Abstract
Background
Burn treatments are complex, and for this reason, a specialised multidisciplinary approach is recommended. Evaluating the quality of care provided to acute burn patients through quality indicators makes it possible to develop and implement measures aiming at better results. There is a lack of information on which indicators to evaluate care in burn patients. The purpose of this scoping review was to identify a list of quality indicators used to evaluate the quality of hospital care provided to acute burn patients and indicate possible aspects of care that do not have specific indicators in the literature.
Method
A comprehensive scoping review (PRISMA-ScR) was conducted in four databases (PubMed, Cochrane Library, Embase, and Lilacs/VHL) between July 25 and 30, 2022 and redone on October 6, 2022. Potentially relevant articles were evaluated for eligibility. General data and the identified quality indicators were collected for each included article. Each indicator was classified as a structure, process, or outcome indicator.
Results
A total of 1548 studies were identified, 82 were included, and their reference lists were searched, adding 19 more publications. Thus, data were collected from 101 studies. This review identified eight structure quality indicators, 72 process indicators, and 19 outcome indicators listed and subdivided according to their objectives.
Conclusion
This study obtained a list of quality indicators already used to monitor and evaluate the hospital care of acute burn patients. These indicators may be useful for further research or implementation in quality improvement programs.
Trial Registration
Protocol was registered on the Open Science Framework platform on June 27, 2022 (https://doi.org/10.17605/OSF.IO/NAW85).
Similar content being viewed by others
Background
According to the World Health Organization (WHO), burns are a public health problem worldwide, accounting for about 180,000 deaths annually, mostly in low- and middle-income countries [1]. In addition to the mortality impact, burns can present devastating results for the individual's health and are associated with expensive and prolonged hospitalisation and rehabilitation programs, with substantial losses in quality of life [2, 3]. Despite the important advances in recent decades, it is currently recommended that these patients be treated by a specialised multidisciplinary team [2].
Quality indicators are increasingly being used in health services worldwide. They consist of measurement tools, usually based on standards of care, aiming to monitor performance, inform policies or strategies, and support improvements in clinical practice [2, 4]. An important step in the process of evaluating the quality of health care is the identification of appropriate indicators. Each indicator will reflect different aspects of quality, and its selection will depend, among others, on the objectives of the analysis, the data available, and for whom it is intended [5].
In the context of burns, infection control, fluid management, and wound treatment, among other factors, are critical for the patient's outcome and survival. Evaluating the quality of care provided to these patients enables the development and implementation of measures to help improve the standard of care and the results achieved [6].
In the literature, it is possible to find studies describing the process and results of developing a list of quality indicators aimed at the care of burns, generally developed through a consensus among experts [2, 4, 7,8,9]. However, none of these instruments are specific to evaluate hospital care. Data demonstrate that hospital-acquired events can further impact the patient's long-term quality of life with burn sequelae [10]. Obtaining a list of indicators that apply to this delicate phase of care enables better practices and, consequently, better results.
The objective of this scoping review is to answer the question: "What indicators are used to evaluate the quality of hospital care provided to acute burns patients?". It aims to identify and obtain a list and indicate possible aspects of care that do not have specific indicators in the literature. It is part of a larger project that aims to build an instrument to evaluate the quality of care provided by Brazilian burn units.
Methods
A scoping review was performed following the PRISMA Extensions for Scoping Reviews (PRISMA-ScR) guidelines [11], conducted according to a protocol registered on the Open Science Framework [12] platform on June 27, 2022, and can be accessed at https://doi.org/https://doi.org/10.17605/OSF.IO/NAW85.
Research strategy
The search was performed between July 25 and 30, 2022, and redone on October 6, 2022, in the following databases: PubMed (MEDLINE), Cochrane Library, EMBASE, Lilacs/VHL.
The search strategy was developed by one of the researchers (DS) and reviewed by two others (VS and LAS). The search strategy was formulated for MEDLINE (Additional_File 1) and adapted for the other databases, using the following descriptors and their respective synonyms: ((Burns[Title/Abstract]) OR (Burns, Inhalation[Title/Abstract]) OR (Smoke Inhalation Injury[Title/Abstract]) OR (Burns, Electric[Title/Abstract]) OR (Burns, Chemical[Title/Abstract])) AND ((Quality Assurance, Health Care[Title/Abstract]) OR (Quality Improvement[Title/Abstract]) OR (Quality Indicators, Health Care[Title/Abstract]) OR (Health Care Quality, Access[Title/Abstract] AND Evaluation[Title/Abstract]) OR (Health Care Evaluation Mechanisms[Title/Abstract]) OR (Patient Reported Outcome Measures[Title/Abstract]) OR (Outcome[Title/Abstract] OR (Quality of Health Care[Title/Abstract])).
In addition, references from included studies were searched manually to identify potential additional studies.
Eligibility criteria
Potentially relevant articles were evaluated for eligibility based on inclusion and exclusion criteria following the PCC guide:
-
Population – acute burn patients
-
Concept – quality indicators
-
Context – hospital care
Original or review studies published in indexed journals and documents in governmental or specialised societies were included, addressing acute burn patients (open wounds), without distinction of age, sex, or causal agent, studies presenting quality of care measurement, and managing patients hospitalised for burn treatment. There were no restrictions on the length of time or language of publication. Studies that did not address burns or quality indicators or addressed burned patients with wounds already healed or in pre-hospital, emergency room, outpatient intervention, or rehabilitation phase were excluded.
As this review is the initial stage of a larger study that aims to develop an instrument to evaluate the quality of care in Brazil, studies that explicitly presented quality indicators and constructs to be considered from a quality perspective were selected.
Screening procedures and data extraction
The references found were organised using the Rayyan Platform [13] and analysed for eligibility by two independent reviewers (DS and JA). In cases of disagreement, a third reviewer was consulted (VS). The reasons for exclusion from the studies were recorded.
