Abstract
Background
ROS1-rearranged lung cancers benefit from first-line crizotinib therapy; however, clinical and molecular factors that could affect crizotinib efficacy in ROS1-rearranged lung cancers are not yet well-elucidated. Our retrospective study aimed to compare the efficacy of chemotherapy and crizotinib in the first-line treatment of ROS1-rearranged advanced lung cancer and evaluate various clinical and molecular factors that might impact crizotinib efficacy in real-world practice.
Methods
Treatment responses, survival outcomes, and patterns of disease progression were analyzed for 235 patients with locally advanced to advanced disease who received first-line chemotherapy (n = 67) or crizotinib (n = 168).
Results
The overall response rate was 85.7% (144/168) for first-line crizotinib and 41.8% (28/67) for chemotherapy. Patients treated with first-line crizotinib (n = 168) had significantly longer median progression-free survival (PFS) than chemotherapy (n = 67) (18.0 months vs. 7.0 months, p < 0.001). Patients harboring single CD74-ROS1 (n = 90) had significantly shorter median PFS with crizotinib than those harboring non-CD74 ROS1 fusions (n = 69) (17.0 months vs. 21.0 months; p = 0.008). Patients with baseline brain metastasis (n = 45) had a significantly shorter PFS on first-line crizotinib than those without brain metastasis (n = 123) (16.0 months vs. 22.0 months; p = 0.03). At progression, intracranial-only progression (n = 40), with or without baseline CNS metastasis, was associated with longer median PFS than those with extracranial-only progression (n = 64) (19.0 months vs. 13.0 months, p < 0.001). TP53 mutations were the most common concomitant mutation, detected in 13.1% (7/54) of patients with CD74-ROS1 fusions, and 18.8% (6/32) with non-CD74 ROS1 fusions. Patients with concomitant TP53 mutations (n=13) had significantly shorter PFS than those who had wild-type TP53 (n = 81) (6.5 months vs. 21.0 months; p < 0.001). PFS was significantly shorter for the patients who harbored concomitant driver mutations (n = 9) (11.0 months vs 24.0 months; p = 0.0167) or concomitant tumor suppressor genes (i.e., TP53, RB1, or PTEN) (n = 25) (9.5 months vs 24.0 months; p < 0.001) as compared to patients without concomitant mutations (n = 58).
Conclusion
Our results demonstrate that baseline brain metastatic status and various molecular factors could contribute to distinct clinical outcomes from first-line crizotinib therapy of patients with ROS1-rearranged lung cancer.
Clinical trials registration
CORE, NCT03646994
Similar content being viewed by others
Background
Genomic rearrangements involving ROS proto-oncogene-1 (ROS1) are actionable targets in the treatment of non-small-cell lung cancer (NSCLC) [1]. The overall prevalence of ROS1 fusions is reported to be 2% in NSCLC and up to 3.3% in lung adenocarcinoma [1,2,3,4]. ROS1, located at the long arm of chromosome 6q22, encodes one of the receptor tyrosine kinases of the insulin receptor family; however, its exact activating ligand remains unidentified and hence is considered an orphan receptor [4, 5]. Since the amino acid sequence of the kinase domains of ROS1 and ALK are highly homologous, selective inhibitors of ALK, including crizotinib, have shown anti-tumor activity in vitro and have been explored clinically in the treatment of patients with ROS1-rearranged tumors [5,6,7,8,9,10,11,12,13]. Crizotinib has been approved for use in ROS1-rearranged NSCLC based on the PROFILE 1001 study, which observed an objective response rate (ORR) of 72%, median progression-free survival (PFS) of 19.2 months, and median overall survival of 51.4 months among the 53 patients with ROS1-rearranged NSCLC included in the expansion cohort [8, 14]. Meanwhile, the largest phase II study conducted to date on crizotinib response of ROS1-positive NSCLC demonstrated an ORR of 71.7% with a median PFS of 15.9 months among 127 East Asian patients [13]. Given the rarity of ROS1 fusions, the effect of ROS1 fusion variants and other clinical and molecular factors on the efficacy of crizotinib is not well-elucidated. So far, the real-world studies describing the efficacy of crizotinib in Asian patients with ROS1-rearranged NSCLC mostly involved smaller cohorts.
This retrospective cohort study aimed to explore the efficacy of crizotinib as a first-line treatment for advanced NSCLC with various ROS1 rearrangements. We also investigated clinical and molecular factors that could impact the clinical outcomes of patients with locally advanced to advanced ROS1-rearranged NSCLC from first-line crizotinib therapy.
Patients
Included patients
We retrospectively screened 21,747 consecutive treatment-naïve patients who were diagnosed with lung cancer from August 1, 2018, to March 31, 2020, and submitted samples for molecular detection of ROS1 rearrangements, including next-generation sequencing (NGS), fluorescence in situ hybridization (FISH), and amplification refractory mutation system (ARMS) at various hospitals in Hunan, Hubei, Guangdong, and Zhejiang Provinces in China. All the patients who were analyzed for clinical outcomes from first-line crizotinib met the following criteria: (1) pathologically-confirmed NSCLC, (2) locally advanced/unresectable disease to advanced/metastatic disease; (3) ROS1 rearrangements identified by NGS, and (4) treatment with crizotinib in the first-line setting. Written informed consent was obtained from all the patients for the use of their data for research purposes. All procedures in our study were performed following the ethical standards of the institutional and national research committees, and the Declaration of Helsinki as revised in 2013. Approval was obtained from the Hunan Cancer Hospital Institutional Review Board Committee (approval number: 2017YYQ-SSB-026). This study was also registered as a clinical trial (CORE, NCT03646994).
