Abstract
Background
Evidence is limited about healthcare cost disparities associated with homelessness, particularly in recent years after major policy and resource changes affecting people experiencing homelessness occurred after the onset of the COVID-19 pandemic. We estimated 1-year healthcare expenditures, overall and by type of service, among a representative sample of people experiencing homelessness in Toronto, Canada, in 2021 and 2022, and compared these to costs among matched housed and low-income housed individuals.
Methods
Data from individuals experiencing homelessness participating in the Ku-gaa-gii pimitizi-win cohort study were linked with Ontario health administrative databases. Participants (n = 640) were matched 1:5 by age, sex-assigned-at-birth and index month to presumed housed individuals (n = 3,200) and to low-income presumed housed individuals (n = 3,200). Groups were followed over 1 year to ascertain healthcare expenditures, overall and by healthcare type. Generalized linear models were used to assess unadjusted and adjusted mean cost ratios between groups.
Results
Average 1-year costs were $12,209 (95% CI $9,762-$14,656) among participants experiencing homelessness compared to $1,769 ($1,453-$2,085) and $1,912 ($1,510-$2,314) among housed and low-income housed individuals. Participants experiencing homelessness had nearly seven times (6.90 [95% confidence interval [CI] 5.98–7.97]) the unadjusted mean ratio (MR) of costs as compared to housed persons. After adjustment for number of comorbidities and history of healthcare for mental health and substance use disorders, participants experiencing homelessness had nearly six times (adjusted MR 5.79 [95% CI 4.13–8.12]) the expected healthcare costs of housed individuals. The two housed groups had similar costs.
Conclusions
Homelessness is associated with substantial excess healthcare costs. Programs to quickly resolve and prevent cases of homelessness are likely to better meet the health and healthcare needs of this population while being a more efficient use of public resources.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Homelessness and housing instability are significant public health challenges in Canada, with one in five Canadians directly or indirectly affected [1] People experiencing homelessness have consistent disparities in adverse health outcomes and mortality compared to housed counterparts [2,3,4], even after accounting for potential confounders such as socioeconomic status and comorbidities [4, 5]. These disparities have historically resulted in this population incurring notably high average healthcare costs relative to housed individuals [6,7,8,9,10,11,12,13,14].
The onset of COVID-19 has further compounded the challenges faced by people experiencing homelessness, both through direct impacts of the SARS-CoV-2 virus through elevated infection rates and subsequent adverse outcomes [15,16,17], as well as through indirect changes including disruptions to essential services [17,18,19] and growing toxicity of drug supply [20, 21]. Meanwhile, the number of people experiencing homelessness, particularly unsheltered homelessness, is also believed to have increased in Canada during this period [22]. Most of these shifts are expected to be long lasting, with the result that changes to healthcare needs and adverse outcomes in this group are likely to persist even as we stabilize into an era of endemic COVID-19. Given the above, there is a need to update our understanding of the healthcare costs of people experiencing homelessness and whether healthcare cost disparities in this group persist.
This study aims to address this gap by analyzing one-year healthcare costs among a prospectively followed, representative cohort of individuals experiencing homelessness in Toronto, Canada in 2021 and 2022. Additionally, we evaluate disparities in healthcare costs incurred by this group as compared to matched housed and low-income housed individuals.
Methods
Study design and setting
We conducted a matched cohort study in Ontario, Canada, which administers healthcare under a single-payer model, with costs of many services funded or reimbursed by the government. This study used a blend of prospectively gathered data from the Ku-gaa-gii pimitizi-win study [23] and retrospective administrative records from ICES [24], an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data for health system evaluation and improvement. The Ku-gaa-gii pimitizi-win study, conducted in Toronto, a city situated on Treaty 13 territory in Canada, followed a random representative sample of people experiencing homelessness during 2021 and 2022. Ku-gaa-gii pimitizi-win, which roughly translates in English to “life is always/forever moving”, is a spirit name given in ceremony by Elder Dylan Courchene from Anishnawbe Health Toronto. Details about the design of the Ku-gaa-gii pimitizi-win study is available in the protocol [23].
Data used in this study were linked using unique encoded identifiers and analyzed at ICES. This study follows the Reporting of Studies Conducted Using Observational Routinely Collected Data (RECORD) reporting guidelines (Supplement Table 1) [25]. Throughout, our study adopts an onto-epistemological framework grounded in positivist statistics and a biomedical perspective on health.
Data sources
Participants from the Ku-gaa-gii pimitizi-win study were defined as the group exposed to homelessness. We used the following data sources at ICES to define participants in the unexposed groups and to ascertain outcomes and covariates for all three groups: the ICES Registered Persons Database (RPDB); the Discharge Abstract Database; the National Ambulatory Care Reporting System database; the Ontario Mental Health Reporting System database; the Ontario Health Insurance Plan (OHIP) claims database; the Community Health Centre database; the Ontario Cancer Registry; and several ICES-derived population‐surveillance databases, including the Chronic Obstructive Pulmonary Disease Database, the Ontario Asthma Database, the Ontario Diabetes Database, the Congestive Heart Failure Database, the Ontario Hypertension Database, and the Ontario HIV database. Data sources are further detailed in Supplement Table 2.
Population
We recruited the exposed group (people experiencing homelessness) by approaching individuals from randomly selected beds or rooms at 62 shelters, physical distancing hotels and encampments across Toronto between June 16 and September 9, 2021. To be eligible, individuals had to be experiencing homelessness; be at least 16 years of age; and provide informed consent for both the study and the linkage of study data to ICES. Full recruitment procedure and sample size calculation details are available in the study protocol [23].
