Abstract
Background
Effective pain control is crucial to optimise the success of medical procedures. Immersive virtual reality (VR) technology could offer an effective non-invasive, non-pharmacological option to distract patients and reduce their experience of pain. We aimed to evaluate the efficacy of Immersive virtual reality (VR) technology in reducing patient’s pain perception during various medical procedures by conducting a systematic review and meta-analysis.
Methods
We searched MEDLINE, EMBASE, CENTRAL, CINAHL, and SIGLE until December 2022 for all randomised clinical trials (RCT) evaluating any type of VR in patients undergoing any medical procedure. We conducted a random effect meta-analysis summarising standardised mean differences (SMD) with 95% confidence intervals (CI). We evaluated heterogeneity using I 2 and explored it using subgroup and meta-regression analyses.
Results
In total, we included 92 RCTs (n = 7133 participants). There was a significant reduction in pain scores with VR across all medical procedures (n = 83, SMD − 0.78, 95% CI − 1.00 to − 0.57, I 2 = 93%, p = < 0.01). Subgroup analysis showed varied reduction in pain scores across trial designs [crossover (n = 13, SMD − 0.86, 95% CI − 1.23 to − 0.49, I 2 = 72%, p = < 0.01) vs parallel RCTs (n = 70, SMD − 0.77, 95% CI − 1.01 to − 0.52, I 2 = 90%, p = < 0.01)]; participant age groups [paediatric (n = 43, SMD − 0.91, 95% CI − 1.26 to − 0.56, I 2 = 87%, p = < 0.01) vs adults (n = 40, SMD − 0.66, 95% CI − 0.94 to − 0.39, I 2 = 89%, p = < 0.01)] or procedures [venepuncture (n = 32, SMD − 0.99, 95% CI − 1.52 to − 0.46, I 2 = 90%, p = < 0.01) vs childbirth (n = 7, SMD − 0.99, 95% CI − 1.59 to − 0.38, I 2 = 88%, p = < 0.01) vs minimally invasive medical procedures (n = 25, SMD − 0.51, 95% CI − 0.79 to − 0.23, I 2 = 85%, p = < 0.01) vs dressing changes in burn patients (n = 19, SMD − 0.8, 95% CI − 1.16 to − 0.45, I 2 = 87%, p = < 0.01)]. We explored heterogeneity using meta-regression which showed no significant impact of different covariates including crossover trials (p = 0.53), minimally invasive procedures (p = 0.37), and among paediatric participants (p = 0.27). Cumulative meta-analysis showed no change in overall effect estimates with the additional RCTs since 2018.
Conclusions
Immersive VR technology offers effective pain control across various medical procedures, albeit statistical heterogeneity. Further research is needed to inform the safe adoption of this technology across different medical disciplines.
Similar content being viewed by others
Background
Pain is the commonest symptom encountered in clinical practice often manifesting as an unavoidable consequence of medical procedures. Effective pain management is crucial to optimise medical procedures, boost patients’ satisfaction [1,2,3], reduce their anxiety, reduce hospital stay and minimise long-term analgesic dependence [4,5,6]. The use of immersive virtual reality (VR) technology has emerged as a potential tool to distract patients and to modify their perception of pain. Its adoption in clinical practice remains limited.
The search for effective, safe, and cheap analgesic treatment options is a priority accelerated in part by the emerging opiates epidemic in several countries associated with dependence risk and narrow safety profile [7, 8]. VR technology seems to offer a credible option for effective acute pain relief either as an alternative or as a combined treatment as part of a multi-modal pain relief strategy [9].
The term ‘virtual reality’ was coined by Jaron Lanier, a writer, musician, visual artist, and computer scientist, who first used it in 1986. The first application of VR in healthcare dates back to the beginning of the 1990s. It stemmed from the need to visualize complex medical data, especially when planning surgical treatment [10]. Since then, the use of VR technology in medicine proliferated into several domains including surgical training, neuropsychiatry, acute and chronic pain management, and rehabilitation [10, 11].
VR devices are designed to alter one’s perception of presence in an alternate reality and augment their immersion, and interactivity [12]. Today, several cheap and user-friendly devices offer an immersive environment largely delivered via high-resolution head-mounted displays (HMDs) with built-in sound capabilities [13]. In clinical practice, immersive VR experience aims to distract patients during medical procedures, suppressing their appreciation of immediate physical surroundings, allowing them to escape into an alternative reality away from the painful stimuli [14,15,16]. Early VR equipment had several technological barriers that limited their use in everyday practice, including high cost, relatively large size, complex operating interface, and user unfamiliarity [17]. Recent advances in audio-visual technology, driven by the wide use of smartphones, have enabled the development of affordable and user-friendly equipment [18]. Coupled with bespoke medical software, these new VR devices offer patients a versatile immersive visual and auditory experience that could be adopted across different clinical settings [11, 19].
Several meta-analyses have evaluated the efficacy of VR showing a beneficial effect with its use. Georgescu et al. [20] performed a meta-analysis for randomised trials that evaluated VR until 2018 (n = 27 RCTs, 1452 patients) showing a beneficial effect for pain reduction following medical procedure although the findings were limited by high heterogeneity and high trial risk of bias [20]. Scapin et al. [21] performed a systematic review including [22] randomised trials on the use of VR in burn patients. The findings were also supportive of the role of VR as an effective complementary drug strategy for pain relief in burn patients [21]. However, these reviews were either limited to specific clinical situations, suffered from high heterogeneity, or lacked detailed subgroup analyses to explore the reasons for heterogeneity [21].
In the year 2022, there have been 24 new randomised clinical trials (RCT) [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] published evaluating VR technology highlighting the increased interest in this technology and offering further insight into its applicability across different medical disciplines. Still, the translation of this evidence has remained poor with respect to implementation of VR technology at scale and with variation in practice where medical specialities have taken steps towards adoption. Appreciation of the role of VR for pain relief can be aided by updated evidence synthesis [46].
In this systematic review, we conducted a comprehensive assessment of the evidence on VR efficacy as a non-invasive and non-pharmacological pain management method in patients undergoing different medical procedures. We performed an overall evidence synthesis pooling data from all relevant RCTs in addition to bespoke subgroup and meta-regression analyses to help interpret the evidence [17, 47].
Methods
We conducted this systematic review using a prospectively registered protocol (CRD 42020195919) [48] and reported in accordance with PRISMA guidelines [49].
Literature search
We searched major electronic databases (MEDLINE, EMBASE, Cochrance CENTRAL, CINAHL, and SIGLE) for randomised trials that evaluated the efficacy of immersive VR technology equipment for pain relief from inception until December 2022. We developed a comprehensive and inclusive search strategy using MeSH search terms and combined them using the Boolean ‘AND’ and ‘OR’ (Additional File 1: Appendix S1). We applied this search strategy to individual databases after amending it to the specification of each database. We then deduplicated the results and produced a final long list of citations. We manually searched the bibliographies of relevant studies to identify any additional trials not captured by our electronic database search. We also conducted supplementary searches in Google Scholar and Trip database to identify additional studies of relevance [50]. We did not apply any search filters or language restrictions. Relevant citations in non-English were obtained and translated for assessment against our inclusion criteria.
Study selection
Five independent reviewers (JJT, DP, SH and RP, AK) completed the study screening and inclusion process in two stages. First, titles and abstracts were screened to identify potentially relevant studies following which, the full text of relevant articles were reviewed against our inclusion criteria. We included all randomised trials of any design that evaluated the efficacy of any immersive VR technology equipment for pain relief during any medical procedure, including labour and childbirth. We initially planned this review to include only adult participants and later extended this to include paediatric participants to provide a more comprehensive evidence synthesis. We excluded non-randomised studies, review articles, and animal studies. We also excluded studies that assessed distraction techniques only (e.g. a display screen with no immersive capabilities), studies in dental procedures, and those that did not assess pain using a standardised measurement tool or reported on pain scores more than an hour after the procedure. Discrepancies and disagreements between reviewers were discussed and resolved in consensus with two additional reviewers (MPR and BHA).
Data extraction
Three reviewers (JJT, DP, SH, AK) extracted data in duplicate using a piloted electronic data extraction tool. We collected data on study design (crossover vs parallel), intervention settings, population characteristics, inclusion and exclusion criteria, type of VR technology and equipment used, nature of the medical procedure or intervention, loss to follow-up, and dropouts. Our primary outcome was pain scores measured immediately after or within an hour of the procedure. We also collected data on anxiety scores where relevant. In trials including paediatric patients, we included the parents’ reported pain scores.
Assessment of risk of bias
We assessed the risk of bias in included trials in duplicate (JJT, RP, AK, DP, MPR, SH) using the Cochrane Risk of Bias assessment tool 2.0 [51]. We assessed studies in five domains: participant randomisation and sequence generation, allocation concealment, outcome assessment, completeness of outcome data, and selective outcome reporting. Due to the nature of the intervention, we did not penalise unblinded trials. Studies with a crossover design were assessed using a modified version of an established tool [52]. We assessed the risk of bias in these studies for appropriate crossover design, randomisation and order of receiving the treatment, risk of carry-over effect, data collection, allocation concealment, outcome detection, data completeness, and selective outcome reporting.
Data synthesis
We pooled data using a meta-analysis with a random effect and adjusted using restricted maximum likelihood (REML) [53]. We reported on the difference in pain scores measured using standardised mean difference (SMD) with 95% confidence intervals (CI). We assessed any detected heterogeneity using the I 2 statistics. The I 2 index is an approach to quantify heterogeneity in meta-analyses. I 2 provides an estimate of the percentage of variability in results across studies that is due to real differences and not due to chance. The I 2 index measures the extent of heterogeneity by dividing the result of Cochran’s Q test and its degrees of freedom by the Q-value itself. An I 2 of less than 25% is usually viewed as low heterogeneity, between 25 and 50% as moderate, and over 50% as high heterogeneity.
