Abstract
Objective
Healthcare for adolescents receives little attention in low-income countries globally despite their large population share in these settings, the importance of disease prevention at these ages for later life outcomes and adolescent health needs differing from those of other ages. We therefore examined healthcare need and use among adolescents in rural Burkina Faso to identify reasons for use and gaps in provision and uptake.
Methods
We interviewed 1,644 adolescents aged 12-20 living in rural northwestern Burkina Faso in 2017. Topics included healthcare need and satisfaction with care provided. We calculated response-weighted prevalence of perceived healthcare need and utilization, then conducted multivariable regression to look at predictors of need, realized access and successful utilization based on the Andersen and Aday model.
Results
43.7 [41.2 - 46.0] % of participants perceived need for healthcare at least once in the preceding 12 months - 52.0 [48.1 - 56.0] % of females and 35.6 [32.5 - 39.0] % of males. Of those with perceived need, 92.6 [90.0 - 94.3] % were able to access care and 79.0 [75.6 - 82.0] % obtained successful utilization. Need was most strongly predicted by gender, education and urbanicity, while predictors of successful use included household wealth and female guardian’s educational attainment.
Conclusion
Healthcare utilization among adolescents is low in rural Burkina Faso, but mostly thought of as sufficient with very few individuals reporting need that was not linked to care. Future objective assessment of healthcare need could help identify whether our results reflect a well-functioning system for these adolescents, or one where barriers lead to low awareness of needs or low expectations for service provision.
Similar content being viewed by others
Introduction
Adolescence is “a critical phase in life for achieving human potential” [1]; prevention of morbidity and mortality at this age is thus an important investment in the future [2, 3]. Ninety percent of the world’s 1.2 billion adolescents (aged 10 to 19) live in low- and middle-income countries (LMIC) [4,5,6]. Sub-Saharan Africa (SSA) has the highest proportion of adolescents of any region in the world, and it is the only region of the world in which the number of adolescents continues to rise significantly [4]. An even greater proportion (97 %) of deaths in young people aged 10 to 24 occur in LMIC, with over 60% of all deaths at these ages occurring in Sub-Saharan Africa and southeast Asia [6]. While mortality rates and disability adjusted life years lost have fallen for SSA children over the past 30 years, reductions for adolescents have been less pronounced [5, 7].
The most important causes of ill health in adolescence are very different from those at other life stages, but habits generated during this phase of life are key to determining later-life risk [8]. The burden of adolescent ill-health in Higher Income Countries Higher Income Countries (HIC) is relatively well understood, with injuries, mental health and substance use being the main causes of morbidity and mortality. The burden of adolescent health in LMIC has also been clearly quantified, and differs from that in HIC. Sexual and reproductive health SRH and communicable diseases (especially in SSA) are more important, however, as at other ages, LMIC adolescents are increasingly facing a multiple burden as conditions prevalent in HIC rise too [7, 9].
Healthcare utilization in LMIC at all ages differs from HIC, with significantly higher utilisation rates for outpatient visits and inpatient admissions in HIC [10]. Data on healthcare utilization amongst SSA adolescents is very limited but suggests low coverage of adolescent health concerns including mental health and nutrition [11]. What work has been done continues to be mainly on maternal and child care and sexually transmitted infections (STIs), especially HIV [12,13,14,15,16]. Similarly, key determinants of need for, and utilization of, healthcare are well-studied in HIC, with socioeconomic status, gender and literacy/school enrolment playing important roles, but much less is known for LMIC adolescents aside from their generally low levels of interaction with the healthcare system [17, 18, 9]. As a result, it is unclear whether low healthcare utilization among LMIC adolescents is a function of less actual need, low perceived need for care or barriers to access - including travel distance and time, and services unfriendly to adolescents. Notably, poverty as a key source of healthcare disparity has been noted both between and within SSA countries, but little has been done to unpack whether this disparity is due to differ economic obstacles, underestimated needs, or a failure of individuals or the health system to react to needs as they arise [19,20,21]. Any understanding of the healthcare needs of LMIC adolescents, and adaptation of programmes which have been successful in HIC, will therefore require adjustment to their greater and differing health requirements [22].
