Abstract
Background
Experiences during childhood and adolescence have enduring impacts on physical and mental well-being, overall quality of life, and socioeconomic status throughout one’s lifetime. This underscores the importance of prioritizing the health of children and adolescents to establish an impactful healthcare system that benefits both individuals and society. It is crucial for healthcare providers and policymakers to examine the relationship between COVID-19 and the health of children and adolescents, as this understanding will guide the creation of interventions and policies for the long-term management of the virus.
Methods
In this umbrella review (PROSPERO ID: CRD42023401106), systematic reviews were identified from the Cochrane Database of Systematic Reviews; EMBASE (OvidSP); and MEDLINE (OvidSP) from December 2019 to February 2023. Pairwise and single-arm meta-analyses were extracted from the included systematic reviews. The methodological quality appraisal was completed using the AMSTAR-2 tool. Single-arm meta-analyses were re-presented under six domains associated with COVID-19 condition. Pairwise meta-analyses were classified into five domains according to the evidence classification criteria. Rosenberg’s FSN was calculated for both binary and continuous measures.
Results
We identified 1551 single-arm and 301 pairwise meta-analyses from 124 systematic reviews that met our predefined criteria for inclusion. The focus of the meta-analytical evidence was predominantly on the physical outcomes of COVID-19, encompassing both single-arm and pairwise study designs. However, the quality of evidence and methodological rigor were suboptimal. Based on the evidence gathered from single-arm meta-analyses, we constructed an illustrative representation of the disease severity, clinical manifestations, laboratory and radiological findings, treatments, and outcomes from 2020 to 2022. Additionally, we discovered 17 instances of strong or highly suggestive pairwise meta-analytical evidence concerning long-COVID, pediatric comorbidity, COVID-19 vaccines, mental health, and depression.
Conclusions
The findings of our study advocate for the implementation of surveillance systems to track health consequences associated with COVID-19 and the establishment of multidisciplinary collaborative rehabilitation programs for affected younger populations. In future research endeavors, it is important to prioritize the investigation of non-physical outcomes to bridge the gap between research findings and clinical application in this field.
Similar content being viewed by others
Background
The coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been spreading globally for more than 3 years [1, 2]. As of April 20, 2023, there have been over 765 million confirmed cases and over 6.9 million deaths reported worldwide [3]. COVID-19 has had varied effects on the health of children and adolescents, both directly and indirectly. COVID-19 infection can cause symptoms and impact the physical health of young people, affecting multiple organ systems directly [4,5,6]. Additionally, the policies implemented during the pandemic, as well as the preventive measures aimed at reducing the direct impact of COVID-19, often give rise to indirect consequences for children and adolescents. These indirect effects of COVID-19 have a disruptive impact on routine healthcare services and social interactions, which can further exacerbate mental and cognitive health challenges and worsen existing health disparities among this vulnerable population [7, 8]. Child and adolescent health refer to the physical, mental/cognitive, quality of life, and social well-being, of individuals from newborns until the age of 19. Experiences during childhood and adolescence have enduring impacts on physical and mental health, quality of life, and socioeconomic status over the lifespan [9]. Consequently, exploring the subsequent effects of COVID-19 on the health of children and adolescents has the potential to influence the future provision and design of comprehensive services for those affected by COVID‐19. By gaining insights into an individual’s informational, spiritual, psychological, social, and physical requirements during follow-up phases, personalized services can be developed to enhance the survivor experience. This endeavor plays a vital role in establishing a resilient and prosperous healthcare system that benefits both individuals and society.
Currently, the World Health Organization (WHO) has declared that the global health emergency caused by COVID-19 has ended. This highlights the need to transition from an emergency response to the long-term management of COVID-19 and other infectious diseases [10, 11]. Even after the emergency phase concludes, the ongoing transmission and emergence of new COVID-19 variants, as well as the remaining unvaccinated younger individuals and the significant global impact on health inequity, societal consequences, and economic repercussions, collectively emphasize the importance of continually assessing the available evidence on the correlation between COVID-19 and the health of children and adolescents. This assessment will inform stakeholders, including patients, healthcare providers, and policymakers, to mitigate conflicting effects and prioritize resources, interventions, and policies.
During the first year of the pandemic, a study analyzed all 6338 pediatric emergency admissions in England related to COVID-19 and found that adolescents have a higher likelihood of being hospitalized due to COVID-19 compared to younger children [12]. Surveys conducted among 13,002 American and 11,681 Chinese adolescents showed a similar 1-year prevalence of clinically significant depressive and anxiety symptoms during the COVID-19 pandemic [13, 14]. These nationally representative studies, conducted with large sample sizes, are commonly regarded as robust evidence to establish a link between COVID-19 and child and adolescent health across diverse domains and time periods. However, the changing public health policies of COVID-19 and the emergence of new viral strains could introduce complexities and inconsistencies in the overall evidence [15, 16]. In addition, many primary studies examining the relationship between COVID-19 and the health of children and adolescents used convenience sampling, including cross-sectional and observational designs that lacked control or comparison groups. The meta-analytical estimates from these studies may not accurately represent the true effects of the disease, as they are prone to biases such as measurement errors, poor control of confounders, biased participant selection, and data publication issues, ultimately weakening the strength of the aggregated scientific evidence [17]. The emergence of meta-analytical evidence through rapid reviews, compared to formal systematic reviews, further complicates this issue due to inadequate reporting of evidence, limited literature search, and increased publication bias [18].
The umbrella review, which involves quantifying systematic reviews and meta-analyses, provides a comprehensive assessment that captures the most extensive and high-quality medical evidence available [19]. By utilizing umbrella reviews, studies have reported evidence on the characteristic features of COVID-19 in children and adolescents during the initial phase of the pandemic [20], as well as the epidemiological impact and associations with mental health problems among this demographic [21, 22]. Although these studies to some extent synthesized evidence on various factors influencing pediatric health outcomes during the COVID-19 pandemic, they fell short of providing a comprehensive perspective on the diverse array of health and well-being outcomes among children and adolescents. Moreover, the conclusions drawn from these umbrella reviews lack an assessment based on evidence grading criteria, neglecting the systematic grading of the evidence obtained from studies. This oversight regarding the overall strength of evidence could potentially limit the credibility of the conclusions presented in umbrella reviews. Therefore, this study aims to conduct an umbrella review to evaluate the strength of meta-analytic estimates and summarize the current evidence linking direct and indirect impacts of COVID-19 to the health/well-being of children and adolescents. Furthermore, we intend to explore the potential impact of future research on the conclusions drawn from existing significant meta-analyses.
Methods
Protocol and reporting
The protocol of this umbrella review was prospectively defined and registered on the PROSPERO [23] website (ID: CRD42023401106) (https://www.crd.york.ac.uk/PROSPERO/). The differences between registered protocol and review were provided in Additional file 1. This review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) 2020 statement guidelines and a PRISMA checklist is included (Additional file 2) [24].
Study search and selection
We performed a comprehensive systematic literature search without any restrictions on the date or language of publication. Three key electronic databases including the Cochrane Database of Systematic Reviews (CDSR) via The Cochrane Library; EMBASE (OvidSP) and MEDLINE (OvidSP) were searched from December 2019 to February 2023. Moreover, the Google Scholar and WHO database of publications on COVID-19 and reference lists of included studies were also searched manually to identify reports of additional studies. We merged keywords and subject headings appropriately for each database using the following search terms: (COVID-19 [MeSH] OR 2019-nCoV.m.p. OR SARS-CoV-2.m.p. OR novel coronavirus pneumonia.m.p.) AND (pediatrics [MeSH] OR pediatrics.m.p. OR neonate.m.p. OR children.m.p. OR adolescence.m.p. OR teenagers.m.p.) AND (meta-analysis [MeSH] OR systematic review.m.p.) (Additional file 3). Two independent authors (C.D. and T.W.) carried out the electronic database search and decided the final inclusion according to the following criteria: (1) systematic reviews with meta-analysis; (2) results from children and adolescents between 0 and 19 years old; (3) observing COVID-19 as the exposure. Full texts were obtained and independently assessed for eligibility if certain studies seemed to have any potentiality for inclusion if they could not be judged completely by titles and abstracts. Any disagreements were settled by consulting a third review author (L.L.). Observational studies, intervention studies, other types of reviews (descriptive, scoping), program evaluations, animal studies, conference abstracts, and letters/comments were excluded from the review.
Data extraction
Two independent reviewers (C.D. and L.L.) screened the titles and abstracts, assigning unique identification numbers to all the included articles. Two authors (C.D. and T.W.) independently extracted the necessary data from each eligible review through a pre-designed extraction table and resolved any disagreements by discussion with a third reviewer (L.L.). Pooled estimates, including prevalence, odds ratio (OR), relative risk (RR), hazard ratio (HR), and standard mean difference (SMD), were extracted from each systematic review for all eligible health and well-being outcomes. The pre-designed extraction table included study identification (authors, year, and origin country), number of studies and participants included in the meta-analysis, outcome domain (physical, psychological/cognitive, quality of life, social, and health system), direct or indirect impact(s), COVID-19 condition(s) being assessed, health and well-being condition(s) of children and adolescents being assessed, methodological quality tool used, effect size and 95% CI, heterogeneity (I2 statistic), and publication bias assessment. We defined the “direct effects” as the consequences that directly correlate with COVID-19 infection or transmission, specifically within outcome domains. On the other hand, the “indirect effects” encompassed the broader consequences that arise from the pandemic, as well as the public health or political regulations associated with it. Furthermore, two senior researchers (Z.J. and G.W.), specializing in epidemiology and disease prevention, critically reviewed both the methodology and the coding results.
To address missing data, we initially reached out to the authors of the meta-analytical studies in an attempt to acquire the missing information directly from the original research teams. If the pooled estimates were not provided and no response was received from the authors, the entire row of data was excluded without any further statistical transformations [25]. In cases where the statistical significance of the combined effect in the meta-analysis was determined using Z-tests but did not include reported P-values, we calculated the corresponding P-values based on the respective Z-value [26]. All data domains were verified to be free of missing values through the aforementioned processes.
Methodological quality appraisal, evidence grading, and presentation
Methodological quality of the systematic review will be made using the A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR-2) [27] tool by two examiners (C.D. and T.W.). In this sense, systematic reviews are categorized as: High (Zero or one non-critical weakness); Moderate (More than one non-critical weakness); Low (One critical flaw with or without non-critical weaknesses); and Critically Low (More than one critical flaw with or without non-critical weaknesses).
For pairwise meta-analytical evidence, statistical quality was assessed by applying the previously published evidence grading protocol [28, 29]. Significant associations shown in meta-analyses were categorized into four evidence levels: strong, highly suggestive, suggestive, and weak evidence. Strong evidence was considered if all the following criteria were met: > 1000 cases included in the meta-analysis; a P-value ≤ 10−6 of statistical significance in valid meta-analysis; heterogeneity (I2) below 50%; the null value was excluded by the 95% prediction interval; and no evidence of small study effects and excess significance bias. Highly suggestive evidence was set if meta-analyses with > 1000 cases; a random effects P-value ≤ 10−6, and the largest study in the meta-analysis was statistically significant. Suggestive evidence was defined if meta-analyses with > 1000 cases, random effects P-value ≤ 10−3 were categorized. If the latter conditions were not verified, the meta-analysis was classified as weak evidence. The classifications were subgrouped based on health domains, and the results were tabulated accordingly: the main focus of interest for this study encompassed the direct and indirect impacts associated with COVID-19, which included physical, psychological/cognitive, quality of life, and social impacts. The data was compared by considering the evidence grade and subgroups, and various methods such as counting and clustering were employed.
For single-arm meta-analytical evidence, six pre-defined COVID-19 condition domains were created: laboratory-confirmed COVID-19, COVID-19-associated MIS-C, newborns from COVID-19-diagnosed mothers, long-COVID, events caused by the COVID-19 vaccine, and health impacts during the pandemic. The domain of newborns from COVID-19 diagnosed mothers is exclusively limited to infants. The remaining domains, however, encompass children and adolescents aged 0–19 years old. Summarizations were conducted under each domain using all relevant meta-analytical evidence regardless of topic overlap to present and describe the current body of systematic review evidence on impacts of COVID-19 on children and adolescents. The most meta-analytical evidence was centered around laboratory-confirmed COVID-19. It is important to acknowledge that data on patient disease presentations collected during the early stages of the COVID-19 pandemic may differ significantly from those observed in later phases. Nonetheless, the effect summaries and publication years of original meta-analyses may not accurately capture these variations. To examine the changing trends in the occurrence rates of various symptoms during the pandemic, taking into account viral strain evolution and diverse health interventions, we conducted additional reanalysis of primary studies in this domain. Specifically, we screened and extracted relevant information from the primary studies included in each systematic review, including details of the authors, data collection years, outcome indicators, number of events, and sample sizes. Subsequently, we removed duplicated evidence and reanalyzed the primary data reported for at least 2 years within the meta-analytical evidence. To account for heterogeneity among the included studies, a random effects model was used to combine the primary data outcomes if Q < 0.05 or I2 > 50% [30]. Alternatively, a fixed-effects model was applied to pool outcomes if these criteria were not met [30, 31].
