Abstract
Background
Over the past two decades, antenatal care (ANC) coverage has increased in most settings across low- and middle-income countries, including Ghana. However, evidence shows that there is a need to focus on both access and quality to improve maternal and newborn health outcomes. We investigated ANC quality among public healthcare facilities in the northern region of Ghana.
Methods
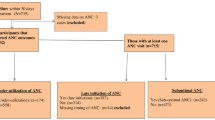
We conducted a facility-based study involving 420 postpartum women, selected randomly from five public health facilities. We collected information on a set of prenatal services that respondents self-reported to have received during their most recent pregnancy. Women who received all the interventions assessed were considered to have received quality ANC. Using multilevel (mixed-effects) regression analysis, we identified the independent factors associated with ANC quality, with healthcare facility as the cluster variable.
Results
Of the 420 women, 31.2% (95% CI: 26.9, 35.8) received ANC services of high quality. ANC quality differed significantly by women’s background characteristics and ANC use. However, gestational age at first ANC and the number of follow-up visits before delivery were significantly associated with ANC quality: booking the first visit in the second or third trimester reduced the odds of receiving high-quality ANC compared to booking in the first trimester (aOR = 0.15, 95% CI: 0.07, 0.31, and aOR = 0.09, 95% CI: 0.01, 0.83, respectively). In contrast, achieving a minimum of eight ANC follow-ups before delivery increased the odds of receiving high-quality ANC compared to attaining fewer than eight visits (aOR = 4.82, 95% CI: 2.33, 9.99).
Conclusions
A significant proportion of pregnant women in the study setting received suboptimal quality ANC during their most recent pregnancy. ANC quality was primarily associated with the timing of the first visit and the number of follow-up visits before delivery. Timely initiation of ANC and frequent follow-up visits will be crucial in the study’s setting for pregnant women to benefit from comprehensive ANC services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Maternal mortality is a significant public health concern that holds a high priority in many countries across the globe and in the international community [1]. The world has seen substantial progress over the past two decades, with a decline in both the absolute number and ratio (i.e., maternal mortality ratio) of women who die annually due to preventable causes relating to pregnancy and childbirth: in 2020, an estimated 287,000 women died globally from a maternal cause, a decline of about 36% from 446,000 in 2000 [2]. This decline is attributed to a variety of factors, including improved healthcare services, better access to skilled birth attendants, and enhanced healthcare policies targeting maternal health [3]. Despite these improvements, maternal mortality remains unacceptably high, particularly in low- and middle-income countries (LMICs). Sub-Saharan Africa (SSA) bears the highest burden, with a notably high maternal mortality ratio (MMR) of 545 deaths per 100,000 live births in 2020, making it the region with the highest rate globally [2]. The world has committed to reducing the global maternal mortality ratio to less than 70 per 100,000 live births [1].
Antenatal care (ANC) is a critical component of maternal healthcare that aims to monitor and promote the health of pregnant women and their unborn babies. ANC provides an opportunity for healthcare professionals to identify and manage potential complications during pregnancy, ensuring both maternal and foetal well-being [4]. Comprehensive ANC services should include a range of interventions, including health education, nutritional counselling, screening for infections, monitoring foetal development, offering preventive treatment, and preparing for safe delivery and postpartum care. The impact of quality ANC on maternal and newborn health is well documented. Regular ANC visits are associated with reduced risks of preterm births, low birth weight, and neonatal mortality [5,6,7,8]. Moreover, ANC facilitates timely referrals to higher-level care for women with high-risk pregnancies, thereby preventing severe complications that could lead to maternal or neonatal deaths [9].
In SSA, the quality of ANC services is of particular importance due to the high burden of maternal and newborn mortality in the region [2, 10]. Despite an increase in ANC coverage in the region over the past two decades, quality lags behind coverage in most countries [11]. The region faces numerous challenges, including inadequate healthcare infrastructure, insufficient numbers of trained healthcare providers, and limited access to essential medical supplies [12,13,14,15]. These barriers contribute to suboptimal ANC services, resulting in missed opportunities for preventing and managing pregnancy-related complications. Inadequate follow-up visits further compromise ANC quality in the region, reducing women’s chances of receiving essential maternal health interventions to reduce maternal and neonatal morbidity and mortality before delivery [16, 17]. Socio-economic factors, low levels of maternal education, and gender inequality often limit women’s access to ANC services [16, 18, 19].