General data such as title, authors, journal, year and language of publication, country where it was performed, study design, and data on the identified quality indicators were collected. Each indicator was classified as structure, process, and outcome, as proposed by Donabedian [14]. In addition, information on the indicator's purpose and how it was calculated was also collected. The data were extracted through a standardised form developed in Microsoft Word (Additional_File 2).
After data extraction, each indicator was organised into a list of structure, process, and outcome indicators. The structure indicators were divided, according to their objective, into indicators to evaluate the physical structure, human and organisational resources. The process indicators were distributed into indicators to evaluate, the treatment of the burned patient, prophylactic measures, complications, and other process indicators. Finally, the outcome indicators were categorised to evaluate mortality, length of hospital stay, wound healing, physical, functional and nutritional results, and other outcome indicators.
In addition, a table was organised containing the main characteristics of each article and the indicators identified (Additional_File 3).
Results
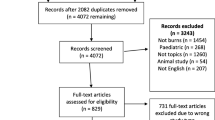
A total of 1548 studies were identified, and after removing the duplicates, 1458 publications were included in the screening process. Among these, 82 were included, and their reference list was searched, adding 19 more, totalling 101 studies. The identification and selection process are shown in Fig. 1.
The main characteristics and the quality indicators identified in each study can be seen in Additional_File 3. The most common study design was a retrospective cohort (n = 33, 32.67%), followed by randomised controlled trials (n = 14, 13.86%). Most of the studies were published starting from 2000 (n = 97, 96%), and most were published in the last ten years, between 2013 and 2022 (n = 77, 76.23%). Regarding the journal of publication, most studies were found in specific burn journals (n = 63, 62.37%), and the most used language was English (n = 76, 75.24%). Most of the studies were conducted by American institutions (n = 41, 40.59%), and two were performed with other countries (Canada and Israel).
Tables 1, 2, and 3 present a list of all quality indicators and constructors identified and the studies in which they were found.
Considering that quality indicators provide a quantitative basis that can be used to monitor and evaluate the quality of care provided [111], all the indicators that were explicitly addressed in the included studies are described in Additional_File 4.
Discussion
The main objective of this study was to identify and generate a list of quality indicators used to evaluate the quality of hospital care provided to patients with acute burns and indicate the gaps in the current literature. This review identified eight structure quality indicators, 72 process indicators, and 19 outcome indicators. Most included studies (76.23%) were published in the last ten years, demonstrating an increasing trend in assessing healthcare quality [2, 4]. Despite many indicators found, there is still a need for more detail regarding the structure indicated for quality care and a lack of evaluation of some aspects, such as speech therapy.
The structure indicators were addressed only in three studies, showing that they are still little explored in the current literature and that most are related to organisational aspects.
Regarding the physical structure of burn units, it is important to highlight that burn patients have unique characteristics and needs, and the units should be designed to address this specific care. Assuming that burn units follow the same standards as general hospitals can result in major deficiencies. A review study that sought to establish the main characteristics of the burn unit design that make it possible to provide best practices found some clinical evidence to support the configuration in closed units, with individual rooms and incorporating ICU capacity for burns [112]. The American Burn Association (ABA) places as one of the criteria for certification of a burn centre that the hospital maintains a specialised unit dedicated to caring for burn patients and has designated beds with the capacity for intensive treatment [113]. The European Burns Association (EBA), in its guideline published in 2017, states that treatment offered in specialised centres brings better results and recommends that they have adequate space, be located within a hospital equipped for all aspects of treatment and include a medical and administrative team dedicated to care and with a high level of specialisation [114]. However, despite the recommendations, there are few structure indicators, leading to a poor evaluation of the necessary structure to achieve good results.
Only a full-time specialised surgeon was highlighted regarding human resources, and a multidisciplinary team provides care. The International Society for Burn Injuries (ISBI) [115] and the EBA guidelines [114], as well as the ABA certification lists [113], recommend that a highly specialised multidisciplinary team provide treatment. In this review, no details were provided on the minimum composition of the team, and no indicators related to the nursing team were identified. Studies performed in New Zealand, Canada, and the United States observed that restructuring the nursing workforce to reduce costs significantly influenced the increase in adverse events, morbidity, and mortality of hospitalised patients [116, 117]. These studies were not specific to burn patients but reflect the need for further research to evaluate the impact that the availability of certain human resources may have on the outcomes of burn patients. The ISBI states that the multidisciplinary team should comprise at least burn surgeons, trained nurses, physiotherapists, occupational therapists, pharmacists, and nutritionists. However, depending on the complexity of the cases, they could benefit from including other professionals [115].
As for the process indicators, an extensive list was identified, corroborating the complexity of care for these patients. Pain evaluation was the most verified indicator among the 15 indicators for evaluating the burned patient. These indicators were identified in 33 studies. Burn patients invariably suffer from pain, one of the main problems for the patient and the treatment team [39]. In addition to the pain associated with the initial trauma, there is also pain related to the treatment itself, such as dressing changes, surgeries, and physiotherapy [43], extremely painful procedures that justify the importance of a specific indicator to evaluate the pain and the results obtained with the control measures adopted.
Twenty-eight indicators related to the treatment of burn patients were found in 48 articles. Nine indicators are related to surgical care, six to nutritional care, and five to resuscitation fluid.
Regarding surgical care, a systematic review with meta-analysis to evaluate the efficacy and safety of early burn excision demonstrated that this practice significantly reduced mortality (in patients without inhalation injury) and length of hospital stay [62]. Another prospective cohort study observed a lower incidence of positive cultures, better graft adherence, and an important reduction in hospital stay in patients submitted to early excision and grafting [78]. The ideal time for early excisions remains under debate; however, it is widely accepted that an adequate surgical intervention interferes considerably with the final results obtained, justifying the importance of various indicators to evaluate this aspect of care.
