Abstract
Background
Stroke is a leading cause of mortality and disability. In higher-income countries, mortality and disability have been reduced with advances in stroke care and early access to rehabilitation services. However, access to such services and the subsequent impact on stroke outcomes in the Philippines, which is a lower- and middle-income countries (LMIC), is unclear. Understanding gaps in service delivery and underpinning research from acute to chronic stages post-stroke will allow future targeting of resources.
Aims
This scoping review aimed to map available literature on stroke services in the Philippines, based on Arksey and O’Malley’s five-stage-process.
Summary of review
A targeted strategy was used to search relevant databases (Focused: MEDLINE (ovid), EMBASE (ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO (ebsco); broad-based: Scopus; review-based: Cochrane Library, International Prospective Register of Systematic Reviews (PROSPERO), JBI (formerly Joanna Briggs Institute) as well as grey literature (Open Grey, Google scholar). The searches were conducted between 12/2022-01/2023 and repeated 12/2023. Literature describing adults with stroke in the Philippines and stroke services that aimed to maximize well-being, participation and function were searched. Studies were selected if they included one or more of: (a) patient numbers and stroke characteristics (b) staff numbers, qualifications and role (c) service resources (e.g., access to a rehabilitation unit) (d) cost of services and methods of payment) (e) content of stroke care (f) duration of stroke care/rehabilitation and interventions undertaken (g) outcome measures used in clinical practice.
A total of 70 papers were included. Articles were assessed, data extracted and classified according to structure, process, or outcome related information. Advances in stroke services, including stroke ready hospitals providing early access to acute care such as thrombectomy and thrombolysis and early referral to rehabilitation coupled with rehabilitation guidelines have been developed. Gaps exist in stroke services structure (e.g., low number of neurologists and neuroimaging, lack of stroke protocols and pathways, inequity of stroke care across urban and rural locations), processes (e.g., delayed arrival to hospital, lack of stroke training among health workers, low awareness of stroke among public and non-stroke care workers, inequitable access to rehabilitation both hospital and community) and outcomes (e.g., low government insurance coverage resulting in high out-of-pocket expenses, limited data on caregiver burden, absence of unified national stroke registry to determine prevalence, incidence and burden of stroke). Potential solutions such as increasing stroke knowledge and awareness, use of mobile stroke units, TeleMedicine, TeleRehab, improving access to rehabilitation, upgrading PhilHealth and a unified national long-term stroke registry representing the real situation across urban and rural were identified.
Conclusion
This scoping review describes the existing evidence-base relating to structure, processes and outcomes of stroke services for adults within the Philippines. Developments in stroke services have been identified however, a wide gap exists between the availability of stroke services and the high burden of stroke in the Philippines. Strategies are critical to address the identified gaps as a precursor to improving stroke outcomes and reducing burden. Potential solutions identified within the review will require healthcare government and policymakers to focus on stroke awareness programs, primary and secondary stroke prevention, establishing and monitoring of stroke protocols and pathways, sustainable national stroke registry, and improve access to and availability of rehabilitation both hospital and community.
What is already known?
Stroke services in the Philippines are inequitable, for example, urban versus rural due to the geography of the Philippines, location of acute stroke ready hospitals and stroke rehabilitation units, limited transport options, and low government healthcare insurance coverage resulting in high out-of-pocket costs for stroke survivors and their families.
What are the new findings?
The Philippines have a higher incidence of stroke in younger adults than other LMICs, which impacts the available workforce and the country’s economy. There is a lack of data on community stroke rehabilitation provision, the content and intensity of stroke rehabilitation being delivered and the role and knowledge/skills of those delivering stroke rehabilitation, unmet needs of stroke survivors and caregiver burden and strain,
What do the new findings imply?
A wide gap exists between the availability of stroke services and the high burden of stroke. The impact of this is unclear due to the lack of a compulsory national stroke registry as well as published data on community or home-based stroke services that are not captured/published.
What does this review offer?
This review provides a broad overview of existing evidence-base of stroke services in the Philippines. It provides a catalyst for a) healthcare government to address stroke inequities and burden; b) development of future evidence-based interventions such as community-based rehabilitation; c) task-shifting e.g., training non-neurologists, barangay workers and caregivers; d) use of digital technologies and innovations e.g., stroke TeleRehab, TeleMedicine, mobile stroke units.
