Abstract
Background
The studies of hospital resilience have been of increasing importance during the last decade due to disasters and pandemics. However, studies in developing the domain and indicators of hospital resilience were limited mainly on disaster response. A few studies of hospital resilience focused on how to deal with disruptions such as environmental turbulence, rapid technological changes, and changes in patient preferences. This study aims to develop domains and indicators of hospital resilience in facing the disruption era.
Methods
This qualitative study focused on exploring the domains and indicators to face disruptions that have been identified in the first exploratory phase of the studies. Key informants included hospital experts from the government, medical practitioners, and academics. A total of 20 key informants were involved in semi-structured interviews which were conducted face-to-face, via telephone and Zoom. Data was analyzed using a grounded theory approach to discover domains for a resilient hospital.
Results
The study identified a number of domains that are fundamental for a hospital to become a resilient in the face of disruption. These include readiness to face digital transformation, effective leadership, and flexibility in managing resources among others. Situation awareness and resilience ethos, implementation of marketing management, networking, and disaster anticipation are found to be equally important. These domains focused on the hospital’s ability to deal with specific shocks from different perspectives as the result of changes from disruptions which are inevitable within the organizational business environment.
Conclusions
The domains identified in the study are able to respond to the limitations of the concept of hospital resilience, which is currently more focused on hospital disaster resilience. They can be used to measure hospital resilience in the context of the volatility, uncertainty, complexity, and ambiguity (VUCA), which are relevant to the context of the Indonesia hospital industry.
Similar content being viewed by others
Introduction
The concept of hospital resilience has gained popularity due to the high number of health crises caused by natural and non-natural disasters in the past decade [1,2,3,4,5]. Hospital resilience reflects organizational capacity to deal with sudden changes or shocks by absorbing, adapting, or transforming their systems to remain functioning [6]. Conventionally, the hospital resilience concept was developed from traditional safety management concepts and resilience engineering [7]. The idea was discussed in Hyogo, Japan, at the World Conference on Disaster Reduction in 2005. It concerned the role of health services in disaster risk reduction and capacity building in disaster management [8].
During the last decades, resilience concepts in health studies have focused on how to develop domains and indicators [9,10,11,12,13] and how the concept is implemented at the national [5, 7, 13,14,15,16,17,18], organizational [12, 19,20,21,22], and individual levels [23,24,25,26]. Several resilience frameworks that have been developed by the WHO and PAHO, for example, are very specific for certain disasters, such as resilience for earthquakes, floods, climate change, and infectious disease outbreaks [4,5,6]. Barbash and Jeremy (2021) stated that the concept of hospital resilience, which focuses on disaster preparedness, needs to shift to a more comprehensive concept that can accommodate any challenges other than disasters [27]. Hospitals as organizations will continuously face disruptions in their business environment [28]. Brendan and Orin (2020) argue that disruption is a condition that changes the current system so that aspects within the system cannot adapt to that change [28].
Disruption in health care could include technological, economic, and societal changes [28, 29]. Additional disruptions could be policy changes [30,31,32], terrorism [33], and political crises [29]. Consequently, hospitals are required to be able to adapt to all these uncertain, ambiguous, and complex conditions [34]. Hospitals with resilience capabilities face disruption by considering multiple solutions to every problem and quickly maneuvering when previously planned strategies do not work [9, 27]. Resilience is more than just a contingency plan. Resilience is a way of being, a mindset, a set of skills, and a specific process that enables an organization to embrace uncertainty, survive, and recover from setbacks [35].
To date, comprehensive hospital resilience concepts are still being developed. In 2022, the WHO developed a toolkit regarding health system resilience in various contexts, including technical resources of resilience concepts at the operational level [36]. Most of the resilience health care documents identified in the toolkit are guidance that is applied in public health emergencies [37, 38], climate changes [39], the Covid-19 pandemic [40, 41], and zoonotic disease [42]. Those concepts were developed in specific contexts and written in different documents. Few hospital resilience concepts account for shocks or disruptions in highly dynamic environments.
Resilience and the need for comprehensive hospital resilience concept
Resilience concept has been used across a number of disciplinary fields [43,44,45,46] and has been implemented and represented in different ways. Resilience in engineering perspective, primarily adopted in safety studies, focuses on the “bounce back” ability after disruption [46]. From a psychological perspective, resilience is an individual capacity to cope with traumas or challenges [47], and the ecological perspective shows resilience as how the biological system adapts and maintains its system in facing threats [47]. From all disciplinary fields, recent literature highlighted the resilience concept more comprehensively to include the ability of individuals, organizations, communities, or systems to face and cope with pressures, failures, errors, and disruptions by means of flexibility and reorganizing or enhancing their capacities to return to normal function [48].
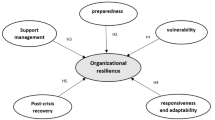
The resilience concept has been implemented at each level of healthcare system in the health sector, particularly in hospitals. Studies of hospital resilience as an organization has developed domains and indicators to measure hospital resilience [20, 49,50,51,52]. However, the domains and indicators developed are mainly about the readiness of the input aspects of the hospital, such as structural, non-structural, and specific disaster organizational functions. In response to the need for the hospital resilience concept in facing any disruption at the organizational level in health care. In this study, we adopted the organizational resilience theory developed in business and management literature, which focuses on a dynamic perspective.
In business and management literature, there are two views of organizational resilience theory, namely static perspective [53,54,55,56] and dynamic perspective [26, 57,58,59,60,61,62,63,64,65,66]. The static perspective views resilience as a function and resilience focusing on the availability of inputs. It compares organization’s conditions before and after a crisis. In contrast, the dynamic perspective views resilience as a capacity and a process where resilience is seen as the spirit of an organization that should always be present in the organization’s daily routines to be ready to face any challenge, whether expected or unexpected [67, 68]. In the Health sector, as the domain of organizational resilience focuses on preparedness that is mostly about the inputs or to prepare the hospital to remain functioning, it can be seen that the organizational resilience view adopted still static perspective. Hospitals, as organizations with complex functions, also will face dynamic situations. There is a need to develop a resilience concept from a dynamic perspective that focuses on capacity and process.
