Abstract
Aspirin is widely used to lessen the risks of cardiovascular events. Some studies suggest that patients with multiple sclerosis have an increased risk for some cardiovascular events, for example, venous thromboembolism and perhaps ischemic strokes, raising the possibility that aspirin could lessen these increased risks in this population or subgroups (patients with limited mobility and/or antiphospholipid antibodies). However, aspirin causes a small increased risk of hemorrhagic stroke, which is a concern as it could potentially worsen a compromised blood-brain barrier. Aspirin has the potential to ameliorate the disease process in multiple sclerosis (for example, by limiting some components of inflammation), but aspirin also has the potential to inhibit mitochondrial complex I activity, which is already reduced in multiple sclerosis. In an experimental setting of a cerebral ischemic lesion, aspirin promoted the proliferation and/or differentiation of oligodendrocyte precursors, raising the possibility that aspirin could facilitate remyelination efforts in multiple sclerosis. Other actions by aspirin may lead to small improvements of some symptoms (for example, lessening fatigue). Here we consider potential benefits and risks of aspirin usage by patients with multiple sclerosis.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is a debilitating chronic disease characterized by inflammation, demyelination, axonal transection, and neurodegeneration in the central nervous system (CNS), leading to motor, sensory, and cognitive difficulties [1, 2]. Although MS is thought to have an autoimmune component, other mechanisms contribute to disease progression, for example, mitochondrial dysfunction, activated microglia, and intracerebral vascular changes [3–6]. Vascular changes include blood-brain barrier (BBB) leakage [7, 8], areas of decreased or increased cerebral perfusion [9–13], and vessel occlusion [14–16]. In line with these vascular changes, some reports have suggested that patients with MS have a greater risk of ischemic stroke and venous thrombosis [17–23]. These patients also have a higher incidence of antiphospholipid antibodies (APLAs), the main feature of antiphospholipid syndrome (APS); and patients with APS have an elevated risk of ischemic stroke and thrombosis.
Aspirin (acetylsalicylic acid, ASA) is a popular and readily available drug that has a variety of effects including alleviating pain and reducing fever, and it is often used for the secondary prevention of cardiovascular events in patients at risk [24–26]. Given the elevated risks for stroke and venous thrombosis in MS, ASA may help counter the development of these conditions [27–29]. ASA may also positively impact other facets of MS disease activity (for example, it may reduce inflammation, lessen fatigue, and promote remyelination). However, ASA usage increases the risk for hemorrhagic stroke [30–32], indicating the possibility that ASA could worsen BBB disruption in MS. ASA also has the potential to interfere with mitochondrial complex I activity [33], which has reduced activity in MS [34, 35]. Thus, the risk-to-benefit ratio for ASA usage by MS patients is unclear. This paper will review the potential benefits (Table 1) and risks (Table 2) associated with ASA usage in patients with MS.
Cardiovascular risks in MS
Patients with MS may have an increased risk for cardiovascular disease
Multiple studies have examined the risks for stroke in patients with MS, but questions remain about the findings. MS patients had a greater likelihood of being hospitalized for ischemic stroke (odds ratio (OR): 1.66, 95 % CI = 1.33–2.09) when compared to non-MS controls [36], but there were no differences or elevated risk for hemorrhagic stroke [36, 37]. A study on 32 different immune-mediated diseases (including MS) found that the risk for ischemic stroke was significantly increased (standardized incidence ratio = 3.05) in the year following a hospitalization for MS [37]. A study of 13,963 patients with MS compared to 66,407 non-MS controls from the Danish National Registry of Patients [17] also found a heightened risk of stroke shortly after MS diagnosis (for example, within a year) with the elevated risk being most pronounced in younger MS patients and absent in older MS subjects (≥56 years) [17]. However, the opposite trend for the effect of age on the risk of strokes in patients with MS was observed in a Swedish study [18]; complicating the interpretation, it is unclear if the same types of strokes were evaluated in these studies. When considering these studies, however, it is important to recognize that patients who are having an MS relapse are often misdiagnosed as having a stroke, particularly early in the course of their disease. Thus, some studies showing elevated risks for stroke in patients with MS may be inaccurate and reflect misdiagnoses or an increase in the surveillance (for example, MRI and more frequent physician visits) of this patient population identifying asymptomatic lesions suggestive of strokes [38].
Venous thromboembolism (VTE) appeared to be elevated in patients with MS compared to controls [18, 19, 21–23]. Ocak and colleagues [39] found an increased risk of venous thrombosis in MS patients: the OR for venous thrombosis in MS was 2.4 (95 % CI 1.3–4.3), and the OR increased to 12.5 (95 % CI 1.5-107.9) in patients with both MS and increased factor VIII levels, which indicates the additional risk factor of thrombophilia. Also, APLAs, which are a diagnostic feature of APS that results in thromboses, occur in a greater percentage of MS patients compared to controls (discussed later in the subsection “ASA and antiphospholipid antibodies”).
Individuals who have an occupation that involves prolonged sedentary behavior or patients experiencing immobilization have an increased risk of venous thrombosis compared to more mobile people [39, 40]. A sedentary lifestyle is also associated with an increased risk of stroke [41]. The activity level of patients with MS is less than that of healthy control subjects [42]. Physical inactivity, particularly in patients needing a wheelchair or who are bedridden, may contribute to the higher prevalence of thrombosis and ischemic strokes in patients with MS [43, 44].
Whether patients with MS have an increased risk for myocardial infarction is unclear [20]. In one study, MS patients were found to have decreased risks of being hospitalized for myocardial infarction and ischemic heart disease [36]; however, a recent study conducted with an initial cohort of 8,281 MS patients in Sweden determined that the risks for myocardial infarction, heart failure, and stroke were increased in individuals with MS compared to matched controls, and that these risks were more pronounced in women than men [18]. Shared pathological factors (for example, inflammation, oxidative stress, thrombogenic factors) between MS and cardiovascular diseases may explain the association between these conditions [18]. Of note, MS patients with ≥ 1 cardiovascular risks had increased MRI indications of disease activity, that is, more brain atrophy and an increase in lesion burden [45].
Treatments for MS may also increase the risk for cardiovascular diseases [20]. For example, systemic glucocorticoids have been reported to increase risks of stroke, myocardial infarction, and atrial fibrillation [20]. Additionally, a positive association was found for cardiovascular risk factors and the use of disease modifying therapies (DMTs) such as interferon-β and glatiramer acetate [46]. For example, about 20 % of MS patients on DMTs versus about 5 % of MS patients naïve to DMTs had diastolic blood pressure above 90 mmHg, and about 25 % of MS patients on DMTs versus about 14 % MS patients naïve to DMTs had glucose > 100 mg/dL [46]. The association was more pronounced in chronic progressive MS patients compared to relapsing remitting MS (RRMS) patients, but the correlation to disease activity (for example, rate of clinical relapse) was weak [46]. Although similar studies have not been conducted for more recent DMTs, cardiac side effects can be associated with these agents. For example, an increase in hypertension has been noted for teriflunomide (4 % treated versus 2 % placebo [47]). A reduction of heart rate can occur within six hours of fingolimod initiation [48], and there can be an increase in blood pressure in a small percentage of patients over the long term [49].
Increased risk of dying from cardiovascular disease in patients with MS
Besides a possibly increased risk of cardiovascular disease (CVD), studies generally suggest that MS patients have a heightened risk of dying from CVD [43, 50]. As reviewed in Christiansen [20], patients with MS have a 6–34 % greater risk of death by CVD or stroke than for the overall population, and greater than 10 % of MS patients may have stroke as the cause of death. An analysis of 9,881 MS patients in the Danish Multiple Sclerosis Registry revealed that the mortality rate from CVD was significantly higher in MS patients compared to matched controls [50], and an analysis of over 6,000 patient deaths in the Danish MS Registry revealed that 17.6 % of deaths were caused by vascular or cardiac diseases, which was the most frequently listed cause of death outside of MS itself [43]. The standard mortality rate (the number of subjects who died from the specific cause divided by the number of deaths expected from population mortality statistics) of cardiac or vascular diseases in this same patient population was 1.34, indicating about a 34 % greater chance of death by CVD in MS patients when compared to general population mortality statistics [43]. In contrast, a study in South Wales revealed that while CVD caused 16 % of deaths in the MS population surveyed, this rate did not differ from the expected death rates in the general population [51].
While it appears that patients with MS have a greater likelihood of dying from cardiovascular-related issues, the underlying causative reason is not clear. These patients may lead a more sedentary lifestyle than healthy individuals due to motor symptoms and fatigue, for example [42], particularly as the disease progresses, and a less active lifestyle has been associated with cardiovascular risk factors such as impaired glucose tolerance and the development of metabolic syndrome in the general population [52, 53]. Furthermore, altered metabolic responses in patients with MS, such as increased adipose lipolytic activity, could be a factor in lower physical performance [54]. Several studies (reviewed in [55]) suggest that patients with MS are more likely to develop vascular disease and comorbidities related to metabolic syndrome (such as obesity, impaired glucose tolerance, and dyslipidemia), but these factors may develop or worsen as a result of progressively debilitating MS symptoms. Because many of these studies are retrospective, correlational designs, the exact cause and effect relationship between MS and CVD risk and mortality cannot be easily discerned. It is unclear whether CVD risk factors contribute to MS disease pathogenesis, whether MS symptoms promote the development of CVD and mortality, or whether a shared underlying disturbance, such as in glucose metabolism [56], underlies both disease processes.
Treatment potential of ASA for cardiovascular disease in patients with MS
ASA mechanisms of action
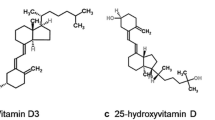
Aspirin (ASA) is a traditional nonsteroidal anti-inflammatory drug (tNSAID) used to treat inflammation, pain, and fever, and to inhibit platelet activation and aggregation. This latter effect inhibits thrombus formation, thus providing cardioprotection, and is the basis for the use of ASA in the prevention of myocardial infarction [31, 57, 58]. The many therapeutic uses of ASA are due to its inhibition of cyclooxygenases (COXs), enzymes that catalyze a step in the production of prostanoids (Fig. 1). Prostanoids include prostaglandins, prostacyclin, and thromboxanes, molecules with pleiotropic effects on a large number of physiologic systems [59].
Aspirin inhibition of the synthetic pathway of prostaglandins I2, E2, and thromboxane A2. Cyclooxygenases metabolize arachidonic acid to PGH2, which in turn is converted into various prostanoids by specific enzymes. Depending on the receptors activated by these molecules, mixed physiologic effects on the vasculature and platelet reactivity occur. Aspirin irreversibly inhibits cyclooxygenase activity. COXs = cyclooxygenases; PGH2 = prostaglandin H2; PGI synthase = prostaglandin-I synthase; PGE synthases = prostaglandin-E synthases; TXA synthase = thromboxane synthase; PGI2 = prostacyclin; PGE2 = prostaglandin E2; TXA2 = thromboxane A2; IP receptor = prostacyclin receptor; EP receptors = prostaglandin E2 receptors; TP receptors = thromboxane A2 receptors
A unique quality of ASA that differentiates it from other tNSAIDs is its ability to covalently acetylate COXs [60], whereas other tNSAIDS are competitive, reversible inhibitors [59, 61]. The irreversible linkage by ASA inhibits the enzyme’s ability to convert arachidonic acid to prostaglandin H2 (PGH2), a committed step in prostanoid synthesis, and recovery of the system is directly related to production of new COX enzymes. Cyclooxygenase-1 (COX-1) is considered to be constitutively expressed and can be identified in most tissues [62]. Cyclooxygenase-2 (COX-2) is generally considered an inducible isozyme found in monocytes, endothelial cells, and fibroblasts, although it is also constitutively expressed in some cells within the brain, testes, and kidney [62]. Therefore, COX-1 is thought to be the dominant source of prostanoids for housekeeping functions and COX-2 is considered to be a main source in inflammation, although platelet-derived prostanoids generated through COX-1 are linked to promotion of an inflammatory state [59, 63–65].