Severe burns result in hypercatabolic syndrome, which can persist for up to two years after injury [118]. These patients have significant energy needs and are often not able to achieve their macro and micronutrient demands orally [119]. While providing nutrition is essential and widely accepted for successful management, there are several conflicts over the best method and timing of enteral nutritional support. A systematic review conducted to evaluate the effectiveness of early vs late enteral nutritional management in burn adults demonstrated some promising results suggesting early nutritional support can attenuate the hypermetabolic response to thermal injury. Still, it was insufficient to indicate benefits in clinical outcomes such as length of hospital stay and mortality [119]. Despite this result, the early onset of nutritional support is a key aspect of managing critically ill burn patients. It is widely cited in clinical practice guidelines [120]. These data highlight the importance of indicators to assess the adequacy of the nutritional care offered to the burned patient and enable better assessments of the impact of this care on outcomes.
Most deaths occurring within 72 h of injury are caused by volume shock associated with burns. Aggressive resuscitation volume is adopted to achieve and maintain the perfusion of target organs in the face of extensive fluid losses by the burned area and fluid load in injured tissues [121]. However, excessive resuscitation can be as dangerous as insufficient resuscitation. Excessive fluid administration further increases capillary permeability, worsening fluid creep, and can lead to devastating complications such as acute respiratory distress syndrome (ARDS), congestive heart failure, abdominal compartment syndrome, and compartment limb syndrome, among others [120]. For these reasons, indicators are important to guide and monitor this initial and crucial phase of treating a critical burn.
Also related to process indicators, 22 quality indicators were found and cited in 46 articles regarding the possible complications of a burn patient. Among the 22 indicators, five are related to psychosocial complications, three are directed to infectious complications, and another three are intended to evaluate surgical complications.
Burns not only have a physical impact but can also affect the patient's psychological and emotional well-being. In addition to an often traumatising event, hospitalisation and subsequent wound treatment are painful and invasive. A systematic review conducted to evaluate the psychological impact on children's mental health after burns observed that there seems to be evidence of high risk for mental health diagnoses, in particular, diagnoses such as anxiety disorders, post-traumatic stress disorders, acute stress disorder, depression, and personality disorders [122]. Most participants in the reviewed studies experienced increased anxiety and other psychological symptoms after a burn compared to the general population [122]. These aspects demonstrate the importance of including quality indicators that evaluate perspectives directed at the mental health of these patients. In this scoping review, indications related to post-traumatic stress disorder were excluded because it is a complication identified later, after the hospitalisation phase.
Also, regarding complications, three indicators were found to evaluate the occurrence of infectious complications. Infections, in conjunction with dysfunction and/or multiple organ failure, are considered the main mortality ratio in burn patients. For burns above 20% of the body surface, in addition to the rupture of the protective skin barrier, humoral and cellular immunity are also altered, making preventing and treating infection more difficult [123]. A prospective cohort study conducted with adult burn patients admitted to an ICU observed a 26% prevalence of sepsis, overall mortality of 11.9%, and 34.4% in patients with sepsis [124], indicating the importance that this type of complication has in the final result obtained and, therefore, the need to monitor these events for better quality care.
Other complications mentioned in the articles were acute respiratory distress syndrome, venous thromboembolism and pulmonary embolism, cardiac arrest, and bacteremia, among others.
Despite the extensive list of process indicators found, some aspects were not considered, such as data related to speech therapy and speech/swallowing complications.
Regarding outcome indicators, the most cited was the "length of hospital stay". Initially, mortality was the only measure of the quality of hospital care adopted. As some standards of care have been established and practices have changed and improved, fortunately, the survivability of burns has increased significantly. Thus, the need to include new indicators arose [125]. In addition to the length of hospital stay, the inclusion of a greater number of physical-functional indicators can also be observed. The scarring changes, developed by excessive skin fibrosis, lead to joint contractures that are associated with changes in muscle strength and functional capacity due to long periods of sedation and immobility and the hypercatabolic state of these patients, leading to physical-functional changes that can impact the quality of life in the long term [72]. A retrospective study found, as the main finding, that extremities contracture is independently associated with a lower return to work at 6, 12, and 24 months after the injury [126]. New strategies implemented in acute care for these patients, such as excision and closure as soon as possible, early mobility strategies, lighter sedations, and previous resumption of exercises after grafting, can impact both the physical-functional results and the length of hospital stay [126], emphasising the importance of using these indicators to evaluate and monitor the care provided.
Study limitations
In our study, we opted not to include grey literature due to the difficulty in retrieving the data and their low reliability because they have not been peer-reviewed. The inclusion of the grey literature could have led to the identification of some other aspect of care, but given the number of studies included, we believe that the inclusion would have added little or nothing to the final results. Another limitation of this study is that despite various efforts, four articles considered eligible by reading their titles and abstracts were not found in their entirety to assess eligibility after full reading. In addition, it was not possible to evaluate the methodological quality of all included studies, although scoping reviews are not required. It was chosen not to delimit the research about the study design in an attempt to encompass a greater number of hospital quality indicators.
Some indicators found in the studies were not included in the data collection, such as indicators related to the evaluation of scars, the cost of care, aspects related to pre-hospital care, adverse effects of a certain procedure that was being analysed in the study, long-term quality of life and post-traumatic stress, as they are related to aspects of care not included in the scope of this study.
Conclusion
This scoping review was performed to identify quality indicators for hospital care of acute burn patients. It is part of a larger project that aims to build an instrument to evaluate the quality of care provided by Brazilian burn units. As a result of this study, a list of indicators already used was obtained, which will be further reviewed by a group of experts. In addition, this list may also be useful for further research or implementation in a program to improve the quality of hospital care provided to acute burn patients. The human resources needed to obtain better results and indicators related to speech therapy and speech/swallowing complications in burned patients were not covered.
Availability of data and materials
All data generated or analysed during this study are included in this article and its supplemental information files.