We planned subgroup analyses to investigate potential effect modifiers (patient age group (paediatric patients defined as < 16 years old) vs adults), type of medical intervention (venepuncture-related procedures, minimally invasive medical procedures (defined as any medical procedure conducted in office setting without the need for general anaesthesia), dressing changes in burn patients, and childbirth), trial design (parallel group vs crossover trials), the trial quality as assessed using the risk of bias tool), the type of VR technology (interactive: arbitrarily defined when VR software is asking the participant to take part in specific activities compared to a passive VR experience), the VR delivery settings (inpatient vs outpatient vs emergency department) and assessed their impact on the effect estimates using a meta-regression [54]. We explored potential sources of heterogeneity using a leave-one-out analysis and a sensitivity analysis excluding potential outliers. We also investigated the risk of publication bias using Egger’s test, a funnel plot, and Galbraith plot to identify potential outliers [55]. Where publication bias was detected, we explore potential impact using the trim and fill method [56] to estimate and adjust for the number and outcomes of missing studies in the meta-analysis. We conducted a cumulative meta-analysis for selected outcomes to evaluate temporal trends and changes in effect estimate over time as new trials emerged [57]. Statistical analyses were conducted in STATA V17 (StataCorp, TX) and Open Meta-analyst software (Brown University; Providence, RI, USA).
Patient and public involvement
No input was sought from lay service consumers in the design, conduct, and reporting of this systematic review.
Results
We identified 51,140 potentially relevant citations, of which we assessed 132 studies against our inclusion criteria and included 90 articles reporting on 92 unique RCTs in our meta-analysis (7133 participants) (Fig. 1) (Additional File 1: Appendix S2. (40 studies were excluded [58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99]). No relevant citations were identified in non-English. The majority of included RCTs had a two-group parallel design (77/92, 84%), including a three-arm RCT [100], and less than one fifth had a crossover design (15/92, 16%).
Forty-two of included trials enrolled adults only (42/92, 46%), three had a mixed population, and fifty included paediatric participants only (50/92, 54%). The majority of trials were conducted in high-income countries; twenty-seven trials were conducted in the USA (27/92, 29%) while nineteen were conducted in Turkey (19/92, 21%), seven trials in Australia, Canada China respectively (7/92, 8%) (Additional File 1: Table S1).
The type of VR technology and equipment used across included trials evolved over time from interactive, immersive games hosted on a personal computer to immersive environment experiences with user-controlled interactive interface and real-time feedback (Table 1). Trials conducted over the last 10 years evaluated newer VR technology with sound immersive augmentation (13/47, 26%) [101,102,103,104,105,106,107,108,109,110,111,112,113] and hand-held mobile phones or mounted goggles (27/47, 58%) [100, 102, 103, 105, 106, 110, 111, 113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131].
Risk of bias
For parallel-group RCTs, the overall quality of the included studies was moderate with the majority of studies showing low or moderate risk of bias for selective reporting (73/77, 95%), outcome assessment (72/77, 94%), completeness of data (74/77, 91%) and randomisation risk of bias (70/77, 91%). Still, nine trials showed high risk for adherence to intervention groups (9/77, 12%), and none reported blinding participants or assessors (Additional File 1: Figure S1). The majority of crossover trials showed a high or unclear risk of bias, specifically for carry-over effect (13/15, 87%), completeness of data (6/15, 40%) and detection bias (12/15, 80%). The risk of bias for allocation concealment was deemed to be high in ten crossover trials (10/15, 67%) (Additional File 1: Figure S1).
Outcomes
Pain
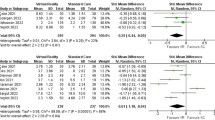
We pooled data from 83 RCTs that reported on pain scores following any medical procedure with nine RCTs excluded from the meta-analysis due to limited outcome reporting ((Additional File 1: Appendix S3). Our meta-analysis showed a significant reduction in pain scores with the use of VR across all types of medical procedures (n = 83, SMD − 0.78, 95% CI − 1.00 to − 0.57, p = < 0.01), although heterogeneity was high (I 2 = 93%) (Fig. 2). We explored the heterogeneity using meta-regression which showed no significant effect of different covariates, including crossover trials (p = 0.53), minimally invasive procedures (p = 0.37) or among paediatric participants (p = 0.27). (Additional File 1: Table S2). We conducted a cumulative meta-analysis to illustrate the chronological change in the effect size of VR on reducing pain which showed no change in overall effect estimates with the addition of new RCTs since 2018 (Fig. 3). We also calculated the predictive intervals of the pooled effect estimated which shows that 95% of the true effect size falls between − 4.02 and 1.05 for all comparable populations.
We performed subgroup analyses across these three identified categories (trial design, type of medical procedure and participant age group). The reduction in pain scores was consistent across crossover trials (n = 13, SMD − 0.86, 95% CI − 1.23 to − 0.49, I 2 = 72%, p = < 0.01) and parallel-group trials (n = 70, SMD − 0.77, 95% CI − 1.01 to − 0.52, I 2 = 90%, p = < 0.01) (Additional File 1: Figure S2). Similarly, VR reduced pain across the different participant age groups, though the effect was higher in paediatric participants (n = 43, SMD − 0.91, 95% CI − 1.26 to − 0.56, I 2 = 87%, p = < 0.01) compared to adults (n = 40, SMD − 0.66, 95% CI − 0.94 to − 0.39, I 2 = 89%, p = < 0.01) (Additional File 1: Figure S2). The efficacy of VR in reducing pain was significant in participants undergoing venepuncture-related procedures (n = 32, SMD − 0.99, 95% CI − 1.52 to − 0.46, I 2 = 90%, p = < 0.01), minimally invasive medical procedures (n = 25, SMD − 0.51, 95% CI − 0.79 to − 0.23, I 2 = 85%, p = < 0.01.), dressing changes in burn patients (n = 19, SMD − 0.8, 95% CI − 1.16 to − 0.45, I 2 = 87%, p = < 0.01) and during childbirth (n = 7, SMD − 0.99, 95% CI − 1.59 to − 0.38, I 2 = 88%, p = < 0.01) (Additional File 1: Figure S2). The use of interactive VR technology did not yield significant difference (SMD − 0.72, 95% CI − 1.11 to − 0.34, p = 0.00) compared to using non-interactive software (SMD − 0.78, 95% CI − 0.99 to − 0.57, p = 0.00). VR was effective in reducing pain across different care settings including inpatient (SMD − 0.79, 95% CI − 1.02 to − 0.57, p = 0.00), outpatient (SMD − 0.87, 95% CI − 1.45 to − 0.28, p = 0.28), and emergency department (SMD − 0.80, 95% CI − 1.70 to 0.11, p = 0.00).
We assessed publication bias using Egger’s test, which was significant (p = 0.11). We visually inspected the variance in effect estimates for potential small study effect using a funnel plot (Additional File 1: Figure S3) and a Galbraith plot (Additional File 1: Figure S3) which identified several outliers although the overall precision in the effect estimate was high. We explored the potential impact of publication bias using the trim and fill method which did not identify any missing studies (Hedge’s g 0.00, 95%CI − 0.051 to 0.051) (Additional File 1: Figure S3).
We conducted a leave-one-out analysis, which identified five studies as potential outliers [101, 126, 131, 134, 153, 154]. We then conducted a sensitivity analysis excluding these trials, which led to a small reduction in the overall effect estimate (SMD − 0.58, 95% CI − 0.71 to − 0.45), but did not resolve the observed heterogeneity (I 2 = 82%).
Anxiety
Thirty-one trials reported on changes in anxiety between the VR group and routine care, mainly involving minor medical procedures and venepuncture procedures [101, 111, 117, 120, 127, 128, 142]. The overall effect estimate showed a significant reduction in anxiety scores with the use of VR across all populations, although heterogeneity was high (n = 31, SMD − 0.82, 95% CI − 1.09 to − 0.54, I 2 = 91%, p = < 0.01) (Additional File 1: Figure S4). The cumulative meta-analysis showed more precise effect estimates with the addition of newer trials over the last 2 years, although the confidence interval remained relatively wide (Additional File 1: Figure S4).
We performed subgroup analyses across these three identified categories (trial design, type of medical procedure, and participant age group). The effect of VR technology on anxiety reduction was higher among paediatric participants (n = 15, SMD − 0.96, 95% CI − 1.37 to − 0.54, I 2 = 91%, p = < 0.01) compared to adults (n = 16, SMD − 0.68, 95% CI − 1.04 to − 0.32, I 2 = 91%, p = < 0.01) (Additional File 1: Figure S5). Reduction in anxiety was highest among trials that evaluated venepuncture-related procedures (n = 15, SMD − 0.99, 95% CI − 1.39 to − 0.58, I 2 = 90%, p = < 0.01) followed by minor medical procedures (n = 10, SMD − 0.42, 95% CI − 0.77 to − 0.07, I 2 = 84%, p = < 0.01) and childbirth (n = 4, SMD − 1.48, 95% CI − 2.19 to − 0.76, I 2 = 93%, p = < 0.01). However, the effect was not significant for dressing changes (n = 2, SMD − 0.17, 95% CI − 0.49 to 0.15, I 2 = 0%, p = 0.56) (Additional File 1: Figure S6). The reduction in anxiety was significant across parallel-group trials (n = 13, SMD − 0.85, 95% CI − 1.14 to − 0.56, I 2 = 91%, p = < 0.01) but not in crossover trials (n = 2, SMD − 0.31, 95% CI − 0.80 to 0.17, I 2 = 38%, p = 0.20) (Additional File 1: Figure S6).
Only 46 trials reported on side effects with the use of VR technology (46/92, 59%). The far majority reporting mild side effects including nausea, vomiting, and headache. No serious side effects were reported (Additional File 1: Table S1).
Discussion
Summary of main findings
Our review summarised evidence sought from different medical disciplines evaluating the efficacy of VR technology. Despite heterogeneity, the reduction in pain perception was consistent across different clinical settings, medical procedures, and patient characteristics. We identified a relatively high number of relevant trials, particularly within the last 5 years. This was associated with a gradual development in the VR equipment used moving from larger head mount display screens to lighter and cheaper smartphones interfaces [100,101,102,103, 105,106,107, 115, 116, 118,119,120,121,122, 125,126,127,128, 130, 133, 155, 159, 160, 164]. The reduction in pain scores was observed across all evaluated medical procedures, participant age groups and trial designs, which increased the generalisability of our findings.