NGS
Patient samples were submitted for NGS-based analysis to Burning Rock Biotech, a College of American Pathologists-accredited, Clinical Laboratory Improvement Amendments -certified clinical laboratory. Briefly, DNA isolated from the tissue biopsy, blood, or pleural effusion samples obtained from all the patients were processed accordingly for NGS using commercially available panels targeting various cancer-related genes and sequenced on a Nextseq 500 (Illumina, CA, USA) with paired-end reads with a target sequencing depth of 1000X for tissue samples and 10,000X for liquid biopsy samples using optimized protocols [15]. All the gene capture panels used in our study, including 8, 56, 108, 168, and 295 cancer-related genes, interrogated whole exons and critical introns for the 8 classic NSCLC oncogenic drivers, which includes EGFR, ALK, BRAF, ERBB2, KRAS, MET, RET, and ROS1. To understand the impact of concomitant mutations, including TP53, other tumor suppressor genes, and oncogenic driver genes, on crizotinib outcomes, we selected the patient samples that were assayed using 168-gene or 295-gene panels (n = 94). We only analyzed the 168 genes common between the 2 panels. Table S1 lists the genes included in the 168 gene panel. The sequencing analyses were performed using optimized bioinformatics pipelines for somatic variant calling that involved accurate identification of base substitutions, small insertions-deletions, copy number variations, and genomic rearrangements as described previously [15].
Non-reciprocal/reciprocal translocations are defined by the simultaneous detection of at least one ROS1 fusion that contains the tyrosine kinase domain and another ROS1 fusion involving the 5′-region of ROS1 fused with other gene partners aside from the gene partner fused to the ROS1 tyrosine kinase domain, as previously described with ALK fusions [16].
Evaluation of treatment efficacy
Crizotinib was orally administered at a dose of 250 mg twice daily. Chemotherapy with either pemetrexed-carboplatin regimen or docetaxel-cisplatin regimen was administered intravenously. The dose for pemetrexed was 500 mg per square meter of body-surface area (m2), plus carboplatin at a dose of target area under the curve of 5 to 6 mg per milliliter per minute. The dose for docetaxel was 75 mg/m2 and 75 mg/m2 for cisplatin. The treatment regimens were administered until progressive disease (PD) or unacceptable toxicity. Patients who experienced toxicity were managed by dose reduction or discontinuation as decided by their physicians. The best responses were assessed by the investigators according to the Response Evaluation Criteria in Solid Tumors version 1.1. For patients treated with crizotinib, as local law for drug purchase, all patients were required to undergo radiologic imaging evaluation including chest computed tomography (CT) scanning and brain magnetic resonance imaging (MRI) every 2 cycles. For patients treated with chemotherapy, as they were all treated in hospital, all patients were required to undergo chest radiologic imaging evaluation including chest CT and brain MRI every 2 cycles. The overall response rate (ORR) was calculated as the proportion of patients with complete response (CR) or partial response (PR). The disease control rate (DCR) was calculated as the proportion of patients with CR, PR, and stable disease (SD). Progression-free survival (PFS) was measured from the start of crizotinib administration until the date of PD or death from any causes. Each image was independently evaluated by two radiologists. The data cutoff date was December 31, 2020. The median follow-up duration was 28 (range: 2–59) months.
Statistical analysis
Continuous variables were summarized as means and standard deviations or medians with range and compared using unpaired t test or Wilcoxon signed-rank test. Categorical variables were summarized as frequencies with percentages and compared using Chi-squared or Fisher’s exact test, as appropriate. Kaplan-Meier analysis was used to estimate the survival functions and log-rank test to determine the difference in survival outcomes between groups. The Cox proportional hazards model was used for multivariate survival analysis. Variables with a p value < 0.2 in the univariate analysis were included in the multivariate analysis. Schoenfeld residuals were used to check the proportional hazards assumption. All tests were two-sided, and p value < 0.05 was considered statistically significant. All statistical analyses were performed with R (version 3.3.3, the R Foundation for Statistical Computing, Vienna, Austria) and RStudio (version 1.1.383).
Results
Patient characteristics and distribution of ROS1 fusions identified through NGS
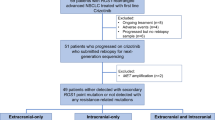
Figure 1 summarizes our study design. Among the 21,747 consecutive treatment-naïve patients diagnosed with various stages of lung cancer who submitted samples for ROS1 detection, 447 were positive for ROS1 rearrangements, revealing an overall prevalence rate of 2.1%. A majority of the ROS1 rearrangements were identified using NGS (59.1%; n = 264), while 23.5% (n = 105) were identified by FISH, and 17.4% (n=78) were identified by ARMS. Of the 264 patients who were identified as ROS1 positive using NGS analysis, a majority (95.5%; n = 252) submitted tissue biopsy samples. The remaining 2.7% (n = 7) of the patients submitted plasma samples, and 1.8% (n = 5) submitted pleural effusion samples. Unfortunately, no patient submitted samples for all three molecular assays or multiple sample types to enable further concordance analyses among the detection methods or sample types.
Study design schematic. Flow chart illustrating the study design. A total of 21,747 treatment-naïve patients diagnosed with lung cancer were retrospectively screened for ROS1 fusion variants. Among them, 447 were detected with ROS1 rearrangements using various methods including NGS (n = 264), FISH (n = 105), and ARMS (n = 78). Clinical outcomes were further analyzed for the 235 patients with ROS1-rearranged locally advanced to advanced lung cancer who received either chemotherapy (n = 67) or crizotinib (n = 168) as first-line therapy
Among the 235 patients with stage IIIB-IV disease, a majority was female (63%; n = 147), with a median age of 52 years (range: 25–79 years). Except for 1 patient having squamous cell carcinoma, all had adenocarcinoma (99.0%; n = 234). Of these 235 patients, 168 received crizotinib and 67 received platinum-based doublet chemotherapy regimen as first-line therapy. Baseline clinical characteristics including local treatment strategies were statistically similar among the subgroups (Table 1).
