Abstract
Background
Triple-negative breast cancer (TNBC) is a biologically diverse disease, with characteristics such as homologous recombination deficiency (HRD), gene mutation, and immune reactions. Japan Breast Cancer Research Group 22 is a multicenter trial examining TNBC’s response to neoadjuvant chemotherapy (NAC) according to the HRD status. This translational research investigated the clinical significance of the immune microenvironment of TNBC in association with HRD, tumor BRCA1/2 (tBRCA1/2) mutation, and response to NAC.
Methods
Patients aged below 65 years with high HRD or germline BRCA1/2 (gBRCA1/2) mutation randomly received paclitaxel + carboplatin (group A1) or eribulin + carboplatin (A2), followed by anthracycline. Patients aged below 65 years with low HRD or those aged 65 years or older without gBRCA1/2 mutation randomly received eribulin + cyclophosphamide (B1) or eribulin + capecitabine (B2); nonresponders to the first four cycles of the therapy received anthracycline. A pathological complete response (pCR) was defined as the absence of residual cancer cells in the tissues. Pretreatment biopsy specimens were stained by multiplexed fluorescent immunohistochemistry using antibodies against CD3, CD4, CD8, Foxp3, CD204, and pan-cytokeratin. Immune cells with specific phenotypes were counted per mm2 in cancer cell nests (intratumor) and stromal regions. The immune cell densities were compared with clinicopathological and genetic factors including tumor response.
Results
This study analyzed 66 samples. T1 tumors had a significantly higher density of intratumoral CD8+ T cells than T2 or larger tumors. The tBRCA1/2 mutation or HRD status was not associated with the density of any immune cell. The density of intratumoral and stromal CD4+ T cells was higher in patients showing pCR than in those without pCR. In a multivariate analysis, intratumoral and stromal CD4+ T cell density significantly predicted pCR independent of age, chemotherapy dose, HRD status, and treatment groups (P = 0.009 and 0.0057, respectively). In a subgroup analysis, the predictive value of intratumoral and stromal CD4+ T cell density persisted in the platinum-containing chemotherapy group (A1+A2) but not in the non-platinum-containing group (B1+B2).
Conclusions
Intratumoral and stromal CD4+ T cell density was an independent predictor of pCR in patients with TNBC. A larger study is warranted to confirm the results.
Trial registration
Similar content being viewed by others
Background
Triple-negative breast cancer (TNBC) is a subset of breast cancer without the expression of estrogen receptor (ER) and progesterone receptor (PgR) and without the overexpression or gene amplification of human epidermal growth factor receptor 2 (HER2) [1]. TNBC still has no specific target for treatment; thus, the current standard systemic therapy for early-stage TNBC is conventional chemotherapy, which includes anthracycline and taxane. However, the prognosis of patients with TNBC is unfavorable compared with other subtypes of breast cancer and the clinical outcome still has to be further improved, and new treatment strategies are needed [1, 2].
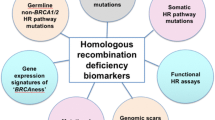
TNBC is a biologically diverse disease. Its biological characteristics include homologous recombination deficiency (HRD), gene mutation, and immune reactions [2,3,4]. Around half of TNBC has been reported to have HRD due to mutations or promotor hypermethylation of relevant genes such as BRCA1/2, PALB2, and RAD51C [5,6,7]. The assay to score HRD using cancer tissues has been developed based on loss of heterozygosity, telomeric allelic imbalance, and large-scale state transitions [8]. Several studies examined the association between HRD score and response to chemotherapy, in particular platinum agents, but the results were inconsistent [9,10,11,12].
TNBC shows a relatively high mutation burden compared with other breast cancer subtypes, and TP53 is the most frequently mutated gene in TNBC [13,14,15]. In general, a higher mutation burden is considered to lead to more neoantigen production. Indeed, the association between higher mutation burden and greater immune reaction has been reported in a variety of cancers [16]. However, in TNBC, increased immune reactions have been reported to be associated with lower mutation burden and lower clonal heterogeneity, suggesting an immune editing effect where cancer progression by clonal expansion is suppressed by immune surveillance [15, 17].
