Abstract
Background
Regarding primary and secondary cervical cancer prevention, the World Health Organization proposed the cervical cancer elimination strategy that requires countries to achieve 90% uptake of human papillomavirus (HPV) vaccines and 70% screening uptake. The optimal cervical screening strategy is likely different for unvaccinated and vaccinated cohorts upon national HPV immunization. However, health authorities typically only provide a one-size-fits-all recommendation for the general population. We aimed to evaluate the cost-effectiveness for determining the optimal screening strategies for vaccinated and unvaccinated cohorts.
Methods
We considered the women population in Hong Kong which has a unique HPV infection and cervical cancer epidemiology compared to other regions in China and Asia. We used mathematical models which comprise a deterministic age-structured compartmental dynamic component and a stochastic individual-based cohort component to evaluate the cost-effectiveness of screening strategies for cervical screening. Following the recommendations in local guidelines in Hong Kong, we considered strategies that involved cytology, HPV testing, or co-testing as primary cervical screening. We also explored the impacts of adopting alternative de-intensified strategies for vaccinated cohorts. The 3-year cytology screening was used as the base comparator while no screening was also considered for vaccinated cohorts. Women’s lifetime life years, quality-adjusted life years, and costs of screening and treatment were estimated from the societal perspective based on the year 2022 and were discounted by 3% annually. Incremental cost-effectiveness ratios (ICERs) were compared to a willingness to pay (WTP) threshold of one gross domestic product per capita (US $47,792). Probabilistic and one-way sensitivity analyses were conducted.
Results
Among unvaccinated cohorts, the strategy that adds reflex HPV to triage mild cytology abnormality generated more life years saved than cytology-only screening and could be a cost-effective alternative. Among vaccinated cohorts, when vaccine uptake was 85% (based on the uptake in 2022), all guideline-based strategies (including the cytology-only screening) had ICERs above the WTP threshold when compared with no screening if the vaccine-induced protection duration was 20 years or longer. Under the same conditions, HPV testing with genotyping triage had ICERs (compared with no screening) below the WTP threshold if the routine screening interval was lengthened to 10 and 15 years or screening was initiated at ages 30 and 35 years.
Conclusions
HPV testing is a cost-effective alternative to cytology for vaccinated cohorts, and the associated optimal screening frequency depends on vaccine uptake. Health authorities should optimize screening recommendations by accounting for population vaccine uptake.
Similar content being viewed by others
Background
Cervical cancer is one of the most common cancers among women, with more than 600,000 new cases and 340,000 cancer deaths in 2020 [1]. Regarding primary and secondary cervical cancer prevention, the World Health Organization (WHO) proposed that 90% of girls get fully vaccinated with human papillomavirus (HPV) vaccines by the age of 15 years and 70% of women get screened with a high-performance test (preferably an HPV DNA-based test) by age 35 and again by 45 years [2]. HPV vaccines are more than 90% efficacious against targeted oncogenic high-risk HPV (hrHPV) types; in particular, the second-generation nonavalent HPV (9vHPV) vaccine covers seven hrHPVs, which collectively cause more than 90% of cases of cervical cancer [3]. Over 100 countries have already included routine female HPV vaccination in their national immunization programs; however, vaccine uptake in most countries is well below 90% [4].
Upon vaccination, HPV prevalence in vaccinated cohorts drops through either direct vaccine-induced protection or indirect herd protection, with more substantial reductions in regions with higher vaccine uptake. With a lowered positive predictive value of screening, the benefit of frequent screening falls, and there is a greater risk of unnecessary referrals for colposcopy and unnecessary treatment of women with positive results [5, 6]. In populations where centralized healthcare systems are not mature and national immunization or screening programs are not yet implemented, the database for vaccination and screening records may not be linked well. On that occasion, it may not be easy to identify individuals’ vaccination status by the time when women attend cervical screening. Furthermore, from policymaking and administrative viewpoints, it may potentially be more feasible to adopt different cervical screening strategies for cohorts depending on whether they are of the ages eligible for vaccination due to the different risks of infection, rather than personal risks based on their vaccination status.
In countries such as Australia, Norway, and the UK that have commenced routine HPV vaccination for over a decade [4], the vaccinated cohorts have already reached or will soon reach the age of cervical screening, and updating screening recommendations is an urgent task. Most healthcare authorities provide screening guidelines for the entire population regardless of vaccination history. Recent literature has included discussions of the implementation of different cervical screening strategies per women’s vaccination status. Several modeling studies suggested that vaccinated women could be screened less frequently (when compared to unvaccinated women) for cervical screening remaining cost-effective on top of mass HPV vaccination [5, 7, 8]. In particular, the optimal number of lifetime screens may depend on the type of HPV vaccines received as well as population-specific disease epidemiology [9,10,11]. Most of these studies considered populations that have implemented mass HPV vaccination programs in the early phase when HPV vaccines were available on the market.
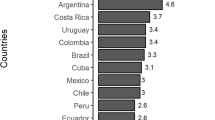
China has been suffering substantially from cervical cancer with more than 100,000 new cases annually (attributing to approximately 20% of the global incidence). Cervical screening uptake was low (< 30%) in China, and HPV vaccination has not yet been completely included in its national immunization program [12, 13]. To optimize healthcare resource utilization, our study aimed to evaluate the cost-effectiveness of cervical screening strategies for cohorts of eligible and non-eligible ages for vaccination upon the implementation of routine HPV immunization in the country. We considered the case of the Hong Kong population which has recently started a population-based HPV vaccination program. Hong Kong has a unique epidemiology of HPV prevalence and cervical cancer when compared to other regions in China. HPV prevalence in Hong Kong showed a major peak in younger ages (20–29 years) and a minor peak at older ages (approximately 50 or above) [14, 15]. Such a bimodal pattern was different from the observed HPV prevalence in China which showed a single peak at 35–54 years [16]. The cervical cancer incidence in Hong Kong was quite steady (at approximately 20 per 100,000 women) throughout the ages of 40 to 85 or above, with a small peak at ages 80–84 [17]. In contrast, cervical cancer incidence in China peaked at age 45–54 and then dropped as age increased [16]. Furthermore, the recently updated cervical screening guidelines in Hong Kong indicated several approaches to triage higher-risk women for further investigation (such as involving combinations of with/without HPV genotyping and cytology for HPV-positive screenees) [18, 19]. This may be worthwhile to compare the cost-effectiveness across different management, in addition to varying screening ages and frequencies. Despite the difference in epidemiology, we aimed to use our work to serve as a reference for an assessment framework for switching cervical screening strategies in the context of routine HPV vaccination for the Chinese population.