In the early months of the COVID-19 pandemic (from March 2020 to approximately March 2021, after the initial wave of Omicron variant infections), extensive lockdowns in the region caused significant disruptions to many types of healthcare service in the region [26, 27]. These restrictions had less of an impact on the healthcare of people experiencing homelessness compared to housed people [28], due to the former group’s greater reliance on essential services. To ensure that our findings were not the result of lockdown-related changes rather than broader healthcare utilization trends, we set the participants’ index dates to the earliest date the individual reported experiencing homelessness after Ontario began officially lifting extensive pandemic-related public health measures and lockdowns (June 11, 2021) [29].
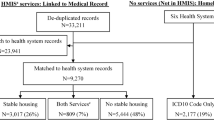
We further created two unexposed groups from the RPDB, which includes all individuals who have ever been eligible for OHIP, Ontario’s healthcare insurance plan. The first group, presumed housed individuals, were eligible if they were alive and at least 16 years of age as of June 11, 2021. Individuals were excluded if they were not residents of the Toronto Census Metropolitan Area (including the census divisions of Durham, York, Toronto and Peel), ineligible for OHIP during the study period, or were already in the exposed group. Index dates were randomly assigned following the distribution of index dates in the exposed group. Individuals were further excluded from the presumed housed group if they had a death date occurring on or before their randomly assigned index date. This group includes people of all income levels.
The second group, low-income housed individuals, had the same eligibility criteria as the presumed housed group except they had to also reside within a lowest-income quintile neighborhood, as determined by Statistics Canada census data [30], and not already be in either the exposed group or the first, matched unexposed group. We included this second matched group to determine the relative importance of homelessness as compared to low income (a proxy for poverty) in altering healthcare costs.
Both unexposed groups were matched to the exposed group 5 to 1 without replacement by age (+/-2 years), sex-assigned-at-birth (exact) and index month (+/- 3 months). We matched on sex-assigned-at-birth rather than gender because gender information was not available in the ICES databases for the control groups. We matched on age and sex-assigned-at-birth due to clear healthcare utilization differences by sex [31] and different stages of life [32], and by index month to ensure seasonality in healthcare utilization did not factor in to results [33]. We opted not to match on measures of comorbidity, because we were also interested in evaluating the degree to which excess healthcare costs among people experiencing homelessness were the result of systematic differences in group comorbidity (physical or mental) rather than homelessness itself.
Outcomes
The primary outcome of interest was overall healthcare costs accumulated over the 1 year observation period, a composite measure comprised of expenditures associated with acute care admissions, psychiatric admissions, emergency department visits, outpatient ambulatory care, and prescriptions publicly funded through the Ontario Drug Benefit. Costs were determined utilizing the ICES costing algorithm [34], which multiplies usage units for a specified healthcare service type during the predetermined period, by its individual cost. Prescription and fee-for-service outpatient care costs were derived from the payments made for each prescription or visit. Costs for outpatient visits under capitation or blended capitation models of care were estimated by applying the monthly fee paid for enrolment in the practice. Costs associated with admissions and visits to the emergency department were computed by first weighting the visit using the Resource Intensity Weighting method [34] then multiplying the weighted volume of services by the average provincial cost per weighted case. In Ontario, there is no additional or differential reimbursement for services rendered to clients experiencing homelessness. All expenses were adjusted to 2021 Canadian dollars using the Consumer Price Index provided by Statistics Canada [35]. Secondary outcomes include each type of healthcare cost noted above.
A small number (< 15) of participants in each group had fewer than 365 days of observation time available, primarily due to death during follow-up. People experiencing homelessness have higher 1-year mortality rates compared to housed people [36]; therefore, we assigned exposed and unexposed individuals the same number of observation days to ensure balanced follow-up time between groups. We opted not to annualize costs in these few cases as this was unnecessary for the analysis of disparities between groups; furthermore, annualization is known to introduce significant error in results [37], particularly when using data obtained proximal to death when healthcare costs are often highest [38].
Covariates
We obtained characteristics for participants in all groups at the start of their 1-year follow-up period. These included age, sex-assigned-at-birth, presence and number of specific physical comorbidities including hypertension, diabetes, asthma, chronic lung disease, chronic heart disease, history of stroke within the past five years, chronic kidney disease, chronic neurological disorder, liver disease, cancer within the past 10 years, or HIV/AIDS. We also obtained history of any healthcare for mental health or substance use disorders, as well as healthcare for psychotic disorders including schizophrenia, substance use disorders, mood and anxiety disorders, obsessive compulsive disorder (OCD)/personality disorders or intentional self-injury. Finally, we measured whether participants were rostered with a primary care physician operating through a capitation or blended capitation model, since the primary care model is known to impact both primary and overall healthcare cost [39]. Supplement Table 3 details all covariates used in this study.
Statistical analysis
We present baseline characteristics of study participants by group membership, using χ2 or analysis of variance (ANOVA) tests as appropriate to compare groups. We also report group-specific means for each type of healthcare cost, as well as group-specific costs at each of the 10th, 25th 50th 75th and 90th percentiles. One-way ANOVA and Wilcoxon rank sum tests were used (as appropriate) to compare unadjusted costs between the exposed and unexposed groups and to calculate 95% confidence intervals for group means.