Similar content being viewed by others

Introduction
In the Philippines, stroke is the second leading cause of death, with a prevalence of 0·9% equating to 87,402 deaths per annum [1, 2]. Approximately 500,000 Filipinos will be affected by stroke, with an estimated US$350 million to $1·2 billion needed to meet the cost of medical care [1]. As healthcare is largely private, the cost is borne out-of-pocket by patients and their families. This provides a major obstacle for the lower socio-demographic groups in the country.
Research on implementation of locally and regionally adapted stroke-services and cost-effective secondary prevention programs in the Philippines have been cited as priorities [3, 4]. Prior to developing, implementing, and evaluating future context-specific acute stroke management services and community-based models of rehabilitation, it was important to map out the available literature on stroke services and characteristics of stroke in the Philippines.
Methods
The scoping review followed a predefined protocol, established methodology [5] and is reported according to the Preferred Reporting Items for Systematic Review and Meta-Analyses Extension for Scoping Reviews Guidelines (PRISMA-ScR) [6, 7]. Healthcare quality will be described according to the following three aspects: structures, processes, and outcomes following the Donabedian model [8, 9].The review is based on Arksey and O'Malley’s five stages framework [5].
Stage 1: The research question:
What stroke services are available for adults within the Philippines? The objective was to systematically scope the literature to describe the availability, structure, processes, and outcome of stroke services for adults within the Philippines.
Stage 2: Identifying relevant studies:
The following databases were searched. Focused: MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO; broad-based: Scopus; review-based: Cochrane Library, Prospero, JBI (formerly Joanna Briggs Institute); Grey literature: Herdin, North Grey, Grey matters, MedRxiv, NIHR health technology assessment, Department of Health Philippines, The Kings Fund, Ethos, Carrot2. Additionally, reference lists of full text included studies were searched.
The targeted search strategy, developed in consultation with an information scientist, was adapted for each database (see supplemental data). Search terms were peer reviewed using the PRESS (Peer Review of Electronic Search Strategies) checklist [10].
The key search concepts from the Population, Concept and Context (PCC) framework were ≥ 18 years with a stroke living in the Philippines (population), stroke services aiming to maximize well-being, participation and function following a stroke (concept) and stroke services from acute to chronic including those involving healthcare professionals, non-healthcare related personnel or family or friends (context). Search tools such as medical subject headings (MESH) and truncation to narrow or expand searches were used. Single and combined search terms were included (see supplemental data). The search was initially conducted over two weeks in December 2022 and re-run in December 2023.
Studies were selected if they described stroke care in the Philippines in terms of one or more of the following: (a) patient numbers and stroke characteristics (b) staff numbers, qualifications and role (c) service resources (e.g., number of beds/access to a rehabilitation unit, equipment used) (d) cost of services and methods of payment (UHC, Insurance, private) (e) content of stroke care (f) duration of stroke care (hours of personnel contact e.g., Therapy hours per day); interventions undertaken (g) outcome measures used in clinical practice.
Additional criteria:
-
Context: all environments (home, hospital, outpatients, clinic, academic institute).
-
Date limits: published between 2002 onwards. This is based on the Philippines Community Rehabilitation Guidelines published in 2009 that would suggest that papers earlier than 2002 may not reflect current practice [11].
-
Qualitative and quantitative studies including grey literature.
-
Language: reported in English or Filipino only.
-
Publication status: no limit because the level of rigor was not assessed.
-
Type of study: no limit which included conference abstracts, as the level of rigor was not assessed.
Studies were excluded if they were in non-stroke populations or the full text article could not be obtained. Conference abstracts were excluded if there were insufficient data about methods and results.
Searches of databases were performed by one researcher (JM) and searches of grey literature were performed by one researcher (AO). All retrieved articles were uploaded into Endnote X9 software™, and duplicates identified and removed before transferring them to Rayyan [12] for screening.
Stage 3: study selection
The title and abstract were selected using eligibility criteria. Two pairs of researchers independently screened abstracts and titles;(Databases: JM and AL and grey literature by AO and LF). Where a discrepancy existed for title and abstract screening, the study was automatically included for full text review and discussed among reviewers.