Abbreviations
- WHO:
-
World Health Organization
- PRISMA-ScR:
-
PRISMA Extensions for Scoping Reviews
- BMI:
-
Body mass index
- TBSA:
-
Total body surface area
- VAP:
-
Ventilation-Associated Pneumonia
- ICU:
-
Intensive Care Unit
- LA50:
-
Lethal Area 50 – Total Burned Body Surface with 50% mortality
- ABA:
-
American Burn Association
- EBA:
-
European Burns Association
- ISBI:
-
International Society for Burn Injuries
- ARDS:
-
Acute Respiratory Distress Syndrome
References
World Health Organization. Burns; 2018. https://www.who.int/news-room/fact-sheets/detail/burns. Accessed January 30 2022.
Gong J, Singer Y, Cleland H, Wood F, Cameron P, Tracy LM, et al. Driving improved burns care and patient outcomes through clinical registry data: A review of quality indicators in the Burns Registry of Australia and New Zealand. Burns. 2021;47(1):14–24.
Santos JV, Souza J, Amarante J, Freitas A. Burden of Burns in Brazil from 2000 to 2014: A Nationwide Hospital-Based Study. World J Surg. 2017;41(8):2006–12.
Watterson D, Cleland H, Darton A, Edgar D, Fong J, Harvey J, et al. Developing clinical quality indicators for a Bi-National Burn Registry. Burns. 2011;37(8):1296–308.
Berenholtz SM, Pronovost PJ. Monitoring patient safety. Crit Care Clin. 2007;23(3):659–73. https://doi.org/10.1016/j.ccc.2007.05.003.
Zia N, Latif A, Mashreky SR, Al-Ibran E, Hashmi M, Rahman AKMF, et al. Applying quality improvement methods to neglected conditions: development of the South Asia Burn Registry (SABR). BMC Res Notes. 2019;12(1):1–6.
Helvig EI, Upright J, Bartleson BJ. The development of outcome statements for burn care. Semln Perioper Nurs. 1997;6(4):197–200.
Patterson KN, Fabia R, Giles S, Verlee SN, Marx D, Aguayo P, et al. Defining Benchmarks in Pediatric Burn Care: Inception of the Pediatric Injury Quality Improvement Collaborative. J Burn Care Res. 2022;43(1):277–80.
Gibran NS, Wiechman S, Meyer W, Edelman L, Fauerbach J, Gibbons L, et al. American Burn Association consensus statements. J Burn Care Res. 2013;34(4):361–85.
Deeter L, Seaton M, Carrougher GJ, McMullen K, Mandell SP, Amtmann D, et al. Hospital-acquired complications alter quality of life in adult burn survivors: Report from a burn model system. Burns. 2019;45(1):42–7.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73.
Center for Open Science. Open Science Framework. 2022. Available from: https://osf.io/dashboard.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Donabedian A, Health AA. The Quality of Care How Can It Be Assessed? JAMA. 1988;260(12):1743–8.
Kamanga P, Ngala P, Hebron C. Improving hand hygiene in a low-resource setting: A nurse-led quality improvement project. Int Wound J. 2022;19(3):482–92.
Cornell RG, Feller I, Roi LD, Schork MA, Flora JD Jr, Wolfe RA. Evaluation of burn care utilising a national burn registry. Emerg Med Serv. 1978;7(6):107–17.
Angulo M, Aramendi I, Cabrera J, Burghi G. Mortality analysis of adult burn patients in Uruguay. Rev Bras Ter Intensiva. 2020;32(1):43–8.
Hultman CS, van Duin D, Sickbert-Bennett E, DiBiase LM, Jones SW, Cairns BA, et al. Systems-based Practice in Burn Care: Prevention, Management, and Economic Impact of Health Care–associated Infections. Clin Plast Surg. 2017;44(4):935–42.
Barrow RE, Jeschke MG, Herndon DN. Early fluid resuscitation improves outcomes in severely burned children. Resuscitation. 2000;45(2):91–6. Available from: www.elsevier.com/locate/resuscitation.
Palmieri TL, Przkora R, Meyer WJ, Carrougher GJ. Measuring burn injury outcomes. Surg Clin North Am. 2014;94:909–16.
Wood FM. Quality assurance in burn patient care: The James Laing Memorial Essay, 1994. Burns. 1995;21(8):563–8.
Hussain A, Dunn KW. Accuracy of commercial reporting systems to monitor quality of care in burns. Burns. 2014;40(2):251–6.
Andel D, Kamolz LP, Niedermayr M, Hoerauf K, Schramm W, Andel H. Which of the abbreviated burn severity index variables are having impact on the hospital length of stay? J Burn Care Res. 2007;28(1):163–6.
Louhau EMO, Ochoa YL, Mora MCF, Lorié AT, Morán ZM. Calidad de la atención hospitalaria a niños con lesiones por quemaduras. MEDISAN. 2011;15(4):454–61.
Smith MTD, Allorto NL, Clarke DL. Modified first world mortality scores can be used in a regional South African burn service with resource limitations. Burns. 2016;42(6):1340–4.
Arruda FCF. Comparação de escores de gravidade para previsão de mortalidade e tempo de internação em unidade de queimados. Rev Bras Queimaduras. 2017;16(3):142–9.
Patterson KN, Onwuka A, Schwartz DM, Fabia RB, Thakkar RK. Length of Stay Per Total Body Surface Area Burn: A Validation Study Using the National Burn Registry. J Burn Care Res. 2022;43(6):1227–32.
Berger MM, Revelly JP, Wasserfallen JB, Schmid A, Bouvry S, Cayeux MC, et al. Impact of a computerised information system on quality of nutritional support in the ICU. Nutrition. 2006;22(3):221–9.
Tramonti N, Lema J, Araujo MB, Basílico H, Villasboas RM, Laborde S, et al. Resultados de la implementación de un protocolo de soporte nutricional en grandes quemados pediátricos internados en la Unidad de Cuidados Intensivos. Arch Argent Pediatr. 2018;116(4):e515–21.