Tumor-infiltrating lymphocytes (TILs) are associated with prognosis; they can predict TNBC response to neoadjuvant chemotherapy (NAC) [18,19,20,21,22,23,24,25]. The International Immuno-Oncology Biomarker Working Group published recommendations for the standardized assessment of TILs in breast cancer tissues [26, 27]. Several international guidelines, such as the European Society of Medical Oncology Guidelines, have included TILs as a prognostic biomarker [28]. However, the subsets of lymphocytes that contribute the most to the prognostic and predictive values of TILs for TNBC remain unclear.
Japan Breast Cancer Research Group 22 (JBCRG22) trial is a multicenter trial that examined response to NAC according to the HRD status in patients with TNBC and showed good pCR rates of 65% and 45% by weekly paclitaxel + carboplatin and eribulin + carboplatin, respectively [29]. This translational research aimed to investigate the clinical significance of the immune microenvironment of TNBC in association with HRD, tumor BRCA1/2 (tBRCA1/2) mutation, and response to NAC in order to give further insights in TNBC biology including tumor microenvironment for the improvement of treatment strategies of TNBC.
Methods
JBCRG22 study
The study design, endpoints, and results of JBCRG22 have been reported previously [29]. Briefly, patients aged below 65 years with TNBC showing a high HRD status (HRD score ≧ 42) (Myriad Genetics, Inc., Salt Lake City, Utah) [8] or germline BRCA1/2 (gBRCA1/2) mutation randomly received 4 cycles of either weekly paclitaxel 80mg/m2 on days 1, 8, and 15 + carboplatin AUC6 on day 1 of a 21-day cycle (group A1) or eribulin 1.4mg/m2 on days 1 and 8 + carboplatin AUC6 on day 1 of a 21-day cycle (group A2), followed by an anthracycline-containing regimen (5-fluorouracil–epirubicin–cyclophosphamide, FEC or doxorubicin–cyclophosphamide, AC) every 21 days for 4 cycles. Patients aged below 65 years with TNBC showing a low HRD status (HRD score < 42) or those aged 65 years or older without gBRCA1/2 mutation were randomly assigned to 6 cycles of either eribulin 1.4mg/m2 on days 1 and 8 + cyclophosphamide 600mg/m2 on day 1 of a 21-day cycle (group B1) or eribulin 1.4mg/m2 on days 1 and 8 + capecitabine 2000mg/m2 b.i.d. for 14 days of a 21-day cycle (group B2); nonresponders to the first 4 cycles of the therapy received an anthracycline-containing regimen (FEC or AC) every 21 days for 4 cycles. The major exclusion criteria included having bilateral breast cancer, multiple cancers other than breast cancer, axillary lymph node dissection before the study treatment, and severe uncontrolled systemic diseases [29].
All study participants provided written informed consent. The institutional review board approved the research protocol, which conformed to the Declaration of Helsinki.
Pathological assessment of treatment response
The centralized pathologic review committee, as well as each participating institution, assessed the pathological response. The absence of residual cancer cells in the tissues indicated a pathological complete response (pCR).
Multiplex fluorescent immunohistochemistry
As previously described [30], pretreatment biopsy specimens in formalin-fixed paraffin-embedded blocks were stained by multiplexed fluorescent immunohistochemistry with an Opal IHC kit (AKOYA Biosciences, CA, USA) using antibodies against CD3 (clone SP7; Abcam, Tokyo, Japan), CD4 (4B12; Leica Microsystems, Tokyo, Japan), CD8 (4B11; Leica Microsystems, Tokyo, Japan), Foxp3 (D608R; Cell Signaling Technology, Danvers, MA, USA), CD204 (SRA-E5; TransGenic, Kobe, Japan), and pan-cytokeratin (AE1/AE3, Dako). Briefly, a whole slide was scanned using an automated imaging system (Vectra ver. 3.0, AKOYA Biosciences). After being stained by hematoxylin and eosin, the tissue slides were used to annotate the tumoral and stromal fields according to the International Immuno-Oncology Biomarker Working Group’s recommendation [27]. The whole specimens were captured, with an average of 20 areas at ×200 magnification. Using an image-analyzing software (InForm, AKOYA Biosciences), we segmented tumor tissues into cancer cell nests and stromal regions and identified immune cells with specific phenotypes (Additional file 1: Fig. S1). Before the final evaluation, manual training sessions for tissue segmentation and phenotype recognition were conducted, followed by automatic machine learning for the algorithm. An analytic software program (Spotfire, TIBCO software, CA, USA) counted the infiltrating immune cells with specific phenotypes per mm2 in cancer cell nests (intratumor) and stromal regions (stroma).