Implications for clinical practice
The rapid progress in immersive VR technology has facilitated its evaluation within different clinical settings driven by smaller, cheaper, and more user-friendly VR equipment. VR immersion was defined as according to this point of view VR is described as ‘an advanced form of human–computer interface that allows the user to interact with and become immersed in a computer-generated environment in a naturalistic fashion’ [169].
As this technology becomes more widespread within the general population, its use within the health sector will gradually become mainstream with higher user acceptability and satisfaction [170]. Unlike other disciplines, e.g. engineering [171] and education [172], where VR use has grown organically, introducing it into healthcare requires deliberate implementation steps to ensure feasibility and patients’ safety [173]. Considering the beneficial effect observed in our meta-analysis, we argue that health policy makers should incorporate the use of VR within their pain management guidelines to enable its safe adoption [174]. This is particularly relevant for certain patient groups, such as in paediatric phlebotomy [175].
Implications for future research
Our review is focused on evaluating VR technology in acute pain relief settings, largely using non-standardised software. Such versatile and easy-to-use technology has the potential to help chronic pain patients within the community enabled by virtual reality meditation and mindfulness techniques [176]. Similarly, developing procedure or condition-specific software could also help to maximise its analgesic effect as shown by some early experimental studies [177]. Lastly, clinical implementation pathways should consider the ideal format, frequency, and timing of using VR for medical procedures as per local feasibility.
Previous systematic reviews [20, 178,179,180] called for larger trials to address the perceived heterogeneity. Our trim and fill analysis suggests that larger trials are unlikely to nullify the depicted cumulative beneficial effect across the trials included in our analysis, thus offering low added value.
The majority of the included trials in our review focused on acute pain control following medical intervention. VR could be a game-changer to convert several inpatient procedures to outpatient settings, thus driving down cost, hospital stay, and in-hospital complications [120].
The reduction in pain management cost alone could offer a substantial advantage to reduce the length of hospital stay and associated costs, which was estimated at around $5.4 per patient (95% CI − 11 to 156) with VR use compared to routine care [181]. In this case, VR will prove dominant without the need for a formal cost-effectiveness study.
Most of the included trials used varied pain scales with no clear justifications, which may have led to higher heterogeneity at evidence synthesis. Adopting available standardised and validated outcome measurement tools would enable precise evidence synthesis and help to eliminate across trial heterogeneity. Leveraging the advances in VR user interfaces could enable interactive and contemporary built-in outcomes assessment, thus eliminating assessment bias in future studies.
Strengths and limitations
The main strength of our review stems from our comprehensive approach to evaluating the efficacy of VR technology across different medical disciplines in contrast to previous reviews that focused on particular patient demographics or medical conditions [21]. We undertook a prospective registration, employed an exhaustive search strategy, and evaluated the sources of bias. We followed an established methodology to explore potential sources of heterogeneity and evaluated the risk of publication bias.
Our findings suffered some limitations, most notably the heterogeneity of effects among included trials. We explored this heterogeneity in a meta-regression which suggested a higher effect in minor procedures and in trials involving children. However, the observed beneficial effect pertaining across all evaluated subgroups with relatively narrow confidence intervals supports the overall benefit of VR technology for pain control. We explored this heterogeneity using a cumulative meta-analysis which confirmed that future trials are unlikely to change the certainty in the beneficial effect of VR in reducing pain following medical procedures. The prediction intervals also suggest that most population would see a benefit from using VR although a small portion might not observe this benefit (Additional File 1: Figure S7).
A potential source of heterogeneity could stem from the assumed variation in the reported common comparator (routine care). Several analgesic agents, doses, and frequencies could have been used in the control group across included studies which we were unable to adjust for in our analysis.
Several factors could drive this heterogeneity, including variations in the common comparator, background, type of software (e.g. interactive vs static), hardware fidelity, procedure and exposure duration, patient morbidity and pain tolerance, and measurement assessment tools. Exploring these effect modifiers is only possible using individual patient data. However, such analysis might fail to add significant value especially when evaluating a subjective outcome such as pain, even within the context of an individual patient data meta-analysis [182].
Most of the included studies had a small sample size, with some evident outliers identified on the funnel plot. To address the risk of publication bias, we conducted a cumulative and one-out trial analysis, excluding obvious outliers, which helped us to refine the effect estimates. While some of the included crossover RCTs suffered from risk of bias [124, 125, 131], our subgroup analysis supported the overall beneficial effect of VR across both crossover and parallel-group RCTs. Majority of the included crossover trials only reported on the effect estimates after the final crossover step which limited our ability to adjust for the potential risk of bias when pooling data from such trials. We explored the limitation of evidence sought from crossover trials using a subgroup analysis which demonstrated a wider confidence intervals compared to evidence from parallel-group trials. However, evidence of reduction in pain scores remained significant (Additional File 1: Figure S2).
Lastly, we were unable to report on the planned secondary outcomes in our protocol due to limitations in reporting across the included trials.
Conclusions
Immersive VR technology offers effective pain control across various medical procedures, albeit statistical heterogeneity, albeit statistical heterogeneity. Further research is needed to inform the safe adoption of this technology across different medical disciplines.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RCT:
-
Randomised clinical trials
- VR:
-
Virtual reality
References
Akbar N, Teo SP, Artini Hj-Abdul-Rahman HN, et al. Barriers and solutions for improving pain management practices in acute hospital settings: perspectives of healthcare practitioners for a pain-free hospital initiative. Ann Geriatr Med Res. 2019;23(4):190–6. https://doi.org/10.4235/agmr.19.0037. [publishedOnlineFirst:2020/08/04].
Glowacki D. Effective pain management and improvements in patients’ outcomes and satisfaction. Crit Care Nurse. 2015;35(3):33–41; quiz 43. https://doi.org/10.4037/ccn2015440. [published Online First: 2015/06/03].
Gordon DB, Dahl JL, Miaskowski C, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med. 2005;165(14):1574–80. https://doi.org/10.1001/archinte.165.14.1574. [publishedOnlineFirst:2005/07/27].
Rosenblum A, Marsch LA, Joseph H, et al. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16(5):405–16. https://doi.org/10.1037/a0013628. [publishedOnlineFirst:2008/10/08].
Katz N. The impact of pain management on quality of life. J Pain Symptom Manage. 2002;24(1 Suppl):S38–47. https://doi.org/10.1016/s0885-3924(02)00411-6. [publishedOnlineFirst:2002/09/03].
Lin RJ, Reid MC, Liu LL, et al. The barriers to high-quality inpatient pain management: a qualitative study. Am J Hosp Palliat Care. 2015;32(6):594–9. https://doi.org/10.1177/1049909114530491. [publishedOnlineFirst:2014/04/15].
Murray M, Stone A, Pearson V, et al. Clinical solutions to chronic pain and the opiate epidemic. Prev Med. 2019;118:171–5. https://doi.org/10.1016/j.ypmed.2018.10.004.
Nadeau SE, Wu JK, Lawhern RA. Opioids and chronic pain: an analytic review of the clinical evidence. Front Pain Res. 2021;2. https://doi.org/10.3389/fpain.2021.721357.
Honzel E, Murthi S, Brawn-Cinani B, et al. Virtual reality, music, and pain: developing the premise for an interdisciplinary approach to pain management. PAIN. 2019;160(9):1909–19.
Mazurek J, Kiper P, Cieślik B, et al. Virtual reality in medicine: a brief overview and future research directions. Hum Mov. 2019;20:16–22. https://doi.org/10.5114/hm.2019.83529.
Li L, Yu F, Shi D, et al. Application of virtual reality technology in clinical medicine. Am J Transl Res. 2017;9(9):3867–80. [published Online First: 2017/10/06].
Mütterlein J. The three pillars of virtual reality? Investigating the roles of immersion, presence, and interactivity. 2018.
Lin HT, Li YI, Hu WP, et al. A scoping review of the efficacy of virtual reality and exergaming on patients of musculoskeletal system disorder. J Clin Med. 2019;8(6). https://doi.org/10.3390/jcm8060791. [published Online First: 2019/06/07].
Sherman WR, Craig AB. Understanding virtual reality: Interface, application, and design: Morgan Kaufmann. 2018.
Schneider SM, Workman ML. Effects of virtual reality on symptom distress in children receiving chemotherapy. Cyberpsychol Behav. 1999;2(2):125–34. https://doi.org/10.1089/cpb.1999.2.125. [publishedOnlineFirst:1999/01/01].
Garrett B, Taverner T, Gromala D, et al. Virtual reality clinical research: promises and challenges. JMIR Serious Games. 2018;6(4):e10839. https://doi.org/10.2196/10839. [publishedOnlineFirst:2018/10/20].
Baniasadi T, Ayyoubzadeh SM, Mohammadzadeh N. Challenges and practical considerations in applying virtual reality in medical education and treatment. Oman Med J. 2020;35(3):e125. https://doi.org/10.5001/omj.2020.43. [publishedOnlineFirst:2020/06/04].
Cipresso P, Giglioli IAC, Raya MA, et al. The past, present, and future of virtual and augmented reality research: a network and cluster analysis of the literature. Front Psychol. 2018;9:2086. https://doi.org/10.3389/fpsyg.2018.02086. [publishedOnlineFirst:2018/11/22].
Bun P, Gorski F, Grajewski D, et al. Low–cost devices used in virtual reality exposure therapy. Procedia Comput Sci. 2017;104:445–51.
Georgescu R, Fodor LA, Dobrean A, et al. Psychological interventions using virtual reality for pain associated with medical procedures: a systematic review and meta-analysis. Psychol Med. 2020;50(11):1795–807. https://doi.org/10.1017/S0033291719001855. [publishedOnlineFirst:2019/08/28].
Scapin S, Echevarría-Guanilo ME, BoeiraFuculo Junior PR, et al. Virtual Reality in the treatment of burn patients: a systematic review. Burns. 2018;44(6):1403–16. https://doi.org/10.1016/j.burns.2017.11.002.
Perdue MJ, Umar MA, Walker JD, Kubena B. Immersive Virtual Reality for Pain Control and Anxiolysis During IV Blood Draws in Adults: A Randomized Controlled Trial. Mil Med. 2022:usac249. https://doi.org/10.1093/milmed/usac249.
