg, q = 0.009; preschooler, mean 59.18 vs. 57.95 mmHg, q = 0.001; school age children, mean 65.12 vs. 64.16 mmHg, q = 0.154) (Table 4).
Compared with AGA subjects, LGAs conceived from ART subjects had significantly higher odds of insulin resistance (greater than or equal 95th percentile of HOMA-IR of healthy Chinese children) (OR = 1.58, 95% CI: 1.22–2.06; Table 2). FBG, FIN, and HOMA-IR were significantly higher in LGA children conceived through ART than in their AGA counterparts (FBG: mean 4.98 vs. 4.94 mmol/L; FIN: mean 5.61 vs. 5.12 mIU/L; HOMA-IR: mean 1.29 vs. 1.15) (Table 3). However, there were no significant differences in TC, TG, LDL, and HDL, between the LGA and AGA groups. When stratified by age, there were no significant differences in FBG, FIN, and HOMA-IR between LGA and AGA toddlers (Table 4). In addition, FBG and HOMA-IR were significantly higher in the LGA group, among preschool age and school age children (Table 4). Stratification based on gender yielded different results. FBG was significantly higher in the LGA group, among females (FBG: mean 4.94 vs. 4.89 mmol/L, FIN: mean 5.80 vs. 5.27 mIU/L; HOMA-IR: mean 1.32 vs. 1.17) (Additional file 5: Tab. S3). However, there were no differences in FBG, FIN, and HOMA-IR between the LGA and AGA groups, in males (Additional file 5: Tab. S3). Additionally, in male subjects, TC and LDL levels were significantly higher in the LGA group, even after correcting for confounders (Additional file 5: Tab. S3).
Mediating
The direct and indirect effects of LGA are presented in Table 5. For FBG, FIN, and HOMA-IR the mediating effect of BMI is significant from preschool age to school age children. And in toddler’s age, the mediating effect of BMI for FBG and FIN is also significant (although it no longer has statistical significance after adjusting the p). Higher BMI in LGA children may have adverse effects on glucose metabolism at all developmental stages we have studied. However, the total effect a significant only in school age children (Because the mediation effect analysis only included the first follow-up data for each developmental stage, the results were slightly different from the results in Table 4). In school age children, the mediating effects of BMI on FIN and HOMA-IR accounted for 52.4% and 42.9% respectively, which indicated that when the elevated BMI cannot return to normal, LGA children may have adverse glucose metabolism outcomes in the future. For SBP and DBP the mediating effect of BMI is significant at all developmental stages we have studied. In other words, elevated BMI can have adverse effects on BP, regardless of developmental stage.
Discussion
In the present study, involving children aged 0.4–9.9 years, LGAs conceived through ART were shown to have higher cardiovascular risk profiles than their AGA counterparts, including higher BMI, BP, FBG, FIN, and HOMA-IR values even after controlling for all covariates. The odds of overweight and insulin resistance are also higher in LGA subjects. The elevated BMI appeared as early as in infancy in the LGA children and remained consistently high to their pre-puberty.
Consistent with previous research, our study showed that LGA individuals had a higher BMI [15, 30,31,32]. The determinants of LGA including GDM and parental obesity have been confirmed to be independent risk factors for childhood obesity [33, 34]. Even after adjusting for those covariates, LGAs still had a significantly higher BMI which was consistent with earlier studies that demonstrated the independent effect of LGA [16, 30, 32]. However, several studies did not show the influence of LGA in children born to women without GDM and obesity [13, 35]. But the positive association between the LGA and BMI was found in our sensitivity analysis which excluded those children whose mothers suffer from GDM and obesity (Additional file 8: Tab. S5). Although there is limited data available to explain this effect, one potential biological mechanism is “fetal programming.” Caused by an adverse early life environment, “fetal programming” could influence the development of the liver and hypothalamus, affect the volume, number, and distribution of adipocytes, alter gene expression levels, and change responses to the postnatal nutritional environment [36,37,38].