Miquet Romero LM, Rodríguez Garcell R, Barreto Penié J, Santana PS. Estado de la provisión de cuidados nutricionales al paciente quemado: Auditoría de procesos en un Servicio de Quemados de un hospital terciario [Current status of nutritional care provision to burnt patients: processes audit of a burnt patients department from a tertiary hospital]. Nutr Hosp. 2008;23(4):354–65.
Medeiros NI, Schott E, Silva R, Czarnobay SA. Efeitos da terapia nutricional enteral em pacientes queimados atendidos em hospital público de Joinville/SC. Rev Bras Queimaduras. 2009;8(3):97–100.
Silva JP, Colombo-Souza P. Perfil alimentar de pacientes internados por queimaduras em hospital público especializado. Rev Bras Queimaduras. 2017;16(1):3–9.
Prather JL, Tummel EK, Patel AB, Smith DJ, Gould LJ. Prospective Randomized Controlled Trial Comparing the Effects of Noncontact Low-Frequency Ultrasound with Standard Care in Healing Split-Thickness Donor Sites. J Am Coll Surg. 2015;221(2):309–18.
Egan KG, Guest R, Sinik LM, Nazir N, De Ruyter M, Ponnuru S, et al. Evaluation of Liposomal Bupivacaine at Split-Thickness Skin Graft Donor Sites through a Randomized, Controlled Trial. J Burn Care Res. 2021;42(6):1280–5.
Hoogewerf CJ, Hop MJ, Nieuwenhuis MK, Oen IMMH, Middelkoop E, Van Baar ME. Topical treatment for facial burns. Cochrane Database Syst Rev. 2020;2020(7):1–84.
Kabuk A, Şendir M, Filinte G. The effect of reflexology massage and passive music therapy intervention before burn dressing on pain, anxiety level and sleep quality. Burns. 2022;48(7):1743–52.
do Vale AHB, da Videira RLR, Gomez DS, Carmona MJC, Tsuchie SY, Flório C, et al. Effect of nitrous oxide on fentanyl consumption in burned patients undergoing dressing change. Brazilian Journal of Anesthesiology. 2016;66(1):7–11.
Pinto DCS, Monteiro AA Jr, Mota WM, Almeida PCC, Goméz DS, Gemperli R. Custo- efetividade do uso do curativo de colágeno e alginato no tratamento de áreas doadoras de enxerto de pele de espessura parcial. Rev Bras Queimaduras. 2017;16(2):62–7.
Davodabady F, Naseri-Salahshour V, Sajadi M, Mohtarami A, Rafiei F. Randomized controlled trial of the foot reflexology on pain and anxiety severity during dressing change in burn patients. Burns. 2021;47(1):215–21.
Luca-Pozner V, Nischwitz SP, Conti E, Lipa G, Ghezal S, Luze H, et al. The use of a novel burn dressing out of bacterial nanocellulose compared to the French standard of care in paediatric 2nd degree burns – A retrospective analysis. Burns. 2022;48(6):1472–80.
Jorge JLG, Naif C, Marques EGSC, Andrade GAM, Lima RVKS, Müiller Neto BF, et al. Malha de algodão parafinado versus malha de fibra de celulose salinizada como curativo temporário de áreas doadoras de pele parcial. Rev Bras Queimaduras. 2015;14(2):103–8.
Jafarizadeh H, Lotfi M, Ajoudani F, Kiani A, Alinejad V. Hypnosis for reduction of background pain and pain anxiety in men with burns: A blinded, randomised, placebo-controlled study. Burns. 2018;44(1):108–17.
Burns-Nader S, Joe L, Pinion K. Computer tablet distraction reduces pain and anxiety in pediatric burn patients undergoing hydrotherapy: A randomised trial. Burns. 2017;43(6):1203–11.
Shoham Y, Krieger Y, Rubin G, Koenigs I, Hartmann B, Sander F, et al. Rapid enzymatic burn debridement: A review of the paediatric clinical trial experience. Int Wound J. 2020;17(5):1337–45.
Rosenberg L, Krieger Y, Bogdanov-Berezovski A, Silberstein E, Shoham Y, Singer AJ. A novel rapid and selective enzymatic debridement agent for burn wound management: A multi-center RCT. Burns. 2014;40(3):466–74.
Fahlstrom K, Boyle C, Makic MBF. Implementation of a nurse-driven burn resuscitation protocol: A quality improvement project. Crit Care Nurse. 2013;33(1):25–35.
Lawrence A, Faraklas I, Watkins H, Allen A, Cochran A, Morris S, et al. Colloid administration normalises resuscitation ratio and ameliorates “fluid creep.” J Burn Care Res. 2010;31(1):40–7.
Hershberger RC, Hunt JL, Arnoldo BD, Purdue GF. Abdominal compartment syndrome in the severely burned patient. J Burn Care Res. 2007;28(5):708–14.
Yano Y, Sakata N, Fushimi K. Establishing a hospital transfusion management system promotes appropriate clinical use of human albumin in Japan: a nationwide retrospective study. BMC Health Serv Res. 2019;19(1):1–11.
Caleman G, Morais JF, Puga MES, Riera R, Atallah AN. Use of albumin as a risk factor for hospital mortality among burn patients in Brazil: non-concurrent cohort study. Sao Paulo Med J. 2010;128(5):289–95.
Lemus-Lima E, Hernández-Pérez R, Beltrán-Borao BL, Molina-Borges M, Vázquez- Lazo C. Efectividad del esquema de reposición hídrica de Brooke modificado para el tratamiento del paciente quemado. Available from: http://orcid.org/0000-0003-2640-4698.
Castanon L, Asmar S, Bible L, Chehab M, Ditillo M, Khurrum M, et al. Early Enteral Nutrition in Geriatric Burn Patients: Is There a Benefit? Available from: https://doi.org/10.1093/jbcr/iraa109/5864763.