Yıldırım BG, Gerçeker GÖ. The Effect of Virtual Reality and Buzzy on First Insertion Success, Procedure-Related Fear, Anxiety, and Pain in Children during Intravenous Insertion in the Pediatric Emergency Unit: A Randomized Controlled Trial. J Emerg Nurs. 2023;49(1):62–74. https://doi.org/10.1016/j.jen.2022.09.018.
Xie J, Zeng Q. Application of virtual reality technology combined with moderate perineal protection in natural childbirth. Ginekologia Polska. 2022;0(0). https://doi.org/10.5603/GP.a2022.0134.
Wang Y, Guo L, Xiong X. Effects of virtual reality-based distraction of pain, fear, and anxiety during needle-related procedures in children and adolescents. Front Psychol. 2022;13:842847.
Thybo KH, Friis SM, Aagaard G, et al. A randomized controlled trial on virtual reality distraction during venous cannulation in young children. Acta Anaesthesiol Scand. 2022;66(9):1077–82. https://doi.org/10.1111/aas.14120.
Ryu JH, Oh AY, Yoo HJ, et al. The effect of an immersive virtual reality tour of the operating theater on emergence delirium in children undergoing general anesthesia: a randomized controlled trial. Pediatr Anesth. 2019;29(1):98–105. https://doi.org/10.1111/pan.13535.
Luo W, Chen C, Zhou W, Cao A, Zhu W, Zhou Y, et al. Biophilic virtual reality on children's anxiety and pain during circumcision: A randomized controlled study. J Pediatr Urol. 2023;19(2):201–10. https://doi.org/10.1016/j.jpurol.2022.10.023.
Liu Q, Zang Y, Zang W, Cai W, Li W, Guo Y, et al. Implementation of virtual reality technology to decrease patients' pain and nervousness during colonoscopies: a prospective randomised controlled single-blinded trial. Clin Med (Lond). 2022;22(3):237–40. https://doi.org/10.7861/clinmed.2022-0001.
Leopold I, et al. Virtual Reality and its Effect on the Reduction of Pain During Interventional Radiology Procedures. Abstract No. 14 Virtual reality and its effect on reduction of pain during interventional radiology procedures. Journal of Vascular and Interventional Radiology. Conference: SIR 2022 Annual Scientific Meeting Program. Boston United States. 33(6 Supplement) (pp S8), 2022. Date of Publication: June 2022.
Ketsuwan C, Matang W, Ratanapornsompong W, Sangkum P, Phengsalae Y, Kongchareonsombat W, Jongwannasiri M. Prospective randomized controlled trial to evaluate effectiveness of virtual reality to decrease anxiety in office-based flexible cystoscopy patients. World J Urol. 2022;40(10):2575–81. https://doi.org/10.1007/s00345-022-04142-9.
Kaya M, Karaman Özlü Z. The effect of virtual reality on pain, anxiety, and fear during burn dressing in children: A randomized controlled study. Burns. 2022;S0305-4179(22):00143–7. https://doi.org/10.1016/j.burns.2022.06.001.
Hundert AS, Birnie KA, Abla O, Positano K, Cassiani C, Lloyd S, et al. A Pilot Randomized Controlled Trial of Virtual Reality Distraction to Reduce Procedural Pain During Subcutaneous Port Access in Children and Adolescents With Cancer. Clin J Pain. 2021;38(3):189–96. https://doi.org/10.1097/AJP.0000000000001017.
Hsu MF, Whu YW, Lin IC, Liu CY, Lai FC, Liu PC, Chen CW. Effectiveness of Virtual Reality Interactive Play for Children During Intravenous Placement: A Randomized Controlled Trial. Asian Nurs Res (Korean Soc Nurs Sci). 2022;16(2):87–93. https://doi.org/10.1016/j.anr.2022.03.002.
Goergen DI, Freitas DMO. Virtual Reality as a distraction therapy during cystoscopy: a clinical trial. Rev Col Bras Cir. 2022;49:e20223138. https://doi.org/10.1590/0100-6991e-20223138-en.
Genç H, Korkmaz M, Akkurt A. The effect of virtual reality glasses and stress balls on pain and vital findings during transrectal prostate biopsy: a randomized controlled trial. J PeriAnesth Nurs. 2022;37(3):344–50. https://doi.org/10.1016/j.jopan.2021.09.006.
Fouks Y, Kern G, Cohen A, Reicher L, Shapira Z, Many A, et al. A virtual reality system for pain and anxiety management during outpatient hysteroscopy-A randomized control trial. Eur J Pain. 2022;26(3):600–9. https://doi.org/10.1002/ejp.1882.
Ebrahimian A, Bilandi RR, Bilandī MRR, Sabzeh Z. Comparison of the effectiveness of virtual reality and chewing mint gum on labor pain and anxiety: a randomized controlled trial. BMC Pregnancy Childbirth. 2022;22(1):49. https://doi.org/10.1186/s12884-021-04359-3.
Chang ZY, Kang GC, Koh EYL, Fong RJK, Tang J, Goh CK, Tan NC. Immersive Virtual Reality in Alleviating Pain and Anxiety in Children During Immunization in Primary Care: A Pilot Randomized Controlled Trial. Front Pediatr. 2022;10:847257. https://doi.org/10.3389/fped.2022.847257.
Carus EG, Albayrak N, Bildirici HM, Ozmen SG. Immersive virtual reality on childbirth experience for women: a randomized controlled trial. BMC Pregnancy Childbirth. 2022;22(1):354. https://doi.org/10.1186/s12884-022-04598-y.
Brunn E, Cheney M, Hazen N, Morozov V, Robinson JK. Virtual-Reality Effects on Acute Pain During Office Hysteroscopy: A Randomized Controlled Trial. J Gynecol Surg. 2022;38(3):214–20.
Yesilot SB, Yeşilkuş R, Beyaz F. Use of virtual reality for reducing pain and anxiety after laparoscopic sleeve gastrectomy: a randomized controlled trial. Pain Manag Nurs. 2022;23(6):826–31. https://doi.org/10.1016/j.pmn.2022.07.001.
Bosso L, Espejo T, Taffé P, Caillet-Bois D, Christen T, Berna C, Hugli O. Analgesic and Anxiolytic Effects of Virtual Reality During Minor Procedures in an Emergency Department: A Randomized Controlled Study. Ann Emerg Med. 2023;81(1):84–94. https://doi.org/10.1016/j.annemergmed.2022.04.015.
Boonreunya N, Nopawong E, Yongsiriwit K, Chirapongsathorn S. Virtual reality distraction during upper gastrointestinal endoscopy: a randomized controlled trial. J Gastroenterol Hepatol. 2022;37(5):855–60. https://doi.org/10.1111/jgh.15786.
Atzori B, Vagnoli L, Graziani D, Hoffman HG, Sampaio M, Alhalabi W, et al. An Exploratory Study on the Effectiveness of Virtual Reality Analgesia for Children and Adolescents with Kidney Diseases Undergoing Venipuncture. Int J Environ Res Public Health. 2022;19(4):2291. https://doi.org/10.3390/ijerph19042291.
Mankoff SP, Brander C, Ferrone S, et al. Lost in translation: obstacles to translational medicine. J Transl Med. 2004;2(1):14. https://doi.org/10.1186/1479-5876-2-14. [publishedOnlineFirst:2004/05/20].
Ogourtsova T, Archambault PS, Lamontagne A. Exploring barriers and facilitators to the clinical use of virtual reality for post-stroke unilateral spatial neglect assessment. Disabil Rehabil. 2019;41(3):284–92. https://doi.org/10.1080/09638288.2017.1387292.
PROSPERO Registration. Virtual reality as analgesia for medical procedures and labour 2020. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020195919.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;1(88):105906.
Victor MM, Jon OE. TRIP database. Evid Based Med. 2002;7(4):104. https://doi.org/10.1136/ebm.7.4.104.
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. Cochrane Handb Syst Rev Interv. 2019:205–28.
Ding H, Hu GL, Zheng XY, et al. The method quality of cross-over studies involved in cochrane systematic reviews. PLoS ONE. 2015;10(4):e0120519. https://doi.org/10.1371/journal.pone.0120519.
Kontopantelis E, Reeves D. Performance of statistical methods for meta-analysis when true study effects are non-normally distributed: a comparison between DerSimonian-Laird and restricted maximum likelihood. Stat Methods Med Res. 2012;21:657–9. https://doi.org/10.1177/0962280211413451.
Harbord RM, Steichen T. METAREG: Stata module to perform meta-analysis regression. Software, Boston College Department of Economics, Statistical Software Components series. 2005.
Sterne JAC, Harbord R. Funnel plots in meta-analysis. Stata J. 2004;4(2):127–41.
Duval S, Tweedie R. A nonparametric, “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95(449):89–98. https://doi.org/10.1080/01621459.2000.10473905.
Muellerleile P, Mullen B. Sufficiency and stability of evidence for public health interventions using cumulative meta-analysis. Am J Public Health. 2006;96(3):515–22. https://doi.org/10.2105/ajph.2003.036343.
Piskorz JE, Czub M, Šulžickaja B, Kiliś-Pstrusińska K. Mobile virtual reality distraction reduces needle pain and stress in children?. Cyberpsychology. 2020;14(1):3. https://doi.org/10.5817/CP2020-1-3.
Asl Aminabadi N, Erfanparast L, Sohrabi A, Ghertasi Oskouei S, Naghili A. The impact of virtual reality distraction on pain and anxiety during dental treatment in 4–6 year-old children: a randomized controlled clinical trial. J Dent Res Dent Clin Dent Prospects. 2012 Fall;6(4):117–24. https://doi.org/10.5681/joddd.2012.025. Epub 2012 Nov 12. PMID: 23277857; PMCID: PMC3529924.
Niharika P, Reddy NV, Srujana P, Srikanth K, Daneswari V, Geetha KS. Effects of distraction using virtual reality technology on pain perception and anxiety levels in children during pulp therapy of primary molars. J Indian Soc Pedod Prev Dent. 2018;36(4):364–369. https://doi.org/10.4103/JISPPD.JISPPD_1158_17. PMID: 30324926.
