Abstract
Background
Patients with heart failure (HF) and colorectal cancer (CRC) are prone to comorbidity, a high rate of readmission, and complex healthcare needs. Self-care for people with HF and CRC after hospitalisation can be challenging, and patients may leave the hospital unprepared to self-manage their disease at home. eHealth solutions may be a beneficial tool to engage patients in self-care.
Methods
A randomised controlled trial with an embedded evaluation of intervention engagement and cost-effectiveness will be conducted to investigate the effect of eHealth intervention after hospital discharge on the self-efficacy of self-care. Eligible patients with HF or CRC will be recruited before discharge from two Norwegian university hospitals. The intervention group will use a nurse-assisted intervention—eHealth@Hospital-2-Home—for six weeks. The intervention includes remote monitoring of vital signs; patients’ self-reports of symptoms, health and well-being; secure messaging between patients and hospital-based nurse navigators; and access to specific HF and CRC health-related information. The control group will receive routine care. Data collection will take place before the intervention (baseline), at the end of the intervention (Post-1), and at six months (Post-2). The primary outcome will be self-efficacy in self-care. The secondary outcomes will include measures of burden of treatment, health-related quality of life and 30- and 90-day readmissions. Sub-study analyses are planned in the HF patient population with primary outcomes of self-care behaviour and secondary outcomes of medication adherence, and readmission at 30 days, 90 days and 6 months. Patients’ and nurse navigators’ engagement and experiences with the eHealth intervention and cost-effectiveness will be investigated. Data will be analysed according to intention-to-treat principles. Qualitative data will be analysed using thematic analysis.
Discussion
This protocol will examine the effects of the eHealth@ Hospital-2-Home intervention on self-care in two prevalent patient groups, HF and CRC. It will allow the exploration of a generic framework for an eHealth intervention after hospital discharge, which could be adapted to other patient groups, upscaled, and implemented into clinical practice.
Trial registration
Clinical trials.gov (ID 301472).
Similar content being viewed by others
Background
Worldwide healthcare systems are increasingly relying on patients to manage their treatment and illness through self-care due to the rising rates and pressures created by chronic illness [1, 2]. In Norway and globally, cancer and cardiovascular conditions are illnesses with considerable burdens for patients and healthcare costs [3]. In 2020, approximately 15,000 Norwegians were diagnosed with heart failure (HF) [4] with the prevalence of known HF being 1–2% of the global population [5]. In 2020, nearly 4,500 Norwegians were diagnosed with colorectal cancer (CRC) with the prevalence increasing by 1.8% per year in Norway between 2012 and 2016 [6]. Both conditions are prone to comorbidity and complex healthcare needs, including high readmission rates [5, 7,8,9].
While the two illnesses are different in terms of diagnosis, treatment, prognosis and trajectory [10, 11], HF and CRC have similar needs for follow-up care and the development of patients’ self-care skills [12, 13]. Individuals with either HF or CRC have challenges with unmet health needs and limited access to healthcare professionals, particularly after hospitalisation [14,15,16]. Between hospital admissions and specialist appointments, patients must self-care at home [17]. Patients also often receive limited support with the transition from hospital to home [18]. Inadequate follow-up of HF and CRC patients after hospitalisation can potentially result in unsafe and anxious patients [16, 19], which may lead to poor adherence to medical treatment and self-care tasks [20], resulting in readmission [21] and low quality of life [22]. Unsupportive healthcare service pathways lead to a higher burden of treatment [23].
The burden of treatment is the delicate balance between a patient’s capacity (capability and resources) and the workload (tasks required by illness management and treatments) [24]. If that balance tips so the workload exceeds the patient’s capacity, patients experience poorer outcomes, health-related quality of life (HRQoL) [25] and self-care [24]. Self-care refers to ‘the ability of the patient to deal with a chronic illness including symptoms, treatment, physical and social consequences, and lifestyle changes’ [26]. It is a complex construct with multiple processes and influencing factors [27]. Self-efficacy is key to influencing patient decisions around self-care behaviours [27]. It refers to an individual’s confidence in their capacity to act in the ways necessary to reach specific goals [28] and is linked to self-management [1].
eHealth solutions may provide a way to support self-care in illnesses such as HF and CRC. eHealth is both the delivery of health services and information [29] as well as the conceptualisation of user interactions with the technology (e.g., monitoring of vital signs, communication with healthcare providers and utilisation of data to restore health) [30]. Patients who use eHealth may be more motivated to engage in self-care behaviours [31, 32]. eHealth-based self-care interventions have been found to improve confidence in self-care of cancer patients and coronary heart disease patients [33, 34]. Within HF, a review of eHealth follow-up programmes has reported significantly increased HRQoL, but the impact on readmissions and self-care is less clear [35]. In cancer survivors, Chan et al. [36] reported that telemedicine significantly improved HRQoL and symptom burden. A cost-effectiveness review suggested that nurse-assisted follow-up is a promising method for reducing costs (compared with rehospitalisation) without endangering patient outcomes, following cancer treatment [37].