We adhered to the presentation guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions to effectively present our current work [25]. To present pairwise meta-analytical evidence, we initially employed the “summarizing outcome data” [25] strategy. This strategy enabled us to systematically summarize the meta-analyzed data, along with the previously mentioned quality assessments, without considering any overlap in study topics. By doing so, we were able to provide a comprehensive overview of the current body of evidence from systematic reviews on the study topic. To present single-arm meta-analytical evidence, we also utilized the “summarizing outcome data” strategy to offer a comprehensive perspective on the available evidence. Additionally, we conducted a “reanalyzing outcome data” [25] specifically for primary studies of laboratory-confirmed COVID-19. This reanalysis aided in the elimination of duplicated primary studies and standardized the collection years of data. As a result, we achieved a more coherent and consistent presentation of disease severity, clinical manifestations, laboratory and radiological findings, treatments, and outcomes associated with laboratory-confirmed COVID-19 across different years.
Calculations of FSN
The Rosenberg’s FSN is the number of missing studies averaging a z-value of zero that should be added to make the combined effect size statistically insignificant. For statistically significant meta-analytic evidence, Rosenberg’s FSN was calculated using the workbook “Meta-Essentials” [32] for binary and continuous measures.
Data handling and processing
All the data were collected using MS Office 365. Data processing and statistical analysis were conducted in the R programming environment (version 4.1.0). The “bibliometrix” package (version 4.1.2) was employed to perform bibliometric analysis on the included studies, following its standard analyzing protocol [33]. The “meta” package (version 6.2.1) was used for statistical transformation and reanalysis of the primary studies from single-arm meta-analytical evidence [34]. To visualize the reanalyzed data, the “forestploter” package (version 1.1.2) was utilized (https://github.com/cran/forestploter). Data table formatting and cleaning were achieved through the utilization of the “tidyverse” (version 1.3.1) and “reshape2” packages (version 1.4.4) [35, 36].
Results
Selection and characteristics of the included meta-analyses
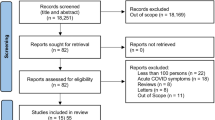
We retrieved a total of 1100 records from databases and registers (Fig. 1). After removing duplicates (n = 87), the title and abstract of 1013 records were screened against including criteria, and 814 records were excluded. Cohen’s kappa coefficient for title and abstract screening was 0.97 (95% CI 0.95–0.99). The full-text analysis was conducted on the remaining 199 records, 76 records were excluded, and 1 additional record was added through citation searching of reference lists. The list of excluded studies with reasons for exclusion is detailed in Additional file 4. Cohen’s kappa coefficient for full-text screening was 0.93 (95% CI 0.86–0.94), confirming excellent inter-examiner reliability. Ultimately, 124 systematic reviews with meta-analyses were included for data extraction and further analysis (Additional file 5) [4, 6, 20, 37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157]. Cohen’s kappa coefficient for data extraction was 0.90 (95% CI 0.89–0.91).
All the included systematic reviews were published in 2020–2023. There was an increased trend of publishing relevant systematic reviews (Fig. 2a). The top 15 most cited journals in the field of interest are shown in Fig. 2b, in which 5 journals are multidisciplinary, 7 journals are focusing on pediatrics, and 3 journals are focusing on infectious disease and virology. Based on the number and relationship of publications in each country, a collaborative network was constructed and visualized (Fig. 2c). China, the USA, Australia, India, and the UK shared most collaborations.
Most included studies adhered to PRISMA guidelines (n = 99, 78.6%), followed by Meta-analyses of Observational Studies in Epidemiology (MOOSE) guidelines (n = 12, 9.5%) or a combination of multiple reporting guidelines (n = 9, 7.1%). However, a small portion of studies (n = 7, 7.9%) did not report following any systematic review reporting guidelines. To assess methodological quality, the Newcastle–Ottawa Scale (NOS) was used in most studies (n = 36, 28.6%), followed by the National Institutes of Health (NIH) Quality Assessment Tool (n = 14, 11.1%) and Joanna Briggs Institute (JBI) tools (n = 13, 10.3%).
In addition to encompassing the field of neonates for COVID19-diagnosed mothers, other domains include children and adolescents aged 0–19 years. We also explicitly indicate the age group sources of the relevant evidence for each subset within these domains. The descriptive characteristics of included meta-analyses under five major outcome domains (physical, psychological/cognitive, quality of life, social, and health system) are summarized in Tables 1 and 2. For pre-defined COVID-19 condition domains, the six domains were not evenly distributed: most topics focused on laboratory-confirmed infections (n = 60; 48.4%), followed by health impacts during the pandemic (n = 21; 16.9%), adverse events (AEs) caused by the COVID-19 vaccine (n = 20; 16.1%), COVID-19 associated multisystem inflammatory syndrome (MIS-C) (n = 15; 12.1%), newborns from diagnosed mothers (n = 6; 4.8%), and long-COVID (n = 2; 1.6%).
Methodological quality assessment
The Cohen kappa score for the AMSTAR-2 assessments was 0.89 (95% CI 0.83–0.91). No meta-analysis gained high overall confidence for methodological quality, 1 with moderate (0.8%), 18 studies were scored as low quality (14.5%), and 105 studies presented as critically low quality (84.7%) (Additional file 6). For critical flaws, most studies did not report a list of excluded studies and justify the exclusions (n = 116, 93.5%). In addition, inadequate accounting for the risk of bias (RoB) in primary studies when interpreting/discussing the results (n = 92, 74.2%), lacking report review methods as a priori (n = 60, 48.4%), and neglecting publication bias analysis during conducting relevant meta-analyses (n = 22, 17.7%) were also evident critical flaws. Most included studies have non-critical flaws such as lacking reports on the sources of funding (n = 115, 92.7%), inadequate assessment of the impact of individual RoB when performing evidence synthesis (n = 105, 84.7%), inadequate discussion of heterogeneity (n = 80), and lacking statements of the study designs for inclusion (n = 50, 40.3%).
COVID-19-related evidence from single-arm meta-analyses
In total, 1551 meta-analytical comparisons were included in this umbrella review. These single-armed meta-analyses commonly utilized prevalence as effect size (n = 1464; 94.4%). Figures 3 and 4 present a comprehensive overview based on the reanalysis of primary data (Additional file 7) on the disease severity, clinical manifestations, laboratory and radiological findings, treatments, and outcomes related to laboratory-confirmed COVID-19.
Forest plot for laboratory findings, radiological findings, treatment, and outcomes associated with single-arm meta-analytical evidence of laboratory-confirmed COVID-19. Data are presented as effect size (ES) with 95% confidence intervals (CI). SAA serum amyloid A, PCT procalcitonin, LDH lactate dehydrogenase, LFTs liver function tests, CK-MB creatine kinase-MB, IL-6 interleukin-6, ALT alanine transaminase, BNP brain natriuretic peptide, CRP C-reactive protein, AST aspartate aminotransferase, CT computed tomography, ECMO extracorporeal membrane oxygenation, ICU intensive care unit, NA not available
Disease severity
In the past 3 years, mild symptoms consistently remained the primary manifestation of the disease, with a prevalence of approximately 50%. In contrast, the prevalence of severe and critical symptoms consistently stayed below 15% over the same period, showing a declining trend year by year. Notably, there was an upward trend in the prevalence of asymptomatic cases. In 2020, the percentage was 29.0% (95% CI 24.0–33.0%), which increased to 34.0% (95% CI 28.0–39.0%) in 2021, and further increased to 45.0% (95% CI 21.0–69.0%) in 2022.
Clinical manifestations
Fever consistently emerged as the most frequently reported symptom over the past 3 years, with a prevalence close to 50%. Concurrently, respiratory symptoms, primarily cough, also sustained a prevalence exceeding 30% throughout this period. Noteworthy patterns emerged in 2020, indicating a higher incidence of hematologic symptoms such as anemia, lymphocytosis, lymphocytopenia, neutropenia, thrombocytopenia, and thrombocytosis, with prevalence rates ranging from 22 to 46%. Subsequent observations in 2021 revealed a more frequent occurrence of low oxygen saturation (46%, 95% CI 23.0–70.0%) compared to preceding years. However, conjunctivitis (50.0%, 95% CI 31.0–69.0%) and rhinorrhea (32.0%, 95% CI 0–80.0%) appeared to be more prevalent in 2022. Conversely, cardiovascular and neurologic symptoms exhibited considerably lower combined prevalence rates of 4.0% (95% CI 0–9.0%) and 3.0% (95% CI 1.0–5.0%), respectively.
Laboratory findings
Most laboratory results were reported in studies conducted between 2020 and 2021. In 2020, there seemed to be a more pronounced prevalence of abnormal laboratory markers, with abnormalities observed in fibrinogen, troponin, ferritin, SAA, BNP, ESR, and albumin, each surpassing 40%. Contrastingly, by 2021, the prevalence of albumin, troponin, BNP, and SAA abnormalities did not exceed 6%. In 2022, abnormalities in D-dimer, PCT, and LDH became more prevalent, surpassing the threshold of 40%.
Radiological findings
In 2021 and 2022, normal CT scans and lung chest radiographs exhibited a high prevalence of 65.0% (CI 52.0–77.0%) and 54.0% (CI 35.0–72.0%), respectively, surpassing the prevalence of 38.0% (CI 30.0–47.0%) observed in 2020. Abnormal imaging findings such as bilateral pneumonia lesions, unilateral pneumonia lesions, and multiple lung lobe lesions were notably prevalent in 2020, exceeding 30% prevalence, which markedly decreased in the subsequent 2 years.
COVID-19-related treatments
During the 3-year duration, antibiotics emerged as a common treatment for COVID-19 in youths. However, therapies such as anticoagulation, antiviral medications, glucocorticoids, and intravenous immunoglobulin were sparingly utilized, each with a prevalence not exceeding 37.0%. The use of oxygen therapy exhibited an increasing trend, reaching 39.0% (CI 9.0–70.0%) in 2022. Conversely, mechanical ventilation was predominantly employed in 2020, with a prevalence of 15.0% (95% CI 11.0–19.0%), which notably decreased to 3.0% (95% CI 1.0–5.0%) by 2022.
COVID-19-related outcomes
Reported outcomes and prognoses for COVID-19 patients among youths consistently show relatively high rates of recovery and discharge. Additionally, a declining trend in the prevalence of ICU admissions and mortality has been observed year by year. Merely 3% (CI 0–6%) of cases necessitated ICU admission, and there were no reported mortalities in 2022.
Additional File 8 provides further details on COVID-19-related evidence obtained from single-arm meta-analyses. Additional file 9 [40, 69, 75, 97, 108, 109, 117, 122, 123, 132, 137] summarizes single-arm evidence about COVID-19-associated MIS-C. Additional file 10 [62, 156, 157] summarizes single-arm evidence about newborns from COVID-19-diagnosed mothers. Additional file 11 [47, 87] summarizes single-arm evidence about long-COVID. Additional file 12 [54, 67, 77, 139, 153] summarizes single-arm evidence about events caused by the COVID-19 vaccine. Additional file 13 [49, 50, 58, 82, 99, 113, 142] summarizes single-arm evidence about health impacts during the pandemic.
COVID-19-related evidence from pairwise meta-analyses
Three hundred one meta-analytic comparisons from 47 pairwise systematic reviews were analyzed. Out of these, only 1.7% (n = 5) were considered to have strong meta-analytical evidence, while 4.0% (n = 12) and 8.0% (n = 24) were categorized as highly suggestive and suggestive evidence respectively (Table 2). A stricter P-value threshold revealed that 8.9% (n = 27) and 7.3% (n = 22) of the meta-analyses had significance at 10−3 and 10−6. The remaining 39.9% (n = 120) were statistically significant (p < 0.05). In terms of heterogeneity, approximately 49.2% (n = 148) of the included meta-analyses had high heterogeneity (I2 > 50%), while 29.6% (n = 89) presented low heterogeneity (I2 ≤ 25%).
A total of 176 meta-analyses (58.4%) explored the direct impact of COVID-19 on children and adolescents. The existing evidence base is largely skewed in favor of a biomedical evaluation of health outcomes in COVID-19-infected individuals, focusing primarily on physical outcomes and suggesting an increased risk of impaired health (Fig. 5). Only one had strong meta-analytical evidence: long COVID-19 impact on physical outcomes (n = 1), while pediatric comorbidities presented highly suggestive evidence of impacting COVID-19 severity (n = 2). In addition, suggestive evidence was found on the effect of long-COVID (n = 1) as well as survival and associated complications (n = 1) on physical outcomes. Furthermore, transmission and risks for COVID-19 in children present suggestive evidence on both physical (n = 1) and social (n = 1) outcomes. A total of 84 meta-analyses indicated weak evidence, leaving 85 meta-analyses with no statistically significant results.
