Abstract
Background
Lungsco01 is the first study assessing the real benefits and the medico-economic impact of video-thoracoscopy versus open thoracotomy for non-small cell lung cancer in the French context.
Methods
Two hundred and fifty nine adult patients from 10 French centres were randomised in this prospective multicentre randomised controlled trial, between July 29, 2016, and November 24, 2020. Survival from surgical intervention to day 30 and later was compared with the log-rank test. Total quality-adjusted-life-years (QALYs) were calculated using the EQ-5D-3L®. For medico-economic analyses at 30 days and at 3 months after surgery, resources consumed were valorised (€ 2018) from a hospital perspective. First, since mortality was infrequent and not different between the two arms, cost-minimisation analyses were performed considering only the cost differential. Second, based on complete cases on QALYs, cost-utility analyses were performed taking into account cost and QALY differential. Acceptability curves and the 95% confidence intervals for the incremental ratios were then obtained using the non-parametric bootstrap method (10,000 replications). Sensitivity analyses were performed using multiple imputations with the chained equation method.
Results
The average cumulative costs of thoracotomy were lower than those of video-thoracoscopy at 30 days (€9,730 (SD = 3,597) vs. €11,290 (SD = 4,729)) and at 3 months (€9,863 (SD = 3,508) vs. €11,912 (SD = 5,159)). In the cost-utility analyses, the incremental cost-utility ratio was €19,162 per additional QALY gained at 30 days (€36,733 at 3 months). The acceptability curve revealed a 64% probability of efficiency at 30 days for video-thoracoscopy, at a widely-accepted willingness-to-pay threshold of €25,000 (34% at 3 months). Ratios increased after multiple imputations, implying a higher cost for video-thoracoscopy for an additional QALY gain (ratios: €26,015 at 30 days, €42,779 at 3 months).
Conclusions
Given our results, the economic efficiency of video-thoracoscopy at 30 days remains fragile at a willingness-to-pay threshold of €25,000/QALY. The economic efficiency is not established beyond that time horizon. The acceptability curves given will allow decision-makers to judge the probability of efficiency of this technology at other willingness-to-pay thresholds.
Trial registration
NCT02502318.
Similar content being viewed by others
Background
Lung cancer (LC) remains a major health problem with an estimated 130,180 deaths in 2022 in the US, which makes it the leading cause of cancer death in both sexes [1]. For early-stage LC, surgery remains the cornerstone of management and results in better overall survival [2]. Lobectomy with mediastinal lymph node dissection is therefore recommended in order to limit the risk of local recurrence [3]. However, lobectomy is associated with a high proportion of postoperative complications, especially respiratory complications, ranging from 12% in the analysis of the American Society of Thoracic Surgeons database, around 15% in the French National Epithor database, to 30% in a recent study using the SEER database [4,5,6]. Moreover, as reported by Stéphan et al., postoperative respiratory complications are associated with increases in mortality and length of stay in the intensive care or surgical ward, which has an effect on health system spending [7].
During the last decade, the use of video-assisted thoracoscopic surgery (VATS) lobectomy for LC has grown considerably. In France, the use of VATS jumped from 12% of lobectomies in 2012 to 48% in 2017 [8].
Recommendations from the American College of Chest Physicians in 2013 and the European Society of Medical oncology in 2014 suggest that VATS lobectomy be performed depending on the experience of the surgeon and for tumors of any stage [2, 3]. These recommendations are based on meta-analyses from the last decade, which indicated that VATS resulted in shorter hospital stays and fewer postoperative complications such as atelectasis or pneumonia [9,10,11,12,13,14]. However, the data used to formulate these recommendations were of poor quality. There are few randomized controlled trials (RCTs) in the literature evaluating the benefits of VATS compared to open thoracotomy for LC. In fact, only Bendixen et al., in a trial involving 206 patients, found that there was a benefit regarding postoperative pain and quality of life during the first year of follow-up in favor of VATS versus open thoracotomy [15].
To date, only four RCTs comparing complications and overall survival following VATS lobectomy or open thoracotomy for the treatment of lung cancer have been published in English [16,17,18,19]. The authors did not find VATS to be more beneficial than open thoracotomy except for intraoperative blood loss and median time of surgery. There were no benefits in terms of postoperative complications, mortality or length of hospital stay.