Overview of Hospital Industries in Indonesia
Indonesia has a healthcare system comprising public and private providers. The public system in Indonesia follows the decentralized governance system, where the responsibilities are divided among the central, provincial, and district governments [69]. There are three types of healthcare services in Indonesia, namely primary, secondary, and tertiary. Primary healthcare services provide basic preventive and curatice services through community health centers and clinics. Secondary healthcare services are intended for individuals who require outpatient or inpatient care that are provided by type C hospitals and type D hospitals. Tertiary healthcare services are provided by type A and type B hospitals to include both broad and priority specialist care by specialist doctors [70]. In January 2014, the Government of Indonesia launched a social insurance plan called Jaminan Kesehatan Nasional (JKN), which was implemented by BPJS Kesehatan involving financial contributions from members and the government. Primary care providers receive payments through capitations, while hospitals are reimbursed based on episodes of service payments using INA-CBGs [69].
The development of the hospital industry in Indonesia has accelerated over the past decade. In 2021, the total number of hospitals in Indonesia increased by 169.73% compared to 2011. Based on ownership, private hospitals in Indonesia amounted to 1496 units out of 2522 units in 2021 [71]. This number has increased by 83.55% since 2012, when there were only 815 units [70]. Hospitals in Indonesia are categorized based on ownership and class. Based on the ownership, there are public and private hospital [72]. Public hospitals consist of hospitals owned by the Ministry of Health, provincial governments, district/city governments, the Indonesian National Army, the Indonesian National Police, or other ministries. Private hospitals are owned by foundations, companies, or investors (domestic and foreign). Based on the hospital classification, the hospitals are categorized into hospitals type A (> 250 beds), type B (200- < 250 beds), type C (100- < 200 beds) and type D (50- < 100 beds) [73].
The COVID-19 pandemic has made all stakeholders in the health sector realize that health resilience policies are a priority issue, so the concept of resilience becomes one of the six pillars of the transformation of the health system discussed in the Minister of Health’s Regulation No. 13 of 2022 regarding the Strategic Plan of the Ministry of Health for the year 2020–2024. Unfortunately, the transformation of the health resilience system in this policy only discusses improving the health system’s resilience for the pharmaceutical and medical device sectors. This policy does not address the role of hospitals in the context of disruptions era [74].
Background
In 2020, the COVID-19 pandemic in Indonesia became a turning point in adapting the concept of resilience. Hospital services struggled to keep functioning during the pandemic. At the same time, various policies for organizing hospitals in a new normal way, the growth of online start-up health consulting, digitization in health care, consumer behavior changes, and improvement of hospital quality standards were established. These responses to the pandemic changed the landscape of the healthcare in the country in general and hospital industry in particular.
Before the COVID-19 pandemic, the hospital resilience concept was recognized as an indicator in The National Hospital Accreditation Standard Edition-1 [75]. It was stated in the ‘Facilities and Health Management standard; which discussed how to be a safe hospital by applying the Hospital Safety Index (HSI) measurement once every year [76]. The Hospital Safety Index is a tool for self-assessment to measure a hospital’s readiness and resilience so that a hospital will remain operational in emergencies and disasters [77]. This traditional concept of resilience was adopted from safety management strategies. The domains and indicators of hospital resilience used are similar to the concept in Hospital Disaster Resilience (HDR) studies focusing on disaster preparedness [78,79,80].
Based on national hospital accreditation data in 2022, of the 3072 hospitals in the country, 78% of them received full accreditation, while the remaining 22% are not accredited [81]. This represents the number of hospitals that have not implemented the Hospital Safety Index (HSI) self-assessment possibly due to lack for conducting assessments that can describe a hospital’s readiness to prepare for disasters. A study conducted by Sunindijo et al. (2020) found that the level of HSI achievement in West Java is only 0.553 and in Yogyakarta, it is 0.527 (Level B),. Even In Yogyakarta, the achievement of the disaster and emergency management module is only 0.305 (level C) [82]. These findings indicate the need for intervention measures to address the issue.
It is important to acknowledge the fact that one of the weaknesses of using HSI to measure hospital resilience is that this tool is only used to deal with emergencies and disaster shock conditions [83]. At the time of COVID-19 pandemic, hospitals in Indonesia faced a significant increase in demand for COVID-19 services [84], a decrease in non-Covid-19 service utilities [85], allocation of healthcare spending to mobilize sufficient resources to combat the pandemic [86], and changes in society’s behavior in accessing healthcare services [85, 87, 88].
Experience in the COVID-19 pandemic showed the need for health system transformation even at the hospital service level. The world is rapidly evolving, creating a sense of urgency for organizations to adapt for their sustainability. This change has been labeled as VUCA (Volatility, Uncertainty, Complexity, and Ambiguity), referring to the future world on the brink of transformation [89]. The healthcare industry has experienced the most VUCA times. The COVID-19 pandemic has presented unique challenges to leadership teams, resulting in the need for significant changes to their practices [89].
Due to health system transformation policies that focus on the agenda of strengthening hospital resilience. The substantial changes in the landscape of the hospital industry in Indonesia could not be accommodated by the Hospital Safety Index Concept. There is a need to develop comprehensive hospital resilience that focuses on organizational processes that can face the complexity of disruption in the health care system. This study is a part of the exploratory phase of Hospital Resilience which aims to identify the domains and indicators to tackle the shocks identified in the first phase of the study.
Methods
This current study is the second phase of the Conceptual Model of Hospital Resilience study. Interviews are conducted in two phases. The first phase was to explore the shocks that hospitals face in the disruption era in the context of the Indonesian hospital industry. The results of this phase are presented in a separate manuscript that is submitted for publication. The second phase consists of interviews regarding capacities needed to tackle the shocks that are reported by informants in the first phase, which focused on capacities to be resilient hospitals. The interviews of two phases of studies were conducted using interview questionnaire that is provided as a supplementary file (Supplementary file 1).
