Abstract
Background
Faecal immunochemical tests (FITs) are used to triage primary care patients with symptoms that could be caused by colorectal cancer for referral to colonoscopy. The aim of this study was to determine whether combining FIT with routine blood test results could improve the performance of FIT in the primary care setting.
Methods
Results of all consecutive FITs requested by primary care providers between March 2017 and December 2020 were retrieved from the Oxford University Hospitals NHS Foundation Trust. Demographic factors (age, sex), reason for referral, and results of blood tests within 90 days were also retrieved. Patients were followed up for incident colorectal cancer in linked hospital records. The sensitivity, specificity, positive and negative predictive values of FIT alone, FIT paired with blood test results, and several multivariable FIT models, were compared.
Results
One hundred thirty-nine colorectal cancers were diagnosed (0.8%). Sensitivity and specificity of FIT alone at a threshold of 10 μg Hb/g were 92.1 and 91.5% respectively. Compared to FIT alone, blood test results did not improve the performance of FIT. Pairing blood test results with FIT increased specificity but decreased sensitivity. Multivariable models including blood tests performed similarly to FIT alone.
Conclusions
FIT is a highly sensitive tool for identifying higher risk individuals presenting to primary care with lower risk symptoms. Combining blood test results with FIT does not appear to lead to better discrimination for colorectal cancer than using FIT alone.
Similar content being viewed by others
Background
Diagnosing colorectal cancer in patients who present to primary care can be challenging because many of the symptoms of colorectal cancer are shared with other, less serious causes. Colonoscopy is the definitive test to diagnose colorectal cancer, but referring all patients with symptoms of possible colorectal cancer for colonoscopy would cause significant strain on health care resources and present unnecessary risks to patients [1]. After recommending that FIT be used in the national bowel cancer screening programme in 2016, in 2017, the faecal immunochemical test (FIT) was recommended by the National Institute for Health and Care Excellence (NICE) as a triage test for patients presenting to primary care with low risk symptoms of possible colorectal cancer [2]. The evidence underpinning that recommendation was drawn primarily from higher risk populations, and there was limited evidence about how it would perform in primary care [3,4,5].
There has been a rapid increase in publications about FIT use in symptomatic patients over the last 5 years [3, 6, 7]. FIT has consistently been shown to have high sensitivity and specificity for colorectal cancer at a threshold of 10μg Hb/g faeces or lower, in primary and secondary care [7,8,9]. Despite a high negative predictive value, nearly one in ten colorectal cancers will be missed using FIT alone to select who should be referred for investigation [10]. Developing strategies to identify symptomatic people with FIT-negative colorectal cancer has become an urgent priority due to the increased use of FIT to defer or decline colorectal investigation during the COVID-19 pandemic [11]. Furthermore, as the number of colorectal cancer presentations is expected to increase, and health care resources continue to be strained by ongoing effects of the pandemic, efforts to reduce unnecessary referrals by increasing specificity would be especially worthwhile [11].
Clinical prediction models are one strategy to achieve these aims. However, the faecal haemoglobin age and sex test (FAST) score did not improve utility over FIT alone [12]. FIT has also been shown to outperform multivariable models including age, sex, and symptoms prompting urgent cancer referral [13]. Combining commonly used blood tests with FIT could further optimise the triage of symptomatic patients in primary care for colorectal cancer investigation [14, 15]. Using the largest existing UK cohort of symptomatic patients tested with FIT in primary care [16], the aim of this study was to assess whether complementing FIT with blood test values could improve the predictive performance of FIT.
Methods
Study design
Population/setting
Data were retrieved from the Oxford University Hospitals NHS Foundation Trust (OUH). OUH serves all 67 General Practice (GP) surgeries in the county of Oxfordshire, UK, with a population of approximately 660,000. Based at the John Radcliffe Hospital, the Clinical Biochemistry Laboratory performs over 8 million tests a year. This study was registered as a service evaluation on the OUH Datix register (CSS-BIO-3 4730).
FITs
All consecutive FIT results (measured in μg Hb/g faeces) between March 2017 and December 21, 2020, were retrieved retrospectively from the OUH Clinical Biochemistry Laboratory Information Management System.
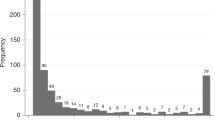
After restricting to FITs requested by primary care clinicians and the first FIT in any given individual, FITs were retained for inclusion in this analysis if the five most common “core” blood tests (haemoglobin, platelets, white cell count, mean cell haemoglobin [MCH], and mean cell volume [MCV]) were available, patients were aged 18 or older, had known sex, and had non-missing FIT results (Fig. 1).