Statistical analysis
We used the Mann–Whitney test for comparing two groups, the Kruskal–Wallis test for comparing more than two groups, and the χ2-test for comparing pCR rates between groups. For multivariate analyses, logistic regression analysis was performed. The doses of paclitaxel in group A1 and eribulin in groups A2, B1, and B2 were used for the analyses. All statistical data were analyzed using the JMP version 13.2.1 (SAS Institute, Inc., Cary, NC, USA). All P values were two-sided, and a P value of less than 0.05 was considered statistically significant. All graphs were produced using the GraphPad Prism version 8.4.3 (GraphPad Software, San Diego, CA, USA) and the JMP version 13.2.1.
Results
Background characteristics of patients
A total of 66 TNBC samples from the JBCRG22 study were available and analyzed in this study. Table 1 summarizes the background characteristics of these 66 patients. The age of patients in group A (A1 or A2) was lower than that in group B (B1 or B2) because treatment groups A and B have different entry criteria including age.
Immune cells in cancer tissues in association with background characteristics
The densities of CD3+CD4+ cells (CD4+ T cells), CD3+CD8+ cells (CD8+ T cells), CD4+Foxp3+ cells (Treg cells), and CD204+ cells were compared with the patients’ background tumor characteristics (Fig. 1). The density of intratumoral CD8+ T cells was associated with T stage (P = 0.025, Fig. 2), and it was highest in T1 tumor (≤2 cm). Conversely, nodal status, histological grade, and Ki67 labeling index were not associated with the density of any immune cell type.
Immune cell density according to T stage. The vertical axis indicates cell count/mm2 and the horizontal axis indicates tumor T stage. Statistically significant P values are shown in bold italics. The numbers of patients are as follows: T1, N = 13; T2, N = 48; and T3, N = 5. The density of intratumoral CD8+ T cells was higher in T1 tumors than in T2 or T3 tumors (P = 0.025)
Tumor BRCA1/2 mutation and HRD status and immune cells
Patients with tBRCA1/2 mutation had a relatively high density of intratumoral and stromal CD8+ T cells, but no statistical significance was observed (Fig. 3). The HRD status was not associated with the density of any immune cells (Fig. 4).
Immune cell density according to tumor BRCA1/2 mutation status. The vertical axis indicates cell count/mm2, and the horizontal axis indicates the tumor BRCA1/2 mutation status. The numbers of patients are as follows: positive, N = 12; negative, N = 43. Immune cell density showed no association with tumor BRCA1/2 mutation status
Treatment response and immune cells
Patients with pCR to NAC showed a higher density of intratumoral and stromal CD4+ T cells than those with non-pCR in the whole population (P = 0.036 and 0.031, respectively; Fig. 5). The multivariate analysis revealed that the density of intratumoral and stromal CD4+ T cells significantly predicted pCR independent of age, dose, HRD status, and treatment groups (P = 0.009 and 0.0057, respectively; Table 2).
Immune cell density according to the pathological response. The vertical axis indicates cell count/mm2, and the horizontal axis indicates the pathological response. Statistically significant P values are shown in bold italics. The numbers of patients are as follows: pCR, N = 23; non-pCR, N = 43. Patients with pCR to neoadjuvant chemotherapy showed a higher density of intratumoral and stromal CD4+ T cells than those with non-pCR (P = 0.036 and 0.031, respectively).
Subgroup analyses of patients who received platinum-containing chemotherapy (groups A1+A2) and those who received non-platinum-containing chemotherapy (groups B1+B2) were performed. The HRD status was excluded from the analysis because all patients in the platinum-containing chemotherapy group had tumors with a high HRD status (Table 1). Consistent with the whole population, both intratumoral and stromal CD4+ T cell densities independently predicted pCR in the platinum-containing chemotherapy group (P = 0.018 and 0.022, respectively, Table 3), but not in the non-platinum-containing chemotherapy group (P = 0.38 and 0.73, respectively; Table 3). As an exploratory analysis, the predictive value of the density of each immune cell type for pCR was assessed in each treatment group, which showed no significant association of any immune cell type with pCR (Additional file 1: Fig. S2 A to D).
