Abstract
The aim of this study is to identify (1) the extent of work-related stress and (2) stressors associated with cognitive and behavioral stress reactions, burnout symptoms, health status, quality of sleep, job satisfaction, and intention to leave the organization and the profession among health professionals working in acute care /rehabilitation hospitals, psychiatric hospitals, nursing homes, and home care organizations.
Background
Health professionals are faced with various stressors at work and as a consequence are leaving their profession prematurely. This study aimed to identify the extent of work-related stress and stressors associated with stress reactions, job satisfaction, and intention to leave and health-related outcomes among health professionals working in different healthcare sectors (acute care, rehabilitation and psychiatric hospitals, nursing homes and home care organizations).
Methods
This study is based on a repeated cross-sectional design, which includes three data measures between 2017 and 2020 and 19,340 participating health professionals from 26 acute care / rehabilitation hospitals, 12 psychiatric hospitals, 86 nursing homes and 41 home care organizations in Switzerland. For data analysis, hierarchical multilevel models (using AIC) were calculated separately for hospitals, nursing homes, and home care organizations, regarding health professionals’ stress symptoms, job satisfaction, intention to leave the organization / profession, general health status, burnout symptoms, and quality of sleep.
Results
The main findings reveal that the incompatibility of health professionals’ work and private life was significantly associated (p < 0.05) with their stress reactions, job satisfaction, intention to leave, and health-related outcomes in all the included work areas. The direct supervisor’s good leadership qualities were also associated with health professionals’ job satisfaction regarding all work areas (B ≥ 0.22, p = 0.000). In addition, a positive perceived bond with the organization (B ≥ 0.13, p < 0.01) and better development opportunities (B ≥ 0.05, p < 0.05) were associated with higher job satisfaction and a lower intention to leave the organization and profession among health professionals. Also, a younger age of health professionals was associated with a higher intention to leave the organization and the profession prematurely in all the included work areas. High physical (B ≥ 0.04, p < 0.05) and quantitative demands (B ≥ 0.05, p = 0.000) at work were also associated with negative health-related outcomes.
Similar content being viewed by others
Introduction
Around the globe, healthcare systems are struggling with a shortage of health professionals and a potential destabilization of the quality and availability of care provided [1]. Work-related stress and poor working conditions are among the main reasons why health professionals leave their profession prematurely [2,3,4]. As recent studies show, the COVID-19 pandemic has further exacerbated the problem of stress and poor working conditions among health professionals in various countries and work areas [5,6,7].
Work-related stress can be defined as “a pattern of reactions that occur when workers are confronted with demands or pressures that are not matched to their knowledge, abilities and skills, and which challenge their ability to cope” [8, 9]. The model of ‘causes and consequences of work-related stress’ [8, 10] is the underlying theoretical background of this study. It explains the causes of stress (stressors), stress reactions (short-term), and consequences of work-related stress (long-term) on the employee as well as their inter-reactions (stressors are associated with stress reactions and long-term consequences) [8, 10]. Stressors at work are particularly pronounced in the daily work of health professionals, such as high emotional demands due to confrontation with sickness and death, or aggression at work, or high physical demands when lifting or moving patients [11,12,13]. Working under time pressure, doing overtime, long working hours, and understaffing are also well-known stressors among health professionals [14,15,16]. In addition, they are confronted with a lack of opportunities for development, poor leadership qualities of superiors and a high exposure to infectious disease or hazardous substances in their daily work [4, 17]. Furthermore, they are strongly affected by incompatibilities of work and private life, shift work, and problems with demarcation between work and leisure time [4, 18,19,20]. As previous studies indicate, a high level of stressors at work is associated with health professionals’ increasing anxiety, depression, job dissatisfaction, and the intention to leave their profession prematurely [21, 22].
There are multiple studies regarding stressors, stress reactions, and long-term consequences among health professionals working in different management levels [23, 24], professional roles [2, 3, 21, 25], or work areas [14, 26, 27]. However, most studies focus on one specific work area (e.g., acute care hospitals or nursing homes) [3, 15, 19] or on only one specific health profession (e.g., nurses) [14, 28]. Thus, studies with a focus on work-related stress among health professionals combining and comparing different work areas in the healthcare sector are rare.
Therefore, the aim of this study is to identify (1) the extent as well as differences of work-related stress in various work areas and (2) stressors associated with cognitive and behavioral stress reactions, burnout symptoms, health status, quality of sleep, job satisfaction, and intention to leave the organization and the profession among health professionals working in acute care /rehabilitation hospitals, psychiatric hospitals, nursing homes, and home care organizations.
Methods
Design
This study presents the results of the national STRAIN project ‘work-related stress among health professionals in Switzerland’ [4, 23]. These results are based on a repeated cross-sectional design, using three measurements between September 2017 – March 2018 (T0), January – April 2019 (T1), and March – September 2020 (T2), conducted among Swiss health professionals working in acute care / rehabilitation hospitals, psychiatric hospitals, nursing homes, and home care organizations. Only 4% of participants took part in all three measurement points. Participating organizations were free to choose the time for data collection when it suited them best.