Methods
Model overview
We adopted our previously calibrated model of HPV vaccination and cervical cancer screening to estimate the costs and health outcomes of cervical screening strategies for Hong Kong [20]. Briefly, the model comprises (i) a deterministic age-structured compartmental dynamic model for simulating the heterosexual transmission of hrHPVs and (ii) a stochastic individual-based cohort model for simulating the development of cervical cancer over the lifetime of each female [20]. Both dynamic and stochastic components were based on the same natural history model of cervical cancer development that includes health states such as HPV infection, precancerous cervical intraepithelial neoplasia (CIN), and preclinical asymptomatic and clinical symptomatic cancers. Regarding HPV infection, we grouped hrHPVs into four classes: (i) HPV-16; (ii) HPV-18; (iii) HPV-OV (for “other vaccine types”), which comprises the other five hrHPVs targeted by the 9vHPV vaccine, namely, HPV-31, 33, 45, 52, and 58; and (iv) HPV-NV, which comprises all the non-vaccine hrHPVs (i.e., HPV-26, 35, 39, 51, 53, 56, 59, 66, 67, 68, 69, 73, and 82) [14]. The dynamic model was used to infer the model parameters using empirical data from the prevaccination era and then to estimate herd effects after routine female adolescent HPV vaccination had begun. The age-specific force of infection from the dynamic model was used in the stochastic individual-based model to simulate cervical cancer incidence for each birth cohort. The cohort model simulated cervical screening practices and treatments according to the guidelines issued by the Hong Kong College of Obstetricians and Gynaecologists (HKCOG; 2016) [19]. A monthly stepsize was used, and individuals in the population up were simulated up to age 85 years.
Based on the natural history model, the inferring parameters include transition rates between health states and the assortativeness variables in the formation of sexual partnerships between females and males. We assumed that respective parameters that were related to HPV infection were the same in both genders. We estimated the jointly correlated parameters by calibrating the model to empirical data. We first simulated the natural history model based on a given parameter set. We then compared the similarity between the modeled and observed fitting outcomes which included local age-specific HPV prevalence and cervical cancer incidence [14, 15, 17]. The process was iterated to identify parameter sets that showed good calibration (i.e., high similarity) to the fitting targets. We used the Markov chain Monte Carlo approach to update the parameters when calibrating the model. This technique of parameter inference that synthesizes the disease’s natural history model and multiple empirical targets has also been adopted in building microsimulation models for cervical cancer screening and vaccination and screening of colorectal and breast cancers in overseas studies [21,22,23]. Additional file 1: Supplementary Information lists more details on model description (pages 2-6; Additional file 1: Fig. S1 and Table S1) [14, 21, 24,25,26,27,28,29,30,31,32,33,34], parameterization, and calibration (pages 7–11; Additional file 1: Figs. S2-S3, Tables S2-S3) [14, 15, 17, 20, 22, 23, 33, 35,36,37,38,39,40,41,42].
HPV vaccination
Following the most recent statistics, we set the 2-dose vaccine uptake at 85% as the base case scenario and also explored scenarios with lower vaccine uptakes of 75%, 50%, and 25% [43]. The latest literature suggests that first-generation HPV (bivalent [2vHPV] and quadrivalent [4vHPV]) vaccines remain protective beyond 10 years, with no indication of secondary vaccine failure in the cohorts who received 4vHPV vaccines more than 15 years ago in 2006 [44, 45]. As such, we considered three scenarios, namely lifelong, 30-year, and 20-year, for the protection durations induced by the 9vHPV vaccines. We assumed lifelong vaccine-induced protection as the base case scenario. The vaccine efficacy of the 9vHPV vaccine against HPV-16, HPV-18, and HPV-OV was based on 9vHPV vaccine trial data and local HPV epidemiology [3, 14, 46]. Additional file 1 lists more related details (page 12) [3, 14, 43, 46,47,48,49,50].
Cervical screening
We referred to the screening strategies that are recommended by the latest local screening guidelines by the Cancer Expert Working Group and the HKCOG guidelines (Fig. 1) [19, 51]. We considered strategies that use (A) cytology, (B) high-risk HPV DNA testing (HPV testing), or (C) “co-testing” (i.e., combining cytology and HPV testing) as the primary test modality. Following the HKCOG guidelines, we assumed that the routine screening interval was 3 years for (A) primary cytology and 5 years for (B) primary HPV testing and (C) co-testing as the primary screening method. Screening would start at age 25 with primary cytology for all screening strategies examined. Under strategies B1–B3 and C1–C3, HPV testing and co-testing at age 30 were the primary testing strategies, respectively. Additional file 1: Supplementary Information provides more relevant details (pages 12–16; Additional file 1: Fig. S4) [18, 19, 51,52,53,54,55,56].
The analysis was performed separately for (a) cohorts who were too old to be eligible for the routine HPV vaccination program (i.e., no longer studying in primary schools, usually aged 13 years or above) when it commenced in 2019 (the unvaccinated cohorts) and (b) the first ten cohorts who had the opportunity to receive HPV vaccination via the routine program (the vaccinated cohorts). That is, the unvaccinated cohorts included women aged 16 to 64 years, and the vaccinated cohorts included those aged 6 to 15 years in 2022. According to the findings in local surveys, we assumed that 70% of eligible women would undergo cervical screening at each visit [18]. We also assumed that all women who have initiated cervical screening would follow recommended screening visits and clinical appointments for evaluating the maximum impacts of screening [8].
The current HKCOG guidelines were developed before the routine HPV vaccination program commenced in 2019 [19]. Studies outside Hong Kong suggested that in the era of HPV vaccination, women may perceive a lower risk of HPV infection [5, 8]. The current frequency of routine screening in Hong Kong may no longer be cost-effective among vaccinated cohorts. Thus, we further explored the cost-effectiveness of de-intensified strategies that (a) involve longer routine screening intervals (e.g., every 10 or 15 years), (b) initiate screening at older ages (e.g., at 30 or 35 years), or (c) stop screening after a predetermined number of normal screens during a lifetime for vaccinated cohorts.
We adopted the findings reported in the meta-analyses for the sensitivity and specificity of cytology and HPV testing (Additional file 1: Table S4) [19, 57,58,59,60,61].
Cost-effectiveness analysis (CEA)
We estimated the incremental cost-effectiveness of each screening option using a societal perspective. We consulted local oncologists and gynecologists for the standard management procedures of cervical precancerous lesions and cervical cancers and then referred to corresponding treatment charges for private services provided in public hospitals by the Hospital Authority [62]. The Hospital Authority manages all public hospitals which accounted for over 90% of inpatient care in Hong Kong, and we assumed that the costing parameters could be generalizable in Hong Kong [63]. The private charges excluded subsidies from the government, and we assumed that the public hospitals make these charges for covering their costs instead of making a profit. We used life year (LY) and quality-adjusted life year (QALY) as the metrics for quantifying health outcomes and considered LY as the primary metric because it was more commonly used in international CEAs on cervical screening [5, 6, 8, 64]. When calculating QALYs, we adopted health utility weights for screening and cancer outcomes based on international studies due to the lack of local data [6]. Both cost and health benefits were calculated and discounted at 3% annually, starting from 2022. The costs were denominated in US dollars (US $1 = HK $7.8). Table 1 lists the cost and health utility parameters we used in the analysis, with more details in Additional file 1: Supplementary Information (page 18) [6, 19, 20, 25, 31, 62, 63, 65,66,67,68,69,70,71,72,73,74,75].