More recently, Bendixen et al. reported the results of the cost-utility analysis of VATS lobectomy performing a RCT including 103 patients in each group. They highlighted that VATS lobectomy was a cost-effective alternative to open thoracotomy for stage I LC [20].
The medico-economic literature on this subject is poor, which is why a medico-economic study is now needed to determine whether the costs induced by VATS are offset by the reduction in postoperative complications. This paper presents the results of a large RCT assessing the medico-economic impact of VATS lobectomy when compared with open thoracotomy in the French context.
The primary aim of this study was to evaluate the cost-effectiveness and the cost-utility impacts of VATS lobectomy when compared with open thoracotomy for the management of non-small cell lung cancer (NSCLC). These medico-economic analyses were performed at 30 days after surgery. The secondary aim was to evaluate the cost-effectiveness and cost-utility impacts at 3 months after surgery.
Material and methods
Lungsco01 is an open two-arm parallel RCT comparing lobectomy or segmentectomy performed by VATS with lobectomy or segmentectomy using thoracotomy for the treatment of LC. As specified in the published study protocol, the study involved French thoracic surgery departments that had already performed more than 50 VATS lobectomies [21]. The number of patients in each of the treatment groups was calculated and planned to be equal (300 patients in each arm), with a ratio of 1:1 and a stratification by centre since the different practices of each team may have an impact on the judgement criterion [21]. The list of randomised patients was divided into blocks of 12 to obtain balanced groups. Randomisation was available after patients had met the inclusion criteria [21].
Study population
The study population included patients with proven or suspected NSCLC which could be treated by lobectomy or segmentectomy performed by VATS or lobectomy or segmentectomy using thoracotomy. Inclusion criteria and exclusion criteria were described in the published protocol [21].
Procedures
There were two potential approaches for lobectomy or segmentectomy using video-thoracoscopy (VATS) and two potential types of thoracotomy: posterolateral thoracotomy with muscle sparing or lateral thoracotomy [18, 21]. At the start of the study, each surgical team chose one of the two approaches according to their experience. The chosen approach was the one to be used throughout the trial.
Post-operative care
Postoperatively, whether after VATS or thoracotomy, analgesia (morphine) was delivered via the epidural catheter or paravertebral catheter or intravenously. All patients had respiratory and motor physiotherapy immediately after the surgery at least twice a day during the hospital stay. All patients had a nasal cannula. Saline aerosols were prescribed if the patient had difficulty expectorating. Thrombophlebitis was prevented by stockings and anticoagulants (managed according to the usual practice of each centre) [21].
Outcomes
As part of the cost-effectiveness analyses initially planned, incremental cost-effectiveness ratios (ICER) were to be calculated taking into account the cost differential and the survival differential between the two groups. The ratios would have been expressed as the additional cost per life-year gained using the innovative technique (VATS) compared with the reference technique (thoracotomy), at 30 days and at 3 months after surgery. However, since death was infrequent and not different at these time horizons, only the cost differential was considered. This led us to perform cost-minimisation analyses [22], which corresponds to a sub-category of cost-effectiveness analyses.
As part of the cost-utility analyses, incremental cost-utility ratios (ICER) were estimated by relating the cost differential to the average differential in quality adjusted life years (QALYs) between the two strategies, at 30 days and at 3 months. The ICER represent the additional cost necessary to gain one additional QALY using the innovative technique (VATS) compared with the reference technique (thoracotomy).
Data collection
All the clinical data, resources consumed and responses to the EQ-5D-3L® questionnaire were collected prospectively via an electronic Case Report Form (e-CRF).
Cost estimations
The costs of VATS and thoracotomy were estimated for each patient for the 30 first days and the 3 first months after surgery. Costs were estimated from the hospital perspective given the available data on resources consumed (hospital stays). They included: (i) the production costs of the initial stays (including surgery); (ii) the production costs of all re-hospitalisations related to post-surgical complications; and (iii) the production costs of all admissions to rehabilitation care.