Recruitment and study sample
For recruitment, potential healthcare organizations were randomly selected from a register (Swiss Federal Statistical Office in 2016) of all hospitals, nursing homes, and home care organizations in Switzerland. We excluded organizations that were too small in size (average number of beds < 20, fewer than 7 employees) or that were specialized (e.g., in neonatology) [23]. The randomization process was computer-based using randomizer.org and considered a geographically representative sample for Switzerland (69% Swiss or Standard German-speaking, 23% French-speaking, 8% Italian-speaking). Thereby, 100 hospitals, 100 nursing homes, and 100 home care organizations were randomly selected and invited to participate in the study. The invited organizations received information about the study using a study flyer and a short film. In the end, a total of 26 acute care / rehabilitation hospitals, 12 psychiatric hospitals, 86 nursing homes, and 41 home care organizations (117 German-speaking, 39 French-speaking, 9 Italian-speaking) took part in the study.
Data collection
For the data collection, a contact person in each participating organization was responsible for distributing the questionnaire. The questionnaire was distributed to all healthcare professionals working in the organization at the time of data collection. Nurses, midwives, physicians, medical-technical professionals, medical-therapeutic professionals, and employees from the administration and research at all hierarchies and skill levels (e.g., health professionals in training) were included in the study. The questionnaire was available in German, French, and Italian in two online versions (Surveymonkey®, UmfrageOnline®), as well as in a paper version. Participating health professionals had one month to complete the questionnaire and received a reminder after the first two weeks during the data collection period. The data collection was on a voluntary basis for all participating organizations as well as all participating health professionals within them.
STRAIN – questionnaire
The study used the STRAIN questionnaire, which is designed based on the model of ‘causes and consequences of work-related stress’ [8, 10] and, therefore, is composed of scales assessing stressors at work (e.g., demands at work, work–private life conflict), stress reactions (behavioral and cognitive stress reactions) and long-term consequences (e.g., burnout symptoms, job satisfaction, general health status, quality of sleep, intention to leave the organization or profession). The STRAIN questionnaire consists of widely used, valid, and reliable scales (e.g., on quantitative demands, influence at work, role clarity) from the Copenhagen Psychosocial Questionnaire (COPSOQ) [29, 30], which is the questionnaire used in the ‘Nurses Early Exit Study’ (NEXT) [31, 32]. The COPSOQ item responses are scored on a five-point Likert scale (to a very large extent, to a large extent, somewhat, to a small extent, to a very small extent, or always, often, sometimes, seldom, never/hardly ever). COPSOQ scale score value ranges from 0 (to a very small extent or never/hardly ever) to 100 (to a very large extent or always). In addition, the 4-item scale on physical demands from the sixth European Working Conditions Survey – EWCS [33] (7-point Likert scale) and the self-rated general health status on a range from 0 (worst health, you can imagine) to 100 (best health, you can imagine) (using EQ-5D-5L [34] were included. Further details on the STRAIN questionnaire were published previously [4, 36, 37].
Data analysis
Data were analyzed using SPSS 25® and R Studio 4.2.2 [37]. According to the original author, all items from the COPSOQ, EWCS and NEXT were transformed to a value range from 0 (minimum value) to 100 points (maximum value) [29, 33]. If less than half of the questions in a scale were answered, no average score was calculated [29].
In the first step, we calculated the descriptive statistics describing the study sample divided into the included work areas (hospitals, nursing homes, home care organization).
In the second step, we calculated the extent of stressors, stress reactions, and long-term consequences among health professionals working in acute care/ rehabilitation hospitals, psychiatric hospitals, nursing homes, and home care organizations and tested for significant differences using the Kruskal–Wallis H test (significance level of 0.05, using the Bonferroni correction for multiple tests) as well as a pairwise comparison (Dunn-Bonferroni tests), since the test of homogeneity of variance was significant. There were no equal-sized samples of data.
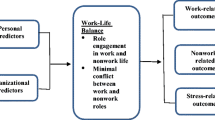
In the third step, we calculated separate hierarchical multiple regression models for (1) acute care /rehabilitation hospitals, (2) psychiatric hospitals, (3) nursing homes, and (4) home care organizations using health professionals’ data’ (level 1) nested in organizations (level 2). Regression models were calculated for the following outcome variables: behavioral stress symptoms; cognitive stress symptoms; job satisfaction; intention to leave the organization; intention to leave the profession; general health status; burnout symptoms; and quality of sleep. All the independent variables included in the regression models are presented in Fig. 1. A backward model selection with the MASS package was conducted with Akaike Information Criterion [38]. The models were then fitted using the lme4 package. We computed standardized and nonstandardized beta coefficients, p-values, standard errors, CI, and R-squared (marginal / conditional) [39, 40]. Since the assumption of heteroskedasticity was not met for the models, standard errors, p-values, and CI were bootstrapped (r = 999, bias corrected and accelerated, 95% CI).