Burkina Faso is both one of the poorest countries in the world, with 44% of people living on less than $1.90 per day and one of the youngest, with a median age of 17 and 24% of citizens aged 10 to 19 [5, 23]. The few data on Burkinabe adolescent health are particularly sparse outside of the SRH topics. Fertility rates are high and median age of first birth is under 20 [14, 21]. Fortunately, the burden of HIV and other STIs is low in Burkina Faso [5]. However, knowledge about STIs is very low even compared to other SSA countries [15]. This could be due to the low burden on the one hand, but also ultimatively to insufficient sexual health education, especially in schools; these factors combine to increase risks for STIs [24]. There is thus likely to be substantial need for healthcare services among rural Burkinabe adolescents.
Healthcare provision in Burkina Faso is limited in terms of physician, hospital bed and Community Health Worker (CHW) numbers [25]. This reflects low health expenditures even by SSA standards with over two-thirds of healthcare payments are made privately, largely out-of-pocket [26]. Adult use of healthcare in rural Burkina Faso is limited by several barriers, including a lack of money, low literacy and high distance to care [27,28,29]. CHW appear to play an increasingly important role in healthcare provision in rural Burkina Faso, which may overcome some of these barriers [30, 31]. However, evidence on healthcare use by adolescents remains scant and important factors influencing adolescent health and healthcare utilization have not been examined [32].
We therefore analysed a recent population-based survey in Boucle du Mouhoun province in north-western Burkina Faso, a mostly rural region bordering Mali with about 1.9 million inhabitants, 23.7% of whom are young people between 10 and 19 years old [33]. In a country comparison it has a higher rate of illiteracy and less infrastructure [34]. In this analysis, we describe healthcare utilization by rural adolescents, to identify levels of their unmet need for care, and to ascertain predictors of and barriers to healthcare utilization in this population.
Methods
Setting and sample
We used data from a study conducted at the Centre de Recherche en Santé de Nouna (CRSN), a Health and Demographic Surveillance System (HDSS) site in Boucle du Mouhoun province, north-western BF [35]. This BF study was part of the Africa Research, Implementation Science and Education (ARISE) Network, a collaboration between nine sub-Saharan African institutions, the Harvard T.H. Chan School of Public Health, and the University of Heidelberg [36]. The CRSN HDSS includes 58 villages and the rural town of Nouna, with a total population of about 107.000 in 2015, of who approximately 22.000 were aged 12 to 19.
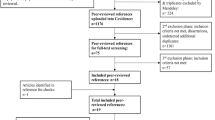
The study selected 10 villages purposively sampled to ensure variation in ethnicity, and one sector of Nouna. Within each selected village, a random sample of households was drawn from the most recent available CRSN census and all household members aged 12 to 19 years at the date of sampling were invited to participate (\(n=1795\)).
CRSN census and all 12 to 19 year old household members household members aged 12 to 19 years at the date of sampling were invited to participate (\(n = 1795\)).
In the selected Nouna sector, 749 ageeligible adolescents were sampled. The ratio of urban to rural individuals respected the ratio seen in the overall HDSS. All 2544 adolescents in the initial sample were sought for interview; 1644 completed a study interview.
Data was collected in November and December 2017 using tablet computers in private spaces around adolescents’ place of residence. Questions were either asked in French or translated into Dioula or Mooré, the most frequently spoken (but rarely written) local languages by fieldworkers. Fieldworker training included translation practice. Sampled individuals had to have been primarily resident in the Nouna HDSS for at least six months to be eligible to participate.
Measures
The study collected self-reported information on socio-demographics, behaviours, health practices and health outcomes using a questionnaire that was largely derived from the Global School-Based Student Health Survey with some additional questions [37]. We selected measures for this study based on the phase 2 Anderson and Aday model [38].