In the first step, diagnosis-related groups (DRGs) corresponding to all patient stays were identified in accordance with the rules for the classification of stays in France. Thus, the DRG for each initial stay and each re-hospitalisation for complications were assigned according to comorbidities, the reason for admission, the complications arising during the stay (and possible re-intervention), and length of stay (LOS). DRGs for stays in rehabilitation care were assigned using patient comorbidities, the reason for admission, the patient’s age, and time between the date of surgery and admission to rehabilitation care.
In the second step, a production cost was applied to each stay from the Etude Nationale des Coûts à méthodologie Commune (ENCC), a national survey of production costs per DRG estimated from a sample of representative hospitals in France. These production costs are broken down by expenditure item and type of service attended, and published annually by the French Agency for Information on Hospital Care (ATIH) [23, 24]. The last year available in the ENCC at the time of analyses was 2018, which determined our reference year for costing.
Especially for initial stays (including surgery), using the ‘adjusted-DRG’ method made it possible to replace the cost of the operating room issued from the ENCC with the actual real production costs of surgery estimated by micro-costing [25]. These real costs (VATS: €3,870.49; Thoracotomy: €2,455.58) were estimated in a previous publication from a sample of fifty patients from the Lungsco01 trial, from July 2015 to July 2016 [26]. For the needs of the paper, the costs have been updated to 2018 euros using the annual harmonized Consumer Price Index (CPI—base 100 in 2015) from the European Classification of Individual Consumption by Purpose (ECOICOP nomenclature – Health division—06.3.0.1.1 Hospital services—France) [27]. Finally, since the ENCC database contains the national LOS per DRG, an average daily cost was calculated in order to reconstitute a cost for the rest of the stay weighted by the LOS for each patient [28]. No discounting has been undertaken on costs in the absence of a time horizon greater than 12 months.
Utility measure
QALYs were evaluated using collected responses to the EQ-5D-3L® generic questionnaire completed pre-operatively, 3 days after surgery, during the day-30 visit and during the 3-month visit after surgery [29]. For each patient, final QALYs at 30 days and at 3 months were calculated by taking into account the periods between two administration times, as recommended [30]. No discounting has been undertaken in the absence of a time horizon greater than 12 months.
Statistical analyses
Analyses were performed on an intention-to-treat basis. Qualitative variables were compared using the χ2 test (or Fisher’s test if the expected values were < 5). Continuous variables were compared using Student’s t-test, which was also used for cost comparisons since non-parametric statistical tests are not recommended [31]. We used the difference in risk of death and logistic regression model to compare deaths at 30 days and 90 days, allowing estimation of odds ratios with their 95% confidence intervals.
The cost-utility analyses at 30 days and at 3 months were performed on cases with complete QALYs (no missing data). Then, a non-parametric bootstrap method (10,000 replications) was used in order to study the uncertainty associated with the sample and to construct a 95% confidence interval (95% CI) for the ICERs. This was followed by the construction of a Cost-Utility plane (CU-plane) and an acceptability curve from the bootstrap and the 95% CI of the ICERs. This curve is used to represent the probability that the VATS strategy is efficient when compared to the thoracotomy strategy (y-axis) as a function of different possible values of society’s Willingness-To-Pay (WTP) for an additional health unit (x-axis). A sensitivity analysis was performed using multiple imputation by chained equation method in order to take into account patients with missing data [31]. As done previously, this was followed by bootstrap analyses (10,000 replications) to construct the 95% CI for the ICERs. For the multiple imputation procedure, the following variables were used in the imputed datasets in order to improve the accuracy of imputed data: age; gender; performance status; smoking status (smoker/ex-smoker/non-smoker); body mass index; responses to the 5 items of the EQ-5D-3L® preoperatively, 3 days, 30 days and 3 months after surgery; and all hospital cost variables (cost of initial stay, re-hospitalisations and admissions in rehabilitation). The number of imputations was 10. The characteristics of patients with and without missing data were compared (results not shown). The stability between results of the complete cases and imputed data analysis were described.
The version 9.4 SAS was used for the analyses. The threshold for significance was set at 0.05.