We further explored the various ROS1 fusion variants and gene partners among the 235 patients with NGS data who received first-line therapy. A majority of the patients (93.6%, 220/235) were detected with only a single ROS1 fusion partner, with CD74-ROS1 as the most common (59.1%, 130/220), followed by SDC4-ROS1 (13.2%, 29/220), and EZR-ROS1 (11.4%, 25/220) (Table S2, Fig. 2A). Five previously unreported ROS1 fusion partners were identified from our cohort, including MYH9-ROS1 (n = 2), AQP4-ROS1 (n = 1), CTNND2-ROS1 (n = 1), PHACTR3-ROS1 (n = 1), and PTM-ROS1 (n = 1). Six percent (6.4%, 15/235) of the patients with ROS1-rearranged NSCLCs were detected with more than 1 genomic rearrangement involving ROS1, of which at least 1 of the rearrangements retained the kinase domain of ROS1, while the other ROS1 fusion did not retain the kinase domain, which was referred to as non-reciprocal/reciprocal translocation. Among them, a majority had CD74-ROS1 (47.1%; n = 8) as the ROS1 fusion which retained the kinase domain. Interestingly, 1 patient was detected with 3 fusions (CD74-ROS1, SDC4-ROS1, and SLC34A2-ROS1), which all retained the kinase domain. Table S3 summarizes the detailed breakpoint information for the non-reciprocal/reciprocal ROS1 translocations detected from our cohort.
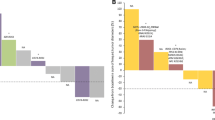
ROS1-rearranged NSCLCs had better objective response rate (ORR), disease control rate (DCR), and progression-free survival (PFS) with first-line crizotinib therapy than chemotherapy. A Distribution of various ROS1 fusions detected using NGS-based method in 235 patients with locally advanced to advanced disease who received first-line therapy. B Treatment outcomes of patients with ROS1-rearranged NSCLCs who received either chemotherapy (red) or crizotinib therapy (green) in the first-line setting. C, D Kaplan-Meier survival curves illustrating the significantly better PFS for patients with ROS1-rearranged NSCLC (D) who received crizotinib (green) as compared to those who received chemotherapy (red) in the first-line setting; and (E) who received crizotinib and had non-CD74 ROS1 fusions (green) as compared to those with single CD74-ROS1 (red). The risk table below summarizes the number of patients included per time point
Comparison between chemotherapy and crizotinib as first-line therapy
Clinical outcomes were analyzed for the 235 patients with advanced or locally advanced ROS1-rearranged NSCLCs who received first-line therapy of either chemotherapy (n = 67; pemetrexed and carboplatin regimen (97%; n = 65), docetaxel and cisplatin regimen (n = 2)) or crizotinib (n = 168). As compared to patients who received chemotherapy (n = 67), patients who received crizotinib (n = 168) had significantly better ORR (85.7% (n = 144) vs 44% (n = 28), p = 0.003; Fig. 2B) and significantly longer median PFS (18.0 months vs. 7.0 months, p < 0.001, Fig. 2C).
Impact of ROS1 fusion types on crizotinib efficacy
Next, we explored the clinical impact of ROS1 fusion variants among the 168 patients with NGS data who received first-line crizotinib. Baseline clinicopathologic characteristics were similar for the patients regardless of ROS1 fusion (Table 1).
PFS was significantly shorter for patients with single CD74-ROS1 fusion (n = 90) than those with single non-CD74 ROS1 fusions (n = 69) (17.0 months vs 21.0 months; p = 0.008; Fig. 2D). PFS was comparable among patients with single CD74-ROS1 fusions (n = 90) and those with single SDC4-ROS1 (n = 23; 16.0 months [95% confidence intervals (CI): 14.2–17.7 months]; p = 0.175), or single EZR-ROS1 (n=21; 19.0 months [95% CI: 12.7–25.2 months]; p = 0.07), but was significantly longer for patients with uncommon non-CD74 ROS1 fusions (n = 25; 22.0 months [95% CI: 14.5–29.5 months]; p = 0.02) (Figure S1A). The ORR (88.9% vs 82.6%; p = 0.92) and DCR (96.7% vs 97.1%; p = 0.96) was similar for patients with CD74-ROS1 and non-CD74 ROS1 fusions (Table S4). With first-line crizotinib therapy, the ORR was 91.3% for patients with SDC4-ROS1 (n = 23), 85.7% for EZR-ROS1 (n = 21), 91.7% for TPM3-ROS1 (n = 12), and 88% for other uncommon non-CD74 ROS1, including SLC34A2-ROS1 (n = 3), LRIG3-ROS1 (n = 3), MYH9-ROS1 (n = 1), CCDC6-ROS1 (n = 1), AQP4-ROS1 (n = 1), CTNND2-ROS1 (n = 1), PHACTR3-ROS1 (n = 1), GOPC-ROS1 (n = 1), and PTM-ROS1 (n = 1), which were grouped together due to small numbers. As compared to patients with single ROS1 fusion (both CD74-ROS1 and non-CD74 ROS1) (n = 159), patients with non-reciprocal/reciprocal ROS1 translocations (n = 9) had comparable ORR (77.8% vs 86.2%; p = 0.951; Table S3), DCR (100.0% vs 96.9%; p = 1.0; Table S4), and PFS (not reached vs 18.0 months; p = 0.116; Figure S1B) with crizotinib. Baseline clinicopathologic characteristics were similar for patients with single ROS1 fusion and non-reciprocal/reciprocal ROS1 translocations (Table S5). Table S6 lists the treatment outcomes on first-line crizotinib therapy of the 159 patients with single ROS1 fusion grouped according to ROS1 fusion partners. Table S7 and S8 list the detailed clinicopathologic features and clinical outcomes of the 13 patients with uncommon non-CD74 ROS1 fusions and the 15 patients with non-reciprocal/reciprocal ROS1 translocations, respectively.