We then fitted generalized linear regression models using the Tweedie distribution (power parameter estimated by maximum likelihood) to estimate unadjusted mean cost ratios and 95% confidence intervals of overall health care costs for group membership and other potential covariates for adjustment. The Tweedie distribution is helpful for modelling costs as it supports distributions with a mixture of zero and positive values [40], which is very common in cost data.
For each outcome, a multivariable model estimated the adjusted mean cost ratio (aMR) and 95% confidence interval of group membership, with the presumed housed group held as the reference group. For each outcome, the adjusted model‘s power parameter was optimized to ensure maximized goodness of fit as determined by the value of the scaled Pearson/DF value (as close as possible to 1). Each model was adjusted for covariates significantly associated with excess healthcare costs that remained unbalanced between groups after matching. Generally, variables grouping series of variables together (such as number of comorbidities) were prioritized over more individual variables to maximize coverage and avoid potential issues of multicollinearity.
All tests were two-sided with P < 0.05 used to define statistical significance, and cells ≤ 5 were suppressed in order to protect patient privacy. All analyses were conducted at ICES using SAS enterprise guide v8.3 [41].
Ethical review
This study received ethics approval from the Research Ethics Board at Unity Health Toronto (REB# 20–272).
Results
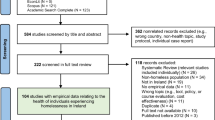
We included 640 participants experiencing homelessness, 3,200 matched presumed housed individuals and 3,200 matched low-income presumed housed individuals (Fig. 1). Self-reported characteristics of participants experiencing homelessness successfully linked to ICES were very similar to that of the Ku-gaa-gii pimitizi-win study cohort overall (Supplement Table 4). After matching, participants experiencing homelessness had significantly higher rates of many comorbidities compared to the matched groups, including asthma (20.9% vs. 10.9% and 10.1%), chronic lung disease (14.5% vs. 4.6% and 4.8%), chronic heart disease (2.7% vs. 1.2% and 1.4%), history of stroke (3.3% vs. 0.8% and 1.1%), chronic kidney disease (1.7% vs. 0.4%), chronic neurological disorder (4.7% vs. 0.8% and 1.0%), liver disease (5.9% vs. 1.6% and 2.2%), and HIV/AIDS (2.0% vs. 0.3% and 0.5%)(Table 1). They were also much more likely to have healthcare for any type of mental health or substance use related disorder (any mental health or substance use disorder: 42.0% vs. 5.3% and 5.2%) and were less likely to be formally rostered with a primary care physician (40.8% vs. 59.2% and 50.4%).
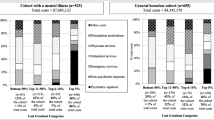
Healthcare costs over the follow-up period are presented in Table 2. Individuals experiencing homelessness had significantly higher overall healthcare costs than either matched group (mean $12,209 [$9,766 - $14,652] vs. $1,769 [$1,453 - $2,084] and $1,912 [$1,511 - $2,314]; median $2,916 vs. $237 and $183). Only 8.1% of the Ku-gaa-gii pimitizi-win cohort had zero healthcare costs (compared to 24.9% and 32.5% of housed and low-income housed controls). Costs diverged by the 25th percentile and crude cost ratios for the exposed group hovered around 12 times higher than unexposed groups at each percentile thereafter. Each component of the overall healthcare costs contributed to this disparity, including acute care admissions (mean $3,148 [$1,847 - $4,449] vs. $664 [$413 - $914] and $626 [$359 - $893]), psychiatric admissions (mean $2,051 [$641 - $3,461] vs. $39 [$-6 - $84] and $139 [$-57 - $335]), ED visits (mean $1,381 [$994 - $1,768] vs. $86 [$75 - $98] and $110 [$92 - $128]), non-hospital outpatient care (mean $2,380 [$2,035 - $2,725] vs. $692 [$633 - $750] and $646 [$587 - $706]) and publically-funded prescriptions (mean $3,247 [$2,533 - $3,961] vs. $286 [$212 - $360] and $390 [$302 - $478]). However, most people in all three groups had no acute care admissions (85.6% of Ku-gaa-gii pimitizi-win participants; 96.3% of housed controls and 96.5% of low-income housed controls) or psychiatric admissions (92.5% of Ku-gaa-gii pimitizi-win participants; 99.8% of housed controls and 99.7% of low-income housed controls) and therefore no admission costs during the observation period.
Table 3 presents unadjusted overall healthcare cost mean ratios (uMRs), by covariate. Ku-gaa-gii pimitizi-win participants had nearly 7 times the uMR of matched controls (uMR 6.9 [95% CI 5.98–7.97]), while low-income controls were not significantly different to matched controls (uMR 1.08 [95% CI 0.98–1.19]). All other covariates were significantly associated with overall healthcare cost; the strongest associations existed for having two or more comorbidities (uMR 8.19 [95% CI 7.28–9.21]); having specific comorbidities like chronic kidney disease (uMR 18.56 [95% CI 10.24–33.62]), chronic neurological disorder (uMR 8.29 [95% CI 5.87–11.71]) or HIV/AIDS (uMR 9.92 [95% CI 5.84–16.85]); or history of healthcare for substance use disorders (uMR 10.40 [95% CI 8.35–12.95]), personality disorders (uMR 13.16 [95% CI 7.82–22.15]) or intentional self-injury (uMR 16.60 [95% CI 10.14–27.15]).