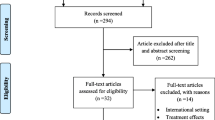
Two reviewers (JM and AL) undertook full-text screening of the selected studies. Discrepancies were resolved through consensus discussions without the need for a third reviewer. There were no discrepancies that required a third reviewer. Reason for exclusion were documented according to pre-determined eligibility criteria. References of included full text articles were screened by each reviewer independently and identified articles were subjected to the same screening process as per the PRISMA-ScR checklist (Fig. 1).
Stage 4: Charting the data
Two reviewers independently extracted the data using a piloted customized and standardized data extraction form including (1) Structure: financial (e.g., costs, insurance, government funding), resources (structure and number of stroke facilities, staff (number, profession/specialism, qualifications etc.), stroke characteristics (2) Process: duration of care, content of stroke care within acute, secondary care, community, outcome measures used; (3) Outcome: survival, function, patient satisfaction, cost (admission and interventions), and (4) year of publication, geographical location (including if Philippines only or multiple international locations) and type of evidence (e.g., policy, review, observational, experimental, clinical guidelines). Critical appraisal of included studies was not undertaken because the purpose of the review was to map available evidence on stroke services available within the Philippines.
Stage 5: Collating, summarising and reporting the results
The search identified 351 records from databases and registers. A total of 70 records are included and reasons for non-inclusion are summarized in Fig. 1.
Study descriptors
The characteristics of included studies are shown in Supplementary Material Table 1. Of the 70 included studies, 36 were observational with most being based on a retrospective review of case notes (n = 31), two were audits, eight were surveys or questionnaires, four were consensus opinion and/or guideline development, three were randomized controlled trial (RCT) or feasibility RCT, 1 was a systematic review, two were policy and guidelines, 11 were narrative reviews or opinion pieces, two were case series or reports and one was an experimental study.
Of the 70 studies, 32 (45.7%) were based in a single tertiary hospital site. There were only three papers based in the community (4.3%). Papers that were opinion pieces or reviews were classified as having a national focus. Of the 22 papers classified as having a national focus, 10 (45.5%) were narrative reviews/ opinion pieces (Table 1).
The primary focus of the research studies (excluding the 11 narrative reviews and 2 policy documents) were classified as describing structure (n = 8, 14%); process (n = 21,36.8%) or outcomes (n = 29, 49.2%). The structure of acute care was described in seven studies out of eight studies (n = 7/8 87.5%) whilst neurosurgery structures were described in one out of eight studies (12.5%). Acute care processes were described in 11 out of 21 studies (n = 11/21 52.3%) whilst rehabilitation processes were described in six out of 21 studies (28.6%), with three out of 21 studies primarily describing outcome measurement (14.3%). The primary focus of the outcomes were stroke characteristics (25 out of 28 papers, 89.2%) in terms of number of stroke (prevalence), mortality or severity of stroke. Measures of stroke quality of life were not reported. Healthcare professional knowledge was described in two studies (n = 2/28 7.1%) whilst risk factors for stroke were described in one study (n = 1/28, 3.6%). Carer burden was described in one study (n = 1/28, 3.6%).
A summary of the findings is presented in Table 2.
Discussion
This scoping review describes the available literature on stroke services within the Philippines across the lifespan of an adult (> 18 years) with a stroke. The review has identified gaps in information about structures, processes and outcomes as well as deficits in provision of stroke services and processes as recommended by WHO. These included a low number of specialist clinicians including neurologists, neuro-radiographers and neurosurgeons. The high prevalence of stroke suggests attention and resources need to focus on primary and secondary prevention. Awareness of stroke is low, especially in terms of what a stroke is, the signs/symptoms and how to minimize risk of stroke [25]. Barriers exist, such as lack of healthcare resources, maldistribution of health facilities, inadequate training on stroke treatment among health care workers, poor stroke awareness, insufficient government support and limited health insurance coverage [22].
The scoping review also highlighted areas where further work is needed, for example, descriptions and research into the frequency, intensity, and content of rehabilitation services especially in the community setting and the outcome measures used to monitor recovery and impairment. PARM published stroke rehabilitation clinical practice guidelines in 2012, which incorporated an innovative approach to contextualize Western clinical practice guidelines for stroke care to the Philippines [42]. Unfortunately, availability and equitable access to evidence-based rehabilitation for people with stroke in the Philippines pose significant challenges because of multiple factors impacting the country (e.g., geographical, social, personal, environmental, educational, economic, workforce) [25, 40, 43].