Impact of various molecular factors on crizotinib efficacy in ROS1-rearranged NSCLCs
Numerous reports have implicated the presence of other concomitant mutations in various genes including TP53 in the poor response of ALK-rearranged NSCLC to crizotinib therapy [17, 18]; however, very limited reports have explored the clinical impact of other concomitant mutations on crizotinib therapy of ROS1-rearranged NSCLC. We then analyzed the genomic profile of 94 patients with ROS1 fusions whose samples were sequenced using a panel with at least 168 genes and evaluable for survival outcomes on first-line crizotinib to investigate the correlation between the presence of certain concomitant mutations at baseline and crizotinib efficacy. For this analysis, concurrent mutations in only the 168 genes common across the gene panels used for NGS were analyzed. Among the 54 evaluable patients with CD74-ROS1 fusions, 21 patients (38.9%) were detected with other concomitant mutations, with TP53 (13.1%, 7/54) as the most common co-occurring mutation. Other co-occurring mutations in classic NSCLC oncogenic drivers, including EGFR L858R (n=1), MET amplification (n = 1), and KRAS G12D (n = 4), were detected from tissue samples of 6 patients. Meanwhile, among the 32 patients with non-CD74 ROS1 fusions, 14 patients (43.7%) had other concomitant mutations, with TP53 (18.8%, 6/32) as the most common. Concurrent mutations in classic NSCLC oncogenic drivers, including MET amplification (n = 3), were detected from tissue samples of 3 patients with non-CD74 ROS1 fusion. The distribution of concurrent mutations detected among patients with CD74-ROS1 fusions (n = 54) was not statistically different from those with non-CD74 ROS1 fusions (n = 32) (38.9% vs. 43.7%; p = 0.774; Table S9).
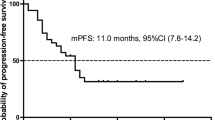
In general, as compared to patients with no co-occurring mutations (n = 58), PFS was significantly shorter for those who harbored concomitant driver mutations (n = 9) (11.0 months vs 24.0 months; p = 0.0167; Fig. 3A) or concomitant tumor suppressor genes (i.e., TP53, RB1, or PTEN) (n = 25) (9.5 months vs 24.0 months; p < 0.001; Fig. 3A). Patients with concomitant TP53 mutations (n = 13) had significantly shorter PFS than those who had wild-type TP53 (n = 81) (6.5 months vs. 21.0 months; p < 0.001; Fig. 3B). Multivariate analysis consistently demonstrate the impact of harboring concomitant TP53 mutations (p = 0.028; hazard ratio: 0.41, 95% CI: 0.19–0.91) and harboring any concomitant mutations (p = 0.048; HR = 0.537, 95% CI: 0.290–0.995; Table S10) on PFS. These data suggest that the presence of concomitant mutations contributes to poor survival outcomes with first-line crizotinib therapy. Table S11 summarizes the clinical information of the 9 patients with concomitant driver mutations.
The presence of concomitant mutations is associated with poor prognosis. Kaplan-Meier survival curves illustrating the PFS for (A) patients with only ROS1 fusions (green), for those with concurrent driver mutations (red), and with concomitant mutations in tumor suppressor genes (blue), and (B) patients with (red) and without (green) concomitant TP53 mutations. The risk table below summarizes the number of patients included per time point
Impact of baseline brain metastasis on crizotinib and chemotherapy efficacy
Since a substantial number of patients with advanced-stage NSCLC present with brain metastasis at initial presentation and that crizotinib is known to have limited penetrability to the blood-brain barrier, we assessed the clinical impact of baseline brain metastasis on crizotinib and chemotherapy efficacy. Among the 235 patients with advanced or locally advanced ROS1-rearranged NSCLCs, brain metastasis at presentation was detected from 58 patients (24.6%), which were detected using either MRI or CT scanning. Of them, 10 patients received whole-brain radiotherapy (WBRT) and 9 patients received stereotactic body radiotherapy (SBRT) for the management of their brain metastasis (Table 1). As compared to patients without brain metastasis at baseline, patients with baseline brain metastasis had a trend of shorter median PFS on first-line chemotherapy (4.0 months (n = 16) vs 7.0 months (n = 51); p = 0.09; Fig. 4A) and significantly shorter PFS on first-line crizotinib (16.0 months (n = 45) vs. 22.0 months (n = 123); p = 0.03; Fig. 4B). However, patients with brain metastasis at baseline had significantly longer median PFS with crizotinib therapy than with chemotherapy (16.0 months (n = 45) vs. 4.0 months (n = 16); p < 0.0001). The ORR (77.8% vs. 87.8%; p = 0.642) and DCR (95.6% vs. 97.5%; p = 0.933) with crizotinib therapy were comparable between patients with or without brain metastasis at baseline (Table S4). No difference in the presence of baseline brain metastasis was found among patients with CD74-ROS1 and non-CD74 ROS1 fusions (25.6% (23/90) vs. 27.5% (19/69); p = 0.830; Table 1). These findings indicate that despite the presence of brain metastasis at presentation, patients with ROS1-rearranged NSCLC still benefit more from crizotinib than chemotherapy.