In the extended analyses of CD4+/CD8+, CD4+/Foxp3+, Foxp3+/CD4+, and CD8+/Foxp3+ ratios, the pathological response was not associated with any of these ratios.
We further performed exploratory analyses to examine whether pCR rates differ depending on the immune phenotypes [31]. We categorized the immune microenvironment into three groups based on the densities of immune cells, either CD4+ T cells or CD8+ T cells, in cancer cell nests and stromal regions: immune inflamed, high cell density in both cancer cell nests and stromal regions; immune excluded, low cell density in cancer cell nests and high cell density in stromal regions; and immune desert, low cell densities in both cancer cell nests and stromal regions (Additional file 1: Fig. S3 A to C). No significant differences in pCR rate were observed between different immune phenotypes for both CD4+ T cells and CD8+ T cells (P = 0.43 and 0.33, respectively; Additional file 1: Fig. S3 D).
Discussion
This study demonstrated that intratumoral and stromal CD4+ T cell densities were independent predictive factors of pCR in patients with TNBC who received NAC, particularly platinum-containing chemotherapy. However, previous studies that examined the predictive values of TILs for pCR to neoadjuvant platinum-containing chemotherapy obtained inconsistent results. A study using samples from GeparSixto showed that TILs were associated with pCR in patients with TNBC who received platinum-containing NAC [20]. In contrast, a pooled analysis of five phase II studies of neoadjuvant platinum-based chemotherapy in TNBC failed to show the predictive values of intratumoral and stromal TILs for pCR [32]. Although such discrepancy cannot be clearly explained, differences in combined chemotherapeutic agents could be one reason. Another explanation would be that among TILs, different subsets of immune cells may have different clinical significance in TNBC. In patients who received NAC with anthracycline- and/or taxane-based chemotherapies, CD8+ TILs are associated with pCR [33, 34]. Our results indicate that of all the cells in cancer tissues, CD4+ T cells may predict pathological response to platinum-containing NAC in patients with HRD-high TNBC. Thus, different subsets of immune cells may have different clinical values. A detailed analysis of the subset of TILs will help elucidate the clinical utilities of tumor-associated immune cells, leading to improved treatment strategies for TNBC.
When examining the clinical significance of immune cell subsets, assessing how to define each immune cell subset is important. For example, CD4 may be expressed not only in T cells but also in a subpopulation of monocytes, causing a bias and discrepancies between studies [35]. Our studies used CD4 or CD8 markers together with CD3; thus, we could better identify CD4+ or CD8+ T cell subset. When comparing the results from different studies, knowing the definition of each immune subset is crucial.
Our study revealed that immune cells were not associated with either tBRCA1/2 mutation or HRD status, consistent with a pooled analysis that showed no association between intratumoral or stromal TIL density and either the HRD status or tumor BRCA1/2 mutation status in TNBC [32]. Thus, TILs and the HRD status or tBRCA1/2 mutation status may have distinct clinical values. In a study with 414 Danish patients with breast cancer showing gBRCA1/2 mutation, patients with gBRCA1 mutation had a higher rate of CD4+ cells than those with gBRCA2 mutation [36]. However, the present study did not compare patients with and without gBRCA1/2 mutation and examined patients with tumor mutation but not those with germline mutation.
Immune editing is a concept depicting the immune cell status depending on the cancer progression stage [17, 37]. In the elimination phase, immune cells work actively to eliminate developing cancer cells, as reflected by immune cell accumulation. In the equilibrium phase, immunologic mechanisms prevent cancer growth. Then, in the escape phase, the immune cells no longer block tumor growth. In our study, T1 tumors had a higher density of intratumoral CD8+ T cells than T2 or larger tumors, which might be a reflection of immune editing. This result is similar to those studies showing that larger tumors had a lower density of immune cells than smaller tumors [33, 34].