Evidence grading on direct effects of COVID-19 on physical, psychological/cognitive, quality of life, social, and health system domains. The right side illustrates associations that elevate the risk for the respective health condition (in red), while the left side demonstrates associations that lower the risk (in green). COVID coronavirus disease, MIS-C multisystem inflammatory syndrome in children, ICU intensive care unit
The COVID-19 pandemic’s indirect impacts on children and adolescents were reported in 125 meta-analyses (41.6%). Existing evidence tends to show an increased health risk for children and adolescents, particularly in physical, psychological, and quality of life outcomes. Specifically, among these meta-analyses, two were categorized as having strong evidence (Fig. 6), indicating an elevated risk of depression (n = 1) and weight gain (n = 1). Five meta-analyses presented highly suggestive evidence, associating the increased risk with myopia progression (n = 2), depression (n = 2), and mental health issues (n = 1). The population examined in the meta-analysis, which yielded highly suggestive evidence regarding mental health issues, consisted of children aged 5 to 13 years. In terms of health system outcomes, an additional meta-analysis offered highly suggestive evidence, highlighting an increased risk of asthma-related hospitalization during the COVID-19 pandemic. A further twenty meta-analyses had suggestive evidence, ten of which pertained to associations that already received strong or highly suggestive evidence. The remaining ten meta-analyses showed an increased risk in outcomes, including complicated appendicitis (n = 2), neurodevelopmental impairment (n = 1), pediatric new-onset type 1 diabetes and diabetic ketoacidosis (n = 2), pregnancy and neonatal outcomes (n = 1), sleep quality (n = 2), and physical activity decline (n = 1). A total of 53 meta-analyses were supported by weak evidence, while the remaining 48 meta-analyses did not have nominally statistically significant findings. Additionally, the health system outcomes section notably emphasized evidence concerning the effectiveness and safety of COVID-19 vaccines. Two more meta-analyses focusing on the effectiveness of COVID-19 vaccines (n = 2) were categorized as having strong evidence (Fig. 6). Four other meta-analyses presented highly suggestive evidence, reporting the effectiveness (n = 3) and safety (n = 1) of COVID-19 vaccines. The meta-analysis that provided highly suggestive evidence regarding the effectiveness of COVID-19 vaccines focused on a study population comprising children aged 5 to 11 years.
Evidence grading on indirect effects of COVID-19 on physical, psychological/cognitive, quality of life, social, and health system domains. The right side illustrates associations that elevate the risk for the respective health condition (in red), while the left side demonstrates associations that lower the risk (in green). COVID coronavirus disease
Number of additional studies needed to change current pairwise meta-analytic evidence
For strong evidence, the median fail-safe number (FSN) was 8 (range 4–25). For highly suggestive and suggestive evidence the median FSN were 13 (range 4–158) and 11 (range 1–163), respectively. The FSN in 73.2% of these studies (n = 30) were higher than the number of studies included in the meta-analyses, meaning that adding studies in the future is unlikely to change the robustness of the statistical significance for these metanalytic evidence. For weak evidence, the median FSN was 11 (range 1–2569), and only 37.8% of studies (n = 48) had FSN higher than the number of studies included in the meta-analyses.
Discussion
Main findings from the single-arm meta-analytical evidence
Single-arm meta-analyses have provided extensive evidence on the prevalence and estimations across six domains associated with COVID-19 condition. These domains include laboratory-confirmed COVID-19, COVID-19-associated MIS-C, newborns from COVID-19-diagnosed mothers, long-COVID, events caused by the COVID-19 vaccine, and health impacts during the pandemic.
In this umbrella review, we specifically focus on laboratory-confirmed COVID-19 infections. Through reanalyzing the primary studies from these meta-analyses by removing overlapping data and remapping the actual data collection year, we investigated the distinct clinical characteristics, management, and outcomes of children and adolescents with COVID-19 infections from 2020 to 2022. Clinical manifestations among children exhibited variability over the years, illustrating a diverse range of features. More than half of these manifestations demonstrated a downward trend over time. Our analysis illustrates prevailing patterns in prevalence, indicating an increase in asymptomatic cases and a decrease in other severity levels of cases. In terms of COVID-19-related outcomes, there was a decrease in both admissions to the intensive care unit (ICU) and mortality rates over the years, while the number of discharged and recovered cases remained relatively stable. Interestingly, hospitalization rates rebounded in 2022, potentially attributed to the emergence and spread of novel COVID-19 strains with immune escape mechanisms [158]. COVID-19-related MIS-C is characterized by recurring high fever, damage to multiple organs, heightened inflammatory indicators, and frequent severe outcomes. Newborns from mothers diagnosed with COVID-19 generally experienced mild symptoms and had a low risk of vertical transmission, although adverse health outcomes were still possible. Furthermore, our findings suggest that children and adolescents affected by long-COVID commonly report symptoms such as fatigue, dyspnea, sore throat, mood changes, and sleep disorders. For events caused by COVID-19 vaccines, we observed that AEs were more frequently reported following booster doses compared to earlier doses. Solicited local and systemic AEs were also found to be common across all doses. Lastly, regarding the domain of pandemic lockdown, our findings reveal a significant correlation between social isolation and adverse effects on the mental health, sleep habits, and physical activity of children and adolescents.
Main findings from the pairwise meta-analytical evidence
Among the pairwise meta-analyses, we observed strong evidence for five effects and highly suggestive evidence for 12 effects. These results were supported by highly significant findings. Based on the available evidence, we have classified the strong and highly suggestive evidence into three primary categories: (i) the direct effects of COVID-19 infection on children’s health, (ii) the indirect impacts of the COVID-19 pandemic on children’s well-being, and (iii) the efficacy and safety of COVID-19 vaccines. The direct effect is demonstrated by a higher risk of severe COVID-19 in children with comorbidities and persistent negative health challenges resulting from long-COVID. Several factors can explain the manifestations linked with long-COVID, including persistent acute organ damage, the presence of the virus in the body, and the activation of autoimmune mechanisms that target both the COVID-19 virus and host tissues [159]. Moreover, the indirect effects of COVID-19 had strong correlations with significant economic disruptions, increased social isolation, mental health challenges, and a shift towards remote work and online activities for children and adolescents [160]. Our study revealed that these indirect impacts are manifested in increased anxiety and depression levels, accelerated myopia progression, as well as significant increases in body weight and BMI during the COVID-19 pandemic home quarantine. The effectiveness and safety of COVID-19 vaccines have been confirmed to a certain extent, although several potential AEs have been reported.
Similarities and disparities of the previous and current studies
In our study, we investigated and presented evidence of the negative physical correlations observed in individuals with long-COVID. Previous umbrella reviews, which primarily focused on adults, have examined the long-term consequences experienced by COVID-19 survivors beyond the acute phase. However, these evaluations were limited by the absence of graded evidence [161, 162]. In contrast, our study pooled single-arm meta-analyses specifically on long-COVID in children and adolescents, demonstrating similar outcomes. Nonetheless, it is important to note that these findings did not achieve high-level evidence ranking like those obtained through pairwise meta-analysis. This limitation can be attributed to the constraints imposed by the study design and sample size, which were influenced by limited time, resources, and evolving understanding of long-term consequences associated with acute COVID-19 [17]. The management of individuals with post-COVID conditions presents significant challenges due to the diverse range of symptoms, unpredictable duration, and absence of definitive risk factors. Furthermore, the symptoms of long-COVID can manifest in various combinations from patient to patient, with fluctuations in both frequency and severity. This dynamic nature adds an extra layer of complexity to the issue of long-COVID.
This umbrella review offered a comprehensive analysis of the correlation between the COVID-19 pandemic and the mental health of children and adolescents. Similar to previous umbrella reviews, we observed differing impacts regarding various mental health issues among this demographic. However, the methodological approaches of these umbrella reviews varied considerably. Due to significant heterogeneity in the methods and outcomes of the reviews included, some lead to a narrative synthesis presentation and an omission in evidence grading [21, 163]. One umbrella review [164] conducted a reanalysis of systematic reviews to re-examine data from preliminary studies captured within each systematic review, aiming to reduce potential biases that could have previously impacted the assessment of mental health during the pandemic. Despite the absence of evidence grading, the insights provided by this evidence remain significant. It is also important to acknowledge that disentangling the direct impact of the pandemic on the mental health of children and adolescents remains challenging due to the complexity of mental health disorders. Additionally, the implementation of bundled mitigation strategies at national or subnational levels complicates the identification of individual strategies that may have contributed to exacerbated mental health effects. To sum up, the integration of our current findings with previous studies has the potential to substantially enhance policymaking and practice in the field of mental and child health, thereby guiding future research endeavors to strengthen the global knowledge base.
Mechanisms and implications from current evidence
The gradual reduction of health risk of COVID-19 in children and adolescents
The health risk of COVID-19 in children and adolescents appears to decrease gradually over time. Our research also indicates a rise in the number of asymptomatic cases among children over the years, alongside a decline in ICU admissions and mortality rates. These trends may be attributed to a globally prevalent variant strain during the period when the data included in the study was collected. With the ongoing pandemic, the Omicron variant (B.1.1.529) emerged as the dominant strain during that time, surpassing Delta in its transmission rate [165]. Additionally, the Omicron variant has demonstrated a lower rate of hospitalization, ICU admission, invasive mechanical ventilation (IMV), and in-hospital deaths, along with a higher prevalence of asymptomatic cases compared to the Delta variant [166, 167]. These observations suggest that the Omicron variant may have reduced pathogenicity and milder symptoms than previous variants. Our findings indicate that the most frequently reported symptoms are fever and cough, which aligns with the previous umbrella reviews not limited by age [20]. However, our study discovered a higher incidence of conjunctivitis in 2022, with a rate of 48.4%. This symptom is considered rare, as its prevalence among positive cases typically ranges from 0.8 to 31.6% [168]. Our findings indicate that the most frequently reported symptoms are fever and cough, which aligns with the previous umbrella reviews not limited by age [20]. However, our study discovered a higher incidence of conjunctivitis in 2022, with a rate of 48.4%. This symptom is considered rare, as its prevalence among positive cases typically ranges from 0.8 to 31.6% [168]. It has been established that frequency of hand-eye contact presents as an independent risk factor for COVID-19-related conjunctivitis [169].
Another key finding in our study is the lower health risk of COVID-19 for children and adolescents when compared to adults. The current umbrella review provides ample evidence to support the notion that most children and adolescents infected with COVID-19 exhibit mild or even asymptomatic symptoms. During the Omicron epidemic, the proportion of asymptomatic cases across all age groups was 33.72% in 2022 and 23.57% in 2021, both of which indicate a lower proportion of asymptomatic cases among adults compared to our reported findings [170]. Umbrella reviews without age limitations often overlook the critical role of age in influencing both COVID-19 susceptibility and disease severity [171]. The relative susceptibility among children and adolescents aged 0–19 years was also notably lower, ranging from 6 to 16% compared to adult groups, with the rate of critical illness in adults being 4.95 times higher than that in children [172]. However, the reasons behind this phenomenon remain incompletely understood, despite available data suggesting similar viral loads in both children and adults at the time of presentation [173]. Several hypotheses have been proposed to explain the disparity in COVID-19 severity between younger and older individuals, including more efficient local tissue responses [174], better thymic function [175], and cross-reactive immunity [176]. Currently, the prevailing viewpoint suggests that the lower incidence and severity of COVID-19 disease in infants can be explained by maternal immune transfer [177], an immature immune system [178], and reduced expression of COVID-19 attachment receptors such as ACE-2 [179]. However, there is also evidence suggesting that maternal COVID-19 may impact the neonatal immune system, potentially leading to an exacerbated inflammatory response and immune activation [180]. Consequently, the programming of the neonatal immune system by the maternal inflammatory milieu induced by COVID-19 remains uncertain.
From the perspective of childhood growth evolution, recent evidence suggests that the body’s energy allocation often avoids costly systemic inflammatory responses [181]. By prioritizing disease tolerance rather than maximal resistance, children are more likely to experience mild or even asymptomatic illness. However, this approach may result in a lower efficiency in clearing viruses, which could lead to some degree of viral persistence and the subsequent manifestation of other diseases associated with such persistence. Therefore, personalized treatments tailored to the severity of the disease should be implemented for pediatric patients, along with thorough long-term monitoring and follow-up care. Furthermore, our findings indicate that dysautonomia often presents symptoms commonly associated with long-COVID. However, whether dysautonomia is a direct consequence of COVID-19 infection or an immune-mediated process remains unclear [182]. Although current evidence suggests that long-COVID has a relatively milder health impact on pediatric patients compared to adults, the life course implications, including psychological, social, and economic impacts, are not fully revealed by current evidence and require more extensive long-term follow-up studies [183]. Insufficient lifecycle observations limit the evidence of the impact of long-COVID on pediatric patients, requiring caution when interpreting the relatively lower impact on this group. Nevertheless, school closure and social distancing measures may further compromise the social well-being of children with long-COVID symptoms [184]. It is crucial to implement social policies that promote the return to school and participation in extracurricular activities among young individuals to address specific risk factors like obesity associated with long-COVID. Additionally, this can help mitigate the negative cultural impact and psychological consequences caused by remote learning [184, 185].