Results
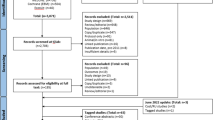
Two hundred and sixty-two patients were assessed for eligibility and signed consent to participate in the study from July 29, 2016 to November 24, 2020. One hundred and thirty-one patients were randomised to the VATS group, 128 to the thoracotomy group, and 3 were not randomized (Fig. 1). Ten centres participated in the study.
Flowchart. This flowchart describes the enrolment of patients in this study, their allocation in the VATS or thoracotomy group, and finally the selection of patients for complete cases analyses. Particularly for the cost-utility analyses, complete cases for Quality-Adjusted Life-Years (QALY) were considered
βVideo-Assisted Thoracoscopic Surgery. µEuroQol-5 Dimensions-3 Levels questionnaire
Patient characteristics
There was no significant difference in the baseline clinical characteristics between the two groups (Table 1). Intervention, post-operative respiratory complications and other major complications, re-hospitalisations, and QALYs assessed at each administration time are described (Table 2). The only significant differences between the two groups were the mean duration of the procedure (4.36 h for VATS vs. 3.73 for thoracotomy; p-value < 0.001), and the percentage of patients re-hospitalized between the 30-day and the 3-month visits (8.39% vs. 2.34%; p-value = 0.05). There was no significant difference in overall survival between the two groups at 30 days after the surgery (99.25% [95% CI: 94.82 – 99.89] for VATS vs. 99.22% [95% CI: 94.58 – 99.89] for thoracotomy), or at 3 months after the surgery (81.21% [95% CI: 45.15 – 94.70] for VATS vs. 79.37% [95% CI: 41.27 – 94.15] for thoracotomy). There was no significant difference in the risk of death between the two groups. The difference in risk of death at 30 days was -0.035 after thoracotomy compared to after VATS (95% CI: -0.09 to 0.02; p-value = 0.2155). The difference in risk of death at 3 months was -0.004 after thoracotomy compared to after VATS (95% CI: -0.07 to 0.06; p-value = 0.8929). For 30-day mortality, the odds ratio was 0.5 (95% CI: 0.17 - 1.52). For 90-day mortality, the odds ratio was 0.94 (95% CI: 0.37–2.4).
The QALYs assessed at each point of administration were slightly higher for VATS compared to thoracotomy, but the difference was not significant (Table 2).
Cost-minimisation analyses
There was a difference in average cumulative costs at 30 days of €1,560 (95% CI: €531 to €2,587) between the groups, with significantly higher costs in the VATS group than in the thoracotomy group (p-value = 0.003). There was a difference in average cumulative costs at 3 months of €2,049 (95% CI: €971 to €3,127) between the groups, with a significantly higher costs in the VATS group than in the thoracotomy group (p-value = < 0.001). In both analyses, the costs attributed to VATS were higher than those of thoracotomy, mainly due to the cost of the initial stay (€10,670 in the VATS group vs. €9,213 in the thoracotomy group; p-value = < 0.001). The detailed cost results are presented in Table 3.
Cost-utility analyses
The cost-utility analysis at 30 days was performed on 189 patients (101 VATS and 88 thoracotomies), after excluding in this order: (i) patients who died before the D30-visit; (ii) patients for whom the D-30 visit was performed much earlier or later than 30 days; (iii) patients with an undated D30-visit; (iv) patients with missing data for the EQ-5D-3L® (Fig. 1). As shown in Table 4, there was a difference in average cumulative costs at 30 days of €1,303 (95% CI: €331 to €2,275), with significantly higher average cumulative costs for the VATS group (p-value = 0.009). There was a difference in the average number of final QALYs at 30 days of 0.068 (95% CI: 0.0036 to 0.1323), significantly in favour of the VATS group (p-value = 0.038). This resulted in an ICER of €19,162 per additional QALY gained. The bootstrap analysis resulted in a mean ICER of €126,304 (95% CI:-€138,157 to €390,765). A total of 97.61% of the bootstrapped cost-utility pairs were located in the northeast quadrant of the CU-plane, meaning higher costs and more QALYs following VATS (Fig. 2).The acceptability curve (Fig. 3) revealed a 64% probability of efficiency at 30 days for VATS at a widely-accepted WTP threshold of €25,000 per QALY gained [32]. The results of the cost-utility analysis by multiple imputation (N = 254 patients) revealed an increase in the ICER (ICER: €26,015 per QALY) (Table 4) due to a slight increase in the average cost differential and a slight decrease in the QALY differential after imputation.
