Abstract
Background
People with disabilities (PWD) have different health service needs and different factors affect the utilization of these services. Therefore, the aim of this present study was to identify determinants of inpatient healthcare utilization among PWDs in Iran.
Methods
This research was a secondary data analysis of a cross-sectional study. The present study used data gathered for 766 PWDs (aged 18 years and older) within the Iranian Society with Disabilities (ISD) between September and December 2020. Multiple logistic regression models calculated adjusted odds ratios (aOR) and 95% confidence intervals in order to identify determinants of inpatient healthcare utilization among PWDs.
Results
Data for 766 people with disabilities were analyzed. A large number of participants were over 28 years of age (70.94%), male (64.36%), and single (54.02%). In the present study, more than 71% of participants had no history of hospitalization during the last year. In this study, males [aOR 2.11(1.14–3.91), participants with Civil Servants health insurance coverage [aOR 3.44 (1.16 − 10.17)] and individuals in the 3th quartile of disability severity [aOR 2.13 (1.01 − 4.51)] had greater odds of inpatient healthcare utilization compared to the other groups. The value of the concentration index (C) for inpatient healthcare utilization was − 0.084 (P.value = 0.046). The decomposition analysis indicated that gender was the greatest contributor (21.92%) to the observed inequality in inpatient healthcare utilization among participants.
Conclusion
Our findings suggested that the likelihood of hospitalization among the study participants could be significantly influenced by factors such as gender, the health insurance scheme, and the degree of disability severity. These results underscore the imperative for enhanced access to outpatient services, affordable insurance coverage, and reduced healthcare expenditures for this vulnerable population. Addressing these issues has the potential to mitigate the burden of hospitalization and promote better health outcomes for disadvantaged individuals.
Similar content being viewed by others
Introduction
People have the basic right to health, which contribute to people’s preference of an acceptable level of overall health, financial protection against high healthcare costs, and responsiveness to the clinical and non-clinical needs of people who seek health services; these are the main goals of the health system [1]. International policy documents, including the Declaration of Alma-Ata [2], the 2030 Agenda for Sustainable Development [3], and the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD) [4] have referred to this issue.
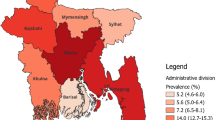
The World Health Organization (WHO) estimates that more than one billion people, or 15% of the world’s population, live with a disability, 80% of which are in low- and middle-income countries [5]. Based on the annual survey of Eurostat statistics on income and living conditions in Europe, the prevalence of disability is higher among female, older and less educated [6].
To support the people with disabilities, there are various policies in the world. The World Health Assembly has emphasized health systems policies and research on disability through the resolution. “Resolution on the Highest Attainable Standard of Health for Persons with Disabilities” which member states requested WHO “to establish a support the global research program. which aligns with UHC, health emergencies and health and well-being, including health systems and policy research” [7].
Also, in Iran, according to the law on the protection of the rights of people with disabilities of the Islamic Council, the Ministry of Health, Treatment and Medical Education is obliged to provide health insurance coverage for people with disabilities covered by the organization in such a way that in addition to providing the medical services needed by these people, physical rehabilitation services and cover the mental health of people with disabilities [8].
Despite these laws, PWDs often experience a lower level of health than healthy people for various reasons [9]. PWDs disproportionately experience unmet healthcare needs and health disparities [10]. According to international evidence, PWDs around the world face certain barriers when accessing healthcare services [11, 12].
In general, PWDs have poorer access to health care despite a greater need for them [13, 14], and inequality in access to health care is a global issue that leads to poorer health outcomes [15]. In addition, this inequality is considerable among PWDs. A recent survey by the WHO shows that 76–85% of PWDs living in developing countries do not receive any healthcare and only 2–3% of these people can access rehabilitation services [16]. Various factors affect access to health services. The results of the study by Shamyr (2011) [17] showed that people with multiple or mobility disabilities and who are less than 78 years of age, and people who experience transportation barriers to health services centers, were more exposed to health service access problems. Therefore, knowing these factors which affect the health service utilization can be an important health indicator to use in improving health care services and utilization for people with disabilities.