The immune microenvironment, physiological and psychological factors, and social activities contribute to disparities in disease susceptibility among children and adolescents at different developmental stages [186, 187]. Previous literature has reported a higher susceptibility to severe COVID-19 and increased hospital admissions among pediatric patients aged ≤ 4 years or 12–17 years, indicating a bimodal age distribution [188]. Our research shows that serious consequences such as dyspnea, ICU admission, and death have also been observed and cannot be ignored, although a lower health risk of COVID-19 for children and adolescents due to uncommon vertical transmission during neonatal admission from infected mothers was observed.
However, at the umbrella review level, the current available primary and meta-analytical evidence has limited the evaluation process of COVID-19’s impact on age-specific subgroups of children and adolescents. Most of the included evidence has focused on the 0–19 age group as a whole [4, 6, 20, 37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151], with only a few studies examining specific age ranges. For example, Yasuhara J’s study included children and adolescents aged 12–19 years [152], while Watanabe A’s study included children aged 5–11 years [153], without direct comparison to other age-specific subgroups. The lack of age-specific research and comparisons poses challenges for subgroup analyses across various age groups, excluding neonatal groups that are typically distinguished in the literature and technically feasible to evaluate [154,155,156,157]. Therefore, our main analysis includes the 0–19 age group, with a separate domain for newborns from COVID-19-diagnosed mothers, to demonstrate the impact of COVID-19 on children and adolescents at different developmental stages.
The mental health risks of COVID-19-related social isolation on children and adolescents
Over the past 3 years, significant efforts have been made to control the spread of COVID-19 through various interventions, such as social distancing, mobility restrictions, and school closures. Nevertheless, these measures may have unintended and detrimental effects on the mental health of children and adolescents [189, 190]. The present umbrella review provides evidence supporting the idea that the pandemic has resulted in an increased burden of mental health concerns among this population, including conditions like depression and sleep disorders. These findings are consistent with previous research studies [21, 22]. However, their report indicated a pooled prevalence rate of 32% for depression (95% CI 27–38%) and 32% for anxiety (95% CI 27–37%) among children and adolescents worldwide following COVID-19 mitigation measures, which was lower than our findings. This suggests that the deterioration of mental health in the younger population during the pandemic may not solely be attributed to indirect impacts during the gradual relaxation of mandatory control measures in many countries. The underlying causes of this phenomenon may vary and encompass financial stressors [191], social isolation [192], physical health concerns [193], and heightened anxiety and fear stemming from the uncertainties of COVID-19 [194]. Therefore, it is crucial to monitor the negative impact on the mental health of children and adolescents in the future, with dedicated efforts aimed at enhancing their well-being. Policymakers and healthcare professionals should adopt a holistic approach that addresses these multifaceted issues to effectively mitigate the detrimental effects on mental health.
The safety and efficacy of vaccines for children
The present study indicates that COVID-19 vaccines effectively prevent severe illness and reduce transmission. Evidence from pooled studies in healthy children and adolescents suggests that the occurrence of AEs, including local and systemic AEs, is similar between the vaccine and placebo groups. Furthermore, serious AEs are mostly unrelated to vaccination [195]. Recent studies have also confirmed the favorable and safe response to COVID-19 vaccination among pediatric patients with inflammatory rheumatic diseases [196], endocrinological disorders [197], or inflammatory bowel disease [198], addressing concerns about potential AEs in vulnerable populations with inadequate or overactive immune responses. However, it is important to note that the evidence supporting these findings is currently limited to cross-sectional studies. Additionally, both local and systemic AEs were reported to occur slightly more frequently than in the adult population. Nonetheless, this does not suggest evidence against the vaccine’s safety, as reactogenicity is more common in young individuals than in adults [199]. Although side effects may vary depending on the person, they typically tend to be mild and temporary, similar to common childhood vaccines [200]. Based on emerging safety and efficacy data, along with increased vaccine availability, widespread vaccination is recommended, particularly for high-risk children.
COVID-19-related global policies related to children and adolescents
The impact of COVID-19-related global policies is a matter of great concern for the health and well-being of children and adolescents. The effects of policies and regulations implemented to control the COVID-19 outbreak are intricate and multifaceted. Policies that specifically target children and young people, such as school closures and healthcare restrictions, have direct consequences on their social interactions [201], education [202], and access to healthcare resources [203]. Moreover, policy decisions and measures have resulted in numerous social conflicts, further impacting the daily lives of children and adolescents. For example, children often find themselves caught in the midst of disputes between parents, friends, schoolmates, teachers, and activity leaders regarding COVID-19 measures [204]. Additionally, the social and economic repercussions of policy measures become apparent in later stages of the pandemic, underscoring the direct impact these challenges have on the everyday lives of children. As an illustration, school children from underprivileged families face multiple hurdles due to the pandemic, including financial insecurity and disparities in remote learning caused by a lack of digital devices [205]. These complex impacts make it difficult to establish a clear link between policies and child health, and limited research has focused on the long-term effects of policies on affected children. Furthermore, as COVID-19 continues to significantly impact the mental health of the general population, countries have developed and revised policies, guidelines, and new initiatives to address the psychological well-being of their citizens. These supportive policies further complicate the discussion surrounding policy impacts.
Evidence of the impact of COVID-19-related policies on children and adolescents is limited. As stated above, current meta-analytical evidence suggests that children may be less affected by certain social settings as a result of policy development, such as the reopening of schools and workplaces. However, the physical and psychological/cognitive effects of the virus may hinder a child’s ability to return to school for several weeks or months. Research on health system utilization in this area primarily focuses on medical resources, such as emergency services and ICU admissions. However, conflicting evidence exists, with only a limited number of studies available. Based on current meta-analytical data, it appears that health system utilization for life-threatening diseases and situations in younger patients is not significantly different from or may even be lower than the pre-pandemic era, except in cases involving younger patients with asthma and obesity. It is important to interpret these results cautiously since medical crowding and inadequate resources may overshadow the utilization of the health system by pediatric COVID-19 patients [206].
Strengths and weaknesses
The strengths and weaknesses of this umbrella review are quite straightforward. First, one of the strengths is that we provided a comprehensive summary of the current available evidence by reviewing previous meta-analyses on the association between COVID-19 and various health outcomes in children and adolescents. Second, our study protocol was registered in PROSPERO, ensuring transparency and robustness in the planned analysis and results. Considering the worldwide prolonged transmission and evolving nature of COVID-19, this study holds clinical and social importance in shaping preventive strategies for children and adolescents in the post-pandemic era. Next, this study utilized a systematic approach, involving thorough searching, selection, and data extraction conducted by two independent authors with excellent inter-examiner reliability. Methodological quality and evidence classification were assessed using two established criteria, AMSTAR-2 [27] and evidence grading criteria [28, 29] to assess the methodological quality and evidence classification. Without limiting study designs and statistical significance, the current umbrella review filled the knowledge gaps and captured temporal changes in key aspects of COVID-19 in children and adolescents. However, some limitations still exist in this review. Firstly, most of the meta-analyses included in this review are based on observational studies, and the prospective or randomized study designs were not prominently featured. This observational nature of the studies introduces the potential for selection bias, as differences in baseline characteristics and confounding factors can exist among the study populations [207]. Consequently, these studies only provide associations between variables and cannot account for all possible confounders or factors that may influence the results. Secondly, many studies within this topic rely on self-reported data, which can be subjective and susceptible to recall bias [208]. The use of self-reporting may lead to inconsistencies or inaccuracies in the data collected. Moreover, the absence of a comparison group in single-arm studies makes it challenging to accurately establish the effects of COVID-19 on children and adolescents. The evaluation of the impact of COVID-19 on age-specific subgroups of children and adolescents is incomplete due to the limited availability of primary and meta-analytical evidence. The lack of age-specific research and comparisons poses challenges for subgroup analyses across various developmental stages, potentially resulting in an incomplete depiction of the differential impacts of COVID-19 across different developmental stages of children and adolescents. In this current study, we chose to present all available meta-analytical data from single-arm studies and categorized them into six predefined COVID-19 condition domains [25]. This approach allows us to illustrate the main findings of COVID-19 on children and adolescents in a time-dependent manner, considering the dynamic changes in disease severity, clinical manifestations, laboratory and radiological findings, treatment, and outcomes. Although this approach has its limitations, it provides valuable insights that can inform public health measures and interventions targeted at this population. It also emphasizes the need for further controlled studies tailored to address the specific impacts of COVID-19 on children and adolescents.
Implications for practice and research
For practice, the effect estimates combined with different topic domains categorized from primary studies can help practitioners identify high-risk younger patients for COVID-19-related direct and indirect health outcomes. However, when it comes to children and adolescents with rare disease conditions, identifying high-risk groups remains a challenge. These individuals are often underrepresented in primary studies, likely due to decreased medical care utilization during the pandemic. This oversight may result in the neglect of rare disease conditions in both practice and policy decisions. Based on the complete picture of available evidence and the COVID-19 and health domains linking mechanisms, policymakers could better prioritize the prevention and intervention methods for children and adolescents affected by COVID-19 (in)directly. Connecting these individuals with appropriate support services is another key question in COVID-19 management. The effects and evidence summarized in this umbrella review suggests that such services could include medical/surgical management of physical illness and comorbidities, psychotherapy, physio and occupational therapy, and nursing. Multidisciplinary collaboration units dedicated to younger COVID-19 patients or pandemic lockdowns can be invaluable in providing tailored prevention and intervention strategies [209, 210]. Shifting the focus of COVID-19 global health emergency management to long-term management, alongside other infectious diseases, can accelerate the implementation of surveillance systems for COVID-19-related health consequences and rehabilitation programs for affected younger patients.
For research, the effect estimates in this review are heavily focused on the physical outcomes, investigating the relationship between COVID-19 and disease severity, clinical manifestations, laboratory/radiological findings, treatment, and outcomes in younger patients. Gaps still exist between available evidence in non-physical outcomes and current clinical practice. Furthermore, some meta-analytical results did not reveal significant associations with many COVID-19-related health conditions, such as the direct effects of long-COVID on the psychological/cognitive well-being and quality of life of younger patients in pairwise studies, which lead to the overall evidence consistency due to poor meta-analytic or methodological reasons. Future studies can provide a more nuanced understanding of how COVID-19 affects children and adolescents at different developmental stages by expanding the scope of research to include a wider range of age groups. This will enable the analysis of the impacts of COVID-19 on various stages of childhood and adolescence, facilitating the development of tailored interventions and guidelines specifically designed for these populations. It is important to note that this does not imply the absence of robust associations, but rather the current body of evidence does not yet support such inferences [211]. Therefore, updating and transforming this review into a living review would be valuable in incorporating emerging evidence from future meta-analytical studies on the impacts of COVID-19 on children and adolescents.
Conclusions
In summary, this work evaluated the meta-analytical evidence regarding the associations between the (in)direct COVID-19 effects and multiple health and well-being domains of children and adolescents. The findings of this study can serve as a comprehensive evidence map to inform, educate, and train various interested parties, including key stakeholders such as policymakers, patients, and practitioners. It is also important to acknowledge that the majority of the findings and recommendations presented in this study are derived from observational studies that have methodological limitations. Thus, it is crucial to exercise caution when interpreting the results and implementing the implications of this study. Additionally, future research should prioritize the execution of high-quality studies utilizing prospective, long-term, or randomized designs to more comprehensively understand the causal effects of COVID-19, both direct and indirect, on children and adolescents.
Availability of data and materials
All data generated and analyzed that support findings in this study are supplemented in the Supplementary Information. The Rscript snippets for generating descriptive summaries and reanalyzing single-arm studies are available on GitHub using the following link: https://github.com/Piperacillin/Child_COVID19_Umbrellareview.
Abbreviations
- AEs:
-
Adverse events
- AMSTAR-2:
-
A Measurement Tool to Assess Systematic Reviews 2
- COVID-19:
-
Coronavirus disease 2019
- CRP:
-
C-reactive protein
- JBI:
-
Joanna Briggs Institute
- LDH:
-
Serum lactate dehydrogenase
- MIS-C:
-
Multisystem inflammatory syndrome
- MOOSE:
-
Meta-analyses of Observational Studies in Epidemiology
- NIH:
-
National Institutes of Health
- NOS:
-
Newcastle-Ottawa Scale
- PCT:
-
Procalcitonin
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses
- RoB:
-
Risk of bias
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- WBC:
-
White blood cell
- WHO:
-
World Health Organization
References
Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med. 2020;8(7):659–61.
Chow EJ, Uyeki TM, Chu HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol. 2023;21(3):195–210.
COVID-19 weekly epidemiological update, edition 139, 2023 [https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---20-april-2023]
Sumner MW, Kanngiesser A, Lotfali-Khani K, Lodha N, Lorenzetti D, Funk AL, Freedman SB. Severe outcomes associated with SARS-CoV-2 infection in children: a systematic review and meta-analysis. Front Pediatr. 2022;10:916655.