Bentsen B, Svensson P, Wenzel A. Evaluation of effect of 3D video glasses on perceived pain and unpleasantness induced by restorative dental treatment. Eur J Pain. 2001;5(4):373–8. https://doi.org/10.1053/eujp.2001.0256. PMID: 11743703.
van Twillert B, Bremer M, Faber AW. Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. J Burn Care Res. 2007;28(5):694–702. https://doi.org/10.1097/BCR.0B013E318148C96F. PMID: 17667488.
Gershon J, Zimand E, Pickering M, Rothbaum BO, Hodges L. A pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatry. 2004;43(10):1243–9. https://doi.org/10.1097/01.chi.0000135621.23145.05. PMID: 15381891.
Morris LD, Louw QA, Crous LC. Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country. Burns. 2010;36(5):659–64. https://doi.org/10.1016/j.burns.2009.09.005. Epub 2009 Dec 21 PMID: 20022431.
Bani Mohammad E, Ahmad M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care. 2019;17(1):29–34. https://doi.org/10.1017/S1478951518000639. Epub 2018 Sep 10 PMID: 30198451.
Austin PD, Siddall PJ, Lovell MR. Feasibility and acceptability of virtual reality for cancer pain in people receiving palliative care: a randomised cross-over study. Support Care Cancer. 2022;30(5):3995–4005. https://doi.org/10.1007/s00520-022-06824-x. Epub 2022 Jan 21. PMID: 35064330; PMCID: PMC8782583.
Balanyuk I, Ledonne G, Provenzano M, Bianco R, Meroni C, Ferri P, Bonetti L. Distraction technique for pain reduction in peripheral venous catheterization: randomized, controlled trial. Acta Biomed. 2018;89(4-S):55–63. https://doi.org/10.23750/abm.v89i4-S.7115. PMID: 29644990; PMCID: PMC6357630.
Matheve T, Bogaerts K, Timmermans A. Virtual reality distraction induces hypoalgesia in patients with chronic low back pain: a randomized controlled trial. J Neuroeng Rehabil. 2020;17(1):55. https://doi.org/10.1186/s12984-020-00688-0. PMID:32321516;PMCID:PMC7178732.
Darnall BD, Krishnamurthy P, Tsuei J, Minor JD. Self-administered skills-based virtual reality intervention for chronic pain: randomized controlled pilot study. JMIR Form Res. 2020;4(7):e17293. https://doi.org/10.2196/17293. PMID:32374272;PMCID:PMC7381022.
Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, Patterson DR. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: preliminary results from 3 ongoing studies. Arch Phys Med Rehabil. 2007;88(12 Suppl 2):S43–9. https://doi.org/10.1016/j.apmr.2007.09.004. PMID: 18036981.
Sweta VR, Abhinav RP, Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Ann Maxillofac Surg. 2019;9(1):110–113. https://doi.org/10.4103/ams.ams_263_18. PMID: 31293937; PMCID: PMC6585215.
Wechsler TF, Pfaller M, van Eickels RE, Schulz LH, Mühlberger A. Look at the audience? A randomized controlled study of shifting attention from self-focus to nonsocial vs. social external stimuli during virtual reality exposure to public speaking in social anxiety. Front Psychiatry. 2021;12:751272. https://doi.org/10.3389/fpsyt.2021.751272. PMID: 34970163; PMCID: PMC8712494.
Lima Rebêlo F, de Souza Silva LF, Doná F, Sales Barreto A, de Souza Siqueira Quintans J. Immersive virtual reality is effective in the rehabilitation of older adults with balance disorders: a randomized clinical trial. Exp Gerontol. 2021;149:111308. https://doi.org/10.1016/j.exger.2021.111308. Epub 2021 Mar 18. PMID: 33744393.
Hoffman HG. Interacting with virtual objects via embodied avatar hands reduces pain intensity and diverts attention. Sci Rep. 2021;11(1):10672. https://doi.org/10.1038/s41598-021-89526-4. PMID:34021173;PMCID:PMC8140079.
Vlake JH, van Bommel J, Hellemons ME, Wils EJ, Gommers D, van Genderen ME. Intensive care unit-specific virtual reality for psychological recovery after ICU treatment for COVID-19; a brief case report. Front Med (Lausanne). 2021;5(7):629086. https://doi.org/10.3389/fmed.2020.629086. PMID:33614677;PMCID:PMC7892581.
Szczepańska-Gieracha J, Jóźwik S, Cieślik B, Mazurek J, Gajda R. Immersive virtual reality therapy as a support for cardiac rehabilitation: a pilot randomized-controlled trial. Cyberpsychol Behav Soc Netw. 2021;24(8):543–549. https://doi.org/10.1089/cyber.2020.0297. Epub 2021 Feb 11. PMID: 33577375; PMCID: PMC8377517.
Merlot B, Dispersyn G, Husson Z, Chanavaz-Lacheray I, Dennis T, Greco-Vuilloud J, Fougère M, Potvin S, Cotty-Eslous M, Roman H, Marchand S. Pain reduction with an immersive digital therapeutic tool in women living with endometriosis-related pelvic pain: randomized controlled trial. J Med Internet Res. 2022;24(9):e39531. https://doi.org/10.2196/39531. PMID:36129733;PMCID:PMC9536521.
Mueller J, Niederer D, Tenberg S, et al. Acute effects of game-based biofeedback training on trunk motion in chronic low back pain: a randomized cross-over pilot trial. BMC Sports Sci Med Rehabil. 2022;14:192. https://doi.org/10.1186/s13102-022-00586-z.
Portêlo A, Shiban Y, Maia TV. Mathematical characterization of changes in fear during exposure therapy. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6(11):1090–9. https://doi.org/10.1016/j.bpsc.2021.01.005. 33508496.
Powers MB, Carl E, Levihn-Coon A, Van Veldhuizen M, Caven A, Pogue J, Fresnedo M, Turner ED, Adams M, Leonard K, Conroy H, Lantrip C, Caven T, Isbell C, Regner J, Garmon E, Foreman M, Miller W, Fares LA, Carlbring P, Otto MW, Weiss DN, Hughes J, Bernhardt JM, Roy R, Oh J, Copt R, MacClements J, Warren AM, Rosenfield B, Rosenfield D, Minns S, Telch MJ, Smits JAJ. Nonpharmacologic pain management among hospitalized inpatients: a randomized waitlist-controlled trial of standard virtual reality (CGI VR) versus video capture VR (360 degrees 3D/Stereoscopic Video Capture VR). Clin J Pain. 2021;37(9):678–87. https://doi.org/10.1097/AJP.0000000000000958. PMID: 34265789.
Bulteau S, Laurin A, Bach-Ngohou K, Péré M, Vibet MA, Hardouin JB, Sebille V, Lagalice L, Faurel-Paul É, Acier D, Rabeyron T, Riche VP, Sauvaget A, Melki F, Vigier T, Perreira Da Silva M, Charlet O, Prié Y. Feasibility of combining transcranial direct current stimulation and active fully embodied virtual reality for visual height intolerance: a double-blind randomized controlled study. J Clin Med. 2022;11(2):345. https://doi.org/10.3390/jcm11020345. PMID: 35054039; PMCID: PMC8779186.
Arnfred B, Bang P, Hjorthøj C, Christensen CW, Stengaard Moeller K, Hvenegaard M, Agerskov L, Krog Gausboel U, Soe D, Wiborg P, Smith CIS, Rosenberg N, Nordentoft M. Group cognitive behavioural therapy with virtual reality exposure versus group cognitive behavioural therapy with in vivo exposure for social anxiety disorder and agoraphobia: a protocol for a randomised clinical trial. BMJ Open. 2022;12(2):e051147. https://doi.org/10.1136/bmjopen-2021-051147. PMID:35110313;PMCID:PMC8811551.
Birckhead B, Eberlein S, Alvarez G, Gale R, Dupuy T, Makaroff K, Fuller G, Liu X, Yu KS, Black JT, Ishimori M, Venuturupalli S, Tu J, Norris T, Tighiouart M, Ross L, McKelvey K, Vrahas M, Danovitch I, Spiegel B. Home-based virtual reality for chronic pain: protocol for an NIH-supported randomised-controlled trial. BMJ Open. 2021;11(6):e050545. https://doi.org/10.1136/bmjopen-2021-050545. PMID:34130965;PMCID:PMC8207994.
Patterson DR, Hoffman HG, Chambers G, Bennetts D, Hunner HH, Wiechman SA, Garcia-Palacios A, Jensen MP. Hypnotic enhancement of virtual reality distraction analgesia during thermal pain: a randomized trial. Int J Clin Exp Hypn. 2021;69(2):225–45. https://doi.org/10.1080/00207144.2021.1882259. Epub 2021 Mar 16. PMID: 33724890; PMCID: PMC8141382.
Lee HN, Bae W, Park JW, Jung JY, Hwang S, Kim DK, Kwak YH. Virtual reality environment using a dome screen for procedural pain in young children during intravenous placement: a pilot randomized controlled trial. PLoS ONE. 2021;16(8):e0256489. https://doi.org/10.1371/journal.pone.0256489. PMID:34464411;PMCID:PMC8407539.
Payne O, Smith V, Rolnik DL, et al. Virtual reality and its use in post-operative pain following laparoscopy: a feasibility study. Sci Rep. 2022;12:13137. https://doi.org/10.1038/s41598-022-17183-2.
Pandrangi VC, Shah SN, Bruening JD, Wax MK, Clayburgh D, Andersen PE, Li RJ. Effect of virtual reality on pain management and opioid use among hospitalized patients after head and neck surgery: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2022;148(8):724–30. https://doi.org/10.1001/jamaoto.2022.1121. PMID:35679057;PMCID:PMC9185522.
Lee HN, Park JW, Hwang S, Jung JY, Kim DK, Kwak YH, Lee EJ. Effect of a virtual reality environment using a domed ceiling screen on procedural pain during intravenous placement in young children: a randomized clinical trial. JAMA Pediatr. 2023;177(1):25–31. https://doi.org/10.1001/jamapediatrics.2022.4426. PMID:36409508;PMCID:PMC9679961.