Cost-utility plane based on 10,000 bootstrapped replicates (at 30 days). The cost-utility plane (CU-plane) of the ICER provides a visual representation of the new strategy compared to the baseline strategy. It is constructed from the 10,000 samples generated by the bootstrap. A total of 97.61% of the bootstrapped ICER were located in the northeast quadrant of the CU-plane, meaning higher costs and more QALYs following VATS
Acceptability curve for the choice of strategy (at 30 days). This curve makes it possible to evaluate the probability that the VATS strategy will be cost-effective at 30 days according to several willingness-to-pay (WTP) thresholds. It is based on the 10,000 samples generated by the bootstrap analysis. At each value of the WTP threshold (x-axis), the curve gives the proportion of samples for which the ICER ratio is below this WTP value. This proportion (y-axis) reflects the probability for which the VATS strategy is more efficient than the thoracotomy strategy at the WTP value
The cost-utility analysis at 3 months was carried out on 147 patients (79 VATS and 68 thoracotomies) (Fig. 1) after excluding, in this order: (i) patients previously excluded from the complete cases cost-utility analysis at 30 days; (ii) patients who died between the D30 and M3-visit; (iii) patients for whom the M3-visit was performed much earlier or later than 30 days; (iv) patients with an undated M3-visit; and finally (v) patients with missing data for the EQ-5D-3L®. As shown in Table 5, there was a difference in cumulative average costs at 3 months of € 1,484 (95% CI: 376 to 2,592), with significantly higher average costs for the VATS group (p-value = 0.009). There was a difference in the average number of final QALYs of 0.0404 (95% CI: 0.0316 to 0.1123) in favour of the VATS group, but the effect was not significant (p-value = 0.2692). This resulted in an ICER of €36,733 per additional QALY gained. The bootstrap analysis resulted in a mean ICER of €324,310 (95% CI:—€273,251 to €921,869). A total of 86.14% of the bootstrapped cost-utility pairs were located in the northeast quadrant of the CU-plane, meaning higher costs and more QALYs following VATS (Fig. 4). The acceptability curve (Fig. 5) revealed a 34% probability of efficiency at 3 months for VATS at a widely-accepted WTP threshold of €25,000 per QALY gained [32]. The results of the cost-utility analysis by multiple imputation (N = 254 patients) revealed an increase in the ICER (ICER: €42,779 per QALY) (Table 5), mainly due to a slight increase in the average cost differential after imputation, and the stability in QALY differentials between complete and imputed data.
Cost-utility plane based on 10,000 bootstrapped replicates (at 3 months). The cost-utility plane (CU-plane) of the ICER provides a visual representation of the new strategy compared to the baseline strategy. It is constructed from the 10,000 samples generated by the bootstrap. A total of 86.14% of the bootstrapped ICER were located in the northeast quadrant of the CU-plane, meaning higher costs and more QALYs following VATS
Acceptability curve for the choice of strategy (at 3 months). Acceptability curve for the choice of strategy. This curve makes it possible to evaluate the probability that the VATS strategy will be cost-effective at 3 months according to several willingness-to-pay (WTP) thresholds. It is based on the 10,000 samples generated by the bootstrap analysis. At each value of the WTP threshold (x-axis), the curve gives the proportion of samples for which the ICER ratio is below this WTP value. This proportion (y-axis) reflects the probability for which the VATS strategy is more efficient than the thoracotomy strategy at the WTP value
Discussion
Of the two strategies, VATS was found to be more expensive, and it did not result in cost reductions in the post-surgical period at 30 days or at 3 months. Like in other RCTs, we did not show significant benefits for VATS in terms of post-operative complications or mortality [16,17,18,19]. However, the cost-utility analysis showed that VATS resulted in a slight but significant higher number of QALYs at 30 days after surgery (given a calculated ICER of €19,162/QALY). The bootstrap analysis revealed a 64% probability of efficiency at this time horizon for VATS, at a widely-accepted willingness-to-pay threshold of €25,000/QALY [32] (and only 34% at 3 months).