Results
Study sample description
A total of 19,340 health professionals took part in the study. Participants were mainly women (83%) and from the German-speaking part of Switzerland (83% German-speaking, 15% French-speaking, 2% Italian-speaking). The study sample included registered nurses (48%), nurse assistants (28%), midwives (1%), medical-technical (3%), medical-therapeutic professionals (9%), physicians (7%), employees in administration and research (3%), and social services (2%). Most participants had no management responsibilities (84%), 11% worked in a lower, 4% in a middle, and 2% in an upper management position. Table 1 provides further details on the distribution of sex, language region, profession, and leadership positions of the participants working in acute care / rehabilitation hospitals, psychiatric hospitals, nursing home, and home care organizations.
Extent of work-related stress in different work areas
Table 2 shows an overview of the extent of various stressors, stress reactions, and long-term consequences among health professionals working in different work areas in the healthcare sector (hospitals, nursing homes, home care organizations).
Extent of various stressors at work
The results on various work stressors shows that health professionals working in acute care and rehabilitation hospitals reported the highest quantitative (e.g., work at a high pace, doing overtime) demands (M = 59.3; SD = 15.5), and sensorial (e.g., precision, vision, attention) demands (M = 86.2; SD = 13.5) at work. Health professionals working in acute care and rehabilitation hospitals also reported having the most demanding work environment (e.g., being exposed to noise, cold, chemicals) (M = 38.4; SD = 19.5) and the lowest influence at work (e.g., the degree of influence with regard to work) (M = 48.0; SD = 20.1) compared to other work areas. In addition, the perceived rewards (M = 54.3; SD = 26.3) and the quality of leadership of the superior at work (e.g., the superior is good at work planning, solving conflicts) (M = 62.7; SD = 22.6) were lowest among health professionals working in acute care / rehabilitation hospitals. Social support received at work from colleagues or superiors (M = 75.6; SD = 16.9) and feedback (M = 49.3, SD = 20.9) was also lowest, while they reported the highest scores on role conflicts due to contradicting role requirements at work (M = 39.2; SD = 20.2). Furthermore, they showed the highest insecurity in terms of the working environment (e.g., due to changes in shift schedules) (M = 31.6, SD = 25.7). In addition, this group reported the highest incompatibility between work and private life (M = 30.8, SD = 21.4) and difficulties with demarcation (e.g., being available in leisure time for work issues) (M = 34.7, SD = 22.0) compared to other work areas.
In psychiatric hospitals, health professionals revealed they have the lowest meaning of work (e.g., perceiving work as meaningful / important) (M = 79.3; SD = 17.4) compared to other work areas. In addition, role clarity (e.g., clear work tasks, objectives, area of responsibility) (M = 73.4; SD = 15.2) was lowest in psychiatric hospitals compared to health professionals working in other work areas.
In nursing homes, health professionals reported the highest emotional (e.g., confrontation with death, aggressive patients) (M = 68.3; SD = 15.6) and physical (e.g., lifting or moving people or heavy loads) (M = 46.8; SD = 23.5) demands at work. In this sector of healthcare, health professionals’ feeling of unfair behavior (e.g., feeling unjustly criticized by colleagues/superior) was also highest (M = 16.9, SD = 23.6) among those working in a nursing home compared to other work areas.
Health professionals working in home care organizations reported receiving less feedback from colleagues / their superior (M = 49.3, SD = 20.7) and to have the lowest social relations at work (e.g., the opportunity to talk to colleagues during work) (M = 36.0; SD = 30.1).
Extent of stress reactions and long-term consequences
Health professionals working in acute hospital or rehabilitation hospitals were most affected by cognitive stress symptoms (e.g., problems concentrating, taking decisions) (M = 28; SD = 19.8), showed higher burnout symptoms (M = 43.59; SD = 20.87), and had lower quality sleep (M = 66.81; SD = 19.12). They also revealed having lower job satisfaction (M = 69.2, SD = 14.8) and the highest intention to leave the organization (M = 17.5; SD = 21.9) or their profession prematurely (M = 17.5, SD = 21.9). Health professionals working in psychiatric hospitals also revealed a high intention to leave the organization (M = 22.5, SD = 22.9). Those health professionals working in nursing homes also showed lower scores regarding their job satisfaction (M = 69.9, SD = 14.7) and higher burnout symptoms (M = 42.8, SD = 22.7).
Results of the regression analysis regarding stress reactions
Results of the multiple regression models revealed that an incompatibility of work and private life was associated with increased behavioral stress symptoms (B ≥ 0.45, p = 0.000) among health professionals working in all the included areas (acute care, rehabilitation or psychiatric hospitals, nursing homes, or home care organizations, see Table 3). In addition, nurse assistants (with a formal education: B ≥ 0.12, p = 0.000 and without a formal education: B ≥ 0.10, p = 0.000) working in acute care, rehabilitation hospitals, and home care organizations seemed to be more highly affected in terms of behavioral stress symptoms. High quantitative demands at work were also associated with increased behavioral stress symptoms among health professionals working in acute care, rehabilitation hospitals, and home care organizations (B ≥ 0.13, p = 0.000).