Ghana, like many other countries in the SSA, has made strides in reducing maternal mortality. Recent estimates show that the maternal mortality ratio decreased from 499 deaths per 100,000 live births in 2000 to 263 deaths per 100,000 live births in 2020 [2]. However, disparities persist, particularly in the northern regions of the country. Access to high-quality ANC services can significantly reduce this mortality ratio by ensuring early detection and management of pregnancy complications [20]. A study in the northern region of Ghana has revealed a high incidence of adverse birth outcomes among women who used ANC at least once before delivery. Specifically, approximately 23% of newborns are born either prematurely or with a low birth weight [21]. Given the region’s high incidence of adverse birth outcomes among ANC users, assessing the quality of ANC services in health facilities is critical for identifying gaps and areas for improvement. However, there is inadequate research on the quality of ANC provided to pregnant women in the region.
The purpose of this study is to determine the proportion of women who receive quality ANC during pregnancy and the factors associated with receiving quality ANC among women of reproductive age in the Tamale Metropolis of the northern region of Ghana.
Methods
Study setting and design
This facility-based cross-sectional study was conducted in the Tamale Metropolitan Area of the northern region of Ghana. The Tamale Metropolitan Area is one of Ghana’s 261 metropolitan, municipal, and district assemblies, as well as one of the 16 MMDAs located in the Northern Region. In 2004, Tamale became the capital and the area gained the status of a metropolis. The area has a population of 374,744, according to the most recent 2021 population and housing census [22]. Three public hospitals, eight health centres, more than ten private hospitals, a hospital run by the Christian Health Association of Ghana (CHAG), and more than 20 private clinics all provide care for the local population. Health centres provide primary healthcare services such as ANC, immunisation, family planning, and basic treatments for common illnesses. On average, each health centre has at least a consulting room, which is used for general consultations, an ANC corner, a delivery room, and an on-site dispensary, ensuring that medications are readily available to patients. Additionally, all the health centres have laboratories. Human resources at these centres include a diverse team of health professionals, including physicians, nurses, midwives, community health nurses, laboratory technicians, and disease control officers.
Sample size
We used the Taro Yamane formula for estimating proportions in populations of known population size to calculate the expected sample size for our study. The formula is expressed as follows:
where \(\:n\) denotes the desired sample size, e denotes the margin of error, and N represents the known population size. Our study considered ‘N’ as the estimated cumulative number of expected pregnancies from the five healthcare facilities for the year 2022 (N = 8489). Furthermore, we assumed a 5% margin of error and a 10% non-response rate. Based on the above parameters, we estimated that we would need 420 postnatal women to achieve the objective of our study. We used the proportional-to-size technique to allocate the final sample among the healthcare facilities that we selected.
Sampling strategy
Our study utilised multiple sampling approaches to select healthcare facilities and respondents. We purposefully selected healthcare facilities because of their comparative advantages in terms of convenience and access to the respondents. We used the lottery method to randomly select five health centres in the metropolis.
We selected participants using a systematic random selection method. The postnatal register at each health facility served as a sampling frame and provided a list of women who had given birth within the past twelve months. The sampling interval was determined by dividing the total number of eligible women by the minimum sample size required from the facility. Starting with a random selection from the first ten names in the sampling frame, respondents were then chosen using the sampling interval until the desired sample size was achieved.
Data collection tool and procedures
The study utilised a semistructured questionnaire (see Additional file 1) to collect data electronically via Google Forms on Apple phones running iOS software. The questionnaire was specifically developed for this study, incorporating feedback from ANC experts, including midwives. The experts assessed the items’ relevance and comprehensiveness in terms of accessing ANC quality in the Ghanaian context. Additionally, we compared the questionnaire items against established guidelines and standards for ANC to ensure comprehensive coverage of essential services. We conducted a pilot test with 42 women from healthcare facilities outside the study area to assess the clarity, comprehension, and appropriateness of the questionnaire items in gathering the necessary information. We made modifications where applicable to clarify unclear questions.
Information was collected from respondents covering various aspects, including their background characteristics, obstetrical history, ANC utilisation during their most recent pregnancy, and self-reported prenatal services received during their most recent pregnancy. Maternal record books were used to confirm information on ANC and services provided. Five trained research assistants conducted the data collection, ensuring adherence to the research protocol and ethical guidelines. We conducted interviews with the women during their visits to the healthcare facility for postnatal care or child welfare services. We collected the data throughout August and September 2023.