Patients with ROS1-rearranged NSCLC who had baseline brain metastasis still benefit from first-line crizotinib than chemotherapy. Kaplan-Meier survival curves illustrating the PFS for patients with ROS1-rearranged NSCLC who had non-brain metastasis (green) and brain metastasis (red) at baseline and received chemotherapy (A) and crizotinib (B) as first-line therapy. C Plot comparing the cumulative incidence of CNS progression in patients receiving crizotinib (green) and chemotherapy (red). D–E Crizotinib-treated patients with ROS1-rearranged NSCLC who experienced CNS only progression had a better prognosis than those who experienced non-CNS progression. D-E. Kaplan-Meier survival curves comparing the PFS of crizotinib-treated patients with ROS1-rearranged NSCLC who had non-CNS only progression (red), CNS only progression (green) and the whole cohort (blue) (D); E crizotinib-treated patients without baseline CNS metastasis who had CNS only progression (green) and non-CNS only progression (pink) and patients with baseline CNS metastasis who had CNS only progression (blue) and non-CNS only progression (red). The risk table below summarizes the number of patients included per time point
Central nervous system (CNS)-related progression is associated with better prognosis
We further investigated the pattern of disease progression and the prognostic role of CNS progression among the patients whose disease progressed from either chemotherapy or crizotinib therapy. Although the frequency of CNS progression was similar between the two treatment groups (crizotinib 28.6% (48/168) vs. chemotherapy 28.4% (19/67)), the median time of the appearance of CNS progression was significantly slower on crizotinib therapy than on chemotherapy (30.0 months vs 22.0 months; p < 0.001; Fig. 4C). Of the 168 patients who received crizotinib, disease progression was observed in 112 patients and the treatment of 56 patients was still ongoing as of the data cut-off. Of the relapsed patients, 35.7% (n = 40) patients had intracranial-only progression, 7.1% (n = 8) patients were simultaneously detected with intracranial and extracranial progression, while 57.1% (n = 64) patients had extracranial-only progression, including the enlargement of the primary lung lesion, and development of other extracranial metastatic lesions. Patients with both intracranial and extracranial progression (n = 8) were omitted from further analysis but their clinical details were summarized in Table S12. Patients who had intracranial-only progression (n = 40) achieved significantly longer PFS than those with extracranial-only progression (n = 64) (23.0 months vs. 13.0 months, p < 0.001; Fig. 4D). The baseline clinical characteristics were similar between the patients with intracranial only and extracranial only progression on crizotinib therapy (Table S13).
We further compared the survival outcomes of the patients based on the pattern of disease progression and the presence of baseline brain metastasis. Of the 40 crizotinib-treated patients who experienced intracranial-only progression, 16 patients had baseline CNS metastasis. Meanwhile, of the 64 crizotinib-treated patients with extracranial-only progression, 16 patients had baseline CNS metastasis (Table S13). The PFS were statistically different among the patients with or without baseline CNS metastasis who progressed with intracranial and extracranial metastasis (p = 0.007; Fig. 4E). Patients with baseline CNS metastasis who experienced intracranial-only progression with crizotinib therapy (n = 16) had significantly longer median PFS than those who experienced extracranial-only progression (n = 18) (17.0 months vs 8.0 months; p = 0.04; hazard ratio: 0.59, 95%CI: 0.23–0.95; Fig. 4E). Consistently, patients without baseline CNS metastasis who experienced intracranial-only progression with crizotinib therapy (n = 24) had longer median PFS than those who experienced extracranial-only progression (n = 46) (26.5 months vs 13.5 months; p < 0.001; hazard ratio: 0.51, 95%CI: 0.31–0.83; Fig. 4E). We found no difference in the pattern of progression with first-line crizotinib therapy among patients with CD74-ROS1 and non-CD74 ROS1 fusions (intracranial progression 41.0% vs. 46.8%; extracranial progression 59.0% vs. 53.2%; p = 0.679; Table 1). And there was also no difference for the local treatment (Table 1). Taken together, these data indicate that patients with CNS progression can still benefit from crizotinib therapy.
Discussion
The current guidelines of the National Comprehensive Cancer Network recommend the use of ROS1 targeted inhibitors such as crizotinib and entrectinib as the preferred first-line treatment for ROS1 rearrangement-positive NSCLC [19]. However, in real-world clinical practice, the use of targeted inhibitors can be restricted by the patient’s socio-economic status for molecular testing services and access to various treatment modalities. Hence, we aimed to investigate the efficacy of crizotinib and chemotherapy in patients with ROS1-rearranged NSCLC to gain a better understanding of the advantages of crizotinib therapy for this subset of patients in the real-world setting. In our retrospective study, we screened the molecular data of a large cohort of lung cancer patients from various hospitals in 4 provinces of China and revealed a prevalence of 2.1% for ROS1 rearrangements among the Chinese patients with lung cancer. The prevalence we have derived from our cohort was consistent with the reported prevalence of 2.2% in another smaller cohort of Chinese patients with lung cancer [20, 21]. To the best of our knowledge, our study included the largest sample obtained from multiple centers, which reflects the actual prevalence of ROS1 rearrangements in our population and could help identify effective therapeutic management of ROS1-rearranged NSCLCs.