Faecal specimens were collected into standard pots by patients in primary care and referred to the central laboratory where sampling was undertaken using the Extel Hemo-Auto MC device. Prepared samples were analysed for FIT using the HM-JACKarc analyser (Hitachi Chemical Diagnostics Systems Co., Ltd., Tokyo, Japan, and distributed in the UK by Alpha Labs Ltd., Eastleigh, Hants) a method recommended for use by NICE [2]. The method had a calibration range of 7–400 μg Hb/g faeces. For the duration of the study period, 7 μg Hb/g was used to define a positive result in the lab, as this threshold was determined prior to the NICE recommendation to use 10 μg Hb/g faeces. Immunoassay reproducibility assessed across 12 months had a coefficient of variation (CV) of between 4.4 and 8.8%. The overall imprecision of the process including sampling variation was between 7.0 and 13.5 CV% [17]. FIT samples were assayed and recorded prior to and independent of the any subsequent pathology findings.
Additional variables
Age, sex, clinical indication, and results of contemporaneous blood tests were retrieved for each patient. To extract the clinical indication, free text fields included in the electronic FIT request were searched for common indications (abdominal pain, bloating, blood in stool, change in bowel habit, constipation, diarrhoea, family history of cancer, fatigue, melaena, rectal pain, and weight loss) using numerous permutations of spelling and phrasing.
Blood test results reported less than 60 days prior to or 30 days post FIT were retrieved. The most routinely used blood tests and those with a hypothesised relationship with colorectal cancer risk were selected for analysis (haemoglobin, platelets, white cell count, MCH, and MCV; serum ferritin; and c-reactive protein [CRP]) [18]. The same analytical methods for the blood tests were used throughout the study period: full blood count, including haemoglobin, platelets, white cell count, MCH, and MCV were analysed using a Sysmex XN analyser (Sysmex UK Ltd, Milton Keynes, UK); ferritin using an Abbott Architect i2000 and CRP using the Abbott Architect c16000 (both Abbott Diagnostics UK, Maidenhead, UK).
Outcomes
The composite reference standard incorporated the review of multiple-linked databases (hospital clinical records, pathology results, and endoscopy and radiology reports) for evidence of a new colorectal cancer diagnosis. In the primary analysis, a patient was considered a colorectal cancer case if a diagnosis occurred within 6 months of the FIT. The cut-off date for eligible FITs (December 21, 2020) was selected to allow for at least 6 months follow-up for all patients (until the end of linked clinical records, June 21, 2021). As patients were observed for outcomes through passive linkage rather than active follow-up, patients were not censored or lost to follow-up during that interval. A composite reference standard was used as not all patients tested with FIT in primary care are referred for definitive testing. A reliance on definitive testing alone would lead to verification bias for FIT-positive patients. Database review was independent of FIT value.
Patient and public involvement
No patients were directly involved in designing the research question or in conducting the research. A patient advocate provided feedback on interpretation of the results and key messages. Our findings will be disseminated to patients and the public through the NIHR BRC, Nuffield Department of Primary Care Health Sciences, Oxford Cancer, and OxCODE.
Statistical analysis
Three approaches were investigated to optimise FIT.
-
1.
FIT alone—dichotomous FIT at a cut-off of greater than or equal to 2 or 10 μg Hb/g faeces;
These cut-offs were based on the assays Limit of Detection (2 μg Hb/g faeces) and the cut-off recommended by NICE for primary care triage in 2017 (10 μg Hb/g faeces) and align with existing research [2, 9].
-
2.
FIT-Blood test pairs—dichotomous FIT and dichotomous blood test result;
A test was considered positive if patients fell above the cut-off value for FIT (2 or 10 μg Hb/g faeces) and had an abnormal blood test result. The threshold for abnormal blood tests were pre-specified based on standard clinical practice [19].
-
3.
Multivariable FIT—modelling including FIT, blood tests, age, and sex.
Logistic regression was used to generate predicted probabilities of colorectal cancer. Backward stepwise selection was used to select covariates. Because serum ferritin and CRP were only available for a subset of cases, stepwise selection was conducted on an imputed dataset with 10 replicates using predictive mean matching. In models where CRP or serum ferritin were retained, coefficients for each variable in the imputed and complete case datasets were compared, and if similar, the model results from the complete case dataset were reported. The three modelling approaches are defined below.
-
Model A: FIT, age, and blood test results (continuous) and sex (dichotomous).