In various studies [18, 19], the socio-economic factors affecting patients health services utilization have been examined. The study of Asghari et al. [20] has investigated health services utilization in mentally disabled children and the factors affecting them, but no study has been conducted that examines the socioeconomic factors affecting the hospitalization rates of people with different degrees of disabilities. Therefore, the main objectives of the present study included: To identify determinants of inpatient healthcare utilization; To measure socio-economic inequalities in inpatient healthcare utilization; and to determine major contributors to the socioeconomic-related inequality in inpatient healthcare utilization among PWDs in Iran.
Methods
Study design
Our study was a secondary data analysis of a cross-sectional dataset.
The study participation
In the present study data for 786 PWDs were analyzed. PWDs were recruited from the Iranian Society with Disabilities (ISD) between September and December 2020. The ISD is a non-governmental organization (NGO) that facilitates access to education and healthcare services for PWDs in all provinces of Iran [21]. At the time of the study, about 50,000 people with disabilities ≥ 18 years were member of the ISD. This institution has 19 branches and 47 local offices nationwide and provides various social, financial, educational and health support to its members. The sampling method in this study was convenience sampling. People with disabilities aged 18 and over and members of ISD with Iranian nationality, were included in the study.
Data collection
The sample of this study was 786 individuals. The sampling method used in this study was the convenience sampling method. To measure socioeconomic inequality, Karami Matin et al.‘s valid and reliable questionnaire was used [22]. This self-reported questionnaire contains questions related to demographic characteristics, socioeconomic status, and access to rehabilitation services. Additionally, the Washington Group short questionnaire on functioning was used to determine the type and the severity of disability [23]. Questions have been developed according to the most basic level of functioning: hearing, seeing, walking or climbing steps; remembering or concentrating; selfcare, and communicating. The six functions were adopted as universal, happening generally, and related to social inclusion. Also, the severity of functional limitation in each item was assessed by a four-point scale: “no difficulty”, “some difficulty”, “a lot of difficulties”, and “unable to do it”. Further details about this questionnaire have been reported by Palmer and Harley [24].
Due to the COVID-19 pandemic, an electronic format was used in collecting the data, and the link of the electronic questionnaire was sent to ISD members through messaging applications i.e., Telegram and WhatsApp.
Variables
The outcome variable was a binary variable showing whether the participants were hospitalized in a hospital during last year.
In this study, the severity of functional limitations was examined by a four-point scale: “no difficulty”, “some difficulty”, “a lot of difficulty”, and “unable to do it”. For further details on this questionnaire see the study by Palmer and Harley [25].
In this study, we utilized data on asset ownership (such as cars, microwave oven, twin refrigerators/side by side refrigerator, vacuum machine, personal computer, washing machine, and dishwasher) and housing features (such as private or rental housing and house area), and educational level of the participants to develop SES variable based on existing data.
To develop SES indicator, we employed Filmer and Pritchett’s method [26], which utilizes principal components analysis (PCA) to reduce multidimensional datasets on household asset ownership to a lower number of dimensions. This approach allowed us to divide the participants into five wealth quintiles, ranging from the lowest (1st quintile) to the highest (5th quintile) groups.
In our study, we examined several potential contributors to the observed socioeconomic inequality in poor financial access to rehabilitation services. These contributors included:
-
Gender: Participants were categorized as male or female; Age: Age groups were defined as 18–27 years, 28–37 years, 38–47 years, 48–57 years, and 58 years or older; Marital Status: Participants were classified as single, married, or widowed/divorced; Place of Residence: Participants were categorized based on their place of residence (urban or rural areas); Head of Household: Participants were identified as either the head of the household or not; Health Insurance coverage: Health insurance coverage was categorized into groups such as no insurance, Social Security, Military, Universal Health Insurance, Civil Servants, and Other; Education: Education levels were classified as illiterate, primary school, secondary school, high school, and academic.
Data analysis
Firstly, the multiple logistic regression model was applied to calculate adjusted odds ratios (aOR) and 95% confidence intervals in order to identify determinants of inpatient healthcare utilization among PWDs.