With regard to cognitive stress symptoms, the incompatibility of work and private life was also revealed as a significant predictor among health professionals working in all the included areas (B ≥ 0.31, p = 0.000). In addition, a lack of role clarity at work showed a significant association with health professionals’ increased cognitive stress symptoms in all the included areas (B≤-0.08, p < 0.01).
Results of the regression analysis regarding job satisfaction and intention to leave
Further results in Table 4 indicate that good leadership qualities of the direct supervisor were associated with health professionals’ job satisfaction in all the included areas (B ≥ 0.22, p = 0.000). Moreover, health professionals’ positive perceived bond with the organization (B ≥ 0.16, p = 0.000), social community at work (e.g., atmosphere, co-operation, B ≥ 0.07, p = 0.000) and opportunities for development (B ≥ 0.13, p = 0.000) were associated with a higher satisfaction at work in all the included areas. The incompatibility of health professionals’ work and private life was shown to be associated with a poorer satisfaction at work in all the included areas (B≤-0.08, p = 0.000).
In addition, the results showed that a poor perceived compatibility of work and private life (B ≥ 0.17, p = 0.000), bond with the organization (B≤-0.13, p < 0.01), quality of leadership (B≤-0.10, p < 0.01), and opportunities for development (B≤-0.06, p < 0.01) were associated with health professionals’ higher intention to leave the organization in all the included areas. Furthermore, this higher intention to leave the organization was also associated with higher role conflicts (e.g., due to contradicting role requirements at work, B ≥ 0.05, p < 0.05) and a perceived unfair behavior (e.g., feeling unjustly criticized by colleagues/superior, B ≥ 0.05, p < 0.05) in all the included work areas.
The incompatibility of work and private life (B ≥ 0.19, p = 0.000), a poor perceived bond with the organization (B≤-0.11, p < 0.01) and a lack of opportunities for development (B≤-0.05, p < 0.05) were also associated with health professionals’ higher intention to leave the profession prematurely in all the included work areas. For health professionals working in hospitals and home care organizations, a lower meaning of work (B≤-0.07, p < 0.05) was also found to be a significant predictor for a higher intention to leave their profession prematurely. Moreover, further results showed that the younger the age of the health professionals, the higher their intention to leave the organization (B≤-0.08, p < 0.01) and their profession prematurely (B≤-0.09, p = 0.000) in all the included work areas.
Results of the regression analysis regarding health-related outcomes
The results in Table 5 on health professionals’ health-related outcomes revealed an incompatibility of work and private life (B≤-0.24, p < 0.01) as well as increased physical demands at work (e.g., lifting or moving people or heavy loads, B≤-0.09, p < 0.01) were associated with a poorer general health status among health professionals working in all the included areas. Physicians working in acute care, rehabilitation, and psychiatric hospitals reported a higher general health status (B ≥ 0.05, p < 0.05).
In addition, incompatibility between work and private life (B ≥ 0.38, p = 0.000) was associated with health professionals’ increased burnout-symptoms in all the included areas. Furthermore, high quantitative (B ≥ 0.05, p = 0.000) and physical (B ≥ 0.04, p < 0.05) demands at work were revealed as significant predictors for increased burnout symptoms among health professionals working in various areas. Further results showed that the younger the age, the higher the burnout symptoms (B≤-0.10, p = 0.000) for health professionals’ working in hospitals and nursing homes.
The incompatibility of health professionals’ work and private life was also significantly associated with a poor quality of sleep (B≤-0.31, p < 0.01) in all the included areas. In addition, a higher insecurity of the working environment (e.g., changes in shift schedules, B≤-0.06, p < 0.05) and difficulties with demarcation (e.g., being available in leisure time for work issues, B≤-0.05, p < 0.05) were associated with a poorer quality of sleep for health professionals working in hospitals and home care organizations. A demanding work environment (e.g., being exposed to noise, cold, chemicals, B≤-0.05, p < 0.05) was also significantly associated with health professionals’ poorer quality of sleep among those working in hospitals and nursing homes. Health professionals’ higher perceived meaning of work was associated with a better quality of sleep (B ≥ 0.06, p < 0.05) among those working in psychiatric hospitals and nursing homes. Further results relating to the specific field of work of health professionals are shown in Tables 3, 4 and 5.
Figure 2 presents an overview of the top four significant predictors of health professionals’ stress reactions, job satisfaction, intention to leave, and health-related outcomes for acute care / rehabilitation hospitals, psychiatric hospitals, nursing homes, and home care organizations.