Spiegel B, Fuller G, Lopez M, Dupuy T, Noah B, Howard A, Albert M, Tashjian V, Lam R, Ahn J, Dailey F, Rosen BT, Vrahas M, Little M, Garlich J, Dzubur E, IsHak W, Danovitch I. Virtual reality for management of pain in hospitalized patients: a randomized comparative effectiveness trial. PLoS ONE. 2019;14(8):e0219115. https://doi.org/10.1371/journal.pone.0219115. PMID:31412029;PMCID:PMC6693733.
Umezawa S, Higurashi T, Uchiyama S, Sakai E, Ohkubo H, Endo H, Nonaka T, Nakajima A. Visual distraction alone for the improvement of colonoscopy-related pain and satisfaction. World J Gastroenterol. 2015;21(15):4707–14. https://doi.org/10.3748/wjg.v21.i15.4707. PMID:25914482;PMCID:PMC4402320.
Patterson DR, Jensen MP, Wiechman SA, Sharar SR. Virtual reality hypnosis for pain associated with recovery from physical trauma. Int J Clin Exp Hypn. 2010;58(3):288–300. https://doi.org/10.1080/00207141003760595. PMID:20509069;PMCID:PMC2913598.
Turrado V, Guzmán Y, Jiménez-Lillo J, Villegas E, de Lacy FB, Blanch J, Balibrea JM, Lacy A. Exposure to virtual reality as a tool to reduce peri-operative anxiety in patients undergoing colorectal cancer surgery: a single-center prospective randomized clinical trial. Surg Endosc. 2021;35(7):4042–7. https://doi.org/10.1007/s00464-021-08407-z. Epub 2021 Mar 8 PMID: 33683433.
Jóźwik S, Cieślik B, Gajda R, Szczepańska-Gieracha J. Evaluation of the impact of virtual reality-enhanced cardiac rehabilitation on depressive and anxiety symptoms in patients with coronary artery disease: a randomised controlled trial. J Clin Med. 2021;10(10):2148. https://doi.org/10.3390/jcm10102148. PMID:34065625;PMCID:PMC8156884.
Solcà M, Krishna V, Young N, Deogaonkar M, Herbelin B, Orepic P, Mange R, Rognini G, Serino A, Rezai A, Blanke O. Enhancing analgesic spinal cord stimulation for chronic pain with personalized immersive virtual reality. Pain. 2021;162(6):1641–9. https://doi.org/10.1097/j.pain.0000000000002160. PMID: 33259460.
Esposito C, Autorino G, Iervolino A, Vozzella EA, Cerulo M, Esposito G, Coppola V, Carulli R, Cortese G, Gallo L, Escolino M. Efficacy of a virtual reality program in pediatric surgery to reduce anxiety and distress symptoms in the preoperative phase: a prospective randomized clinical trial. J Laparoendosc Adv Surg Tech A. 2022;32(2):197–203. https://doi.org/10.1089/lap.2021.0566. Epub 2021 Dec 28 PMID: 34962159.
Li X, Huang J, Kong Z, Sun F, Sit CHP, Li C. Effects of virtual reality-based exercise on physical fitness in people with intellectual disability: a systematic review of randomized controlled trials. Games Health J. 2023;12(2):89–99. https://doi.org/10.1089/g4h.2022.0168. Epub 2023 Jan 27 PMID: 36716183.
Rodríguez-Hernández M, Criado-Álvarez JJ, Corregidor-Sánchez AI, Martín-Conty JL, Mohedano-Moriano A, Polonio-López B. Effects of virtual reality-based therapy on quality of life of patients with subacute stroke: a three-month follow-up randomized controlled trial. Int J Environ Res Public Health. 2021;18(6):2810. https://doi.org/10.3390/ijerph18062810. PMID:33801969;PMCID:PMC7999196.
Nusser M, Knapp S, Kramer M, Krischak G. Effects of virtual reality-based neck-specific sensorimotor training in patients with chronic neck pain: a randomized controlled pilot trial. J Rehabil Med. 2021;53(2):jrm00151. https://doi.org/10.2340/16501977-2786. PMID: 33369684; PMCID: PMC8814879.
Wong CL, Lui MMW, Choi KC. Effects of immersive virtual reality intervention on pain and anxiety among pediatric patients undergoing venipuncture: a study protocol for a randomized controlled trial. Trials. 2019;20:369. https://doi.org/10.1186/s13063-019-3443-z.
Özalp Gerçeker G, Ayar D, Özdemir EZ, Bektaş M. Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5-12 years old: A randomised controlled study. J Clin Nurs. 2020;29(7–8):1151–61. https://doi.org/10.1111/jocn.15173.
Özkan TK, Polat F. The Effect of Virtual Reality and Kaleidoscope on Pain and Anxiety Levels During Venipuncture in Children. J Perianesth Nurs. 2020;35(2):206–11. https://doi.org/10.1016/j.jopan.2019.08.010.
Semerci R, Akgün Kostak M, Eren T, Avci G. Effects of Virtual Reality on Pain During Venous Port Access in Pediatric Oncology Patients: A Randomized Controlled Study. J Pediatr Oncol Nurs. 2020;38(2):142–51. https://doi.org/10.1177/1043454220975702.
Wong MS, Spiegel BMR, Gregory KD. Virtual Reality Reduces Pain in Laboring Women: A Randomized Controlled Trial. Am J Perinatol. 2021b;38(S 01):e167–72. https://doi.org/10.1055/s-0040-1708851.
Le May S, Tsimicalis A, Noel M, et al. Immersive virtual reality vs. non-immersive distraction for pain management of children during bone pins and sutures removal: a randomized clinical trial protocol. J Adv Nurs. 2021;77(1):439–47. https://doi.org/10.1111/jan.14607. [published Online First: 2020/10/25].
Hoffman HG, Rodriguez RA, Gonzalez M, Bernardy M, Peña R, Beck W, et al. Immersive Virtual Reality as an Adjunctive Non-opioid Analgesic for Pre-dominantly Latin American Children With Large Severe Burn Wounds During Burn Wound Cleaning in the Intensive Care Unit: A Pilot Study. Front Hum Neurosci. 2019;13:262. https://doi.org/10.3389/fnhum.2019.00262.
Ding J, He Y, Chen L, Zhu B, Cai Q, Chen K, Liu G. Virtual reality distraction decreases pain during daily dressing changes following haemorrhoid surgery. J Int Med Res. 2019;47(9):4380–8. https://doi.org/10.1177/0300060519857862.
Atzori B, Hoffman HG, Vagnoli L, Patterson DR, Alhalabi W, Messeri A, Lauro Grotto R. Virtual Reality Analgesia During Venipuncture in Pediatric Patients With Onco-Hematological Diseases. Front Psychol. 2018;9:2508. https://doi.org/10.3389/fpsyg.2018.02508.
Carrougher GJ, Hoffman HG, Nakamura D, Lezotte D, Soltani M, Leahy L, Engrav LH, Patterson DR. The effect of virtual reality on pain and range of motion in adults with burn injuries. J Burn Care Res. 2009;30(5):785–91. https://doi.org/10.1097/BCR.0b013e3181b485d3.
Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008;24(4):299–304. https://doi.org/10.1097/AJP.0b013e318164d2cc.
JahaniShoorab N, EbrahimzadehZagami S, Nahvi A, et al. The effect of virtual reality on pain in primiparity women during episiotomy repair: a randomize clinical trial. Iran J Med Sci. 2015;40(3):219–24.
Sander Wint S, Eshelman D, Steele J, Guzzetta CE. Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncol Nurs Forum. 2002;29(1):E8–15. https://doi.org/10.1188/02.ONF.E8-E15.
Gold JI, Kim SH, Kant AJ, Joseph MH, Rizzo AS. Effectiveness of virtual reality for pediatric pain distraction during i.v. placement. Cyberpsychol Behav. 2006;9(2):207–12. https://doi.org/10.1089/cpb.2006.9.207.
Konstantatos AH, Angliss M, Costello V, Cleland H, Stafrace S. Predicting the effectiveness of virtual reality relaxation on pain and anxiety when added to PCA morphine in patients having burns dressings changes. Burns. 2009;35(4):491–9. https://doi.org/10.1016/j.burns.2008.08.017.
Litwin SP, Nguyen C, Hundert A, Stuart S, Liu D, Maguire B, Matava C, Stinson J. Virtual Reality to Reduce Procedural Pain During IV Insertion in the Pediatric Emergency Department: A Pilot Randomized Controlled Trial. Clin J Pain. 2021;37(2):94–101. https://doi.org/10.1097/AJP.0000000000000894.
Huang MY, Scharf S, Chan PY. Effects of immersive virtual reality therapy on intravenous patient-controlled sedation during orthopaedic surgery under regional anesthesia: A randomized controlled trial. PLoS One. 2020;15(2):e0229320. https://doi.org/10.1371/journal.pone.0229320.
Erdogan B, Aytekin Ozdemir A. The Effect of Three Different Methods on Venipuncture Pain and Anxiety in Children: Distraction Cards, Virtual Reality, and Buzzy® (Randomized Controlled Trial). J Pediatr Nurs. 2021;58:e54–62. https://doi.org/10.1016/j.pedn.2021.01.001.
Gray ML, Goldrich DY, McKee S, Schaberg M, Del Signore A, Govindaraj S, Iloreta AM. Virtual Reality as Distraction Analgesia for Office-Based Procedures: A Randomized Crossover-Controlled Trial. Otolaryngol Head Neck Surg. 2021;164(3):580–8. https://doi.org/10.1177/0194599820942215.
Gerçeker GÖ, Bektaş M, Aydınok Y, Ören H, Ellidokuz H, Olgun N. The effect of virtual reality on pain, fear, and anxiety during access of a port with huber needle in pediatric hematology-oncology patients: Randomized controlled trial. Eur J Oncol Nurs. 2021;50:101886. https://doi.org/10.1016/j.ejon.2020.101886.
Chen YJ, Cheng SF, Lee PC, Lai CH, Hou IC, Chen CW. Distraction using virtual reality for children during intravenous injections in an emergency department: A randomised trial. J Clin Nurs. 2020;29(3–4):503–10. https://doi.org/10.1111/jocn.15088.