Also, we used the concentration index (C) to measure the socio-economic inequalities in inpatient healthcare utilization among participants. The C is a standard measure to quantify income-related inequalities in health economics [27]. This index is twice the area between the concentration curve and the 45° line indicating no relationship between the two variables [28]. The concentration curve serves as the bivariate counterpart to the Lorenz curve, providing a visual representation of the cumulative proportion of hospitalizations relative to the cumulative proportion of the population, categorized by their socio-economic status (SES). In situations where income-related inequalities do not exist, the concentration index attains a value of zero.
As per convention, the concentration index assumes a negative value when the curve extends above the line of equality. This signifies an imbalanced concentration of the health variable among individuals with lower socio-economic status, often denoting economic disadvantage. Conversely, a positive value is assigned to the concentration index when the curve falls below the line of equality. Concerning health variables, especially those categorized as ‘undesirable,‘ such as poor health, a negative concentration index suggests a higher prevalence of the health issue within the economically disadvantaged population. The Concentration index is defined as [29]:
The C ranges from 1 − n/n (maximal pro-poor inequality i.e. the health outcome is concentrated on the poorest individual) to n − 1/n (maximal pro-rich inequality).
In addition, C was decomposed to measure the proportion of different socio-economic variables in inequalities.
The estimated value of the normalized C was decomposed to identify the contribution of explanatory variables to the observed socioeconomic inequality in inpatient healthcare utilization. Wagstaff and colleagues [30] showed that if we have a regression model relating a health outcome variable of \(y\) to a set of \(k\) explanatory variables, \(x,\) such as:
The C for \(y\) can be decomposed as:
In this equation, \({\stackrel{-}{x}}_{k}\) indicates the mean of the explanatory variable, \(x\), \({C}_{k}\) is the C for each explanatory variable, and \(G{C}_{\varepsilon }\) shows the generalized C for \(\varepsilon\). In Eq. 2, the first component \(\sum _{k}\left( \frac{{\beta }_{k}{\stackrel{-}{x}}_{k}}{\mu }\right){C}_{k}\) shows the contribution of explanatory variable \(x\) to the overall socioeconomic-related inequality in the outcome variable. The positive contribution of an explanatory variable explains that the SES-related distribution of this variable increases the concentration of inpatient healthcare utlization among the high SES individuals. Also, in Eq. 2, the second component, \(\frac{G{C}_{\varepsilon }}{\mu }\) indicates the proportion of socioeconomic inequality in inpatient healthcare utilization which is not explained by the systematic variation of the included explanatory variables across SES groups. Applying Wagstaff’s [31] correction into Equation results in:
Given that inpatient healthcare utilization was a binary variable, we used marginal effects derived from a logistic model as \(\beta\) in the decomposition of the \({C}_{n}\). Stata version 14.2 software (Stata Corp, College Station, TX, USA) was applied for data analysis
Results
Characteristics of participants
Following the exclusion of missing data, a total of 766 individuals with disabilities were included in the data analysis. A large number of participants were over 28 years of age (70.94%), the majority of the sample were male (64.36%), and single (54.02%), and persons living in urban area (88.33%). Most of respondents (72.39%) are in the first quartile in terms of severity of disability. In terms of socioeconomic status, they are almost equally distributed in the quintiles (Table 1).
Hospitalization frequency among people with disabilities
According to Fig. 1 and 71.84% of participants had no history of hospitalization during the last year. About 17% of participants used inpatient healthcare once a year, while others were hospitalized twice or more than two time within a year.
Determinants of relationship between hospitalization rate and demographic and socioeconomics characteristics of participants
As shown in Table 2, men were 2.11 times more likely to use inpatient healthcare compared to women. The Civil Servants health insurance scheme was associated with a higher hospitalization rate [aOR 3.44 (1.16 − 10.17)]. Also, individuals in the 3th quartile of disability severity had 2.13 times greater odds [ aOR 3.44 (1.01 − 4.51)] of hospitalization compared to the 1st quartile.
Socioeconomic inequality in inpatient healthcare utilization
As shown in Fig. 2, in this study the value of the concentration index (C) for the occurrence of hospitalization was − 0.084 (p-value = 0.046, Standard error = 0.073), indicating that the occurrence of hospitalization was concentrated among the participants with lower SES.