This trial is the first prospective multicentre RCT to assess the medico-economic impact of VATS compared with open thoracotomy for the management of NSCLC in France. To our knowledge, only one other cost-utility study by Bendixen et al. has been published to date comparing the two strategies [20]. This Danish study was performed in parallel to a clinical RCT between 2008 and 2014, including 103 VATS and 103 thoracotomies. Similar to our study, Bendixen et al. observed significantly better QALYs after VATS at 30 days (+ 0.07 QALY at 4 weeks, p-value: 0.008) and higher, but not significantly, QALYs at 3 months (+ 0.02 at 12 weeks, p-value = 0.162). As in our study, QALYs were assessed using EQ-5D-3L® and were imputed in case of missing data. However, they found lower overall costs per patient operated by VATS (- €4,267), and 84.3% of the bootstrapped cost-utility pairs were located in the bottom-right quadrant of the CU-plane, meaning lower costs and more QALYs following VATS. The probability of VATS being cost-effective was 95% at DKK 50,000/QALY (€6,720/QALY) according the acceptability curve. However, there were some differences between our studies: theirs was monocentric, designed for the first 12 months following surgery, from the perspective of healthcare services, and included additional costs (consultations with general practitioners, physiotherapists, psychologists, and chiropractors, and prescription drugs). Another more recent publication from 2021 comparing cost and effectiveness between VATS and open lobectomy in China concluded that hospitalization costs were similar for the two strategies, but that there were lower post-surgical costs and higher effectiveness for VATS [13]. However, this study was monocentric and retrospective, and did not present incremental medico-economic ratios. Its results cannot be compared with ours due to differences in defined costs and effectiveness criteria (blood transfusion rate, lung infection rate and post-operative LOS). Regarding the only cost differential between the two strategies, a recent systematic literature review reported that for 19 of 20 studies analysed up to 2020, VATS was associated with higher operative costs [33]. In 17 of them, this cost was significantly counterbalanced by other costs that were lower in VATS compared to thoracotomy during and after discharge. Finally, 10 studies found lower total costs for VATS, 7 found similar total costs, and 3 found higher total costs despite the lower hospitalization costs. Here again, comparisons between these studies and with our results remain difficult. In addition to the fact that the majority of these studies were retrospective and single-centre, the main difference lies in the methodology used for cost evaluation (the choice of perspective, time horizon, expenditure items, and unit costs) and in the characteristics of the included population and the surgeons (when information was available) [33].
The present study has several limitations. Only the hospital perspective was considered insofar as only hospital resources consumed were available based on the data collected in the e-CRF. In this perspective, in order to calculate the production cost per stay as recommended in medico-economic guidelines [28, 30], the DRG were retrospectively determined based on individual information available in the e-CRF, and with the expertise of the medical information department of the Dijon University Hospital. While the initial stays necessarily had the same DRG root (04C02: “Major surgery on the thorax”) for which we had only to determine a level of severity (04C021: “Major surgery on the thorax, level 1” to 04C024: “Major surgery on the thorax, level 4”), those for other re-hospitalisations had to be determined. Moreover, though the production costs per DRG are available in the ENCC, these remain average costs, calculated from 70 representative establishments in France, with the disadvantage of lacking precision on inter-individual variability [34]. However, the ENCC average costs per DRG are recognized as being close to opportunity cost and relevant for economic analyses [34]. The calculation of production costs per stay in the voluntary sample of the 70 hospitals participating in the ENCC follows a common methodology based on the principle of full costs, obtained by allocating expenses to analysis sections and to individual stays according to allocation keys. The national benchmark of the ENCC is presented according to two cost scales, one for public establishments and one for private for-profit establishments. A detailed analysis of costs is available, making them transferable [34]. Then, since the Lungsco01 trial included a micro-costing study based on fifty randomised patients to evaluate the real production cost of VATS and thoracotomy procedures [26], the average surgery cost values obtained were applied to all patients in the trial according to their arm of randomisation, but without adjustment for individual operative time and for individual consumables used. Indeed, the e-CRF was not designed to collect all resources consumed in the operating room for all patients in the trial (except for those included in the micro-costing). However, it is well recognized that a micro-costing study implies a large amount of work that cannot be done on a larger number of patients, but it is the most accurate approach for estimating the real cost of in-hospital healthcare interventions [26, 35]. The fact that the analysis was conducted in the context of a randomized trial allowed comparisons between the two groups and limited potential biases [26]. Another limitation is the number of patients randomized in the study. While the protocol planned to include 600 patients (300 per group), calculated on the basis of the primary clinical endpoint, only 259 patients were finally randomised, demonstrating the major difficulties in carrying out a RCT of this size in thoracic surgery. Another limitation is that the time horizon was 3 months after surgery, not allowing for any potential longer-term effects. However, this can be justified by the fact that neither of the two procedures is likely influence late outcomes (beyond 90 days). Finally, there were missing responses for the EQ-5D-3L® even though it was administered face-to-face. Unfortunately, missing data are a frequent issue in medico-economic analyses within randomised clinical trials. QALYs were thus imputed using the recommended multiple imputation method [36].