-
Model B: FIT and blood test results (dichotomous), age (categorical), and sex (dichotomous)
-
Model C: FIT (spline), age (continuous), sex, and blood tests (dichotomized).
The restricted cubic spline function for FIT was specified to have knots at 2, 10, 50, and 100 μg Hb/g faeces. Four knots were selected to yield a model with at least 20 events per variable, to minimise optimism bias [20]. Ninety-five percent confidence intervals were estimated using the Wilson Score method [21]. The positive predictive value (PPV) and negative predictive value (NPV) were additionally expressed as the number of positive FITs to detect one cancer (number needed to scope) and the cancer miss rate per 10,000 negative tests. To permit a comparison of model performance, the probability cut-off to determine a positive result was selected to match the sensitivity of the FIT alone at a cut-off of 10 μg Hb/g faeces.
Sensitivity and subgroup analyses
Each of the approaches 1, 2, and 3 outlined above were replicated with 12 months of follow-up. The FIT alone approach was applied to subgroups defined by FIT date (prior to or during the COVID-19 pandemic), age group (<40, >50, >60, >70, >80), sex, blood test results, and clinical indication (individual symptoms and meeting 2017 NICE DG30 guideline criteria for FIT use [yes vs. no]). The predictive value of abnormal blood tests was estimated in subgroups of FIT-negative patients at thresholds of 2 and 10 μg Hb/g faeces.
All analyses were conducted using Stata version 16.1.
Results
Descriptive
A total of 16,604 of 18,656 available FITs (89%) were included in the study. Included patients were representative of the overall sample (Table 1). Study subjects had a median age of 61 and were 58% female. One-hundred thirty-nine (139) cancers were diagnosed within 6 months of the FIT test (0.8%). Patients who were diagnosed with cancer were older (median age 72) and more likely to be male (60%), to have a FIT ≥10 μg Hb/g faeces, and/or to have abnormal blood tests (Table 1, Fig. 2, Additional file 1: Table S1).
For 90% of included patients, the free text in the electronic FIT request mapped onto at least one of the pre-specified 11 clinical indication categories. The most common of these was change in bowel habit (40%), then anaemia (26%) and abdominal pain (18%, Table 1). The most common clinical indications in people with cancer were anaemia (35%), change in bowel habit (32%), blood in stool (16%), and abdominal pain (17%).
Low haemoglobin was the most common abnormal blood test result (31% of all patients, 52% of those with a subsequent cancer diagnosis, Table 1) followed by low MCH (16% and 34%, respectively).
FIT alone
At a threshold of 2 μg Hb/g faeces, 17.1% of patients would be considered FIT positive. Sensitivity was 96.4% (95% CI 91.9–98.5), specificity 83.5% (95% CI 82.9–84.1), PPV 4.7% (95% CI 4.0–5.5), and NPV 100% (95% CI 99.9–100) (Table 2, Additional file 1: Table S2). One cancer was detected for every twenty-one positive FITs, and the cancer miss rate was 4 cancers per 10,000 negative tests (Table 2).
At a threshold of 10 μg Hb/g faeces, 9.2% of patients would be considered FIT positive. Sensitivity was 92.1% (95% CI 86.4–95.5), specificity 91.5% (95% CI 91.1–91.9), PPV 8.4% (95%CI 7.1–9.9), and NPV 99.9% (95% CI 99.9–100) (Table 1, Additional file 1: Table S2). One cancer was detected for every twelve positive FITs, and a miss rate of 7 cancers per 10,000 negative tests (Table 2).
FIT-blood test pairs
Sensitivity ranged from 3.3% (FIT≥2 or 10 μg Hb/g faeces and raised CRP) to 56.8% (FIT≥2 μg Hb/g faeces and low serum ferritin) for pairings of FIT and blood tests. Specificity was higher for almost all pairings compared to a FIT-alone approach leading to fewer positives being needed to detect one cancer. However, the cancer miss rate per 10,000 tests increased 14-fold compared to a FIT alone approach (Table 2).
Multivariable FIT
-
A)
Model A (with continuous FIT): sex and continuous variables for age, serum ferritin, platelets, and CRP were retained. Specificity was 45.9% (95% CI 44.7–47.1), compared to 90.0% for FIT alone (in the subset with serum ferritin and CRP), leading to one cancer in every 57 positive tests compared to one in 12 in the FIT-only approach (Table 3, Additional file 1: Table S2).