This study has several limitations. One of the major limitations is a small sample size in each treatment arm. Considering that JBCRG22 examined four different regimens according to the HRD status, each arm had a small number of patients; thus, the result in each single arm needs to be interpreted with caution. It is of clinical importance to conduct a larger study to validate the results in this study. Another limitation is that survival analysis was not performed because of the short follow-up period. The prognostic value of each immune subset needs to be clarified in future studies with a longer follow-up. Lack of the analysis on different types of CD4+ T cells such as naive, central memory, effector memory, and effector in terms of response to NAC is another limitation. Furthermore, in addition to the previously known Th1 and Th2 types of CD4+ T cells, the existence of Th9, Th17, and Th22 types of cells has recently been reported, but their roles remain unclear. Because studies on the clinical significance of different types of CD4+ T cells will give further insights in the field of immune microenvironment of TNBC, it is of clinical value to conduct such studies in the future.
Conclusions
The density of intratumoral and stromal CD4+ T cells was an independent predictor for pCR to NAC, especially platinum-containing chemotherapies, in patients with TNBC. Because the sample size is limited in this study, a larger study is required to confirm the results.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CD4+ T cells:
-
CD3+CD4+ cells
- CD8+ T cells:
-
CD3+CD8+ cells
- ER:
-
Estrogen receptor
- gBRCA:
-
Germline BRCA
- HER2:
-
Human epidermal growth factor receptor 2
- HRD:
-
Homologous recombination deficiency
- NAC:
-
Neoadjuvant chemotherapy
- pCR:
-
Pathological complete response
- PgR:
-
Progesterone receptor
- tBRCAm:
-
Tumor BRCA mutation
- TIL:
-
Tumor-infiltrating lymphocyte
- TNBC:
-
Triple-negative breast cancer
- Treg cells:
-
CD4+Foxp3+ cells
References
Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13(15 Pt 1):4429–34.
Bianchini G, De Angelis C, Licata L, Gianni L. Treatment landscape of triple-negative breast cancer - expanded options, evolving needs. Nat Rev Clin Oncol. 2022;19(2):91–113.
Denkert C, Liedtke C, Tutt A, von Minckwitz G. Molecular alterations in triple-negative breast cancer-the road to new treatment strategies. Lancet. 2017;389(10087):2430–42.
Jiang YZ, Ma D, Suo C, Shi J, Xue M, Hu X, et al. Genomic and transcriptomic landscape of triple-negative breast cancers: subtypes and treatment strategies. Cancer Cell. 2019;35(3):428–440.e425.
Bertucci F, Ng CKY, Patsouris A, Droin N, Piscuoglio S, Carbuccia N, et al. Genomic characterization of metastatic breast cancers. Nature. 2019;569(7757):560–4.
Sharma P, Barlow WE, Godwin AK, Pathak H, Isakova K, Williams D, et al. Impact of homologous recombination deficiency biomarkers on outcomes in patients with triple-negative breast cancer treated with adjuvant doxorubicin and cyclophosphamide (SWOG S9313). Ann Oncol. 2018;29(3):654–60.
Staaf J, Glodzik D, Bosch A, Vallon-Christersson J, Reuterswärd C, Häkkinen J, et al. Whole-genome sequencing of triple-negative breast cancers in a population-based clinical study. Nat Med. 2019;25(10):1526–33.
Timms KM, Abkevich V, Hughes E, Neff C, Reid J, Morris B, et al. Association of BRCA1/2 defects with genomic scores predictive of DNA damage repair deficiency among breast cancer subtypes. Breast Cancer Res. 2014;16(6):475.
Mayer EL, Abramson V, Jankowitz R, Falkson C, Marcom PK, Traina T, et al. TBCRC 030: a phase II study of preoperative cisplatin versus paclitaxel in triple-negative breast cancer: evaluating the homologous recombination deficiency (HRD) biomarker. Ann Oncol. 2020;31(11):1518–25.
Telli ML, Timms KM, Reid J, Hennessy B, Mills GB, Jensen KC, et al. Homologous recombination deficiency (HRD) score predicts response to platinum-containing neoadjuvant chemotherapy in patients with triple-negative breast cancer. Clin Cancer Res. 2016;22(15):3764–73.
Tutt A, Tovey H, Cheang MCU, Kernaghan S, Kilburn L, Gazinska P, et al. Carboplatin in BRCA1/2-mutated and triple-negative breast cancer BRCAness subgroups: the TNT trial. Nat Med. 2018;24(5):628–37.