Yoon S, Li H, Lee KH, Hong SH, Kim D, Im H, Rah W, Kim E, Cha S, Yang J, et al. Clinical characteristics of asymptomatic and symptomatic pediatric Coronavirus disease 2019 (COVID-19): a systematic review. Medicina (Kaunas). 2020;56(9):474.
Zhao Y, Yin L, Patel J, Tang L, Huang Y. The inflammatory markers of multisystem inflammatory syndrome in children (MIS-C) and adolescents associated with COVID-19: a meta-analysis. J Med Virol. 2021;93(7):4358–69.
Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;17(22):8479.
Djurdjević S, Ghigliazza IC, Dukanac V, Djurdjević A. Anxiety and depressive symptomatology among children and adolescents exposed to the COVID-19 pandemic–a systematic review. Vojnosanit Pregl. 2022;79(4):389–99.
Goodman A, Joyce R, Smith JP. The long shadow cast by childhood physical and mental problems on adult life. Proc Natl Acad Sci U S A. 2011;108(15):6032–7.
Sosin AN, Choo E, Lincoln M. The covid public health emergency is ending: it now joins the ordinary emergency that is American health. BMJ. 2023;381:949.
Wise J. Covid-19: WHO declares end of global health emergency. BMJ. 2023;381:1041.
Ward JL, Harwood R, Smith C, Kenny S, Clark M, Davis PJ, Draper ES, Hargreaves D, Ladhani S, Linney M, et al. Risk factors for PICU admission and death among children and young people hospitalized with COVID-19 and PIMS-TS in England during the first pandemic year. Nat Med. 2022;28(1):193–200.
Cao Y, Huang L, Si T, Wang NQ, Qu M, Zhang XY. The role of only-child status in the psychological impact of COVID-19 on mental health of Chinese adolescents. J Affect Disord. 2021;282:316–21.
McGuine TA, Biese KM, Petrovska L, Hetzel SJ, Reardon C, Kliethermes S, Bell DR, Brooks A, Watson AM. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19-related school closures and sport cancellations: a study of 13 000 athletes. J Athl Train. 2021;56(1):11–9.
Wagner CE, Saad-Roy CM, Grenfell BT. Modelling vaccination strategies for COVID-19. Nat Rev Immunol. 2022;22(3):139–41.
Mostafiz MI, Musteen M, Saiyed A, Ahsan M. COVID-19 and the global value chain: Immediate dynamics and long-term restructuring in the garment industry. J Bus Res. 2022;139:1588–603.
Cucherat M, Laporte S, Delaitre O, Behier JM, participants of Giens XRTCR, d’Andon A, Binlich F, Bureau S, Cornu C, Fouret C, et al. From single-arm studies to externally controlled studies Methodological considerations and guidelines. Therapie. 2020;75(1):21–7.
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, Perrier L, Hutton B, Moher D, Straus SE. A scoping review of rapid review methods. BMC Med. 2015;13:224.
Papatheodorou S. Umbrella reviews: what they are and why we need them. Eur J Epidemiol. 2019;34:543–6.
Shah K, Upadhyaya M, Kandre Y, Pandya A, Saraf V, Saxena D, Mavalankar D. Epidemiological, clinical and biomarker profile of pediatric patients infected with COVID-19. QJM. 2021;114(7):476–95.
Hossain MM, Nesa F, Das J, Aggad R, Tasnim S, Bairwa M, Ma P, Ramirez G. Global burden of mental health problems among children and adolescents during COVID-19 pandemic: an umbrella review. Psychiatry Res. 2022;317:114814.
Harrison L, Carducci B, Klein JD, Bhutta ZA. Indirect effects of COVID-19 on child and adolescent mental health: an overview of systematic reviews. BMJ Glob Health. 2022;7(12):e010713.
Schiavo JH. PROSPERO: an international register of systematic review protocols. Med Ref Serv Q. 2019;38(2):171–80.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane; 2023. Available from www.training.cochrane.org/handbook.
Lin J-T. Approximating the normal tail probability and its inverse for use on a pocket calculator. Appl Stat. 1989;38(1):69–70.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Huang Y, Chen Z, Chen B, Li J, Yuan X, Li J, Wang W, Dai T, Chen H, Wang Y, et al. Dietary sugar consumption and health: umbrella review. BMJ. 2023;381:e071609.
Papadimitriou N, Markozannes G, Kanellopoulou A, Critselis E, Alhardan S, Karafousia V, Kasimis JC, Katsaraki C, Papadopoulou A, Zografou M. An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites. Nat Commun. 2021;12(1):4579.
Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206.
Huang Y, Cao D, Chen Z, Chen B, Li J, Wang R, Guo J, Dong Q, Liu C, Wei Q, et al. Iron intake and multiple health outcomes: umbrella review. Crit Rev Food Sci Nutr. 2023;63(16):2910–27.
Suurmond R, van Rhee H, Hak T. Introduction, comparison, and validation of meta-essentials: a free and simple tool for meta-analysis. Res Synth Methods. 2017;8(4):537–53.
Aria M, Cuccurullo C. bibliometrix : an R-tool for comprehensive science mapping analysis. J Informetr. 2017;11(4):959–75.
Balduzzi S, Rucker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60.
Wickham H, Averick M, Bryan J, Chang W, McGowan L, François R, Grolemund G, Hayes A, Henry L, Hester J, et al. Welcome to the tidyverse. J Open Source Softw. 2019;4(43):1686.
Wickham H. Reshaping data with thereshapepackage. J Stat Softw. 2007;21(12):1–20.
Akobeng AK, Grafton-Clarke C, Abdelgadir I, Twum-Barimah E, Gordon M. Gastrointestinal manifestations of COVID-19 in children: a systematic review and meta-analysis. Front Gastroenterol. 2021;12(4):332–7.
Alhumaid S, Alabdulqader M, Al Dossary N, Al Alawi Z, Alnaim AA, Al Mutared KM, Al Noaim K, Al Ghamdi MA, Albahrani SJ, Alahmari AA, et al. Global coinfections with bacteria, fungi, and respiratory viruses in children with SARS-CoV-2: a systematic review and meta-analysis. Trop Med Infect Dis. 2022;7(11):380.
Amanati A, Vali M, Fatemian H, Maleki Z, Foroozand H, Sahebi K, Rahmanian MR, Meybodi MJE. A comprehensive comparison of COVID-19 characteristics (Wuhan Strain) between children and adults during initial pandemic phase: a meta-analysis study. Arch Pediatr Infect. 2022;10(4):e119701.
Arantes Junior MAF, Conegundes AF, Branco Miranda BC, Radicchi Campos ASR, Franca Vieira AL, Faleiro MD, Campos MA, Kroon EG, Bentes AA. Cardiac manifestations in children with the multisystem inflammatory syndrome (MIS-C) associated with SARS-CoV-2 infection: systematic review and meta-analysis. Rev Med Virol. 2023;33:e2432.
Assaker R, Colas AE, Julien-Marsollier F, Bruneau B, Marsac L, Greff B, Tri N, Fait C, Brasher C, Dahmani S. Presenting symptoms of COVID-19 in children: a meta-analysis of published studies. Br J Anaesth. 2020;125(3):e330–2.
Badal S, Thapa Bajgain K, Badal S, Thapa R, Bajgain BB, Santana MJ. Prevalence, clinical characteristics, and outcomes of pediatric COVID-19: a systematic review and meta-analysis. J Clin Virol. 2021;135:104715.
Behnood SA, Shafran R, Bennett SD, Zhang AXD, O’Mahoney LL, Stephenson TJ, Ladhani SN, De Stavola BL, Viner RM, Swann OV. Persistent symptoms following SARS-CoV-2 infection amongst children and young people: a meta-analysis of controlled and uncontrolled studies. J Infect. 2022;84(2):158–70.
Bhuiyan MU, Stiboy E, Hassan MZ, Chan M, Islam MS, Haider N, Jaffe A, Homaira N. Epidemiology of COVID-19 infection in young children under five years: a systematic review and meta-analysis. Vaccine. 2021;39(4):667–77.
Bolia R, Dhanesh Goel A, Badkur M, Jain V. Gastrointestinal manifestations of pediatric Coronavirus disease and their relationship with a severe clinical course: a systematic review and meta-analysis. J Trop Pediatr. 2021;67(2):fmab051.
Bussieres EL, Malboeuf-Hurtubise C, Meilleur A, Mastine T, Herault E, Chadi N, Montreuil M, Genereux M, Camden C, Team P-C. Consequences of the COVID-19 pandemic on children’s mental health: a meta-analysis. Front Psychiatry. 2021;12:691659.
Campos C, Prokopich S, Loewen H, Sanchez-Ramirez DC. Long-term effect of COVID-19 on lung imaging and function, cardiorespiratory symptoms, fatigue, exercise capacity, and functional capacity in children and adolescents: a systematic review and meta-analysis. Healthc (Basel). 2022;10(12):2492.
Carmona CA, Kuziez M, Freitas CF, Cyrus JW, Bain J, Karam O. Cardiac manifestations of multisystem inflammatory syndrome of children after SARS-CoV-2 infection: a systematic review and meta-analysis. Cardiol Young. 2023;33(11):1–9.
Chaabna K, Chaabane S, Jithesh A, Doraiswamy S, Mamtani R, Cheema S. Effect of the COVID-19 pandemic on the proportion of physically active children and adults worldwide: a systematic review and meta-analysis. Front Public Health. 2022;10:1009703.
Chai J, Xu H, An N, Zhang P, Liu F, He S, Hu N, Xiao X, Cui Y, Li Y. The prevalence of mental problems for Chinese children and adolescents during COVID-19 in China: a systematic review and meta-analysis. Front Pediatr. 2021;9:661796.
Chang TH, Chen YC, Chen WY, Chen CY, Hsu WY, Chou Y, Chang YH. Weight gain associated with COVID-19 lockdown in children and adolescents: a systematic review and meta-analysis. Nutrients. 2021;13(10):3668.
Chang TH, Wu JL, Chang LY. Clinical characteristics and diagnostic challenges of pediatric COVID-19: A systematic review and meta-analysis. J Formos Med Assoc. 2020;119(5):982–9.
Chen J, Yang K, Cao Y, Du Y, Wang N, Qu M. Depressive symptoms among children and adolescents in China during the Coronavirus disease-19 epidemic: a systematic review and meta-analysis. Front Psychiatry. 2022;13:870346.
Chou OHI, Mui J, Chung CT, Radford D, Ranjithkumar S, Evbayekha E, Nam R, Pay L, Satti DI, Garcia-Zamora S, et al. COVID-19 vaccination and carditis in children and adolescents: a systematic review and meta-analysis. Clin Res Cardiol. 2022;111(10):1161–73.
Cui X, Zhai Y, Wang S, Ding K, Yang Z, Tian Y, Huo T. Effect of the COVID-19 pandemic on serum vitamin D levels in people under age 18 years: a systematic review and meta-analysis. Med Sci Monit. 2022;28:e935823.
Dara N, Hosseini A, Sayyari AA, Gaman M-A, Fatahi S. Gastrointestinal manifestations and dynamics of liver enzymes in children and adolescents with COVID-19 infection: a systematic review and meta-analysis. Iran J Pediatr. 2020;30(5):1–9.
de Medeiros KS, Sarmento ACA, Costa APF, Macedo LTA, da Silva LAS, de Freitas CL, Simoes ACZ, Goncalves AK. Consequences and implications of the coronavirus disease (COVID-19) on pregnancy and newborns: a comprehensive systematic review and meta-analysis. Int J Gynaecol Obstet. 2022;156(3):394–405.
Deng J, Zhou F, Hou W, Heybati K, Lohit S, Abbas U, Silver Z, Wong CY, Chang O, Huang E, et al. Prevalence of mental health symptoms in children and adolescents during the COVID-19 pandemic: a meta-analysis. Ann N Y Acad Sci. 2023;1520(1):53–73.
Di Toro F, Gjoka M, Di Lorenzo G, De Santo D, De Seta F, Maso G, Risso FM, Romano F, Wiesenfeld U, Levi-D’Ancona R, et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(1):36–46.
Ding Y, Yan H, Guo W. Clinical characteristics of children with COVID-19: a meta-analysis. Front Pediatr. 2020;8:431.
Du Y, Chen L, Shi Y. Safety, immunogenicity, and efficacy of COVID-19 vaccines in adolescents, children, and infants: a systematic review and meta-analysis. Front Public Health. 2022;10:829176.
Dubey P, Reddy SY, Manuel S, Dwivedi AK. Maternal and neonatal characteristics and outcomes among COVID-19 infected women: an updated systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020;252:490–501.
El-Qushayri AE, Benmelouka AY, Dahy A, Hashan MR. COVID-19 outcomes in paediatric cancer: A large scale pooled meta-analysis of 984 cancer patients. Rev Med Virol. 2022;32(5):e2344.