Nonetheless, this study has several strengths. This is the first multicentre RCT in France to prospectively evaluate the cost-utility impact of VATS versus open thoracotomy in the management of NSCLC, considering costs from the initial stay and patient follow-up (re-admissions), and utility (QALYs). The centres were required to have performed 50 VATS procedures to be included in the study, thus limiting biases linked to the experience of the surgeons performing VATS. The costing methodology used conforms to the methodological recommendations of health economists [35] and the Haute Autorité de Santé (HAS) [28], in terms of DRG-adjusted approach for the initial stays and of combination of micro-costing and gross-costing approaches. While micro-costing identifies and measures the resources consumed by the innovative intervention, gross-costing estimates the cost items that can be valued using standard costs (ex: for readmissions related to complications). Finally, our study is one of the few studies that takes ‘utility’ into consideration, though it is a particularly important dimension for medico-economic studies in lung cancer [15, 37,38,39,40].
Today, the results of medico-economic studies are considered to be a tool for authorities whose mission is to inform public decision-making on the allocation of health resources (ex: decisions regarding reimbursement). Currently, the procedure of lobectomy or segmentectomy by VATS is valorised through act GFFA009 (Pulmonary lobectomy, by thoracotomy, with preparation by thoracoscopy), whose valuation (838.75 €) is insufficient considering the real cost of VATS surgery (3,876.49 €). In our context, the revaluation of VATS should take into account the acceptability threshold of willingness-to-pay that will be set by decision-makers in terms of acceptable supplemental costs per additional QALY gained. Other additional criteria could also be taken into consideration, depending on the decision-making context. For example, multi-criteria decision analysis (MCDA) could also be relevant since it provides information on a wider range of outcomes including physical functioning, psychological well-being, person-centeredness, access to care, and financial affordability [41]. Research comparing MCDA and a cost-utility analysis is needed. Good communication between researchers and decision-makers will be an important part of identifying the most suitable approach [41].
Conclusions
Given our results, the economic efficiency of VATS at a willingness-to-pay threshold of €25,000/QALY remains fragile at 30 days (64% probability). The economic efficiency is not established beyond that time horizon. However, the acceptability curves given will allow decision-makers to judge the probability of efficiency of this technology depending on other WTP thresholds.
Availability of data and materials
The clinical datasets generated and/or analysed during the current study are not publicly available because the indirect nominative data cannot be shared publicly under French law, but they can be made available from the corresponding author on reasonable request. The hospital cost data per DRG used during the current study were obtained from the ENCC database (year 2018). Access to this database is freely available on https://www.scansante.fr/applications/enc-mco for the initial stay and re-hospitalisation for complications, and on https://www.scansante.fr/enc-ssr for rehabilitation stays.