Research on how eHealth can best support patients with HF and CRC during the period after hospital discharge is sparse [36, 38]. Therefore, a nurse-assisted eHealth intervention eHealth@Hospital-2-Home was developed and tested based on a body of research in HF and CRC patients [15, 35, 39, 40]. Existing software and application technology—the Dignio Connected Care [41]—was selected as the platform for the intervention. The eHealth intervention includes:
-
monitoring of vital signs using connected technology (heart rate, blood pressure, pulse oximetry, temperature, weight)
-
patient self-reporting of symptoms, health and well-being
-
secure messaging between patients and hospital-based nurse navigators when patients’ vital signs exceed the acceptable range
-
access to HF and CRC health-related educational information.
This paper presents the protocol for a randomised controlled trial (RCT) evaluating a complex intervention [42] to study the effects of the eHealth@Hospital-2-Home intervention on the primary outcome of self-efficacy in self-care in HF and CRC patients. The protocol was informed by the preliminary results from a feasibility study with the two patient groups [43] and follows the recommendations for protocol items for a clinical trial (SPIRIT) checklist [44] and the CONSORT checklist for reporting items of a randomised trial [45].
The aims of the RCT are as follows.
Primary aims:
-
1) To evaluate the immediate (Post-1: 6 weeks) and extended effects (Post-2: 6 months) of an eHealth intervention after hospital discharge to improve patients’ self-efficacy to self-manage chronic illness. We hypothesise that participants in the intervention group will report higher levels of self-efficacy at six weeks after hospital discharge and at six months after baseline compared with the control group.
Secondary aims:
-
2) To investigate the effects of the intervention on the secondary outcomes of the burden of treatment, HRQoL, perceived collaboration and social support from healthcare personnel, healthcare utilisation and 30- and 90-day readmission rates in the two patient groups.
-
3) HF sub-study: To investigate the effects of the intervention on self-care behaviour, medication compliance and 6- and 12-month readmissions in participants with HF only. We hypothesise that the HF intervention group will report higher levels of self-care behaviours, better medication compliance and reduced 6- and 12-month hospital readmissions compared with the HF control group.
Explorative aim:
-
4) To evaluate patients’ and nurse navigators’ engagement and experiences with the eHealth intervention and estimate cost-effectiveness. Evaluation will use mixed methods [42].
The logic model for the intervention [46] and RCT (see Fig. 1) illustrates the resources needed (i.e., intervention) to implement change (i.e., mechanisms of change) that may lead to the result we intend to achieve (i.e., outcomes).
Methods
Study design and setting
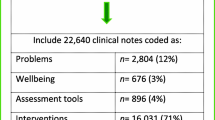
This study is an RCT with an embedded evaluation of intervention engagement and cost-effectiveness. The RCT is part of a larger study ‘Nurse-assisted eHealth service from the hospital to home: Ameliorating the burden of treatment among patients with noncommunicable diseases’ funded by the Norwegian Research Council (Funding No. 301472). An overview of the trial design is shown in Fig. 2.
The trial will include study participants with HF and CRC from two similar-sized university hospitals in Norway (Study Sites A and B). Study Site A is a university hospital in the western part of Norway that provides specialist health care for approximately 370,000 inhabitants. Study Site B is a university hospital in the middle of Norway, providing specialist health care for approximately 300,000 inhabitants (as of September 2023).
Eligibility of study participants
Eligible patients will be adults aged ≥ 18 years with either HF or CRC chronic illness admitted to the hospital, and able to speak and write in Norwegian. See Table 1 for detailed illness-specific eligibility criteria.
Sample size calculations
The sample size goal is 240 patients (HF = 180, CRC = 60) equally divided between the intervention and control group. Assuming a 20% dropout, a sample size of 240 will provide a power of 80% to detect, at an α error probability of < 0.05, a medium-sized standardised difference in the primary outcome (self-efficacy for managing chronic disease) of 0.4 in the disease groups combined at the first time point (Post-1). For the HF sub-study, assuming the same dropout rate of 20%, there will be 80% power to detect a standardised effect of size 0.5 for the outcome of self-reported self-care.
Patient screening and recruitment
All patients will be screened and recruited during their hospital admission. Patients with HF will be recruited from both sites, whereas those with CRC will be recruited from a surgical ward at Study Site A. Hospital ward patient lists will be screened by the nurse navigators daily for eligible patients using the eligibility criteria (see Table 1). Nurse navigators will approach those who are eligible, providing written and oral study information. A short, animated video about the research project and the nurse-assisted eHealth intervention will be provided for viewing [49]. The patient will be included if informed written consent has been provided.
Randomisation
Patients who agree to participate will be randomised. Randomisation occurs after the patients have completed the baseline assessment. Participants will be allocated by stratified block randomisation (1:1) to either the intervention or control group using sequentially numbered, opaque, sealed envelopes. Stratification will occur by diagnostic groups (HF and CRC) and study sites. Separate randomisation lists will be produced for all three strata by a statistician (ID) and concealed from researchers. Randomisation allocation will be blinded for statisticians and researchers performing the data analyses.
Intervention group: eHealth@Hospital-2-Home intervention
The eHealth intervention is a non-acute, alert- and communication-based service operated by nurse navigators. The intervention duration is six weeks following hospital discharge and aims to monitor and support participants.