The number of stroke survivors with disability has not been reported previously, thus, the extent and burden of stroke from acute to chronic is unknown. The recent introduction of a national stroke registry across public and private facilities may provide some of this data [82]. The project started in 2021 and captures data on people hospitalized for transient ischemic attack or stroke in the Philippines. National stroke registries have been identified as a pragmatic solution to reduce the global burden of stroke [83] through surveillance of incidence, prevalence, and outcomes (e.g., death, disability) of, and quality of care for, stroke, and prevalence of risk factors. For the Philippine government to know the full impact and burden of stroke nationally, identify areas for improvement and make meaningful changes for the benefit of Filipinos, the registry would need to be compulsory for all public and private facilities and include out of hospital data. This will require information technology, trained workforces for data capture, monitoring and sharing, as well as governance and funding [83].
This scoping review has generated a better understanding of the published evidence focusing on availability of stroke services in the Philippines, as well as the existing gaps through the lens of Donabedian’s Structure, Process and Outcome framework. The findings have helped to inform a wider investigation of current stroke service utilization conducted using survey and interview methods with stroke survivors, carers and key stakeholders in the Philippines, and drive forward local, regional and national policy and service changes.
Conclusions
This scoping review describes the existing evidence-based relating to structure, processes and outcomes of stroke services for adults within the Philippines. The review revealed limited information in certain areas, such as the impact of stroke on functional ability, participation in everyday life, and quality of life; the content and intensity of rehabilitation both in the hospital or community setting; and the outcome measures used to evaluate clinical practice. Developments in stroke services have been identified however, a wide gap exists between the availability of stroke services and the high burden of stroke in the Philippines. Strategies are critical to address the identified gaps as a precursor to improving stroke outcomes and reducing burden. Potential solutions identified within the review will require a comprehensive approach from healthcare policymakers to focus on stroke awareness programs, primary and secondary prevention, establishing and monitoring of stroke protocols and pathways, implementation of a compulsory national stroke registry, use of TeleRehab, TeleMedicine and mobile stroke units and improve access to and availability of both hospital- and community-based stroke rehabilitation. Furthermore, changes in PhilHealth coverage and universal credit to minimize catastrophic out-of-pocket costs.
Limitations
Although a comprehensive search was undertaken, data were taken from a limited number of located published studies on stroke in the Philippines. This, together with data from databases and grey literature, may not reflect the current state of stroke services in the country.
Availability of data and materials
Not applicable.
Data availability
No datasets were generated or analysed during the current study.
References
Navarro JC, Baroque AC, Lokin JK, Venketasubramanian N. The real stroke burden in the Philippines. Int J Stroke. 2014;9(5):640–1.
Philippines TSSot. Phillipines: stroke 2024. Available from: https://www.strokesocietyphilippines.org/philippines-stroke/#:~:text=Stroke%20is%20the%20Philippines'%20second,or%2014.12%25%20of%20total%20deaths.
Banaag MS, Dayrit MM, Mendoza RU. Health Inequity in the Philippines. In: Batabyal A, Higano Y, Nijkamp P (eds). Disease, Human Health, and Regional Growth and Development in Asia. New Frontiers in Regional Science: Asian Perspectives, vol 38. Singapore: Springer; 2019.
Hodge A, Firth S, Bermejo R, Zeck W, Jimenez-Soto E. Utilisation of health services and the poor: deconstructing wealth-based differences in facility-based delivering in teh Philippines. BMC Public Health. 2016;16:1–12.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–8.
McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, et al. Closing the quality gap: a critical analysis of quality improvement strategies. Tech Rev. 2007;7(9).
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
McGlade B, Mendoza VE. Philippines CBR manual: an inclusive development strategy. Philippines: CBM-CBR Coordinating office; 2009.
Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(210). https://doi.org/10.1186/s13643-016-0384-4.
Baliguas B. Adherence to the clinical practice guidelines of the stroke society of the Philippines in the management of ischemic stroke in young adults admitted in 3 tertiary hospitals in Bacolod City, Philippines from May to October 2010. Neurology. 2018;90(15).