We conducted probabilistic sensitivity analysis (PSA) to account for parameter uncertainty. A total of 10,000 combinations of parameters were sampled with Latin hypercube sampling (pages 18–19, Additional file 1: Supplementary Information). We calculated the incremental cost-effectiveness ratio (ICER), which is defined as the incremental cost divided by the incremental health outcome, when comparing the two strategies. The incremental cost and health outcome were estimated as the difference in the mean cost and health outcome based on the PSA for the corresponding strategies, respectively. There is no official willingness to pay (WTP) threshold for CEAs in Hong Kong, and the WHO no longer recommends directly correlating the threshold with the gross domestic product per capita (GDPpc). Instead, we set the threshold at one GDPpc based on previous studies conducted there [20, 72]. The average GDPpc in Hong Kong during 2017–2021 was US $47,792 [76]. We considered the 3-year cytology screening (strategy A1), which was recommended before the recent update in 2021, as the base comparator when comparing the impacts of alternative strategies. When sorting strategies on the frontier for incremental CEAs, the strategy with the lowest cost-effectiveness ratio with respect to the scenario of no screening would be ranked the first non-dominated strategy in the league table and then followed by strategies with the lowest ICERs compared with the previous non-dominated strategies [66]. Additional file 1: Supplementary Information provides more information on the analysis (page 19) [20, 66, 76,77,78,79,80,81].
We performed a one-way sensitivity analysis (OWSA) on selected strategy comparisons (Additional file 1: Supplementary Information; page 19) [82, 83]. We tested annual discount rates at 0% (i.e., undiscounted) and 6% as well as screening participation rates at 50% and 100% in the sensitivity analysis. Furthermore, we included a scenario analysis which assumed that males have a faster HPV clearance and shorter natural immunity, based on the observations in some clinical studies (page 19, Additional file 1: Supplementary Information) [21, 24, 32, 84,85,86,87].
We followed the Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement and HPV-FRAME checklist for reporting health economic and HPV-related cancer control evaluations, respectively (Additional file 2; CHEERS 2022 and HPV-FRAME checklists) [88, 89].
Results
Cohorts without a routine vaccination program (unvaccinated cohorts)
In the base case scenario where vaccine uptake was 85% and vaccine protection was lifelong, strategies B1–3 that adopt HPV testing as primary screening with a 5-year regular screening interval generated fewer LYs/QALYs than the 3-year cytology screening (strategy A1); among which, strategy B2 (HPV + genotyping) was less costly than A1 (Additional file 1: Table S5). If LYs were used as the metric for health outcomes, strategy B2 incurred a lower ICER than A1, when both were compared with no screening (US $21,644 for B2 vs US $22,239 for A1 per LY gained), suggesting that B2 was the first non-dominated strategy among the guideline-based strategies evaluated. Strategy A2 (cytology + reflex HPV testing) incurred a lower ICER than A1 when both were compared with B2 (i.e., A2 dominated A1; Additional file 1: Table S5). Strategy A2 was the next most cost-effective strategy with an ICER of US $40,137 per LY gained (Fig. 2). The remaining strategies were either dominated or associated with ICERs above 3 times the WTP threshold. If QALYs were used as the metric for health outcomes instead, strategy A1 was the most cost-effective strategy, with an ICER of US $23,389 per QALY gained compared with no screening (Fig. 2). Switching to the next most cost-effective strategy, namely, strategy A2, would incur an ICER of US $181,297 per QALY gained. The remaining strategies were dominated.
Cost-effectiveness of guideline-based screening strategies for cohorts without a routine vaccination program (unvaccinated cohorts). Using A life years (LYs) and B quality-adjusted life years (QALYs) as metrics for quantifying health outcomes. Note: The thick black lines are the cost-effectiveness frontiers, with the numbers in round-cornered rectangles representing the incremental cost-effectiveness ratios compared to “no screening” (for the first non-dominated strategy, denoted with #) or the previous non-dominated strategy
The comparative cost-effectiveness of the optimal strategies for unvaccinated cohorts was not sensitive to vaccine uptake and duration of vaccine protection among the unvaccinated cohorts (Additional file 1: Table S6). The conclusions of the comparative cost-effectiveness when varying the annual discount rate to 0% and 6% were similar to the scenario of a 3% annual discount rate (Additional file 1: Table S7), except that when QALY was the metric for quantifying health outcomes, the estimated ICER for A1 (cytology-only) vs no screening became not cost-effective and exceeded the WTP threshold by 11%. The OWSA suggested that the estimated ICERs were more sensitive to test performance, such as the specificity of the cytology and/or HPV test and the sensitivity of detecting CIN (Additional file 1: Fig. S5). The estimated ICERs for switching to A2 (cytology + reflex HPV) from A1 (cytology-only) and adopting A1 compared with no screening remained below the WTP threshold when LY and QALY were the metrics for health outcomes, respectively. The detailed findings of sensitivity analyses are presented in Additional file 1: Supplementary Information (pages 21–26; Additional file 1: Tables S5-S8, Fig. S5).
Cohorts with the opportunity to receive routine vaccination (vaccinated cohorts)
The comparative cost-effectiveness of the evaluated strategies for the vaccinated cohorts was sensitive to vaccine uptake and duration of vaccine protection among the vaccinated cohorts. In the base case scenario where vaccine uptake was 85% and vaccine protection was lifelong, the ICERs of all guideline-based strategies with recommended routine screening intervals, including the 3-year cytology screening (strategy A1), exceeded the WTP threshold when compared with no screening (Additional file 1: Table S9). Strategy B2 (HPV testing + genotyping) and strategy A1 (cytology-only) had the lowest ICERs at US $59,863 per LY gained and US $78,003 per QALY gained when compared with no screening, respectively. The ICERs of strategies B2 and A1 remained above the WTP threshold for using LYs and QALYs as the metrics for health outcomes, respectively, when the vaccine uptake of immunization programs was 75% or above among the evaluated scenarios, unless the vaccine uptake was 50% or below (Fig. 3 and Additional file 1: Table S10).
Incremental cost-effectiveness ratios (ICERs) of the most cost-effective guideline-based screening strategy across scenarios of vaccine uptake and duration of vaccine protection for cohorts in the routine vaccination program (vaccinated cohorts). A Using life years (LYs) as metrics for health outcomes. Comparing B2 (HPV + genotyping) vs no screening. B Using quality-adjusted life years (QALYs) as metrics for health outcomes. Comparing A1 (cytology-only) vs no screening. Note: The gray dashed lines represent the willingness to pay threshold at 1 GDPpc (US $47,792)
If the annual discount rate was 0% (i.e., undiscounted), strategy B2 was the most cost-effective in the settings where LY and QALY were the metrics for health outcomes, with estimated ICERs below US $27,000 when compared with no screening (Additional file 1: Table S11). Continuing to adopt strategy A1 (cytology-only) was less effective (but more costly) or incurred an ICER exceeding the WTP threshold when compared with B2. If the discount rate was 6%, the estimated ICERs were greater than at least 2.8 times the WTP threshold even for the most cost-effective strategies compared with no screening (Additional file 1: Table S11). The OWSA suggested that the estimated ICERs were more sensitive to test performance, such as the specificity of cytology and/or HPV test and the sensitivity of detecting CIN, as well as the cost of cancer treatment (Additional file 1: Fig. S6). Under OWSA, the estimated ICERs of strategies B2 and A1 (which are the most optimal strategies compared with no screening when LY and QALY were the metrics for health outcomes, respectively) remained above the WTP threshold. In the scenario analysis that assumed the HPV clearance rate and waning rate of natural immunity were faster in males, the incremental CEA was similar to the original findings, under the setting of substantial vaccination impacts with 85% vaccine uptake and lifelong vaccine protection (Additional file 1: Table S12). The detailed findings of the sensitivity analysis are presented in Additional file 1: Supplementary Information (pages 27–33; Additional file 1: Tables S9-S13, Fig. S6).