Consistent with previous observations [5], chromosomal rearrangements involving ROS1 in our cohort were mostly identified from younger patients with a median of 52 years old, females (63–66%), never smokers (75–76%), and with adenocarcinoma histology (97–98%). Our study has provided real-world clinical evidence on the efficacy of crizotinib in the first-line setting as reported in numerous clinical trials and other studies [8, 13, 14, 21,22,23]. The clinical outcomes we have observed from the 168 crizotinib-treated patients were consistent with another study that reported the better ORR, DCR, and PFS with first-line crizotinib as compared to chemotherapy for ROS1-rearranged NSCLC (ORR 80.0% vs 40.8%; DCR 90.0% vs. 71.4%; PFS 9.8 months vs 6.0 months) [21, 24]. Moreover, our results that demonstrated better survival outcomes with first-line crizotinib for patients with non-CD74 ROS1 fusions than those who harbor CD74-ROS1 fusions (21.0 months vs 17.0 months) were consistent with a prior report that demonstrated a PFS of 17.6 months and 12.6 months, respectively [12]. Meanwhile, another study reported an opposite trend of longer PFS with crizotinib for patients with CD74-ROS1 than non-CD74-ROS1 (20.1 months vs. 12.0 months) [24], while no difference in PFS with chemotherapy was observed between CD74-ROS1 and non-CD74-ROS1 (8.6 months vs. 4.3 months) [24]. Since some of the ROS1 fusion partners are not as common as CD74, survival outcome data for patients with these fusion partners remains limited. Our results demonstrated a median PFS of 16.0 months for patients with SDC4-ROS1, 19.0 months each for patients with EZR-ROS1 and TPM3-ROS1, and 22.0 months for patients with other uncommon non-CD74 ROS1 fusion partners. Our study is the first to provide data on the treatment and survival outcomes on first-line crizotinib for patients harboring various novel/uncommon non-CD74 ROS1 fusion partners as detailed in Table S7.
TP53 is one of the most frequent concomitant mutations in NSCLC, and has been associated with poor prognosis of not only patients with EGFR-mutant NSCLC treated with EGFR-TKI but also patients with ALK-rearranged NSCLC treated with crizotinib or chemotherapy [17, 18, 25, 26]. TP53 is a tumor suppressor gene and plays a critical role in regulating cell proliferation, and its loss-of-function promotes uncontrolled cell proliferation, tumor growth, and drug resistance [27,28,29]. Moreover, the detection of various concomitant mutations represents the molecular heterogeneity of the tumor, which could contribute to variable inhibitor response [30]. Our findings demonstrate poorer survival outcomes of patients with ROS1-rearranged NSCLC who harbored concomitant mutations in TP53, other tumor suppressor genes such as PTEN and RB1, and other oncogenic drivers such as EGFR, MET amplification, and KRAS. Our findings were consistent with the subgroup analysis of EUCROSS study on the shorter PFS of patients with ROS1-rearranged lung cancers with concomitant TP53 mutations, treated with crizotinib than their wild-type counterpart [31].
Our study is limited by its retrospective nature; hence, some data are not available for analysis. Since the cohort with survival outcomes was based on the patients who submitted samples for NGS, inherent sampling bias might exist including the economic capability of the patients to submit samples for NGS and the decision on receiving chemotherapy or targeted therapy, which could limit our conclusion. Our study only analyzed the DNA-based NGS analysis of ROS1 fusion variants and does not include in vitro functional assays or RNA-based analysis of patient samples to confirm the transcription of novel ROS1 fusions or reciprocal/non-reciprocal ROS1 translocations that we have identified from our cohort. Further in vitro experiments are necessary to provide functional evidence for these ROS1 fusions.
Conclusions
Our study provided real-world clinical evidence of the distinct efficacy of crizotinib among NSCLCs with various ROS1 fusion partners including some novel non-CD74 ROS1 fusions. Our findings demonstrate that as compared to chemotherapy, crizotinib is a better first-line therapy for patients with ROS1-rearranged NSCLC, with or without brain metastasis at presentation. Moreover, concurrent mutations may contribute to the poor clinical outcomes with crizotinib; hence, a better understanding of the patient’s mutation landscape is necessary for optimal treatment planning. Our study contributes to the understanding that baseline clinical and molecular factors could impact the survival outcomes of patients with locally advanced to advanced ROS1-rearranged NSCLC treated with first-line crizotinib.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ARMS:
-
Amplification refractory mutation system
- CI:
-
Confidence intervals
- CNS:
-
Central nervous system
- CR:
-
Complete response
- CT:
-
Computed tomography
- DCR:
-
Disease control rate
- EGFR:
-
Epidermal growth factor receptor
- FISH:
-
Fluorescence in situ hybridization
- HR:
-
Hazard ratio
- MRI:
-
Magnetic resonance imaging
- NGS:
-
Next-generation sequencing
- NSCLC:
-
Non-small-cell lung cancer
- ORR:
-
objective response rate
- PFS:
-
Progression-free survival
- PD:
-
Progressive disease
- PR:
-
Partial response
- ROS1:
-
ROS proto-oncogene-1
- SD:
-
Stable disease
- TKI:
-
Tyrosine kinase inhibitor
- WBRT:
-
Whole-brain radiotherapy
References
Bergethon K, Shaw AT, Ou SH, Katayama R, Lovly CM, McDonald NT, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012;30(8):863–70.
Davies KD, Le AT, Theodoro MF, Skokan MC, Aisner DL, Berge EM, et al. Identifying and targeting ROS1 gene fusions in non-small cell lung cancer. Clin Cancer Res. 2012;18(17):4570–9.
Rimkunas VM, Crosby KE, Li D, Hu Y, Kelly ME, Gu TL, et al. Analysis of receptor tyrosine kinase ROS1-positive tumors in non-small cell lung cancer: identification of a FIG-ROS1 fusion. Clin Cancer Res. 2012;18(16):4449–57.
Rikova K, Guo A, Zeng Q, Possemato A, Yu J, Haack H, et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell. 2007;131(6):1190–203.