Barcelon EA, Moll MAKDN, Serondo DJ, Collantes MEV. Validation of the Filipino version of national institute of health stroke scale. Clinical Neurology. 2016;56:S379.
Baticulon RE, Lucena LLN, Gimenez MLA, Sabalza MN, Soriano JA. The Neurosurgical Workforce of the Philippines. Neurosurgery. 2024;94(1):202–11. https://doi.org/10.1227/neu.0000000000002630.
Berroya RM. Incidence of symptomatic intracerebral hemorrhage after thrombolysis for acute ischemic stroke at St. Luke’s Medical Center-Global City from January 2010 to February 2017. J Neurol Sci. 2010;2017(381):398–9.
Carcel C, Espiritu-Picar R. Circadian variation of ischemic and hemorrhagic strokes in adults at a tertiary hospital: a retrospective study. J Neurol Sci. 2009;285:S174.
Cayco CS, Gorgon EJR, Lazaro RT. Proprioceptive neuromuscular facilitation to improve motor outcomes in older adults with chronic stroke. Neurosciences (Riyadh). 2019;24(1):53–60.
Co COC, Yu JRT, Macrohon-Valdez MC, Laxamana LC, De Guzman VPE, Berroya-Moreno RMM, et al. Acute stroke care algorithm in a private tertiary hospital in the Philippines during the COVID-19 pandemic: a third world country experience. J Stroke Cerebrovasc Dis. 2020;29(9):105059.
Co COC, Yu JRT, Laxamana LC, David-Ona DIA. Intravenous thrombolysis for stroke in a COVID-19 positive Filipino patient, a case report. J Clin Neurosci. 2020;77:234–6.
Collantes ME. Evaluation of change in stroke care in the Philippines using RES-Q data. Eur Stroke J. 2019;4:318.
Collantes ME. Improving stroke systems of care in lmic: Philippines. Int J Stroke. 2021;16(2):4.
Collantes ME, Navarro J, Belen A, Gan R. Stroke systems of care in the Philippines: addressing gaps and developing strategies. Front Neurol. 2022;13:1046351.
Collantes MEV, Yves Miel H, Zuñiga Uezono DR. Incidence and prevalence of stroke and its risk factors in the Philippines: a systematic review. Acta Medica Philippina. 2022;56:26–34.
Collantes MV, Zuniga YH, Granada CN, Uezono DR, De Castillo LC, Enriquez CG, et al. Current state of stroke care in the Philippines. Front Neurol. 2021;12:665086.
Constantino GA, Soliven JA. Points of in-hospital delays in thrombolytic therapy among patients with acute ischemic stroke: a single center 5-year retrospective study. Neurology. 2020;94(15). https://doi.org/10.1212/WNL.94.15_supplement.2901.
Constantino GAA, Señga MMA, Soliven JAR, Jocson VED. Emerging Utility of Endovascular Thrombectomy in the Philippines: A Single-center Clinical Experience. Acta Med Philipp [Internet]. 2023;57(5). Available from: https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/view/5113. [cited 2024 Aug 21].
Dans AL, Punzalan FE, Villaruz MV. National Nutrition and Health Survey (NNHeS): atherosclerosis-related diseases and risk factors. Philipp J Intern Med. 2005;43:103–15.
De Castillo LL, Collantes ME. Thrombolysis for stroke at the Philippine general hospital: a descriptive analysis. Cerebrovasc Dis. 2019;48:54.
de Castillo LLC, Diestro JDB, Tuazon CAM, Sy MCC, Añonuevo JC, San Jose MCZ. J Stroke Cerebrovasc Dis. 2021;30(7):105831.
Delfino JPM, Carandang-Chacon CA. Comparison of acute ischemic stroke care quality before and during the COVID-19 pandemic in a private tertiary hospital in metro Manila, Philippines. Neurol Asia. 2023;28(1):13–7.
Department of Health. Department of Health Administrative Order 2011-0003. 2011. [Accessed online: 12/2022], from the Philippine Department of Health].
Department of Health. The national policy framework on the prevention, control and management of acute stroke in the Philippines. 2020.