To further assess the cost-effectiveness of cervical screening in vaccinated cohorts with high vaccine uptake, we examined de-intensified strategies that use HPV testing as the primary screening tool per the WHO’s recommendation. We considered variants of strategy B2 (HPV testing + genotyping) which incurred the lowest ICERs among the primary HPV testing strategies (i.e., strategies B1–B3) indicated in the local guidelines. Figure 4 presents the cost-effectiveness of variants of strategy B2 (HPV testing + genotyping) that meet the WHO’s proposal of screening women between ages 35 and 45 years for vaccinated cohorts, under the base case scenario of 85% vaccine uptake and lifelong vaccine protection. Assuming that women stopped screening after obtaining two normal HPV test results (as the minimum requirement per the WHO’s proposal), the ICER of a variant of strategy B2 that initiated cervical screening at age 35 with another screen 10 years later was US $13,994 per LY gained and US $14,682 per QALY gained when compared with no screening. Screening women at the ages of 30 and 45 was the next non-dominated strategy; the ICERs were US $24,583 per LY gained and US $32,469 per QALY gained when compared with screening women at the ages of 35 and 45. Other evaluated potential alternatives, including strategies that relaxed the restriction that women stop screening after obtaining two normal HPV test results (i.e., women may continue to screen until age 65), were either dominated or associated with an ICER above 3 times the WTP threshold (Additional file 1: Table S14 and S15).
Cost-effectiveness of variants of strategy B2 (HPV + genotyping) that meet WHO’s proposal of screening women between the ages of 35 and 45 years for cohorts implemented with the routine vaccination program (vaccinated cohorts). Using A life years (LYs) and B quality-adjusted life years (QALYs) as metrics for quantifying health outcomes. aAssume that 9vHPV vaccines provided lifelong protection and the vaccine uptake was 85%. bFollowing the HKCOG guidelines, for strategy B2 (HPV + genotyping), women would start screening with cytology at the age of 25 years and then switch to the primary HPV test after 30 years. For variants of strategy B2 that start screening age at 30 and 35 years, women would directly undergo primary HPV testing at 30 and 35 years, respectively, without the prior cytology screening at age 25–29 years. cThe x- and y-axes represent the incremental discounted cost and LY/QALY compared with “no screening.” dThe black thick lines are the cost-effectiveness frontiers, with the numbers in round-cornered rectangles representing the ICERs compared to “no screening” (for the first non-dominated strategy, denoted with #) or the previous non-dominated strategy
Discussion
We evaluated the cost-effectiveness of guideline-based cervical screening strategies and potential alternatives for the situation in Hong Kong, where the vaccine uptake (among cohorts via the immunization program) and screening uptake are close to the WHO’s proposed targets while the public health impacts of incorporating hrHPV testing as a primary tool in cervical screening in the era of HPV vaccination are currently lacking [2, 19, 51]. Our findings demonstrate that the optimal screening strategy is different for cohorts that are of eligible and non-eligible ages for the HPV vaccination program (i.e., vaccinated and unvaccinated cohorts, respectively) when vaccine uptake is high. In line with the WHO’s recommendation of using HPV testing as the primary screening tool [2], the HKCOG guidelines stated three approaches to triage HPV-positive cases with 5-year regular screening intervals (i.e., strategies B1–3). For unvaccinated cohorts, our findings suggested that HPV-primary screening strategies generated fewer LY gained than the 3-year cytology screening (strategy A1). Instead, strategy A2 which uses a reflex HPV test to triage mild cytology abnormality (atypical squamous cells of undetermined significance, ASCUS) may be considered a cost-effective alternative to A1 (cytology-only) with more LY gained.
For vaccinated cohorts, the comparative cost-effectiveness of screening strategies depends on vaccine uptake and duration of vaccine protection. When the impact of the immunization program is high (e.g., when vaccine uptake is high or vaccine protection is long), the marginal benefit of screening is lower, and the corresponding ICERs of screening strategies are higher. Across the scenarios considered here, vaccine impact is the highest when vaccine uptake is 85% (the status quo) and vaccine protection is lifelong. In this scenario, all evaluated screening strategies with guideline-based routine screening intervals, including the 3-year cytology screening strategy (A1), are not cost-effective when compared with no screening. This suggests the need to adopt less-intensive strategies for screening to remain a cost-effective add-on in the scenario of high vaccine uptake. However, when vaccine uptake is low to moderate (e.g., at 50% or below), strategies with guideline-based routine screening intervals may achieve ICERs below the WTP threshold, suggesting that a one-size-fits-all screening strategy may be used for both unvaccinated and vaccinated cohorts.
The WHO recommends the target of 70% female screening coverage (preferably with HPV testing) at least twice by the age of 35 and another test by the age of 45 [2]. The triage approaches used in national screening programs vary across different countries. For example, Public Health England recommends using cytology tests as triage, while genotyping of HPV-16/18 is adopted in Australia [90, 91]. We evaluated de-intensified variants of strategy B2 (HPV + genotyping) which is the most cost-effective among the three primary HPV testing strategies stated in the HKCOG guidelines. Our results suggest that for vaccinated cohorts, HPV testing with genotyping triage, by which women were screened twice either at ages 35 and 45 (10 years apart) or at ages 30 and 45 (15 years apart), achieved ICERs below US $16,000 per LY or QALY gained when compared with no screening. In particular, initiating screening at a younger age of 30 years with a longer interval of 15 years for the second routine screen may generate more LYs and QALYs gained while remaining cost-effective with an ICER under the WTP threshold when compared with screening women at ages 35 and 45. This demonstrates the feasibility of exploring alternatives that provide better value for money in resource allocation. However, the safety and compliance of the alternative strategies should also be monitored regularly.
To follow the status quo policy implementation in Hong Kong, we evaluated the cost-effectiveness of cervical screening in the context of female-only HPV vaccination and did not consider the case of a gender-neutral vaccination. In Hong Kong, the acceptance of HPV vaccination among adolescent male students was low. In a recent local survey, only 23% of the responded male students aged 18–26 years found HPV vaccination in males to be acceptable [92]. An overseas comparative modeling study predicted that if a 90% vaccine uptake among females was achieved, vaccine-targeted HPV types could almost be eliminated, and the corresponding incremental impact on reducing cervical cancer was limited for additionally vaccinating males [93]. Health economic studies also suggested that if HPV vaccination coverage among females was high (e.g., above 75%), including males in the vaccination was likely not cost-effective when compared with vaccinating females only [94]. Furthermore, given the supply shortage of HPV vaccines, the Strategic Advisory Group of Experts on Immunization of the WHO recommended temporarily pausing and lowering the priority of male vaccination [95, 96]. Therefore, we did not include the scenario of a gender-neutral HPV vaccination because this is less likely to be implemented in Hong Kong shortly. However, the impact of cervical screening in the context of vaccinating both genders would be worthwhile to be considered if the policy implementation changes in the future, particularly when the acceptance of male vaccination increases substantially.