Ou SH, Tan J, Yen Y, Soo RA. ROS1 as a 'druggable' receptor tyrosine kinase: lessons learned from inhibiting the ALK pathway. Expert Rev Anticancer Ther. 2012;12(4):447–56.
Gu TL, Deng X, Huang F, Tucker M, Crosby K, Rimkunas V, et al. Survey of tyrosine kinase signaling reveals ROS kinase fusions in human cholangiocarcinoma. PLoS One. 2011;6(1):e15640.
Yasuda H, de Figueiredo-Pontes LL, Kobayashi S, Costa DB. Preclinical rationale for use of the clinically available multitargeted tyrosine kinase inhibitor crizotinib in ROS1-translocated lung cancer. J Thorac Oncol. 2012;7(7):1086–90.
Shaw AT, Ou SH, Bang YJ, Camidge DR, Solomon BJ, Salgia R, et al. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N Engl J Med. 2014;371(21):1963–71.
Zou HY, Li Q, Engstrom LD, West M, Appleman V, Wong KA, et al. PF-06463922 is a potent and selective next-generation ROS1/ALK inhibitor capable of blocking crizotinib-resistant ROS1 mutations. Proc Natl Acad Sci U S A. 2015;112(11):3493–8.
Menichincheri M, Ardini E, Magnaghi P, Avanzi N, Banfi P, Bossi R, et al. Discovery of Entrectinib: A New 3-Aminoindazole As a Potent Anaplastic Lymphoma Kinase (ALK), c-ros Oncogene 1 Kinase (ROS1), and Pan-Tropomyosin Receptor Kinases (Pan-TRKs) inhibitor. J Med Chem. 2016;59(7):3392–408.
Shaw AT, Felip E, Bauer TM, Besse B, Navarro A, Postel-Vinay S, et al. Lorlatinib in non-small-cell lung cancer with ALK or ROS1 rearrangement: an international, multicentre, open-label, single-arm first-in-man phase 1 trial. Lancet Oncol. 2017;18(12):1590–9.
Li Z, Shen L, Ding D, Huang J, Zhang J, Chen Z, et al. Efficacy of Crizotinib among Different Types of ROS1 Fusion Partners in Patients with ROS1-Rearranged Non-Small Cell Lung Cancer. J Thorac Oncol. 2018;13(7):987–95.
Wu YL, Yang JC, Kim DW, Lu S, Zhou J, Seto T, et al. Phase II Study of Crizotinib in East Asian Patients With ROS1-Positive Advanced Non-Small-Cell Lung Cancer. J Clin Oncol. 2018;36(14):1405–11.
Shaw AT, Riely GJ, Bang YJ, Kim DW, Camidge DR, Solomon BJ, et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): updated results, including overall survival, from PROFILE 1001. Ann Oncol. 2019;30(7):1121–6.
Mao X, Zhang Z, Zheng X, Xie F, Duan F, Jiang L, et al. Capture-Based Targeted Ultradeep Sequencing in Paired Tissue and Plasma Samples Demonstrates Differential Subclonal ctDNA-Releasing Capability in Advanced Lung Cancer. J Thorac Oncol. 2017;12(4):663–72.
Zhang Y, Zeng L, Zhou C, Li Y, Wu L, Xia C, et al. Detection of Nonreciprocal/Reciprocal ALK Translocation as Poor Predictive Marker in Patients With First-Line Crizotinib-Treated ALK-Rearranged NSCLC. J Thorac Oncol. 2020;15(6):1027–36.
Song P, Zhang F, Li Y, Yang G, Li W, Ying J, et al. Concomitant TP53 mutations with response to crizotinib treatment in patients with ALK-rearranged non-small-cell lung cancer. Cancer Med. 2019;8(4):1551–7.
Qin K, Hou H, Liang Y, Zhang X. Prognostic value of TP53 concurrent mutations for EGFR- TKIs and ALK-TKIs based targeted therapy in advanced non-small cell lung cancer: a meta-analysis. BMC Cancer. 2020;20(1):328.
NCCN Clinical Practice Guidelines in Oncology. Non-Small Cell Lung Cancer Version 3.2020 [Internet]. National Comprehensive Cancer Network (NCCN). 2020.
Cai W, Li X, Su C, Fan L, Zheng L, Fei K, et al. ROS1 fusions in Chinese patients with non-small-cell lung cancer. Ann Oncol. 2013;24(7):1822–7.
Zhang L, Jiang T, Zhao C, Li W, Li X, Zhao S, et al. Efficacy of crizotinib and pemetrexed-based chemotherapy in Chinese NSCLC patients with ROS1 rearrangement. Oncotarget. 2016;7(46):75145–54.
Liu C, Yu H, Chang J, Chen H, Li Y, Zhao W, et al. Crizotinib in Chinese Patients with ROS1-Rearranged Advanced NonSmall-Cell Lung Cancer in Routine Clinical Practice. Target Oncol. 2019;14(3):315–23.
He Y, Sheng W, Hu W, Lin J, Liu J, Yu B, et al. Different Types of ROS1 Fusion Partners Yield Comparable Efficacy to Crizotinib. Oncol Res. 2019;27(8):901–10.
Xu H, Zhang Q, Liang L, Li J, Liu Z, Li W, et al. Crizotinib vs platinum-based chemotherapy as first-line treatment for advanced non-small cell lung cancer with different ROS1 fusion variants. Cancer Med. 2020;9(10):3328–36.
Canale M, Petracci E, Delmonte A, Chiadini E, Dazzi C, Papi M, et al. Impact of TP53 Mutations on Outcome in EGFR-Mutated Patients Treated with First-Line Tyrosine Kinase Inhibitors. Clin Cancer Res. 2017;23(9):2195–202.