Diestro JDB, Omar AT, Sarmiento RJC, Enriquez CAG, Castillo LLC, Ho BL, et al. Cost of hospitalization for stroke in a low-middle-income country: Findings from a public tertiary hospital in the Philippines. Int J Stroke. 2021;16(1):39–42.
Duenas M, Ranoa G, Benjamin VS. Assessment of post-stroke caregivers’ burden through the modified caregivers strain index (MCSI) in a tertiary center in the Philippines: a cross-sectional study. Cerebrovasc Dis. 2019;48:56–7.
Duya JE, Hernandez K, San Jose MC. The evolving clinical and echocardiographic profile of patients admitted for acute cardioembolic stroke at a Tertiary Hospital in the Philippines. J Hong Kong Coll Cardiol. 2019;27(1):58.
Espiritu AI, San Jose MCZ. A call for a stroke referral network between primary care and stroke-ready hospitals in the philippines: a narrative review. Neurologist. 2021;26(6):253–60.
Gambito ED, Gonzalez-Suarez CB, Grimmer KA, Valdecañas CM, Dizon JM, Beredo ME, et al. Updating contextualized clinical practice guidelines on stroke rehabilitation and low back pain management using a novel assessment framework that standardizes decisions. BMC Res Notes. 2015;8:643.
Gelisanga MA, Gorgon EJ. Upright motor control test: interrater reliability, retest reliability, and concurrent validity in adults with subacute stroke. Eur Stroke J. 2017;2(1):357–8.
Gonzalez-Suarez C, Grimmer K, Alipio I, Anota-Canencia EG, Santos-Carpio ML, Dizon JM, et al. Stroke rehabilitation in the Philippines: an audit study. Disabil CBR Inclusive Develop. 2015;26(3):44–67.
Gonzalez-Suarez CB, Grimmer K, Cabrera JTC, Alipio IP, Anota-Canencia EGG, Santos-Carpio MLP, et al. Predictors of medical complications in stroke patients confined in hospitals with rehabilitation facilities: a Filipino audit of practice. Neurology Asia. 2018;23(3):199–208.
Gonzalez-Suarez CB, Grimmer-Somers K, Margarita Dizon J, King E, Lorenzo S, Valdecanas C, et al. Contextualizing Western guidelines for stroke and low back pain to a developing country (Philippines): an innovative approach to putting evidence into practice efficiently. J Healthc Leadersh. 2012;4:141–56.
Gonzalez-Suarez CB, Margarita J, Dizon R, Grimmer K, Estrada MS, Uyehara ED, et al. Implementation of recommendations from the Philippine Academy of Rehabilitation Medicine's Stroke Rehabilitation Guideline: a plan of action. Clin Audit. 2013;5:77–89.
Ignacio KHD, Diestro JDB, Medrano JMM, Salabi SKU, Logronio AJ, Factor SJV, et al. Depression and anxiety after stroke in young adult Filipinos. J Stroke Cerebrovasc Dis. 2022;31(2):106232.
Inting K, Canete MT. Ischemic stroke subtypes: a comparison between causative and phenotypic classifications in a tertiary hospital in the Philippines. Int J Stroke. 2021;16(2):28.
Jaca PKM, Chacon CAC, Alvarez RM. Clinical characteristics of cerebrovascular disease with COVID-19: a single-center study in Manila. Philippines Neurology Asia. 2021;26(1):15–25.
Jamora RDG, Corral EV, Ang MA, Epifania M, Collantes V, Gan R. Stroke recurrence among Filipino patients taking aspirin for first-ever non-cardioembolic ischemic stroke. Neurol Clin Neurosci. 2017;5:1–5.
Jamora RDG, Prado MB Jr, Anlacan VMM, Sy MCC, Espiritu AI. Incidence and risk factors for stroke in patients with COVID-19 in the Philippines: an analysis of 10,881 cases. J Stroke Cerebrovasc Dis. 2022;31(11).
Juangco DN, Mariano GS. Endovascular therapy for acute ischemic stroke: a review of cases and outcomes from a primary stroke center (a 5-year retrospective study). Cerebrovasc Dis. 2016;41:54.
Leochico CFD, Austria EMV, Gelisanga MAP, Ignacio SD, Mojica JAP. Home-based telerehabilitation for community-dwelling persons with stroke during the COVID-19 pandemic: a pilot study. J Rehabil Med. 2023;55:jrm4405.