This qualitative study was conducted in Makassar, South Sulawesi Province, Indonesia. Key informants were identified from some provinces of Indonesia who attended the National Seminar of Hospital Accreditation held in August 2022 at Claro Hotel Makassar. Informants in this study were experts in hospital industries or resilience sciences and included policymakers from the Ministry of Health, healthcare practitioners, hospital management practitioners, and academics. The inclusion criteria were having experience of more than 5 years in the field and being willing to take part in an interview. We identified 27 potential informants. 20 informants have confirmed to take part in the study. The first author contacted them to confirm their time and method (face-to-face/virtually) as preferred by informants. 15 of the 20 informants were interviewed by face to face. The remaining five informants were interviewed over the phone or via Zoom. Interviews lasted from 45 to 120 minutes.
Interviews were conducted using semi-structured questionnaire guide. All informants received an explanation letter about the study and filled out informed consent before the interview began. All interviews were conducted in Indonesian by the first author from August – November 2022 using audio recorders. This research was carried out in accordance with ethical clearance approved by the Ethics Council under number 9860/UN4.14.1/TP.01.02/2022.
This study used the grounded theory approach to discover resilience domain capacities. The analysis began with data reading and memos writing by forming a coding scheme to explore data, identify links between themes, and develop broader categories of themes. The first author made a transcript of the data soon after the first interview was completed. The transcription process was conducted while data were still being collected. Each transcription was labeled with a unique identifier as interview number (1.1–1.20). After that, we developed initial codes to identify issues raised by interviewers. We coded hospital capacities mentioned by interviewers by identifying verb words and nouns that describe hospital capacities. After completing the initial coding, the first author discussed them in a regular meeting. This was followed by focused coding. The initial codes were summarised in notes to enable the first author to categorize the focused coding. All process during initial codes and focused codes was written in memos. Regular meetings to compare data with codes, codes with codes, codes with categories, and analyzed with relevant theory and previous research were conducted during the analysis. After regular meetings, categories were grouped into domain and subdomain of hospital resilience capacities.
Results
Table 1 shows the characteristics of the 20 informants. Thirteen (65%) of informants were men, 8 (40%) were between 50 and 59 years old, 12 (60%) were hospital practitioners, 11 (55%) had master’s education, and 17 (85%) had experience of more than 10 years in their field.
Based on interviews, seven domains and 33 indicators to measure hospital resilience in facing the era of disruption were identified. Table 2 shows an example of coding that explains each indicator in the domain. The identified domains were:
-
1.
Hospital resources readiness in facing digital transformation
-
2.
Effective leadership
-
3.
Flexibility in managing existing resources
-
4.
Situation awareness and resilience ethos
-
5.
Implementation of marketing management
-
6.
Networking
-
7.
Disaster anticipation
Hospital resources readiness in facing digital transformations
The readiness of resources in facing digital transformation included the readiness of human resources in dealing with technological changes and the readiness of information system infrastructure to facilitate decision-making, be updated, be compatible with current technology, especially digital transformation. From the human resources aspect, capacity building of human resources in hospitals is necessary as the digitization of operational activities will be a mandatory policy in all hospital systems in Indonesia. The management should be aware that the digitization will change the workflow. All health workers will adapt to the new way of working, for instances, the ability to adapt with the Electronic Medical Records (EMR) system. The roles of hospital information systems that can collect and transform data into information from decision-making is also important. Besides that, the capacity to upgrade the digital infrastructure is also vital to facilitate interoperability of the hospital information system with the BPJS system, registration, payment information system, integrated medical records, data collection, and services.
Effective and visionary leadership
Effective leadership includes leaders who are able to read the current situation and see changes as opportunities. This capacity is important to reflect how leaders see the context of every situation and how the organization responds to the changes, whether it is a threat or an opportunity. Besides that, it is necessary to have leaders who have a vision, are able to mobilize members to achieve this vision, and have excellent communication skills. Communication skills would entail building interpersonal relationships with members within and outside the organization, both health and non-health organizations.
Flexibility in managing existing resources
This domain highlights the importance of flexibility in planning, procuring, and organizing resources. In facing disruptions, the hospital must be flexible in managing finances and procuring resources, for instance, procurement of Personal Protective Equipment (PPE) in facing a sudden significant increase in patient demand during the pandemic. This procurement is out of allocation in financial planning but essential to purchase. Under certain conditions, hospitals also need to be able to procure some medical equipment that is urgently available, redesign rooms, and reconfigure their medical devices for different purposes. This domain also focused on a flexible organizational structure that may enable each manager to coordinate not in a bureaucratic way, such as a director being directly able to discuss with the CEO without the need to go through the hospital board.
Situation awareness and resilience ethos
Situation awareness includes the ability to read organizational situations to identify what should be done, be aware of environmental conditions, and be prepared for potential risks. Besides that, hospitals must be able to manage every change and challenge. To address the threats, learning organization capacities that allow continuous learning and open-mindedness are also important. Besides that, the hospital has a resilient ethos. This capacity could be reflected in individual or team capacities, mindset, and organizational culture. For instance, at the individual or group level, the hospital has teamwork that can learn and operationalize government policy changes into a hospital regulation mindset in doing simple research for hospital innovation. At the organizational level, the hospital has tactical funds that can only be used in times of crisis and a habit of conducting regular briefings to identify the current conditions and even contingency plan mechanisms within the organization.
Implementation of marketing management
This domain represents marketing management functioning in hospitals. In Indonesia, marketing management is still shown as a very modern approach in the transition era of hospitals seen as a social organization to industry managed as a business. Some informants highlighted that the function of marketing management is important. This includes the hospital’s ability to conduct simple research based on patient characteristic data, assess market needs and create services according to community needs, diversify products to improve patient experience, rebranding capabilities for focus on centers of excellence, and have a team to apply marketing and branding function. Besides that, implementing marketing management in hospitals could assist hospitals in finding their unique, excellent value and their centers of excellence.