Outcome
Respondents were asked whether and how often, in the past 12 months, they had: 1) been admitted to hospital; 2) visited a primary care clinic; 3) visited a traditional healer; or 4) needed these services but been unable to use them. For each service type used they were asked to specify their satisfaction on a fivepoint Likert scale (very dissatisfied, dissatisfied, neutral, satisfied, very satisfied). Following Anderson and Aday, we first evaluated whether respondents needed care or not, and if so whether they were able to access care (realized access) and then were fully satisfied with their care (effective access). For service use we divided respondents into those with: (i) no need (no to all four questions); (ii) fully met need (yes to any service, no to unmet need); (iii) partially met need (yes to any service, yes to unmet need); and (iv) entirely unmet need (no to all services, yes to unmet need). For satisfaction, we divided respondents into those with: a) fully satisfied (only satisfied/very satisfied responses); b) not fully satisfied (any other response); c) no service use. We finally placed respondents into three categories: those with effective access (ii and a), those without effective access (ii and b, iii or iv) and those with no need for access (i).
Exposures
To be able to measure inequalities and influencing factors for effective access to healthcare we considered predisposing and enabling factors. Relatively immutable, predisposing variables we included were sex (male or female), age, (12 to 13, 14 to 15, 16 to 17 and 18 to 20), highest attained education (none, primary only, post-primary or higher, Muslim school without grade structure), religion (Animist, Catholic, Muslim, Protestant) and ethnicity (Bwaba, Dafin, Mossi, Peulh, Samo, other). We also included enabling factors that may be amenable to activation and therefore important starting points for interventions. These included household asset index, ranked into quintiles within the HDSS, maternal education (none, any) and urbanicity (small town of Nouna, any village) [39].
Analytic approach
We first described outcome and exposure variables using proportions, testing for differences in each exposure variable by sex in unweighted data, and by level of healthcare need using inverse non-response weights accounting for different participation rates by age, religion, ethnicity and urbanicity. We then created contingency tables and ran chisquared tests of association for survey data using R version 4.3.0 [40]. We then conducted bivariate and multivariable logistic regression to identify factors associated with first need for healthcare among all respondents, and second effective access to healthcare among those reporting any need. Confidence intervals are between 2.5- 97.5 %. For each set of models we first included only predisposing factors, then added enabling ones.
Results
Characteristics of respondents
We were able to locate 1644 of 2544 sampled individuals (64.6 %). Ten participants were dropped because of inconsistent answers regarding need and healthcare utilization. Of the remaining 1634 respondents, 58% were male. Half of participants were attending school at the time of interview but two thirds (66.4 %) of respondents’ highest school level was none or primary. Only 12.5% of the female guardians reported any kind of school education. Most participants were Muslims (69.2 %), 27.6% either Catholics or Protestants (Table 1). Females were less likely not to be in school (45.3% vs 53.5 %) and had higher grade attainment, but most other factors were balanced by sex.
Main outcomes
Using weighted percentages, less than half of participants (43.7% [Confidence Intervall [CI] 41.2 - 46.0 %]) stated that they had a need for healthcare within the past 12 months (Table 2). This value was consistent with age for males and females up to age 15, but then rose rapidly to 72% for 18-20 year-old women (Fig. 1). While only 39.7% of participants in the lowest quintile stated need, amongst the wealthiest it was 52.1% (\(p = 0.009\)).
Perceived need varied by both predisposing and enabling factors. With lowest levels amongst males in poorer households (32.0 %/25.5% in 5th/4th quintile, \(p = 0.007\)), not in school (29.1 %, \(p<\) 0.001), or with no school attainment (26.9 %, \(p<\)0.001). So school education of the participants has an impact but it gets smaller in the multivariate regression indicating that there are correlations between age, school education, urbanicity and wealth (Table 3). Muslims reported a lower need than participants with other religious affiliations (41 %, \(p = 0.01\)). There was more demand in Nouna town (52.4 %) than in the villages (40.0 %) (\(p<\)0.001).
One-third of respondents (37.3 %) reported that they had always been able to use a healthcare provider - over 85% of all those reporting any need. Primary care centers were used most frequently as health care providers by the adolescents (33.5% [CI 31.2 - 36.0 %]), to a lesser extent traditional healers (9.3% [CI 7.9 - 11.0 %]) and the Nouna hospital (7.4% [CI 6.1 - 9.0 %]. Only a small minority of respondents reported partially (3.2 %) or entirely (3.3 %) unmet need for healthcare. The proportion of participants with entirely unmet need was similar amongst the participant characteristics, although the figure was lower for those from richer households and rural areas (Table 2).