Mosier MJ, Pham TN, Klein MB, Gibran NS, Arnoldo BD, Gamelli RL, et al. Early enteral nutrition in burns: Compliance with guidelines and associated outcomes in a multicenter study. J Burn Care Res. 2011;32(1):104–9.
Mayes T, Gottschlich MM, Warden GD. Clinical nutrition protocols for continuous quality improvements in the outcomes of patients with burns. J Burn Care Rehabil. 1997;18(4):365–8.
Valentini M, Seganfredo FB, Fernandes SA. Terapia nutricional enteral pediátrica para vítimas de queimaduras: quando iniciar? Rev Bras Ter Intensiva. 2019;31(3):393–402.
Krebs ED, O’Donnell K, Berry A, Guidry CA, Hassinger TE, Sawyer RG. Volume- based feeding improves nutritional adequacy in surgical patients. Am J Surg. 2018;216(6):1155–9.
Real DSS, Reis RP, Piccolo MS, Okamoto RH, Gragnani A, Ferreira LM. Oxandrolone use in adult burn patients. systematic review and meta-analysis. Acta Cir Bras. 2014;29:68–76.
Sousa AES, Batista FOC, Martins TCL, Sales ALCC. O papel da arginina e glutamina na imunomodulação em pacientes queimados - revisão de literatura. Rev Bras Queimaduras. 2015;14(4):295–9.
Lagos JC, Paulos PA, Piñol BP. Comparación de dos técnicas de curación en pacientes quemados pediátricos. Rev pediatr Eléctron. 2018;15(2):2–10.
Moraes RZC, Frempong RFR, Freitas MS, Soares AUS, Pereira RO, Carvalho GG, et al. Análise comparativa da morbimortalidade antes e após implantação de protocolo de atendimento ao queimado. Rev Bras Queimaduras. 2014;13(3):142–8.
Abla H, Brown E, Pang A, Batchinsky M, Raghuram A, Venable A, et al. Synergistic Use of Novel Technological Advances in Burn Care Significantly Reduces Hospital Length of Stay Below Predicted: A Case Series. J Burn Care Res. 2022;43(6):1440–4.
Ong YS, Samuel M, Song C. Meta-analysis of early excision of burns. Burns. 2006;32(2):145–50.
Dolp R, Rehou S, McCann MR, Jeschke MG. Contributors to the length-of-stay trajectory in burn-injured patients. Burns. 2018;44(8):2011–7.
Torres LF. Células madre adultas como opción terapéutica para pacientes adultos con quemaduras que comprometen más del 50 por ciento de la superficie corporal total. Revista Salud Bosque. 2015;5(1):55–62.
Villegas JC, Torres EE, Pedreros CP, Singh EPO, Longton CB, Said JCS, et al. Mortalidad tras un año de protocolización en el manejo del paciente quemado. Rev Chilena de Cirurgia. 2010;62(2):144–9.
Ziolkowski N, Rogers AD, Xiong W, Hong B, Patel S, Trull B, et al. The impact of operative time and hypothermia in acute burn surgery. Burns. 2017;43(8):1673–81.
Austin RE, Merchant N, Shahrokhi S, Jeschke MG. A comparison of Biobrane™ and cadaveric allograft for temporising the acute burn wound: Cost and procedural time. Burns. 2015;41(4):749–53.
Lim J, Liew S, Chan H, Jackson T, Burrows S, Edgar DW, et al. Is the length of time in acute burn surgery associated with poorer outcomes? Burns. 2014;40(2):235–40.
Lukish JR, Eichelberger MR, Newman KD, Pao M, Nobuhara K, Keating M, et al. The use of a bioactive skin substitute decreases length of stay for pediatric burn patients. J Pediatr Surg. 2001;36(8):1118–21.
Barreto MGP, Costa MGNF, Serra MCVF, Afiune JB, Praxedes HEP, Pagani E. Estudo comparativo entre tratamento convencional e tratamento com heparina tópica para a analgesia de queimaduras. Rev Assoc Med Bras. 2010;56(1):51–5.
Deng H, Chen J, Li F, Li-Tsang CWP, Liu Q, Ma X, et al. Effects of mobility training on severe burn patients in the BICU: A retrospective cohort study. Burns. 2016;42(7):1404–12.
de Figueiredo TB, Utsunomiya KF, de Oliveira AMRR, Pires-Neto RC, Tanaka C. Mobilization practices for patients with burn injury in critical care. Burns. 2020;46(2):314–21.
Chen HQ, Shen MY, Shao HW, Han CM. Practice of nosocomial infection management in burn department based on the American hospital evaluation standard of the Joint Commission International. Zhonghua Shao Shang Za Zhin. 2020;36(6):488–92.
Krasnoff CC, Grigorian A, Chin T, Joe V, Kong A, Barrios C, et al. Pediatric burn- trauma patients have increased length of stay compared to trauma-only patients: A propensity matched analysis. Burns. 2021;47(1):78–83.
Popp JA, Layon AJ, Nappo R, Richards WT, Mozingo DW. Hospital-acquired infections and thermally injured patients: Chlorhexidine gluconate baths work. Am J Infect Control. 2014;42(2):129–32.
Kagan RJ, Neely AN, Rieman MT, Hardy A, Warner P, Bailey JK, et al. A performance improvement initiative to determine the impact of increasing the time interval between changing centrally placed intravascular catheters. J Burn Care Res. 2014;35(2):143–7.
Klein MB, Goverman J, Hayden DL, Fagan SP, McDonald-Smith GP, Alexander AK, et al. Benchmarking outcomes in the critically injured burn patient. Ann Surg. 2014;259(5):833–41.
Saaiq M, Zaib S, Ahmad S. Early excision and grafting versus delayed excision and grafting of deep thermal burns up to 40% total body surface area: A comparison of outcome. Ann Burns Fire Disasters. 2012;25(3):143–7.