Once formed, PGH2 may be converted to prostaglandin E2 (PGE2) by prostaglandin-E synthase; prostacyclin (PGI2) by prostaglandin-I synthase; or thromboxane A2 (TXA2) by thromboxane synthase [66, 67]. These mediators interact with specific G-protein coupled receptors that utilize either cAMP or IP3/DAG/Ca2+ as second messengers ultimately to elicit physiologic responses that often are in opposition to each other. In terms of vascular smooth muscle tone and platelet reactivity, PGI2 and TXA2 act conversely, with PGI2 decreasing and TXA2 increasing these parameters [64]. Also, PGI2 inhibits vascular smooth muscle cell proliferation and TXA2 promotes it [64]. Increases or decreases in vascular tone and platelet reactivity can be elicited by PGE2, depending on which of its five receptors are activated [64].
Platelets participate in the thrombus formation process, and as such, hyperactivity built upon underlying atherosclerosis can contribute to the development of pathological cardiovascular events that may result in decreased blood flow, acute coronary syndrome, and stroke [68, 69]. Through irreversible inhibition of platelet COX-1, and the resultant decrease in TXA2 production, ASA decreases platelet activation and aggregation, and demonstrates a cardioprotective effect [57, 64]. Inflammation plays a role in the development of atherosclerotic plaques, and evidence suggests that platelets contribute to inflammatory processes through activation of vascular endothelial cells and leukocytes in inflamed microvessels [70]. Furthermore, platelets contain dense granules and α-granules that store preformed chemical mediators. Upon platelet activation and subsequent degranulation, these mediators, which include growth factors, cytokines, and coagulation factors, are released and can allow the platelet to influence the vascular endothelium and the inflammatory response [70, 71]. In neuroinflammatory disease states like MS, platelet activation could aggravate the disease process [65, 71–73]. In this regard, ASA inhibition of platelet COX-1 could potentially limit production of proinflammatory eicosanoids and attenuate the inflammatory state.
Since the COX inhibition by ASA is irreversible, the antiplatelet effect is dependent on the synthesis of new platelets. Therefore, lower doses of ASA (50–100 mg/day) are effective due to action within platelets, thus making it useful in the treatment of coronary artery disease [31, 57, 58, 64, 74]. Distinct from this platelet effect, higher doses are used for analgesic, antipyretic, and anti-inflammatory effects and are usually taken only as needed as opposed to daily [59].
ASA use in preventing cardiovascular disease
In order to assess the potential impact of ASA to counter cardiovascular events in MS, it is helpful to address its role in reducing CVD in other segments of the population. In the general population, regular ASA use for prevention of cardiovascular events ranges between 18–41 %, and usage can be more prevalent in subpopulations, for example, diabetics and older individuals who are at higher risk for CVD [75–78]. Long-term administration of ASA at low doses helps prevent strokes, heart attacks, and blood clot formation in people at high risk of these events [24–26]. In an analysis of antiplatelet treatment following acute ischemic stroke, Sandercock et al. [79] found a significant decrease in recurrent ischemic stroke and death in patients who began ASA treatment no more than 14 days following a presumed ischemic stroke occurrence (OR 0.95, 95 % CI 0.91–0.99). It has also been noted that although there is a slight increase in the incidence of intracranial hemorrhages with antiplatelet treatment, the benefits of preventing repeat ischemic strokes and other cardiovascular events such as pulmonary embolism (PE) outweigh the risks of intracranial bleeding [30, 79]. ASA monotherapy (50–325 mg/day), clopidogrel, or extended-release dipyridamole (ER-DP) combined with ASA are therapies recommended by the American Heart Association and American Stroke Association, as well as the Eighth American College of Chest Physicians (ACCP), for the secondary prevention of ischemic strokes in individuals with a history of ischemic events including stroke [25, 80, 81]. The combination of ASA and ER-DP is preferable to ASA alone, while the combination of ASA with clopidogrel has a heightened risk of bleeding events, and thus should be avoided [25, 26, 80–83].
Although ASA has been established as effective for preventing secondary cerebrovascular events [26], its prophylactic efficacy is less clear. A significant reduction in the risks for a first myocardial infarction was found with ASA usage, but results for ASA’s efficacy in preventing a first stroke and CVD were inconclusive [31, 84]. A review of 27 studies on the effectiveness of ASA for the primary prevention of cardiovascular events (for example, in patients not at risk for CVD) revealed only modest/minor benefits that did not outweigh the risks of increased bleeding and hemorrhagic strokes [32].
Platelets were traditionally considered to play a greater role in arterial rather than venous thrombosis, but platelets have been shown to have a role in venous thromboembolism (VTE) by inducing the formation of neutrophil extracellular traps, releasing proinflammatory mediators and microparticles, and aggregating as a component of thrombi themselves [27]. While some studies such as the Longitudinal Investigation on Thromboembolism Etiology did not find a reduction in VTE by ASA users [85], other trials report that ASA lowers the risk of deep vein thrombosis (DVT) [29]. The INSPIRE study combined data from two previous studies where patients were given ASA after a first unprovoked VTE to determine its effects on VTE recurrence. The INSPIRE analysis found that ASA reduces the overall risk of recurrent VTE by 42 % (P = 0.005) with only minor bleeding concerns, supporting the use of ASA for secondary prophylaxis of VTE [28]. In the large Pulmonary Embolism Prevention (PEP) trial, which included over 13,000 patients undergoing surgery for hip fracture or elective arthroplasty, PE or DVT was experienced in 105 out of 6,679 (1.5 %) patients receiving 160 mg ASA compared to 165 of 6,677 (2.5 %) patients receiving a placebo, which equals a proportional reduction of 36 % PE/DVT in those treated with ASA (P = 0.0003) [86]. ASA was also found to be effective for the prevention of PE in high-risk patients by the Antithrombotic Trialists’ Collaboration in a 2002 meta-analysis: patients taking an antiplatelet (for example, ASA) had a 25 % reduced risk of acute PE compared with patients on placebo (P < 0.01) [87]. Based on results such as these and the low cost and relatively low risk of bleeding of ASA when compared to warfarin and newer anticoagulants, the American Academy of Orthopedic Surgeons in 2009 and the ACCP in 2012 included ASA as a method in their guidelines to prevent VTE in high-risk orthopedic surgery patients [27, 88].
Considerations regarding ASA use for cardiovascular disease in patients with MS
Given that ASA may reduce cardiovascular events in non-MS patients at risk, the possible elevated risks for stroke and venous thrombosis in MS, along with the observance of vessel congestion [14, 89–91] and altered perfusion of cerebral structures [9–12, 92] in this population, suggests that MS patients taking ASA may have some degree of protection against stroke or venous thrombosis (Table 1). However, the slight risk of increased intracerebral bleeding observed in stroke patients given ASA [79] is troubling, since MS patients have a compromised BBB [7, 8] and ASA treatment could further disrupt the BBB (Table 2). For example, the elevated coagulation proteins observed in the CNS of patients with MS [92] could be performing a protective role by limiting BBB leakage, and if ASA disrupted their deposition, then this could slow the resolution of the leakage. However, ASA can act to limit vascular leakage: ASA reduced arachidonate-induced vascular leakage in the peritoneum [93] and induced lipoxin A4, which was found to reduce vascular leakage following acute ear inflammation [94]. ASA also lowered the permeability of the BBB in non-stroke patients [95].
It might be important to identify patients with MS who have a heightened risk of a cardiovascular event, as they would be expected to have the most favorable risk-to-benefit ratio when using ASA. Besides the traditional risk factors for cardiovascular events, there are features of MS that may potentially lead to increased risk of CVD within the MS population. For example, a more sedentary or immobile state in MS patients [42, 44] or taking an MS DMT [46–49] might be associated with an increased risk of cardiovascular events.
ASA and antiphospholipid antibodies
Multiple studies have reported that APLAs are more prevalent in patients with MS than in the general population [96–98]. APLAs are the main diagnostic feature of APS, an autoimmune disease characterized by thrombosis and/or pregnancy morbidity and elevated levels of anticardiolipin antibodies, lupus anticoagulant, and/or β2 glycoprotein I [99]. MS and APS share various features, and one disorder can sometimes be misdiagnosed for the other [96, 99]. Although the role that APLAs may have in MS is presently unclear, recent studies indicate a relationship between APLAs and a more severe MS disease course [97, 98, 100–102]. In a prospective three-year study following interferon-β (INF-β)-treated MS patients with or without APLAs, Zivanidov et al. found that the APLA-positive patients showed a greater disease progression as measured by higher MRI lesion volumes, increased tissue damage, and loss of brain volume, as well as more clinical relapses [102]. The presence of anti-INF-β binding antibodies may decrease the efficacy of INF-β treatment, and Garg et al. [103] found a significant co-occurrence of high APLAs in MS patients with anti-INF-β binding antibodies. A higher frequency of APLAs has been reported in secondary progressive MS (SPMS) compared to RRMS, which is consistent with the idea that the presence of APLAs is related to a more chronic, advanced stage of the disease [97, 102, 104].
Given that thromboses are a main symptom in APS, anticoagulation, antiaggregation, and ASA are all used as treatment for this syndrome [96, 99, 102]. Although many physicians prescribe daily low-dose ASA for asymptomatic APLA-positive patients to prevent a first thrombotic event, results from studies on the benefit of ASA prophylaxis in this population are mixed [105]. The Antiphospholipid Antibody Acetylsalicylic Acid study found that 81 mg of ASA daily for APLA-positive but asymptomatic patients was not more effective than placebo in protecting against a thrombotic event [106]. In contrast, in an individual patient-level meta-analysis from five international cohort studies, Arnaud and colleagues [107] found that prophylactic low-dose ASA in patients with APLAs significantly reduced the risk of a first thrombotic event. Although the role of APLAs in the pathogenesis of MS is not clear, given that MS is associated with an increased risk of thrombosis and cardiovascular events (see, for example, [18, 20, 21]), MS patients with APLAs may benefit from anticoagulation or ASA treatment.
Potential effects of ASA on vascular pathology in MS
In addition to affecting thrombosis and stroke in MS patients, ASA could affect other components of vascular pathology in MS. Pathological changes to the vascular tissue in the CNS have been observed since the earliest descriptions of MS (see, for example, [89, 108]), and they include platelet and fibrin deposits associated with vessels in active lesions, vessel occlusion, vascular thickening, enhanced deposition of perivascular collagen, BBB disruption, and perivascular inflammation [7, 8, 14–16, 109]. Proteomic analysis revealed the deposition of an array of coagulation proteins in chronic active plaques [110], and anticoagulants decreased the severity of experimental autoimmune encephalomyelitis (EAE) [110], an animal model of MS, indicating that vascular changes have a detrimental role in the disease.