Measures
Dependent variable
The systematic review of quality assessment in antenatal care worldwide identified a variety of indicators used to measure the quality of care provided to pregnant women. These indicators encompassed different aspects of antenatal care, including maternal assessment, preventive measures, and health promotion [23]. Our dependent variable was antenatal care quality. To construct this variable, we used respondents’ self-reports of services they received during their most recent pregnancy. We asked women if they received any of the following services at least once during their most recent pregnancy. The services included screening, vaccination, and prophylaxis, as well as education and counseling. The fifteen prenatal services included blood pressure measurement, hepatitis B, malaria, and HIV screening, blood grouping, iron and folic acid supplementation, drugs against malaria (IPTp), and hookworm. Not only did we rely on women’s recollections of the services they received, but we also confirmed the provision of these services through their maternal health book. These fifteen items gave us a Cronbach alpha reliability coefficient of 0.868 (≈ 87%). We then developed a binary antenatal care quality variable, low and high-quality, based on the services provided, classifying women who received all fifteen services as having received high-quality ANC and those who received fewer than fifteen services as having received low-quality ANC.
Exposure measures
We reviewed the literature and identified that sociodemographic and economic factors, as well as others, were significantly associated with ANC quality among pregnant women. As a result, we selected factors such as maternal age, marital status, level of education, parity, number of pregnancies, ANC use (including gestational age at first ANC), and number of follow-up visits as potential exposure factors in our study [24,25,26,27,28,29].
Statistical analysis
We performed all analyses in Stata 15/IC for Windows (StataCorp LLC, Texas, USA). We used descriptive statistics to explore the distribution of study respondents by their background characteristics, the percentage distribution of prenatal services received prior to delivery, and the coverage of antenatal care quality. We used the chi-square or Fisher’s exact test, where applicable, to investigate whether antenatal care quality differed by women’s background characteristics. We set statistical significance at a p-value < 0.05. We used a multilevel (mixed-effects) logistic regression model to identify the factors independently associated with antenatal care quality, with health facility as the cluster variable. We developed two regression models. In model one, we included all the exposure variables. In model two, we analysed only the factors that were significantly associated with antenatal care quality using the chi-square or Fisher’s tests. A comparison of the two models revealed that model two had lower values for both the Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) compared to model one, suggesting that the latter is a better-fitting model. Consequently, we chose model two and reported the odds ratios with the corresponding 95% confidence interval.
Ethical considerations
We conducted our study following the ethical guidelines specified in the Declaration of Helsinki regarding research with humans [30]. We received approval from the Ghana Health Service Ethics Review Committee (GHS-ERC 101/07/2023). We obtained both written and verbal informed consent from the respondents prior to their participation. Assent was obtained from the parents or legal guardians of respondents younger than 16 years old. We explained the study’s purposes and procedures, as well as the potential benefits and risks, to their understanding. We assured them of anonymity and confidentiality throughout the study.
Results
Background characteristics of the respondents included in the present study
A total of 420 postpartum women were sampled, all of whom participated in the study, resulting in a 100% response rate. Table 1 presents the demographic and obstetrical characteristics of the respondents. Of the 420 women interviewed, a higher proportion (52.6%) were aged 25–34 years, and about a third (33.6%) had basic education. The majority self-reported being married or cohabiting (89.8%), multigravida (79.5%), and multiparous (67.8%). Furthermore, slightly more than half (51.2%) started antenatal care in the second trimester, and 42.9% made at least eight ANC visits before delivery.
Coverage of prenatal services received by women during their most recent pregnancy prior to delivery Fig. 1 shows the results of women’s antenatal service coverage during pregnancy. All respondents reported blood pressure measurement as the most commonly provided screening service (Fig. 1a), followed by ultrasound (93.8%). Among the vaccination and prophylaxis interventions (Fig. 1b), IPTp recorded the highest coverage (88.6%), followed by iron and folic acid supplementation, with hookworm prophylaxis recording the lowest coverage (35.5%). Counselling on nutrition and pregnancy danger signs had almost identical coverage (94.3% versus 95.5%) (Fig. 1c).
Percentage of women who received quality antenatal care prior to delivery
Our analysis revealed that the number of services received prior to delivery among the women ranged from 1 to 15 (see Table 1 Additional file 2). Overall, 131 women reported receiving all fifteen interventions examined, giving ANC quality coverage of 31.2% (95% CI: 26.9, 35.8) (Fig. 2).