Networking
Networking capabilities include how hospitals have a collaborative network with other hospitals, for example, collaboration in hospital resources procurement, collaboration in the use of medical equipment, discussions in determining centers of excellence in each hospital. Networking with non-health organizations would also be beneficial and could include collaborating with the government, academics, business actors, the community, media, and patient groups.
Disaster anticipation
Indonesia is located in a disaster-prone area. It is crucial to have the ability to understand potential disaster risks in work areas and human resources should be exposed to disaster literacy. Hence, they understand what to do when a disaster occurs, prepare resilient hospital infrastructure that can withstand a disaster, and have disaster-related standard operational procedures.
Discussion
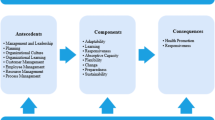
We have presented seven domains for resilient hospitals in facing a disruption era. The domains highlighted the capacities hospitals should have in order to face the disruptions era which is characterized by a rapidly evolving environment that requires capacities to adapt to any changes in all given periods. These domains contrast the past hospital resilience concept, which mainly focused on the hospital’s ability to deal with specific shocks, such as disasters [11, 21, 22, 51, 90]. However, hospital resilience when facing disruptions demonstrates shocks from different perspectives. The changes resulting from disruptions are inevitable within the organizational business environment, which is not categorized in the specific shock and, therefore, not generally discussed in the Hospital Disaster Resilience (HDR) concept [10, 11].
One of the domains that stands out is the readiness to face digital transformation. This domain highlighted specific conditions encountered in the disruption era characterized by digital disruption technology. Several trends in the development of digital transformation that affect health facilities are the use of big data in health services, treatment of patients with Virtual Reality (VR) and Augmented Reality (AR) technology, wearable medical devices, blockchain, and electronic medical records [91]. Digitization makes healthcare less expensive and enables the recreation of healthcare services to become more agile and responsive to technological changes [92]. In Indonesia, the Ministry of Health initiated a digital transformation policy that is made mandatory to all hospitals in 2023. These policies cause shifting in the operational level system as it becomes a mandatory requirement for hospitals to officially join the Social Security Administration Agency (BPJS). Consequently, each hospital must adjust its information system and all resources to prepare the BPJS bridging system.
From the seven domains identified in our study, three domains have been identified in previous health system resilience studies such as leadership [3, 15, 93, 94], flexibility in managing existing resources [95], and networking [3, 15]. Our findings also show that leadership is an essential domain for resilience [67, 96, 97]. The capacities of leaders highlighted in this study focused on envisioning the current situation, empowering others, and having communication skills. Lying et al. (2022) also mentioned these leadership capacities as prioritizing, empowerment, and interaction. Leaders’ ability to read situations will influence the capacity to prioritize strategies based on demands and organizational capacities. This shows the contextual understanding of leaders that affects how leaders adapt and respond in every situation. Empowerment capacity is also shown as encouraging staff to take on responsibilities. The interaction capacities mentioned by Lyeng et al. (2020) focus on the importance of providing support and motivation to staff; good communication skills are necessary to have this capacity.
Another domain identified is situation awareness and resilience ethos. This domain is developed in the organizational resilience concept in management studies [67, 68]. Situation awareness implies the capacity to understand the situation around and be aware of its implication to the current and future position of the organization [54, 67]. Another study revealed this situation awareness capacity as the cognitive resilience of an organization [63]. For example, Lengnick-Hall (2011) describes situation awareness capacities as a genuine orientation that allows the interpretation of unprecedented events and conditions of the organization.
As a result of societal changes, hospitals face changes concerning customer needs and lifestyles that influence patient expectations, hospital revenue, and the hospital market [98]. Therefore, hospitals have to develop new approaches to hospital management, such as marketing management and creating centers of excellence. Marketing management is vital in creating value by understanding consumer needs and expectations, giving the hospital a competitive advantage, and building a strong brand image in the hospital services market [99]. In Indonesia, marketing management is a new function in hospital management. This function seems to be used more in private institutions than in government sectors. The findings of this study highlight the importance of marketing management functions and having centers of excellence in order to enhance hospital capacities to be resilient in Indonesia.
Finally, this study found one domain that focuses on disasters, namely disaster anticipation. This is due to Indonesia’s condition, which is a disaster-prone area for earthquakes, tsunamis, volcanic eruptions, floods, forest fires, droughts, landslides, and flash floods [100, 101]. The concept of disaster in this study focuses on the ability of hospitals to identify disaster risks in their area, establish standard operating procedures in disaster events, and increase disaster literacy in hospital human resources. This disaster concept is aligned with the pillars of disaster resilience developed by the National Planning Development Agency (2015); every institution must understand the concepts of risk identification, risk reduction, preparation, financial protection, and resilient recovery.
However, this study has some limitations. As part of the Conceptual Model of Hospital Resilience Study in Indonesia, informants such as policymakers, hospital practitioners, and academicians involved are only from Indonesia. The capacity of hospital resilience could be specific based on the context of disruption faced by the hospital Industry in Indonesia. The domain of hospital resilience in the context of the global hospital industries in the disruption era could be highlighted if the informants also involved collaborators to gain a global perspective. Besides, this exploratory study could not show which domain significantly contributes to hospital resilience. Therefore, future studies need to show the influence of each domain on hospital resilience and how each domain correlates.
Conclusion
This paper addresses comprehensive hospital resilience domains and indicators that do not only focus on disaster aspects but also the disruptions faced by hospitals. The domain of hospital resilience in the era of disruption is more to prepare hospitals to face digitalization and compete with the market through centers of excellence, organizational structure flexibility, effective leadership, and the ability to redesign resources. In addition, in the context of a continuously changing hospital environment, hospitals need to have situation awareness capabilities, implement marketing management, expand networking, manage hospitals with modern management, and remain prepared in the face of disasters. This domain is a resilience capability that is developed according to experts from the perspective of the hospital context in Indonesia. The results of this qualitative research need to be continued for future research by verifying the construct indicators for the domains that have been identified. These findings give us insight into how resilience could be operationalized at the level of health facilities and could be used as self-assessment tools for hospitals to determine the level of hospital resilience.