In addition, the value of the concentration index (C) for the occurrence of hospitalization for men and women were − 0.077 (p-value = 0.442, Standard error = 0.1), and − 0.095 (p-value = 0.038, Standard error = 0.11), respectively, indicating that the occurrence of hospitalization was concentrated among women with lower SES than men (Fig. 3).
Decomposition analysis of socioeconomic-related inequalities in inpatient healthcare utilization
Regarding Table 3, the decomposition analysis indicated that gender was the greatest contributor (21.92%) to the observed inequality in inpatient healthcare utilization among participants. In other words, decomposition analysis reveals that being male is associated with lower SES and higher likelihood of inpatient healthcare utilization. This positive contribution is a result of both the negative C for males and the positive elasticity of all measures of inpatient healthcare utilization with respect to gender status.
Discussion
This study aimed to identify the determinants of hospitalization rate among people with disabilities in Iran. Based on the findings, more than 28% of participants had at least one hospitalization in the last year and occurrence of hospitalization was concentrated among the participants with a lower SES.
In our study, C was negative, which indicates a high level of hospitalization rate in people with lower socioeconomic status, which has been confirmed in previous studies [18]. Thomas and Ellis [32], in the United States, found that among Medicaid enrollees with disabilities who utilize outpatient services, the extent of service utilization is inversely linked to employment rates. In other words, individuals who use these services most frequently, specifically those with 54 or more days of usage, had the lowest employment rates. Conversely, they observed that there is a positive correlation between the diversity of service utilization and employment, indicating that individuals with higher socioeconomic status are more likely to access a wide range of healthcare services.
In the study by Ahmadi et al. [33], in Iran, the use of specialized medical and dental services, inequality was in favor of high-income groups, and for general medical, family doctor, and primary health care services, inequality was in favor of low income groups. Additionally, Nooraei Motlagh [34], and Lorent [35] showed that economic status has the largest contribution to inequality in the use of outpatient and inpatient health services. Various studies [36,37,38,39,40] indicate that people with a higher SES and those who have health insurance coverage are more likely to receive outpatient services than inpatient care.
Studies highlighted that PWDs due to disability and associated health problems need more inpatient care compared to people without disabilities. For example, Venkata et al. indicated that PWDs (18.4%) significantly needed to visit a hospital more often during a year compared to people without a disability (8.8%) [41]. Also, studies indicate that SES can affect unmet need for disability-related health care services among adults with disabilities. Accordingly, Henry et al. [42], in the USA, reported that PWDs with greater unmet healthcare needs were significantly less likely to be working. Their unmet needs were particularly greater for physical health services (durable medical equipment, personal assistance services, supplies) and medications.
Our findings showed that men were more likely to use more inpatient healthcare compared to women. Also, decomposition analysis showed that being male is associated with lower SES and higher likelihood of inpatient healthcare utilization. This result was due to negative Ck for males and the positive elasticity for all measures of inpatient healthcare utilization with respect to the male gender. There can be several factors such as different healthcare–seeking behaviors, type and severity of disability, socioeconomic factors, communication, support systems, health literacy, and geographic and regional differences that contribute to the observation [43,44,45,46,47,48,49,50]. For example, Kung et al. [51], in Taiwan, reported that the rate of preventive health services is significantly higher among women with disabilities compared to men. Some studies note that women demonstrate a heightened awareness of their well-being in contrast to men, resulting in a higher utilization of preventive or/and outpatient services by the female population [52, 53].
Decomposition analysis indicated that health insurance has made a negative contribution to socioeconomic-related inequality in inpatient healthcare utilization. A negative Ck indicates that this factor has a negative impact on reducing the observed inequalities. In contrast, positive elasticity suggests that the utilization of inpatient healthcare services is positively responsive to the health insurance scheme. In other words, the presence of this scheme is associated with an increase in healthcare utilization. Overall, the result suggests that, among participants with disabilities, the health insurance scheme is having a positive impact on inpatient healthcare utilization. However, despite this positive effect, the overall socioeconomic-related inequalities in healthcare utilization still exist, and this may be due to other negative factors (such as negative Ck coefficients) offsetting the benefits of the health insurance scheme.