Comparison of antenatal care quality by women’s background characteristics
Table 2 presents results comparing antenatal care quality based on women’s background characteristics, including the facility where they were recruited. The results indicate significant variations in antenatal care quality among respondents, influenced by most of the factors considered, except for gravidity, parity, and the healthcare facility itself. Specifically, the age group of 25–34 years (39.0%), tertiary education (69.0%), self-identification with Christianity (60.6%), and employment (35.1%) accounted for a significantly higher percentage of respondents who received quality antenatal care. Furthermore, these respondents were more likely to start their first antenatal care visit in the first trimester (62.2%) and have at least eight follow-up visits before delivery (62.2%).
Analysis of the independent factors associated with antenatal care quality among pregnant women
Table 3 presents the results of ordinal regression analysis to determine the independent factors associated with antenatal care quality among pregnant women. The results revealed that gestational age at first ANC booking and the number of ANC follow-up visits were important determinants of antenatal care quality among pregnant women in the study setting. Booking the first antenatal care visits in the second or third trimester reduces the odds of receiving high-quality antenatal care by 85% (aOR = 0.15, 95% CI: 0.07, 0.31) and 91% (aOR = 0.09, 95% CI: 0.01, 0.83), respectively, compared to booking in the first trimester. In contrast, achieving a minimum of eight antenatal care follow-ups before delivery increases the odds of receiving high-quality antenatal care compared to fewer than eight visits (aOR = 4.82, 95% CI: 2.33, 9.99). The random effects suggest that differences between health centres do not contribute much to variations in ANC quality.
Discussion
ANC plays a crucial role in preventing maternal and newborn morbidity and mortality, yet gaps in service provision remain a challenge in many LMICs [31, 32]. We aimed to determine the quality of ANC received by women during pregnancy prior to delivery in the northern region of Ghana. We found that approximately 31.2% of the women received quality ANC before delivery, which is higher than the 8% reported by a study conducted in a tertiary hospital in Ghana [33]. Our coverage also varies from studies conducted in other African settings. A population-based study in Nigeria revealed that approximately 5% of pregnant women receive good-quality ANC services [25]. An analysis of nationally representative surveys in East Africa reveals that only about 11% of pregnant women receive quality ANC [24]. Pregnant women receiving care from public health facilities in the Asian context report ANC quality at 30%, a figure that aligns favourably with our coverage [34]. Different ANC quality measures and facility readiness to deliver essential services may partially explain the differences in coverage across studies. Particularly in SSA, researchers have documented variations in healthcare facilities’ readiness to deliver certain ANC services [35].
We found that all the pregnant women had their blood pressure checked, and at least 90% underwent ultrasound scans and received counselling on nutrition and pregnancy danger signs. Approximately 80% of our sample were screened for hepatitis B, took malaria prophylaxis, had their urine analysed, and underwent a haemoglobin check. However, a wider gap was obvious in hookworm prophylaxis, with about two-thirds of the women reporting not taking drugs against hookworm infections. Other studies across the globe have also reported the variability in the coverage of prenatal interventions across healthcare facilities [24, 25, 34, 36, 37]. Our study failed to explore the underlying factors affecting ANC quality in the selected facilities. However, research has documented that late reimbursement of funds to facilities providing care to insured clients, uneven staff distribution, heavy workloads for providers, a lack of essential drugs, and a stockout of medical supplies compromise ANC quality in most SSA countries [14].
We found that women who made their first visit in the first trimester and had a minimum of eight visits before delivery were more likely to report receiving high-quality ANC. Research indicates that reduced ANC visits significantly increase perinatal mortality [38]. Consequently, in 2016, the WHO revised their guidance on ANC, increasing the number of contacts a pregnant woman has with health providers throughout her pregnancy from four to eight [4]. Researchers have found that a minimum of eight ANC visits leads to a higher number of ANC interventions and a reduction in the incidence of adverse birth outcomes [21, 39]. However, with the significantly poor levels of quality ANC services as documented in this study and other assessments, focussing only on an increased number of visits may not produce the desired maternal and neonatal health outcomes [40].