Participants
Participants in this group will be issued an iPad with only the eHealth application MyDignio. MyDignio uses a cloud-based secure database that can be accessed without an IP address, allowing information exchange using an encrypted message exchange system. Communication via chat and video links between the patients and the nurse navigators in the hospital is supported in the application. MyDignio app is linked to monitoring devices by Bluetooth for each participant to record clinical measures (i.e., blood pressure, pulse, temperature and weight).
Participants will be asked to register clinical measurements HF and CRC daily, register symptoms daily and weekly, and register well-being daily (see Table 2 for overview) into MyDignio app, which will be monitored by nurse navigators employed at the two hospitals [41]. Participants are asked to perform the clinical measurements at approximately the same time to minimise daily variance caused by meals, fluid intake and bowel movements. They will receive a reminder in the system if they have not reported the data. Additionally, participants can communicate with the nurse navigator at any time via chat and video links through the application. Before discharge from the hospital, participants will receive training from the nurse navigators on the use of MyDignio app and the monitoring devices. Instructions and contact details for accessing technical support will be provided.
Nurse navigators
Eight registered nurses will be recruited as nurse navigators to work either with HF (nurse navigators = 4) or CRC (nurse navigators = 4). The nurse navigators are experienced hospital nurses with the clinical skills required to identify and monitor high-needs patients. Digital and in-person training (13 h) is provided in the study procedures and using DignioPrevent.
DignioPrevent is the clinical interface to the eHealth intervention application. Nurse navigators use DignioPrevent to monitor and respond to participant data. They will contact participants 24 to 48 h after their hospital discharge to offer further support in using the MyDignio app. Nurse navigators also monitor participants using DignioPrevent to respond to messages daily and schedule calls. The private messaging system in DignioPrevent allows nurse navigators to answer questions about the patient’s health and provide feedback and advice to the participants about medications, nutrition, fluid intake and activity based on the participant-reported data, facilitating informed and supportive self-care. Nurse navigators can also provide information about available websites with information about HF and CRC, resources and peer support services relevant to the patient’s situation.
Each participant profile will have personalised predefined thresholds that trigger green, yellow or red flags. Yellow and red flags require the nurse navigator to respond to those patients within 48 h. Red flags require the nurse navigator to advise the patient to first conduct extra clinical measures to ensure that they are correct; and second, advise the patient to contact their general practitioner or the municipal emergency department to ensure proper treatment, as the intervention is not an emergency service. Nurse navigators can consult with the medical doctor or surgeon collaborating with the research project to provide medical oversight for the trial about possible medical interventions. The intervention group is considered low risk to participants and provides more support than routine care. Actions to mitigate participant risk include setting specific clinical thresholds on all patient-inputted data, providing research-specific training and provisioning technical support.
Control group: routine care
The control group will only receive routine care. Routine care refers to the standard care offered after hospital discharge. For all participants in this group, this includes written discharge information, information on how to schedule a follow-up appointment at the hospital outpatient clinic or with their general practitioner if needed, and information to contact their general practitioner or municipal emergency department if worrying symptoms occur after hospital discharge. The participants will receive pertinent disease-specific information as part of routine care for both patient groups. To support participants in this group, they will be contacted by telephone between Post-1 and Post-2 to confirm their continuous participation in the trial and to offer any additional support as required.
Patient and public involvement
The eHealth intervention was developed in collaboration with representatives from both patient groups and nurses. The representatives aided in tailoring the content and follow-up plan for both HF and CRC patients’ specific health needs post-hospital discharge. Patient representatives and nurses have participated in workshops with the research team to review and assess all information provided to participants as well as the content in the eHealth application MyDignio.
Outcome measures
An overview of all outcome measures is presented in Table 3.
Primary outcome measures
The primary outcome measure for this study will be patients’ self-reports of self-efficacy to manage their HF or CRC disease as measured by the six-item questionnaire Self-Efficacy for Managing Chronic Disease developed by Lorig et al. [50]. The items ask participants to rate their confidence in doing activities across several domains common for many chronic diseases (i.e., symptom control, role function, emotional functioning and communicating with physicians). All items are scored on a 10-point scale (1 = not at all confident to 10 = confident). The total score is the mean score of the six items.
Secondary outcome measures
Multiple measures will be used to examine secondary outcomes. These are outlined in Table 3 and briefly described below:
-
Treatment burden will be measured with the Norwegian Patient Experiences with Treatment and Self-Management [51, 52]. The four dimensions—medical information (seven items), monitoring health (four items), medications (seven items) and medical appointments (six items)—will be used to focus on treatment burden related to areas of non-adherence in chronic illness.
-
HRQoL will be measured using the validated and reliable EuroQoL 5-Dimension 5-Level (EQ-5D-5L) questionnaire [25]. It includes five health dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Patients are asked to rate their current health status with responses that range from no problem to an extreme problem. It includes the EuroQoL visual analogue scale, which is a one-item visual analogue scale where patients report on ‘your health today’ using a scale between 0 and 100.
-
Perceived support from healthcare personnel will be measured using 12 items on constructive support [55, 56]. All items are measured on a five-point Likert scale, ranging from ‘agree strongly’ to ‘disagree strongly’.