-
B)
Model B (dichotomous FIT, blood tests): FIT, sex, and low MCV were retained. Specificity was 90.1% (95% CI 89.6–90.5), similar to FIT alone at FIT≥10 μg Hb/g faeces, leading to 14 positive tests to detect one cancer.
-
C)
Model C (FIT spline): FIT, sex, and low MCV were retained. Specificity was 91.5% (95% CI 91.1–91.9) with one cancer detected for every 12 positive FITs.
In summary, Models B and C performed similarly to FIT alone but no approach that integrated blood test results improved the overall performance of FIT. While FIT was always retained in stepwise selection irrespective of form, including the blood test variables in different forms (e.g., continuous vs. dichotomized) resulted in different variables being retained in the models. Odds ratios for the predictors and the log likelihood and area under the curve for each model are provided in Additional file 1: Table S3. A plot of apparent calibration did not reveal any causes for concern.
The age-specific probabilities of colorectal cancer by sex and FIT score based on Model C are illustrated in Fig. 3. For males and females, the probability of colorectal cancer reached 3% (the cut-off specified to prompt urgent investigation by NICE [22]) at FIT values of 17 and 25, respectively. There were no significant differences by age since age was not a significant predictor of cancer risk after accounting for FIT (Additional file 1: Table S3).
FIT-negative cancers
The characteristics of the 11 patients with false negative tests at a FIT threshold of 10 μg Hb/g faeces are provided in Table 3. Ten had at least one GP-reported clinical indication with the most common being change in bowel habit (n = 6). Eight of the 11 had at least one abnormal blood test with the most common being raised CRP (5 of 10 with known values). Median days from FIT to cancer diagnosis was 27 days among false negatives (interquartile range 21 to 55) compared to 34 (21, 64) among persons diagnosed with cancer overall (Table 4).
Subgroup and sensitivity analyses
Patient demographics, clinical indication, prevalence of abnormal blood tests, FIT score, and performance of FIT were largely consistent prior to and during the COVID-19 pandemic (Additional file 1: Tables S4 and S5). The median age of persons undergoing FIT was older during COVID (64 vs. 59 years), but the interquartile range was similar (51 to 76 vs. 51 to 74). There were no significant differences in sensitivity, specificity, PPV, or NPV of FIT.
PPV was higher among males than females, but the confidence intervals for the two sexes overlapped at a threshold of 10 μg Hb/g faeces. At 2 μg Hb/g faeces, PPV and NPV decreased with increasing age. At 10 μg Hb/g faeces, PPV and NPV were largely consistent by age group (Additional file 1: Table S6).
There was no evidence that the PPV of FIT was significantly higher within subgroups defined by symptoms at presentation or blood test other than MCV (Additional file 1: Table S6). Sensitivity increased and specificity decreased in subgroups defined by increasingly severe anaemia (Additional file 1: Table S7). Fifty-seven percent of patients met the criteria for FIT under the DG30, which specifies use for patients without rectal bleeding and specific symptoms depending on age [2]. The incidence of cancer was slightly lower in the DG30-qualifying group (0.8 vs. 0.9%), and specificity was marginally higher (84.3 vs. 82.5% in other, Supplementary Table 8). Results did not meaningfully change when the follow-up period was extended to 12 months (Additional file 1: Tables S9 and S10). The positive predictive value of an abnormal blood test in the FIT-negative population was consistently less than 1% (Additional file 1: Table S11).
Discussion
Statement of principal findings
In this large cohort of patients tested with FIT in primary care, neither age, nor blood test results remained strong enough predictors of colorectal cancer to improve on the performance of FIT. While the number of false positives could be reduced by taking into account blood tests, the large associated increase in false negatives outweighed the benefit. In addition, there was no evidence to suggest that using clinical indication as a rule-out or rule-in factor would improve the efficiency of FIT triage. The lack of an apparent age-effect after taking into account FIT suggests that age-specific thresholds for FIT positivity would not improve test performance.
Strengths and weaknesses of the study
This is the largest cohort of primary care patients tested with FIT in the UK. The sample comprises patients reflecting true clinical practice which involves uptake of the DG30 guideline over time and clinical judgement. The study also comprises tests prior to and during the COVID-19 pandemic and suggests that the performance of FIT in primary care has remained stable throughout. Centralised FIT and blood testing at the the OUH Clinical Biochemistry Laboratory allowed for highly complete assessment of FIT and blood test values. We accessed the referral text to explore the performance of FIT in strata defined by GP-reported symptoms. The prevalence of and type of symptoms reported may have differed if we had accessed primary care records or asked patients to report their symptoms directly [23]. A 6-month follow-up period was used for the primary analysis to optimise the number of cancers included, but in sensitivity analyses that aligned with national guideline-setting, a 12-month follow-up showed similar results.