Table 4 reports the results of the multivariable model estimating mean ratio of each type of healthcare between groups after adjustment. We adjusted between groups in the model using number of comorbidities (with zero as the reference), and history of healthcare for any mental health or substance use concern. Rostering with a primary care physician was also included in the outpatient care model [39]. Overall healthcare costs were only somewhat attenuated for participants experiencing homelessness, who continued to have more than five times the aMR (5.79 [95% CI 4.13–8.12]) after adjustment for confounding. No differences were observed between housed and low-income housed individuals (aMR 0.97 [95% CI 0.80–1.17]). Adjusted mean ratios for each component of the overall expenditures were also high, ranging from 2.95 (95% CI 2.39–3.64) for outpatient visits to 14.42 (95% CI 5.55–37.46) for psychiatric admissions.
Discussion
In this cohort of people experiencing homelessness in Toronto, we found high 1-year healthcare expenditures, nearly seven times higher than that of housed and low-income housed individuals matched on age, sex-assigned-at-birth, and index month. Disparities remained very substantial (nearly six times the adjusted mean ratio) after adjusting for number of comorbidities and history of healthcare for mental health or substance use. Notably, every subcomponent of the overall healthcare expenditures included in this study was elevated within the cohort experiencing homelessness (ranging from an adjusted mean ratio of 3.0 to 14.4), indicating that differences are not merely the result of this group disproportionately accessing more intensive (and thus expensive) hospital-based healthcare services.
Our results extend previous work from before the COVID-19 pandemic in Canada [6,7,8,9], the US [10, 11, 40], the UK [12], Denmark [13], and Australia [14]. In all of these settings, people experiencing homelessness are shown to have substantial healthcare costs. In a few of these studies, costs are also shown to be much higher than for housed patients not experiencing homelessness [6, 10]. The vast majority of this literature [6, 10, 12,13,14] assessed costs among patients experiencing homelessness, who by definition require some amount of eligible healthcare to be included. Yet, healthcare utilization is known to be highly heterogeneous in this population [9, 42, 43]: for example, in our sample fewer than 15% of participants would have been included in a study restricted to patients admitted to acute care hospitals. Therefore, we contribute to the existing literature by providing estimates of absolute healthcare cost and estimated disparities in healthcare cost for a representative sample of people experiencing homelessness in Canada, including those whose use of healthcare services is low or nonexistent.
We also provide one of the first estimates of absolute healthcare cost and healthcare cost disparities in the COVID-19 pandemic era. In the pre-pandemic study most similar to our study design (a cohort recruited in Toronto in 2009) [8], average overall healthcare costs per person-year were $6,837 ($6,675 - $6,999); by contrast, in our analysis, the average overall 1-year healthcare cost was nearly twice as high, at $12,209. Each specific type of healthcare cost evaluated in both of these studies also approximately doubled. By contrast, healthcare spending per capita in Ontario increased only 42% over the same period [44, 45]. Unfortunately, because this previous analysis of costs among people experiencing homelessness did not provide percentile costs, it is unclear whether this change represents broad shifts in the healthcare costs of the population experiencing homelessness overall, or outliers (often described as ‘high-cost users’, or high-cost healthcare clients) [46] becoming more expensive in recent years and thus increasing mean values. It is also unclear whether the change we observe represents a recent shift occurring after the onset of the pandemic, rather than steady increases occurring throughout the 2010s.
Even prior to the COVID-19 era, Toronto faced significant challenges in resolving and preventing homelessness. By the time Canada declared the right to housing in 2019 [47], decades of underfinancing left municipal and provincial governments struggling to maintain an adequate supply of affordable and supportive housing [48], a crucial resource to help people exit homelessness. However, these issues only became worse after the pandemic’s onset. Very limited social housing stock [49], soaring housing costs [50] reducing the footprint of rent subsidies such as the Canada-Ontario Housing Benefit [51], and large proportions of Canada’s refugee claimants going to Toronto without the requisite federal supports to the City [52] have all resulted in deteriorated conditions for people experiencing homelessness since March 2020. Meanwhile, distancing protocols and fears of SARS-CoV-2 infection and violence in shelters have led to a substantial increase in unsheltered homelessness in Canada [22], raising concerns about exposure to the elements and subsequent adverse health outcomes and downstream healthcare [53, 54]. Finally, there has been a concurrent, significant increase to the toxicity of the local drug supply [55], leading to a substantial increase in overdoses among people experiencing homelessness [56]. These factors collectively may explain some or all of the healthcare cost increases observed in our study as compared to previous work. Most concerning is that, because most of these changes are unrelated to the pandemic itself, these conditions are likely to persist even as pandemic-related public health measures subside.
The City of Toronto’s Shelter and Support Services served over 20,000 individuals experiencing homelessness in 2022 [57], with approximately half of these experiencing chronic homelessness (at least 180 days in the past year or 546 days in the past three years) [58]. Assuming a 10,000 person-year equivalent population experiencing homelessness in Toronto (which is almost certainly an underestimate [59, 60]), our results suggest an estimated $69.8 to $99.7 million dollars in healthcare costs are attributable annually to homelessness in Toronto alone. In other words, the downstream healthcare costs of homelessness in Canada are considerable. The profound health and quality of life repercussions of homelessness warrant renewed commitment to implementing program and policy responses aimed at quickly and effectively resolving current homelessness and preventing future cases. However, for those most convinced through cost-efficiency, the proposition that mitigating homelessness could lead to reductions in costs across ancillary systems such as the healthcare system stands as a compelling argument for initiatives such as Housing First, which in many places has been found to be cost-effective [61,62,63,64,65].