Our study has some limitations. First, we assumed one screening strategy for both vaccinated and unvaccinated women in the vaccinated cohorts. Naber et al. reported that when herd protection is over 50% (i.e., infections are reduced by over 50% among unvaccinated women in vaccinated age cohorts), a shorter screening interval (e.g., a strategy that is optimized for prevaccination scenarios) for unvaccinated individuals in vaccinated cohorts might not be cost-effective [97]. That is, in cohorts with high vaccine uptake, such as in Hong Kong, the UK, and Australia where over 75% of schoolgirls are vaccinated via routine immunization programs, there is little advantage in conditioning screening strategies on women’s vaccination status. Therefore, we evaluated the impacts of cervical screening (by population-level vaccine uptake) in the cohorts regardless of individual vaccination status.
Furthermore, based on current data from Hong Kong, we assumed vaccine uptake to be 85% in the base case. We did not consider the case of 90% uptake, which the WHO recommends as a target, because only a few countries (e.g., Norway) have achieved such a high uptake [4]. Additionally, we considered the scenario of using 9vHPV vaccines in the immunization program, rather than 2vHPV and 4vHPV vaccines which have been used in some countries. Nevertheless, our conclusions about stratifying screening strategies per vaccination cohort likely remain valid as long as vaccine uptake exceeds 50% and when the 2vHPV and 4VHPV vaccines also provide high efficacy against HPV-16/18, which collectively contributes to 70% of cervical cancer cases.
Similar to other HPV modeling studies, we assumed that parameters that are related to HPV infection were the same in both genders [21, 24, 32]. Some studies suggested that clearance of HPV infection among males was comparable to that among females [84, 85], while some clinical findings observed that the time to clearance of HPV infection was shorter in males [87, 98]. On the other hand, some studies indicated that the natural immunity following recovery from HPV infection may be less persistent in males than that in females [86]. HPV prevalence is affected by multiple parameters relating to the natural history of HPV infection and sexual behavior. The HPV prevalence curve among males was more stable over older ages when compared to that among females which generally peaked at younger ages and declined afterwards [99, 100]. The scenario analysis (which assumed a faster HPV clearance rate and waning rate of natural immunity among males) suggested that under the setting of high vaccination impacts, the respective incremental CEA was comparable to the original findings which assumed that natural history parameters relating to HPV infection were the same in both genders (Additional file 1: Table S12). Moreover, in line with other studies on cervical screening, our study concludes that a longer screening interval could be adopted in vaccinated female cohorts when the vaccine uptake was high (e.g., over 75%) [5, 8, 11]. Nevertheless, the respective impacts of the gender-specific assumptions for the natural history parameters regarding HPV infection on the estimation of HPV burden and HPV vaccination may be worthwhile for further investigation.
Last, we estimated the model parameters by fitting simulated population-level HPV prevalence and cancer incidence to different empirical data sources [14, 15, 17]. This method has also been adopted for developing simulation models in colorectal and breast cancer screening [22, 23]. Using individual-level data from organized screening programs or longitudinal trials that trace the changes in health states across time horizons could be alternative approaches to estimating disease transition parameters [101]. In Hong Kong, cervical cytology has been used as the primary modality in cervical screening for decades. The use of HPV testing in cervical screening was introduced in the recent guidelines in 2016 [19]. To our knowledge, longitudinal data on HPV prevalence and incidence of precancerous CINs are not publicly available at the moment in Hong Kong. Therefore, we did not include individual-level data when inferring parameters in this study.
Conclusions
When following the WHO’s targets to eliminate cervical cancer, high uptake of HPV vaccination is likely observed. For vaccinated cohorts, adopting de-intensified strategies with a reduced expected number of lifetime screens for HPV-based screening may be cost-effective if vaccine uptake of routine vaccination is 75% or above. To maximize the cost-effectiveness of cervical screening, health authorities should explicitly propose screening recommendations that are tailored separately with respect to birth cohorts involved in routine vaccination programs and base these recommendations on the actual vaccine uptake attained.
Availability of data and materials
The data generating the findings of this article are included within the article and its additional file.
Abbreviations
- 2vHPV:
-
Bivalent human papillomavirus vaccine
- 4vHPV:
-
Quadrivalent human papillomavirus vaccine
- 9vHPV:
-
Nonavalent human papillomavirus vaccine
- ASCUS:
-
Atypical squamous cells of undetermined significance
- CEA:
-
Cost-effectiveness analysis
- CIN:
-
Cervical intraepithelial neoplasia
- GDPpc:
-
Gross domestic product per capita
- HKCOG:
-
Hong Kong College of Obstetricians and Gynaecologists
- HPV:
-
Human papillomavirus
- HPV-NV:
-
Non-vaccine human papillomavirus types
- HPV-OV:
-
Other vaccine human papillomavirus types
- hrHPV:
-
High-risk human papillomavirus
- ICER:
-
Incremental cost-effectiveness ratio
- LEEP:
-
Loop electro-surgical excision procedure
- LSIL:
-
Low-grade squamous intraepithelial lesion
- LY:
-
Life year
- OWSA:
-
One-way sensitivity analysis
- PSA:
-
Probabilistic sensitivity analysis
- QALY:
-
Quality-adjusted life year
- WHO:
-
World Health Organization
- WTP:
-
Willingness to pay
References
International Agency for Research on Cancer (IARC), World Health Organization. Global cancer observatory. https://gco.iarc.fr/.
World Health Organization. Cervical cancer elimination initiative. https://www.who.int/initiatives/cervical-cancer-elimination-initiative.
Joura EA, Giuliano AR, Iversen O-E, Bouchard C, Mao C, Mehlsen J, et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N Engl J Med. 2015;372(8):711–23.
Bruni L, Saura-Lazaro A, Montoliu A, Brotons M, Alemany L, Diallo MS, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev Med. 2021;144:106399.
Lew JB, Simms KT, Smith MA, Hall M, Kang YJ, Xu XM, et al. Primary HPV testing versus cytology-based cervical screening in women in Australia vaccinated for HPV and unvaccinated: effectiveness and economic assessment for the National Cervical Screening Program. Lancet Public Health. 2017;2(2):e96–e107.
Bains I, Choi YH, Soldan K, Jit M. Clinical impact and cost-effectiveness of primary cytology versus human papillomavirus testing for cervical cancer screening in England. Int J Gynecol Cancer. 2019;29(4):669–75.
Inturrisi F, Lissenberg-Witte BI, Veldhuijzen NJ, Bogaards JA, Ronco G, Meijer C, et al. Estimating the direct effect of human papillomavirus vaccination on the lifetime risk of screen-detected cervical precancer. Int J Cancer. 2021;148(2):320–8.
Kim JJ, Burger EA, Sy S, Campos NG. Optimal cervical cancer screening in women vaccinated against human papillomavirus. J Natl Cancer Inst. 2017;109(2):djw216. https://academic.oup.com/jnci/article/109/2/djw216/2905864.