The study by Yahyavi Dizaj et al. [55] shows that the use of rehabilitation services was higher in households ranked in higher income groups. Regarding the incomplete insurance coverage for rehabilitation services, people with a higher SES have more chances to use such services which in turn can reduce the probability of the occurrence of hospitalization among PWDs. Also, it should be noted that people with severe disabilities may need to receive appropriate home care services, but these services are not covered by health insurances in Iran which can increase the possibility of hospitalization among PWDs in low-income groups.
Also, the results of logistic regression analysis indicate that people with civil servant insurance 3.44 were more likely to be hospitalized than people without insurance coverage. Regarding a direct relationship between insurance coverage and the quantity of service utilization [54, 55], this group can use more of these services compared to uninsured people. It can also be said that coverage of home care and rehabilitation services by military insurance is better than other insurances, so the inpatient health services need is reduced. Additionally, the results of Tajvar et al. [54] indicate that people who did not have basic insurance access were less likely to receive outpatient care compared to those without basic insurance, and this factor can lead to increase in hospitalization rates .
A negative summed percentage contribution for the wealth index indicates that, in the context of the decomposition analysis, the wealth index has a negative impact on these inequalities. In other words, higher wealth is associated with reduced inpatient healthcare utilization among individuals with disabilities, and this effect is strong enough to result in a negative overall contribution when considering all the factors involved in the analysis. The negative value of this parameter suggests that the wealth index’s contribution to inequalities is in the opposite direction of reducing healthcare utilization. In the context of healthcare access and utilization, a negative contribution from wealth indicates that higher wealth is associated with a lower likelihood of utilizing inpatient healthcare services among individuals with disabilities. This could be due to a variety of factors, such as financial barriers, access to alternative healthcare options, or differences in healthcare-seeking behaviors among wealthier individuals with disabilities [56,57,58].
Furthermore, decomposition analysis revealed that education has made a negative contribution to the observed inequality in inpatient healthcare utilization. The results of this analysis suggest that among participants with disabilities, higher education levels (such as academic level) are associated with increased inpatient healthcare utilization. However, paradoxically, this increased utilization might contribute to negative socioeconomic-related inequalities, meaning that individuals with higher education levels tend to be poorer and use more inpatient services. Understanding these dynamics is essential for addressing healthcare inequalities and tailoring interventions to ensure equitable access and utilization of healthcare services.
Limitations
Firstly, the emergence of the COVID-19 pandemic in Iran posed significant impediments to access PWDs, thereby exerting an impact on the data collection process. Furthermore, the utilization of online data collection methods may have inadvertently excluded individuals with disabilities who lacked access to essential communication tools, such as mobile phones or computers, as well as those with limited educational attainment. Consequently, it is imperative to acknowledge that our sample may not offer a comprehensive representation of the entire PWD population.
Also, the prevalence of the Covid-19 pandemic during the present study might have influenced the accessibility of inpatient healthcare services and hospitalization rates among PWDs. Additionally, it is worth noting that the exclusion of participants under the age of 18 in this study could potentially impact the generalizability of the results. The cross-sectional nature of this study, the lack of accurate clinical information about the disability status of participants, and self-reporting measures were the other limitations of this study.
Conclusion
Our findings suggested that the likelihood of hospitalization among the study participants could be significantly influenced by factors such as gender, the health insurance scheme, and the degree of disability severity. These results underscore the imperative for enhanced access to outpatient services, affordable insurance coverage, and reduced healthcare expenditures for this vulnerable population. Addressing these issues has the potential to mitigate the burden of hospitalization and promote better health outcomes for disadvantaged individuals.
Availability of data and materials
Data and all other materials for this study are kept at the deputy of research and technology of Kermanshah University of Medical Sciences. The datasets generated and/or analyzed during the current study are not publicly available due to the terms of consent in which the participants agreed too, but which are available from the corresponding author on reasonable request.
Abbreviations
- PWD:
-
People with disabilities
- C:
-
Concentration Index
- SES:
-
Socioeconomic Status
- PCA:
-
Principal Component Analysis
- ISD:
-
Iranian Society with Disabilities (ISD)
References
World Health Organization. The world health report 2000: health systems: improving performance. Geneva: World Health Organization; 2000.