Strengths and limitations
Our study benefits from several design strengths. As a longitudinal analysis of a representative cohort of people experiencing homelessness in Toronto, we were able to derive a reliable estimate of costs including from individuals experiencing homelessness who accessed little or no healthcare over follow-up. As cost information were acquired through a well-established individual-level costing algorithm accessing health administrative records in a single payer universal health system [34], costing data thus provided complete coverage of healthcare encounters of their type in our region. Finally, our follow-up period was restricted to a one-year window, limiting issues with variable healthcare costs which may have been associated with changes in housing situation.
However, we note the following limitations. First, only Ku-gaa-gii pimitizi win participants who gave consent and were successfully linked to ICES could be included in this study. While the vast majority were linked and the profile of linked participants is very similar to that of Ku-gaa-gii pimitizi-win participants overall (see Supplement Table 4), refugees and individuals with temporary legal status in Canada were somewhat less likely to be included. This is likely because individuals in these groups are more likely to have federal, as opposed to provincial, healthcare coverage, and ICES encrypts unique identifiers using provincial health card numbers; thus, linkage for these individuals would be impossible. Our estimates may thus be somewhat less representative within these subgroups.
Second, despite our efforts to address residual confounding between groups through adjustment, administrative data has inherent limitations in what types of factors are measurable. It is conceivable that unmeasured sociodemographic factors or physical comorbidities, mental illness, or substance use that are not being treated with healthcare may exist at different rates in our groups, impacting the ability of our models to adjust for them when assessing cost disparities. Additionally, although the costing algorithm we used covers a wide range of healthcare services, certain types of healthcare, including Community Health Centre (CHC) visits or other outpatient outreach services not covered by OHIP, were not available to be included. However, as CHCs disproportionately serve marginalized populations facing barriers to healthcare access (including people experiencing homelessness), the consequence of omitting these service types is likely to be an underestimation of the disparity in healthcare costs between groups.
Conclusions
In this representative sample of people experiencing homelessness in Toronto in 2021 and 2022, one-year healthcare expenditures were very high, and significantly higher than among housed and low-income housed counterparts with similar age, sex-assigned-at-birth, number of comorbidities, and history of healthcare for mental health or substance use disorders. Homelessness is strongly associated with increased healthcare costs, which suggests that upstream programs to quickly and effectively resolve homelessness and prevent future cases are likely to result in reduced healthcare costs while better meeting the health and healthcare needs of this highly marginalized population.
Data availability
Legal data sharing agreements between ICES and its data providers (e.g., healthcare organizations and government) prohibit ICES from making the dataset underlying analysis publicly available. However, access may be granted to those who meet pre-specified criteria for confidential access, available at the ICES DAS program (email: das@ices.on.ca). Requests to review the analytic protocol and code underlying the results presented in this study can also be directed to the Corresponding Author.
References
Nanos Research. One in five Canadians have a friend or acquaintance who has been homeless; Majority support building new affordable housing. https://nanos.co/wp-content/uploads/2020/08/2020-1698-CND-Alliance-to-End-Homelessness-FINAL-with-Tabs.pdf. Published August 2020. Accessed 2020 December 8.
Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–40. https://doi.org/10.1016/S0140-6736(14)61132-6.
Baggett TP, Hwang SW, O’Connell JJ, Porneala BC, Stringfellow EJ, Orav EJ, et al. Mortality among homeless adults in Boston. JAMA Intern Med. 2013;173(3):189.
Feodor Nilsson S, Laursen TM, Hjorthøj C, Nordentoft M. Homelessness as a predictor of mortality: an 11-year register-based cohort study. Soc Psychiatry Psychiatr Epidemiol. 2018;53(1):63–75.
Tweed EJ, Leyland AH, Morrison D, Katikireddi SV. Premature mortality in people affected by co-occurring homelessness, justice involvement, opioid dependence, and psychosis: a retrospective cohort study using linked administrative data. Lancet Public Health. 2022;7(9):e733–43.
Hwang SW, Weaver J, Aubry T, Hoch JS. Hospital costs and length of stay among homeless patients admitted to medical, surgical, and psychiatric services. Med Care. 2011;49(4):350–4.
Latimer EA, Rabouin D, Cao Z, Ly A, Powell G, Aubry T, et al. Costs of services for homeless people with mental illness in 5 Canadian cities: a large prospective follow-up study. CMAJ Open. 2017;5(3):E576–85.
Wiens K, Nisenbaum R, Sucha E, Aubry T, Farrell S, Palepu A, et al. Does housing improve health care utilization and costs? A longitudinal analysis of health administrative data linked to a cohort of individuals with a history of homelessness. Med Care. 2021;59:S110–6.
Wiens K, Rosella LC, Kurdyak P, Chen S, Aubry T, Stergiopoulos V, et al. Factors associated with higher healthcare costs in a cohort of homeless adults with a mental illness and a general cohort of adults with a history of homelessness. BMC Health Serv Res. 2021;21(1):555.
Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338(24):1734–40.
Mitchell MS, León CL, Byrne TH, Lin WC, Bharel M. Cost of health care utilization among homeless frequent emergency department users. Psychol Serv. 2017;14(2):193.