Almost four in five participants (79 %) reported effective access to healthcare. In contrast to the stated need, where predisposing factors played an important role, enabling factors particularly influenced effective / successful access to healthcare, except that Bwaba (Odds ratio [OR] 0.23 [ CI 0.08 - 0.71]) and other minority ethnic groups (OR 0.16 [CI 0.04 - 0.66]) had poorer access than members of other ethnic groups. With increasing prosperity, the healthcare of the participants was better (Fig. 2), with the highest quintile having 2.97 times the odds (CI 1.51-5.95) of receiving efficient access compared to the lowest quintile. The participants whose mother had no school education also received worse care (OR 0.43 [CI 0.20-0.84]) (Table 4). Accounting for those with no need and those without access to care overall 59.5% of all participants never had any kind of contact with the healthcare system mostly because they had no perceived need (56.3 %). Thus, of those in need, 92.6% [CI 90.0 - 94.3 %] had access to the healthcare system.
Discussion
Evidence of the perceived need for, and use of, healthcare by adolescents in LMICs in general, and sub-Saharan Africa in particular, is sparse. This is despite their demands on the health system being substantial and different from those of other age groups. It is important to understand not only what adolescent health needs there are and what other factors are important to properly understand their behaviour [38, 41]. We also need to know whether healthcare systems and policy makers are prepared to meet adolescent health demands in order to be able to take the right approaches [42]. The success of these implementations seems to be achievable only when considering all intervention types [43]. We therefore analysed self-reported data on healthcare system need and use by young people in rural north-western Burkina Faso, a region particularly affected by poverty in a country that is already one of the poorest in the world and therefore represents an extreme in a global comparison. More than 40% of participants stating a perceived need for healthcare in the past year, with notably more need among older female adolescents. Still, healthcare need was considerably lower than that seen in HICs [44, 45].
Perceived need was most strongly associated with predisposing demographic factors such as age, gender, education and religion - although it was also higher in urban areas (Table 5). These findings highlight that inequity in perceived healthcare need arises when it is influenced not only by demographic factors and symptom severity, but also by, e.g., the ability to recognize these symptoms and to have the necessary knowledge about the health system and the possibilities of use [46]. This pattern of mainly predisposing factors predicting perceived need independently of enabling factors is similar to that seen in studies of Canadian and US adolescents [41, 47].
Research on healthcare need and use in LMIC often focuses either on level of access or level of demand and the health system’s capacity to meet this demand. In most studies (including ours) it is the same factors that cause inequality in the health system [48]. In contrast to other studies however we did not only limit ourselves to one of these aspects or subgroup, but took into account age, gender, socio-economic background, education and residence, but also religion, ethnicity and maternal education. Our study shows that perceived need is influenced by age and gender, but also residence, ethnicity, religion and wealth suggesting that it matters where you live and from which ethnic or religious background you come from implying that information on health care and needs are still not evenly supplied to everyone.
Among those Burkinabe adolescents perceiving need, over 90% had access to the health system when needed. More than three quarters of those with need had effective access (always available with a high level of satisfaction). These numbers are high and in contrast to the findings of other studies in Sub-Saharan Africa, which find poor accessibility and lower levels of satisfaction [49, 50]. This difference may well reflect healthcare being sufficient for this age group in this setting. However it may also reflect an underestimation of personal needs, or that the level of care required for satisfaction is particularly low. Since this study did not attempt to capture objective healthcare need, we are not able to directly assess which scenario is more likely. In a four-country study of STIs among male adolescents, Burkinabé reported higher healthcare system utilization and greater trust and satisfaction, but also less knowledge of STIs shows a higher level of utilization and greater trust and satisfaction, but also less knowledge of STIs in Burkina Faso than in Ghana, Malawi and Uganda [42]. Were this pattern also true in our study, it might be the case that adolescents are both able to access good care and may not identify certain needs. Additional research - both quantitatively including objective measures of need and qualitatively through indepth discussion of need and use - would help answer these questions.