Availability of data and materials
The datasets generated and analyzed in this study are available from the corresponding author upon reasonable request.
Abbreviations
- VUCA:
-
Volatility, Uncertainty, Complexity, Ambiguity
- EMR:
-
Electronic Medical Records
- HSI:
-
Hospital Safety Index
- HDR:
-
Hospital Disaster Resilience
- AI:
-
Artificial Intellilgent
References
Nemeth C, Wears R, Woods D, Hollnagel E, Cook R. Minding the Gaps: Creating Resilience in Health Care. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Rockville (MD). 2008.
Haldane V, De Foo C, Abdalla SM, Jung A-S, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80. https://doi.org/10.1038/s41591-021-01381-y.
Thomas S, Sagan A, Larkin J, Cylus J, Figueras J, Karanikolos M. Strengthening health systems resilience: Key concepts and strategies. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559803/.
Fridell M, Edwin S, von Schreeb J, Saulnier DD. Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Plann Manage. 2020;9(1):6–16. https://doi.org/10.15171/ijhpm.2019.71.
Biddle L, Wahedi K, Bozorgmehr K. Health system resilience: a literature review of empirical research. Health Policy Plan. 2020;35(8):1084–109. Available from: https://doi.org/10.1093/heapol/czaa032.
Harisuthan S, Hasalanka H, Kularatne D, Siriwardana C. Applicability of the PTVA-4 model to evaluate the structural vulnerability of hospitals in Sri Lanka against tsunami. Int J Disaster Resil Built Environ. 2020;11(5):581–96.
Iflaifel M, Lim RH, Ryan K, Crowley C. Resilient health care: a systematic review of conceptualisations, study methods and factors that develop resilience. BMC Health Serv Res. 2020;20(1):1–21.
United Nations. Hyogo Framework for Action 2005-2015: Building the Resilience of Nations and Communities to Disasters. 2005. Available from: https://www.unisdr.org/2005/wcdr/intergover/official-doc/L-docs/Hyogo-framework-for-action-english.pdf.
Arab M, Khankeh H, policy AM-… and healthcare, 2019 undefined. Developing a hospital disaster risk management evaluation model. ncbi.nlm.nih.gov [Internet]. [cited 2020 Nov 4]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6911334/.
Aliabadi S, Ostadtaghizadeh A, Ardalan A, Fatemi F, Aliabadi S, Ardalan A, et al. Towards Developing a Model for the Evaluation of Hospital Disaster Resilience: A Systematic Review. Springer [Internet]. 2020 Jan 29 [cited 2020 Nov 4];20(1):64. Available from: https://www.researchsquare.com/article/rs-3063/latest.pdf.
Fallah-Aliabadi S, Ostadtaghizadeh A, Ardalan A, Fatemi F, Khazai B, Mirjalili MR. Towards developing a model for the evaluation of hospital disaster resilience: a systematic review. BMC Health Serv Res. 2020 Jan;20(1):1–11.
Zhong S. Zhong, S. (2014). Developing an evaluation framework for hospital disaster resilience: tertiary hospitals of Shandong province, China [internet]. Queensland University of Technology; 2014. Available from: http://eprints.qut.edu.au/76090/1/Shuang_Zhong_Thesis.pdf.
EU Expert Group on Health Systems Performance Assessment (HSPA). Assessing the resilience of health systems in Europe: an overview of the theory, current practice and strategies for improvement [Internet]. 2020. 88 p. Available from: https://ec.europa.eu/health/sites/health/files/systems_performance_assessment/docs/2020_resilience_en.pdf.
Blanchet K, Nam SL, Ramalingam B, Pozo-Martin F. Governance and capacity to manage resilience of health systems: towards a new conceptual framework. Int J Health Policy Manag. 2017;6(8):431–5. https://doi.org/10.15171/ijhpm.2017.36.
Nuzzo JB, Meyer D, Snyder M, Ravi SJ, Lapascu A, Souleles J, et al. What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Public Health. 2019;19(1):1–9.
Kieny M, Evans DB, Kadandale S. Health-system resilience: reflections on the Ebola crisis in western Africa. Bull World Health Organ. 2014;92:850.
The Infrastructure Security Partnership (TISP). Regional Resilience Disaster a Guide for Developing an Action Plan 2011 edition. Alexandria: The Infrastructure Security Partnership; 2011.
Coiera E, Braithwaite J. Turbulence health systems: engineering a rapidly adaptive health system for times of crisis. BMJ Health Care Inform. 2021;30(01):017–25.
Cristian B. Hospital resilience: a recent concept in disaster preparedness. J Crit Care Med. 2018;4(3):81–2.
Zhong S, Clark M, Hou X-YY, Zang Y, Fitzgerald G. Validation of a framework for measuring hospital disaster resilience using factor analysis. Int J Environ Res Public Health. 2014;11(6):6335–53. Available from: www.mdpi.com/journal/ijerphArticle.
Samsuddin NM, Takim R, Nawawi AH, Syed Alwee SNA. Disaster preparedness attributes and Hospital’s resilience in Malaysia. Procedia Eng. 2017;2018(212):371–8. https://doi.org/10.1016/j.proeng.2018.01.048.
Khademi Jolgehnejad A, Ahmadi Kahnali R, Heyrani Al. Factors Influencing Hospital Resilience. Disaster Med Public Health Prep. 2021;15(5):661–8.
Suk JW, Koh MS. Development of nursing workplace spirituality instrument: confirmatory factor analysis. J Korean Acad Nurs Adm. 2016;22(1):99.
Jo S, Kurt S, Bennett JA, Mayer K, Pituch KA, Simpson V, et al. Nurses’ resilience in the face of coronavirus (COVID-19): an international view. Nurs Health Sci. 2021;23:646–57.
Madrigano J, Chandra A, Costigan T, Acosta JD. Beyond disaster preparedness: building a resilience-orientedworkforce for the future. Int J Environ Res Public Health. 2017;14(12):1563.