Organization WH. Declaration of alma-ata. Regional Office for Europe: World Health Organization; 1978.
Horvath Z. Transforming our world-new agenda and goals for sustainable development. Hungarian YB Int’l L and Eur L. 2016;167:18-21.
Márton SM, Polk G, Fiala DRC. Convention on the rights of persons with disabilities. USA: United Nations; 2013.
Bright T, Wallace S, Kuper H. A systematic review of access to rehabilitation for people with disabilities in low-and middle-income countries. Int J Environ Res Public Health. 2018;15(10): 2165.
Marie L. Understanding EU policies for people with disabilities. 2022.
Organization WH. Global report on health equity for persons with disabilities. World Health Organization; 2022.
Center ICR. The Law on the Protection of the Rights of the Disabled Tehran Chairman of the Islamic Council; 2018.
Organization WH. World Bank (2011). World report on disability. 2017;15.
Pharr JR. Accommodations for patients with disabilities in primary care: a mixed methods study of practice administrators. Global J Health Sci. 2014;6(1):23.
Tomlinson M, Swartz L, Officer A, Chan KY, Rudan I, Saxena S. Research priorities for health of people with disabilities: an expert opinion exercise. Lancet. 2009;374(9704):1857–62.
Officer A, Posarac A. World report on disability. Geneva: World Health Organ; 2011.
Abdi K, Arab M, Rashidian A, Kamali M, Khankeh HR, Farahani FK. Exploring barriers of the health system to rehabilitation services for people with disabilities in Iran: a qualitative study. Electron Physician. 2015;7(7): 1476.
Abdi K, Arab M, Khankeh HR, Kamali M, Rashidian A, Farahani FK, et al. Challenges in providing rehabilitation services for people with disabilities in Iran: a qualitative study. J Adv Med Med Res. 2016;13(4):1–11.
Mulumba M, Nantaba J, Brolan CE, Ruano AL, Brooker K, Hammonds R. Perceptions and experiences of access to public healthcare by people with disabilities and older people in Uganda. Int J Equity Health. 2014;13(1):1–9.
Srivastava DK, Khan JA, Pandey S, Pillai DS, Bhavsar AB. Awareness and utilization of rehabilitation services among physically disabled people of rural population of a district of Uttar Pradesh, India. Int J Med Sci Public Health. 2014;3:1157–60.
Castro SS, Cieza A, Cesar CL. Problems with accessibility to health services by persons with disabilities in São Paulo. Brazil Disabil Rehabilitation. 2011;33(17–18):1693–8.
Rezapoor ARY, Ebadi Fard Azar F, Ghazanfari S, Abstract Mirzaei S, Sarabi Asiabar A, Bagheri Faradonbe S. Effective factors on utilization and access to health care:a population-based study in Kerman. J Health Adm. 2015;18(60):24–36.
Raghfar H, Zargari N, Sangari MK. Measuring inequality in households’health care expenditures in Iran. 2013.
Asghari MA, Holakoei Nayini, Majdzadeh, Soleimani A. The rate of benefiting from health services in mentally disabled children and the factors affecting it. Q J Health Fac Health Res Inst. 2007;5(1):29–37.
Disabilities ISw. Iranian Society with Disabilities. About Iranian Society with Disabilities; Available from: https://www.iransdp.com/about-iranian-society-sabled/. 2022 . Cited 2022 Oct 14.
Matin BK, Kamali M, Williamson HJ, Moradi F, Solatni S. The predictors of access to health services for people with disabilities: a cross sectional study in Iranian context. Med J Islamic Repub Iran. 2019;33:125.
The Washington Group. WG Short Set on Functioning Questions 2022 [Available from: https://www.washingtongroup-disability.com/fileadmin/uploads/wg/Washington_Group_Questionnaire__1_-_WG_Short_Set_on_Functioning__October_2022_.pdf. Accessed 18 Oct 2023.
Palmer M, Harley D. Models and measurement in disability: an international review. Health Policy Plann. 2012;27(5):357–64.
Palmer M, Harley D. Models and measurement in disability: an international review. Health Policy Plann. 2011;27(5):357–64.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in States of India*. Demography. 2001;38(1):115–32.