Predictors of effective HC use were mainly enabling factors, in line with other studies in both LMIC and HIC [48, 51, 52]. While our data suggest high levels of effective access, it was notable that respondents from lower income houses and rural areas had both lower stated need and a higher unmet need amongst those with need. Our findings are therefore in line with other studies showing the poor do not only understate their needs, they or the healthcare system-on average-also respond inadequately to their needs [21]. This reinforces the importance of considering both barriers to care access and to identifying need. It‘s already been shown that knowledge about adequate care seems to be little, care is available, but quality is poor [51]. Use of preventative services, which are particularly important in this age group, were especially low in other studies. The large influence of urbanicity on healthcare use in Burkina Faso is described before while wealth playing the most important factor in all other countries, suggesting ability to reach care may be the primary factor [20]. Our finding that successful access was most strongly associated with wealth and education in our setting suggests that the distribution of healthcare still favours those who can afford it. Interventions that improve access to the poorest, even in generally poor communities, may generate the greatest benefits while also reducing inequality.
Strengths and limitations
This analysis has several limitations. First, the underlying dataset was cross-sectional, limiting ability to determine the temporal directions of any associations seen, conflating participants’ age and cohort and making evaluation of intra-individual development impossible. Future work following up this cohort could allow such issues to be examined. Second, the study was limited to one geographic area in rural Burkina Faso. While the study sampled from a local population census and non-response weights were used to minimize selection bias, generalization to the national level or beyond should only be done with caution. However, to the best of our knowledge this is a novel study in its examination of the usage patterns of health services for adolescents in Burkina Faso and more widely across low-income settings and is thus an important initial contribution to the literature. Third, needs and utilization were based on self-report, not objectively measured, e.g., by physical examination or medical history. While self-reports capture perceived need, objective measurement would help evaluate if actual needs were over or underreported, either overall or differentially by key covariates. Fourth, the distance to the nearest primary care center or hospital was not included in the analysis, since distance and difficulty of travel between villages differs by precise route and season. As a result it is possible that some of our findings might reflect confounding by difficulty of reaching care. Although unmet need in this population is very low. Finally, the study did not enquire as to why participants needed healthcare, were unable to access it, and were/were not satisfied. Such insight would be a valuable next step in designing interventions.
Conclusion
In our analysis of healthcare need and utilization by adolescents in rural Burkina Faso, we find relatively low overall contact rates, but very high levels of successful utilization by those self-identifying need. Perceived need was strongly patterned by age, gender, school education and urbanicity, while effective access to care was linked to household wealth and maternal education. Over half of participants did not have contact with the healthcare system in the past twelve months, considerably more than in HIC, where prevention amongst adolescents is increasingly emphasized. Our results support the findings that low education, low household wealth and rurality decrease healthcare access. Further research can extend our work by assessing objective healthcare need and better understanding the context of healthcare need and use, possibly also through other approaches such as in-depth interviews or ethnographic approaches. Such work would help determine the extent to which our results reflect a well-functioning system for these young people, or one where barriers lead to low awareness of needs or low expectations for service provision.
Availability of data and materials
Data are not publicly available due to consent not being given by participants for data to be shared openly, and due to the risk of deductive disclosure with sufficient local information given the inclusion of large proportions of age cohorts in the study villages. Anonymised data are available from ARISE study data controllers only following signature of a data use agreement restricting onward transmission. Anyone wishing to replicate the analyses presented, or conduct further collaborative analyses using ARISE (which are welcomed and considered based on a letter of intent), should contact Dr Guy Harling (g.harling@ucl.ac.uk) in the first instance.
Abbreviations
- ARISE:
-
Africa Research, Implementation Science and Education
- BF:
-
Burkina Faso
- CHW:
-
Community Health Worker
- CRSN:
-
Centre de Recherche en Santé de Nouna
- HDSS:
-
Health and Demographic Surveillance System
- HIC:
-
Higher Income Countries
- LMIC:
-
Lower and Middle Income Countries
- SRH:
-
Sexual and Reproductive Health
- SSA:
-
Sub-Saharan Africa
References
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78.