Platelets are activated in MS and have been implicated in contributing to pathogenesis, for example, by promoting inflammation [65, 71–73]. Platelets were identified in MS and EAE CNS lesions, and depletion of platelets lessened EAE severity [73]. Two indicators of platelet activation, β-thromboglobulin (β-TG) and platelet factor 4 (PF4), were higher in the plasma of MS patients during quiescent disease compared to control subjects (P < 0.001) [111]. ASA 50 mg/day taken orally by patients with MS significantly lowered plasma β-TG levels (P < 0.001), but not to normal levels [111]. PF4 levels did not undergo a significant decline following ASA treatment, suggesting that a source other than platelets, for example, mast cells, could have been an important contributor to PF4 levels in the plasma of these patients [111]. In normal male subjects, ASA decreased platelet aggregation and P-selectin expression in a dose-dependent manner, and low ASA doses increased the dilatation of the brachial artery while high doses decreased flow [112]. Although these studies suggest a benefit of ASA by inhibiting platelet activation, more studies are needed to confirm the results and elucidate the specific mechanism of action.
Besides platelets acting to promote inflammation in EAE [73], fibrin deposition has been credited with activation of microglia, which have been associated with tissue damage [113]. Depending on the type, microglia can have different influences on disease activity in MS; that is, they can induce tissue damage or promote repair [5]. Blockage of fibrin formation lessened disease activity in EAE [114, 115]. ASA may promote fibrinolysis or interfere with fibrin deposition [116].
In addition to fibrin, thrombin activity has been associated with worsening of inflammatory CNS disease states such as MS [117], and thrombin activity in the spinal cord of mice with EAE is associated with multiple pathological features [118]. ASA may decrease thrombin levels at sites of microvascular injury [119]. In experimental APS, which models a condition that results in clots in deep veins and in organs such as the brain, ASA also reduced tumor necrosis factor alpha (TNFα) and prostaglandin E synthesis and increased thrombin inhibitors [120].
Vascular changes may contribute to the decreased perfusion observed in MS [9–12, 92, 121]. Decreased perfusion has been observed in the cortex [9, 10, 12], deep gray matter structures (for example, thalamus, caudate) [10–12], and normal-appearing white matter (NAWM) [92] of patients with MS. In addition, white matter lesions from patients with RRMS had altered perfusion (some with decreased perfusion and others with an increased perfusion compared to that from white matter in control subjects) [10, 122]. The extent of white matter lesions was correlated with decreased cortical blood flow [123], and decreased cerebral blood flow has also been observed in EAE [124, 125].
Decreased perfusion could impair tissue oxygenation. Decreased tissue oxygenation in MS patients has been detected in white matter and cortex gray matter by positron emission tomography [126], and decreased utilization of oxygen in MS was revealed in periventricular veins by susceptibility-weighted imaging (SWI) [127] and by T2-relaxation-under-spin-tagging of venous sinus blood [128]. Additionally, lesions observed by SWI in the spinal cord of EAE mice were thought to be detected largely due to deoxyhemoglobin, whose presence was likely a result of hypoxia [129]. At the molecular level, upregulation of hypoxia-inducible factor-1α (HIF-1α) has been observed in active MS plaques by immunohistochemistry [130, 131], and the upregulation of genes associated with ischemic preconditioning, including HIF-1α, has been observed in NAWM in patients with MS [132]. Additionally, endoplasmic reticulum stress proteins, which have been associated with ischemic injury, are overexpressed in active MS lesions [133, 134] and in gray matter MS lesions [135]. Although altered perfusion may reduce oxygen delivery and impair energy production [136], vascular changes, that is, microvascular thrombosis, as the cause of hypoxia-like changes in MS have been questioned, since hypoxia-like changes have been observed in MS patients in the absence of vascular pathology [137].
Mitochondrial dysfunction has been observed in multiple sites in the CNS of MS patients, including NAWM, lesions, and cortex, and altered mitochondria function may help create a hypoxic state [35, 137–139]. ASA may act to inhibit complex I of the respiratory chain [33]. Complex I is decreased in chronic active white matter lesions and in the motor cortex of patients with MS [34, 35]. Thus, ASA has the potential to further lower complex I activity in MS, and ASA’s inhibitory effect may be more pronounced with depletion of glutathione [140], which is thought to occur in patients with MS [141, 142]. Furthermore, inhibition of complex I activity can lead to an increased production of reactive oxygen species (ROS) [143], which could amplify cellular damage.
Cerebrovascular reactivity, the ability of the cerebral vasculature to increase local blood flow via arteriole dilation in response to neural activity, is impaired in MS, perhaps as a result of vascular desensitization from chronic high levels of nitric oxide stemming from inflammation [144]. Interestingly, ASA has been found to increase endothelial nitric oxide synthase activity [145, 146], which would favor an increase in blood flow, but not if vascular desensitization has developed [144].
ASA effects on MS symptoms
ASA in MS, EAE, and related studies
The cardiovascular effects of ASA would not be expected to readily translate into gross alterations of MS disease activity. Only a couple of studies have looked directly at the effects of ASA on MS disease activity, and they were performed decades ago using relatively elementary outcome measures. Two studies in the early 1960s examined the effects of calcium aspirin (Solprin) (3.5 g divided over 3 doses per day) against prednisolone (15 mg once per day initially; reduced to 10 mg per day at 8 months) and placebo (lactate tablets) [147], or chloroquine (250 mg once per day) and placebo [148], in MS. Each patient’s disease condition was measured using Alexander’s 1958 numerical scoring system prior to treatment and at 6 and 18 or 6 and 14 months following treatment, respectively. No significant differences were found between treatment groups in either study, although patients receiving Solprin in the prednisolone study deteriorated the least over 18 months [147], and Solprin performed better than chloroquine but worse than the placebo in the latter experiment [148]. Given that these studies were conducted using an outdated measure of MS disease activity, the interpretation of the results should be viewed cautiously. MRI studies, including those examining the vasculature and blood flow, and other more current measures of MS disease activity could provide greater insights regarding the effect of ASA on disease progression.
Studies examining ASA in animal models of MS also have been relatively sparse. One study published in 1949 examined the prophylactic and therapeutic effects of sodium salicylate (the main metabolite of ASA) and para-aminobenzoic acid, either alone or in combination, in a guinea pig EAE model [149]. Although neither compound showed effects against disease onset and progression at moderate dosage levels, the combination of sodium salicylate and para-aminobenzoic acid, as well as larger doses of sodium salicylate by itself, seemed to delay onset, lessen incidence, and inhibit disease severity if administration was begun prior to or shortly after (5 days or less) EAE induction [149]. Treatment with sodium salicylate or the combined drugs after the animals became sick had no effect on the disease [149]. When ASA was tested in the guinea pig EAE model by another group, there was no beneficial effect [150]. In the Lewis rat model of EAE, ASA delayed the onset of disease but increased the severity of disease [151], while sodium salicylate postponed disease onset and reduced clinical signs [152].
More recent studies have looked at the role of COX-1 and COX-2 in EAE. Naproxen, a COX-1 and COX-2 inhibitor, was shown to delay EAE onset and reduce the severity of the disease when treatment was started on the day of EAE immunization [153]. In another study, celecoxib, a new generation COX-2 inhibitor, reduced EAE incidence and/or severity when animals were treated beginning on the day of EAE induction or 8 days post-induction [154]. But celecoxib also reduced disease severity in COX-2-deficient mice; and nimesulide, another COX-2 inhibitor, did not affect disease development or severity, which indicates that the mechanism of action of celecoxib on EAE is not via the COX-2 pathway [154].
ASA was found to limit the production of ROS and proinflammatory cytokines (for example, TNFα and IL-1β) by a microglial cell line treated with the activator lipopolysaccharide [155, 156], and ASA limited proinflammatory cytokine production and microglial activation following middle cerebral arterial occlusion in the rat [157]. Activated microglia can mediate tissue damage in MS [3–5], and lessening their production of inflammatory mediators by ASA could have possible benefits. Also, it may be that ASA could promote resolution of inflammation in MS by inducing lipoxin A4 [158], which is an anti-inflammatory mediator [159].
In salt-loaded, stroke-prone, spontaneously hypertensive rats, ASA suppressed BBB damage and reduced several markers of inflammation (for example, matrix metalloproteinase-9 activity, superoxide production, and macrophage accumulation) [160], raising the possibility that ASA could limit similar pathological processes in MS.
Recent studies found that ASA upregulated the production of the ciliary neurotrophic factor [161], which augments myelin formation [162]. ASA also induced the proliferation and differentiation of oligodendrocyte precursors and limited demyelination following a cerebral ischemic lesion [163]. If ASA acted similarly in response to MS lesions, then it could promote remyelination efforts [161].
ASA and fatigue
Fatigue is a pervasive and debilitating symptom associated with a marked decrease in the quality of life for patients with MS. The cause of fatigue is not understood. Some possible theories concerning the causes of fatigue have included: elevated body temperature (in RRMS patients) [164], sleep disturbances and depression [165, 166], proinflammatory cytokines [167], reduced metabolism and degeneration of cerebral and deep gray matter structures [168, 169], reduced connectivity [170], and reduced perfusion of deep gray matter [11]. There are a limited number of approaches used to counter fatigue in MS, for example, amantadine, modafinil, vitamin D analog, treatment for sleep disorder, and exercise [171–175]. Overall, studies have been conflicting as to the benefits of these modalities, and better management of fatigue is sorely needed.
ASA has been tested as a way to counter fatigue (Table 1). Following observations in a clinical setting that some MS patients seemed to experience a lessening of fatigue while taking ASA for non-MS-related symptoms, a double-blind, randomized, crossover study of 650 mg oral ASA twice daily or placebo for 6 weeks was initiated, where a modest but detectable improvement was found during the treatment phase with ASA [176]. The mean obtained from the Modified Fatigue Impact Scale (MFIS, range 0–84), which was administered weekly, decreased from 46.3 ± 16.0 at baseline to 38.1 ± 17.0 during ASA administration versus 42.5 ± 18.8 during placebo (ASA versus placebo, P = 0.043) [176]. In addition, of the patients completing the crossover components of the study, only 1/26 patients preferred placebo compared to 10/26 of patients preferring ASA treatment (P = 0.012) when responding to the Global Fatigue Change self-assessment [176]. None of the other outcome measures for fatigue assessment revealed statistically significant differences (10-point Visual Analog Scale, Fatigue Severity Scale [FSS], MS-Specific Fatigue Scale), but there was a trend towards a greater reduction of fatigue symptoms while taking ASA on the Visual Analog Scale (ASA versus placebo, P = 0.076) [176].
A subsequent randomized double-blind crossover clinical trial for 52 patients with MS was conducted over a ten-week period to study the effectiveness of ASA and amantadine for alleviating fatigue in MS. Half of the patients were randomly assigned to receive 500 mg ASA orally once daily for the first four weeks, and following a two-week washout period were switched to 100 mg amantadine orally twice a day for the final four weeks; the other half of the patients received the treatments in reverse order [177]. A significant decrease in self-reported fatigue levels measured using the FSS with both ASA and amantadine was found following a baseline measurement [177]. After the first round of treatment, mean FSS scores decreased by 1.1 (from a maximum of 7) for ASA and by 0.8 for amantadine [177]. During the two-week washout period, the mean FSS scores increased back to baseline levels [177]. In the second phase of the study, where patients received crossover treatments, self-reported fatigue scores were once again reduced significantly for each treatment regimen: mean FSS decreased by 0.7 for ASA and by 1.6 for amantadine [177]. The authors noted that both ASA and amantadine were well-tolerated by patients with few and mild side effects, none of which led to participant dropouts. Given the promising results shown by both treatments in these studies, they suggest that ASA and amantadine deserve further consideration as potential treatments to combat fatigue in MS [177].