Von Minckwitz G, Timms K, Untch M, Elkin EP, Fasching PA, Schneeweiss A, et al. Prediction of pathological complete response (pCR) by homologous recombination deficiency (HRD) after carboplatin-containing neoadjuvant chemotherapy in patients with TNBC: results from GeparSixto. J Clin Oncol. 2015 (suppl; abstr 1004);33:2015.
Callens C, Driouch K, Boulai A, Tariq Z, Comte A, Berger F, et al. Molecular features of untreated breast cancer and initial metastatic event inform clinical decision-making and predict outcome: long-term results of ESOPE, a single-arm prospective multicenter study. Genome Med. 2021;13(1):44.
Cancer Genome Atlas Network.: Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70.
Safonov A, Jiang T, Bianchini G, Győrffy B, Karn T, Hatzis C, et al. Immune gene expression is associated with genomic aberrations in breast cancer. Cancer Res. 2017;77(12):3317–24.
Rooney MS, Shukla SA, Wu CJ, Getz G, Hacohen N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell. 2015;160(1-2):48–61.
Karn T, Jiang T, Hatzis C, Sänger N, El-Balat A, Rody A, et al. Association between genomic metrics and immune infiltration in triple-negative breast cancer. JAMA Oncol. 2017;3(12):1707–11.
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 2014;32(27):2959–66.
Denkert C, Loibl S, Noske A, Roller M, Muller BM, Komor M, et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol. 2010;28(1):105–13.
Denkert C, von Minckwitz G, Brase JC, Sinn BV, Gade S, Kronenwett R, et al. Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol. 2015;33(9):983–91.
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19(1):40–50.
Loi S, Michiels S, Adams S, Loibl S, Budczies J, Denkert C, et al. The journey of tumor-infiltrating lymphocytes as a biomarker in breast cancer: clinical utility in an era of checkpoint inhibition. Ann Oncol. 2021;32(10):1236–44.
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol. 2013;31(7):860–7.
Loi S, Drubay D, Adams S, Pruneri G, Francis PA, Lacroix-Triki M, et al. Tumor-infiltrating lymphocytes and prognosis: a pooled individual patient analysis of early-stage triple-negative breast cancers. J Clin Oncol. 2019;37(7):559–69.
Dieci MV, Mathieu MC, Guarneri V, Conte P, Delaloge S, Andre F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in two phase III randomized adjuvant breast cancer trials. Ann Oncol. 2015;26(8):1698–704.
Hendry S, Salgado R, Gevaert T, Russell PA, John T, Thapa B, et al. Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the International Immunooncology Biomarkers Working Group: part 1: assessing the host immune response, TILs in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv Anat Pathol. 2017;24(5):235–51.
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol. 2015;26(2):259–71.
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30(8):1194–220.
Masuda N, Bando H, Yamanaka T, Kadoya T, Takahashi M, Nagai SE, et al. Eribulin-based neoadjuvant chemotherapy for triple-negative breast cancer patients stratified by homologous recombination deficiency status: a multicenter randomized phase II clinical trial. Breast Cancer Res Treat. 2021;188(1):117–31.
Ikarashi D, Kitano S, Tsuyukubo T, Takenouchi K, Nakayama T, Onagi H, et al. Pretreatment tumour immune microenvironment predicts clinical response and prognosis of muscle-invasive bladder cancer in the neoadjuvant chemotherapy setting. Br J Cancer. 2022;126(4):606–614.
Chen DS, Mellman I. Elements of cancer immunity and the cancer-immune set point. Nature. 2017;541(7637):321–30.
Telli ML, Chu C, Badve SS, Vinayak S, Silver DP, Isakoff SJ, et al. Association of tumor-infiltrating lymphocytes with homologous recombination deficiency and BRCA1/2 status in patients with early triple-negative breast cancer: a pooled analysis. Clin Cancer Res. 2020;26(11):2704–10.
Miyashita M, Sasano H, Tamaki K, Chan M, Hirakawa H, Suzuki A, et al. Tumor-infiltrating CD8+ and FOXP3+ lymphocytes in triple-negative breast cancer: its correlation with pathological complete response to neoadjuvant chemotherapy. Breast Cancer Res Treat. 2014;148(3):525–34.
Seo AN, Lee HJ, Kim EJ, Kim HJ, Jang MH, Lee HE, et al. Tumour-infiltrating CD8+ lymphocytes as an independent predictive factor for pathological complete response to primary systemic therapy in breast cancer. Br J Cancer. 2013;109(10):2705–13.
