Abstract
Background
An integrated practice unit (IPU) that provides a multidisciplinary approach to patient care, typically involving a primary care provider, registered nurse, social worker, and pharmacist has been shown to reduce healthcare utilization among high-cost super-utilizer (SU) patients or multi-visit patients (MVP). However, less is known about differences in the impact of these interventions on insured vs. uninsured SU patients and super high frequency SUs (\(\ge\)8 ED visits per 6 months) vs. high frequency SUs (4–7 ED visits per 6 months).
Methods
We assessed the percent reduction in ED visits, ED cost, hospitalizations, hospital days, and hospitalization costs following implementation of an IPU for SUs located in an academic tertiary care facility. We compared outcomes for publicly insured with uninsured patients, and super high frequency SUs with high frequency SUs 6 months before vs. 6 months after enrollment in the IPU.
Results
There was an overall 25% reduction in hospitalizations (p < 0.001), and 23% reduction in hospital days (p = 0.0045), when comparing 6 months before vs. 6 months after enrollment in the program. There was a 26% reduction in average total direct hospitalization costs per patient (p = 0.002). Further analysis revealed a greater reduction in health care utilization for uninsured SU patients compared with publicly insured patients. The program reduced hospitalizations for super high frequency SUs. However, there was no statistically significant impact on overall health care utilization of super high frequency SUs when compared with high frequency SUs.
Conclusions
Our study supports existing evidence that dedicated IPUs for SUs can achieve significant reductions in acute care utilization, particularly for uninsured and high frequency SU patients.
Trial Registration
IRB201500212. Retrospectively registered.
Similar content being viewed by others
Background
An analysis by the Agency for Healthcare Research and Quality (AHRQ) in 2012 showed that the sickest 5% of U.S. patients account for 58.9% of U.S. health care costs, and these figures have been relatively constant since the 1970s [1, 2]. Many of these high cost patients are super-utilizers (SUs), defined by the Robert Wood Johnson Foundation as, “individuals whose complex physical, behavioral, and social needs are not well met through the current fragmented health care system.” [3]. Multiple criteria for identifying super-utilizers exist, but no standard methodology is available for determining which criteria should be used for a specific population. Cluster analysis can aid in selecting characteristics from the literature that systematically differentiate super-utilizer groups from other beneficiaries [4, 5]. In 2013, several promising SU programs convened to outline key elements of success. While all interventions utilized a care team approach that typically consisted of a social worker, nurse, and community health worker, notably, successful interventions also implemented a patient-centered approach and emphasized a solid investment in human relationships [5, 6].
Robust integrated practice units (IPUs) have shown promise in reducing healthcare utilization by vulnerable patients. IPUs provide a multidisciplinary approach to patient care, typically involving a primary care provider, registered nurse, social worker, and pharmacist. Althaus and colleagues conducted a systematic review of primarily case management-based interventions aiming to reduce ED visits. Seven of the 11 reviewed studies showed significant reductions in ED utilization after intervention [7].
Several similar interventions that used IPUs have also shown marked reductions in acute care usage and costs [8, 9]. However, there are no published studies to our knowledge that have compared the impact of interdisciplinary programs on utilization outcomes with respect to the analysis of the patient’s payor status and frequency of ED utilization. The purpose of this study was to determine if establishing an IPU for our SU patient population would lead to decreased acute care utilization and decreased healthcare costs. In addition, we hoped to determine if frequency of ED use and insurance status would identify patient populations most likely to benefit from this intervention.
Methods
Study setting
This study was conducted at a southeastern US academic tertiary care facility housing a state-designated Level I Trauma center. With 946 licensed beds, this health system has on average 42,000 admissions and 100,000 adult ED visits per year. Our facility received grant funding from Centers for Medicare and Medicaid Services through the $35 Million Low Income Pool Award in the amount of $660,000 over 2 years.
Selection of participants
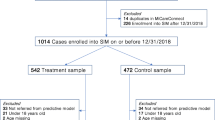
According to Locker and colleagues, ED visits of more than 4 per year are considered to be nonrandom events, and thus suggested this as a cutoff for defining patients who are ED super-utilizers [10]. In the year prior to the opening of our IPU (November 1, 2011 to October 31, 2012), we identified 2,485 patients who presented to our adult ED more than 4 times, accounting for 23% of ED visits and 20% of our total ED and hospitalization costs. Given the large size of this group and the small scale of our planned IPU intervention, we elected to focus on a smaller subset of patients with greater than or equal to 4 ED visits in 6 months. This group was further divided into high frequency patients (4–7 visits in 6 months) and super high frequency patients (\(\ge\) 8 visits in 6 months). During the study period of May 2012 to April 2015, a SU patient list was generated every 2 months on a rolling basis and was uploaded into our electronic medical record (EMR) so we could determine in real time, which SU patients were in the ED or hospitalized. The clinic Social Worker then contacted inpatient case managers recommending a referral to the clinic if appropriate. Enrollment in the IPU was optional, and those that attended the first IPU appointment were considered study participants.