A placebo-controlled, double-blind, multicenter study was performed comparing placebo, 162 mg/d and 1,300 mg/d of ASA [178]. Although the study was not completed, an intermediate analysis of the placebo and high dose groups revealed a difference of 4.6 points on the MFIS, that is, adjusted mean scores of 42.7 versus 38.1 in the respective groups. However, the study was underpowered and it did not reveal a statistically significant effect [178]. The authors indicated that it is unlikely that ASA provides a clinically relevant benefit for MS patients [178]. It is possible that confounding factors, such as an undiagnosed sleep disorder [166], could interfere with ASA effect on fatigue.
The mechanism of action by which ASA might lessen fatigue, even minimally, is unclear. ASA’s reduction of fatigue symptoms may be through the drug’s antipyretic effects [176, 177], which is supported by a recent study that found a correlation between fatigue, as measured by FSS and MFIS, and elevated body temperature in RRMS patients [164]. In addition, ASA could have affected other systems (for example, autonomic or neuroendocrine) involved in the perception of fatigue [176, 177]. ASA also could have countered proinflammatory cytokines [176, 177], which may contribute to fatigue [167, 179]. ASA may also act on fatigue associated with some form of interferon-β therapy, which was taken by 5/30 patients in the Wingerchuck et al. (2005) study [176] and by 52/52 patients in the Shaygannejad et al. (2012) study [177].
ASA and depression
Patients with MS are more likely to experience depression than the general population [180]. Although depression has traditionally been thought of as a neurotransmitter-related/driven disease, evidence suggests that inflammation may play a role in the disorder [181]. As such, drugs that reduce inflammation may be beneficial in depression [181].
The use of ASA may lower the risk of major depression [182]. A study on depression and anxiety in patients with myocardial infarction found that those taking ASA reported fewer depression and anxiety symptoms (P < 0.01) as measured by the Hamilton Depression and Hamilton Anxiety Rating Scales, respectively [183]; and an analysis of 174 male coronary angiography patients (99 on ASA) found fewer depressive symptoms in those taking ASA regularly (range from 80 mg every other day to 325 mg daily), both by self-report (P = 0.016) and reported perceptions from a significant other (P = 0.048) [184].
In an established rodent model of depression, ASA lessened immobility in a forced swim test in rats and concurrently attenuated cytokine levels (IL-6 and TNF-α) [185]. Additionally, preliminary clinical trials have reported that ASA in combination with antidepressants (fluoxetine) can shorten the onset of antidepressant action and be effective against treatment-resistant depression [186], and this effect has also been demonstrated in rats [187, 188]. However, 8 participants in a small clinical sample (10 total) of patients experiencing depression who were treated with 160 mg/day ASA in combination with 20 mg/day of the antidepressant citalopram experienced severe side effects (anxiety and akathesia) that necessitated the hospitalization of 4 participants while 2 other patients exhibited suicidal behavior, resulting in the termination of the study at 14 days [189]. As such, the authors caution the use of ASA in combination with certain antidepressants such as citalopram [189]. Furthermore, NSAIDs such as ibuprofen and ASA may interfere with the antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) [190]. It has also been found that the combined treatment of ASA with an antidepressant (SSRI) increases the risk of bleeding over ASA alone in patients who had experienced an acute myocardial infarction [191]. Because damage of the BBB [7, 8] and microhemorrhages [192–195] occur in MS, caution is warranted when adding ASA to the treatment regimen for MS patients who may be concurrently receiving antidepressant treatment for depressive symptoms.
Potential risks associated with ASA use in MS
Due to the known pleiotropic effects of the prostaglandins and thromboxanes on multiple physiological systems, it is not unexpected that inhibition of their production by ASA could potentially cause various adverse effects. Many of the major adverse effects related to ASA use are discussed below and summarized in Table 2.
While the incidence of cerebral hemorrhage during ASA treatment is low in most studies, the antiplatelet effect of ASA can contribute to the development of increased cerebral bleeding [30]. The Antithrombotic Trialists’ Collaboration performed a meta-analysis (6 primary prevention trials and 16 secondary prevention trials) of serious vascular events, including stroke and major bleeds comparing long-term ASA versus control [31]. Their conclusions included that ASA increased incidences of hemorrhagic stroke in both primary (P = 0.05) and secondary (P = 0.07) prevention trials and when analyzed in combination (P = 0.01), while ASA showed a protective effect concerning ischemic stroke (P = 0.005) [31]. Sutcliffe et al. [32] reviewed data from randomized trials assessing ASA in the primary prevention of CVD and cancer and concluded that the benefits of ASA for primary prevention of CVD are modest, and are much less than those for secondary prevention. Furthermore, while benefits and harms were low based on person-years, they estimated an increased risk of hemorrhagic stroke ranging from 32–38 % [32].
Although the increases in incidents of hemorrhagic stroke noted are slight, it is possible that in disease states like MS, where the BBB is disrupted or compromised [7, 8], the risk of intracerebral bleeding may be greater with ASA usage. Additionally, there is an increased risk of immune thrombocytopenia in patients with MS [196], which would be a counter indication of ASA usage due to the enhanced risk of bleeding with ASA in this patient population [197].
An adverse effect that is well associated with ASA use is upper gastrointestinal (GI) tract injury and bleeding. Because ASA inhibits the production of prostaglandins by GI-located COX-1, these gastroprotective substances are unavailable and damage may occur. The risk of complications is increased with aging, concomitant use of anticoagulants, history of NSAID-associated bleeding, and comorbidities [198]. The Antithrombotic Trialists’ Collaboration study noted above determined that ASA usage increased major GI and extracranial bleeds to 0.10 % versus 0.07 % per year in controls (RR = 1.54 [1.30–1.82], P < 0.0001) [31].
ASA and salicylate, the active metabolite of ASA, are known to cause hearing loss and tinnitus at high doses (for example, 6–8 g/day) [199–203]. The mechanisms behind these effects are unclear, but salicylate seems to have effects centrally on GABAergic neurotransmission [203, 204], as well as more peripherally by affecting cochlear function [200, 204]. Moreover, a strong linear relationship exists between unbound salicylate plasma concentration and a resultant decrease in auditory sensitivity [205], and the salicylate toxicity model is used by auditory scientists to investigate mechanisms underlying tinnitus [204].
Certain asthmatic patients have a sensitivity to ASA that manifests itself as a respiratory/asthma-type attack. Jenkins et al. performed a systematic review and found that the pooled incidence of ASA-induced asthma was 21 % in adults and 5 % in children [206]. This is higher than the value of approximately 10 % that has been published elsewhere [207, 208]. The mechanism of this reaction in ASA sensitive-individuals is thought to occur due to COX inhibition resulting in decreased PGE2 and thus unabated activation of the 5-lipoxygenase pathway. This, in turn, increases production of leukotrienes and mast cell release of histamine, leading to airway hyperreactivity [209, 210].
Prostaglandin-mediated vasodilation is necessary for proper renal plasma flow, especially in individuals with underlying renal disease, congestive heart failure, or cirrhosis. Through inhibition of renal COX-2, ASA and other NSAIDs can cause volume-dependent renal failure and that resulting from interstitial nephritis and nephritic syndrome [198].
Conclusion
Although ASA use is relatively common in the general population, ASA usage by MS patients has the potential for positive and/or negative influences on different facets of the disease, that is, symptoms, disease mechanisms, and associated disease risks. Understanding the impact of ASA use on these features would help to further establish the risk-to-benefit ratio of ASA usage in this patient population. Venous thrombosis and possibly stroke have an elevated likelihood in MS [17–23, 37], and given that ASA can lessen the risks of these cerebrovascular diseases [25, 26, 29], it is likely that ASA confers a similar benefit of lower risk for MS patients. Fatigue is a relatively common symptom in MS, and ASA may ameliorate fatigue in MS patients [176, 177], although the effect size might be small [178]. ASA could also impact pathogenic processes. For example, ASA could act to reduce inflammation by limiting the production of proinflammatory mediators from activated microglia [155–157] or by inducing the production of lipoxin A4, which acts to resolve inflammation [158, 159]. Since a pathogenic role has been attributed to platelets and thrombin [65, 71–73, 117, 118], lessening their activation by ASA could potentially reduce their ability to stimulate inflammation or impair blood flow [112, 116, 119]. Despite these potential benefits, ASA usage can have negative side effects such as being associated with an elevated risk of hemorrhagic stroke [30–32]. ASA may also worsen some specific components of MS pathology, for example, enhancing leakage of the BBB and possibly inhibiting mitochondrial complex I activity [33], which is already reduced in MS [34, 35]. It is possible that subgroups of MS patients may find particular benefit from ASA, for example, immobile patients with increased risk for DVTs or patients with APLAs, which could counterbalance the risks associated with ASA usage. It is also possible that ASA usage has a small beneficial impact on overall disease progression. Thus, further studies are needed to determine the benefits and risks of ASA in patients with MS in order to establish proper guidance for ASA use by this patient population. Given the widespread usage of aspirin and the likelihood that many effects could be small, traditional placebo controlled trials would be unlikely to yield meaningful results. Carefully crafted population-based studies, while not definitive, may help guide our understanding of this complex issue.
Abbreviations
- ACCP:
-
American College of Chest Physicians
- APLA:
-
antiphospholipid antibody
- APS:
-
antiphospholipid syndrome
- ASA:
-
aspirin
- BBB:
-
blood-brain barrier
- CNS:
-
central nervous system
- COX-1:
-
cyclooxygenase-1
- COX-2:
-
cyclooxygenase-2
- COXs:
-
cyclooxygenases
- CVD:
-
cardiovascular disease
- DMT:
-
disease modifying therapy
- DVT:
-
deep vein thrombosis
- EAE:
-
experimental autoimmune encephalomyelitis
- ER-DP:
-
extended-release dipyridamole
- GI:
-
gastrointestinal
- HIF-1α:
-
hypoxia-inducible factor-1α
- MFIS:
-
Modified Fatigue Impact Scale
- MS:
-
multiple sclerosis
- NAWM:
-
normal-appearing white matter
- OR:
-
odds ratio
- PE:
-
pulmonary embolism
- PEP:
-
Pulmonary Embolism Prevention (trial)
- PF4:
-
platelet factor 4
- PGE synthase:
-
prostaglandin-E synthase
- PGE2:
-
prostaglandin E2
- PGH2:
-
prostaglandin H2
- PGI2:
-
prostacyclin
- ROS:
-
reactive oxygen species
- RRMS:
-
relapsing remitting MS
- SSRI:
-
selective serotonin reuptake inhibitor
- SWI:
-
susceptibility-weighted imaging
- tNSAID:
-
traditional nonsteroidal anti-inflammatory drug
- TXA2:
-
thromboxane A2
- VTE:
-
venous thromboembolism
- β-TG:
-
β-thromboglobulin
References
Karussis D. The diagnosis of multiple sclerosis and the various related demyelinating syndromes: a critical review. J Autoimmun. 2014;48–49:134–42.
Kutzelnigg A, Lassmann H. Pathology of multiple sclerosis and related inflammatory demyelinating diseases. Handb Clin Neurol. 2014;122:15–58.