Deo N, Khan KS, Mak J, Allotey J, Gonzalez Carreras FJ, Fusari G, Benn J. Virtual reality for acute pain in outpatient hysteroscopy: a randomised controlled trial. BJOG. 2021;128(1):87–95. https://doi.org/10.1111/1471-0528.16377.
Dumoulin S, Bouchard S, Ellis J, Lavoie KL, Vézina MP, Charbonneau P, et al. A Randomized Controlled Trial on the Use of Virtual Reality for Needle-Related Procedures in Children and Adolescents in the Emergency Department. Games Health J. 2019;8(4):285–93. https://doi.org/10.1089/g4h.2018.0111.
Chan E, Hovenden M, Ramage E, Ling N, Pham JH, Rahim A, et al. Virtual Reality for Pediatric Needle Procedural Pain: Two Randomized Clinical Trials. J Pediatr. 2019;209:160–7.e4. https://doi.org/10.1016/j.jpeds.2019.02.034.
Chan EA, Chung JW, Wong TK, Lien AS, Yang JY. Application of a virtual reality prototype for pain relief of pediatric burn in Taiwan. J Clin Nurs. 2007;16(4):786–93. https://doi.org/10.1111/j.1365-2702.2006.01719.x.
Das DA, Grimmer KA, Sparnon AL, McRae SE, Thomas BH. The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomized controlled trial [ISRCTN87413556]. BMC Pediatr. 2005;5(1):1. https://doi.org/10.1186/1471-2431-5-1.
Frey DP, Bauer ME, Bell CL, Low LK, Hassett AL, Cassidy RB, Boyer KD, Sharar SR. Virtual Reality Analgesia in Labor: The VRAIL Pilot Study-A Preliminary Randomized Controlled Trial Suggesting Benefit of Immersive Virtual Reality Analgesia in Unmedicated Laboring Women. Anesth Analg. 2019;128(6):e93–6. https://doi.org/10.1213/ANE.0000000000003649.
Gerçeker GÖ, Binay Ş, Bilsin E, Kahraman A, Yılmaz HB. Effects of Virtual Reality and External Cold and Vibration on Pain in 7- to 12-Year-Old Children During Phlebotomy: A Randomized Controlled Trial. J Perianesth Nurs. 2018;33(6):981–9. https://doi.org/10.1016/j.jopan.2017.12.010.
Gold JI, Mahrer NE. Is Virtual Reality Ready for Prime Time in the Medical Space? A Randomized Control Trial of Pediatric Virtual Reality for Acute Procedural Pain Management. J Pediatr Psychol. 2018;43(3):266–75. https://doi.org/10.1093/jpepsy/jsx129.
Guo C, Deng H, Yang J. Effect of virtual reality distraction on pain among patients with hand injury undergoing dressing change. J Clin Nurs. 2015;24(1–2):115–20. https://doi.org/10.1111/jocn.12626.
Maani CV, Hoffman HG, Morrow M, Maiers A, Gaylord K, McGhee LL, DeSocio PA. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. J Trauma. 2011;71(1 Suppl):S125–30. https://doi.org/10.1097/TA.0b013e31822192e2.
McSherry T, Atterbury M, Gartner S, et al. Randomized, crossover study of immersive virtual reality to decrease opioid use during painful wound care procedures in adults. J Burn Care Res. 2018;39(2):278–85. https://doi.org/10.1097/bcr.0000000000000589.
Hoffman HG, Patterson DR, Carrougher GJ, Sharar SR. Effectiveness of virtual reality-based pain control with multiple treatments. Clin J Pain. 2001;17(3):229–35. https://doi.org/10.1097/00002508-200109000-00007.
Akin B, Yilmaz Kocak M, Küçükaydın Z, Güzel K. The Effect of Showing Images of the Foetus with the Virtual Reality Glass During Labour Process on Labour Pain, Birth Perception and Anxiety. J Clin Nurs. 2021;30(15–16):2301–8. https://doi.org/10.1111/jocn.15768.
Aydın Aİ, Özyazıcıoğlu N. Using a Virtual Reality Headset to Decrease Pain Felt During a Venipuncture Procedure in Children. J Perianesth Nurs. 2019;34(6):1215–21. https://doi.org/10.1016/j.jopan.2019.05.134.
Basak T, Demirtas A, Yorubulut SM. Virtual reality and distraction cards to reduce pain during intramuscular benzathine penicillin injection procedure in adults: A randomized controlled trial. J Adv Nurs. 2021;77(5):2511–8. https://doi.org/10.1111/jan.14782.
Bozdoğan Yeşilot S, Ciftci H, Yener MK. Using a Virtual Reality and Communication Intervention to Reduce Pain and Anxiety in Patients Undergoing Lipoma Excision With Local Anesthesia: A Randomized Controlled Trial. AORN J. 2022;115(5):437–49. https://doi.org/10.1002/aorn.13665.
Karaveli Çakır S, Evirgen S. The Effect of Virtual Reality on Pain and Anxiety During Colonoscopy: A Randomized Controlled Trial. Turk J Gastroenterol. 2021;32(5):451–7. https://doi.org/10.5152/tjg.2021.191081.
Canares T, Parrish C, Santos C, Badawi A, Kleinman K, Stewart A, et al. Optimizing Coping during Venipuncture Procedures with Virtual Reality in the Pediatric Emergency Department: A Randomized Controlled Trial. Pediatrics. 2021;147(3_MeetingAbstract):307–8.
Clerc PGB, Arneja JS, Zwimpfer CM, Behboudi A, Goldman RD. A Randomized Controlled Trial of Virtual Reality in Awake Minor Pediatric Plastic Surgery Procedures. Plast Reconstr Surg. 2021;148(2):400–8. https://doi.org/10.1097/PRS.0000000000008196.
Estrella-Juarez F, Requena-Mullor M, Garcia-Gonzalez J, Lopez-Villen A, Alarcon-Rodriguez R. Effect of Virtual Reality and Music Therapy on the Physiologic Parameters of Pregnant Women and Fetuses and on Anxiety Levels: A Randomized Controlled Trial. J Midwifery Womens Health. 2023;68(1):35–43. https://doi.org/10.1111/jmwh.13413.
Gold JI, SooHoo M, Laikin AM, Lane AS, Klein MJ. Effect of an Immersive Virtual Reality Intervention on Pain and Anxiety Associated With Peripheral Intravenous Catheter Placement in the Pediatric Setting: A Randomized Clinical Trial. JAMA Netw Open. 2021;4(8):e2122569. https://doi.org/10.1001/jamanetworkopen.2021.22569.
Goldman RD, Behboudi A. Pilot Randomized Controlled Trial of Virtual Reality vs. Standard-of-Care During Pediatric Laceration Repair. J Child Adolesc Trauma. 2021a;14(2):295–8. https://doi.org/10.1007/s40653-021-00350-4.
Goldman RD, Behboudi A. Virtual reality for intravenous placement in the emergency department-a randomized controlled trial. Eur J Pediatr. 2021b;180(3):725–31. https://doi.org/10.1007/s00431-020-03771-9.
Hua Y, Qiu R, Yao WY, Zhang Q, Chen XL. The Effect of Virtual Reality Distraction on Pain Relief During Dressing Changes in Children with Chronic Wounds on Lower Limbs. Pain Manag Nurs. 2015;16(5):685–91. https://doi.org/10.1016/j.pmn.2015.03.001.
Jeffs D, Dorman D, Brown S, Files A, Graves T, Kirk E, et al. Effect of virtual reality on adolescent pain during burn wound care. J Burn Care Res. 2014;35(5):395–408. https://doi.org/10.1097/BCR.0000000000000019.
Joo Y, Kim EK, Song HG, Jung H, Park H, Moon JY. Effectiveness of virtual reality immersion on procedurerelated pain and anxiety in outpatient pain clinic: an exploratory randomized controlled trial. Korean J Pain. 2021;34(3):304–14. https://doi.org/10.3344/kjp.2021.34.3.304.
Karaman D, Taşdemir N. The Effect of Using Virtual Reality During Breast Biopsy on Pain and Anxiety: A Randomized Controlled Trial. J Perianesth Nurs. 2021;36(6):702–5. https://doi.org/10.1016/j.jopan.2021.04.007.
Kipping B, Rodger S, Miller K, Kimble RM. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns. 2012;38(5):650–7. https://doi.org/10.1016/j.burns.2011.11.010.
Liu KY, Ninan SJ, Laitman BM, Goldrich DY, Iloreta AM, Londino AV 3rd. Virtual Reality as Distraction Analgesia and Anxiolysis for Pediatric Otolaryngology Procedures. Laryngoscope. 2021;131(5):E1714–21. https://doi.org/10.1002/lary.29148.
Łuczak M, Nowak Ł, Chorbińska J, Galik K, Kiełb P, Łaszkiewicz J, et al. Influence of Virtual Reality Devices on Pain and Anxiety in Patients Undergoing Cystoscopy Performed under Local Anaesthesia. J Pers Med. 2021;11(11):1214. https://doi.org/10.3390/jpm11111214.
Melcer Y, Maymon R, Gal-Kochav M, Pekar-Zlotin M, Levinsohn-Tavor O, Meizner I, Svirsky R. Analgesic efficacy of virtual reality for acute pain in amniocentesis: A randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2021;261:134–8. https://doi.org/10.1016/j.ejogrb.2021.04.024.
Momenyan N, Safaei AA, Hantoushzadeh S. Immersive virtual reality analgesia in unmedicated laboring women (during stage 1 and 2): a randomized controlled trial. Clin Exp Obstet Gynecol. 2021;48(1):110–6. https://doi.org/10.31083/j.ceog.2021.01.2116.
Osmanlliu E, Trottier ED, Bailey B, Lagacé M, Certain M, Khadra C, et al. Distraction in the Emergency department using Virtual reality for INtravenous procedures in Children to Improve comfort (DEVINCI): a pilot pragmatic randomized controlled trial. CJEM. 2021;23(1):94–102. https://doi.org/10.1007/s43678-020-00006-6.
Özsoy F, Ulus B. Comparison of Two Different Methods in Reducing Pain and Fear Due to Dressing Change in 7-10 Years Old Children. 2022;9(1):0–0.