-
Collaboration with healthcare personnel will be measured using the validated three-item questionnaire CollaboRATE [53, 54]. The three items represent three core shared decision-making activities: explanation of the health issue, preference elicitation and preference integration [60]. Each item is scored on a 10-point anchor scale from 0 (‘No effort was made’) to 9 (‘Every effort was made’).
-
Healthcare utilisation will be captured using patients’ self-reporting of the number of visits to the primary healthcare service (i.e., general practitioner, municipal emergency department) and/or the specialist healthcare service (i.e., outpatient clinic).
-
Days alive and out of hospital [57] will be measured by comparing a patient’s self-report data with hospital records and subtracting the number of days spent away from home due to HF- or CRC-related hospitalisation from the first reporting in MyDignio up to six months (Post-2) [61].
-
Numbers of readmissions within 30 and 90 days will be collected from the electronic healthcare record system in the hospital.
HF sub-study outcome measures
Participants with HF will participate in a sub-study that aims to explore the effects of the digital eHealth intervention on HF self-care behaviours, readmissions and medication adherence. The primary outcome of this study uses the revised European Heart Failure Self-Care Behaviour Scale, a validated questionnaire comprising nine items [58], to evaluate any changes in self-care behaviours within and between the groups. Secondary outcomes will examine the number of readmissions at 30 days, 90 days and 6 months from the electronic healthcare record system in the hospital. The validated Medication Adherence Reasons Scale-5, which consists of five items [59], will be used to measure medication adherence and non-adherence behaviours for between-group comparisons.
Patients’ and nurse navigators’ engagement with the intervention
Engagement [62] with the eHealth intervention will be assessed and explored against self-efficacy for any observable relationship. According to the World Health Organization [63], intervention adherence is the extent to which the patient’s behaviour corresponds to the intervention assigned to them. In this RCT, adherence will refer to the dose received by the participants or the extent to which participants actively engage with, are receptive to, and/or use the materials (i.e., symptom checklists) or recommended resources (i.e., monitoring equipment) [64]. Adherence will refer to engagement, for which adherence is set at 80–100% of the dose delivered (i.e., completing both daily measurements and symptom checklists). Similarly, nurse navigators’ engagement with the digital application will also be explored and evaluated. Finally, engagement data will be used to estimate cost-effectiveness.
Data collection
Demographic variables collected will include sex, age, education, work, living situation, other health conditions, frequency of contact with the hospital and use of digital tools. Questionnaires will be administered electronically or postally (by participant choice) at three different times: baseline, the end of the intervention (Post-1), and 6 months after baseline (Post-2). The baseline measurements will be collected in the hospital, where Post-1 and Post-2 questionnaires will be completed by the patients at home (electronically or paper, by patient choice).
Interviews will be conducted with participants in the intervention group (n = 30, HF n = 20, CRC n = 10) to explore the experience with the intervention around the themes of usability and acceptability and to inform the results of the intervention effects and future implementation [42]. Participants in the intervention group will also complete the Post Study System Usability Questionnaire [65] to assess satisfaction with the usability of the MyDignio app. Additionally, participants in the HF sub-study (n = 12) will be invited to interview twice (Post-1 and Post-2) about their experiences on HF self-care. Interviews with the nurse navigators (n = 8) will be conducted in one focus group. Questions will focus on their experiences of delivering the intervention and factors influencing the implementation of the intervention in the hospital. All interview guides will be co-created with patient representatives and the project group. The interviews will be conducted at the location chosen by the patients and nurse navigators. Interviews will be audio recorded, transcribed verbatim and translated into English.
Data management
Collection of personalised data is limited and only includes personal data necessary for the trial. The Services for Sensitive Data (TSD) administered by the University of Oslo [66] will be used to retrieve, store and process data from the questionnaires and interviews. Electronic questionnaire data will be retrieved using an application that includes an integrated solution for collecting sensitive data (Nettskjema), which is linked to the TSD [66]. All data containing personal identifying information and clinical variables obtained from patient’s medical records will be stored separately on research servers at Sites A and B. Only the project manager and nurse navigators will be able to access the code list connecting personal identifying data to the individual participant.
Statistical methods
The primary assessment of the intervention effect will be performed using a mixed-model approach to the analysis of covariance (ANCOVA) with the two post-intervention scores of self-efficacy to self-care (at Post-1 and Post-2) as the dependent variable and pre-intervention self-efficacy to self-management, measurement occasion and intervention group as independent variables. The difference in treatment effects between the time points will be determined with an interaction term between the measurement occasion and intervention group. Important predictors of self-efficacy to self-managing HF or CRC or dropout will also be included in the model, as well as the stratifying variables used in the randomisation. Random effects will be included to address dependencies between repeated measures and with dropouts. The sub-study analyses of HF self-care behaviour and medication adherence comprise the primary assessment of intervention effect using the same approach. All analyses will be conducted according to intention-to-treat principles (i.e., including all participants as randomised, disregarding adherence to the assigned treatment). The main comparison will be at the six weeks (Post-1) timepoint. The analysis of secondary continuous outcomes will be performed similarly, whereas readmissions will be analysed using Cox regression. The computer software SPSS [67] and R [68] will be used for analysis and statistical calculations.