Intervention
The clinic was open five half days per week and staffed by 1 hospitalist-at any time, a social worker, a clinical pharmacist, a registered nurse, and an addiction and pain management psychiatrist. The clinic provided patients with intensive but temporary services with an eventual plan to transition to a medical home [11]. At the first visit, a social worker performed a needs assessment to identify barriers to care such as lack of insurance, housing, and transportation. This assessment also included screenings for substance abuse, depression, and low health literacy. On subsequent visits the social worker connected patients to several resources available in the community, health insurance, transportation vouchers, and medication assistance. Hospitalists who staffed the clinic provided limited primary care services, subspecialty referrals, and referrals to an embedded pain management and addiction psychiatrist. The pharmacist reconciled medications, provided education regarding medication compliance, put medication in pill boxes, monitored opioid use when indicated, and recommended affordable medication options. The specifics of these interventions are detailed elsewhere [5]. The clinic served a dual purpose as a post-discharge clinic for non-super utilizing uninsured patients; however, outcomes for these patients are not included in this study.
Data
A retrospective chart review was conducted for the period of November 1, 2012 to April 30, 2015. All hospital utilization and demographic data were extracted from the EMR and cost data was extracted from the hospital data warehouse. We used a pre/post design such that each patient served as his/her own historical control comparing outcomes 6 months before vs. 6 months after the initial IPU appointment.
Outcomes
Primary outcomes evaluated pre and post enrollment were ED visits, ED total direct costs, hospitalizations, hospital days, and hospitalization total direct costs. Attendance at the first clinic appointment was considered enrollment in the study and the starting point of the post enrollment period. Patients who died during the study period were excluded from the analysis, as their inclusion could artificially affect the outcomes measured.
Analysis
For the enrolled SU patients, we compared the six-month period before vs. the first six-month period after enrollment in the clinic. Thus, each subject had two values for an outcome, be it number of visits or cost, denoted by Y1 (pre) and Y2 (post). This comparison is completely distribution-free but is conditional to the population who joined the SU program. The methods, following classical survey sampling ratio estimation, were selected prior to looking at any study data.
From central limit theory and the delta method, [12] using natural logarithms,
Log(\(\overline{Y}\)2 /\(\overline{Y}\)1) has an asymptotic normal distribution with mean log(µ2 / µ1) and variance.
V={(σ1/ µ1)2+(σ2/ µ2)2 -2ρ[σ1 σ2 /(µ1 µ2)}/N.
where µj and σj (j = 1 and 2) are the population mean and population standard deviation of Y1 and Y2, ρ is the correlation between Y1 and Y2 and N = sample size.
V can be replaced by, \(\hat {V}\), where the sample moments (mean, standard deviation, and correlation replace the population quantity without changing the large sample distribution.
-
(a)
The point estimate of µ2 / µ1 is \(\overline{Y}\)2 /\(\overline{Y}\)1.
-
(b)
A 95% confidence interval for µ2 / µ1 is bounded by.
\(\overline{Y}\)2 /\(\overline{Y}\)1 exp(± 1.96sqrt[\(\hat {V}\)]) where exp() is the natural antilog.
Estimated_Pct_reduction = 100 [(\(\overline{Y}\)2 /\(\overline{Y}\)1)-1]
Endpoints of the confidence limits are likewise calculated for percentage reduction.
The two-sided P-value is obtained from Z=|Log(\(\overline{Y}\)2 /\(\overline{Y}\)1)|/Sqrt(\(\hat {V}\))and we compared this against the standard normal distribution.
Results
Characteristics of study subjects
The study population included 186 SU patients who had 4 or more ED visits in the 6 months prior to their first clinic appointment. Demographic information can be found in Table 1. Pre-enrollment indices can be found in Table 2. 93% of patients enrolled had a mental health diagnosis and 66% had a substance use diagnosis.
Main results
Statistical analyses of all patients and 4 subgroups are summarized in Table 3. There was an 11% reduction in ED visits (p = 0.22), a 25% reduction in hospitalizations (p < 0.001), and a 23% reduction in hospital days (p = 0.0045), when comparing 6 months before versus 6 months after enrollment in the clinic for all patients enrolled in the study. There was also a 26% reduction in average total direct hospitalization costs per patient (p = 0.002).