Le BS. estubazioni non pianificate nelle terapie intensive: quali implicazioni per l´assistenza infermieristica? [Accidental extubation in intensive care units: what implications for nursing care?]. Assist Inferm Ric. 2004;23(1):36–47.
Maguiña P, Kirkland-Walsh H. Hospital-acquired pressure ulcer prevention: A burn surgeon’s team approach. J Burn Care Res. 2014;35(5):e287–93.
Rogers AD, Saggaf M, Ziolkowski N. A quality improvement project incorporating preoperative warming to prevent perioperative hypothermia in major burns. Burns. 2018;44(5):1279–86.
de Morais Carneiro JMGV, Alves J, Conde P, Xambre F, Almeida E, Marques C, et al. Factor XIII-guided treatment algorithm reduces blood transfusion in burn surgery. Braz J Anesthesiol. 2018;68(3):238–43.
Butts CC, Bose K, Frotan MA, Hodge J, Gulati S. Controlling intraoperative hemorrhage during burn surgery: A prospective, randomised trial comparing NuStat® hemostatic dressing to the historic standard of care. Burns. 2017;43(2):374–8.
Clark DE, Lowman JD, Griffin RL, Matthews HM, Reiff DA. Effectiveness of an early mobilisation protocol in a trauma and burns intensive care unit: A retrospective cohort study. Phys Ther. 2013;93(2):186–96.
Jain M, Khadilkar N, De Sousa A. Burn-related factors affecting anxiety, depression and self-steem in burn patients: An exploratory study. Ann Burns Fire Disasters. 2017;30(1):30–4.
Harorani M, Davodabady F, Masmouei B, Barati N. The effect of progressive muscle relaxation on anxiety and sleep quality in burn patients: A randomised clinical trial. Burns. 2020;46(5):1107–13.
Mandell SP, Robinson EF, Cooper CL, Klein MB, Gibran NS. Patient safety measures in burn care: Do national reporting systems accurately reflect quality of burn care? J Burn Care Res. 2010;31(1):125–9.
Zakeri S, Shafipour V, Yazdani Charati J, Ghasemi Charati F, Jafari H. Investigating the effect of seeing patients’ pre-burn face photo on the quality of care and level of empathy of nurses with patients admitted to BICU. Burns. 2021;47(8):1906–11.
Friedstat JS, Ryan CM, Gibran N. Outcome Metrics After Burn Injury: From Patient- Reported Outcome Measures to Value-Based Health Care. Clin Plast Surg. 2017;44(4):911–5.
Louri NA, Dey N, Ebrahim FK, Jose J, Philip S, Shanmugasundaram T, et al. Epidemiology of burn at a military hospital in Bahrain: initial experience of patient outcomes and quality indicators. Int J Burn Trauma [Internet]. 2018;8(3):54–62. Available from: www.IJBT.org.
Seyed-Forootan K, Karimi H, Motevalian SA, Momeni M, Safari R, Ghadarjani M. LA50 IN BURN INJURIES. Ann Burns Fire Disasters. 2016;29(1):14–7.
Frugoni B, Gabriel RA, Rafaat K, Abanobi M, Rantael B, Brzenski A. A predictive model for prolonged hospital length of stay in surgical burn patients. Burns. 2020;46(7):1565–70.
Smith RR, Hill DM, Hickerson WL, Velamuri SR. Analysis of factors impacting length of stay in thermal and inhalation injury. Burns. 2019;45(7):1593–9.
Hussain A, Dunn KW. Predicting length of stay in thermal burns: A systematic review of prognostic factors. Burns. 2013;39(7):1331–40.
Taylor SL, Sen S, Greenhalgh DG, Lawless MB, Curri T, Palmieri TL. Not all patients meet the 1 day per percent burn rule: A simple method for predicting hospital length of stay in patients with burn. Burns. 2017;43(2):282–9.
Gibbs D, Ehwerhemuepha L, Moreno T, Guner Y, Yu P, Schomberg J, et al. Prolonged hospital length of stay in pediatric trauma: a model for targeted interventions. Pediatr Res. 2021;90(2):464–71.
Amani H, Dougherty WR, Blome-Eberwein S. Use of Transcyte® and dermabrasion to treat burns reduces length of stay in burns of all size and etiology. Burns. 2006;32(7):828–32.
Chao T, Parry I, Palackic A, Sen S, Spratt H, Mlcak RP, et al. The effects of short bouts of ergometric exercise for severely burned children in intensive care: A randomised controlled trial. Clin Rehabil. 2022;36(8):1052–61.
Patterson KN, Onwuka A, Horvath KZ, Fabia R, Giles S, Marx D, et al. Length of Stay per Total Body Surface Area Burn Relative to Mechanism: A Pediatric Injury Quality Improvement Collaborative Study. J Burn Care Res. 2022;43(4):863–7.
da Silva Maciel AB, Ortiz JF, Siqueira BS, Zanette GF. Tissue healing efficacy in burn patients treated with 1% silver sulfadiazine versus other treatments: a systematic review and meta-analysis of randomised controlled trials. An Bras Dermatol. 2019;94(2):204–10.
Yelvington M, Godleski M, Lee AF, Goverman J, Parry I, Herndon DN, et al. Contracture Severity at Hospital Discharge in Children: A Burn Model System Database Study. J Burn Care Res. 2021;42(3):425–33.
Goverman J, Mathews K, Goldstein R, Holavanahalli R, Kowalske K, Esselman P, et al. Adult Contractures in Burn Injury: A Burn Model System National Database Study. J Burn Care Res. 2017;38(1):e328–36.
Godleski M, Lee AF, Goverman J, Herndon DN, Suman OE, Kowalske KJ, et al. Quantifying Contracture Severity at Hospital Discharge in Adults: A Burn Model System National Database Study. J Burn Care Res. 2018;39(4):604–11.
Costa ACSM, Santos KA, Santos CRV. Intervenção fisioterapêutica no paciente queimado: uma abordagem pneumofuncional em estudo piloto. Rev Bras Queimaduras. 2016;15(2):69–73.