Collectively, while we found that more than two-thirds of women in the study setting did not receive all essential services during pregnancy prior to delivery, we identified that the timing and frequency of ANC are important determinants of ANC quality from the demand side. However, only about 12% of women book early, and more than 60% of pregnant women in the northern region are unable to make a minimum of eight visits before giving birth [21]. Moreover, in our study, less than half (≈ 43%) of the women attended ANC early in their pregnancy and completed eight visits before delivery. This underscores the need for comprehensive strategies that promote both early initiation and frequent attendance of ANC. Policy interventions should address barriers that prevent women from accessing early and frequent ANC. Our study contributes to a body of evidence emphasising the importance of ensuring content and quality. This is crucial for improving birth outcomes and reducing the mortality and morbidity associated with pregnancy and childbirth among the rising proportion of women in LMICs who are making contact with ANC providers. Additionally, it highlights the persistent gaps in ANC quality in LMICs.
Our study has several limitations that must be considered when interpreting the findings. We conducted the study at only five public healthcare facilities. This could be considered a limitation when generalising these findings to a broader population, including private care facilities. Concerns regarding the quality of maternal services in the private sector have also surfaced, underscoring the need to evaluate these facilities’ ANC services to offer a comprehensive picture of the region’s ANC services. Furthermore, given that health facilities in Ghana are classified based on certain criteria, including infrastructure, staffing, and service provision, we anticipate consistent standards across all health centres, which supports our decision to randomly select facilities. However, variations may still occur. For instance, differences in the number of staff between facilities could potentially affect the quality of service delivery. We acknowledge this as one of our study’s limitations.
Our assessment of ANC quality focused solely on the process dimension, which is just one aspect of quality. The quality of care is multidimensional, encompassing structure, process, and outcome measures. By not including structural elements such as facility infrastructure, equipment, and staffing and outcome measures, including maternal and neonatal health outcomes, we may not capture the complete picture of ANC quality. As a result, our analysis is useful for determining whether women receive essential ANC services prior to delivery, but it does not capture women’s experiences with the health system, including the quality of the services received. Additionally, the indicators we used to measure the quality of care do not allow for a comprehensive assessment of prenatal care quality. While our study focused on 15 prenatal activities, it did not include other important aspects of prenatal care, such as measuring weight gain. Future research should consider a more holistic approach that includes these additional dimensions to provide a more thorough evaluation of ANC services. Moreover, we only reported on the coverage of selected ANC interventions without investigating the underlying reasons for the identified gaps. We recommend further research to investigate the underlying obstacles affecting ANC quality in the study area and to inform strategies for improving maternal and newborn health outcomes. Finally, creating a binary outcome from the number of services received may lead to some loss of information. However, our primary objective is to examine the proportion of women who receive the full spectrum of ANC interventions versus those who do not, as well as their associated factors. We cannot identify any approach that achieves this objective without generating categories.
Conclusions
Our study highlights that, while ANC coverage is relatively high, a significant proportion of pregnant women in the study setting received ANC of suboptimal quality during their most recent pregnancy. ANC quality was primarily associated with the timing of the first visit and the number of follow-up visits before delivery. Timely initiation of ANC and frequent follow-up visits will be crucial in the study’s setting for pregnant women to benefit from comprehensive ANC services.
Data availability
The minimal dataset that would be necessary to interpret, replicate and build upon the findings reported in the article are contained within the publication.
Abbreviations
- ANC:
-
antenatal care
- aOR:
-
adjusted odds ratio
- BP:
-
blood pressure
- CHAG:
-
Christian Health Association of Ghana
- CI:
-
confidence interval
- HC:
-
health centre
- Hep B:
-
hepatitis B
- HIV:
-
human immune deficiency virus
- IPTp:
-
intermittent preventive treatment of malaria during pregnancy
- LMICs:
-
low- and middle-income countries
- RCH:
-
reproductive and child health
- SSA:
-
Sub-Saharan Africa
- TT-Dip:
-
tetanus toxoid diphtheria
- WHO:
-
World Health Organization
References
Boldosser-Boesch A, Brun M, Carvajal L, Chou D, de Bernis L, Fogg K, et al. Setting maternal mortality targets for the SDGs. Lancet. 2017;389:696–7.
UNICEF, UNFPA. Trends in maternal mortality 2000 to 2020: estimates by WHO. World Bank Group and UNDESA/Population Division. Gevena; 2023.