Elgenidy A, Awad AK, Saad K, Atef M, El-Leithy HH, Obiedallah AA, Hammad EM, Ahmad FA, Ali AM, Dailah HG, et al. Incidence of diabetic ketoacidosis during COVID-19 pandemic: a meta-analysis of 124,597 children with diabetes. Pediatr Res. 2023;93(5):1149–60.
Gabriel IWM, Lima DGS, Pires JP, Vieira NB, Brasil A, Pereira YTG, de Oliveira EG, de Menezes HL, Lima NNR, Reis AOA, et al. Impacts of COVID-19 on children and adolescents: a systematic review analyzing its psychiatric effects. World J Psychiatry. 2022;12(11):1313–22.
Gao P, Cai S, Liu Q, Du M, Liu J, Liu M. Effectiveness and safety of SARS-CoV-2 vaccines among children and adolescents: a systematic review and meta-analysis. Vaccines (Basel). 2022;10(3):421.
Gao P, Kang LY, Liu J, Liu M. Immunogenicity, effectiveness, and safety of COVID-19 vaccines among children and adolescents aged 2–18 years: an updated systematic review and meta-analysis. World J Pediatr. 2023;19(11):1041–54.
Gaythorpe KAM, Bhatia S, Mangal T, Unwin HJT, Imai N, Cuomo-Dannenburg G, Walters CE, Jauneikaite E, Bayley H, Kont MD, et al. Children’s role in the COVID-19 pandemic: a systematic review of early surveillance data on susceptibility, severity, and transmissibility. Sci Rep. 2021;11(1):13903.
Haghighi Aski B, Manafi Anari A, Abolhasan Choobdar F, Zareh Mahmoudabadi R, Sakhaei M. Cardiac abnormalities due to multisystem inflammatory syndrome temporally associated with Covid-19 among children: a systematic review and meta-analysis. Int J Cardiol Heart Vasc. 2021;33:100764.
Han Y, Chen Y, Sun C, Zhou Z. The impact of COVID lockdown on glycaemic control in paediatric patients with type 1 diabetes: a systematic review and meta-analysis of 22 observational studies. Front Endocrinol (Lausanne). 2022;13:1069559.
Henry BM, Benoit SW, de Oliveira MHS, Hsieh WC, Benoit J, Ballout RA, Plebani M, Lippi G. Laboratory abnormalities in children with mild and severe coronavirus disease 2019 (COVID-19): A pooled analysis and review. Clin Biochem. 2020;81:1–8.
Hessami K, Norooznezhad AH, Monteiro S, Barrozo ER, Abdolmaleki AS, Arian SE, Zargarzadeh N, Shekerdemian LS, Aagaard KM, Shamshirsaz AA. COVID-19 pandemic and infant neurodevelopmental Impairment: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(10):e2238941.
Irfan O, Li J, Tang K, Wang Z, Bhutta ZA. Risk of infection and transmission of SARS-CoV-2 among children and adolescents in households, communities and educational settings: A systematic review and meta-analysis. J Glob Health. 2021;11:05013.
Irfan O, Muttalib F, Tang K, Jiang L, Lassi ZS, Bhutta Z. Clinical characteristics, treatment and outcomes of paediatric COVID-19: a systematic review and meta-analysis. Arch Dis Child. 2021;106(5):440–8.
Jiang L, Tang K, Irfan O, Li X, Zhang E, Bhutta Z. Epidemiology, clinical features, and outcomes of Multisystem Inflammatory Syndrome in Children (MIS-C) and adolescents-a live systematic review and meta-analysis. Curr Pediatr Rep. 2022;10(2):19–30.
Kandiah T, Li X, MacMillan Y, Malvankar-Mehta MS. Access to pediatric eye care during a pandemic: systematic review and meta-analysis. Pediatr Ann. 2023;52(2):e68–75.
Katoto P, Brand AS, Byamungu LN, Tamuzi JL, Mahwire TC, Kitenge MK, Wiysonge CS, Gray G. Safety of COVID-19 Pfizer-BioNtech (BNT162b2) mRNA vaccination in adolescents aged 12–17 years: a systematic review and meta-analysis. Hum Vaccin Immunother. 2022;18(6):2144039.
Kharoud HK, Asim R, Siegel L, Chahal L, Singh GD: Review of clinical characteristics and laboratory findings of COVID-19 in children-Systematic review and Meta-analysis. medRxiv 2020, https://doi.org/10.1101/2020.09.23.20200410. (Accessed Feb 15,2024)
Kim JH, Ahn C. A meta-analysis of testicular torsion and orchiectomy in pediatric patients during the COVID-19 pandemic. J Pediatr Surg. 2022;57(8):1708–9.
Kumar J, Meena J, Yadav A, Yadav J. Radiological findings of COVID-19 in children: a systematic review and meta-analysis. J Trop Pediatr. 2021;67(3):fmaa045.
La Fauci G, Montalti M, Di Valerio Z, Gori D, Salomoni MG, Salussolia A, Solda G, Guaraldi F. Obesity and COVID-19 in children and adolescents: reciprocal detrimental influence-systematic literature review and meta-analysis. Int J Environ Res Public Health. 2022;19(13):7603.
Lee H, Kim E. Global prevalence of physical and psychological child abuse during COVID-19: a systematic review and meta-analysis. Child Abuse Negl. 2023;135:105984.
Li B, Zhang S, Zhang R, Chen X, Wang Y, Zhu C. Epidemiological and clinical characteristics of COVID-19 in children: a systematic review and meta-analysis. Front Pediatr. 2020;8:591132.
Li M, Wang X, Feng J, Feng Z, Li W, Ya B. Myocarditis or Pericarditis following the COVID-19 vaccination in adolescents: a systematic review. Vaccines (Basel). 2022;10(8):1316.
Liu C, He Y, Liu L, Li F, Shi Y. Children with COVID-19 behaving milder may challenge the public policies: a systematic review and meta-analysis. BMC Pediatr. 2020;20(1):410.
Lo TC, Chen YY. Ocular and systemic manifestations in paediatric multisystem inflammatory syndrome associated with COVID-19. J Clin Med. 2021;10(13):2953.
Lopez-Leon S, Wegman-Ostrosky T, Ayuzo Del Valle NC, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, Villapol S. Long-COVID in children and adolescents: a systematic review and meta-analyses. Sci Rep. 2022;12(1):9950.
Ludwig-Walz H, Dannheim I, Pfadenhauer LM, Fegert JM, Bujard M. Increase of depression among children and adolescents after the onset of the COVID-19 pandemic in Europe: a systematic review and meta-analysis. Child Adolesc Psychiatry Ment Health. 2022;16(1):109.
Ma L, Mazidi M, Li K, Li Y, Chen S, Kirwan R, Zhou H, Yan N, Rahman A, Wang W, et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;293:78–89.
Ma X, Liu S, Chen L, Zhuang L, Zhang J, Xin Y. The clinical characteristics of pediatric inpatients with SARS-CoV-2 infection: a meta-analysis and systematic review. J Med Virol. 2021;93(1):234–40.
Madigan S, Eirich R, Pador P, McArthur BA, Neville RD. Assessment of changes in child and adolescent screen time during the COVID-19 pandemic: a systematic review and meta-analysis. JAMA Pediatr. 2022;176(12):1188–98.
Mansourian M, Ghandi Y, Habibi D, Mehrabi S. COVID-19 infection in children: a systematic review and meta-analysis of clinical features and laboratory findings. Arch Pediatr. 2021;28(3):242–8.
Mantovani A, Rinaldi E, Zusi C, Beatrice G, Saccomani MD, Dalbeni A. Coronavirus disease 2019 (COVID-19) in children and/or adolescents: a meta-analysis. Pediatr Res. 2021;89(4):733–7.
Meena J, Yadav J, Saini L, Yadav A, Kumar J. Clinical features and outcome of SARS-CoV-2 infection in children: a systematic review and meta-analysis. Indian Pediatr. 2020;57(9):820–6.
Mongkonsritragoon W, Prueksapraoprong C, Kewcharoen J, Tokavanich N, Prasitlumkum N, Huang J, Poowuttikul P. Prevalence and risk associated with asthma in children hospitalized with SARS-CoV-2: a meta-analysis and systematic review. J Allergy Clin Immunol Pract. 2022;10(5):1382-1384.e1381.
Navolokina A, Smereka J, Bottiger BW, Pruc M, Juarez-Vela R, Rahnama-Hezavah M, Rafique Z, Peacock FW, Safiejko K, Szarpak L. The impact of COVID-19 on pediatric cardiac arrest outcomes: a systematic review and meta-analysis. Int J Environ Res Public Health. 2023;20(2):1104.
Nepal G, Shrestha GS, Rehrig JH, Gajurel BP, Ojha R, Agrawal A, Panthi S, Khatri B, Adhikari I. Neurological manifestations of COVID-19 associated multi-system inflammatory syndrome in children: a systematic review and meta-analysis. J Nepal Health Res Counc. 2021;19(1):10–8.
Nino G, Zember J, Sanchez-Jacob R, Gutierrez MJ, Sharma K, Linguraru MG. Pediatric lung imaging features of COVID-19: a systematic review and meta-analysis. Pediatr Pulmonol. 2021;56(1):252–63.
Panda PK, Gupta J, Chowdhury SR, Kumar R, Meena AK, Madaan P, Sharawat IK, Gulati S. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J Trop Pediatr. 2021;67(1):fmaa122.
Panda PK, Sharawat IK, Panda P, Natarajan V, Bhakat R, Dawman L. Neurological complications of SARS-CoV-2 infection in children: a systematic review and meta-analysis. J Trop Pediatr. 2021;67(3):070.
Pogorelic Z, Anand S, Artukovic L, Krishnan N. Comparison of the outcomes of testicular torsion among children presenting during the Coronavirus Disease 2019 (COVID-19) pandemic versus the pre-pandemic period: a systematic review and meta-analysis. J Pediatr Urol. 2022;18(2):202–9.
Pogorelic Z, Anand S, Zuvela T, Singh A, Krizanac Z, Krishnan N. Incidence of complicated appendicitis during the COVID-19 pandemic versus the pre-pandemic period: a systematic review and meta-analysis of 2782 pediatric Appendectomies. Diagnostics (Basel). 2022;12(1):127.
Qi K, Zeng W, Ye M, Zheng L, Song C, Hu S, Duan C, Wei Y, Peng J, Zhang W, et al. Clinical, laboratory, and imaging features of pediatric COVID-19: a systematic review and meta-analysis. Medicine (Baltimore). 2021;100(15):e25230.
Raccanello D, Rocca E, Vicentini G, Brondino M. Eighteen months of COVID-19 pandemic through the lenses of self or others: a meta-analysis on children and adolescents’ mental health. Child Youth Care Forum. 2022;52:1–24.
Rahmati M, Keshvari M, Mirnasuri S, Yon DK, Lee SW, Il Shin J, Smith L. The global impact of COVID-19 pandemic on the incidence of pediatric new-onset type 1 diabetes and ketoacidosis: a systematic review and meta-analysis. J Med Virol. 2022;94(11):5112–27.
Raschetti R, Vivanti AJ, Vauloup-Fellous C, Loi B, Benachi A, De Luca D. Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat Commun. 2020;11(1):5164.
Richter SA, Ferraz-Rodrigues C, Schilling LB, Camargo NF, Nunes ML. Effects of the COVID-19 pandemic on sleep quality in children and adolescents: a systematic review and meta-analysis. J Sleep Res. 2023;32(1):e13720.
Rodriguez-Gonzalez M, Castellano-Martinez A, Cascales-Poyatos HM, Perez-Reviriego AA. Cardiovascular impact of COVID-19 with a focus on children: a systematic review. World J Clin Cases. 2020;8(21):5250–83.
Ruvinsky S, Voto C, Roel M, Fustinana A, Veliz N, Brizuela M, Rodriguez S, Ulloa-Gutierrez R, Bardach A. Multisystem inflammatory syndrome temporally related to COVID-19 in children from Latin America and the Caribbean Region: a systematic review with a meta-analysis of data from regional surveillance systems. Front Pediatr. 2022;10:881765.
Sabu JM, Zahid I, Jacob N, Alele FO, Malau-Aduli BS. Effectiveness of the BNT162b2 (Pfizer-BioNTech) vaccine in children and adolescents: a systematic review and meta-analysis. Vaccines (Basel). 2022;10(11):1880.
Shah K, Varna VP, Pandya A, Saxena D. Low vitamin D levels and prognosis in a COVID-19 pediatric population: a systematic review. QJM. 2021;114(7):447–53.
Sharma D, Bhaskar SMM. Prevalence of paediatric hyperinflammatory conditions in paediatric and adolescent hospitalized COVID-19 patients: a systematic review and meta-analysis. APMIS. 2022;130(2):101–10.
Sharma M, Aggarwal S, Madaan P, Saini L, Bhutani M. Impact of COVID-19 pandemic on sleep in children and adolescents: a systematic review and meta-analysis. Sleep Med. 2021;84:259–67.
Shi Q, Wang Z, Liu J, Wang X, Zhou Q, Li Q, Yu Y, Luo Z, Liu E, Chen Y, et al. Risk factors for poor prognosis in children and adolescents with COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021;41:101155.