Discussion
This study presents, for the first time, detailed results for health professionals working in different work areas in Switzerland and enables a direct comparison of working conditions among hospitals, nursing homes, and home care organizations. The results of this study indicate a higher extent of various stressors (e.g., higher quantitative, sensorial demands, role conflicts, and work-private life conflicts, lower influence at work, rewards, feedback, and quality of leadership), stress reactions (higher cognitive stress symptoms) and long-term consequences (e.g., lower job satisfaction and quality of sleep, higher intention to leave and burnout-symptoms) among health professionals working in acute care and rehabilitation hospitals (compared to other sectors). However, there are also relevant stressors regarding other work areas (e.g., high emotional and physical demands in nursing homes, the lower meaning of work and role clarity in psychiatric hospitals, lower feedback and social relations at work in home care organisations). This appears to be related to the specific role, job content and responsibilities of health professionals, their different working environments and the nature of patient care in these different areas of work [4, 41].
Further results of this study show that the incompatibility of work and private life is one of the most important predictors for health professionals’ increased stress reactions, job dissatisfaction, higher intention to leave the organization and the profession, as well as negative health-related outcomes in acute care, rehabilitation, and psychiatric hospitals, nursing homes, and home care organizations, which is in line with prior literature [4, 16, 18, 19]. A previous literature review including various EU and non-EU studies identified job satisfaction, work–life balance and career development as the main determinants for health professionals’ job retention [42]. A lack of opportunities for development was also associated with health professionals’ lower job satisfaction and greater intention to leave the organization and their profession in all the included work areas in this study.
Moreover, further results of this study revealed that good leadership qualities of the direct supervisor are also significantly associated with health professionals’ satisfaction at work in all the work areas included in this study. Previous studies indicate that health professional leaders have an important role regarding work-related stress among their employees [16, 43]. As the results of a previous review on leadership and health professionals’ job satisfaction conclude, it is important to identify and close the gaps in leadership knowledge and for leaders to play a key role in improving health professionals’ satisfaction at work [44].
Another important result of this study revealed that the intention to leave the organization and the profession prematurely was associated with a younger age of health professionals working in all of the included work areas. In addition, a younger age was also significantly associated with increased burnout symptoms for those working in acute care, rehabilitation, and psychiatric hospitals, and nursing homes. These results are essential regarding the shortage of health professionals in the future [1, 45]. Previous study results indicate that newly graduated health professionals are at risk of leaving their profession prematurely and also determined increased burnout symptoms [46, 47]. Especially during their first year of practice, 60–74% of newly graduated nurses showed the intention to leave their profession right away [48,49,50]. Several studies identified stressors at work (high quantitative demands, working overtime, work–private life conflicts), insufficient induction and support from colleagues and leaders, unfulfilled expectations along with a lack of support in finding one’s own role as possible causes [46, 47, 50, 51]. However, for an effective job retention of health professionals and an adequate future staffing in the healthcare sector, better support of young health professionals is essential. Therefore, evidence-based and effective programs to support newly graduated health professionals during their transition phase into daily practice are important in order to retain them for the long-term in the healthcare sector [52, 53].
Strengths and limitations
These results differ mainly from those of other studies because they are based on a large sample of health professionals (including nurses, midwives, physicians, medical-technical, and medical-therapeutic professionals) working in different work areas (acute care, rehabilitation, psychiatric hospitals, nursing homes, home care organizations) among different language regions (German, French, Italian). Moreover, the results of this study rely on several data measurements, using well established, valid, and reliable scales to assess work stressors, stress reactions, and long-term consequences.
However, participation in the study was on a voluntary basis for all the invited organizations and health professionals, and so a selection bias cannot be excluded (e.g., whether health professionals with higher levels of work-related stress did not participate due to restricted time resources). Also, nurses dominated the study sample in nursing homes and home care organizations, while in acute care, rehabilitation, and psychiatric hospitals a greater variation of health professions was represented. In addition, the third data measurement (T2) was conducted during the coronavirus pandemic, which could have had a negative impact on the willingness to participate by health professionals and also on their self-reports with regard to stressors and consequences at work. The generalisability of the results may be limited, as nurses and midwives are slightly overrepresented in the study sample.
Conclusions
Strategies for practice organisations, shaped to their specific working conditions regarding salient stressors in their area of work, are important (e.g., reducing workload and work-private live conflicts among health professionals in acute care and rehabilitation hospitals, stronger emotional support and use of patient lifter to reduce physical demands in nursing homes, improving role clarity in psychiatric hospitals and improving information transfer and team communication in home care organisations.
In addition, the importance of a good work–life balance, actively managing staff career development, and fostering staff commitment to their organization have emerged as key topics for healthcare organizations in all sectors to keep their staff healthy and satisfied in the long term. Furthermore, as the results of this study indicate, leaders should be aware of the most relevant stressors in their work area. While there are common stressors (e.g. work–private life conflicts, lack of opportunities for development), there are also differences across settings (as presented in Fig. 2). As our results show, it is also important to pay special attention to young health professionals in order to keep them in the healthcare system long-term and are not lost as soon as they enter the workforce. Therefore, evidence-based, effective, and interprofessional programs are important in order to better support young health professionals in dealing with stressors at work and finding their role during their transition phase. On the one hand, health organizations as employers are in demand, and on the other hand, the educational organizations that train future health professionals.