Pathoulas JT, Flanagan KE, Walker CJ, et al. Use of virtual reality during scalp injections: a randomized interventional crossover study. J Am Acad Dermatol. 2022;87(5):1091–3. https://doi.org/10.1016/j.jaad.2021.12.048.
Pratiw IG, Husin F, Ganiem AR, Susiarno H, Arifin A, Wirakusuma F. The Effect of Virtual Reality on Pain in Primiparity Women. Int J Nurs Health Sci. 2017;4(4)46–50.
Ryu JH, Han SH, Hwang SM, Lee J, Do SH, Kim JH, Park JW. Effects of Virtual Reality Education on Procedural Pain and Anxiety During Venipuncture in Children: A Randomized Clinical Trial. Front Med (Lausanne). 2022;9:849541. https://doi.org/10.3389/fmed.2022.849541.
Schlechter AK, Whitaker W, Iyer S, Gabriele G, Wilkinson M. Virtual reality distraction during pediatric intravenous line placement in the emergency department: A prospective randomized comparison study. Am J Emerg Med. 2021;44:296–9. https://doi.org/10.1016/j.ajem.2020.04.009.
Schmitt YS, Hoffman HG, Blough DK, Patterson DR, Jensen MP, Soltani M, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns. 2011;37(1):61–8. https://doi.org/10.1016/j.burns.2010.07.007.
Smith V, Warty RR, Kashyap R, Neil P, Adriaans C, Nair A, Krishnan S, Da Silva Costa F, Vollenhoven B, Wallace EM. A randomised controlled trial to assess the feasibility of utilising virtual reality to facilitate analgesia during external cephalic version. Sci Rep. 2020;10(1):3141. https://doi.org/10.1038/s41598-020-60040-3.
Soltani M, Drever SA, Hoffman HG, Sharar SR, Wiechman SA, Jensen MP, Patterson DR. Virtual reality analgesia for burn joint flexibility: A randomized controlled trial. Rehabil Psychol. 2018;63(4):487–94. https://doi.org/10.1037/rep0000239.
Stunden C, Stratton K, Zakani S, Jacob J. Comparing a Virtual Reality-Based Simulation App (VR-MRI) With a Standard Preparatory Manual and Child Life Program for Improving Success and Reducing Anxiety During Pediatric Medical Imaging: Randomized Clinical Trial. J Med Internet Res. 2021;23(9):e22942. https://doi.org/10.2196/22942.
Top FU, Ayyıldız TK. Pain management in children during invasive procedures: A randomized clinical trial. Nurs Forum. 2021;56(4):816–22. https://doi.org/10.1111/nuf.12616.
Walker MR, Kallingal GJ, Musser JE, Folen R, Stetz MC, Clark JY. Treatment efficacy of virtual reality distraction in the reduction of pain and anxiety during cystoscopy. Mil Med. 2014;179(8):891–6. https://doi.org/10.7205/MILMED-D-13-00343.
Walther-Larsen S, Petersen T, Friis SM, Aagaard G, Drivenes B, Opstrup P. Immersive Virtual Reality for Pediatric Procedural Pain: A Randomized Clinical Trial. Hosp Pediatr. 2019;9(7):501–7. https://doi.org/10.1542/hpeds.2018-0249.
Wang Q, Xu S, Guo B, Xu Y, Lu W. Virtual reality as an adjunctive non-pharmacological therapy to reduce pain in school-aged children with burn wounds. J Burn Care Res. 2022:irac149. https://doi.org/10.1093/jbcr/irac149. Epub ahead of print.
Wolitzky K, Fivush R, Zimand E, Hodges L, Rothbaum BO. Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychol Health. 2005;20(6):817–24, https://doi.org/10.1080/14768320500143339.
Wong CL, Li CK, Chan CWH, Choi KC, Chen J, Yeung MT, Chan ON. Virtual Reality Intervention Targeting Pain and Anxiety Among Pediatric Cancer Patients Undergoing Peripheral Intravenous Cannulation: A Randomized Controlled Trial. Cancer Nurs. 2021a;44(6):435–42. https://doi.org/10.1097/NCC.0000000000000844.
Xiang H, Shen J, Wheeler KK, Patterson J, Lever K, Armstrong M, et al. Efficacy of Smartphone Active and Passive Virtual Reality Distraction vs Standard Care on Burn Pain Among Pediatric Patients: A Randomized Clinical Trial. JAMA Netw Open. 2021;4(6):e2112082. https://doi.org/10.1001/jamanetworkopen.2021.12082.
Schultheis MT, Himelstein J, Rizzo AA. Virtual reality and neuropsychology: upgrading the current tools. J Head Trauma Rehabil. 2002;17(5):378–94. https://doi.org/10.1097/00001199-200210000-00002.
Checa D, Bustillo A. A review of immersive virtual reality serious games to enhance learning and training. Multimed Tools Appl. 2020;79(9):5501–27. https://doi.org/10.1007/s11042-019-08348-9.
Development of virtual reality game-based interfaces for civil engineering education. 2017 IEEE Global Engineering Education Conference (EDUCON); 2017 25–28 April 2017.
Samadbeik M, Yaaghobi D, Bastani P, et al. The applications of virtual reality technology in medical groups teaching. J Adv Med Educ Prof. 2018;6(3):123–9. [published Online First: 2018/07/18].
Grunwald A. Technology assessment in practice and theory. Routledge; 2018.
Stone AB, Yuan CT, Rosen MA, et al. Barriers to and facilitators of implementing enhanced recovery pathways using an implementation framework: a systematic review. JAMA Surg. 2018;153(3):270–9. https://doi.org/10.1001/jamasurg.2017.5565. [publishedOnlineFirst:2018/01/19].
Eijlers R, Utens E, Staals LM, et al. Systematic review and meta-analysis of virtual reality in pediatrics: effects on pain and anxiety. Anesth Analg. 2019;129(5):1344–53. https://doi.org/10.1213/ane.0000000000004165. [publishedOnlineFirst:2019/05/29].
Navarro-Haro MV, López-del-Hoyo Y, Campos D, et al. Meditation experts try Virtual Reality Mindfulness: a pilot study evaluation of the feasibility and acceptability of Virtual Reality to facilitate mindfulness practice in people attending a Mindfulness conference. PLoS ONE. 2017;12(11):e0187777. https://doi.org/10.1371/journal.pone.0187777.
Eijlers R, Dierckx B, Staals LM, et al. Virtual reality exposure before elective day care surgery to reduce anxiety and pain in children: a randomised controlled trial. Eur J Anaesthesiol. 2019;36(10):728–37. https://doi.org/10.1097/eja.0000000000001059. [publishedOnlineFirst:2019/07/30].
Chi B, Chau B, Yeo E, et al. Virtual reality for spinal cord injury-associated neuropathic pain: systematic review. Ann Phys Rehabil Med. 2019;62(1):49–57. https://doi.org/10.1016/j.rehab.2018.09.006.
Mallari B, Spaeth EK, Goh H, et al. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019;12:2053–85. https://doi.org/10.2147/jpr.S200498. [publishedOnlineFirst:2019/07/17].
Chan E, Foster S, Sambell R, et al. Clinical efficacy of virtual reality for acute procedural pain management: a systematic review and meta-analysis. PLoS ONE. 2018;13(7):e0200987. https://doi.org/10.1371/journal.pone.0200987.
Delshad SD, Almario CV, Fuller G, et al. Economic analysis of implementing virtual reality therapy for pain among hospitalized patients. NPJ Digit Med. 2018;1:22. https://doi.org/10.1038/s41746-018-0026-4. [publishedOnlineFirst:2019/07/16].
Rogozińska E, Marlin N, Thangaratinam S, et al. Meta-analysis using individual participant data from randomised trials: opportunities and limitations created by access to raw data. Evid Based Med. 2017;22(5):157–62. https://doi.org/10.1136/ebmed-2017-110775.
Acknowledgements
None.
Funding
No direct funding was provided to support this work. MPR is funded by the Medical Research Council Centre for Reproductive Health Grant. Grant No: MR/N022556/1. KSK is a Distinguished Investigator funded by the Beatriz Galindo (senor modality) Program grant given to the University of Granada by the Ministry of Science, Innovation, and Universities of the Spanish Government.
Author information
Authors and Affiliations
Contributions
JJT, MPR, and BW conceived the idea, undertook the analysis, and prepared the manuscript. DP, SH, RP, and AK undertook the literature search, data extraction, and drafted the manuscript. KK supported the project from conception, data analysis, and prepared the manuscript. All authors approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study used aggregate data of published trials and therefore is exempt from ethics approval. Participant consent is not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix S1.
Search strategy to identify relevant randomised trials evaluating the effectiveness of virtual reality for pain control in medical procedures. Appendix S2. List of studies excluded from the systematic review on the effectiveness of virtual reality for pain control in medical procedures. Appendix S3. List of studies excluded from the meta-analysis due to limited outcome reporting. Figure S1. Risk of bias in included randomised trials evaluating the effectiveness of virtual reality for pain control in medical procedures. Figure S2. Subgroup meta-analyses on the effectiveness of VR technology for pain control compared to routine care across different medical procedures. Figure S3. Funnel, Galbraith, and Trim and fill funnel plots evaluating risk of publication bias in randomised trials evaluating the effectiveness of VR technology for pain control compared to routine care across different medical procedures. Figure S4. One-out and sensitivity meta-analysis excluding outlier studies evaluating the effectiveness of VR technology for pain control compared to routine care across different medical procedures. Figure S5. Meta-analysis on the effectiveness of VR technology on anxiety compared to routine care across different medical procedures. Figure S6. Subgroup meta-analyses on the effectiveness of VR technology on anxiety compared to routine care across different medical procedures. Figure S7. Prediction intervals for the pooled effect size on pain reduction with the use of VR technology compared to routine care across all comparable populations. Table S1. Characteristics of randomised trials evaluating the effectiveness of virtual reality for pain control in medical procedures. Table S2. Meta-regression evaluating the impact of covariates on the effectiveness of VR technology on pain control across different covariates.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Teh, J.J., Pascoe, D.J., Hafeji, S. et al. Efficacy of virtual reality for pain relief in medical procedures: a systematic review and meta-analysis. BMC Med 22, 64 (2024). https://doi.org/10.1186/s12916-024-03266-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03266-6