Qualitative data analysis
The text transcripts from the interviews with patients and the focus group interview with nurse navigators will be analysed using thematic analysis [69]. The analysis process will be iterative, in which members of the research team independently read and code the text transcripts. The codes will be sorted into preliminary themes, which will be discussed by the research team before concluding on the final themes to be reported. The software tool NVivo will be used [70].
Cost-effectiveness
Cost-effectiveness analyses will be performed at both time points, informed by the EQ-5D-5L. Data on resource use in the hospital (inpatient stay, outpatient visits) will be collected from the hospital’s electronic medical records, while use of health- and care services in the municipality (visits to the general practitioner, emergency room and home health care) will be collected from standardised questionnaires in the patient’s home. We will estimate a standard cost for the intervention per patient. The intervention cost includes the digital equipment (e.g., tablet, scale), costs of the nurse navigators’ working hours connected to the patient that receives MyDignio and costs connected to nurse navigators’ weekly work hours spent following up with patients through DignioPrevent.
Data monitoring and auditing
Data monitoring will be continuously performed by the research team. Nurse navigators will attend regular meetings with the research team to report on their activities and challenges. The researchers have access to the Dignio Prevent system and can remotely monitor nurse navigators’ actions. Twice a year, we will conduct project meetings with a scientific advisory committee (SAC). The SAC members are internationally recognised leading experts in the fields of HF, cancer care, self-care interventions, complex intervention studies, eHealth innovation and health services research. The SAC will provide advice and monitor trial progress.
Research ethics
The protocol received ethical approval from the Western Regional Committee for Medical and Health Research Ethics (REC west) (REC ID 556114) on 2 February, 2023. Local approvals for each recruiting site were obtained. The research will be conducted according to the Helsinki Declaration [71]. The patients will be included in the study when informed written consent has been provided. The RCT began recruiting in May 2023. Participants will have the right to access the registered information and to correct any errors found in the information. Participants have the right to withdraw from the study at any time. All information will be processed without directly recognisable information. A code will link the participant to the registered information through a list of names that only the project manager can access. The data collected from patients will be stored in a secure research data server (i.e., TSD) until 2028.
De-identified clinical (i.e., hospitalisations) and self-report (self-care behaviour) data on HF patients will be shared with collaborators at Vestre Viken Trust, Drammen Hospital, who are conducting a similar clinical trial (registered in ClinicalTrial.gov #NCT05447598). The purpose of this data sharing is to increase the participants’ contributions to generalisable knowledge, by potentially facilitating additional findings beyond the original, prespecified clinical trial outcomes. The HF participants will be informed about data sharing during the consent process.
Ancillary and post-trial care
All participants who were surgically treated for CRC will, as part of standard care, attend a post-surgical follow-up appointment at the gastrosurgical outpatient clinic and systematic follow-up according to national guidelines. Patients with HF will be followed up by their general practitioner or at an HF outpatient clinic. All participants will receive a follow-up call when the study is complete with information that the study has ended, how they can access information about trial results and to ask if they have feedback to provide to the research team.
Dissemination
Trial results will be published as scientific articles in peer-reviewed academic journals. We will also share the results with stakeholders of the project through patient organisation channels, at seminars for relevant healthcare personnel and regularly as popular science contributions in local and social media.
Discussion
HF and CRC are two major illnesses representing challenges to healthcare systems and self-care for patients. The two illnesses are different in terms of treatment and course of illness [10, 11], but the patients share a similar need for follow-up care to support their self-management after hospital discharge. eHealth interventions and remote follow-up of patients may be a possible solution to patients’ need for support after hospitalisation but will require the development and testing of robust interventions with the two patient groups to ensure that their shared needs are addressed. The intervention presented in this protocol was developed using the Medical Research Council Complex Interventions Framework [42]. It is built on a solid foundation of literature reviews [35, 39] and feasibility research [15, 43] and has been informed by HF and CRC patients, representatives from the two patient groups, and clinicians. Currently, the feasibility data are undergoing analysis, but preliminary results indicate that the intervention meets the shared post-hospital needs of the two patient groups and that an RCT is feasible.
This protocol will facilitate the examination and exploration of the effects of the eHealth @ Hospital-2-Home intervention on two prevalent patient groups, HF and CRC. The inclusion of both groups will allow the exploration of a generic framework for an eHealth intervention after hospital discharge, which if effective, could be adapted to other patient groups, upscaled, and implemented into clinical practice. The use of mixed methods will facilitate the exploration of the effects and experiences of patients and nurse navigators, enabling a more in-depth description of the intervention and its effects. It will also enable the refinement of the intervention for future research.
Availability of data and materials
Not applicable. No data are available.
Abbreviations
- RCT:
-
Randomised Controlled Trial
- CRC:
-
Colorectal Cancer
- HF:
-
Heart Failure
- HRQoL:
-
Health-Related Quality of Life
- EQ-5D-5L:
-
EuroQoL 5-Dimension 5-Level
- TSD:
-
The Services for Sensitive Data
- SAC:
-
Scientific Advisory Committee
References
Dineen-Griffin S, Garcia-Cardenas V, Williams K, Benrimoj SI. Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. Leroyer C, editor. PLOS One. 2019;14(8):e0220116.
Narasimhan M, Kapila M. Implications of self-care for health service provision. Bull World Health Organ. 2019;97(2):76-76A.