Sheehan P, Sweeny K, Rasmussen B, Wils A, Friedman HS, Mahon J, et al. Building the foundations for sustainable development: a case for global investment in the capabilities of adolescents. Lancet. 2017;390(10104):1792–806.
Bank W. World development report 2007: Development and the next generation. The World Bank; 2006.
Cappa C, Wardlaw T, Langevin-Falcon C, Diers J. Progress for children: a report card on adolescents. Lancet. 2012;379(9834):2323–5.
United Nations Children’s Fund Staff U United Nations. Progress for Children: a Report Card on Adolescents. New York: United Nations Publications; 2012. http://www.unicef.org/publications/files/Progress_for_Children_-_No._10_EN_04272012.pdf.
Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009;374(9693):881–92.
Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377(9783):2093–102.
Lancet The. Putting adolescents at the Centre of health and development. Lancet. 2012;379(9826):1561. https://doi.org/10.1016/S0140-6736(12)60536-4.
Patton GC, Coffey C, Cappa C, Currie D, Riley L, Gore F, et al. Health of the world’s adolescents: a synthesis of internationally comparable data. Lancet. 2012;379(9826):1665–75.
Moses MW, Pedroza P, Baral R, Bloom S, Brown J, Chapin A, et al. Funding and services needed to achieve universal health coverage: applications of global, regional, and national estimates of utilisation of outpatient visits and inpatient admissions from 1990 to 2016, and unit costs from 1995 to 2016. Lancet Public Health. 2019;4(1):e49–73.
Doyle AM, Mchunu L, Koole O, Mthembu S, Dlamini S, Ngwenya N, et al. Primary healthcare and school health service utilisation by adolescents and young adults in KwaZulu-Natal. South Africa BMC Health Serv Res. 2019;19(1):1–11.
Mank I, Vandormael A, Traoré I, Ouédraogo WA, Sauerborn R, Danquah I. Dietary habits associated with growth development of children aged\(<\) 5 years in the Nouna Health and Demographic Surveillance System. Burkina Faso Nutr J. 2020;19(1):1–14.
Østergaard LR, Bjertrup PJ, Samuelsen H. “Children get sick all the time”: a qualitative study of socio-cultural and health system factors contributing to recurrent child illnesses in rural Burkina Faso. BMC Public Health. 2016;16(1):1–9.
Sauerborn R, Nougtara A, Sorgho G, Bidiga J, Tiebelesse L, Diesfeld H. Assessment of MCH services in the district of Solenzo, Burkina Faso. II Acceptability J Trop Pediatr. 1989;35:10–3.
Biddlecom AE, Munthali A, Singh S, Woog V. Adolescents’ views of and preferences for sexual and reproductive health services in Burkina Faso, Ghana, Malawi and Uganda. Afr J Reprod Health. 2007;11(3):99.
Kassebaum N, Kyu HH, Zoeckler L, Olsen HE, Thomas K, Pinho C, et al. Child and adolescent health from 1990 to 2015: findings from the global burden of diseases, injuries, and risk factors 2015 study. JAMA Pediatr. 2017;171(6):573–92.
Goodman E, Huang B, Schafer-Kalkhoff T, Adler NE. Perceived socioeconomic status: a new type of identity that influences adolescents’ self-rated health. J Adolesc Health. 2007;41(5):479–87.
Newacheck PW, Hung YY, Jane Park M, Brindis CD, Irwin CE Jr. Disparities in adolescent health and health care: does socioeconomic status matter? Health Serv Res. 2003;38(5):1235–52.
Gwatkin DR, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socio-economic differences in health, nutrition, and population within developing countries: an overview. Washington: Worldbank (20093081364); 2007. p. 287.
Bonfrer I, Van de Poel E, Grimm M, Van Doorslaer E. Does the distribution of healthcare utilization match needs in Africa? Health Pol Plan. 2014;29(7):921–37.
Bago d’Uva T, Lindeboom M, O’Donnell O, Van Doorslaer E. Education-related inequity in healthcare with heterogeneous reporting of health. J R Stat Soc Ser A Stat Soc. 2011;174(3):639–64.