Neumann H. Molecular mechanisms of axonal damage in inflammatory central nervous system diseases. Curr Opin Neurol. 2003;16:267–73.
Lassmann H. Axonal and neuronal pathology in multiple sclerosis: what have we learnt from animal models. Exp Neurol. 2010;225:2–8.
Correale J. The role of microglial activation in disease progression. Mult Scler. 2014;20:1288–95.
Witte ME, Mahad DJ, Lassmann H, van Horssen J. Mitochondrial dysfunction contributes to neurodegeneration in multiple sclerosis. Trends Mol Med. 2014;20:179–87.
de Vries HE, Kooij G, Frenkel D, Georgopoulos S, Monsonego A, Janigro D. Inflammatory events at blood-brain barrier in neuroinflammatory and neurodegenerative disorders: implications for clinical disease. Epilepsia. 2012;53(s6):45–52.
Cramer SP, Simonsen H, Frederiksen JL, Rostrup E, Larsson HB. Abnormal blood-brain barrier permeability in normal appearing white matter in multiple sclerosis investigated by MRI. Neuroimage Clin. 2013;4:182–9.
Lycke J, Wikkelsö C, Bergh AC, Jacobsson L, Andersen O. Regional cerebral blood flow in multiple sclerosis measured by single photon emission tomography with technetium-99m hexamethylpropyleneamine oxime. Eur Neurol. 1993;33:163–7.
Rashid W, Parkes LM, Ingle GT, Chard DT, Toosy AT, Altmann DR, et al. Abnormalities of cerebral perfusion in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2004;75:1288–93.
Inglese M, Park SJ, Johnson G, Babb JS, Miles L, Jaggi H, et al. Deep gray matter perfusion in multiple sclerosis: dynamic susceptibility contrast perfusion magnetic resonance imaging at 3 T. Arch Neurol. 2007;64:196–202.
Debernard L, Melzer TR, Van Stockum S, Graham C, Wheeler-Kingshott CA, Dalrymple-Alford JC, et al. Reduced grey matter perfusion without volume loss in early relapsing-remitting multiple sclerosis. J Neurol Neurosurg Psychiatry. 2014;85:544–51.
Wuerfel J, Paul F, Zipp F. Cerebral blood perfusion changes in multiple sclerosis. J Neurol Sci. 2007;259:16–20.
Wakefield AJ, More LJ, Difford J, McLaughlin JE. Immunohistochemical study of vascular injury in acute multiple sclerosis. J Clin Pathol. 1994;47:129–33.
Adams CW. A color atlas of multiple sclerosis and other myelin disorders. Dobbs Ferry, NY: Sheridan House Inc.; 1989.
Mohan H, Krumbholz M, Sharma R, Eisele S, Junker A, Sixt M, et al. Extracellular matrix in multiple sclerosis lesions: fibrillar collagens, biglycan and decorin are upregulated and associated with infiltrating immune cells. Brain Pathol. 2010;20:966–75.
Christiansen CF, Christensen S, Farkas DK, Miret M, Sorensen HT, Pedersen L. Risk of arterial cardiovascular diseases in patients with multiple sclerosis: a population-based cohort study. Neuroepidemiology. 2010;35:267–74.
Jadidi E, Mohammadi M, Moradi T. High risk of cardiovascular diseases after diagnosis of multiple sclerosis. Mult Scler. 2013;19:1336–40.
Ramagopalan SV, Wotton CJ, Handel AE, Yeates D, Goldacre MJ. Risk of venous thromboembolism in people admitted to hospital with selected immune-mediated diseases: record-linkage study. BMC Med. 2011;9:1.
Christiansen CF. Risk of vascular disease in patients with multiple sclerosis: a review. Neurol Res. 2012;34:746–53.
Christensen S, Farkas DK, Pedersen L, Miret M, Christiansen CF, Sorensen HT. Multiple sclerosis and risk of venous thromboembolism: a population-based cohort study. Neuroepidemiology. 2012;38:76–83.
Zöller B, Li X, Sundquist J, Sundquist K. Risk of pulmonary embolism in patients with autoimmune disorders: a nationwide follow-up study from Sweden. Lancet. 2012;379:244–9.
Peeters PJ, Bazelier MT, Uitdehaag BM, Leufkens HG, De Bruin ML, de Vries F. The risk of venous thromboembolism in patients with multiple sclerosis: the Clinical Practice Research Datalink. J Thromb Haemost. 2014;12:444–51.
Lewis Jr HD, Davis JW, Archibald DG, Steinke WE, Smitherman TC, Doherty 3rd JE, et al. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study. N Engl J Med. 1983;309:396–403.
Guthrie R. Review and management of side effects associated with antiplatelet therapy for prevention of recurrent cerebrovascular events. Adv Ther. 2011;28:473–82.
Kirshner HS. Prevention of secondary stroke and transient ischaemic attack with antiplatelet therapy: the role of the primary care physician [corrected]. Int J Clin Pract. 2007;61:1739–48.
Becattini C, Agnelli G. Aspirin for prevention and treatment of venous thromboembolism. Blood Rev. 2014;28:103–8.
Simes J, Becattini C, Agnelli G. Aspirin for the prevention of recurrent venous thromboembolism: the INSPIRE collaboration. J Vasc Surg. 2014;60:1711.
Undas A, Brummel-Ziedins K, Mann KG. Why does aspirin decrease the risk of venous thromboembolism? On old and novel antithrombotic effects of acetyl salicylic acid. J Thromb Haemost. 2014;12:1776–87.
Cattaneo M. Haemorrhagic stroke during anti-platelet therapy. Eur J Anaesthesiol Suppl. 2008;42:12–5.
Antithrombotic Trialists’ (ATT) Collaboration, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–60.
Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Ngianga-Bakwin K, et al. Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials. PLoS One. 2013;8:e81970.
Sandoval-Acuña C, Lopez-Alarcón C, Aliaga ME, Speisky H. Inhibition of mitochondrial complex I by various non-steroidal anti-inflammatory drugs and its protection by quercetin via a coenzyme Q-like action. Chem Biol Interact. 2012;199:18–28.
Lu F, Selak M, O’Connor J, Croul S, Lorenzana C, Butunoi C, et al. Oxidative damage to mitochondrial DNA and activity of mitochondrial enzymes in chronic active lesions of multiple sclerosis. J Neurol Sci. 2000;177:95–103.
Dutta R, McDonough J, Yin X, Peterson J, Chang A, Torres T, et al. Mitochondrial dysfunction as a cause of axonal degeneration in multiple sclerosis patients. Ann Neurol. 2006;59:478–89.
Allen NB, Lichtman JH, Cohen HW, Fang J, Brass LM, Alderman MH. Vascular disease among hospitalized multiple sclerosis patients. Neuroepidemiology. 2008;30:234–8.
Zöller B, Li X, Sundquist J, Sundquist K. Risk of subsequent ischemic and hemorrhagic stroke in patients hospitalized for immune-mediated diseases: a nationwide follow-up study from Sweden. BMC Neurol. 2012;12:41.
Roshanisefat H, Bahmanyar S, Hillert J, Olsson T, Montgomery S. Multiple sclerosis clinical course and cardiovascular disease risk - Swedish cohort study. Eur J Neurol. 2014;21:1353–e88.
Ocak G, Vossen CY, Verduijn M, Dekker FW, Rosendaal FR, Cannegieter SC, et al. Risk of venous thrombosis in patients with major illnesses: results from the MEGA study. J Thromb Haemost. 2013;11:116–23.
Healy B, Levin E, Perrin K, Weatherall M, Beasley R. Prolonged work- and computer-related seated immobility and risk of venous thromboembolism. J R Soc Med. 2010;103:447–54.
Shah SM, Shah SM, Khan S, Rehman SU, Khan ZA, Ahmed W, et al. “Addressing the impact of stroke risk factors in a case control study in tertiary care hospitals”: a case control study in Tertiary Care Hospitals of Peshawar, Khyber Phukhtoonkhwa (KPK) Pakistan. BMC Res Notes. 2013;6:268.
Stuifbergen AK. Physical activity and perceived health status in persons with multiple sclerosis. J Neurosci Nurs. 1997;29:238–43.
Koch-Henriksen N, Brønnum-Hansen H, Stenager E. Underlying cause of death in Danish patients with multiple sclerosis: results from the Danish Multiple Sclerosis Registry. J Neurol Neurosurg Psychiatry. 1998;65:56–9.
Arpaia G, Bavera PM, Caputo D, Mendozzi L, Cavarretta R, Agus GB, et al. Risk of deep venous thrombosis (DVT) in bedridden or wheelchair-bound multiple sclerosis patients: a prospective study. Thromb Res. 2010;125:315–7.
Kappus N, Weinstock-Guttman B, Hagemeier J, Kennedy C, Melia R, Carl E, et al. Cardiovascular risk factors are associated with increased lesion burden and brain atrophy in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2015. doi: 10.1136/jnnp-2014-310051. [Epub ahead of print].
Sternberg Z, Leung C, Sternberg D, Yu J, Hojnacki D. Disease modifying therapies modulate cardiovascular risk factors in patients with multiple sclerosis. Cardiovasc Ther. 2014;32:33–9.
Canadian Agency for Drugs and Technologies in Health. CADTH Common Drug Review. CDR Clinical Review Report for Aubagio [Internet]. Ottawa: The Agency; 2014. Oct [cited 2015 May 15]. https://www.cadth.ca/media/cdr/clinical/SR0350_Aubagio_CL_Report_e.pdf.
Gold R, Comi G, Palace J, Siever A, Gottschalk R, Bijarnia M, et al. Assessment of cardiac safety during fingolimod treatment initiation in a real-world relapsing multiple sclerosis population: a phase 3b, open-label study. J Neurol. 2014;261:267–76.
Paolicelli D, Manni A, Direnzo V, D’Onghia M, Tortorella C, Zoccolella S, Trojano M. Long term cardiac safety and tolerability of fingolimod in multiple sclerosis: a post-marketing study. J Clin Pharmacol 2015. doi:10.1002/jcph.519. [Epub ahead of print].
Brønnum-Hansen H, Koch-Henriksen N, Stenager E. Trends in survival and cause of death in Danish patients with multiple sclerosis. Brain. 2004;127:844–50.
Hirst C, Swingler R, Compston DA, Ben-Shlomo Y, Robertson NP. Survival and cause of death in multiple sclerosis: a prospective population-based study. J Neurol Neurosurg Psychiatry. 2008;79:1016–21.
Grundy SM, Hansen B, Smith Jr SC, Cleeman JI, Kahn RA, American Heart Association; National Heart, Lung, and Blood Institute; American Diabetes Association. Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Arterioscler Thromb Vasc Biol. 2004;24:e19–24.
Wens I, Dalgas U, Deckx N, Cools N, Eijnde B. Does multiple sclerosis affect glucose tolerance? Mult Scler. 2013;20:1273–6.
Mähler A, Steiniger J, Bock M, Brandt AU, Haas V, Boschmann M, et al. Is metabolic flexibility altered in multiple sclerosis patients? PLoS One. 2012;7:e43675.
Wens I, Dalgas U, Stenager E, Eijnde BO. Risk factors related to cardiovascular diseases and the metabolic syndrome in multiple sclerosis - a systematic review. Mult Scler. 2013;19:1556–64.
Mathur D, López-Rodas G, Casanova B, Marti MB. Perturbed glucose metabolism: insights into multiple sclerosis pathogenesis. Front Neurol. 2014;5:250.