Saelendsminde K, Line TM, Olsen CB. Samfunnskostnader ved sykdom og ulykker 2015 Sykdomsbyrde, helsetjenestekostnader og produksjonstap fordelt på sykdomsgrupper. 2015. Report No.: IS-2839. Available from: https://www.helsedirektoratet.no/rapporter/samfunnskostnader-ved-sykdom-og-ulykker/Samfunnskostnader%20ved%20sykdom%20og%20ulykker%202015.pdf/_/attachment/inline/761dd2be-6458-4baf-99c9-34d58a621aad:e3291994cf460a6d1c5174eab5f27b4165208afe/Samfunnskostnader%20ved%20sykdom%20og%20ulykker%202015.pdf. Accessed 27 Dec 2023.
Kvåle R. Folkehelseinstituttet. 2021 [cited 2023 Oct 16]. Forekomst av hjerte- og karsykdommer i 2020. Available from: https://www.fhi.no/is/hjertekar2/forekomst-av-hjerte--og-karsykdommer-i-2020/.
Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020;22(8):1342–56.
Høydahl Ø, Edna TH, Xanthoulis A, Lydersen S, Endreseth BH. Long-term trends in colorectal cancer: incidence, localization, and presentation. BMC Cancer. 2020;20(1):1077.
Ang CW, Seretis C, Wanigasooriya K, Mahadik Y, Singh J, Chapman MAS. The most frequent cause of 90-day unplanned hospital readmission following colorectal cancer resection is chemotherapy complications. Colorectal Dis. 2015;17(9):779–86.
Khan MS, Sreenivasan J, Lateef N, Abougergi MS, Greene SJ, Ahmad T, et al. Trends in 30- and 90-Day Readmission Rates for Heart Failure. Circ Heart Fail. 2021;14(4):e008335.
Wideqvist M, Cui X, Magnusson C, Schaufelberger M, Fu M. Hospital readmissions of patients with heart failure from real world: timing and associated risk factors. ESC Heart Fail. 2021;8(2):1388–97.
Ramani GV, Uber PA, Mehra MR. Chronic Heart Failure: Contemporary Diagnosis and Management. Mayo Clin Proc. 2010;85(2):180–95.
Qaderi SM, Swartjes H, Vromen H, Bremers AJA, Custers JAE, De Wilt JHW. Acceptability, quality of life and cost overview of a remote follow-up plan for patients with colorectal cancer. Eur J Surg Oncol. 2021;47(7):1637–44.
Zaharova S, Litwack K, Gopalakrishnan S, Ellis J, Saltzberg MT. Self-management in Heart Failure: The Importance of Self-regulation but not Complexity of Condition. West J Nurs Res. 2022;44(4):375–82.
Lo PS, Lin YP, Hsu HH, Chang SC, Yang SP, Huang WC, et al. Health self-management experiences of colorectal cancer patients in postoperative recovery: A qualitative study. Eur J Oncol Nurs. 2021;51:101906.
Nordfonn OK, Morken IM, Lunde Husebø AM. A qualitative study of living with the burden from heart failure treatment: Exploring the patient capacity for self-care. Nurs Open. 2020;7(3):804–13.
Wathne H, Morken IM, Storm M, Husebø AML. Designing a Future eHealth Service for Posthospitalization Self-management Support in Long-term Illness: Qualitative Interview Study. JMIR Hum Factors. 2023;10:e39391.
Husebø AML. Stakeholders’ Perspectives on eHealth Support in Colorectal Cancer Survivorship: Qualitative Interview Study. JMIR Cancer. 2021;7(3):e28279.
Xiao Y. The ‘expert patient’ approach for non-communicable disease management in low and middle income settings: When the reality confronts the rhetoric. Chronic Dis Transl Med. 2015;1(3):145–51.
Storm M, Siemsen IMD, Laugaland KA, Dyrstad DN, Aase K. Quality in transitional care of the elderly: Key challenges and relevant improvement measures. Int J Integr Care. 2014;14(2). Available from: http://www.ijic.org/article/10.5334/ijic.1194/. Cited 2023 Sep 20.
Nordfonn OK, Morken IM, Bru LE, Husebø AML. Patients’ experience with heart failure treatment and self-care—A qualitative study exploring the burden of treatment. J Clin Nurs. 2019;28(9–10):1782–93.
Martin LR, Williams SL, Haskard KB, DiMatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1(3):189–99.
Rosen OZ, Fridman R, Rosen BT, Shane R, Pevnick JM. Medication adherence as a predictor of 30-day hospital readmissions. Patient Prefer Adherence. 2017;11:801–10.
Silavanich V, Nathisuwan S, Phrommintikul A, Permsuwan U. Relationship of medication adherence and quality of life among heart failure patients. Heart Lung. 2019;48(2):105–10.
Lippiett KA, Richardson A, Myall M, Cummings A, May CR. Patients and informal caregivers’ experiences of burden of treatment in lung cancer and chronic obstructive pulmonary disease (COPD): a systematic review and synthesis of qualitative research. BMJ Open. 2019;9(2):e020515.
May CR, Eton DT, Boehmer K, Gallacher K, Hunt K, MacDonald S, et al. Rethinking the patient: using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Serv Res. 2014;14(1):281.
Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72.
Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–87.
Riegel B, Dickson VV, Faulkner KM. The Situation-Specific Theory of Heart Failure Self-Care: Revised and Updated. J Cardiovasc Nurs. 2016;31(3):226–35.
Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):e20.
Shaw T, McGregor D, Brunner M, Keep M, Janssen A, Barnet S. What is eHealth (6)? Development of a Conceptual Model for eHealth: Qualitative Study with Key Informants. J Med Internet Res. 2017;19(10):e324.
Radhakrishnan K, Jacelon C. Impact of Telehealth on Patient Self-management of Heart Failure: A Review of Literature. J Cardiovasc Nurs. 2012;27(1):33–43.
Odeh B, Kayyali R, Nabhani-Gebara S, Philip N. Optimizing cancer care through mobile health. Support Care Cancer. 2015;23(7):2183–8.
Xu A, Wang Y, Wu X. Effectiveness of e-health based self-management to improve cancer-related fatigue, self-efficacy and quality of life in cancer patients: Systematic review and meta-analysis. J Adv Nurs. 2019;75(12):3434–47.
Su JJ, Yu DS. Effects of a nurse-led eHealth cardiac rehabilitation programme on health outcomes of patients with coronary heart disease: A randomised controlled trial. Int J Nurs Stud. 2021;122:104040.
Morken IM, Storm M, Søreide JA, Urstad KH, Karlsen B, Husebø AML. Posthospitalization Follow-Up of Patients With Heart Failure Using eHealth Solutions: Restricted Systematic Review. J Med Internet Res. 2022;24(2):e32946.
Chan RJ, Crichton M, Crawford-Williams F, Agbejule OA, Yu K, Hart NH, et al. The efficacy, challenges, and facilitators of telemedicine in post-treatment cancer survivorship care: an overview of systematic reviews. Ann Oncol. 2021;32(12):1552–70.
Barbieri M, Richardson G, Paisley S. The cost-effectiveness of follow-up strategies after cancer treatment: a systematic literature review. Br Med Bull. 2018;126(1):85–100.
Albert NM, Barnason S, Deswal A, Hernandez A, Kociol R, Lee E, et al. Transitions of Care in Heart Failure: A Scientific Statement From the American Heart Association. Circ Heart Fail. 2015;8(2):384–409.
Husebø AML, Søreide JA, Kørner H, Storm M, Wathne H, Richardson A, et al. eHealth interventions to support colorectal cancer patients’ self-management after discharge from surgery – an integrative literature review. Support Care Cancer. 2023;32(1):11. https://doi.org/10.1007/s00520-023-08191-7.
Husebø AML, Storm M, Morken IM, Espeland J, Hagen LG, Karlsen B. Discussing a Nurse Assisted eHealth Service From Hospital to Home. In: 2019 International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob). 2019. p. 1–6. Available from: https://ieeexplore.ieee.org/document/8923545. Cited 2023 Oct 18.
AS. Dignio Connected Care. 2022. Available from: https://dignio.com/. Cited 2023 Sep 20.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061.
Morken IM, Wathne HB, Karlsen B, Storm M, Nordfonn OK, Gjeilo KH, et al. Assessing a nurse-assisted eHealth intervention posthospital discharge in adult patients with non-communicable diseases: a protocol for a feasibility study. BMJ Open. 2023;13(8):e069599.
Chan A-W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, Hróbjartsson A, Mann H, Dickersin K, Berlin J, Doré C, Parulekar W, Summerskill W, Groves T, Schulz K, Sox H, Rockhold FW, Rennie D, Moher D. SPIRIT 2013 Statement: Defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7.
Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Int Med. 2010;152(11):726–32.
Smith JD, Li DH, Rafferty MR. The Implementation Research Logic Model: a method for planning, executing, reporting, and synthesizing implementation projects. Implement Sci. 2020;15(1):84.
Quirke P, Williams GT, Ectors N, Ensari A, Piard F, Nagtegaal I. The future of the TNM staging system in colorectal cancer: time for a debate? Lancet Oncol. 2007;8(7):651–7.
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo Classification of Surgical Complications: Five-Year Experience. Ann Surg. 2009;250(2):187–96.
University of Stavanger. eHealth @ Hospital-2-Home. Available from: https://www.uis.no/en/research/ehealth-hospital-2-home. Cited 2023 Sep 20.
Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract ECP. 2001;4(6):256–62.
Eton DT, Yost KJ, Lai JS, Ridgeway JL, Egginton JS, Rosedahl JK, et al. Development and validation of the Patient Experience with Treatment and Self-management (PETS): a patient-reported measure of treatment burden. Qual Life Res. 2017;26(2):489–503.
Husebø AML, Morken IM, Eriksen KS, Nordfonn OK. The patient experience with treatment and self-management (PETS) questionnaire: translation and cultural adaption of the Norwegian version. BMC Med Res Methodol. 2018;18(1):147.
Elwyn G, Barr PJ, Grande SW, Thompson R, Walsh T, Ozanne EM. Developing CollaboRATE: A fast and frugal patient-reported measure of shared decision making in clinical encounters. Patient Educ Couns. 2013;93(1):102–7.