Souza TJA. Qualidade de vida do paciente internado em uma unidade de queimados. Revista Brasileira de Cirurgia Plástica. 2011;26(1):10–5.
Guimarães IBA, Martins ABT, Guimarães SB. Qualidade de vida de pacientes com queimaduras internados em um hospital de referência no nordeste brasileiro. Rev Bras Queimaduras. 2013;12(2):103–7.
Silva AFR, Oliveira LP, Vale MB, Batista KNM. Análise da qualidade de vida de pacientes queimados submetidos ao tratamento fisioterapêutico internados no Centro de Tratamento de Queimados. Rev Bras Queimaduras. 2013;12(4):260–4.
Gómez Martín C, García Morato RA, de los Reyes Cortés N, Fernández-Cañamaque JL, Holguín P. Patient satisfaction in a Spanish burn unit. Burns. 2019;45(2):341–7.
Pompermaier L, Af Hagelsrum ED, Ydenius V, Sjöberg F, Steinvall I, Elmasry M. Patient Reported Experiences at a Swedish National Burn Centre. J Burn Care Res. 2022;43(1):249–55.
Lunardi N, Mehta A, Ezzeddine H, Varma S, Winfield RD, Kent A, et al. Unplanned readmission after traumatic injury: A long-term nationwide analysis. J Trauma Acute Care Surg. 2019;87(1):188–94.
Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15(6):523–30. https://doi.org/10.1093/intqhc/mzg081. (PMID: 14660535).
Gus E, Almeland SK, Barnes D, Elmasry M, Singer Y, Sjöberg F, et al. Burn Unit Design - The Missing Link for Quality and Safety. J Burn Care Res. 2021;42(3):369–75.
American Burn Association. Verifcation Criteria 2023 Dev Update; 2023. https://ameriburn.org/quality-care/verification/verification-criteria/verification-criteria-effective-october-1-2019/. Accessed February 6 2024.
Brychta P. European practice guidelines for burn care: minimum level of burn care provision in Europe. In: Jeschke MG, Kamolz LP, Sjöberg F, Wolf SE, editors. Handbook of Burns. Vienna: Springer; 2012. https://doi.org/10.1007/978-3-7091-0348-7_6.
ISBI Practice Guidelines Committee; Steering Subcommittee; Advisory Subcommittee. ISBI Practice Guidelines for Burn Care. Burns. 2016;42(5):953–1021. https://doi.org/10.1016/j.burns.2016.05.013. (PMID: 27542292).
Mccloskey BA, Diers DK. Effects of New Zealand’s Health Reengineering on Nursing and Patient Outcomes. Med Care. 2005;43(11):1140–6.
Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giovannetti P. The Impact of Hospital Nursing Characteristics on 30-Day Mortality. J Nurs Adm. 2011;41(7–8 Suppl):S58–68. Available from: http://journals.lww.com/jonajournal.
Jeschke MG, Gauglitz GG, Kulp GA, Finnerty CC, Williams FN, Kraft R, Suman OE, Mlcak RP, Herndon DN. Long-term persistance of the pathophysiologic response to severe burn injury. PLoS One. 2011;6(7):e21245. https://doi.org/10.1371/journal.pone.0021245. Epub 2011 July 18. PMID: 21789167; PMCID: PMC3138751.
Wasiak J, Cleland H, Jeffery R. Early versus delayed enteral nutrition support for burn injuries. Cochrane Database Syst Rev. 2006;(3):CD005489. https://doi.org/10.1002/14651858.CD005489.pub2.
Datta PK, Roy Chowdhury S, Aravindan A, Saha S, Rapaka S. Medical and surgical care of critical burn patients: a comprehensive review of current evidence and practice. Cureus. 2022;14(11):1–13.
Kao Y, Loh EW, Hsu CC, Lin HJ, Huang CC, Chou YY, et al. Fluid Resuscitation in Patients With Severe Burns: A Meta-analysis of Randomized Controlled Trials. Acad Emerg Med. 2018;25(3):320–9.
Woolard A, Hill NTM, McQueen M, Martin L, Milroy H, Wood FM, et al. The psychological impact of paediatric burn injuries: a systematic review. BMC Public Health. 2021;21(1):1–27.
Hu Y, Li D, Xu L, Hu Y, Sang Y, Zhang G, et al. Epidemiology and outcomes of bloodstream infections in severe burn patients: a six-year retrospective study. Antimicrob Resist Infect Control. 2021;10(1):1–8.
Belba MK, Petrela EY, Belba AG. Epidemiology and outcome analysis of sepsis and organ dysfunction/failure after burns. Burns. 2017;43(6):1335–47.
Hardwicke J. The influence of outcomes on the provision and practice of burn care. Burns. 2016;42(2):307–15.
Pham TN, Goldstein R, Carrougher GJ, Gibran NS, Goverman J, Esselman PC, et al. The impact of discharge contracture on return to work after burn injury: A Burn Model System investigation. Burns. 2020;46(3):539–45.
Acknowledgements
To Fernanda Almeida Ribeiro for assisting in obtaining some manuscripts.
Funding
This research was funded by Fundação de Apoio a Pesquisa do Distrito Federal (FAPDF), Brasília, Distrito Federal, Brazil.
Author information
Authors and Affiliations
Contributions
DS was the main author and worked at all stages of the study. VM worked on the elaboration of the research strategy, the selection of the included studies, and the revision of the manuscript. LS worked on the elaboration of the research strategy and the revision of the manuscript. JA worked on the selection of the included studies and the review of the manuscript. FA, GM and LG worked on the revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Suzuki, D.R.R., Santana, L.A., Ávila, J.E.H.G. et al. Quality indicators for hospital burn care: a scoping review. BMC Health Serv Res 24, 486 (2024). https://doi.org/10.1186/s12913-024-10980-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10980-7