This study also showed that the ponderal index of LGA newborns was significantly higher than that of AGA newborns. Similarly, previous studies on the body composition of newborns demonstrated that LGA children born to women with GDM and obesity had an increase in both fat and lean body mass [39]. Moreover, our study also indicated that the elevated BMI in LGAs appeared as early as in infancy and remained consistent to pre-puberty. And the studies focused on adolescence and adulthood also found a high risk of obesity in LGAs [14, 40]. Evidence of childhood obesity persisting into adulthood was confirmed in a systematic review including 25 publications [4]. Therefore, LGA is not only a marker of “fetal obesity” but is also the earliest indicator of future obesity. According to previous research, an effort to normalize BMI before puberty was beneficial as it was shown to significantly reduce the risk of metabolic disorders and cardiovascular disease in adulthood [41, 42]. Furthermore, existing literature shows that if obesity starts at around the age of 7 and BMI increases from age 7 to adolescence, the risk of type 2 diabetes in middle age increases significantly, even if the weight was normal before age 7 [41]. However, the BMI gap between the LGAs and AGAs did not disappear with age in both genders, which might indicate that LGA was not “metabolically normal obese.”
In the present study, higher odds of insulin resistance and higher FBG, FIN, and HOMA-IR values were observed in LGA children compared to their AGA peers, even after adjusting for covariates. These results were consistent with those previous studies, which showed that LGA was positively associated with increased insulin resistance [13, 35, 43]. However, contrary to our findings, numerous previous studies did not report significant differences in glucose metabolism between the LGAs and AGAs [16, 44, 45]. The difference in BMI between LGA and AGA children may be the reason for the contradictory results. According to existing reports, BMI was significantly correlated with insulin resistance, increased BMI occurred earlier than insulin resistance, and BMI interventions could significantly improve insulin sensitivity [46,47,48]. Our intermediary effect analysis showed that the impact of LGA on children’s FIN and HOMRA-IR was explained by elevated BMI. The results also showed that impaired glucose metabolism in LGA children was more significant in girls. The potential underlying mechanisms include differential expression of metabolic-related genes, varying hormone sensitivity, and body composition [49, 50]. The different sex ratios in previous studies may also be the reason for the conflicting results. Moreover, the heterogeneity of the population might be a potential reason. In this study, significant differences in BMI and glucose metabolism were observed in children conceived through ART. However, it was not clear if there was any interaction between ART and LGA.
In the present study, higher blood pressure was observed in LGA children compared to their AGA peers. Moreover, the age subgroup showed that a higher BP in LGA children was observed in toddlers and preschoolers, but not in school aged children. Previous studies suggested that being LGA was associated with a significantly higher risk of hypertension by 1.4–1.8-fold in adolescents and young adults, but not in school aged or younger children [51, 52]. However, other reports did not show significant differences between LGAs and AGAs in either SBP or DBP [17, 35, 53]. The intermediary effect analysis showed that elevated BMI could explain approximately one-fourth to two-thirds of the effect of LGA on BP. The difference in BMI could be one of the reasons for the inconsistent results. A previous study reported that children conceived through ART were associated with an increased risk of cardiovascular metabolic dysfunction, compared to the natural controls [19]. Another possible explanation might be the interaction between LGA and ART.
This study had several strengths including the use of longitudinal and detailed data, a wide range of covariates, a homogeneous population, and a large sample size. However, despite the insightful findings, it also had some limitations. First, although various measures were taken to enhance the response rate, non-response was inevitable (Additional file 1: Fig. S1, Additional file 9: Tab. S6). Children with younger parents are more likely to receive follow-up (Additional file 3: Tab. S1), which may lead to selection bias.
In addition, despite our best efforts to adjust for confounding factors, we cannot observe all confounding factors (known and unknown). Secondly, based on current data, we are unable to distinguish LGA represents a condition arising from physiological processes and pathological conditions. Our analysis represents the combined results of all types of LGA, and the more detailed analysis requires further well-designed research [54]. In addition, live birth is one of the necessary inclusion criteria for evaluating the long-term health of offspring born from ART, which inevitably leads to selection bias. This study is more representative of the children born to couples who are able to have live birth infants. And this study is focused on participants from the ART cohort, whether the results can be extrapolated to the naturally pregnant population requires more well-designed research to confirm. Third, the samples were detected on different dates because of the large sample size. Our biospecimen results may be influenced by the potential batch effects.