McCormick B, White J. Hospital care and costs for homeless people. Clin Med. 2016;16(6):506.
Bring C, Kruse M, Ankarfeldt MZ, Brünés N, Pedersen M, Petersen J, Andersen O. Post-hospital medical respite care for homeless people in Denmark: a randomized controlled trial and cost-utility analysis. BMC Health Serv Res. 2020;20:1–1.
Mitchell RJ, Karin E, Power J, Foung H, Jones N, Nielssen O. Health service use and predictors of high health service use among adults experiencing homelessness: a retrospective cohort study. Aust N Z J Public Health. 2022;46(6):896–902.
Richard L, Booth R, Rayner J, Clemens KK, Forchuk C, Shariff SZ. Testing, infection and complication rates of COVID-19 among people with a recent history of homelessness in Ontario, Canada: a retrospective cohort study. CMAJ Open. 2021; 9 (1).
Porter NAC, Brosnan HK, Chang AH, Henwood BF, Kuhn R. Race and ethnicity and sex variation in COVID-19 mortality risks among adults experiencing homelessness in Los Angeles County, California. JAMA Netw Open. 2022;5(12):e2245263–2245263.
Corey J, Lyons J, O’carroll A, Stafford R, Ivers JH. A scoping review of the Health Impact of the COVID-19 pandemic on persons experiencing homelessness in North America and Europe. Int J Environ Res Public Health. 2022 Mar 1.
Radfar SR, De Jong CAJ, Farhoudian A, Ebrahimi M, Rafei P, Vahidi M, et al. Reorganization of Substance Use Treatment and Harm Reduction services during the COVID-19 pandemic: A Global Survey. Front Psychiatry. 2021;12:639393.
Picchio CA, Valencia J, Doran J, Swan T, Pastor M, Martró E, et al. The impact of the COVID-19 pandemic on harm reduction services in Spain. Harm Reduct J. 2020;17(1):1–11.
Gomes T, Murray R, Kolla G, Leece P, Bansal S, Besharah J, Ontario Drug Policy Research Network. Changing Circumstances Surrounding Opioid-Related Deaths in Ontario during the COVID-19 Pandemic. 2021 May. https://odprn.ca/wp-content/uploads/2021/05/Changing-Circumstances-Surrounding-Opioid-Related-Deaths.pdf. Accessed August 28 2023.
Cawley C, Kanzaria HK, Zevin B, Doran KM, Kushel M, Raven MC. Mortality among people experiencing homelessness in San Francisco during the COVID-19 pandemic. JAMA Netw Open. 2022;5(3):e221870.
Infrastructure Canada. Everyone Counts 2020–2022: Preliminary Highlights Report. 2023. Available: https://www.infrastructure.gc.ca/homelessness-sans-abri/reports-rapports/pit-counts-dp-2020-2022-highlights-eng.html#h2.2 Accessed 2024 April 8.
Richard L, Nisenbaum R, Liu M, McGeer A, Mishra S, Gingras AC, et al. Ku-gaa-gii pimitizi-win, the COVID-19 Cohort Study of people experiencing homelessness in Toronto, Canada: a study protocol. BMJ open. 2022;12(8):e063234. https://doi.org/10.1136/bmjopen-2022-063234.
ICES. Institute for Clinical Evaluative Sciences. https://www.ices.on.ca/. Accessed August 3 2023.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies conducted using Observational routinely-collected health data (RECORD) Statement. PLoS Med. 2015;12(10):e1001885.
Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ open. 2021;11(3):e045343.
Zeitouny S, Cheung DC, Bremner KE, Pataky RE, Pequeno P, Matelski J, et al. The impact of the early COVID-19 pandemic on healthcare system resource use and costs in two provinces in Canada: an interrupted time series analysis. PLoS ONE. 2023;18(9):e0290646.
Liu M, Richard L, Campitelli MA, Nisenbaum R, Dhalla IA, Wadhera RK, et al. Hospitalizations during the COVID-19 pandemic among recently homeless individuals: a retrospective population-based matched cohort study. J Gen Intern Med. 2022;37(8):2016–25.
Government of Ontario. Ontario to move to step one of roadmap to reopen on June 11. https://news.ontario.ca/en/release/1000279/ontario-to-move-to-step-one-of-roadmap-to-reopen-on-june-11. Accessed 2024 Apr 3.
Statistics Canada. Income. https://www12.statcan.gc.ca/census-recensement/2021/rt-td/income-revenu-eng.cfm. Accessed 2024 Apr 3.
Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49(2).
Tillmann BW, Fu L, Hill AD, Scales DC, Fowler RA, Cuthbertson BH, et al. Acute healthcare resource utilization by age: a cohort study. PLoS ONE. 2021;16(5):e0251877.
Upshur RE, Moineddin R, Crighton E, Kiefer L, Mamdani M. Simplicity within complexity: seasonality and predictability of hospital admissions in the province of Ontario 1988–2001, a population-based analysis. BMC Health Serv Res. 2005;5:1–7.
Wodchis W, Buchmeneva K, Nikitovic M, McKillop I. Guidelines on person-level costing using administrative databases in Ontario. Toronto, 2013. http://www.hsprn.ca/uploads/fles/Guidelines_on_PersonLevel_Costing_May_2013.pdf. Accessed 2024 Mar 29.
Statistics Canada. Consumer Price Indexes Portal. https://www.statcan.gc.ca/en/subjects-start/prices_and_price_indexes/consumer_price_indexes. Accessed 2024 Apr 2.