Silverberg SL, Zhang BY, Li SNJ, Burgert C, Shulha HP, Kitchin V, Sauvé L, Sadarangani M. Child transmission of SARS-CoV-2: a systematic review and meta-analysis. BMC Pediatr. 2022;22(1):172.
Smith ER, Oakley E, Grandner GW, Ferguson K, Farooq F, Afshar Y, Ahlberg M, Ahmadzia H, Akelo V, Aldrovandi G, et al. Adverse maternal, fetal, and newborn outcomes among pregnant women with SARS-CoV-2 infection: an individual participant data meta-analysis. BMJ Glob Health. 2023;8(1):009495.
Sood M, Sharma S, Sood I, Sharma K, Kaushik A. Emerging evidence on multisystem inflammatory syndrome in children associated with SARS-CoV-2 infection: a systematic review with meta-analysis. SN Compr Clin Med. 2021;3(1):38–47.
Taheri L, Gheiasi SF, Taher M, Basirinezhad MH, Shaikh ZA, Dehghan Nayeri N. Clinical features of COVID-19 in newborns, infants, and children: a systematic review and meta-analysis. Compr Child Adolesc Nurs. 2022;45(2):137–55.
Tang Y, Dang X, Lv M, Norris SL, Chen Y, Ren L, Liu E. Changes in the prevalence of respiratory pathogens in children due to the COVID-19 pandemic: a systematic review and meta-analysis. J Infect. 2023;86(2):154–225.
Tian Y, Chen L, Shi Y. Safety, efficacy, and immunogenicity of varying types of COVID-19 vaccines in children younger than 18 years: an update of systematic review and meta-analysis. Vaccines (Basel). 2022;11(1):87.
Toba N, Gupta S, Ali AY, ElSaban M, Khamis AH, Ho SB, Popatia R. COVID-19 under 19: a meta-analysis. Pediatr Pulmonol. 2021;56(6):1332–41.
Toraih EA, Hussein MH, Elshazli RM, Kline A, Munshi R, Sultana N, Taghavi S, Killackey M, Duchesne J, Fawzy MS, et al. Multisystem inflammatory syndrome in pediatric COVID-19 patients: a meta-analysis. World J Pediatr. 2021;17(2):141–51.
Tripathi AK, Pilania RK, Bhatt GC, Atlani M, Kumar A, Malik S. Acute kidney injury following multisystem inflammatory syndrome associated with SARS-CoV-2 infection in children: a systematic review and meta-analysis. Pediatr Nephrol. 2023;38(2):357–70.
Tsankov BK, Allaire JM, Irvine MA, Lopez AA, Sauve LJ, Vallance BA, Jacobson K. Severe COVID-19 infection and pediatric comorbidities: a systematic review and meta-Analysis. Int J Infect Dis. 2021;103:246–56.
Viner R, Waddington C, Mytton O, Booy R, Cruz J, Ward J, Ladhani S, Panovska-Griffiths J, Bonell C, Melendez-Torres GJ. Transmission of SARS-CoV-2 by children and young people in households and schools: a meta-analysis of population-based and contact-tracing studies. J Infect. 2022;84(3):361–82.
Viner RM, Mytton OT, Bonell C, Melendez-Torres GJ, Ward J, Hudson L, Waddington C, Thomas J, Russell S, van der Klis F, et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 2021;175(2):143–56.
Vitaliti G, Giacchi V, Sciacca M, Ruggieri M, Falsaperla R. Thrombotic events in children and adolescent patients with SARS-CoV-2 infection: a systematic review with meta-analysis on incidence and management. Expert Rev Hematol. 2022;15(7):635–43.
Vosoughi F, Makuku R, Tantuoyir MM, Yousefi F, Shobeiri P, Karimi A, Alilou S, LaPorte R, Tilves C, Nabian MH, et al. A systematic review and meta-analysis of the epidemiological characteristics of COVID-19 in children. BMC Pediatr. 2022;22(1):613.
Wang J, Yuan X. Digestive system symptoms and function in children with COVID-19: a meta-analysis. Medicine (Baltimore). 2021;100(11):e24897.
Wang JG, Cui HR, Tang HB, Deng XL. Gastrointestinal symptoms and fecal nucleic acid testing of children with 2019 coronavirus disease: a systematic review and meta-analysis. Sci Rep. 2020;10(1):17846.
Wang JG, Mo YF, Su YH, Wang LC, Liu GB, Li M, Qin QQ. Computed tomography features of COVID-19 in children: a systematic review and meta-analysis. Medicine (Baltimore). 2021;100(38):e22571.
Wang JG, Zhong ZJ, Li M, Fu J, Su YH, Ping YM, Xu ZJ, Li H, Chen YH, Huang YL. Coronavirus disease 2019-related multisystem inflammatory syndrome in children: a systematic review and meta-analysis. Biochem Res Int. 2021;2021:5596727.
Wang JG, Zhong ZJ, Mo YF, Wang LC, Chen R. Epidemiological features of coronavirus disease 2019 in children: a meta-analysis. Eur Rev Med Pharmacol Sci. 2021;25(2):1146–57.
Wang S, Chen L, Ran H, Che Y, Fang D, Sun H, Peng J, Liang X, Xiao Y. Depression and anxiety among children and adolescents pre and post COVID-19: a comparative meta-analysis. Front Psychiatry. 2022;13:917552.
Wang Z, Zhou Q, Wang C, Shi Q, Lu S, Ma Y, Luo X, Xun Y, Li W, Baskota M, et al. Clinical characteristics of children with COVID-19: a rapid review and meta-analysis. Ann Transl Med. 2020;8(10):620.
Watcharapalakorn A, Poyomtip T, Tawonkasiwattanakun P. Coronavirus disease 2019 outbreak and associated public health measures increase the progression of myopia among children and adolescents: evidence synthesis. Ophthalmic Physiol Opt. 2022;42(4):744–52.
Williams V, Dash N, Suthar R, Mohandoss V, Jaiswal N, Kavitha TK, Nallasamy K, Angurana SK. Clinicolaboratory profile, treatment, intensive care needs, and outcome of pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2: a systematic review and meta-analysis. J Pediatr Intensive Care. 2022;11(1):1–12.
Xiao F, Tang M, Yan K, Zhou W. Clinical features of infants with SARS-CoV-2 infection: a systematic review and meta-analysis. Ann Palliat Med. 2022;11(11):3394–408.
Xu W, Tang J, Chen C, Wang C, Wen W, Cheng Y, Zhou M, Wu Q, Zhang X, Feng Z, et al. Safety and efficacy of the COVID-19 vaccine in children and/or adolescents: a meta-analysis. J Infect. 2022;84(5):722–46.
Yadav M, Singh A, Meena J, Sankar JM. A systematic review and meta-analysis of otorhinolaryngological manifestations of coronavirus disease 2019 in paediatric patients. J Laryngol Otol. 2022;136(7):588–603.
Yan Q, Qiu D, Liu X, Guo X, Hu Y. Prevalence of smell or taste dysfunction among children with COVID-19 infection: a systematic review and meta-Analysis. Front Pediatr. 2021;9:686600.
Yang F, Wen J, Huang N, Riem MME, Lodder P, Guo J. Prevalence and related factors of child posttraumatic stress disorder during COVID-19 pandemic: a systematic review and meta-analysis. Eur Psychiatry. 2022;65(1):e37.
Yang J, D’Souza R, Kharrat A, Fell DB, Snelgrove JW, Murphy KE, Shah PS. Coronavirus disease 2019 pandemic and pregnancy and neonatal outcomes in general population: a living systematic review and meta-analysis (updated Aug 14, 2021). Acta Obstet Gynecol Scand. 2022;101(1):7–24.
Yang Z, Wang X, Wan XG, Wang ML, Qiu ZH, Chen JL, Shi MH, Zhang SY, Xia YL. Pediatric asthma control during the COVID-19 pandemic: a systematic review and meta-analysis. Pediatr Pulmonol. 2022;57(1):20–5.
Yang Z, Wang X, Zhang S, Ye H, Chen Y, Xia Y. Pediatric myopia progression during the COVID-19 pandemic home quarantine and the risk factors: a systematic review and meta-analysis. Front Public Health. 2022;10:835449.
Yasuhara J, Watanabe K, Takagi H, Sumitomo N, Kuno T. COVID-19 and multisystem inflammatory syndrome in children: a systematic review and meta-analysis. Pediatr Pulmonol. 2021;56(5):837–48.
Zang ST, Han X, Cui Q, Chang Q, Wu QJ, Zhao YH. Imaging characteristics of coronavirus disease 2019 (COVID-19) in pediatric cases: a systematic review and meta-analysis. Transl Pediatr. 2021;10(1):1–16.
Zhang L, Peres TG, Silva MVF, Camargos P. What we know so far about Coronavirus Disease 2019 in children: a meta-analysis of 551 laboratory-confirmed cases. Pediatr Pulmonol. 2020;55(8):2115–27.
Zhao Y, Patel J, Huang Y, Yin L, Tang L. Cardiac markers of multisystem inflammatory syndrome in children (MIS-C) in COVID-19 patients: a meta-analysis. Am J Emerg Med. 2021;49:62–70.
Zheng B, Wang H, Yu C. An increasing public health burden arising from children infected with SARS-CoV2: a systematic review and meta-analysis. Pediatr Pulmonol. 2020;55(12):3487–96.
Zou H, Lu J, Liu J, Wong JH, Cheng S, Li Q, Shen Y, Li C, Jia X. Characteristics of pediatric multi-system inflammatory syndrome (PMIS) associated with COVID-19: a meta-analysis and insights into pathogenesis. Int J Infect Dis. 2021;102:319–26.
Yasuhara J, Masuda K, Aikawa T, Shirasu T, Takagi H, Lee S, Kuno T. Myopericarditis after COVID-19 mRNA vaccination among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2023;177(1):42–52.
Watanabe A, Kani R, Iwagami M, Takagi H, Yasuhara J, Kuno T. Assessment of efficacy and safety of mRNA COVID-19 vaccines in children aged 5 to 11 years: a systematic review and meta-analysis. JAMA Pediatr. 2023;144(4):384–94.
Cui X, Zhao Z, Zhang T, Guo W, Guo W, Zheng J, Zhang J, Dong C, Na R, Zheng L, et al. A systematic review and meta-analysis of children with coronavirus disease 2019 (COVID-19). J Med Virol. 2021;93(2):1057–69.
Dorantes-Acosta E, Avila-Montiel D, Klunder-Klunder M, Juarez-Villegas L, Marquez-Gonzalez H. Survival and complications in pediatric patients with cancer and COVID-19: a meta-analysis. Front Oncol. 2020;10:608282.
Mustafa NM. L AS: characterisation of COVID-19 pandemic in paediatric age group: a systematic review and meta-analysis. J Clin Virol. 2020;128:104395.
Neef V, Buxmann H, Rabenau HF, Zacharowski K, Raimann FJ. Characterization of neonates born to mothers with SARS-CoV-2 infection: review and meta-analysis. Pediatr Neonatol. 2021;62(1):11–20.
Carabelli AM, Peacock TP, Thorne LG, Harvey WT, Hughes J, Consortium C-GU, Peacock SJ, Barclay WS, de Silva TI, Towers GJ, et al. SARS-CoV-2 variant biology: immune escape, transmission and fitness. Nat Rev Microbiol. 2023;21(3):162–77.
Stephenson T, Shafran R, Ladhani SN. Long COVID in children and adolescents. Curr Opin Infect Dis. 2022;35(5):461–7.
Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–20.
Paterson C, Davis D, Roche M, Bissett B, Roberts C, Turner M, Baldock E, Mitchell I. What are the long-term holistic health consequences of COVID-19 among survivors? An umbrella systematic review. J Med Virol. 2022;94(12):5653–68.
Nittas V, Gao M, West EA, Ballouz T, Menges D, Wulf Hanson S, Puhan MA. Long COVID through a public health lens: an umbrella review. Public Health Rev. 2022;43:1604501.
Witteveen AB, Young SY, Cuijpers P, Ayuso-Mateos JL, Barbui C, Bertolini F, Cabello M, Cadorin C, Downes N, Franzoi D, et al. COVID-19 and common mental health symptoms in the early phase of the pandemic: an umbrella review of the evidence. Plos Med. 2023;20(4):e1004206.
Bevilacqua L, Fox-Smith L, Lewins A, Jetha P, Sideri A, Barton G, Meiser-Stedman R, Beazley P. Impact of COVID-19 on the mental health of children and young people: an umbrella review. J Epidemiol Community Health. 2023;77(11):704–9.
Fan Y, Li X, Zhang L, Wan S, Zhang L, Zhou F. SARS-CoV-2 Omicron variant: recent progress and future perspectives. Signal Transduct Target Ther. 2022;7(1):141.
Iuliano AD, Brunkard JM, Boehmer TK, Peterson E, Adjei S, Binder AM, Cobb S, Graff P, Hidalgo P, Panaggio MJ, et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods - United States, December 2020-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(4):146–52.