Conclusions
In conclusion, LGA conceived from ART were at a higher risk of cardiovascular metabolic dysfunction in childhood, were more predisposed to obesity, and had decreased insulin sensitivity. These could be identified as early as in infancy and persisted consistently to pre-puberty. In addition, the BMI in LGA children may be an intermediary that serves to block further deterioration of cardiovascular metabolism. Therefore, controlling birth weight and post birth overweight and obesity may be effective measures to reduce cardiovascular metabolic risks in children conceived from ART. And prevention of overweight and obesity in these children should begin at infancy.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AGA:
-
Appropriate for gestational age
- ART:
-
Assisted reproductive technology
- B/H:
-
Benjamini/Hochberg
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- BW/L:
-
Birth weight/length
- BW/L2 :
-
Birth weight/length2
- CI:
-
Confidence interval
- DBP:
-
Diastolic blood pressure
- FBG:
-
Fasting blood glucose
- FDR:
-
False discovery rate
- FIN:
-
Fasting insulin
- GA:
-
Gestational age
- GDM:
-
Gestational diabetes mellitus
- GEE:
-
Generalized estimating equations
- HDL:
-
High-density lipoprotein
- HDP:
-
Hypertensive disorders in pregnancy
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- LDL:
-
Low-density lipoprotein
- LGA:
-
Large for gestational age
- NHBPEP:
-
National High Blood Pressure Education Program
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- TC:
-
Total cholesterol
- TG:
-
Triacylglycerol
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197–209.
Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–88.
Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, Lauer RM. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: the Muscatine Study. J Am Coll Cardiol. 1996;27(2):277–84.
Harvey L, van Elburg R, van der Beek EM. Macrosomia and large for gestational age in Asia: one size does not fit all. J Obstet Gynaecol Res. 2021;47(6):1929–45.
Ahlsson F, Gustafsson J, Tuvemo T, Lundgren M. Females born large for gestational age have a doubled risk of giving birth to large for gestational age infants. Acta Paediatr. 2007;96(3):358–62.
Tutlam NT, Liu Y, Nelson EJ, Flick LH, Chang JJ. The effects of race and ethnicity on the risk of large-for-gestational-age newborns in women without gestational diabetes by prepregnancy body mass index categories. Matern Child Health J. 2017;21(8):1643–54.
Marchi J, Berg M, Dencker A, Olander EK, Begley C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev. 2015;16(8):621–38.
Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, Li N, Hu G, Corrado F, Rode L, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017;317(21):2207–25.
Ye W, Luo C, Huang J, Li C, Liu Z, Liu F. Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. 2022;377:e067946.
Ishihara O, Araki R, Kuwahara A, Itakura A, Saito H, Adamson GD. Impact of frozen-thawed single-blastocyst transfer on maternal and neonatal outcome: an analysis of 277,042 single-embryo transfer cycles from 2008 to 2010 in Japan. Fertil Steril. 2014;101(1):128–33.
Evagelidou EN, Kiortsis DN, Bairaktari ET, Giapros VI, Cholevas VK, Tzallas CS, Andronikou SK. Lipid profile, glucose homeostasis, blood pressure, and obesity-anthropometric markers in macrosomic offspring of nondiabetic mothers. Diabetes Care. 2006;29(6):1197–201.
Derraik JGB, Maessen SE, Gibbins JD, Cutfield WS, Lundgren M, Ahlsson F. Large-for-gestational-age phenotypes and obesity risk in adulthood: a study of 195,936 women. Sci Rep. 2020;10(1):2157.
Kapral N, Miller SE, Scharf RJ, Gurka MJ, DeBoer MD. Associations between birthweight and overweight and obesity in school-age children. Pediatr Obes. 2018;13(6):333–41.
Kampmann FB, Thuesen ACB, Hjort L, Olsen SF, Pires SM, Tetens I, Grunnet LG. Exposure to gestational diabetes is a stronger predictor of dysmetabolic traits in children than size at birth. J Clin Endocrinol Metab. 2019;104(5):1766–76.
Kuhle S, Maguire B, Ata N, MacInnis N, Dodds L. Birth weight for gestational age, anthropometric measures, and cardiovascular disease markers in children. J Pediatr. 2017;182:99–106.
Crawford GE, Ledger WL. In vitro fertilisation/intracytoplasmic sperm injection beyond 2020. BJOG. 2019;126(2):237–43.
Cui L, Zhou W, Xi B, Ma J, Hu J, Fang M, Hu K, Qin Y, You L, Cao Y, et al. Increased risk of metabolic dysfunction in children conceived by assisted reproductive technology. Diabetologia. 2020;63(10):2150–7.
Scherrer U, Rexhaj E, Allemann Y, Sartori C, Rimoldi SF. Cardiovascular dysfunction in children conceived by assisted reproductive technologies. Eur Heart J. 2015;36(25):1583–9.