Filion LG, Izaguirre CA, Garber GE, Huebsh L, Aye MT. Detection of surface and cytoplasmic CD4 on blood monocytes from normal and HIV-1 infected individuals. J Immunol Methods. 1990;135(1-2):59–69.
Jørgensen N, Hviid TVF, Nielsen LB, Sønderstrup IMH, Eriksen JO, Ejlertsen B, et al. Tumour-infiltrating CD4-, CD8- and FOXP3-positive immune cells as predictive markers of mortality in BRCA1- and BRCA2-associated breast cancer. Br J Cancer. 2021;125(10):1388–98.
Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science. 2011;331(6024):1565–70.
Acknowledgements
The authors would like to thank the patients who participated in the JBCRG22 TR study and their families and the investigators and research coordinators at the participating institutions. The authors would also like to thank Nobuko Aoki, Atsuko Kuzuha, Michiro Soma, and colleagues in the Japan Breast Cancer Research Group (JBCRG) administrative office for their contribution to the management of this study. In addition, the authors would like to thank the JBCRG data center for its contribution to patient registration, data management, and analyses.
Funding
This study was a physician-led clinical trial funded by the Japan Breast Cancer Research Group and Eisai Co., Ltd.
Author information
Authors and Affiliations
Contributions
TU, SK, NM, DI RV, and KK conceived and designed the study. DI and MY carried out the analysis. MT2 and SO advised on the study design. TC and HH contributed to the pathological assessment. SM advised on the statistical approaches. TU, TK, HB, TY, SO1, SN, TN, MT1, SS, KA, KK, and SO2 contributed to data acquisition. All authors contributed to the interpretation of the findings. TU drafted the initial manuscript, and all authors contributed to the revisions of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the institutional review board of each participating institution. All patients provided written informed consent for this translational research. Some of the study results were presented in Poster session at the ESMO Virtual Congress 2021.
Consent for publication
Not applicable.
Competing interests
TU: honoraria from Eisai Co., Ltd., Chugai Pharmaceutical Co., Ltd., Astra Zeneca, Novartis Pharma K.K.; support for attending meetings from Eisai Co., Ltd.; consulting fees from Taiho, SK: personal fees from Astra Zeneca, personal fees from Pfizer, grants and personal fees from Boehringer Ingelheim, personal fees from Taiho, personal fees from Novartis, grants and personal fees from MSD, personal fees from Sumitomo Dainippon Pharma, grants and personal fees from Eisai, grants from Astellas, grants from Gilead Sciences, grants and personal fees from Ono Pharmaceutical Co., Ltd., personal fees from Bristol-Myers Squibb, grants and personal fees from REGENERON, personal fees from Rakuten Medical, grants from PACT Pharma, grants from Takara Bio Inc., personal fees from GSK, grants and personal fees from Daiichi-Sankyo, grants and personal fees from Chugai , personal fees from ImmuniT Research Inc., grants from AMED (Japan Agency for Medical Research and Development), grants from JSPS (Japan Society for the Promotion of Science), and personal fees from PMDA (Pharmaceuticals and Medical Devices Agency), outside the submitted work, NM: grand from Chugai, Eli Lilly, Astra Zeneca, Pfizer, Daiichi-Sankyo, MSD, Eisai, Novartis, Sanofi, Kyowa-Kirin, and Nippon-Kayaku; honoraria from Chugai, Pfizer, Astra Zeneca, Eli Lilly, and Eisai; executive board and board of directors of JBCRG; TY: honoraria from Astra Zeneca, Daiichi-Sankyo, Eli Lilly, Novartis, Chugai, Eisai, Kyowa-Kirin, and Pfizer; SN: honoraria from Eli Lilly, Chugai, Pfizer, and Eisai; TN: honoraria from Chugai, Eli Lilly, Novartis, Astra Zeneca, Pfizer, Taiho, Daiichi-Sankyo, and