Data availability
The raw data set analyzed in the current study is available from the corresponding author on reasonable request.
References
WHO. Global strategy on human resources for health: workforce 2030. Geneva: World Health Organization; 2016.
Addor V, Schwendimann R, Gauthier JA, Wernli B, Jäckel D, Paignon A. «Nurses at work» – studie zu den Laufbahnen Im Pflegeberuf über die letzten 40 Jahre in Der Schweiz. Neuchâtel: Schweizerisches Gesundheitsobservatorium; 2016.
Hämmig O. Explaining burnout and the intention to leave the profession among health professionals - a cross-sectional study in a hospital setting in Switzerland. BMC Health Service Res. 2018;18:785. https://doi.org/10.1186/s12913-018-3556-1.
Peter KA, Hahn S, Schols J, Halfens R. Work-related stress among health professionals in Swiss acute care and rehabilitation hospitals-A cross-sectional study. J Clin Nurs. 2020;29:3064–81. https://doi.org/10.1111/jocn.15340.
Martínez-López JÁ, Lázaro-Pérez C, Gómez-Galán J. Burnout among direct-care workers in nursing homes during the COVID-19 pandemic in Spain: A Preventive and Educational Focus for sustainable workplaces. Sustainability. 2021;13:2782.
Mattila E, Peltokoski J, Neva MH, Kaunonen M, Helminen M, Parkkila A-K. COVID-19: anxiety among hospital staff and associated factors. Ann Med. 2021;53:237–46. https://doi.org/10.1080/07853890.2020.1862905.
Pniak B, Leszczak J, Adamczyk M, Rusek W, Matłosz P, Guzik A. Occupational burnout among active physiotherapists working in clinical hospitals during the COVID-19 pandemic in south-eastern Poland. Work. 2021;68:285–95. https://doi.org/10.3233/WOR-203375.
Eurofound. Work-related stress. Dublin: Eurofound; 2005.
Leka S, Jain A. Health impact of psychosocial hazards at work: an overview. Geneva: World Health Organization; 2010.
Kompier M, Marcelissen F. Handbook of work stress: a systematic Approach for Organizational Practice. Amsterdam: NIA; 1990.
Hahn S, Hantikainen V, Needham I, Kok G, Dassen T, Halfens RJ. Patient and visitor violence in the general hospital, occurrence, staff interventions and consequences: a cross-sectional survey. J Adv Nurs. 2012;68:2685–99. https://doi.org/10.1111/j.1365-2648.2012.05967.x.
Lim J, Bogossian F, Ahern K. Stress and coping in Australian nurses: a systematic review. Int Nurs Rev. 2010;57:22–31. https://doi.org/10.1111/j.1466-7657.2009.00765.x.
Long MH, Johnston V, Bogossian F. Work-related upper quadrant musculoskeletal disorders in midwives, nurses and physicians: a systematic review of risk factors and functional consequences. Appl Ergon. 2012;43:455–67. https://doi.org/10.1016/j.apergo.2011.07.002.
Aiken LH, Sloane DM, Bruyneel L, van den Heede K, Sermeus W, Consortium RC. Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud. 2013;50:143–53. https://doi.org/10.1016/j.ijnurstu.2012.11.009.
Dhaini SR, Zuniga F, Ausserhofer D, Simon M, Kunz R, de Geest S, Schwendimann R. Care workers health in Swiss nursing homes and its association with psychosocial work environment: a cross-sectional study. Int J Nurs Stud. 2016;53:105–15. https://doi.org/10.1016/j.ijnurstu.2015.08.011.
Peter KA, Halfens R, Hahn S, Schols J. Factors associated with work-private life conflict and leadership qualities among line managers of health professionals in Swiss acute and rehabilitation hospitals – a cross-sectional study. BMC Health Serv Res. 2021;21:81. https://doi.org/10.1186/s12913-021-06092-1.
NIOSH. Exposure to Stress.: National Institute for Occupational Safety and Health; 2008.
Albertsen K, Rafnsdottir GL, Grimsmo A, Tomasson K, Kauppinen K. Workhours and worklife balance. Scand J Work Env Hea. 2008;5:14–21.
Hausler N, Bopp M, Hammig O, Effort-Reward, Imbalance. Work-privacy conflict, and Burnout among Hospital employees. J Occup Environ Med. 2018;60:e183–7. https://doi.org/10.1097/JOM.0000000000001287.
Peter KA, Meier-Kaeppeli B, Pehlke-Milde J, Grylka-Baeschlin S. Work-related stress and intention to leave among midwives working in Swiss maternity hospitals – a cross-sectional study. BMC Health Serv Res. 2021. https://doi.org/10.1186/s12913-021-06706-8.