Huang L, Wang Y, Liu J, Ye P, Cheng B, Xu H, et al. Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 novel coronavirus disease (COVID-19): a cross-sectional study. Med Sci Monit. 2020;26:1–10.
Barbash IJ, Kahn JM. Fostering hospital resilience—lessons from COVID-19. J Am Med Assoc. 2021;15213:7–8.
Shaw B, Chisholm O. Creeping through the backdoor: disruption in medicine and health. Front Pharmacol. 2020;11(June):1–7.
Massuda A, Hone T, Gomes Leles FA, De Castro MC, Atun R. The Brazilian health system at crossroads: progress, crisis and resilience. BMJ Glob Health. 2018;3:829. Available from: http://gh.bmj.com/.
Lewis R, Pereira P, Thorlby R, Warburton W. Understanding and Sustaining the Health Care Service Shifts Accelerated by COVID-19. The Health Foundation [Internet]. 2020;(September):1–17. Available from: https://www.health.org.uk/publications/long-reads/understanding-and-sustaining-the-health-care-service-shifts-accelerated-by-COVID-19.
Blas E, Limbambala ME. The challenge of hospitals in health sector reform: the case of Zambia. Health Policy Plan. 2001;16(SUPPL. 2):29–43.
Nong S, Yao NA. Reasons behind stymied public hospital governance reform in China. PLoS One. 2019;14(9):1–11.
Chung S, Shannon M. Hospital planning for acts of terrorism and other public health emergencies involving children. Arch Dis Child. 2005;90(12):1300–7.
Kaivo-oja JRL, Lauraeus IT. The VUCA approach as a solution concept to corporate foresight challenges and global technological disruption. Foresight. 2018;20(1):27–49.
Partners Global. Resiliency Ethos : Embracing Uncertainty. 2020. Available from: https://www.partnersglobal.org/newsroom/resiliency-ethos-embracing-uncertainty/.
World Health Organization. Health systems resilience toolkit [Internet]. 2022. Available from: https://www.who.int/publications/i/item/9789240048751.
World Health Organization. Implementation guide for health systems recovery in emergencies: transforming challenges into opportunities. World Health Organization. Regional Office for the Eastern Mediterranean. p. 40. Available from: https://iris.who.int/bitstream/handle/10665/336472/9789290223351-eng.pdf?sequence=1&isAllowed=y.
USAID. Blueprint for Global Health Resilience. 2021;(January):1–25. Available from: https://www.usaid.gov/global-health/health-systems-innovation/health-systems/resources/blueprint-resilience.
World Health Organization. Operational framework for building climate resilient health systems. Geneva: World Health Organisation; 2015. Available from: https://www.who.int/publications/i/item/9789240081888.
WHO. Practical actions in cities to strengthen preparedness for the COVID-19 pandemic and beyond: an interim checklist for local authorities. World Health Organization [Internet] 2020;(July):23. Available from: https://apps.who.int/iris/bitstream/handle/10665/333296/WHO-2019-nCoV-ActionsforPreparedness-Tool-2020.1-eng.xlsx.
World Health Organization (WHO). Ensuring a safe environment for patients and staff in COVID-19 health-care facilities: a module from the suite of health service capacity assessments in the context of the COVID-19 pandemic. 2020;(October):1–49. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-HCF_assessment-Safe_environment-2020.1.
World Health Organization (WHO). A tripartite guide to addressing zoonotic diseases in countries [internet]. World Organisation for Animal Health (OIE) 2019. 1–166 p. Available from: https://books.google.com.mt/books/about/Taking_a_Multisectoral_One_Health_Approa.html?id=uDC1DwAAQBAJ&printsec=frontcover&source=kp_read_button&redir_esc=y#v=onepage&q&f=false.
Wiig S, Aase K, Billett S, Canfield C, Røise O, Njå O, et al. Defining the boundaries and operational concepts of resilience in the resilience in healthcare research program. BMC Health Serv Res. 2020 Apr;20(1):330.
Comfort LK, Boin A, Demchak CC, editors. Designing resilience: preparing for extreme events. University of Pittsburgh Press; 2010. Available from: http://www.jstor.org/stable/j.ctt5hjq0c.
Xue X, Wang L, Yang R. Exploring the science of resilience: critical review and bibliometric analysis. Nat Hazards. 2018;1:90.
Johan Bergström SD. The 2010s and onward resilience engineering. Routledge: Foundation of Safety Science; 2019. p. 39.
Levine S. Psychological and social aspects of resilience: a synthesis of risks and resources Saul. Rev Gen Psychol. 2003;6:307–24.
Wiig S, Fahlbruch B. Exploring Resilience A Scientific Journey from Practice to Theory. Cham: Springer; 2022. p. 79–87. Available from: https://doi.org/10.1007/978-3-030-03189-3.
Cimellaro G, Malavisi M, Risk SM-A-AJ of, 2018 undefined. Factor analysis to evaluate hospital resilience. ascelibrary.org [Internet]. [cited 2020 Nov 4]; Available from: https://ascelibrary.org/doi/abs/10.1061/AJRUA6.0000952.
Zaboli R, Seyedin H, Nasiri A, Malmoon Z. Standardization and Validation of Organizational Resilience Tools in Military Hospitals. Journal of Military Medicine [Internet]. [cited 2020 Nov 19];2020(7). Available from: http://militarymedj.ir/browse.php?a_id=2363&sid=1&slc_lang=en&ftxt=1.
Zhong S, Hou X-YY, Zang Y-LLYY-L, Fitzgerald G, Clark M, Hou X-YY, et al. Development of hospital disaster resilience: conceptual framework and potential measurement. Emerg Med J. 2013;31(11):930–8. Available from: http://journals.bmj.com/cgi/reprintform.
Samsuddin NM, Takim R, Nawawi AH, Syed Alwee SNA. Disaster preparedness attributes and Hospital’s resilience in Malaysia. Procedia Eng. 2018;212(January):371–8.
Wicker P, Filo K, Cuskelly G. Organizational resilience of community sport clubs impacted by natural disasters. J Sport Manag. 2013;27(6):510–25.