Eisai; MT: honoraria from Astra Zeneca, Eli Lilly, Pfizer, Eisai, and Chugai; SS: grants from Taiho, Eisai, Chugai, Takeda, MSD, Novartis, Astra Zeneca, Daiichi Sankyo, and Eli Lilly; honoraria from Chugai, Kyowa Kirin, MSD, Novartis, Eisai, Takeda, Daiichi Sankyo, Eli Lilly, Astra Zeneca, Pfizer, Taiho, Nipponkayaku, data safety monitoring board or advisory board of Chugai/Roche, Astra Zeneca, Eli Lilly, Pfizer, Kyowa Kirin, Daiichi Sankyo, Novartis, executive board member of JBCRG, JBCS, BIG; KA: grants from Chugai Pharmaceutical, Eisai, and Takeda Pharmaceutical; honoraria from Chugai Pharmaceutical, Astra Zeneca, Novartis Pharma, Mochida Pharmaceutical, Eli Lilly, Eisai, Taiho Pharmaceutical, Daiichi Sankyo, Ono Pharmaceutical; KK: grants from TERUMO, Astellas, Eli Lilly, Kyoto Breast Cancer Research Network; consulting fees from Becton Dickinson Japan; honoraria from Eisai, Chugai, and Takeda; SM: grants from Nippon Boehringer Ingelheim, Eisai; honoraria from Astra Zeneca, Taiho Pharmaceutical Co. Ltd, Chugai Pharmaceutical, Nippon Boehringer Ingelheim, Bristol Myers Squibb Co. Ltd, Novartis Pharma KK, MSD KK, Kyowa Kirin Co. Ltd, Astellas Pharma, Pfizer Japan, Ono Pharmaceutical Co. Ltd, Eli Lilly Japan; SO: grant from Taiho, Eisai; honoraria from Astra Zeneca, Chugai, Eli Lilly, Taiho, Pfizer, Daiichi Sankyo; executive board member of JBCRG, JBCS; MT: grant from Chugai, Takeda, Pfizer, Kyowa-Kirin, Taiho, JBCRG assoc., Eisai, Eli Lilly, Daiichi-Sankyo, AstraZeneca, Astellas, Shimadzu, Yakult, Nippon Kayaku, AFI technology, Luxonus, Shionogi, and GL Science; honoraria from Chugai, Takeda, Pfizer, Kyowa-Kirin, Taiho, Eisai, Daiichi-Sankyo, AstraZeneca, Eli Lilly, MSD, Exact Science, Novartis, Konica Minolta, Shimadzu, Yakult, and Nippon Kayaku; Advisory board of Kyowa-Kirin, Daiichi-Sankyo, Eli Lilly, Konica Minolta, BMS, Athenex Oncology, Bertis, Terumo, Kansai Medical Net; board of directors of JBCRG assoc., KBCRN, OOTR; associate editor of the British Journal of Cancer, Scientific Reports, Breast Cancer Research and Treatment, Cancer Science, Frontiers in Women’s Cancer, Asian Journal of Surgery, Asian Journal of Breast Surgery; deputy editor of International Journal of Oncology.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Image analysis. Representative image of immunofluorescence with the following markers: CD3 (blue), CD4 (yellow), CD8 (red), FoxP3 (pink), CD204 (green), and cytokeratin (brown) (A); tissue segmentation of the intratumoral (red) and stromal (green) areas (B); cell segmentation (C) and cell phenotyping (D) which merged with tissue segmentation (E): cancer cells (orange), CD4+ T cells (yellow), CD8+ T cells (red), CD204+ cells (green), other stromal cells (gray). Figure S2. Immune cell density according to pathological response in each treatment group: group A1 (A), group A2 (B), group B1 (C), group B2 (D). Figure S3. Immune phenotype and pCR. (A) Immune inflamed, high cell density in both cancer cell nests and stromal regions; immune excluded, low cell density in cancer cell nests and high cell density in stromal regions; immune desert, low cell densities in both cancer cell nests and stromal regions. (B) Immune phenotype for CD4+ T cells. (C) Immune phenotype for CD8+ T cells. (D) pCR rate according to immune phenotype for CD4+ T cells and CD8+ T cells.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ueno, T., Kitano, S., Masuda, N. et al. Immune microenvironment, homologous recombination deficiency, and therapeutic response to neoadjuvant chemotherapy in triple-negative breast cancer: Japan Breast Cancer Research Group (JBCRG)22 TR. BMC Med 20, 136 (2022). https://doi.org/10.1186/s12916-022-02332-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-022-02332-1