Garrett N, Tapley A, Andriesen J, Seocharan I, Fisher LH, Bunts L, Espy N, Wallis CL, Randhawa AK, Miner MD, et al. High asymptomatic carriage with the omicron variant in South Africa. Clin Infect Dis. 2022;75(1):e289–92.
Mocanu V, Bhagwani D, Sharma A, Borza C, Rosca CI, Stelian M, Bhagwani S, Haidar L, Kshtriya L, Kundnani NR, et al. COVID-19 and the human eye: conjunctivitis, a lone COVID-19 finding - a case-control study. Med Princ Pract. 2022;31(1):66–73.
Al-Namaeh M. Ocular manifestations of COVID-19. Ther Adv Ophthalmol. 2022;14:25158414221083376.
Shang W, Kang L, Cao G, Wang Y, Gao P, Liu J, Liu M. Percentage of asymptomatic infections among SARS-CoV-2 omicron variant-positive individuals: a systematic review and meta-analysis. Vaccines (Basel). 2022;10(7):1049.
Zhang JJ, Dong X, Liu GH, Gao YD. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. 2023;64(1):90–107.
Zhao S, Luo K, Guo Y, Fang M, Sun Q, Dai Z, Yang H, Zhan Z, Hu S, Chen T, et al. Analysis of factors influencing the clinical severity of omicron and delta variants. Trop Med Infect Dis. 2023;8(6):330.
Jones TC, Biele G, Muhlemann B, Veith T, Schneider J, Beheim-Schwarzbach J, Bleicker T, Tesch J, Schmidt ML, Sander LE, et al. Estimating infectiousness throughout SARS-CoV-2 infection course. Science. 2021;373(6551):eabi5273.
Reyman M, Clerc M, van Houten MA, Arp K, Chu M, Hasrat R, Sanders EAM, Bogaert D. Microbial community networks across body sites are associated with susceptibility to respiratory infections in infants. Commun Biol. 2021;4(1):1233.
Bastard P, Gervais A, Le Voyer T, Rosain J, Philippot Q, Manry J, Michailidis E, Hoffmann HH, Eto S, Garcia-Prat M, et al. Autoantibodies neutralizing type I IFNs are present in ~4% of uninfected individuals over 70 years old and account for ~20% of COVID-19 deaths. Sci Immunol. 2021;6(62):eabl4340.
Niessl J, Sekine T, Lange J, Konya V, Forkel M, Maric J, Rao A, Mazzurana L, Kokkinou E, Weigel W, et al. Identification of resident memory CD8(+) T cells with functional specificity for SARS-CoV-2 in unexposed oropharyngeal lymphoid tissue. Sci Immunol. 2021;6(64):eabk0894.
Flannery DD, Gouma S, Dhudasia MB, Mukhopadhyay S, Pfeifer MR, Woodford EC, Triebwasser JE, Gerber JS, Morris JS, Weirick ME, et al. Assessment of maternal and neonatal cord blood SARS-CoV-2 antibodies and placental transfer ratios. JAMA Pediatr. 2021;175(6):594–600.
Grimsholm O, Piano Mortari E, Davydov AN, Shugay M, Obraztsova AS, Bocci C, Marasco E, Marcellini V, Aranburu A, Farroni C, et al. The interplay between CD27(dull) and CD27(bright) B cells ensures the flexibility, stability, and resilience of human B cell memory. Cell Rep. 2020;30(9):2963-2977.e2966.
Saheb Sharif-Askari N, Saheb Sharif-Askari F, Alabed M, Temsah MH, Al Heialy S, Hamid Q, Halwani R. Airways expression of SARS-CoV-2 receptor, ACE2, and TMPRSS2 is lower in children than adults and increases with smoking and COPD. Mol Ther Methods Clin Dev. 2020;18:1–6.
Bradley T, Tucker M, Sampath V: Triggered - does maternal COVID-19 program an exaggerated immune response in neonates? Pediatr Res 2024 early eprint. https://www.nature.com/articles/s41390-023-03007-0#citeas.
Brodin P. SARS-CoV-2 infections in children: Understanding diverse outcomes. Immunity. 2022;55(2):201–9.
Noval Rivas M, Porritt RA, Cheng MH, Bahar I, Arditi M. Multisystem inflammatory syndrome in children and long COVID: The SARS-CoV-2 viral superantigen hypothesis. Front Immunol. 2022;13:941009.
Borel M, Xie L, Kapera O, Mihalcea A, Kahn J, Messiah SE. Long-term physical, mental and social health effects of COVID-19 in the pediatric population: a scoping review. World J Pediatr. 2022;18(3):149–59.
Kikkenborg Berg S, Palm P, Nygaard U, Bundgaard H, Petersen MNS, Rosenkilde S, Thorsted AB, Ersboll AK, Thygesen LC, Nielsen SD, et al. Long COVID symptoms in SARS-CoV-2-positive children aged 0–14 years and matched controls in Denmark (LongCOVIDKidsDK): a national, cross-sectional study. Lancet Child Adolesc Health. 2022;6(9):614–23.
Bloise S, Isoldi S, Marcellino A, De Luca E, Dilillo A, Mallardo S, Martucci V, Sanseviero M, Del Giudice E, Iorfida D, et al. Clinical picture and long-term symptoms of SARS-CoV-2 infection in an Italian pediatric population. Ital J Pediatr. 2022;48(1):79.
Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137(6):959–97.
Cao X, Ma C, Zheng Z, He L, Hao M, Chen X, Crimmins EM, Gill TM, Levine ME, Liu Z. Contribution of life course circumstances to the acceleration of phenotypic and functional aging: a retrospective study. EClinicalMedicine. 2022;51:101548.
Siegel DA, Reses HE, Cool AJ, Shapiro CN, Hsu J, Boehmer TK, Cornwell CR, Gray EB, Henley SJ, Lochner K, et al. Trends in COVID-19 cases, emergency department visits, and hospital admissions among children and adolescents aged 0–17 Years - United States, August 2020-August 2021. MMWR Morb Mortal Wkly Rep. 2021;70(36):1249–54.
de Miranda DM, da Silva AB, Oliveira ACS, Simoes-e-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduction. 2020;51:101845.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Linney C, McManus MN, Borwick C, Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239 e1213.
Shelleby EC, Pittman LD, Bridgett DJ, Keane J, Zolinski S, Caradec J. Associations between local COVID-19 case rates, pandemic-related financial stress and parent and child functioning. J Fam Psychol. 2022;36(6):932–42.
Suarez-Lopez JR, Cairns MR, Sripada K, Quiros-Alcala L, Mielke HW, Eskenazi B, Etzel RA, Kordas K. COVID-19 and children’s health in the United States: consideration of physical and social environments during the pandemic. Environ Res. 2021;197:111160.
Tandon PS, Zhou C, Johnson AM, Gonzalez ES, Kroshus E. Association of children’s physical activity and screen time with mental health during the COVID-19 pandemic. JAMA Netw Open. 2021;4(10):e2127892.
Montero-Marin J, Hinze V, Mansfield K, Slaghekke Y, Blakemore SJ, Byford S, Dalgleish T, Greenberg MT, Viner RM, Ukoumunne OC, et al. Young people’s mental health changes, risk, and resilience during the COVID-19 pandemic. JAMA Netw Open. 2023;6(9):e2335016.
Tian F, Yang R, Chen Z. Safety and efficacy of COVID-19 vaccines in children and adolescents: a systematic review of randomized controlled trials. J Med Virol. 2022;94(10):4644–53.
Haslak F, Gunalp A, Cebi MN, Yildiz M, Adrovic A, Sahin S, Barut K, Kasapcopur O. Early experience of COVID-19 vaccine-related adverse events among adolescents and young adults with rheumatic diseases: a single-center study. Int J Rheum Dis. 2022;25(3):353–63.
Erbas IM, Erbas IC, Kagizmanli GA, Yuksek Acinikli K, Besci O, Demir K, Bober E, Belet N, Abaci A. Adverse events associated with COVID-19 vaccination in adolescents with endocrinological disorders: a cross-sectional study. J Clin Res Pediatr Endocrinol. 2023;15(3):248–56.
Kastl AJ, Weaver KN, Zhang X, Strople JA, Adler J, Dubinsky MC, Bousvaros A, Watkins R, Dai X, Chen W, et al. Humoral immune response and safety of SARS-CoV-2 vaccination in pediatric inflammatory bowel disease. Am J Gastroenterol. 2023;118(1):129–37.
Thomas SJ, Moreira ED Jr, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Polack FP, Zerbini C, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med. 2021;385(19):1761–73.
Price AM, Olson SM, Newhams MM, Halasa NB, Boom JA, Sahni LC, Pannaraj PS, Irby K, Bline KE, Maddux AB, et al. BNT162b2 protection against the omicron variant in children and adolescents. N Engl J Med. 2022;386(20):1899–909.
Breaux R, Cash AR, Lewis J, Garcia KM, Dvorsky MR, Becker SP. Impacts of COVID-19 quarantine and isolation on adolescent social functioning. Curr Opin Psychol. 2023;52:101613.
Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, Mytton O, Bonell C, Booy R. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4(5):397–404.
Graetz D, Agulnik A, Ranadive R, Vedaraju Y, Chen Y, Chantada G, Metzger ML, Mukkada S, Force LM, Friedrich P, et al. Global effect of the COVID-19 pandemic on paediatric cancer care: a cross-sectional study. Lancet Child Adolesc Health. 2021;5(5):332–40.
Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221(264–266): e261.
Masse LC, Edache IY, Pitblado M, Hutchison SM. The impact of financial and psychological wellbeing on children’s physical activity and screen-based activities during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(16):8694.
Wilder JL, Parsons CR, Growdon AS, Toomey SL, Mansbach JM. Pediatric hospitalizations during the COVID-19 pandemic. Pediatrics. 2020;146(6):e2020005983.
Dekkers OM, Vandenbroucke JP, Cevallos M, Renehan AG, Altman DG, Egger M. COSMOS-E: Guidance on conducting systematic reviews and meta-analyses of observational studies of etiology. Plos Med. 2019;16(2):e1002742.
Varsavsky T, Graham MS, Canas LS, Ganesh S, Capdevila Pujol J, Sudre CH, Murray B, Modat M, Jorge Cardoso M, Astley CM, et al. Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study. Lancet Public Health. 2021;6(1):e21–9.
Essig RM, Jones BA. Challenges in the multidisciplinary management of pediatric patients with intestinal failure during the COVID-19 pandemic. Pediatr Ann. 2022;51(7):e277–80.
Sniderman ER, Graetz DE, Agulnik A, Ranadive R, Vedaraju Y, Chen Y, Devidas M, Chantada GL, Hessissen L, Dalvi R, et al. Impact of the COVID-19 pandemic on pediatric oncology providers globally: a mixed-methods study. Cancer. 2022;128(7):1493–502.
Gelman A, Stern H. The difference between “significant” and “not significant” is not itself statistically significant. Am Stat. 2006;60(4):328–31.
Acknowledgements
None.
Funding
This work is supported by the National Natural Science Foundation of China (82301106), Natural Science Foundation of Sichuan province (24NSFSC3535), Fundamental Research Funds for the Central Universities and Research and Develop Program, West China Hospital of Stomatology Sichuan University (RD-02–202409).
Author information
Authors and Affiliations
Contributions
The research was conceptualized and designed by Y.C. and L.C. The data were obtained and compiled by T.W., C.D., G.Z., L.Y., and L.L., and analyzed by L.L. and C.D. The manuscript was drafted by L.L., C.D., T.W., and G.W., and critically reviewed for significant intellectual content by L.L., C.D., T.W., Z.J., H.L., C.L., and Y.C. All authors read and approved the final manuscript.
Authors’ Twitter handles
@LiuLiu_DDS (Liu Liu); @YubinCao (Yubin Cao).
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Differences between protocol and review.
Additional file 2.
PRISMA 2020 checklist.
Additional file 3.
Search strategy.
Additional file 4.
List of excluded studies with justification for exclusion.
Additional file 5.
Detailed information on the characteristics of the included systematic reviews.
Additional file 6.
AMSTAR2 methodological quality assessments.
Additional file 7.
Primary studies data extracted from single-armed meta-analyses of laboratory-confirmed COVID-19.
Additional file 8.
Additional COVID-19-related evidence from single-armed meta-analyses.
Additional file 9.
Effect sizes and forest plots on COVID-19-associated multisystem inflammatory syndrome.
Additional file 10.
Effect sizes and forest plots on newborns from COVID-19-diagnosed mothers.
Additional file 11.
Effect sizes and forest plots on long-COVID.
Additional file 12.
Effect sizes and forest plots on events caused by the COVID-19 vaccine.
Additional file 13.
Effect sizes and forest plots on health impacts during the pandemic.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Duan, C., Liu, L., Wang, T. et al. Evidence linking COVID-19 and the health/well-being of children and adolescents: an umbrella review. BMC Med 22, 116 (2024). https://doi.org/10.1186/s12916-024-03334-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03334-x