Additional analysis showed that the intervention had a greater impact on uninsured patients compared to publicly insured patients (Table 3). For the uninsured subgroup, there was a 28% reduction in ED visits (p = 0.02), 29% reduction in ED costs (p = 0.028), 49% reduction in hospitalizations (p < 0.001), 50% reduction in hospitalization cost (p = 0.002), and a 44% reduction in hospital days (p = 0.005). In comparison, the only marginally significant outcome for the publicly insured subgroup was a 15% reduction in hospitalizations (p = 0.04).
Further subgroup analysis was conducted comparing high frequency (4–7 ED visits in 6 months) with super high frequency (\(\ge\)8 ED visits in 6 months) groups. In the high frequency subgroup, there was a 27% reduction in average ED visits (p = 0.01), 24% reduction in average ED cost (p-value= 0.039), 28% reduction in average hospitalizations (p < 0.001), 30% reduction in hospitalization cost (p = 0.005), and a 30% reduction in average hospital days (p = 0.003). In comparison, the super high frequency group outcomes were not statistically significant, with the exception of a 21% reduction in average hospitalizations (p = 0.04).
Discussion
Our study supports existing evidence that a dedicated IPU for super-utilizers can achieve significant reductions in acute care utilization and costs. Our subgroup analysis additionally revealed a significant reduction in hospitalizations (p < 0.01) and costs (p < 0.01) for uninsured patients and high ED frequency patients with minimal reductions in utilization and costs in the publicly insured and super-high ED frequency subgroups.
These findings help identify the patient subsets that are most likely to benefit from targeted multidisciplinary interventions. The results of this study suggest that uninsured patients and patients with high ED frequency may benefit from embedding social services, pharmacist-led education, and chronic pain and addiction treatment into low or no cost primary care settings.
We initially suspected differences between high ED frequency and super-high ED frequency patient groups could be accounted for by differences in mental and substance use, however we found that 96% of patients in the super-high ED frequency group had a mental health diagnosis and 71% a substance use diagnosis, compared with 92% with mental health issue and 64% with substance use in the high ED frequency groups. The publicly insured and uninsured groups also lacked significant differences in frequency of mental health diagnosis and substance use. One potential explanation is that the diagnoses present in the medical record problem lists are not specific enough to distinguish between disabling diagnoses which require attention and diagnoses with less clinical severity which overall do not impact the patient’s outcomes.
Another possible explanation for the differences between these subgroups is that our uninsured and high ED frequency patients may not have been as medically ill as our insured and super high ED groups. Future study involving in depth chart review and inclusion of the Charlson Comorbidity Index may further help to determine if medical complexity was comparable in these groups.
This study is limited in that it was observational and was done at one center, making generalization difficult. It is based on comparisons between pre-enrollment and post-enrollment. There are potential biases in both directions. On the one hand, there could be selection bias in the eligibility to join the intervention program that could create regression to the mean. But on the other hand, the general health of these frequent users could be deteriorating, leading to increased utilization.
Conclusion
In an era of acute care over-utilization, it is imperative that we develop targeted interventions that can ease preventable burdens on our healthcare system [13,14,15] High-utilizers with multiple chronic diseases and socioeconomic challenges often experience significant care fragmentation which can be exacerbated with each compounding condition [16]. The primary obstacle to delivering efficient supportive care lies in determining which individuals would benefit most from such targeted programs [5] Our study findings indicate that an IPU was associated with a potential reduction on acute care utilization and reduction in costs for uninsured and high ED frequency patients. Further study and investigation are needed to understand which components of the IPU may benefit uninsured and high ED frequency patients. In addition, future research should determine what types of interventions would better serve the publicly insured and super high frequency patient groups.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due presence of patient health information and privacy concerns but are available from the corresponding author on reasonable request.
References
Cohen S. Differentials in the Concentration of Health Expenditures across Population Subgroups in the U.S., 2012 Statistical Brief #448. September 2014. Agency for Healthcare Research and Quality, Rockville, MD. http://meps.ahrq.gov/mepsweb/data_files/publications/st448/stat448.shtml.
Stanton MW, Rutherford MK. The high concentration of US health care expenditures. AHRQ Pub No. 06–0060. June 2006. Agency for Healthcare Research and Quality Rockville, MD. Available at: https://archive.ahrq.gov/research/findings/factsheets/costs/expriach/.
Better Care for Super-Utilizers. Available at: http://www.rwjf.org/en/library/collections/super-utilizers.html. Accessed October 21, 2016.