Richard L, Carter B, Wu L, Hwang SWH. Disparities in all-cause mortality among people experiencing homelessness in Toronto, Canada during the COVID-19 pandemic: a cohort study. Front Public Health. 2024; 12: 1401662.
Linden A, Samuels SJ. Estimating measurement error when annualizing health care costs. J Eval Clin Pract. 2013;19(5):933–7.
Von Wyl V. Proximity to death and health care expenditure increase revisited: a 15-year panel analysis of elderly persons. Health Econ Rev. 2019;9:1–6.
Laberge M, Wodchis WP, Barnsley J, Laporte A. Costs of health care across primary care models in Ontario. BMC Health Serv Res. 2017;17:1–9.
Kurz CF. Tweedie distributions for fitting semicontinuous health care utilization cost data. BMC Med Res Methodol. 2017;17:1–8.
SAS Institute Inc. Cary, NC, USA.
Poulin SR, Maguire M, Metraux S, Culhane DP. Service use and costs for persons experiencing chronic homelessness in Philadelphia: a population-based study. Psychiatric Serv. 2010;61(11):1093–8.
Zaretzky K, Flatau P, Spicer B, Conroy E, Burns L. What drives the high health care costs of the homeless? Hous Stud. 2017;32(7):931–47.
Statistics Canada. Canadian classification of functions of government, by general government component. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1010002401&pickMembers%5B0%5D=1.7&pickMembers%5B1%5D=2.2&cubeTimeFrame.startYear=2008&cubeTimeFrame.endYear=2022&referencePeriods=20080101%2C20220101. Accessed July 11th 2024.
Statistics Canada. Population estimates on July 1 by age and gender. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501&pickMembers%5B0%5D=1.7&pickMembers%5B1%5D=2.1&cubeTimeFrame.startYear=2008&cubeTimeFrame.endYear=2023&referencePeriods=20080101%2C20230101. Accessed July 11th 2024.
Rosella LC, Fitzpatrick T, Wodchis WP, Calzavara A, Manson H, Goel V. High-cost health care users in Ontario, Canada: demographic, socio-economic, and health status characteristics. BMC Health Serv Res. 2014;14:1–3.
Government of Canada. National Housing Strategy Act. https://laws.justice.gc.ca/eng/acts/N-11.2/FullText.html. Accessed 2024 June 4.
Canadian Human Rights Commission. The Financialization of Housing in Canada: A Summary Report for the Office of the Federal Housing Advocate. https://publications.gc.ca/collections/collection_2023/ccdp-chrc/HR34-7-2022-eng.pdf. Accessed 2024 June 4.
City of Toronto. Social Housing Waiting List Reports. https://www.toronto.ca/city-government/data-research-maps/research-reports/housing-and-homelessness-research-and-reports/social-housing-waiting-list-reports/. Accessed 2024 June 4.
Tsekouras P, CTV News Toronto. This is how much Toronto’s home prices have changed over the last 5 years: report. 2024 Feb 29. https://toronto.ctvnews.ca/this-is-how-much-toronto-s-home-prices-have-changed-over-the-last-5-years-report-1.6788626. Accessed 2024 June 4.
Gibson V. Toronto to run out of money to help homeless people pay market rents after only two months, city says. Toronto Star. 2023 July 19. https://www.thestar.com/news/gta/toronto-to-run-out-of-money-to-help-homeless-people-pay-market-rents-after-only/article_393d9127-ce2b-5abc-a658-81c9fb54f5d1.html. Accessed 2024 June 4.
City of Toronto. Report for Action: Immediate Federal Government Support Required for Refugee Claimants in Toronto. 2023 Sept 5. https://www.toronto.ca/legdocs/mmis/2023/cc/bgrd/backgroundfile-239033.pdf. Accessed 2024 June 4.
Richard L, Golding H, Saskin R, Jenkinson JI, Francombe Pridham K, Gogosis E, et al. Cold-related injuries among patients experiencing homelessness in Toronto: a descriptive analysis of emergency department visits. Can J Emerg Med. 2023;25(8):695–703.
Richard L, Golding H, Saskin R, Shariff SZ, Jenkinson JI, Pridham KF, et al. Trends in emergency department visits during cold weather seasons among patients experiencing homelessness in Ontario, Canada: a retrospective population-based cohort study. Can J Emerg Med. 2024 Apr;5:1–0.
Gomes T, Murray R, Kolla G, Leece P, Bansal S, Besharah J, Ontario Drug Policy Research Network. Changing Circumstances Surrounding Opioid-Related Deaths in Ontario during the COVID-19 Pandemic. 2021 May. https://odprn.ca/wp-content/uploads/2021/05/Changing-Circumstances-Surrounding-Opioid-Related-Deaths.pdf. Accessed 2023 August 28.
Liu M, Richard L, Campitelli MA, Nisenbaum R, Dosani N, Dhalla IA, et al. Drug overdoses during the COVID-19 pandemic among recently homeless individuals. Addiction. 2022;117(6):1692–701.
City of Toronto. City of Toronto’s 2023/24 Winter Services Plan for people experiencing homelessness. https://www.toronto.ca/news/city-of-torontos-2023-24-winter-services-plan-for-people-experiencing-homelessness/ Accessed 17 October 2023.