Fetal-Growth Disorders. In: Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, Casey BM,Sheffield JS, editors. Williams Obstetrics. 24th ed. McGraw-Hill Education. 2014. p. 2035–2054.
Zong XN, Li H, Zhang YQ, Wu HH. Reference values and growth curves of weight/length, body mass index, and ponderal index of Chinese newborns of different gestational ages. Chin J Obstet Gynecol. 2021;59(3):181–8.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis e, and treatment of high blood pressure in children and adolescents: the fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–576.
Hui F, Yinkun Y, Jie M. Updating blood pressure references for Chinese children aged 3–17 years. Chin J Hypertens. 2017;25:428–35.
Chinese Diabetes Society Insulin Resistance Study Group (preparatory). Expert guidance on insulin resistance assessment methods and applications. Chin J Diabetes Mellitus. 2018;10(6):377–385.
Isganaitis E, Laffel L. Recommendations for screening children and adolescents for prediabetes and type 2 diabetes. JAMA. 2022;328(10):933–4.
Zou CC. Expert consensus on diagnosis and management of dyslipidemia in children. Chin J Pediatr. 2022;60(7):633–9.
Burlutskaya AV, Tril VE, Polischuk LV, Pokrovskii VM. Dyslipidemia in pediatrician’s practice. Rev Cardiovasc Med. 2021;22(3):817–34.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82.
Chen YL, Han LL, Shi XL, Su WJ, Liu W, Wang LY, Huang PY, Lin MZ, Song HQ, Li XJ. Adverse pregnancy outcomes on the risk of overweight offspring: a population-based retrospective study in Xiamen, China. Sci Rep. 2020;10(1):1549.
Xie C, Wang Y, Li X, Wen X. Childhood growth trajectories of etiological subgroups of large for gestational age newborns. J Pediatr. 2016;170:60-66.e61-65.
Kaul P, Bowker SL, Savu A, Yeung RO, Donovan LE, Ryan EA. Association between maternal diabetes, being large for gestational age and breast-feeding on being overweight or obese in childhood. Diabetologia. 2019;62(2):249–58.
Kaseva N, Vääräsmäki M, Matinolli HM, Sipola-Leppänen M, Tikanmäki M, Heinonen K, Lano A, Wolke D, Andersson S, Järvelin MR, et al. Pre-pregnancy overweight or obesity and gestational diabetes as predictors of body composition in offspring twenty years later: evidence from two birth cohort studies. Int J Obes (Lond). 2018;42(4):872–9.
Farias DR, Poston L, Franco-Sena AB, Moura da Silva AA, Pinto T, de Oliveira LC, Kac G. Maternal lipids and leptin concentrations are associated with large-for-gestational-age births: a prospective cohort study. Sci Rep. 2017;7(1):804.
Chiavaroli V, Marcovecchio ML, de Giorgis T, Diesse L, Chiarelli F, Mohn A. Progression of cardio-metabolic risk factors in subjects born small and large for gestational age. PLoS One. 2014;9(8):e104278.
Heerwagen MJ, Miller MR, Barbour LA, Friedman JE. Maternal obesity and fetal metabolic programming: a fertile epigenetic soil. Am J Physiol Regul Integr Comp Physiol. 2010;299(3):R711-722.
Grissom NM, Reyes TM. Gestational overgrowth and undergrowth affect neurodevelopment: similarities and differences from behavior to epigenetics. Int J Dev Neurosci. 2013;31(6):406–14.
Lin XH, Wu DD, Gao L, Zhang JY, Pan HT, Wang H, Li C, Zhang P, Guo MX, Wu YT, et al. Altered DNA methylation in neonates born large-for-gestational-age is associated with cardiometabolic risk in children. Oncotarget. 2016;7(52):86511–21.
Sewell MF, Huston-Presley L, Super DM, Catalano P. Increased neonatal fat mass, not lean body mass, is associated with maternal obesity. Am J Obstet Gynecol. 2006;195(4):1100–3.
Loaiza S, Atalah E. Birth weight and obesity risk at first grade of high school in a non-concurrent cohort of Chilean children. Public Health Nutr. 2013;16(2):228–32.
Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365(20):1876–85.
Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357(23):2329–37.
Wang X, Liang L, Junfen FU, Lizhong DU. Metabolic syndrome in obese children born large for gestational age. Indian J Pediatr. 2007;74(6):561–5.