Loo KW, Gan SH. Burden of stroke in the Philippines. Int J Stroke. 2013;8(2):131–4.
Mansouri A, Ku JC, Khu KJ, Mahmud MR, Sedney C, Ammar A, et al. Exploratory analysis into reasonable timeframes for the provision of neurosurgical care in low- and middle-income countries. World Neurosurg. 2018;117:e679–91.
Mendoza RA. The clinical profile and treatment outcome of acute ischemic stroke patients who underwent thrombolysis with recombinant tissue plasminogen activator therapy, Philippine experience: a retrospective study. J Neurol Sci. 2009;285:S85–6.
Navarro J. Prevalence of stroke: a community survey. Philipp J Neurol. 2005;9(2):11–5.
Navarro JC, Venketasubramanian N. Stroke burden and services in the Philippines. Cerebrovasc Dis Extra. 2021;11(2):52–4.
Navarro JC, Baroque AC 2nd, Lokin JK. Stroke education in the Philippines. Int J Stroke. 2013;8 Suppl A100:114–5.
Navarro JC, Chen CL, Lee CF, Gan HH, Lao AY, Baroque AC, et al. Durability of the beneficial effect of MLC601 (NeuroAiD™) on functional recovery among stroke patients from the Philippines in the CHIMES and CHIMES-E studies. Int J Stroke. 2017;12(3):285–91.
Navarro JC, Escabillas C, Aquino A, Macrohon C, Belen A, Abbariao M, et al. Stroke units in the Philippines: an observational study. Int J Stroke. 2021;16(7):849–54.
Navarro JC, San Jose MC, Collantes E, Macrohon-Valdez MC, Roxas A, Hivadan J, et al. Stroke thrombolysis in the Philippines. Neurol Asia. 2018;23(2):115.
Ng JC, Churojana A, Pongpech S, Vu LD, Sadikin C, Mahadevan J, et al. Current state of acute stroke care in Southeast Asian countries. Interv Neuroradiol. 2019;25(3):291–6.
Ocampo FF, De Leon-Gacrama FRG, Cuanang JR, Navarro JC. Profile of stroke mimics in a tertiary medical center in the Philippines. Neurol Asia. 2021;26(1):35–9.
Pascua R, Hiyadan JH. Outcome of decompressive hemicraniectomy without evacuation of hematoma in supratentorial intracerebral hemorrhage in a tertiary government hospital in the Philippines: a retrospective study. Eur Stroke J. 2023;8(2):586.
Prado M, Jamora RD, Charmaine Sy M, Anlacan M, Espiritu A. Determinants and Outcomes of Cerebrovascular Disease in Patients with COVID19 in the Philippines: An Analysis of 10881 Cases. Neurology. 2022;98(18). https://doi.org/10.1212/WNL.98.18_supplement.2076.
Qua CV, Tiqui V, Villatima NE, Perales DJ, Rubio SM, Santos ER, et al. A predictive assessment of early neurological deterioration among Filipino acute ischemic stroke patients utilizing hematological, lipid profile, and metabolic parameters in a tertiary hospital in Pampanga. Philippines Cerebrovasc Dis. 2022;51:101.
Que DL, Cuanang J, San Jose MC. Clinical profile, management and outcomes of patients with cerebralvenous thrombosis in atertiary hospital in the Philippines. Int J Stroke. 2020;15(1):511.
Quiles LEP, Diamante PAB, Pascual JLV. Impact of the COVID-19 pandemic in the acute stroke admissions and outcomes in a Philippine Tertiary Hospital. Cerebrovasc Dis Extra. 2022;12(2):76–84.
Roxas AA. The RIFASAF project: a case-control study on risk factors for stroke among Filipinos. Philippine J Neurol. 2002;6(1):1–7.
Roxas AAC, Carabal-Handumon J. Knowledge and perceptions among the barangay health workers in Plaridel, Misamis Occidental. Philipp J Neurol. 2002;6(1):44.
Sasikumar S, Bengzon Diestro JD. Global & community health: acute ischemic stroke in Toronto and Manila: bridging the gap. Neurology. 2020;95(13):604–6.