Souza JP, Day LT, Rezende-Gomes AC, Zhang J, Mori R, Baguiya A, et al. A global analysis of the determinants of maternal health and transitions in maternal mortality. Lancet Glob Heal. 2024;12:e306–16.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva; 2016.
Weyori AE, Seidu A-A, Aboagye RG, Holmes FA, Okyere J, Ahinkorah BO. Antenatal care attendance and low birth weight of institutional births in sub-saharan Africa. BMC Pregnancy Childbirth. 2022;22:283.
Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. 2017;7:e017122.
Arunda M, Emmelin A, Asamoah BO. Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: analysis of national survey data. Glob Health Action. 2017;10:1–11.
Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on neonatal mortality in sub-saharan Africa: a systematic review and meta-analysis. PLoS ONE. 2019;14:e0222566.
Lincetto O, Mothebesoane-anoh S, Gomez P, Munjanja S. Antenatal Care: opportunities for Africa’s newborns. Int J Sci Technol Res. 2013;2:51–62.
Hug L, Alexander M, You D, Alkema L. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Heal. 2019;7:e710–20.
Carvajal–Aguirre L, Amouzou A, Mehra V, Ziqi M, Zaka N, Newby H. Gap between contact and content in maternal and newborn care: an analysis of data from 20 countries in sub–Saharan Africa. J Glob Health. 2017;7:1–8.
Kruk ME, Chukwuma A, Mbaruku G, Leslie HH. Variation in quality of primary-care services in Kenya, Malawi, Namibia, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ. 2017;95:408–18.
Kruk ME, Leslie HH, Verguet S, Mbaruku GM, Adanu RMK, Langer A. Quality of basic maternal care functions in health facilities of five African countries: an analysis of national health system surveys. Lancet Glob Heal. 2016;4:e845–55.
Ansu-Mensah M, Danquah FI, Bawontuo V, Ansu-Mensah P, Mohammed T, Udoh RH, et al. Quality of care in the free maternal healthcare era in sub-saharan Africa: a scoping review of providers’ and managers’ perceptions. BMC Pregnancy Childbirth. 2021;21:220.
Nyamtema AS, Jong AB, Urassa DP, Hagen JP, van Roosmalen J. The quality of antenatal care in rural Tanzania: what is behind the number of visits? BMC Pregnancy Childbirth. 2012;12:70.
Adedokun ST, Yaya S. Correlates of antenatal care utilization among women of reproductive age in sub-saharan Africa: evidence from multinomial analysis of demographic and health surveys (2010–2018) from 31 countries. Arch Public Heal. 2020;78:134.
Tessema ZT, Teshale AB, Tesema GA, Tamirat KS. Determinants of completing recommended antenatal care utilization in sub-saharan from 2006 to 2018: evidence from 36 countries using demographic and health surveys. BMC Pregnancy Childbirth. 2021;21:192.
Andegiorgish AK, Elhoumed M, Qi Q, Zhu Z, Zeng L. Determinants of antenatal care use in nine sub-saharan African countries: a statistical analysis of cross-sectional data from demographic and health surveys. BMJ Open. 2022;12:e051675.
Okedo-Alex IN, Akamike IC, Ezeanosike OB, Uneke CJ. Determinants of antenatal care utilisation in sub-saharan Africa: a systematic review. BMJ Open. 2019;9:e031890.
Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384:347–70.
Akum LA, Offei EA, Kpordoxah MR, Yeboah D, Issah A, Boah M. Compliance with the World Health Organization’s 2016 prenatal care contact recommendation reduces the incidence rate of adverse birth outcomes among pregnant women in northern Ghana. PLoS ONE. 2023;18:e0285621.
Ghana Statistical Service. Ghana 2021 Population and Housing Census: General Report Volumn 3A. Accra; 2021.
Morón-Duarte LS, Ramirez Varela A, Segura O, Freitas da Silveira M. Quality assessment indicators in antenatal care worldwide: a systematic review. Int J Qual Heal Care. 2019;31:497–505.
Raru TB, Mamo Ayana G, Bahiru N, Deressa A, Alemu A, Birhanu A, et al. Quality of antenatal care and associated factors among pregnant women in East Africa using demographic and health surveys: a multilevel analysis. Women’s Heal. 2022;18:174550652210767.
Fagbamigbe AF, Idemudia ES. Assessment of quality of antenatal care services in Nigeria: evidence from a population-based survey. Reprod Health. 2015;12:88.