Landy R, Windridge P, Gillman MS, Sasieni PD. What cervical screening is appropriate for women who have been vaccinated against high risk HPV? A simulation study. Int J Cancer. 2018;142(4):709–18.
Pedersen K, Burger EA, Nygard M, Kristiansen IS, Kim JJ. Adapting cervical cancer screening for women vaccinated against human papillomavirus infections: the value of stratifying guidelines. Eur J Cancer. 2018;91:68–75.
Simms KT, Smith MA, Lew JB, Kitchener HC, Castle PE, Canfell K. Will cervical screening remain cost-effective in women offered the next generation nonavalent HPV vaccine? Results for four developed countries. Int J Cancer. 2016;139(12):2771–80.
Aoki ES, Yin R, Li K, Bhatla N, Singhal S, Ocviyanti D, et al. National screening programs for cervical cancer in Asian countries. J Gynecol Oncol. 2020;31(3):e55.
National Health Commission of the People’s Republic of China. Nation plans to launch free HPV vaccinations; 2022.
Chan PKS, Ho WCS, Wong MCS, Chang AR, Chor JSY, Yu M-Y. Epidemiologic risk profile of infection with different groups of human papillomaviruses. J Med Virol. 2009;81:1635–44.
Liu SS, Chan KYK, Leung RCY, Chan KKL, Tam KF, Luk MHM, et al. Prevalence and risk factors of human papillomavirus (HPV) infection in southern Chinese women - a population-based study. PLoS One. 2011;6(5):e19244.
Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gomez D, et al. Human papillomavirus and related diseases in China. Summary Report 22 October 2021. In: ICO/IARC Information Centre on HPV and Cervical Cancer (HPV Information Centre); 2021.
Hong Kong Cancer Registry. http://www3.ha.org.hk/cancereg/.
Cervical Screening Programme, Department of Health. https://www.cervicalscreening.gov.hk/en/index.html.
The Hong Kong College of Obstetricians and Gynaecologists. Guidelines for cervical cancer prevention and screening. In: The Hong Kong College of obstetricians and gynaecologists; 2016.
Choi HCW, Jit M, Leung GM, Tsui K-L, Wu JT. Simultaneously characterizing the comparative economics of routine female adolescent nonavalent human papillomavirus (HPV) vaccination and assortativity of sexual mixing in Hong Kong Chinese: a modeling analysis. BMC Med. 2018;16:127.
Kim JJ, Goldie SJ. Health and economic implications of HPV vaccination in the United States. N Engl J Med. 2008;259(8):821–32.
Silva-Illanes N, Espinoza M. Critical analysis of Markov models used for the economic evaluation of colorectal cancer screening: a systematic review. Value Health. 2018;21(7):858–73.
Tan KH, Simonella L, Wee HL, Roellin A, Lim YW, Lim WY, et al. Quantifying the natural history of breast cancer. Br J Cancer. 2013;109(8):2035–43.
Choi YH, Jit M, Gay N, Cox A, Garnett GP, Edmunds WJ. Transmission dynamic modelling of the impact of human papillomavirus vaccination in the United Kingdom. Vaccine. 2010;28(24):4091–102.
Elbasha EH, Dasbach EJ, Insinga RP. Model for assessing human papillomavirus vaccination strategies. Emerg Infect Dis. 2007;13(1):28–41.
Goldie SJ, Grima D, Kohli M, Wright TC, Weinstein MC, Franco EL. A comprehensive natural history model of HPV infection and cervical cancer to estimate the clinical impact of a prophylactic HPV-16/18 vaccine. Int J Cancer. 2003;106:896–904.
Wearing HJ, Rohani P, Keeling MJ. Appropriate models for the management of infectious diseases. PLoS Med. 2005;2(7):e174.
Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370(9590):890–907.
Gunther OP, Ogilvie G, Naus M, Young E, Patrick DM, Dobson S, et al. Protecting the next generation: what is the role of the duration of human papillomavirus vaccine-related immunity? J Infect Dis. 2008;197(12):1653–61.
Cheung FY, Mang OWK, Law SCK. A population-based analysis of incidence, mortality, and stage-specific survival of cervical cancer patients in Hong Kong: 1997-2006. Hong Kong Med J. 2011;17(2):89–95.
de Kok IMCM, van Ballegooijen M, Habbema JDF. Cost-effectiveness analysis of human papillomavirus vaccination in the Netherlands. J Natl Cancer Inst. 2009;101(15):1083–92.
Johnson HC, Elfstrom KM, Edmunds WJ. Inference of type-specific HPV transmissibility, progression and clearance rates: a mathematical modelling approach. PLoS One. 2012;7(11):e49614.
Census and Statistics Department. http://www.censtatd.gov.hk/home/index.jsp.
Barnabas RV, Laukkanen P, Koskela P, Kontula O, Lehtinen M, Garnett GP. Epidemiology of HPV 16 and cervical cancer in Finland and the potential impact of vaccination: mathematical modelling analyses. PLoS Med. 2006;3(5):e138.
Korostil IA, Peters GW, Cornebise J, Regan DG. Adaptive Markov chain Monte Carlo forward projection for statistical analysis in epidemic modelling of human papillomavirus. Stat Med. 2013;32(11):1917–53.
Calderhead B. A general construction for parallelizing Metropolis-Hastings algorithms. Proc Natl Acad Sci U S A. 2014;111(49):17408–13.
Chan PKS, Ho WCS, Yu M-Y, Pong W-M, Chan ACL, Chan AKC, et al. Distribution of human papillomavirus types in cervical cancers in Hong Kong: current situation and changes over the last decades. Int J Cancer. 2009;125(7):1671–7.
Insinga RP, Perez G, Wheeler CM, Koutsky LA, Garland SM, Leodolter S, et al. Incident cervical HPV infections in young women: transition probabilities for CIN and infection clearance. Cancer Epidemiol Biomark Prev. 2011;20(2):287–96.
Moscicki A-B, Ma Y, Wibbelsman C, Darragh TM, Powers A, Farhat S, et al. Rate of and risks for regression of cervical intraepithelial neoplasia 2 in adolescents and young women. Obstet Gynecol. 2010;116:1373–80.
Jackson C, Jit M, Sharples L, DeAngelis D. Calibration of complex models through Bayesian evidence synthesis: a demonstration and tutorial. Med Decis Mak. 2015;35(2):148–61.
Whyte S, Walsh C, Chilcott J. Bayesian calibration of a natural history model with application to a population model for colorectal cancer. Med Decis Mak. 2011;31(4):625–41.
Geweke J. Evaluating the accuracy of sampling-based approaches to the calculation of posterior moments. In: Bernardo JM, Berger JO, Dawid AP, AFM S, editors. Bayesian statistics, vol. Volume 4. Oxford: Oxford University Press; 1992. p. 169–93.
Legislative Council. LCQ10: human papillomavirus vaccination programme; 2021.
Porras C, Tsang SH, Herrero R, Guillen D, Darragh TM, Stoler MH, et al. Efficacy of the bivalent HPV vaccine against HPV 16/18-associated precancer: long-term follow-up results from the Costa Rica Vaccine Trial. Lancet Oncol. 2020;21(12):1643–52.