Dick B, Ferguson BJ. Health for the world’s adolescents: a second chance in the second decade. J Adolesc Health. 2015;56(1):3–6.
UNDP. 2018 Statistical Update: Human Development Indices and Indicators. 2018. http://hdr.undp.org/en/content/human-development-indices-indicators-2018-statistical-update. Accessed 23 June 2019.
Bankole A, Biddlecom A, Guiella G, Singh S, Zulu E. Sexual behavior, knowledge and information sources of very young adolescents in four sub-Saharan African countries. Afr J Reprod Health. 2007;11(3):28.
WHO. Number of community health workers. 2020. https://apps.who.int/gho/data/node.main.HWFGRP_0180?lang=en. Accessed 01 July 2019.
WHO. BURKINA FASO Factsheet of Health Statistics 2018. 2019. http://www.aho.afro.who.int/profiles_information/index.php/Burkina_Faso:Index. Accessed 22 May 2022.
Sarrassat S, Meda N, Badolo H, Ouedraogo M, Somé H, Cousens S. Distance to care, care seeking and child mortality in rural Burkina Faso: findings from a population-based cross-sectional survey. Trop Med Int Health. 2019;24(1):31–42.
Mugisha F, Bocar K, Dong H, Chepng’eno G, Sauerborn R. The two faces of enhancing utilization of health-care services: determinants of patient initiation and retention in rural Burkina Faso. Bull World Health Organ. 2004;82:572–9.
Dong H, Kouyate B, Cairns J, Mugisha F, Sauerborn R. Willingness-to-pay for community-based insurance in Burkina Faso. Health Econ. 2003;12(10):849–62.
Brieger B. Community-based health workers in Burkina Faso: are they ready to take on a larger role to prevent malaria in pregnancy? 2018. http://malariamatters.org/community-based-health-workers-in-burkina-faso-are-they-ready-to-take-on-a-larger-role-to-prevent-malaria-in-pregnancy/. Accessed 26 Mar 2021.
Sauerborn R, Nougtara A, Diesfeld HJ. Low utilization of community health workers: results from a household interview survey in Burkina Faso. Soc Sci Med. 1989;29(10):1163–74.
Blum RW, Bastos FI, Kabiru CW, Le LC. Adolescent health in the 21st century. Lancet. 2012;379(9826):1567–8. https://doi.org/10.1016/S0140-6736(12)60407-3.
Institut national de la statistique et de la démographie (INSD). Résultats cinquieme recensement general de la population et de l’habitation monographie de la region de la boucle du mouhoun. 2022. https://burkinafaso.opendataforafrica.org/bbiuprb/indicateurs-du-5e-rgph-2019. Accessed 27 Aug 2023.
Institut national de la statistique et de la démographie (INSD). Resultats Volume 2: Caracteristiques des menages et de la Population. 2022. https://www.insd.bf/fr/resultats. Accessed 27 Aug 2023.
Sie A, Louis V, Gbangou A, Müller O, Niamba L, Stieglbauer G, et al. The health and demographic surveillance system (HDSS) in Nouna, Burkina Faso, 1993–2007. Glob Health Action. 2010;3(1):5284.
Darling AM, Sunguya B, Ismail A, Manu A, Canavan C, Assefa N, et al. Gender differences in nutritional status, diet and physical activity among adolescents in eight countries in sub-Saharan Africa. Trop Med Int Health. 2020;25(1):33–43.
WHO Team Surveillance, Monitoring and Reporting. Global School-based Student Health Survey (GSHS) 2013 Core-Expanded Questions. https://www.who.int/publications/m/item/gshs-core-expanded-questionnaire-modules-(2013-2017). Accessed 07 Oct 2023.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. https://doi.org/10.2307/2137284.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data-or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32.
R Core Team. R: a language and environment for statistical computing. Vienna; 2023. https://www.R-project.org/. Accessed 27 May 2023.
Vingilis E, Wade T, Seeley J. Predictors of adolescent health care utilization. J Adolesc. 2007;30(5):773–800.