City of Toronto. Shelter System Flow Data. https://www.toronto.ca/city-government/data-research-maps/research-reports/housing-and-homelessness-research-and-reports/shelter-system-flow-data/. Accessed 2024 April 8.
O’Neill N, CTV News. True scale of homelessness in Canada is being undercounted, experts say. 2022 Dec 27. https://www.ctvnews.ca/canada/true-scale-of-homelessness-in-canada-is-being-undercounted-experts-say-1.6153449. Accessed 2024 April 8.
Richard L, Hwang SW, Forchuk C, Nisenbaum R, Clemens K, Wiens K, et al. Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada. BMJ open. 2019;9(10):e030221.
Latimer EA, Rabouin D, Cao Z, Ly A, Powell G, Adair CE, Sareen J, Somers JM, Stergiopoulos V, Pinto AD, Moodie EE. Cost-effectiveness of Housing First intervention with intensive case management compared with treatment as usual for homeless adults with mental illness: secondary analysis of a randomized clinical trial. JAMA Netw open. 2019;2(8):e199782.
Wright BJ, Vartanian KB, Li HF, Royal N, Matson JK. Formerly homeless people had lower overall health care expenditures after moving into supportive housing. Health Aff. 2016;35(1):20–7.
Larimer ME, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, Tanzer K, Ginzler J, Clifasefi SL, Hobson WG, Marlatt GA. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–57.
Rosenheck R, Kasprow W, Frisman L, Liu-Mares W. Cost-effectiveness of supported housing for homeless persons with mental illness. Arch Gen Psychiatry. 2003;60(9):940–51.
Tinland A, Loubière S, Boucekine M, Boyer L, Fond G, Girard V, Auquier P. Effectiveness of a housing support team intervention with a recovery-oriented approach on hospital and emergency department use by homeless people with severe mental illness: a randomised controlled trial. Epidemiol Psychiatric Sci. 2020;29:e169.
Acknowledgements
The authors thank the Ku-gaa-gii pimitizi-win study’s research participants, without whom this study would not have been possible and who participated even while navigating numerous other priorities. We also wish to thank Survey Research Unit staff, including Olivia Spandier, Alexandra Carasco, Annika Khan, and the entire SRU interview team for undertaking recruitment and data collection; shelter and COVID-19 physical distancing shelter hotel staff for facilitating visits; Dr. Suzanne Stewart from the Waakebiness-Bryce Institute for Indigenous Health, Joe Hester from Anishnawbe Health Toronto and members of MAP’s Community Expert Group for participating in the review of this project; and finally, staff at the MAP Centre for Urban Health Solutions who contributed in numerous ways to the study. This research was supported by the Canadian Institutes of Health Research (CIHR) (FDN VR5-173211) in partnership with the Public Health Agency of Canada as part of the COVID-19 Immunity Task Force (CITF). This study was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Ministry of Long-Term Care. The work was completed at the ICES Western site, whose core funding is provided by the Academic Medical Organization of Southwestern Ontario, the Schulich School of Medicine and Dentistry, Western University, and the Lawson Health Research Institute. Parts of this material are based on data and information compiled and provided by the Ontario Ministry of Health, Canadian Institute for Health Information, and Statistics Canada. We also thank IQVIA Solutions Canada Inc. for use of their Drug Information File. This study used data adapted from the Statistics Canada Postal Code Conversion File, which is based on data licensed from Canada Post Corporation and/or data adapted from the Ontario Ministry of Health Postal Code Conversion File, which contains data copied under license from ©Canada Post Corporation and Statistics Canada. It also uses income data adapted from Statistics Canada Census 2021. The analyses, conclusions, opinions, and statements expressed herein are those of the authors and do not reflect those of the funding sources or data providers; no endorsement is intended or should be inferred. The Ku-gaa-gii pimitizi-win study was conducted on Anishnawbe and Haudenosaunee territories. The authors acknowledge and pay respects to the Elders and the communities of past, present and future.
Funding
This research was funded by the Canadian Institutes of Health Research (CIHR) (FDN VR5-173211) in partnership with the Public Health Agency of Canada as part of the COVID-19 Immunity Task Force (CITF). This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Ministry of Long-Term Care. The study was completed at the ICES Western site, whose core funding is provided by the Academic Medical Organization of Southwestern Ontario, the Schulich School of Medicine and Dentistry, Western University, and the Lawson Health Research Institute. Parts of this material are based on data and information compiled and provided by the Ontario Ministry of Health, Ministry of Long-term Care, Canadian Institute for Health Information, and Statistics Canada. The analyses, conclusions, opinions, and statements expressed herein are those of the authors and do not reflect those of the funding sources or data providers; no endorsement is intended or should be inferred.
Author information
Authors and Affiliations
Contributions
LR conceived and designed the study; BC conducted the statistical analysis; LR, SWH, BC and RN interpreted the data and made revisions to the methodology; LR drafted the manuscript; SWH obtained funding and resources making the analysis possible. All authors were substantially involved in the acquisition of data and substantially contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All Ku-gaa-gii pimitizi-win study participants gave informed consent to participate and have their data linked with administrative health records. This study received ethics approval from the Unity Health Toronto Research Ethics Board (REB# 20–272).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Richard, L., Carter, B., Nisenbaum, R. et al. Disparities in healthcare costs of people experiencing homelessness in Toronto, Canada in the post COVID-19 pandemic era: a matched cohort study. BMC Health Serv Res 24, 1074 (2024). https://doi.org/10.1186/s12913-024-11501-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11501-2