Kron A, Alidousty C, Scheffler M, Merkelbach-Bruse S, Seidel D, Riedel R, et al. Impact of TP53 mutation status on systemic treatment outcome in ALK-rearranged non-small-cell lung cancer. Ann Oncol. 2018;29(10):2068–75.
Robles AI, Jen J, Harris CC. Clinical Outcomes of TP53 Mutations in Cancers. Cold Spring Harb Perspect Med. 2016;6(9):a026294.
Mantovani F, Collavin L, Del Sal G. Mutant p53 as a guardian of the cancer cell. Cell Death Differ. 2019;26(2):199–212.
Levine AJ. p53: 800 million years of evolution and 40 years of discovery. Nat Rev Cancer. 2020;20(8):471–80.
Skoulidis F, Heymach JV. Co-occurring genomic alterations in non-small-cell lung cancer biology and therapy. Nat Rev Cancer. 2019;19(9):495–509.
Michels S, Massuti B, Schildhaus HU, Franklin J, Sebastian M, Felip E, et al. Safety and Efficacy of Crizotinib in Patients With Advanced or Metastatic ROS1-Rearranged Lung Cancer (EUCROSS): A European Phase II Clinical Trial. J Thorac Oncol. 2019;14(7):1266–76.
Acknowledgements
The authors would like to thank all the patients and their families for their cooperation and participation. We would also like to thank the other clinical practitioners, nurses, and other hospital staff of all the participating institutions for their invaluable support to our patients.
Funding
This work received financial support from the Natural Science Foundation of Hunan Province (grant numbers: 2020SK2031, kq1801102, 2020SK2030, 2018RS3106, 2019-TJ-N04, 2019SK4010, and 2020JJ3025), and CAS “Light of West China Program”. The funding agencies had no role in the study design, data collection, analysis, interpretation, manuscript writing, and decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
YZ, NY, and S-HIO: Conceptualization, Organization, Data collection, Auditing, Supervision, Project administration, Funding acquisition, Writing- Reviewing, and Editing. LZ, YL, RZ, and XZ: Data curation, Methodology, Formal analysis, Writing-Original Draft Preparation, Writing- Reviewing, and Editing. QX, HY: Software, Validation, Writing- Reviewing, and Editing. JL: Formal analysis and Visualization, Writing- Reviewing, and Editing. CX, ZS, and JZ: Critical comments and Suggestions, Writing- Reviewing and Editing. AL: Formal analysis, Writing- Reviewing, and Editing. All authors read, reviewed, and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Approval of the study protocol was obtained from the Hunan Cancer Hospital Institutional Review Board Committee (approval number: 2017YYQ-SSB-026). All patients provided written informed consent for the use of their clinical and molecular data for research purposes.
Consent for publication
Not applicable
Competing interests
Analyn Lizaso declared that she is employed by Burning Rock Biotech. Sai-Hong Ignatius Ou has stock ownership and was on the scientific advisory board of Turning Point Therapeutics Inc (until Feb 28, 2019), is a member of the SAB of Elevation Oncology and has stock ownership in Elevation Oncology, and has received speaker honorarium from Merck, Roche/Genentech, Astra Zeneca, Takeda/ARIAD and Pfizer; has received advisory fees from Roche/Genentech, Astra Zeneca, Takeda/ARIAD, Pfizer, Foundation Medicine Inc, Spectrum, Daiichi Sankyo, Jassen/JNJ, and X-Covery. All the other authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Figure S1. Kaplan Meier curves comparing the progression-free survival (expressed in months) of patients with (A) single CD74-ROS1 and various single non-CD74 ROS1 fusions; and (B) single ROS1 fusions and non-reciprocal/reciprocal ROS1 translocations. The risk table below summarizes the number of patients included per time point
Additional file 2:.
Table S1. List of genes included in the 168-gene panel (Lung Plasma, Burning Rock Biotech). Table S2. Distribution of ROS1 fusions among the 220 patients with single ROS1 fusion and 15 patients with non-reciprocal/reciprocal ROS1 translocations. Table S3. Detailed breakpoint information for the non-reciprocal/reciprocal ROS1 translocations detected in the cohort. Table S4. Response to crizotinib of ROS1-rearranged lung cancers. Table S5. Clinicopathologic characteristics of the patients with single ROS1 fusions and non-reciprocal/reciprocal ROS1 translocations. Table S6. Treatment outcomes on first-line crizotinib therapy of the 159 patients with single ROS1 fusion grouped according to ROS1 fusion partners. Table S7. Detailed clinicopathologic characteristics and clinical outcomes of the 13 patients with uncommon non-CD74 ROS1 fusions. Table S8. Detailed clinicopathologic characteristics and clinical outcomes of the patients with non-reciprocal/reciprocal ROS1 translocations. Table S9. Comparison of concurrent mutation according to ROS1 mutation. Table S10. Cox regression analysis for progression-free survival (n=168). Table S11. Detailed clinicopathological characteristics and clinical outcomes of the 9 patients with concomitant driver mutations. Table S12. Detailed clinicopathological characteristics and clinical outcomes of the 8 patients with concomitant brain and non-brain progression on first-line crizotinib therapy. Table S13. Clinicopathological characteristics of the patients with brain progression and non-brain progression on first-line crizotinib therapy
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Y., Zhang, X., Zhang, R. et al. Clinical and molecular factors that impact the efficacy of first-line crizotinib in ROS1-rearranged non-small-cell lung cancer: a large multicenter retrospective study. BMC Med 19, 206 (2021). https://doi.org/10.1186/s12916-021-02082-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-021-02082-6