Patrono C, García Rodríguez LA, Landolfi R, Baigent C. Low-dose aspirin for the prevention of atherothrombosis. N Engl J Med. 2005;353:2373–83.
Patrono C, Baigent C. Low-dose aspirin, coxibs, and other NSAIDS: a clinical mosaic emerges. Mol Interv. 2009;9:31–9.
Grosser T, Smyth E, FitzGerald G. Anti-inflammatory, antipyretic, and analgesic agents; pharmacotherapy of gout. In: Brunton L, Chabner B, Knollmann B, editors. Goodman and Gilman’s pharmacological basis of therapeutics, 12E. New York, NY: The McGraw-Hill Companies; 2011.
Roth GJ, Stanford N, Majerus PW. Acetylation of prostaglandin synthase by aspirin. Proc Natl Acad Sci U S A. 1975;72:3073–6.
Stanford N, Roth GJ, Shen TY, Majerus PW. Lack of covalent modification of prostaglandin synthetase (cyclo-oxygenase) by indomethacin. Prostaglandins. 1977;13:669–75.
Smith W, Garavito R, DeWitt D. Prostaglandin endoperoxide H synthases (cyclooxygenases)-1 and -2. J Biol Chem. 1996;271:33157–60.
McAdam B, Mardini I, Habib A, Burke A, Lawson J, Kapoor S, et al. Effect of regulated expression of human cyclooxygenase isoforms on eicosanoid and isoeicosanoid production in inflammation. J Clin Invest. 2000;105:1473–82.
Warner TD, Nylander S, Whatling C. Anti-platelet therapy: cyclo-oxygenase inhibition and the use of aspirin with particular regard to dual anti-platelet therapy. Br J Clin Pharmacol. 2011;72:619–33.
Langer HF, Chavakis T. Platelets and neurovascular inflammation. Thromb Haemost. 2013;110:888–93.
Dubois RN, Abramson SB, Crofford L, Gupta RA, Simon LS, Van De Putte LB, et al. Cyclooxygenase in biology and disease. FASEB J. 1998;12:1063–73.
Vane J, Bakhle Y, Botting R. Cyclooxygenases 1 and 2. Ann Rev Pharmacol Toxicol. 1998;38:97–120.
Angiolillo D, Ueno M, Goto S. Basic principles of platelet biology and clinical implications. Circ J. 2010;74:597–607.
Gleim S, Stitham J, Tang WH, Martin KA, Hwa J. An eicosanoid-centric view of atherothrombotic risk factors. Cell Mol Life Sci. 2012;69:3361–80.
Stokes KY, Granger DN. Platelets: a critical link between inflammation and microvascular dysfunction. J Physiol. 2012;590:1023–34.
Horstman LL, Jy W, Ahn YS, Zivadinov R, Maghzi AH, Etemadifar M, et al. Role of platelets in neuroinflammation: a wide-angle perspective. J Neuroinflammation. 2010;7:10.
Sheremata W, Jy W, Horstman LL, Ahn YS, Alexander JS, Minagar A. Evidence of platelet activation in multiple sclerosis. J Neuroinflammation. 2008;5:27.
Langer HF, Choi EY, Zhou H, Schleicher R, Chung KJ, Tang Z, et al. Platelets contribute to the pathogenesis of experimental autoimmune encephalomyelitis. Circ Res. 2012;110:1202–10.
Guyatt G, Akl E, Crowther M, Gutterman D, Schünemann H. Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:7S–47.
Ajani UA, Ford ES, Greenland KJ, Giles WH, Mokdad AH. Aspirin use among U.S. adults: Behavioral Risk Factor Surveillance System. Am J Prev Med. 2006;30:74–7.
Pignone M, Anderson GK, Binns K, Tilson HH, Weisman SM. Aspirin use among adults aged 40 and older in the United States: results of a national survey. Am J Prev Med. 2007;32:403–7.
VanWormer JJ, Greenlee RT, McBride PE, Peppard PE, Malecki KC, Che J, et al. Aspirin for primary prevention of CVD: are the right people using it? J Fam Pract. 2012;61:525–32.
Zhou Y, Boudreau DM, Freedman AN. Trends in the use of aspirin and nonsteroidal anti-inflammatory drugs in the general U.S. population. Pharmacoepidemiol Drug Saf. 2014;23:43–50.
Sandercock PA, Counsell C, Tseng MC, Cecconi E. Oral antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev. 2014;3:CD000029.
Vande Griend JP, Saseen JJ. Combination antiplatelet agents for secondary prevention of ischemic stroke. Pharmacotherapy. 2008;28:1233–42.
Simmons BB, Gadegbeku AB, Cirignano B. Transient ischemic attack: Part II. Risk factor modification and treatment. Am Fam Physician. 2012;86:527–32.
Jamieson DG, Parekh A, Ezekowitz MD. Review of antiplatelet therapy in secondary prevention of cerebrovascular events: a need for direct comparisons between antiplatelet agents. J Cardiovasc Pharmacol Ther. 2005;10:153–61.
Chaturvedi S. Acetylsalicylic acid + extended-release dipyridamole combination therapy for secondary stroke prevention. Clin Ther. 2008;30:1196–205.
Hennekens CH. Aspirin in the treatment and prevention of cardiovascular disease: current perspectives and future directions. Curr Atheroscler Rep. 2007;9:409–16.
Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the Longitudinal Investigation of Thromboembolism Etiology. Arch Intern Med. 2002;162:1182–9.
PEP Trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295–302.
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86.
Stewart DW, Freshour JE. Aspirin for the prophylaxis of venous thromboembolic events in orthopedic surgery patients: a comparison of the AAOS and ACCP guidelines with review of the evidence. Ann Pharmacother. 2013;47:63–74.
Putnam TJ, Adler A. Vascular architecture of the lesions of multiple sclerosis. Arch Neurol Psychiatr. 1937;58:1–15.
Dow RS, Berglund G. Vascular pattern of lesions of multiple sclerosis. Arch Neurol Psych. 1942;47:1–18.
Scheinker H. Histogenesis of the early lesions of multiple sclerosis. I. Significance of vascular changes. Arch Neurol Psych. 1943;49:178–85.
Law M, Saindane AM, Ge Y, Babb JS, Johnson G, Mannon LJ, et al. Microvascular abnormality in relapsing-remitting multiple sclerosis: perfusion MR imaging findings in normal-appearing white matter. Radiology. 2004;231:645–52.
Alvarez-Guerra M, Hannaert P, Hider H, Chiavaroli C, Garay RP. Vascular permeabilization by intravenous arachidonate in the rat peritoneal cavity: antagonism by antioxidants. Eur J Pharmacol. 2003;466:199–205.
Serhan CN, Takano T, Chiang N, Gronert K, Clish CB. Formation of endogenous “antiinflammatory” lipid mediators by transcellular biosynthesis. Lipoxins and aspirin-triggered lipoxins inhibit neutrophil recruitment and vascular permeability. Am J Respir Crit Care Med. 2000;161:S95–101.
Dankbaar JW, Hom J, Schneider T, Cheng SC, Lau BC, van der Schaaf I, et al. Age- and anatomy-related values of blood-brain barrier permeability measured by perfusion-CT in non-stroke patients. J Neuroradiol. 2009;36:219–27.
Chapman J. The interface of multiple sclerosis and antiphospholipid antibodies. Thromb Res. 2004;114:477–81.
Bidot CJ, Horstman LL, Jy W, Jimenez JJ, Bidot Jr C, Ahn YS, et al. Clinical and neuroimaging correlates of antiphospholipid antibodies in multiple sclerosis: a preliminary study. BMC Neurol. 2007;7:36.
Garg N, Zivadinov R, Ramanathan M, Vasiliu I, Locke J, Watts K, et al. Clinical and MRI correlates of autoreactive antibodies in multiple sclerosis patients. J Neuroimmunol. 2007;187:159–65.
Mayer M, Cerovec M, Rados M, Cikes N. Antiphospholipid syndrome and central nervous system. Clin Neurol Neurosurg. 2010;112:602–8.
Horstman LL, Jy W, Bidot CJ, Ahn YS, Kelley RE, Zivadinov R, et al. Antiphospholipid antibodies: paradigm in transition. J Neuroinflammation. 2009;6:3.
Stosic M, Ambrus J, Garg N, Weinstock-Guttman B, Ramanathan M, Kalman B, et al. MRI characteristics of patients with antiphospholipid syndrome and multiple sclerosis. J Neurol. 2010;257:63–71.
Zivadinov R, Ramanathan M, Ambrus J, Hussein S, Ramasamy DP, Dwyer MG, et al. Anti-phospholipid antibodies are associated with response to interferon-beta1a treatment in MS: results from a 3-year longitudinal study. Neurol Res. 2012;34:761–9.
Garg N, Weinstock-Guttman B, Bhasi K, Locke J, Ramanathan M. An association between autoreactive antibodies and anti-interferon-beta antibodies in multiple sclerosis. Mult Scler. 2007;13:895–9.
Szmyrka-Kaczmarek M, Pokryszko-Dragan A, Pawlik B, Gruszka E, Korman L, Podemski R, et al. Antinuclear and antiphospholipid antibodies in patients with multiple sclerosis. Lupus. 2012;21:412–20.
Puente D, Pombo G, Forastiero R. Current management of antiphospholipid syndrome-related thrombosis. Expert Rev Cardiovasc Ther. 2009;7:1551–8.
Erkan D, Harrison MJ, Levy R, Peterson M, Petri M, Sammaritano L, et al. Aspirin for primary thrombosis prevention in the antiphospholipid syndrome: a randomized, double-blind, placebo-controlled trial in asymptomatic antiphospholipid antibody-positive individuals. Arthritis Rheum. 2007;56:2382–91.
Arnaud L, Mathian A, Devilliers H, Ruffatti A, Tektonidou M, Forastiero R, et al. Patient-level analysis of five international cohorts further confirms the efficacy of aspirin for the primary prevention of thrombosis in patients with antiphospholipid antibodies. Autoimmun Rev. 2015;14:192–200.
Ganesh A, Stahnisch FW. On the historical succession of vessel-based therapies in the treatment of multiple sclerosis. Eur Neurol. 2013;70:48–58.
Claudio L, Raine CS, Brosnan CF. Evidence of persistent blood-brain barrier abnormalities in chronic-progressive multiple sclerosis. Acta Neuropathol. 1995;90:228–38.
Han MH, Hwang SI, Roy DB, Lundgren DH, Price JV, Ousman SS, et al. Proteomic analysis of active multiple sclerosis lesions reveals therapeutic targets. Nature. 2008;451:1076–81.
Cananzi AR, Ferro-Milone F, Grigoletto F, Toldo M, Meneghini F, Bortolon F, et al. Relevance of platelet factor four (PF4) plasma levels in multiple sclerosis. Acta Neurol Scand. 1987;76:79–85.
Furuno T, Yamasaki F, Yokoyama T, Sato K, Sato T, Doi Y, et al. Effects of various doses of aspirin on platelet activity and endothelial function. Heart Vessels. 2011;26:267–73.
Davalos D, Ryu JK, Merlini M, Baeten KM, Le Moan N, Petersen MA, et al. Fibrinogen-induced perivascular microglial clustering is required for the development of axonal damage in neuroinflammation. Nat Commun. 2012;3:1227.