McManus S, Seville E, Vargo J, Brunsdon D. Facilitated process for improving resilience. Nat Hazards Rev. 2008;9(May):81–90.
Sincorá LA, de Oliveira MPV, Zanquetto-Filho H, Ladeira MB. Business analytics leveraging resilience in organizational processes. RAUSP Manag J. 2018;53(3):385–403.
Gittell JH. Relationships and resilience: care provider responses to pressures from managed care. J Appl Behav Sci. 2008;44(1):25–47.
Duchek S. Organizational resilience: a capability-based conceptualization. Bus Res. 2020;13(1):215–46. https://doi.org/10.1007/s40685-019-0085-7.
Koronis E, Ponis S, Koronis E, Ponis S. Better than before : the resilient organization in crisis mode. J Bus Strategy. 2018;39(1):32–42.
Annarelli A, Nonino F. Author ’ s accepted manuscript strategic and operational Management of Organizational Resilience : current state of research and future directions strategic and operational Management of Organizational Resilience : current state of research and future Dir. Omega. 2015;62:1–18.
Kim JS, Choi JS. Factors influencing emergency nurses’ burnout during an outbreak of Middle East respiratory syndrome coronavirus in Korea. Asian Nurs Res. 2016;10(4):295–9. Available from: http://www.sciencedirect.com/science/article/pii/S1976131716302572.
Ortiz-Barrios M, Gul M, … PL-M-I journal of, 2020 undefined. Evaluation of hospital disaster preparedness by a multi-criteria decision making approach: The case of Turkish hospitals. Elsevier [Internet]. [cited 2020 Nov 19]; Available from: https://www.sciencedirect.com/science/article/pii/S221242092030354X.
Mafabi S, Munene J, Ntayi J. Knowledge management and organisational resilience: Organisational innovation as a mediator in Uganda parastatals. J Strateg Manag. 2012;5(1):57–80.
Lengnick-Hall CA, Beck TE, Lengnick-Hall ML. Developing a capacity for organizational resilience through strategic human resource management. Hum ResourManag Rev. 2011;21(3):243–55. https://doi.org/10.1016/j.hrmr.2010.07.001.
Hamel G, Välikangas L. The quest for resilience by Gary Hamel and Liisa Välikangas. Harv Bus Rev. 2003;81:52–63.
Kativhu S, Mwale M, Francis J. Approaches to measuring resilience and their applicability to small retail business resilience. Probl Perspect Manag. 2018;16(4):275–84.
Allen R, Toder F. A model of organizational recovery. J Emerg Manag. 2004;2(1):41–5.
Lee AV, Vargo J, Seville E. Developing a tool to measure and compare organizations’ resilience. Nat Hazards Rev. 2013;14(1):29–41.
Hillmann J, Guenther E. Organizational Resilience: A Valuable Construct for Management Research? Int J Manage Rev. 2021;23(1):7–44. Available from: https://onlinelibrary.wiley.com/doi/10.1111/ijmr.12239.
Mahendradhata Y, Trisnantoro L, Listyadewi S, Soewondo P, MArthias T, Harimurti P, et al. The Republic of Indonesia Health System Review. Health Syst Transit. 2017;7:1.
Kementerian Perencanaan Pembangunan Nasional. Buku Putih Reformasi Sistem Kesehatan Nasional. Jakarta: Direktorat Kesehatan dan Gizi Masyarakat Kedeputian Pembangunan Manusia, Masyarakat, dan Kebudayaan; 2022. Available from: https://perpustakaan.bappenas.go.id/e-library/file_upload/koleksi/migrasi-data-publikasi/file/Policy_Paper/BukuPutihReformasiSKN.pdf.
Nurhayati-wolff H. Health in Indonesia - Statistics & Facts. 2022. p. 7–10. Available from: https://www.statista.com/topics/4873/health-in-indonesia/#topicOverview.
Kementrian Kesehatan RI. UU no. 44 Tahun 2009 Tentang RS. Undang-Undang Republik Indonesia [Internet] 2009;1:41. Available from: https://peraturan.go.id/common/dokumen/ln/2009/uu0442009.pdf.
Peraturan Pemerintah. Peraturan Pemerintah Nomor 47 Tahun 2021 tentang Penyelenggaraan Bidang Perumahsakitan. 2021;(086146). Available from: https://peraturan.bpk.go.id/Details/161982/pp-no-47-tahun-2021.
Ministry of Health. Peraturan Menteri Kesehatan Tentang Perubahan Atas Peraturan Menteri Kesehatan Nomor 21 Tahun 2020 Tentang Rencana Strategis Kementerian Kesehatan Tahun 2020-2024. 16 Januari 2020. 2020;(3):1–592. Available from: https://peraturan.bpk.go.id/Home/Download/212694/PermenkesNomor13Tahun2022.pdf.
Indonesia Ministry of Health. Instrumen Survei SNARS edisi 1 Tahun 2018. Available from: https://rspmanguharjo.jatimprov.go.id/wp-content/uploads/2020/09/Instrumen-Survei-SNARS-ed-1-Tahun-2018-1.pdf.
Ministry of Health. Pedoman Standar Akreditasi Rumah Sakit Kemkes 2022 [Internet]. 2022. Available from: https://yankes.kemkes.go.id/unduhan/fileunduhan_1654499045_682777.pdf.
Juharoh. Terapan Hospital Disaster Plan pada Rumah Sakit Umum Daerah Juharoh. Higeia J Public Health Dev. 2021;5(1):24–38.
Jahangiri K, Izadkhah Y, Health AL-IJ of, 2014 undefined. Hospital safety index (HSI) analysis in confronting disasters: A case study from Iran. ijhsdm.org [Internet]. [cited 2020 Nov 19]; Available from: http://www.ijhsdm.org/article.asp?issn=2347-9019;year=2014;volume=2;issue=1;spage=44;epage=49;aulast=Jahangiri.
Peyravi M, Marzaleh MA, Gandomkar F, Zamani AA, Khorram-Manesh A. Hospital safety index analysis in Fars Province hospitals, Iran, 2015-2016. Am J Disaster Med. 2019;14(1):25–32.