With respect to limitations, the gold standard would have been to have every patient undergo a colonoscopy after FIT. Due to the observational nature of this study, we instead used hospital-based records to determine outcomes after FIT. This may have resulted in some underestimation of disease. However, by linking multiple local data sources for patients tested in a single central laboratory in a clearly defined geographical catchment area we increased the likelihood that serious disease diagnosed during the study period was captured. It is plausible that some patients may have been lost to follow-up by moving out of area or by dying, but this is unlikely to have had a meaningful impact on our findings, as we used a short follow-up period and there is minimal patient movement between localities, particularly during investigation. An alternative approach would have been linkage to Public Health England’s National Cancer Registration and Analysis Service (NCRAS). While this may have provided a more complete accounting of outcomes, it would have restricted the timeliness of our analyses as cancer registry data is currently available only up until the end of 2018. Taking into account the follow-up period, this would have limited us to fewer than 4000 FITs for inclusion.
Another potential limitation is that the sample was restricted to individuals for whom blood test results were available within a 90-day window surrounding FIT, but this excluded only 10% of the sample. As no predictive model was identified that performed better than FIT alone, neither internal validation nor optimism correction were pursued.
Comparison with existing literature
Recent studies have reported FIT to be an effective tool to triage for “high-risk” patients referred for definitive investigation [9, 13]. Our findings contribute to a growing literature suggesting that FIT also performs well in the “lower risk” primary care setting [6, 7, 16, 24, 25]. This is the one of few studies to formally and systematically evaluate blood tests in addition to FIT in symptomatic patients, and one of few to analyse FIT supplemented with other variables. The f-Hb, age, and sex test score (FAST) was not superior to FIT alone in the primary care setting [12]. COLONPREDICT included FIT, age, sex, rectal bleeding, benign anorectal lesions, rectal mass, serum carcinoembryonic antigen, blood haemoglobin, colonoscopy in the last 10 years, and treatment with aspirin. COLONPREDICT was derived and validated in a higher-risk referred population [26] and at a threshold equivalent to approximately 90% sensitivity (f-Hb≥20 μg Hb/g faeces and COLONPREDICT score≥5.6) had a specificity of 78.7% compared to 69.6% in FIT alone [27].
A UK-based study of whether demographic, lifestyle (e.g., smoking, physical activity), or clinical factors (family history, symptoms) could add to the predictive value of FIT found that only family history of polyps showed a significant association once FIT was taken into account [28]. In the current study, family history was not retained in stepwise models; however, the indicator was based on referral notes whereas in the aforementioned study, patients were prospectively asked about family history.
Unanswered questions and future research
FIT is a sensitive and specific test and as such can serve as a valuable rule-in and rule-out test for patients presenting to primary care. However, it remains worthwhile to investigate strategies to further enhance the sensitivity and specificity of FIT and guide prioritisation of FIT-positive patients for immediate colonoscopy. Risk stratification tools that have been developed in the screening setting incorporating polygenic risk scores [29,30,31], urinary volatile organic compounds [10, 32], and circulating and/or faecal tumour DNA [33] could be explored to complement FIT for triage of primary care patients.
Currently, there is limited evidence to support the use of repeat FIT testing to select initially FIT-negative patients for referral or to reassure about non-referral. Based on exploratory analyses, 1113 patients in our study had second FITs also meeting inclusion criteria. In that group, there were 6 cancers, and no false negatives at a threshold of 2 or 10. Of the 1007 patients without cancer, forty-four (4.3%) patients had initially negative FITs followed by false-positive FITs at a threshold of 10, and 942 (93.5%) participants without cancer had two negative FITs. Further research is needed to inform the timing, interpretation, and utility of repeat FIT testing for triage in symptomatic patients attending primary care.
Both FIT and the “gold standard” colonoscopy result in false negatives [34]. In this study, no practical rules using blood tests or clinical indication to reduce false negatives were apparent. To reduce the likelihood of false FIT-negative results, future research may benefit from an agnostic approach to building the prediction model. For example, new predictive markers could be discovered by applying machine learning models to large, representative databases of electronic health records [35].