Senga MM, Reyes JPB. Cerebral venous thrombosis in a single center tertiary hospital of a South East Asian country (CVSTS study)-a retrospective study on the clinical profiles of patients with cerebral venous thrombosis. Neurology. 2019;92(15). https://doi.org/10.1212/WNL.92.15_supplement.P5.3-011.
Sese LVC, Guillermo MCL. Strengthening stroke prevention and awareness in the Philippines: a conceptual framework. Front Neurol. 2023;14:1258821.
Suwanwela NC, Chen CLH, Lee CF, Young SH, Tay SS, Umapathi T, et al. Effect of combined treatment with MLC601 (NeuroAiDTM) and rehabilitation on post-stroke recovery: the CHIMES and CHIMES-E studies. Cerebrovasc Dis. 2018;46(1–2):82–8.
Talamera AF, Franco DS. Validation study of Siriraj stroke score in Southern Philippines. Cerebrovasc Dis. 2011;32:9.
Tan A, Navarro J. Outcomes and quality of care outcome of patients with primary intracerebral hemorrhage in a single center in the philippines. Int J Stroke. 2014;9:269.
Tangcuangco NC, Bitanga ES, Roxas AA, Pascual JL, Saniel E, Reyes JP, et al. Intravenous recombinant tissue plasminogen activator (IV-rtPA) use in acute ischemic stroke in a private tertiary hospital: a Philippine setting. Int J Stroke. 2010;5:107.
Tsang ACO, Yang IH, Orru E, Nguyen QA, Pamatmat RV, Medhi G, et al. Overview of endovascular thrombectomy accessibility gap for acute ischemic stroke in Asia: a multi-national survey. Int J Stroke. 2020;15(5):516–20.
Vatanagul J, Cantero-Auguis C. Awareness on acute stroke management among family medicine and internal medicine residents in Metro Cebu. Philippines J Neurol Sci. 2015;357:e418–9.
Vatanagul J, Rulona IA. The incidence of post-stroke depression in a tertiary hospital in Cebu City, Philippines. J Neurol Sci. 2015;357:e419.
Vatanagul JAS, Rulona IA, Belonguel NJ. Cerebral venous thrombosis (CVST): study of four Filipino patients and literature review. Cerebrovasc Dis. 2013;36:81.
Venketasubramanian N, Yoon BW, Pandian J, Navarro JC. Stroke epidemiology in south, east, and south-east Asia: a review. J Stroke. 2017;19(3):286–94.
Yu RF, San Jose MC, Manzanilla BM, Oris MY, Gan R. Sources and reasons for delays in the care of acute stroke patients. J Neurol Sci. 2002;199(1–2):49–54.
Philippine Neurological Association One Database - Stroke DsSMG. Multicentre collection of uniform data on patients hospitalised for transient ischaemic attack or stroke in the Philippines: the Philippine Neurological Association One Database-Stroke (PNA1DB-Stroke) protocol. BMJ Open. 2022;12(5):54.
Feigin VL, Owolabi MO, Group WSOLNCSC. Pragmatic solutions to reduce the global burden of stroke: a world stroke organization-lancet neurology commission. Lancet Neurol. 2023;22(12):1160–206.
Acknowledgements
We acknowledge the TULAY collaborators: Dr Roy Francis Navea, Dr Myrna Estrada, Dr Elda Grace Anota, Dr Maria Mercedes Barba, Dr June Ann De Vera, Dr Maria Elena Tan, Dr Sarah Buckingham and Professor Fiona Jones. We are grateful to Lance de Jesus and Dr Annah Teves, Research Assistants on the TULAY project, for their contribution to some of the data extraction.
Funding
This research was funded by the NIHR Global Health Policy and Systems Research Programme (Award ID: NIHR150244) in association with UK aid from the UK Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK’s Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
Conceptualisation, methodology and setting search terms, AL, LF, AO, JM, BK. Searches and screening, AL, JM, LF, AO. Data extraction, AL, LF, AO, JM, LdJ, AT. Original draft preparation, AL, JM. All authors provided substantive intellectual and editorial revisions and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Logan, A., Faeldon, L., Kent, B. et al. A scoping review of stroke services within the Philippines. BMC Health Serv Res 24, 1006 (2024). https://doi.org/10.1186/s12913-024-11334-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11334-z