Ardalan A, Kandi M, Talebian M, Khankeh HR, Masoumi G, Mohammadi R, et al. Hospitals Safety from Disasters in I.R.Iran: The Results from Assessment of 224 Hospitals. PLoS Curr. 2014;6. Available from: https://www.researchgate.net/publication/260529267_Hospitals_Safety_from_Disasters_in_IRIran_The_Results_from_Assessment_of_224_Hospitals.
Indonesia Ministry of Health. Keputusan Menteri Kesehatan Republik Indonesia No. HK.01.07/Menkes/1128/2022 Tentang Standar Akeditasi Rumah Sakit. 2022. Available from: https://peraturanpedia.id/download/?id=aHR0cHM6Ly9kcml2ZS5nb29nbGUuY29tL2ZpbGUvZC8xTktLVjhDNTlfOVFJUzRieFU4ckVHV3VhRU9xSVZGbE8vdmlldw==#google_vignette.
Sunindijo RY, Lestari F, Wijaya O. Hospital safety index: assessing the readiness and resiliency of hospitals in Indonesia. Facilities. 2019;38(1–2):39–51.
Pan American Health Organization (PAHO). Hospital Safety Index Guide for Evaluators. Washington DC. 2018. Available from: https://iris.paho.org/bitstream/handle/10665.2/51448/9789275120293_eng.pdf?sequence=1&isAllowed=y.
Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. 2020; https://doi.org/10.1377/hlthaff.
Cox BC, Amin K, Kff RK. How have health spending and utilization changed during the coronavirus pandemic? 2021. p. 1–5. Available from: https://healthsystemtracker.org/chart-collection/how-have-healthcare-utilization-and-spending-changed-so-far-during-the-coronavirus-pandemic/.
Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127–8.
Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3):11–7.
Cordina J, Levin E, Ramish A, Seshan N. How COVID-19 has changed the way US consumers think about healthcare. McKinsey Insights [Internet] 2021;N.PAG-N.PAG. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=bth&AN=150719372&site=eds-live.
Ustgorul S. Why Healthcare Managers Should Understand and Apply the World of VUCA? In: Akkaya B, Guah MW, Jermsittiparsert K, Bulinska-Stangrecka H, Kaya Y, editors. Agile management and VUCA-RR: opportunities and threats in industry 40 towards society 50 [internet]. Emerald Publishing Limited; 2022. p. 115–27. https://doi.org/10.1108/978-1-80262-325-320220008.
Sharma SK, Sharma N. Hospital preparedness and resilience in public health emergencies at district hospitals and community health Centres. J Health Manag. 2020;22(2):146–56.
Reddy M. Digital Transformation in Healthcare in 2021: 7 key trends. Digital Authority Partners. 2022:1–15. Available from: https://www.digitalauthority.me/resources/state-of-digital-transformation-healthcare/.
Ruiz Morilla MD, Sans M, Casasa A, Giménez N. Implementing technology in healthcare: insights from physicians. BMC Medical Inform Decis Mak. 2017;17(1):1–9.
Hanefeld J, Mayhew S, Legido-Quigley H, Martineau F, Karanikolos M, Blanchet K, et al. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan. 2018;33(3):355–67.
World Health Organization (WHO). Strengthening hospital resilience in the Eastern Mediterranean Region: A policy paper on facility-level preparedness. Cairo. 2022. Available from: https://applications.emro.who.int/docs/9789290229582-eng.pdf.
Approaches N, Challenges E. A systemic resilience approach to dealing with Covid-19 and future shocks. OECD Publishing; 2020. p. 1–18.
Kruk C, Ling EJ, Bitton A, Cammett M, Cavanaugh K, Chopra M, et al. Building Resilient Health Systems: A Proposal for a Resilience Index. bmj.com [Internet]. 2017 [cited 2020 Nov 4]; Available from: http://www.bmj.com/subscribe.
Barasa E, Mbau R, Policy LG-IJ of H, 2018 undefined. What is resilience and how can it be nurtured? A systematic review of empirical literature on organizational resilience. ncbi.nlm.nih.gov [Internet]. [cited 2020 Nov 19]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6015506/.
Elger C. 3 Reasons Why Health Care Providers are Facing Disruption. 2019. Available from: https://ideawake.com/3-reasons-why-health-care-providers-are-facing-disruption/.
Purcarea VL. The impact of marketing strategies in healthcare systems. J Med Life. 2019;12(2):93–6.
Gunawan I, Sopaheluwakan J, Sagala SAH, Zawani H, Amin S, Mangunsong RTJ. Building Indonesia’s resilience to disaster : experiences from mainstreaming disaster risk reduction in Indonesia program. The World Bank; 2016. p. 1–348.
Djalante R, Garschagen M, Thomalla F, Shaw R. Introduction: Disaster Risk Reduction in Indonesia: Progress, Challenges, and Issues. 2017. p. 1–17. Available from: https://www.researchgate.net/publication/316627019_Introduction_Disaster_Risk_Reduction_in_Indonesia_Progress_Challenges_and_Issues/citation/download.
Acknowledgements
Not applicable.
Funding
This research was supported by the Ministry of Research, Technology, and Higher Education Indonesia for research funding Grant 2022.
Author information
Authors and Affiliations
Contributions
NS: wrote the main manuscript, conducted interviews and data analysis. MO: drafted the manuscript and review the data interpretation. SAP, AIS, AZ advised in study design and data interpretation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and consent to participate in this study were given by the Research Ethics Review Committee of the Public Health Faculty, Hasanuddin University (Approval No. 9860/UN4.14.1/TP.01.02/2022). All methods were carried out in accordance with relevant guidelines and regulations. All subjects’ informed consent was obtained from all subjects and/or their legal guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sari, N., Omar, M., Pasinringi, S.A. et al. Developing hospital resilience domains in facing disruption era in Indonesia: a qualitative study. BMC Health Serv Res 23, 1395 (2023). https://doi.org/10.1186/s12913-023-10416-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10416-8