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–93. https://doi.org/10.1001/jama.288.16.1987.
Weibelzahl S, Reiter J, Duden G. Depression and anxiety in healthcare professionals during the COVID-19 pandemic. Epidemiol Infect. 2021;149:e46. https://doi.org/10.1017/S0950268821000303.
Peter KA, Schols J, Halfens R, Hahn S. Investigating work-related stress among health professionals at different hierarchical levels: a cross-sectional study. Nurs Open. 2020;7:969–79. https://doi.org/10.1002/nop2.469.
Skakon J, Kristensen TS, Christensen KB, Lund T, Labriola M. Do managers experience more stress than employees? Results from the intervention project on absence and well-being (IPAW) study among Danish managers and their employees. Work (Reading Mass). 2011;38:103–9. https://doi.org/10.3233/wor-2011-1112.
Streit S, Da Costa BR, Christensen S, Tal K, Tandjung R, Juni P. One in seven Swiss physicians has left patient care - results from a national cohort study from 1980–2009. Swiss Med Wkly. 2019;149:w20116. https://doi.org/10.4414/smw.2019.20116.
Peter K, Hahn S, Schols J, Halfens RJ. Work-related stress among health professionals in Swiss acute and rehabilitation hospitals – results of a cross-sectional study. In: 18th European Doctoral Conference in Nursing Science; Graz; 2019.
Vogel B, de Geest S, Fierz K, Beckmann S, Zuniga F. Dementia care worker stress associations with unit type, resident, and work environment characteristics: a cross-sectional secondary data analysis of the Swiss nursing Homes Human resources Project (SHURP). Int Psychogeriatr. 2017;29:441–54. https://doi.org/10.1017/S1041610216002027.
Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. J Epidemiol Community Health. 2000;54:502–9. https://doi.org/10.1136/jech.54.7.502.
Kristensen TS, Hannerz H, Høgh A, Borg V. The Copenhagen Psychosocial Questionnaire-a tool for the assessment and improvement ofthe psychosocial work environment. Scand J Work Environ Health. 2005;31:438–49.
Nübling M, Vomstein M, Nolle I, Lindner A, Haug A, Lincke HJ. Deutsche Standard-Version Des COPSOQ 2017. Freiburg: FFAW-Freiburger Forschungsstelle für Arbeitswissenschaften GmbH; 2017.
Hasselhorn HM, Tackenberg P, Müller H. Working conditions and intent to leave the profession among nursing staff in Europe. Sweden: National Institute for Working Life; 2003.
de Jonge J, Mulder MJ, Nijhuis FJ. The incorporation of different demand concepts in the job demand-control model: effects on health care professionals. Soc Sci Med. 1999;48:1149–60. https://doi.org/10.1016/s0277-9536(98)00429-8.
Eurofound. Sixth European Working conditions Survey - Questionnaire. Luxembourg: Publications Office of the European Union; 2015.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual life Research: Int J Qual life Aspects Treat care Rehabilitation. 2011;20:1727–36. https://doi.org/10.1007/s11136-011-9903-x.
Golz C, Peter KA, Hahn S. Cognitive pretesting and pretest of the STRAIN questionnaire to elaborate work-related stress of health care staff in Switzerland. Int J Health Professions. 2018;5:109–20. https://doi.org/10.2478/ijhp-2018-0011.
Peter K, Golz C, Bürgin RA, Nübling M, Voirol C, Zürcher SJ, Hahn S. Assessing the psychosocial work environment in the health care setting: translation and psychometric testing of the French and Italian Copenhagen Psychosocial questionnaires (COPSOQ) in a large sample of health professionals in Switzerland. BMC Health Serv Res. 2022;22.
R Core Team. R: a Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2022.
Venables WN, Ripley BD. Modern Applied statistics with S. 4th ed. New York: Springer; 2002.
Bates D, Mächler M, Bolker B, Walker S. Fitting Linear mixed-effects models using lme4. J Stat Soft. 2015;67:1–48. https://doi.org/10.18637/jss.v067.i01.
Nakagawa S, Johnson PCD, Schielzeth H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J Royal Soc Interface. 2017;14:20170213. https://doi.org/10.1098/rsif.2017.0213.
Gilles I, Burnand B, Peytremann-Bridevaux I. Factors associated with healthcare professionals’ intent to stay in hospital: a comparison across five occupational categories. Int J Qual Health care: J Int Soc Qual Health Care. 2014;26:158–66. https://doi.org/10.1093/intqhc/mzu006.
de Vries N, Boone A, Godderis L, Bouman J, Szemik S, Matranga D, de Winter P. The race to Retain Healthcare Workers: a systematic review on factors that Impact Retention of Nurses and Physicians in hospitals. Inquiry. 2023;60:469580231159318. https://doi.org/10.1177/00469580231159318.