Conclusions
FIT alone is simple, easily implemented and effective to triage patients from primary care to colonoscopy. Particularly in light of the COVID pandemic and the suspected accumulation of undiagnosed cancers and unscreened adults [11], effective methods to triage low and/or “intermediate” risk patients to referral are more needed than ever [36]. Our results suggest however, that neither age, nor blood tests, nor clinical indication as recorded by the physician should be used to inform referral to colonoscopy after FIT. We found that the performance of FIT was maintained in patients with increasingly severe anaemia supporting that FIT can still be used in this group prior to referral for secondary care.
In the absence of alternate strategies to complement FIT, follow-up care of FIT-negative patients should focus on safety netting, including the re-evaluation of patients with persistent and unexplained symptoms within a pre-specified timeframe in primary care, and the possibility of urgent specialist assessment of FIT-negative patients for whom there is ongoing clinical concern [37,38,39].
Availability of data and materials
The datasets analysed during the current study were not collected for research purposes and are not publicly available due to anonymity reasons.
Abbreviations
- BRC:
-
Biomedical Research Center
- CRP:
-
C-reactive protein
- CV:
-
Coefficient of variation
- FAST:
-
Faecal haemoglobin Age and Sex Test
- FIT:
-
Faecal immunochemical test
- GP:
-
General practitioner
- MCH:
-
Mean cell haemoglobin
- MCV:
-
Mean cell volume
- NICE:
-
National Institute for health and Care Excellence
- NIHR:
-
National Institute for Health Research
- NPV:
-
Negative predictive value
- OUH:
-
Oxford University Hospitals
- PPV:
-
Positive predictive value
References
Thompson M, O’Leary D, Heath I, Wood LF, Ellis B, Flashman K, et al. Have large increases in fast track referrals improved bowel cancer outcomes in UK? BMJ. 2020;371:m3273.
NICE. Quantitative faecal immunochemical tests to guide referral for colorectal cancer in primary care [DG30]. 2017.
Westwood M, Ramos IC, Lang S, Luyendijk M, Zaim R, Stirk L, et al. Faecal immunochemical tests to triage patients with lower abdominal symptoms for suspected colorectal cancer referrals in primary care: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2017;21(33):1.
Mowat C, Digby J, Strachan JA, Wilson R, Carey FA, Fraser CG, et al. Faecal haemoglobin and faecal calprotectin as indicators of bowel disease in patients presenting to primary care with bowel symptoms. Gut. 2016;65(9):1463–9.
Nicholson BD, James T, East JE, Grimshaw D, Paddon M, Justice S, et al. Experience of adopting faecal immunochemical testing to meet the NICE colorectal cancer referral criteria for low-risk symptomatic primary care patients in Oxfordshire, UK. Frontline Gastroenterol. 2019;10(4):347–55.
van Melle M, Yep Manzano SIS, Wilson H, Hamilton W, Walter FM, Bailey SER. Faecal immunochemical test to triage patients with abdominal symptoms for suspected colorectal cancer in primary care: review of international use and guidelines. Fam Pract. 2020;37(5):606–15.
Bailey SER, Abel GA, Atkins A, Byford R, Davies SJ, Mays J, et al. Diagnostic performance of a faecal immunochemical test for patients with low-risk symptoms of colorectal cancer in primary care: an evaluation in the South West of England. Br J Cancer. 2021;124(7):1231–6.
Pin-Vieito N, Tejido-Sandoval C, de Vicente-Bielza N, Sánchez-Gómez C, Cubiella J. Faecal immunochemical tests safely enhance rational use of resources during the assessment of suspected symptomatic colorectal cancer in primary care: systematic review and meta-analysis. Gut. 2021;gutjnl-2021-324856.
D’Souza N, Georgiou Delisle T, Chen M, Benton S, Abulafi M, Group NFS. Faecal immunochemical test is superior to symptoms in predicting pathology in patients with suspected colorectal cancer symptoms referred on a 2WW pathway: a diagnostic accuracy study. Gut. 2021;70(6):1130–8.
Chandrapalan S, Bosch S, Cubiella J, Guardiola J, Kimani P, Mulder C, et al. Systematic review with meta-analysis: volatile organic compound analysis to improve faecal immunochemical testing in the detection of colorectal cancer. Aliment Pharmacol Ther. 2021;54(1):14–23.
Morris EJA, Goldacre R, Spata E, Mafham M, Finan PJ, Shelton J, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021;6(3):199–208.
Digby J, Strachan JA, Mowat C, Steele RJ, Fraser CG. Appraisal of the faecal haemoglobin, age and sex test (FAST) score in assessment of patients with lower bowel symptoms: an observational study. BMC Gastroenterol. 2019;19(1):1–7.