Kjaer SK, Nygard M, Sundstrom K, Dillner J, Tryggvadottir L, Munk C, et al. Final analysis of a 14-year long-term follow-up study of the effectiveness and immunogenicity of the quadrivalent human papillomavirus vaccine in women from four nordic countries. EClinicalMedicine. 2020;23:100401.
Malagon T, Drolet M, Boily M-C, Franco EL, Jit M, Brisson J, et al. Cross-protective efficacy of two human papillomavirus vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(10):781–9.
Centre for Health Protection, Department of Health. About human papillomavirus (HPV) vaccination. In: Edited by Department of Health: Hong Kong Special Administrative Region; 2020.
Legislative Council. LCQ18: assisting women in preventing gynaecological diseases; 2022.
Choi HCW, Leung GM, Woo PPS, Jit M, Wu JT. Acceptability and uptake of female adolescent HPV vaccination in Hong Kong: a survey of mothers and adolescents. Vaccine. 2013;32(1):78–84.
The Family Planning Association of Hong Kong. Youth Sexuality Study. 2016. https://www.famplan.org.hk/en/media-centre/press-releases/detail/fpahk-report-on-youth-sexuality-study.
Cancer Expert Working Group on Cancer Prevention and Screening, Centre for Health Protection. Recommendations on prevention and screening for cervical cancer; 2021.
Wu JT. Cervical cancer prevention through cytologic and human papillomavirus DNA screening in Hong Kong Chinese women. Hong Kong Med J. 2011;17(Suppl 3):S20–4.
Cervical Screening Programme, Department of Health. Cervical cancer screening coverage. http://www.cervicalscreening.gov.hk/english/sr/sr_statistics_ccsc.html.
Adab P, McGhee SM, Yanova J, Wong CM, Hedley AJ. Effectiveness and efficiency of opportunistic cervical cancer screening: comparison with organized screening. Med Care. 2004;42(6):600–9.
Census and Statistics Department. Thematic household survey report - report no.12; 2003.
eHealth. Electronic Health Record Sharing System (eHRSS). https://www.ehealth.gov.hk/en/index.html.
Pan Q-J, Hu S-y, Zhang X, Ci P-w, Zhang W-h, Guo H-q, et al. Pooled analysis of the performance of liquid-based cytology in population-based cervical cancer screening studies in China. Cancer Cytopathol. 2013;121(9):473–82.
CADTH. HPV testing for primary cervical cancer screening: a health technology assessment. CADTH Optimal Use Report. 2019, 7(1b). https://www.cadth.ca/sites/default/files/ou-tr/op0530-hpv-testing-for-pccreport.pdf.
Cuzick J, Clavel C, Petry K-U, Meijer CJLM, Hoyer H, Ratnam S, et al. Overview of the European and North American studies on HPV testing in primary cervical cancer screening. Int J Cancer. 2006;119:1095–101.
Chan PKS, Cheung TH, Tam AOY, Lo KWK, Yim SF, Yu MMY, et al. Biases in human papillomavirus genotype prevalence assessment associated with commonly used consensus primers. Int J Cancer. 2006;18(1):243–5.
Park KS, Kim J-Y, Ki C-S, Lee NY. Comparison of the Digene HPV genotyping LQ test and the PANArray HPV genotyping chip for detection of high-risk or probable high-risk human papillomavirus genotypes. Ann Lad Med. 2014;34(4):279–85.
Hospital Authority. Revisions to list of charges: Gazette No. 3884: Hong Kong Special Administrative Region; 2017.
Authority H. Hospital authority statistical report; 2020.
Sefuthi T, Nkonki L. A systematic review of economic evaluations of cervical cancer screening methods. Syst Rev. 2022;11(1):162.
Census and Statistics Department. https://www.censtatd.gov.hk/home/index.jsp.
Woo PPS, Kim JJ, Leung GM. What is the most cost-effective population-based cancer screening program for Chinese woman? J Clin Oncol. 2007;25(6):617–24.
Census and Statistics Department. Women and men in Hong Kong - key statistics; 2021.
Myers ER, Green S, Lipkus I. Patient preferences for health states related to HPV infection: visual analog scales vs time trade-off elicitation. In: 21st International Papillomavirus Conference and Clinical Workshop: 2004. Mexico City; 2004.
Hospital Authority. Revisions to list of charges: G.N. 3884. In: Hong Kong Special Administrative Region; 2017.
Legislative Council. Legislative Council Panel on Health Services - review of fees and charges for non-eligible persons and private patients in the Hospital Authority (LC Paper No. CB (2)331/12-13(03)). 2012.
Hospital Authority. Fees and charges. http://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=10045&Lang=ENG.
Cheung TH, Cheng SSY, Hsu DC, Wong QW, Pavelyev A, Walia A, et al. The impact and cost-effectiveness of 9-valent human papillomavirus vaccine in adolescent females in Hong Kong. Cost Eff Resour Alloc. 2021;19(1):75.
Wong CKH, Lam CLK, Poon JTC, McGhee SM, Law WL, Kwong DLW, et al. Direct medical costs of care for Chinese patients with colorectal neoplasia: a health care service provider perspective. J Eval Clin Pract. 2012;18(6):1203–10.
Tse DMW, Chan KS, Lam WM, Leu KS, Lam PT. The impact of palliative care on cancer deaths in Hong Kong: a retrospective study of 494 cancer deaths. Palliat Med. 2007;21(3):425–33.
Simms KT, Laprise J-F, Smith MA, Lew J-B, Caruana M, Brisson M, et al. Cost-effectiveness of the next generation nonavalent human papillomavirus vaccine in the context of primary human papillomavirus screening in Australia: a comparative modelling analysis. Lancet Public Health. 2016;1(2):e66–75.
Census and Statistics Department. National accounts. https://www.censtatd.gov.hk/en/scode250.html.
Bertram MY, Lauer JA, De Joncheere K, Edejer TT-T, Hutubessy R, Kieny M-P, et al. Cost-effectiveness thresholds: pros and cons. Bull World Health Organ. 2016;94(12):925–30.
Wong IOL, Schooling CM, Cowling BJ. Cost-effectiveness of Helicobacter pylori screening and treatment for gastric cancer in Hong Kong: a decision analytic approach. Hong Kong Med J. 2014;20(6, Suppl 7):S13–5.
Lam CL, Law WL, Poon JT, Chan P, Wong CK, McGhee SM, et al. Health-related quality of life in patients with colorectal neoplasm and cost-effectiveness of colorectal cancer screening in Hong Kong. Hong Kong Med J. 2015;21(Suppl 6):4–8.
Lee SF, Choi HCW, Chan SK, Lam KO, Lee VHF, Wong IOL, et al. Cost-effectiveness of anti-epidermal growth factor receptor therapy versus bevacizumab in KRAS wild-type (WT), pan-RAS WT, and pan-RAS WT left-sided metastatic colorectal cancer. Front Oncol. 2021;11:651299.
You JHS, Cho WCS, Ming WK, Li YC, Kwan CK, Au KH, et al. EGFR mutation-guided use of afatinib, erlotinib and gefitinib for advanced non-small-cell lung cancer in Hong Kong - a cost-effectiveness analysis. PLoS One. 2021;16(3):e0247860.