Joshi C, Torvaldsen S, Hodgson R, Hayen A. Factors associated with the use and quality of antenatal care in Nepal: a population-based study using the demographic and health survey data. BMC Pregnancy Childbirth. 2014;14:94.
Demissie DB, Molla G, Tiruneh Tiyare F, Badacho AS, Tadele A. Magnitude, disparity, and predictors of poor-quality antenatal care service: a systematic review and meta-analysis. SAGE Open Med. 2024;12.
Tadesse Berehe T, Modibia LM. Assessment of Quality of Antenatal Care Services and its determinant factors in Public Health Facilities of Hossana Town, Hadiya Zone, Southern Ethiopia: a longitudinal study. Adv Public Heal. 2020;2020:1–11.
Morón-Duarte LS, Varela AR, Bertoldi AD, Domingues MR, Wehrmeister FC, Silveira MF. Quality of antenatal care and its sociodemographic determinants: results of the 2015 Pelotas birth cohort, Brazil. BMC Health Serv Res. 2021;21:1070.
World Medical Association. World Medical Association Declaration of Helsinki. JAMA. 2013;310:2191.
Arsenault C, Jordan K, Lee D, Dinsa G, Manzi F, Marchant T, et al. Equity in antenatal care quality: an analysis of 91 national household surveys. Lancet Glob Heal. 2018;6:e1186–95.
Carvajal–Aguirre L, Vaz LME, Singh K, Sitrin D, Moran AC, Khan SM, et al. Measuring coverage of essential maternal and newborn care interventions: an unfinished agenda. J Glob Health. 2017;7:1–5.
Amponsah-Tabi S, Dassah ET, Asubonteng GO, Ankobea F, Annan JJK, Senu E, et al. An assessment of the quality of antenatal care and pregnancy outcomes in a tertiary hospital in Ghana. PLoS ONE. 2022;17:e0275933.
Dandona R, Majumder M, Akbar M, Bhattacharya D, Nanda P, Kumar GA, et al. Assessment of quality of antenatal care services in public sector facilities in India. BMJ Open. 2022;12:e065200.
Kanyangarara M, Munos MK, Walker N. Quality of antenatal care service provision in health facilities across sub–Saharan Africa: evidence from nationally representative health facility assessments. J Glob Health. 2017;7.
Afulani PA, Buback L, Essandoh F, Kinyua J, Kirumbi L, Cohen CR. Quality of antenatal care and associated factors in a rural county in Kenya: an assessment of service provision and experience dimensions. BMC Health Serv Res. 2019;19:684.
Benova L, Tunçalp Ö, Moran AC, Campbell OMR. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob Heal. 2018;3:e000779.
Vogel JP, Habib NA, Souza JP, Gülmezoglu AM, Dowswell T, Carroli G, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO Antenatal Care Trial. Reprod Health. 2013;10:19.
Boah M, Issah A, Yeboah D, Kpordoxah MR, Sira J. Association between Compliance with the New WHO-Recommended frequency and timing of Antenatal Care contacts and receiving Quality Antenatal Care in Cameroon. SAGE Open. 2022;12:215824402211178.
Hodgins S, D’Agostino A. The quality–coverage gap in antenatal care: toward better measurement of effective coverage. Glob Heal Sci Pract. 2014;2:173–81.
Acknowledgements
Not applicable.
Funding
No funding was received for this research from any public, commercial, or not-for-profit entities.
Author information
Authors and Affiliations
Contributions
MB, EAA, and MNA conceptualised and designed the study. MB and EAA implemented the study. MB conducted the data analysis. EAA and MNA interpreted the findings, contributed to the intellectual content, and drafted the manuscript. MB reviewed the draft manuscript. All authors critically reviewed and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received approval from the Ghana Health Service Ethic Review Committee (GHS-ERC 101/07/2023). Prior to participation, the respondents provided both verbal and written informed consent after being briefed on the study’s objectives, procedures, potential benefits and risks, their right to withdraw at any stage, and the guarantee of confidentiality and anonymity throughout the research process. We obtained assent from the parents or legal guardians of respondents younger than 16 years.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Boah, M., Abanga, E.A. & Adokiya, M.N. Quality of antenatal care services received by women of reproductive age prior to delivery in selected public health facilities in the northern zone of Ghana. BMC Health Serv Res 24, 1063 (2024). https://doi.org/10.1186/s12913-024-11491-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11491-1