Forcino RC, Barr PJ, O’Malley AJ, Arend R, Castaldo MG, Ozanne EM, et al. Using CollaboRATE, a brief patient-reported measure of shared decision making: Results from three clinical settings in the United States. Health Expect. 2018;21(1):82–9.
Karlsen B, Idsoe T, Hanestad B, Murberg T, Bru E. Perceptions of support, diabetes-related coping and psychological well-being in adults with type 1 and type 2 diabetes. Psychol Health Med. 2004;9(1):53–70.
Oftedal B, Bru E, Karlsen B. Social support as a motivator of self-management among adults with type 2 diabetes: Social support and motivation among adults with type 2 diabetes. J Nurs Healthc Chronic Illn. 2011;3(1):12–22.
Cohn J, Cleland JGF, Lubsen J, Borer JS, Steg PG, Perelman M, et al. Unconventional End Points in Cardiovascular Clinical Trials: Should We Be Moving Away From Morbidity and Mortality? J Card Fail. 2009;15(3):199–205.
Jaarsma T, Årestedt KF, Mårtensson J, Dracup K, Strömberg A. The European Heart Failure Self-care Behaviour scale revised into a nine-item scale (EHFScB-9): a reliable and valid international instrument. Eur J Heart Fail. 2009;11(1):99–105.
Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–7.
Drivenes K, Haaland VØ, Mesel T, Tanum L. Practitioners’ positive attitudes promote shared decision-making in mental health care. J Eval Clin Pract. 2019;25(6):1041–9.
Stamford J, Kambhampati C, Pauws S, Clark AL. Patients on Home Telehealth Monitoring have more Days Alive and Out of Hospital. In: 2nd IET International Conference on Technologies for Active and Assisted Living (TechAAL 2016). London, UK: Institution of Engineering and Technology; 2016. p. 7 (7 .)-7 (7 .). Available from: https://digital-library.theiet.org/content/conferences/10.1049/ic.2016.0056. Cited 2023 Sep 20.
Barello S, Triberti S, Graffigna G, Libreri C, Serino S, Hibbard J, et al. eHealth for Patient Engagement: A Systematic Review. Front Psychol. 2016;6. Available from: https://www.frontiersin.org/articles/10.3389/fpsyg.2015.02013. Cited 2023 Sep 20.
World Health Organization. Adherence to long-term therapies : evidence for action [Internet]. World Health Organization; 2003. Available from: https://iris.who.int/handle/10665/42682. Cited 2023 Sep 20.
Lewis EF, Coles TM, Lewis S, Nelson LM, Barrett A, Romano CD, et al. Development, psychometric evaluation, and initial feasibility assessment of a symptom tracker for use by patients with heart failure (HFaST). J Patient-Rep Outcomes. 2019;3(1):26.
Lewis JR. Psychometric Evaluation of the PSSUQ Using Data from Five Years of Usability Studies. Int J Hum-Comput Interact. 2002;14(3–4):463–88.
University of Oslo. Services for sensitive data (TSD). 2022. Available from: https://www.uio.no/english/services/it/research/sensitive-data/index.html. Cited 2023 Sep 20.
IBM Corp. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp; 2021.
RStudio Team. RStudio: Integrated Development for R. Boston: RStudio, PBC; 2020. Available from: http://www.rstudio.com/. Accessed 27 Dec 2023.
Terry G, Hayfield N, Clarke V, Braun V. Thematic Analysis. In: The SAGE Handbook of Qualitative Research in Psychology. SAGE Publications Ltd; 2017. Available from: https://methods.sagepub.com/book/the-sage-handbook-of-qualitative-research-in-psychology-second-edition. Cited 2023 Sep 20.
Lumivero. Lumivero. NVivo. Available from: https://lumivero.com/products/nvivo/. Cited 2023 Sep 20.
Goodyear MDE, Krleza-Jeric K, Lemmens T. The Declaration of Helsinki. BMJ. 2007;335(7621):624–5.
Funding
This work is supported by the Norwegian Research Council (Grant No. 301472) and has undergone independent peer review. The work has also received funding from the Foundation Dam (Grant No. 2023/FO426613) and the University of Stavanger, Norway. Alison Richardson is funded by the National Institute of Health and Care Research (NIHR) ARC Wessex. The views expressed are those of the authors and not necessarily the NHS, NIHR or Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
MS, RA and AMLH drafted the manuscript with extensive contributions from IMM, BK, and KHU, who provided important feedback that improved the manuscript. All authors contributed to the study design, the development and tailoring of the content and functions of the intervention, and the planning of the feasibility study. MS, AMLH, IMM, BK, KHU, HW, EB, AR, GE, and JAS developed the logic model for the study. All authors participated in the review, revision, and approval of the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval obtained from the Western Regional Committee for Medical and Health Research Ethics (REC west) (REC ID 556114). The study will be conducted in accordance with the Helsinki Declaration.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Storm, M., Morken, I.M., Austin, R.C. et al. Evaluation of the nurse-assisted eHealth intervention ‘eHealth@Hospital-2-Home’ on self-care by patients with heart failure and colorectal cancer post-hospital discharge: protocol for a randomised controlled trial. BMC Health Serv Res 24, 18 (2024). https://doi.org/10.1186/s12913-023-10508-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10508-5