Demarteau N, Detournay B, Tehard B, Hasnaoui AE, Standaert B. A generally applicable cost-effectiveness model for the evaluation of vaccines against cervical cancer. Int J Public Health. 2011;56(2):153–62.
Jit M, Choi YH, Edmunds WJ. Economic evaluation of human papillomavirus vaccination in the United Kingdom. Br Med J. 2008;337:a769.
Giuliano AR, Lee J-H, Fulp W, Villa LL, Lazcano E, Papenfuss MR, et al. Incidence and clearance of genital human papillomavirus infection in men (HIM): a cohort study. Lancet. 2011;377(9769):932–40.
Trottier H, Mahmud SM, Lindsay L, Jenkins D, Quint W, Wieting SL, et al. Persistence of an incident human papillomavirus infection and timing of cervical lesions in previously unexposed young women. Cancer Epidemiol Biomark Prev. 2009;18(3):854–62.
Beachler DC, Jenkins G, Safaeian M, Kreimer AR, Wentzensen N. Natural acquired immunity against subsequent genital human papillomavirus infection: a systematic review and meta-analysis. J Infect Dis. 2016;213(9):1444–54.
Sichero L, Giuliano AR, Villa LL. Human papillomavirus and genital disease in men: What we have learned from the HIM study. Acta Cytol. 2019;63(2):109–17.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. BMC Health Serv Res. 2022;22(1):114.
Canfell K, Kim JJ, Kulasingam S, Berkhof J, Barnabas R, Bogaards JA, et al. HPV-FRAME: a consensus statement and quality framework for modelled evaluations of HPV-related cancer control. Papillomavirus Res. 2019;8:100184.
Public Health England. Cervical screening: programme overview. https://www.gov.uk/guidance/cervical-screening-programme-overview.
Department of Health A. National Cervical Screening Program. https://www.health.gov.au/initiatives-and-programs/national-cervical-screening-program.
Cheung T, Lau JTF, Wang JZ, Mo PKH, Ho YS. Acceptability of HPV vaccines and associations with perceptions related to HPV and HPV vaccines among male baccalaureate students in Hong Kong. PLoS One. 2018;13(6):e0198615.
Brisson M, Kim JJ, Canfell K, Drolet M, Gingras G, Burger EA, et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395(10224):575–90.
Ng SS, Hutubessy R, Chaiyakunapruk N. Systematic review of cost-effectiveness studies of human papillomavirus (HPV) vaccination: 9-valent vaccine, gender-neutral and multiple age cohort vaccination. Vaccine. 2018;36(19):2529–44.
World Health Organization. Meeting of the Strategic Advisory Group of Experts on Immunization, October 2019: conclusions and recommendations. Wkly Epidemiol Rec. 2019;94(47):541–60.
World Health Organization. Meeting of the Strategic Advisory Group of Experts on Immunization, April 2022: conclusions and recommendations. Wkly Epidemiol Rec. 2022;97(24):261–76.
Naber SK, Matthijsse SM, Rozemeijer K, Penning C, de Kok IM, van Ballegooijen M. Cervical cancer screening in partly HPV vaccinated cohorts - a cost-effectiveness analysis. PLoS One. 2016;11(1):e0145548.
Giuliano AR, Lu B, Nielson CM, Flores R, Papenfuss MR, Lee J-H, et al. Age-specific prevalence, incidence, and duration of human papillomavirus infections in a cohort of 290 US men. J Infect Dis. 2008;198:827–35.
Wei F, Yin K, Wu X, Lan J, Huang S, Sheng W, et al. Human papillomavirus prevalence and associated factors in women and men in south China: a population-based study. Emerg Microbes Infect. 2016;5(11):e119.
Gargano JW, Unger ER, Liu G, Steinau M, Meites E, Dunne E, et al. Prevalence of genital human papillomavirus in males, United States, 2013-2014. J Infect Dis. 2017;215(7):1070–9.
Duffy SW, Chen HH, Tabar L, Day NE. Estimation of mean sojourn time in breast cancer screening using a Markov chain model of both entry to and exit from the preclinical detectable phase. Stat Med. 1995;14(14):1531–43.
Acknowledgements
This work was supported by grants from the Health and Medical Research Fund (18170902) of the Government of the Hong Kong Special Administrative Region. This work was supported by AIR@InnoHK administered by the Innovation and Technology Commission. The computations were performed using research computing facilities offered by Information Technology Services, the University of Hong Kong.
Funding
Health and Medical Research Fund (18170902) of the Government of the Hong Kong Special Administrative Region.
Author information
Authors and Affiliations
Contributions
HCWC, KL, KKLC, MJ, and JTW designed the study, developed the model, analyzed the data, interpreted the results, and wrote the manuscript. HCWC, KL, YB, and JTW accessed and verified the study data. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Information.
This file provides additional information on model description, parameterization and calibration, settings on cervical screening and HPV vaccination used in the study, extra data for performing the cost-effectiveness analysis, and the supplementary results on sensitivity analyses. Table S1. The distribution of individuals by the level of sexual activity and age group. Table S2. Age distribution and mortality rate in Hong Kong. Table S3. Posterior distributions of inferred parameters. Table S4. Test performance parameters of cytology and HPV test. Table S5. Cost-effectiveness of guidelines-based screening strategies for unvaccinated cohorts. Table S6. ICERs of the most cost-effective screening strategy by vaccine uptake and duration of vaccine protection for unvaccinated cohorts. Table S7. Cost-effectiveness of screening strategies by annual discount rates for unvaccinated cohorts. Table S8. Sensitivity analysis on the estimated costs and health outcomes for unvaccinated cohorts by screen uptake. Table S9. Cost-effectiveness of guidelines-based screening strategies for vaccinated cohorts. Table S10. ICERs of the most cost-effective screening strategy by vaccine uptake and duration of vaccine protection for vaccinated cohorts. Table S11. Cost-effectiveness of screening strategies by annual discount rates for vaccinated cohorts. Table S12. Cost-effectiveness of screening strategies for vaccinated cohorts, with the assumption of faster HPV clearance rate and waning rate of natural immunity in males. Table S13. Sensitivity analysis of the estimated cost and health outcomes of screening strategies for vaccinated cohorts by screening uptake. Table S14. One-way sensitivity analysis on the cost-effectiveness of variants of strategy HPV + Genotyping for vaccinated cohorts. Table S15. Cost-effectiveness of variants of strategy HPV + Genotyping for vaccinated cohorts. Fig. S1. Schematic of the natural history model for high-risk HPV infection and cervical cancer. Fig. S2. Comparison of empirical data and the fitted model. Fig. S3. Trace plots and the posterior distributions of fitted parameters. Fig. S4. Schematic of evaluated cervical screening algorithms. Fig. S5. One-way sensitivity analysis of ICER for unvaccinated cohorts. Fig. S6. One-way sensitivity analysis of ICER for vaccinated cohorts.
Additional file 2:
CHEERS 2022 and HPV-FRAME checklists.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Choi, H.C.W., Leung, K., Chan, K.K.L. et al. Maximizing the cost-effectiveness of cervical screening in the context of routine HPV vaccination by optimizing screening strategies with respect to vaccine uptake: a modeling analysis. BMC Med 21, 48 (2023). https://doi.org/10.1186/s12916-023-02748-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-02748-3