Maguolo A, Olivieri F, Zusi C, Miraglia Del Giudice E, Morandi A, Maffeis C. The risk of metabolic derangements is higher in children and adolescents with overweight or obesity born small for gestational age. Nutr Metab Cardiovasc Dis. 2021;31(6):1903–10.
Nordman H, Voutilainen R, Antikainen L, Jääskeläinen J. Prepubertal children born large for gestational age have lower serum DHEAS concentrations than those with a lower birth weight. Pediatr Res. 2017;82(2):285–9.
Srinivasan SR, Myers L, Berenson GS. Temporal association between obesity and hyperinsulinemia in children, adolescents, and young adults: the Bogalusa Heart Study. Metabolism. 1999;48(7):928–34.
Rönnemaa T, Knip M, Lautala P, Viikari J, Uhari M, Leino A, Kaprio EA, Salo MK, Dahl M, Nuutinen EM, et al. Serum insulin and other cardiovascular risk indicators in children, adolescents and young adults. Ann Med. 1991;23(1):67–72.
Reinehr T, Kiess W, Kapellen T, Andler W. Insulin sensitivity among obese children and adolescents, according to degree of weight loss. Pediatrics. 2004;114(6):1569–73.
Dearden L, Bouret SG, Ozanne SE. Sex and gender differences in developmental programming of metabolism. Mol Metab. 2018;15:8–19.
Wisniewski AB, Chernausek SD. Gender in childhood obesity: family environment, hormones, and genes. Gend Med. 2009;6(Suppl 1):76–85.
Pocobelli G, Dublin S, Enquobahrie DA, Mueller BA. Birth weight and birth weight for gestational age in relation to risk of hospitalization with primary hypertension in children and young adults. Matern Child Health J. 2016;20(7):1415–23.
Kuciene R, Dulskiene V, Medzioniene J. Associations between high birth weight, being large for gestational age, and high blood pressure among adolescents: a cross-sectional study. Eur J Nutr. 2018;57(1):373–81.
Yiu V, Buka S, Zurakowski D, McCormick M, Brenner B, Jabs K. Relationship between birthweight and blood pressure in childhood. Am J Kidney Dis. 1999;33(2):253–60.
Hong YH, Lee JE. Large for gestational age and obesity-related comorbidities. J Obes Metab Syndr. 2021;30(2):124–31.
Acknowledgements
We sincerely thank all participants for participating in this study.
Funding
This study was supported by the National Natural Science Foundation of China (82171692); CAMS Innovation Fund for Medical Sciences(2021-I2M-5-001), Shandong Provincial Natural Science Foundation (ZR2022JQ33); National Special Support Program for High-level Talents, and Taishan Scholars Program for Young Experts of Shandong Province (tsqn201909195).
Author information
Authors and Affiliations
Contributions
LC contributed to the study concept and design. YZ, KD, and XC analyzed data and drafted the paper. Zi-JC contributed to the review and revision of the manuscript. All authors approved the final submitted and published versions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All parents provided signed informed consent and the study was approved by the ethics committee at the Center for Reproductive Medicine, Shandong Provincial Hospital affiliated to Shandong University. Ethics number: [2014] Lun Shen Zi (17) No.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12916_2024_3419_MOESM3_ESM.docx
Additional file 3: Tab. S1. Children Characteristics, Parental Characteristics, and Family Socioeconomic Status in Included and Non-included Singleton Children Conceived from ART.
12916_2024_3419_MOESM5_ESM.docx
Additional file 5: Tab. S3. Measures of Anthropometry, Metabolic Markers of Offspring Born AGA, or LGA which Stratified by Children’s Gender.
12916_2024_3419_MOESM7_ESM.docx
Additional file 7: Tab. S4. Measures of Anthropometry, Metabolic Markers of Offspring Born AGA, or LGA which Stratified by whether Embryos are Frozen.
12916_2024_3419_MOESM8_ESM.docx
Additional file 8: Tab. S5. Measures of Anthropometry, Metabolic Markers of Offspring Born AGA, or LGA in Children Whose Mother without Obesity, Gestational Diabetes Mellitus, and Hyperlipidemia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Y., Dai, K., Chen, X. et al. Association between being large for gestational age and cardiovascular metabolic health in children conceived from assisted reproductive technology: a prospective cohort study. BMC Med 22, 203 (2024). https://doi.org/10.1186/s12916-024-03419-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03419-7