Donaldson-Feilder E, Yarker J, Lewis R. Line management competence: the key to preventing and reducing stress at work. Strategic HR Rev. 2008;7:11–6. https://doi.org/10.1108/14754390810853110.
Specchia ML, Cozzolino MR, Carini E, Di Pilla A, Galletti C, Ricciardi W, Damiani G. Leadership styles and nurses’ job satisfaction. Results of a systematic review. Int J Environ Res Public Health. 2021;18:1552.
Lobsiger M, Liechti D. Berufsaustritte Und Bestand Von Gesundheitspersonal in Der Schweiz - Eine Analyse auf basis Der Strukturerhebungen 2016–2018. Neuchatel: Swiss Health Observatory (OBSAN); 2021.
Çamveren H, Arslan Yürümezoğlu H, Kocaman G. Why do young nurses leave their organization? A qualitative descriptive study. Int Nurs Rev. 2020;67:519–28. https://doi.org/10.1111/inr.12633.
Flinkman M, Laine M, Leino-Kilpi H, Hasselhorn HM, Salanterä S. Explaining young registered Finnish nurses’ intention to leave the profession: a questionnaire survey. Int J Nurs Stud. 2008;45:727–39. https://doi.org/10.1016/j.ijnurstu.2006.12.006.
Labrague LJ, de los Santos JAA. Transition shock and newly graduated nurses’ job outcomes and select patient outcomes: a cross-sectional study. J Nurs Adm Manag. 2020;28:1070–9. https://doi.org/10.1111/jonm.13033.
Rudman A, Gustavsson P, Hultell D. A prospective study of nurses’ intentions to leave the profession during their first five years of practice in Sweden. Int J Nurs Stud. 2014;51:612–24.
Zhang Y, Wu J, Fang Z, Zhang Y, Wong FKY. Newly graduated nurses’ intention to leave in their first year of practice in Shanghai: a longitudinal study. Nurs Outlook. 2017;65:202–11. https://doi.org/10.1016/j.outlook.2016.10.007.
Dwyer PA, Hunter Revell SM. Multilevel influences on New Graduate Nurse Transition: A literature review. J Nurses Prof Dev. 2016;32:112–21. https://doi.org/10.1097/NND.0000000000000265.
Çamveren H, Kocaman G, Vatan F. The effects of a preceptorship program on newcomer nurses’ turnover intention, commitment and job satisfaction: quasi-experimental study. Nurse Educ Pract. 2022;63:103358. https://doi.org/10.1016/j.nepr.2022.103358.
Lin Y-E, Tseng C-N, Wang M-F, Wu S-FV, Jane S-W, Chien L-Y. Anxiety and work stress among newly employed nurses during the first year of a residency programme: a longitudinal study. J Nurs Adm Manag. 2020;28:1598–606. https://doi.org/10.1111/jonm.13114.
Acknowledgements
We are very grateful to all the organizations and health professionals who participated in this study, for sharing their experience and their time.
Funding
This study was financially supported by the University of Applied Sciences, Health Division, Bern, Switzerland (50% of the costs, and the State Secretariat for Education and Research (SER) of Switzerland (50% of the costs). The funders had no influence or control on the planning, conduct, or reporting of the study.
Author information
Authors and Affiliations
Contributions
KAP, CV, SK, AG, FR, TJ, and CG designed the questionnaire and recruited the participating health organizations. KAP, CV, SK, FR, TJ, CG collected and analyzed the data. KAP and CG made substantial contributions to the interpretation of data and in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The responsible Swiss ethical board in Bern (Kantonale Ethikkommission Bern) confirmed that the ‘strain’ study is deemed unnecessary according national legislation and does not fall under the Swiss Federal Act on Research Involving Human Beings (reference number: Req-2016-00616). The study was conducted in accordance with the Declaration of Helsinki. All health employees of the participating organizations were informed about the aim, procedures, risks, benefits, anonymity of data, and alternatives for participating in the study via online announcement / paper flyer and a short explanatory video so that they could make an informed decision about participation. Informed consent was obtained and participants were again informed on the first page of the questionnaire about the aim, procedure, and possible risks and had to actively give their consent (written, using a checkbox) to continue the questionnaire. The study was carried out on a voluntary basis for all organisations and health professionals participating; all participants were free to stop filling out the questionnaire at any time. The study was carried out on a voluntary basis for all participating organizations and health professionals; all participants were free to stop filling out the questionnaire at any time and had the opportunity to contact the research team via hotline if they had any questions. Data were anonymized and analysed only in units of analysis of at least 6 participants (e.g. per occupational group or ward).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peter, K.A., Voirol, C., Kunz, S. et al. Factors associated with health professionals’ stress reactions, job satisfaction, intention to leave and health-related outcomes in acute care, rehabilitation and psychiatric hospitals, nursing homes and home care organisations. BMC Health Serv Res 24, 269 (2024). https://doi.org/10.1186/s12913-024-10718-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10718-5