Wagstaff A. Inequality aversion, health inequalities and health achievement. J Health Econ. 2002;21(4):627–41.
World Bank. Concentration index 2018 [Available from: https://pubdocs.worldbank.org/PubDocsError.jsp?err_msg=Document%20is%20not%20available%20for%20public%20viewing.
O’Donnell O, O’Neill S, Van Ourti T, Walsh B. Conindex: estimation of concentration indices. Stata J. 2016;16(1):112–38.
Wagstaff A, Van Doorslaer E, Watanabe N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J Econom. 2003;112(1):207–23.
Wagstaff A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005;14(4):429–32.
Thomas KC, Ellis AR. Patterns of healthcare use and employment among people with disabilities. Disabil Health J. 2013;6(2):133–40.
Ahmadi A, Nikravan A, Naseri A, Asari A. Effective determinants in household out of packet payments in health system of Iran, using two part regression model. J Health Adm (JHA). 2014;17(56):7-18.
Nooraiee Motlagh S, Saber Mahani A, Barooni M, Asadi Lari M, Vaez Mahdavi MR, Hadian M. Determining factors related to health services utilization. Razi J Med Sci. 2015;21(127):61–72.
Lorant V, Boland B, Humblet P, Deliège D. Equity in prevention and health care. J Epidemiol Community Health. 2002;56(7):510–6.
Hassanzadeh J, Mohammadbeigi A, Eshrati B, Rezaianzadeh A, Rajaeefard A. Determinants of inequity in health care services utilization in Markazi Province of Iran. Iran Red Crescent Med J. 2013;15(5):363.
Hosseinpoor A-R, Naghavi M, Alavian SM, Speybroeck N, Jamshidi H, Vega J. Determinants of seeking needed outpatient care in Iran: results from a national health services utilization survey. Arch Iran Med. 2007;10(4):439–45.
Kim C-W, Lee S-Y, Hong S-C. Equity in utilization of cancer inpatient services by income classes. Health Policy. 2005;72(2):187–200.
Onwujekwe O, Onoka C, Uzochukwu B, Hanson K. Constraints to universal coverage: inequities in health service use and expenditures for different health conditions and providers. Int J Equity Health. 2011;10: 50.
Ferry GA, Dickson SR, Mbaruku G, Freedman LP, Kruk ME. Equity of inpatient health care in rural Tanzania: a population- and facility-based survey. Int J Equity Health. 2012;11(1): 7.
Gudlavalleti MVS, John N, Allagh K, Sagar J, Kamalakannan S, Ramachandra SS, et al. Access to health care and employment status of people with disabilities in South India, the SIDE (South India Disability evidence) study. BMC Public Health. 2014;14(1): 1125.
Henry AD, Long-Bellil L, Zhang J, Himmelstein J. Unmet need for disability-related health care services and employment status among adults with disabilities in the Massachusetts Medicaid program. Disabil Health J. 2011;4(4):209–18.
Whitman A, De Lew N, Chappel A, Aysola V, Zuckerman R, Sommers BD. Addressing social determinants of health: Examples of successful evidence-based strategies and current federal efforts. Off Heal Policy. 2022:1-30.
Green C, Dickinson H, Carey G, Joyce A. Barriers to policy action on social determinants of health for people with disability in Australia. Disabil Soc. 2022;37(2):206–30.
Froehlich-Grobe K, Douglas M, Ochoa C, Betts A. Social determinants of health and disability. Public health perspectives on disability: Science, social justice, ethics, and beyond. 2021:53-89.
McColl MA, Jarzynowska A, Shortt S. Unmet health care needs of people with disabilities: population level evidence. Disabil Soc. 2010;25(2):205–18.
Matin BK, Ballan M, Darabi F, Karyani AK, Soofi M, Soltani S. Sexual health concerns in women with intellectual disabilities: a systematic review in qualitative studies. BMC Public Health. 2021;21(1):1965.
Matin BK, Williamson HJ, Karyani AK, Rezaei S, Soofi M, Soltani S. Barriers in access to healthcare for women with disabilities: a systematic review in qualitative studies. BMC Womens Health. 2021;21(1):44.