Grafe CJ, Horth RZ, Clayton N, Dunn A, Forsythe N. How to classify super-utilizers: a methodological review of Super-Utilizer Criteria Applied to the Utah Medicaid Population, 2016–2017. Popul Health Manag. 2020;23(2):165–73. https://doi.org/10.1089/pop.2019.0076. Epub 2019 Aug 19. PMID: 31424319.
Borde D, Pinkey J, Leverance R. How we promoted sustainable Super-Utilizer Care through Teamwork and taking time to listen. NEJM Catalyst Published 2017 February 5. https://doi.org/10.1056/CAT.17.0534.
Slankamenac K, Zehnder M, Langner TO, Krähenmann K, Keller DI. Recurrent Emergency Department users: two categories with different risk profiles. J Clin Med. 2019;8(3):333. https://doi.org/10.3390/jcm8030333. Published 2019 Mar 9.
Hasselman D. Super-Utilizer Summit: Common Themes from Innovative Complex Care Management Programs Center for Health Care Strategies, Inc. Hamilton, NJ, 2013. Available at: http://www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf407990.
Althaus F, Paroz S, Hugli O, et al. Effectiveness of interventions targeting frequent users of emergency departments: a systematic review. Ann Emerg Med. 2011;58(1):41–52.
Camden Coalition of Healthcare Providers Staff. About the Camden Coalition. Camden Coalition of Providers. Available at: https://www.camdenhealth.org/about/about-the-coalition/history/. Accessed August 17, 2016.
Locker TE, Baston S, Mason SM, Nicholl J. Defining frequent use of an urban emergency department. Emerg Med J. 2007;24(6):398–401.
Bodenheimer T. Strategies to reduce costs and improve care for high-utilizing medicaid patients: reflections on pioneering programs policy brief. Center for Health Care Strategies, Inc.; 2013. Available at: http://www.chcs.org/media/HighUtilizerReport_102413_Final3.pdf.
Serfling RJ. Approximation theorems of mathematical statistics. Volume 162. New York, NY: John Wiley & Sons; 2009.
McWilliams A, Tapp H, Barker J, Dulin M, Med J. Jul- Aug. 2011;72(4):265–71. PMID: 22128684.
Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006;355(13):1300-3. https://doi.org/10.1056/NEJMp068194. PMID: 17005946.
Trunkey DD. A growing crisis in patient access to emergency care: a different interpretation and alternative solutions. Bull Am Coll Surg. 2006;91(11):12–22. PMID: 18557433.
Fernandes R, Fess EG, Sullivan S, Brack M, DeMarco T, Li D. Supportive care for superutilizers of a Managed Care Organization. J Palliat Med. 2020;23(11):1444–51. https://doi.org/10.1089/jpm.2019.0288. Epub 2020 May 26. PMID: 32456602; PMCID: PMC7583336.
Rinehart DJ, Oronce C, Durfee MJ, Ranby KW, Batal HA, Hanratty R, Vogel J, Johnson TL. Identifying subgroups of adult superutilizers in an Urban Safety-Net System using latent class analysis: implications for clinical practice. Med Care. 2018;56(1):e1–e9. https://doi.org/10.1097/MLR.0000000000000628. PMID: 27632768; PMCID: PMC5406260.
Acknowledgements
Not applicable.
Funding
Grant funding of $660,000 over 2 years from Florida Children’s Medical Services (CMS) through the $35 Million Low Income Pool Award (Medicaid Number 053386600).
Author information
Authors and Affiliations
Contributions
DB- study design, implementation, writing of the manuscript. DA- background, analysis, writing of the manuscript. RL- study design, implementation, writing of the manuscript. LP- data acquisition and analysis. JS- statistical analysis. KL- implementation and writing of the manuscript. JP- study design, implementation, writing of manuscript. JW- study design, implementation, writing of manuscript. LW- study design, implementation, writing of manuscript. BA- writing of manuscript. NSR- study design, implementation, writing of manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of University of Florida. Research involving human participants, human material, or human data, have been performed in accordance with the Declaration of Helsinki.
Informed consent
The Institutional Review Board, University of Florida approved a full waiver of informed consent to encourage enrollment of subjects to receive significant benefits in the form of primary care and low cost medications. Enrollment was fully voluntary, so the waiver did not affect the rights of our subjects.
Consent for publication
Not applicable.
Competing interests
None declared
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Borde, D., Agana-Norman, D., Leverence, R. et al. Outcomes of an integrated practice unit for vulnerable emergency department patients. BMC Health Serv Res 23, 1449 (2023). https://doi.org/10.1186/s12913-023-10067-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10067-9