Bailey J, Ibrahim H, Bunce J, Chapman C, Morling J, Simpson J, et al. Quantitative FIT stratification is superior to NICE referral criteria NG12 in a high-risk colorectal cancer population. Tech Coloproctol. 2021;25(10):1151–4.
National Health Service. Clinical guide for triaging patients with lower gastrointestinal symptoms. 2020.
Bailey JA, Weller J, Chapman CJ, Ford A, Hardy K, Oliver S, et al. Faecal immunochemical testing and blood tests for prioritization of urgent colorectal cancer referrals in symptomatic patients: a 2-year evaluation. BJS Open. 2021;5(2):zraa056.
Nicholson BD, James T, Paddon M, Justice S, Oke JL, East JE, et al. Faecal immunochemical testing for adults with symptoms of colorectal cancer attending English primary care: a retrospective cohort study of 14 487 consecutive test requests. Aliment Pharmacol Ther. 2020;52(6):1031–41.
James T, Nicholson B, Marr R, Paddon M, East J, Justice S, et al. Faecal immunochemical testing (FIT): sources of result variation based on three years of routine testing of symptomatic patients in English primary care. Br J Biomed Sci. 2021;78(4):211–7.
Virdee PS, Marian IR, Mansouri A, Elhussein L, Kirtley S, Holt T, et al. The full blood count blood test for colorectal cancer detection: a systematic review, meta-analysis, and critical appraisal. Cancers. 2020;12(9):2348.
Wilkinson I, Wilkinson IB, Raine T, Wiles K, Goodhart A, Hall C, et al. Oxford handbook of clinical medicine. Oxford: Oxford University Press; 2017.
Austin PC, Steyerberg EW. Events per variable (EPV) and the relative performance of different strategies for estimating the out-of-sample validity of logistic regression models. Stat Methods Med Res. 2017;26(2):796–808.
Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17(8):857–72.
NICE. Suspected cancer: recognition and referral [NG12] 2015.
Hogberg C, Karling P, Rutegard J, Lilja M. Patient-reported and doctor-reported symptoms when faecal immunochemical tests are requested in primary care in the diagnosis of colorectal cancer and inflammatory bowel disease: a prospective study. BMC Fam Pract. 2020;21(1):129.
Strachan JA, Mowat C. The use of faecal haemoglobin in deciding which patients presenting to primary care require further investigation (and how quickly)–the FIT approach. EJIFCC. 2021;32(1):52.
McSorley ST, Digby J, Clyde D, Cruickshank N, Burton P, Barker L, et al. Yield of colorectal cancer at colonoscopy according to faecal haemoglobin concentration in symptomatic patients referred from primary care. Color Dis. 2021;23(7):1615–21.
Cubiella J, Vega P, Salve M, Díaz-Ondina M, Alves MT, Quintero E, et al. Development and external validation of a faecal immunochemical test-based prediction model for colorectal cancer detection in symptomatic patients. BMC Med. 2016;14(1):128.
Herrero JM, Vega P, Salve M, Bujanda L, Cubiella J. Symptom or faecal immunochemical test based referral criteria for colorectal cancer detection in symptomatic patients: a diagnostic tests study. BMC Gastroenterol. 2018;18(1):155.
Digby J, Steele RJ, Strachan JA, Mowat C, Anderson AS, McCann R, et al. Do other variables add value to assessment of the risk of colorectal disease using faecal immunochemical tests for haemoglobin? Ann Clin Biochem. 2019;56(4):472–9.
Frampton M, Law P, Litchfield K, Morris E, Kerr D, Turnbull C, et al. Implications of polygenic risk for personalised colorectal cancer screening. Ann Oncol. 2016;27(3):429–34.
Hull MA, Rees CJ, Sharp L, Koo S. A risk-stratified approach to colorectal cancer prevention and diagnosis. Nat Rev Gastroenterol Hepatol. 2020;17(12):773–80.
Melson JE, Imperiale TF, Itzkowitz SH, Llor X, Kochman ML, Grady WM, et al. AGA white paper: roadmap for the future of colorectal cancer screening in the United States. Clin Gastroenterol Hepatol. 2020;18(12):2667–78.e2.
Widlak MM, Neal M, Daulton E, Thomas CL, Tomkins C, Singh B, et al. Risk stratification of symptomatic patients suspected of colorectal cancer using faecal and urinary markers. Color Dis. 2018;20(12):O335–O42.