Biddlecom AE, Munthali A, Singh S, Woog V. Adolescents’ views of and preferences for sexual and reproductive health services in Burkina Faso, Ghana, Malawi and Uganda. Afr J Reprod Health. 2007;11(3):99.
Denno DM, Hoopes AJ, Chandra-Mouli V. Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support. J Adolesc Health. 2015;56(1):S22–41.
Seeling S, Prütz F, Gutsche J. Utilization of paediatric and general medical services by children and adolescents in Germany. Results of the cross-sectional KiGGS Wave 2 study and trends. J Health Monit. 2018;3(4):52–61. https://doi.org/10.17886/RKI-GBE-2018-099.
Zimmer-Gembeck MJ, Alexander T, Nystrom RJ. Adolescents report their need for and use of health care services. J Adolesc Health. 1997;21(6):388–99.
Andersen RM, Davidson PL, Baumeister SE, et al. Improving access to care. Changing the US health care system: key issues in health services policy and management San Francisco: Jossey-Bass. 2014;36(3):33–69.
Marcell AV, Ford CA, Pleck JH, Sonenstein FL. Masculine beliefs, parental communication, and male adolescents’ health care use. Pediatrics. 2007;119(4):e966-75.
Geleto A, Chojenta C, Musa A, Loxton D. Barriers to access and utilization of emergency obstetric care at health facilities in sub-Saharan Africa: a systematic review of literature. Syst Rev. 2018;7(1):1–14.
Yaya S, Bishwajit G, Ekholuenetale M, Shah V, Kadio B, Udenigwe O. Urban-rural difference in satisfaction with primary healthcare services in Ghana. BMC Health Serv Res. 2017;17(1):1–9.
Deaton AS, Tortora R. People in sub-Saharan Africa rate their health and health care among the lowest in the world. Health Aff. 2015;34(3):519–27.
Abekah-Nkrumah G. Trends in utilisation and inequality in the use of reproductive health services in Sub-Saharan Africa. BMC Public Health. 2019;19(1):1–15.
Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–52. https://doi.org/10.1016/S0140-6736(12)60149-4.
Acknowledgements
We acknowledge the contribution of the data collectors and supervisors in enabling the analysis of these data.
Funding
Funding for the Nouna ARISE study was provided by the Alexander von Humboldt Foundation through an Alexander von Humboldt University Professor award to Till Baernighausen, which is funded by the German Federal Ministry of Education and Research. Funding for the ARISE Adolescent Health Study was provided by the Department of Global Health and Population at Harvard T.H. Chan School of Public Health. Guy Harling was supported by a fellowship from the Wellcome Trust and Royal Society (210479/Z/18/Z). This research was funded in whole, or in part, by the Wellcome Trust [Grant number 210479/Z/18/Z]. For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
T. Baernighausen, AS and G. Harling conceived and designed the overall CRSN study. MB and LO oversaw data collection and quality assurance activities. Joshua Krohn conducted the data analysis and interpretation and wrote the first draft of the manuscript, with supervision from G. Harling and T. Baernighausen. Joshua Krohn created the tables and figures. All authors substantively reviewed manuscripts, inputted into revisions, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study obtained ethical approval from the “Centre de Recherche en Santé de Nouna” (CRSN, reference number: 2017-08)’s Institutional Ethics Committee. For the current study the ethics approval was exempted from review by the Heidelberg Medical Faculty’s Ethics Commission as all data received in Germany was anonymized. All procedures were conducted in accordance with relevant guidelines and regulations, including the Declaration of Helsinki. Oral assent was sought from village elders prior to study start. Participants aged over 18 provided written informed consent; those under 18 provided written assent alongside parent/guardian consent. Any illiterate participants were assisted by a witness of their choosing who signed on their behalf after the witness had had the opportunity to read the information materials and the study information was explained to the potential participant orally.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Krohn, J., Bountogo, M., Ouermi, L. et al. Challenges and achievements in the utilization of the health system among adolescents in a region of Burkina Faso particularly affected by poverty. BMC Health Serv Res 23, 1080 (2023). https://doi.org/10.1186/s12913-023-10052-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10052-2