Soltani S, Moghadam MM, Amani S, Akbari S, Shiani A, Soofi M. Socioeconomic disparities in using rehabilitation services among Iranian adults with disabilities: a decomposition analysis. BMC Health Serv Res. 2022;22(1):1449.
Soltani S, Takian A, Akbari Sari A, Majdzadeh R, Kamali M. Cultural barriers in access to healthcare services for people with disability in Iran: a qualitative study. Med J Islam Repub Iran. 2017;31:51.
Kung P-T, Tsai W-C, Li Y-H. Determining factors for utilization of preventive health services among adults with disabilities in Taiwan. Res Dev Disabil. 2012;33(1):205–13.
Vega J, Bedregal P, Jadue L, Delgado I. Gender inequity in the access to health care in Chile. Rev Med Chil. 2003;131(6):669–78.
Socías ME, Koehoorn M, Shoveller J. Gender inequalities in access to health care among adults living in British Columbia, Canada. Women’s Health Issues. 2016;26(1):74–9.
Tajvar M, Yaseri M, Karami B, Mohammadi M. Pattern of outpatient health service utilization by older people in Iran. Salmand: Iranian Journal of Ageing. 2021;15(4):410–27.
Yahyavi Dizaj J, Na’emani F, Fateh M, Soleimanifar M, Arab AM, Zali ME, et al. Inequality in the utilization of rehabilitation services among Urban and Rural households in Iran: a cross-sectional study. Archives of Rehabilitation. 2020;21(3):336–57.
Soltani S, Takian A, Akbari Sari A, Majdzadeh R, Kamali M. Financial barriers to access to health services for adult people with disability in Iran: the challenges for Universal health coverage. Iran J Public Health. 2019;48(3):508–15.
Parish SL, Swaine JG, Son E, Luken K. Determinants of Cervical cancer screening among women with intellectual disabilities: evidence from medical records. Public Health Rep. 2013;128(6):519–26.
Yahyavi Dizaj J, Khoramrooz M, Ramezani-Doroh V, Rezaei S, Hashempour R, Irandoust K, et al. Socioeconomic inequality in informal payments for health services among Iranian households: a national pooled study. BMC Public Health. 2023;23(1):381.
Acknowledgements
The authors would like to thank all people who participated in the study.
Funding
The present study was funded by the Kermanshah University of Medical Sciences through proposal number 4000821.
Author information
Authors and Affiliations
Contributions
BK, HD, RM, FM wrote the manuscript; SR, and FJ analyzed the data and revised the manuscript; SS and SA contributed to the design of the study, analyzing data, and redrafting the manuscript; BK and SS contributed to the literature review; All authors read and approved the submitted version and modified version of the manuscript. Also, all authors agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
• Badriyeh Karami: Ph.D. in Health Care Services Management, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
• Satar Rezaei:Associate Professor of Health Economics, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
• Hadi Darvishi Gillan: Ph.D. in Health Education and Promotion, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
• Shahram Akbari: Ph.D. in Health Care Management, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
• Raheleh Maleki: Ph.D. Candidate in Health care Services Management, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
• Fardin Moradi: Ph.D. in Health policy, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
• Faramarz Jalili: School of Health Administration, Dalhousie University, Halifax, NS, Canada.
• Mohammad Karami: Assistant Professor of Philosophy, Research Center for Environmental Determinants of Health, Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
• Shahin Soltani: Assistant Professor of Health policy, Research Center for Environmental Determinants of Health (RCEDH), Health Institute, Kermanshah University of Medical Sciences, Kermanshah, Iran.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study followed the national research ethics guidelines and was approved by the ethics committee of Kermanshah University of Medical Sciences (ref. nr: IR.KUMS.REC.1401.452). Informed consent was obtained in written format from all study participants. Informed consent for study participation has been obtained from the parents and/or legal guardians of all participating minors. The consent form included detailed information about the nature and purpose of the study, potential risks and benefits, the voluntary nature of participation, and the right to withdraw from the study at any time.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karami, B., Rezaei, S., Gillan, H.D. et al. Inpatient healthcare utilization among people with disabilities in Iran: determinants and inequality patterns. BMC Health Serv Res 24, 62 (2024). https://doi.org/10.1186/s12913-023-10383-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10383-0