Akassoglou K, Adams RA, Bauer J, Mercado P, Tseveleki V, Lassmann H, et al. Fibrin depletion decreases inflammation and delays the onset of demyelination in a tumor necrosis factor transgenic mouse model for multiple sclerosis. Proc Natl Acad Sci U S A. 2004;101:6698–703.
Yang Y, Tian SJ, Wu L, Huang DH, Wu WP. Fibrinogen depleting agent batroxobin has a beneficial effect on experimental autoimmune encephalomyelitis. Cell Mol Neurobiol. 2011;31:437–48.
Undas A, Brummel-Ziedins KE, Mann KG. Antithrombotic properties of aspirin and resistance to aspirin: beyond strictly antiplatelet actions. Blood. 2007;109:2285–92.
Chapman J. Coagulation in inflammatory diseases of the central nervous system. Semin Thromb Hemost. 2013;39:876–80.
Davalos D, Baeten KM, Whitney MA, Mullins ES, Friedman B, Olson ES, et al. Early detection of thrombin activity in neuroinflammatory disease. Ann Neurol. 2014;75:303–8.
Undas A, Brummel K, Musial J, Mann KG, Szczeklik A. Blood coagulation at the site of microvascular injury: effects of low-dose aspirin. Blood. 2001;98:2423–31.
Tanne D, Katzav A, Beilin O, Grigoriadis NC, Blank M, Pick CG, et al. Interaction of inflammation, thrombosis, aspirin and enoxaparin in CNS experimental antiphospholipid syndrome. Neurobiol Dis. 2008;30:56–64.
Sinnecker T, Bozin I, Dörr J, Pfueller CF, Harms L, Niendorf T, et al. Periventricular venous density in multiple sclerosis is inversely associated with T2 lesion count: a 7 Tesla MRI study. Mult Scler. 2013;19:316–25.
Ge Y, Law M, Johnson G, Herbert J, Babb JS, Mannon LJ, et al. Dynamic susceptibility contrast perfusion MR imaging of multiple sclerosis lesions: characterizing hemodynamic impairment and inflammatory activity. AJNR Am J Neuroradiol. 2005;26:1539–47.
Amann M, Achtnichts L, Hirsch JG, Naegelin Y, Gregori J, Weier K, et al. 3D GRASE arterial spin labelling reveals an inverse correlation of cortical perfusion with the white matter lesion volume in MS. Mult Scler. 2012;18:1570–6.
Juhler M, Paulson OB. Regional cerebral blood flow in acute experimental allergic encephalomyelitis. Brain Res. 1986;363:272–8.
Williams R, Rohr AM, Wang WT, Choi IY, Lee P, Berman NE, et al. Iron deposition is independent of cellular inflammation in a cerebral model of multiple sclerosis. BMC Neurosci. 2011;12:59.
Brooks DJ, Leenders KL, Head G, Marshall J, Legg NJ, Jones T. Studies on regional cerebral oxygen utilisation and cognitive function in multiple sclerosis. J Neurol Neurosurg Psychiatry. 1984;47:1182–91.
Ge Y, Zohrabian VM, Osa EO, Xu J, Jaggi H, Herbert J, et al. Diminished visibility of cerebral venous vasculature in multiple sclerosis by susceptibility-weighted imaging at 3.0 Tesla. J Magn Reson Imaging. 2009;29:1190–4.
Ge Y, Zhang Z, Lu H, Tang L, Jaggi H, Herbert J, et al. Characterizing brain oxygen metabolism in patients with multiple sclerosis with T2-relaxation-under-spin-tagging MRI. J Cereb Blood Flow Metab. 2012;32:403–12.
Nathoo N, Agrawal S, Wu Y, Haylock-Jacobs S, Yong VW, Foniok T, et al. Susceptibility-weighted imaging in the experimental autoimmune encephalomyelitis model of multiple sclerosis indicates elevated deoxyhemoglobin, iron deposition and demyelination. Mult Scler. 2013;19:721–31.
Aboul-Enein F, Rauschka H, Kornek B, Stadelmann C, Stefferl A, Brück W, et al. Preferential loss of myelin-associated glycoprotein reflects hypoxia-like white matter damage in stroke and inflammatory brain diseases. J Neuropathol Exp Neurol. 2003;62:25–33.
Lassmann H. Hypoxia-like tissue injury as a component of multiple sclerosis lesions. J Neurol Sci. 2003;206:187–91.
Graumann U, Reynolds R, Steck AJ, Schaeren-Wiemers N. Molecular changes in normal appearing white matter in multiple sclerosis are characteristic of neuroprotective mechanisms against hypoxic insult. Brain Pathol. 2003;13:554–73.
Mháille AN, McQuaid S, Windebank A, Cunnea P, McMahon J, Samali A, et al. Increased expression of endoplasmic reticulum stress-related signaling pathway molecules in multiple sclerosis lesions. J Neuropathol Exp Neurol. 2008;67:200–11.
Cunnea P, Mháille AN, McQuaid S, Farrell M, McMahon J, FitzGerald U. Expression profiles of endoplasmic reticulum stress-related molecules in demyelinating lesions and multiple sclerosis. Mult Scler. 2011;17:808–18.
McMahon JM, McQuaid S, Reynolds R, FitzGerald UF. Increased expression of ER stress- and hypoxia-associated molecules in grey matter lesions in multiple sclerosis. Mult Scler. 2012;18:1437–47.
Paling D, Golay X, Wheeler-Kingshott C, Kapoor R, Miller D. Energy failure in multiple sclerosis and its investigation using MR techniques. J Neurol. 2011;258:2113–27.
Aboul-Enein F, Lassmann H. Mitochondrial damage and histotoxic hypoxia: a pathway of tissue injury in inflammatory brain disease? Acta Neuropathol. 2005;109:49–55.
Mahad D, Lassmann H, Turnbull D. Review: Mitochondria and disease progression in multiple sclerosis. Neuropathol Appl Neurobiol. 2008;34:577–89.
Campbell GR, Mahad DJ. Mitochondrial changes associated with demyelination: consequences for axonal integrity. Mitochondrion. 2012;12:173–9.
Raza H, John A. Implications of altered glutathione metabolism in aspirin-induced oxidative stress and mitochondrial dysfunction in HepG2 cells. PLoS One. 2012;7:e36325.
Srinivasan R, Ratiney H, Hammond-Rosenbluth KE, Pelletier D, Nelson SJ. MR spectroscopic imaging of glutathione in the white and gray matter at 7 T with an application to multiple sclerosis. Magn Reson Imaging. 2010;28:163–70.
Choi IY, Lee SP, Denney DR, Lynch SG. Lower levels of glutathione in the brains of secondary progressive multiple sclerosis patients measured by 1H magnetic resonance chemical shift imaging at 3 T. Mult Scler. 2011;17:289–96.
Hirst J, King MS, Pryde KR. The production of reactive oxygen species by complex I. Biochem Soc Trans. 2008;36:976–80.
Marshall O, Lu H, Brisset JC, Xu F, Liu P, Herbert J, et al. Impaired cerebrovascular reactivity in multiple sclerosis. JAMA Neurol. 2014;71:1275–81.
Schröder H. Nitric oxide and aspirin: a new mediator for an old drug. Am J Ther. 2009;16:17–23.
Kabirian F, Amoabediny G, Haghighipour N, Salehi-Nik N, Zandieh-Doulabi B. Nitric oxide secretion by endothelial cells in response to fluid shear stress, aspirin, and temperature. J Biomed Mater Res A. 2015;103:1231–7.
Miller H, Newell DJ, Ridley A. Multiple Sclerosis. Trials of maintenance treatment with prednisolone and soluble aspirin. Lancet. 1961;1:127–9.
Miller HG, Foster JB, Newell DJ, Barwick DD, Brewis RA. Multiple sclerosis: therapeutic trials of chloroquine, soluble aspirin, and gammaglobulin. Br Med J. 1963;2:1436–9.
Good RA, Campbell B, Good TA. Prophylactic and therapeutic effect of para-aminobenzoic acid and sodium salicylate on experimental allergic encephalomyelitis. Proc Soc Exp Biol Med. 1949;72:341–7.
Kolb LC, Karlson AG, Sayre GP. Prevention of experimental allergic encephalomyelitis by various agents. Trans Am Neurol Assoc. 1952;56:117–21.
Weston PG, Johnston PV. Incidence and severity of experimental allergic encephalomyelitis and cerebral prostaglandin synthesis in essential fatty acid deficient and aspirin-treated rats. Lipids. 1978;13:867–72.
Moon C, Ahn M, Jee Y, Heo S, Kim S, Kim H, et al. Sodium salicylate-induced amelioration of experimental autoimmune encephalomyelitis in Lewis rats is associated with the suppression of inducible nitric oxide synthase and cyclooxygenases. Neurosci Lett. 2004;356:123–6.
Marusic S, Thakker P, Pelker JW, Stedman NL, Lee KL, McKew JC, et al. Blockade of cytosolic phospholipase A2 alpha prevents experimental autoimmune encephalomyelitis and diminishes development of Th1 and Th17 responses. J Neuroimmunol. 2008;204:29–37.
Miyamoto K, Miyake S, Mizuno M, Oka N, Kusunoki S, Yamamura T. Selective COX-2 inhibitor celecoxib prevents experimental autoimmune encephalomyelitis through COX-2-independent pathway. Brain. 2006;129:1984–92.
Wang YP, Wu Y, Li LY, Zheng J, Liu RG, Zhou JP, et al. Aspirin-triggered lipoxin A4 attenuates LPS-induced pro-inflammatory responses by inhibiting activation of NF-κB and MAPKs in BV-2 microglial cells. J Neuroinflammation. 2011;8:95.
Wu Y, Zhai H, Wang Y, Li L, Wu J, Wang F, et al. Aspirin-triggered lipoxin A4 attenuates lipopolysaccharide-induced intracellular ROS in BV2 microglia cells by inhibiting the function of NADPH oxidase. Neurochem Res. 2012;37:1690–6.
Wang Z, Huang W, Zuo Z. Perioperative aspirin improves neurological outcome after focal brain ischemia possibly via inhibition of Notch 1 in rat. J Neuroinflammation. 2014;11:56.
Prüss H, Rosche B, Sullivan AB, Brommer B, Wengert O, Gronert K, et al. Proresolution lipid mediators in multiple sclerosis - differential, disease severity-dependent synthesis - a clinical pilot trial. PLoS One. 2013;8:e55859.
Schwab JM, Serhan CN. Lipoxins and new lipid mediators in the resolution of inflammation. Curr Opin Pharmacol. 2006;6:414–20.
Ishizuka T, Niwa A, Tabuchi M, Ooshima K, Higashino H. Acetylsalicylic acid provides cerebrovascular protection from oxidant damage in salt-loaded stroke-prone rats. Life Sci. 2008;82:806–15.
Modi KK, Sendtner M, Pahan K. Up-regulation of ciliary neurotrophic factor in astrocytes by aspirin: implications for remyelination in multiple sclerosis. J Biol Chem. 2013;288:18533–45.
Stankoff B, Aigrot MS, Noël F, Wattilliaux A, Zalc B, Lubetzki C. Ciliary neurotrophic factor (CNTF) enhances myelin formation: a novel role for CNTF and CNTF-related molecules. J Neurosci. 2002;22:9221–7.
Chen J, Zuo S, Wang J, Huang J, Zhang X, Liu Y, et al. Aspirin promotes oligodendrocyte precursor cell proliferation and differentiation after white matter lesion. Front Aging Neurosci. 2014;6:7.