Bach S, Sluiter NR, Beagan JJ, Mekke JM, Ket JC, van Grieken NC, et al. Circulating tumor DNA analysis: clinical implications for colorectal cancer patients. A systematic review. JNCI Cancer Spectrum. 2019;3(3):pkz042.
Van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, Van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Off J Am Coll Gastroenterol. 2006;101(2):343–50.
Goldstein BA, Navar AM, Pencina MJ, Ioannidis J. Opportunities and challenges in developing risk prediction models with electronic health records data: a systematic review. J Am Med Inform Assoc. 2017;24(1):198–208.
Arasaradnam RP, Bhala N, Evans C, Greenaway J, Logan R, Penman I, et al. Faecal immunochemical testing in the COVID-19 era: balancing risk and costs. Lancet Gastroenterol Hepatol. 2020;5(8):717–9.
Cubiella J, Marzo-Castillejo M, Mascort-Roca JJ, Amador-Romero FJ, Bellas-Beceiro B, Clofent-Vilaplana J, et al. Clinical practice guideline. Diagnosis and prevention of colorectal cancer. 2018 update. Gastroenterol Hepatol. 2018;41(9):585–96.
Turvill J, Mellen S, Jeffery L, Bevan S, Keding A, Turnock D. Diagnostic accuracy of one or two faecal haemoglobin and calprotectin measurements in patients with suspected colorectal cancer. Scand J Gastroenterol. 2018;53(12):1526–34.
Nicholson BD, Mant D, Bankhead C. Can safety-netting improve cancer detection in patients with vague symptoms? BMJ. 2016;355:i5515.
Acknowledgements
This research uses data provided by patients and collected by the NHS as part of their care and support. We appreciate feedback from Patrick McGuire. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, or the Department of Health.
Funding
The work was supported by the Cancer Research UK (CR-UK) grant number C5255/A18085 through the Cancer Research UK Oxford Centre and Oxford Centre for Early Cancer Detection (OxCODE). James East and Jim Davies are funded by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre. BDN is an NIHR Academic Clinical Lecturer and is supported by the NIHR Oxford Medtech and In-Vitro Diagnostics Co-operative. JO is part funded by the NIHR Oxford Biomedical Research Centre, Oxford University Hospitals NHS Foundation Trust. None of the funding sources had any involvement in the conduct of study or preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
DRW was responsible for conceptualisation, data curation, formal analysis, investigation, methodology, visualisation, and writing. BS was responsible for data curation, methodology, resources, reviewing, and editing. JO was responsible for conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, supervision, and writing—review and editing. AT was responsible for formal analysis, methodology, visualisation, reviewing, and editing. TJ was responsible for data curation, methodology, project administration, reviewing, and editing. EM was responsible for supervision, reviewing, and editing. JD was responsible for data curation, reviewing, and editing. SH was responsible for data curation, reviewing, and editing. JE was responsible for conceptualisation, funding acquisition, supervision, reviewing, and editing. BDN was responsible for conceptualisation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, writing, review, and editing. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted as a service evaluation with registration, review, and approval process within the OUH Datix governance structure (Service evaluation registration identifier: CSS-BIO-3-4730). As service evaluation, this work is not subject to the Department of Health’s UK Policy Framework for Health and Social Care Research (2017). The Sponsorship and Ethics Lead within the Research Governance, Ethics and Assurance Team, in the Research Support Office at the University of Oxford has confirmed that it requires neither sponsorship nor research ethics review.
Consent for publication
Not applicable
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
[Frequency of abnormal blood test results by outcome and FIT score]. Table S2. [Distribution of test results within study population by approach]. Table S3. [Model parameters for models resulting from backward stepwise regression]. Table S4. [Characteristics of patients receiving symptomatic FIT tests by date of FIT relative to COVID-19 pandemic]. Table S5. [Test performance comparing pre and post COVID19]. Table S6. [Test performance by demographic and clinical subgroups]. Table S7. [Test performance by subgroups defined by increasingly severe anaemia]. Table S8. [Test performance comparing patients who meet the DG30 criteria]. Table S9. [Test performance with 12 months of follow-up, FIT alone and FIT-blood test pairs]. Table S10. [Test performance with 12 months of follow-up, FIT alone and model-based approach.]. Table S11. [Predictive performance of abnormal blood tests among patients who are FIT negative].
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Withrow, D.R., Shine, B., Oke, J. et al. Combining faecal immunochemical testing with blood test results for colorectal cancer risk stratification: a consecutive cohort of 16,604 patients presenting to primary care. BMC Med 20, 116 (2022). https://doi.org/10.1186/s12916-022-02272-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-022-02272-w