Sumowski JF, Leavitt VM. Body temperature is elevated and linked to fatigue in relapsing-remitting multiple sclerosis, even without heat exposure. Arch Phys Med Rehabil. 2014;95:1298–302.
Nagaraj K, Taly AB, Gupta A, Prasad C, Christopher R. Depression and sleep disturbances in patients with multiple sclerosis and correlation with associated fatigue. J Neurosci Rural Pract. 2013;4:387–91.
Veauthier C, Paul F. Sleep disorders in multiple sclerosis and their relationship to fatigue. Sleep Med. 2014;15:5–14.
Heesen C, Nawrath L, Reich C, Bauer N, Schulz KH, Gold SM. Fatigue in multiple sclerosis: an example of cytokine mediated sickness behaviour? J Neurol Neurosurg Psychiatry. 2006;77:34–9.
Roelcke U, Kappos L, Lechner-Scott J, Brunnschweiler H, Huber S, Ammann W, et al. Reduced glucose metabolism in the frontal cortex and basal ganglia of multiple sclerosis patients with fatigue: a 18Ffluorodeoxyglucose positron emission tomography study. Neurology. 1997;48:1566–71.
Calabrese M, Rinaldi F, Grossi P, Mattisi I, Bernardi V, Favaretto A, et al. Basal ganglia and frontal/parietal cortical atrophy is associated with fatigue in relapsing-remitting multiple sclerosis. Mult Scler. 2010;16:1220–8.
Finke C, Schlichting J, Papazoglou S, Scheel M, Freing A, Soemmer C, et al. Altered basal ganglia functional connectivity in multiple sclerosis patients with fatigue. Mult Scler. 2014. [Epub ahead of print].
Schwid SR, Murray TJ. Treating fatigue in patients with MS: one step forward, one step back. Neurology. 2005;64:1111–2.
Côté I, Trojan DA, Kaminska M, Cardoso M, Benedetti A, Weiss D, et al. Impact of sleep disorder treatment on fatigue in multiple sclerosis. Mult Scler. 2013;19:480–9.
Veauthier C, Gaede G, Radbruch H, Gottschalk S, Wernecke KD, Paul F. Treatment of sleep disorders may improve fatigue in multiple sclerosis. Clin Neurol Neurosurg. 2013;115:1826–30.
Carter A, Daley A, Humphreys L, Snowdon N, Woodroofe N, Petty J, et al. Pragmatic intervention for increasing self-directed exercise behaviour and improving important health outcomes in people with multiple sclerosis: a randomised controlled trial. Mult Scler. 2014;20:1112–22.
Achiron A, Givon U, Magalashvili D, Dolev M, Liraz Zaltzman S, Kalron A, et al. Effect of Alfacalcidol on multiple sclerosis-related fatigue: a randomized, double-blind placebo-controlled study. Mult Scler. 2015;21:767–75.
Wingerchuk DM, Benarroch EE, O’Brien PC, Keegan BM, Lucchinetti CF, Noseworthy JH, et al. A randomized controlled crossover trial of aspirin for fatigue in multiple sclerosis. Neurology. 2005;64:1267–9.
Shaygannejad V, Janghorbani M, Ashtari F, Zakeri H. Comparison of the effect of aspirin and amantadine for the treatment of fatigue in multiple sclerosis: a randomized, blinded, crossover study. Neurol Res. 2012;34:854–8.
Wingerchuk D, Keegan M, Shuster E, Carter J, Hentz J, Thaera G, et al. Aspirin is unlikely to have a clinically meaningful effect on multiple sclerosis-related fatigue: data from a randomized controlled trial (P7.245). Neurol. 2014;82:P7.245.
Comi G, Leocani L, Rossi P, Colombo B. Physiopathology and treatment of fatigue in multiple sclerosis. J Neurol. 2001;248:174–9.
Koch MW, Patten S, Berzins S, Zhornitsky S, Greenfield J, Wall W, et al. Depression in multiple sclerosis: a long-term longitudinal study. Mult Scler. 2015;21:76–82.
Berk M, Dean O, Drexhage H, McNeil JJ, Moylan S, O’Neil A, et al. Aspirin: a review of its neurobiological properties and therapeutic potential for mental illness. BMC Med. 2013;11:74.
Pasco JA, Jacka FN, Williams LJ, Henry MJ, Nicholson GC, Kotowicz MA, et al. Clinical implications of the cytokine hypothesis of depression: the association between use of statins and aspirin and the risk of major depression. Psychother Psychosom. 2010;79:323–5.
Sarkar S, Chadda RK, Kumar N, Narang R. Anxiety and depression in patients with myocardial infarction: findings from a centre in India. Gen Hosp Psychiatry. 2012;34:160–6.
Ketterer MW, Brymer J, Rhoads K, Kraft P, Lovallo WR. Is aspirin, as used for antithrombosis, an emotion-modulating agent? J Psychosom Res. 1996;40:53–8.
Guan XT, Shao F, Xie X, Chen L, Wang W. Effects of aspirin on immobile behavior and endocrine and immune changes in the forced swimming test: comparison to fluoxetine and imipramine. Pharmacol Biochem Behav. 2014;124:361–6.
Mendlewicz J, Kriwin P, Oswald P, Souery D, Alboni S, Brunello N. Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int Clin Psychopharmacol. 2006;21:227–31.
Brunello N, Alboni S, Capone G, Benatti C, Blom JM, Tascedda F, et al. Acetylsalicylic acid accelerates the antidepressant effect of fluoxetine in the chronic escape deficit model of depression. Int Clin Psychopharmacol. 2006;21:219–25.
Wang Y, Yang F, Liu YF, Gao F, Jiang W. Acetylsalicylic acid as an augmentation agent in fluoxetine treatment resistant depressive rats. Neurosci Lett. 2011;499:74–9.
Ghanizadeh A, Hedayati A. Augmentation of citalopram with aspirin for treating major depressive disorder, a double blind randomized placebo controlled clinical trial. Antiinflamm Antiallergy Agents Med Chem. 2014;13:108–11.
Warner-Schmidt JL, Vanover KE, Chen EY, Marshall JJ, Greengard P. Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans. Proc Natl Acad Sci U S A. 2011;108:9262–7.
Labos C, Dasgupta K, Nedjar H, Turecki G, Rahme E. Risk of bleeding associated with combined use of selective serotonin reuptake inhibitors and antiplatelet therapy following acute myocardial infarction. CMAJ. 2011;183:1835–43.
Adams CW. Perivascular iron deposition and other vascular damage in multiple sclerosis. J Neurol Neurosurg Psychiatry. 1988;51:260–5.
Bagnato F, Hametner S, Yao B, van Gelderen P, Merkle H, Cantor FK, et al. Tracking iron in multiple sclerosis: a combined imaging and histopathological study at 7 Tesla. Brain. 2011;134:3602–15.
Mehta V, Pei W, Yang G, Li S, Swamy E, Boster A, et al. Iron is a sensitive biomarker for inflammation in multiple sclerosis lesions. PLoS One. 2013;8:e57573.
Bamm VV, Harauz G. Hemoglobin as a source of iron overload in multiple sclerosis: does multiple sclerosis share risk factors with vascular disorders? Cell Mol Life Sci. 2014;71:1789–98.
Segal JB, Powe NR. Prevalence of immune thrombocytopenia: analyses of administrative data. J Thromb Haemost. 2006;4:2377–83.
Kessler CM. Immune thrombocytopenic purpura treatment & management. Medscape 2014. http://emedicine.medscape.com/article/202158-treatment. Accessed 8 Jan 2015.
Risser A, Donovan D, Heintzman J, Page T. NSAID prescribing precautions. Am Fam Physician. 2009;80:1371–8.
Myers EN, Bernstein JM. Salicylate ototoxicity; a clinical and experimental study. Arch Otolaryngol. 1965;82:483–93.
Cazals Y. Auditory sensori-neural alterations induced by salicylate. Prog Neurobiol. 2000;62:583–631.
Lobarinas E, Sun W, Cushing R, Salvi R. A novel behavioral paradigm for assessing tinnitus using schedule-induced polydipsia avoidance conditioning (SIP-AC). Hear Res. 2004;190:109–14.
Cianfrone G, Pentangelo D, Cianfrone F, Mazzei F, Turchetta R, Orlando MP, et al. Pharmacological drugs inducing ototoxicity, vestibular symptoms and tinnitus: a reasoned and updated guide. Eur Rev Med Pharmacol Sci. 2011;15:601–36.
Sheppard A, Hayes SH, Chen GD, Ralli M, Salvi R. Review of salicylate-induced hearing loss, neurotoxicity, tinnitus and neuropathophysiology. Acta Otorhinolaryngol Ital. 2014;34:79–93.
Stolzberg D, Salvi RJ, Allman BL. Salicylate toxicity model of tinnitus. Front Syst Neurosci. 2012;6:28.
Day RO, Graham GG, Bieri D, Brown M, Cairns D, Harris G, et al. Concentration-response relationships for salicylate-induced ototoxicity in normal volunteers. Br J Clin Pharmacol. 1989;28:695–702.
Jenkins C, Costello J, Hodge L. Systematic review of prevalence of aspirin induced asthma and its implications for clinical practice. BMJ. 2004;328:434.
Vally H, Taylor ML, Thompson PJ. The prevalence of aspirin intolerant asthma (AIA) in Australian asthmatic patients. Thorax. 2002;57:569–74.
Levy S, Volans G. The use of analgesics in patients with asthma. Drug Saf. 2001;24:829–41.
Szczeklik A, Stevenson DD. Aspirin-induced asthma: advances in pathogenesis, diagnosis, and management. J Allergy Clin Immunol. 2003;111:913–21.
Gollapudi RR, Teirstein PS, Stevenson DD, Simon RA. Aspirin sensitivity: implications for patients with coronary artery disease. JAMA. 2004;292:3017–23.
Lider O, Baharav E, Mekori YA, Miller T, Naparstek Y, Vlodavsky I, et al. Suppression of experimental autoimmune diseases and prolongation of allograft survival by treatment of animals with low doses of heparins. J Clin Invest. 1989;83:752–6.
Olsen JA, Akirav EM. Remyelination in multiple sclerosis: cellular mechanisms and novel therapeutic approaches. J Neurosci Res. 2015;93:687–96.
Curhan SG, Eavey R, Shargorodsky J, Curhan GC. Analgesic use and the risk of hearing loss in men. Am J Med. 2010;123:231–7.
Acknowledgements
This work was supported by the National Multiple Sclerosis Society (NMSS) and an NICHD Center Grant (HD 02528). Publication costs were also partially funded by intramural funds from the Midwestern University College of Pharmacy-Glendale (MRE) and the University of Kansas Medical Center (SML). The contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies listed above.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
SML has received past and current grant support from ApoPharma, Inc. SGL has participated in multi-center clinical trials sponsored by Biogen, Bayer, Teva, Acorda, Medimmune, Alexion, Chugai, Novartis, Genzyme, Roche, Vaccinex, Opexa, Actelion, NMSS, and NIH. Publication costs were also partially funded by intramural funds from the Midwestern University College of Pharmacy-Glendale (MRE) and the University of Kansas Medical Center (SML).
Author’s contributions
Wrote manuscript: ST, MRE, SGL, SML. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tsau, S., Emerson, M.R., Lynch, S.G. et al. Aspirin and multiple sclerosis. BMC Med 13, 153 (2015). https://doi.org/10.1186/s12916-015-0394-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-015-0394-4