Abbreviations
- ARDS:
-
Acute Respiratory Distress Syndrome
- ATIH:
-
Agence Technique d’Information Hospitalière (Agency for Information on Hospital Care)
- CPI:
-
Consumer Price Index
- CRF:
-
Case Report Form
- CU:
-
Cost-Utility
- CU-plane:
-
Cost-Utility plane
- DRG:
-
Diagnosis Related Group
- ECOICOP:
-
European Classification of Household Consumption Functions
- ENCC:
-
Etude Nationale des Coûts à méthodologie Commune
- EQ-5D-3L®:
-
EuroQol 5 Dimensions 3 Levels
- ICER:
-
Incremental Cost-Effectiveness Ratio (in context of Cost-Effectiveness Analyses), or: Incremental Cost-Utility Ratio (in context of Cost-Utility Analyses)
- LC:
-
Lung Cancer
- LOS:
-
Length Of Stay
- MCDA:
-
Multi-Criteria Decision Analysis
- NSCLC:
-
Non-Small Cell Lung Cancer
- QALY:
-
Quality-Adjusted Life Years
- RCT:
-
Randomised Controlled Trial
- SD:
-
Standard Deviation
- VATS:
-
Video-Assisted Thoracoscopic Surgery
- WTP:
-
Willingness-To-Pay
References
Siegel R, Miller K, Fuchs H, Jemal A. Cancer statistics. CA Cancer J Clin 2022;72:7–33.
Vansteenkiste J, De Ruysscher D, Eberhardt W, Lim E, Senan S, Felip E, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clnical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24:vi89-98.
Howington J, Blum M, Chang A, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer. Chest. 2013:e278S-313. https://doi.org/10.1378/chest.12-2359.
Paul S, Altorki N, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg. 2010;139:366–78. https://doi.org/10.1016/j.jtcvs.2009.08.026.
Thomas P, Berbiz J, Falcoz P, EPITHOR Group, et al. National perioperative outcomes of pulmonary lobectomy for cancer: the influence of nutritional status. Eur J Cardiothorac Surg. 2014;45:652–9. https://doi.org/10.1093/ejcts/ezt452.
Ezer N, Kale M, Sigel K, Lakha S, Mhango G, Goodman E, et al. Outcomes after video-assisted thoracoscopic lobectomy versus open lobectomy for early-stage lung cancer in older adults. Ann Am Thorac Soc. 2018;15:76–82.
Stéphan F, Boucheseiche S, Holland J, et al. Pulmonary complications following lung resection: a comprehensive analysis of incidence and possible risk factors. Chest. 2000;118:1263–70. https://doi.org/10.1378/chest.118.5.1263.
Die Loucou J, Pagès P, Falcoz P, Thomas P, Rivera C, Brouchet L, et al. Validation and update of the thoracic surgery scoring system (Thoracoscore) risk model. Eur J Cardiothorac Surg. 2020;58:350–6.
Li Z, Liu H, Li L. Video-assisted thoracoscopic surgery versus open lobectomy for stage I lung cancer: a meta-analysis of long-term outcomes. Exp Ther Med. 2012;3:886–92. https://doi.org/10.3892/etm.2012.485.
Zhang Z, Zhang Y, Feng H, et al. Is video-assisted thoracic surgery lobectomy better than thoracotomy for early-stage non-small-cell lun Cancer? A systematic review and meta-analysis. Eur J Cardiothorac Surg. 2013;44:407–14. https://doi.org/10.1093/ejcts/ezt015.
Cao C, Manganas C, Ang S, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg. 2012;1:16–23. https://doi.org/10.3978/j.issn.2225-319X.2012.04.18.
Taioli E, Lee D, Lesser M, et al. Long-term survival in video-assisted thoracoscopic lobectomy vs open lobectomy in lung-cancer patients: a meta-analysis. Eur J Cardiothorac Surg. 2013;44:591–7. https://doi.org/10.1093/ejcts/ezt051.
Chen W, Yu Z, Liu H. Comparison of cost effectiveness between video-assisted thoracoscopic surgery (vats) and open lobectomy: a retrospective study. Cost Eff Resour Alloc. 2021;19(1):55.
Cai Y, Fu X, Xu Q, et al. Thoracoscopic lobectomy versus open lobectomy in stage I non-small cell lung Cancer: a meta-analysis. PLoS ONE. 2013;8:e82366.
Bendixen M, Jørgensen O, Kronborg C, et al. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17:836–44. https://doi.org/10.1016/S1470-2045(16)00173-X.
Kirby T, Mack M, Landreneau R, et al. Lobectomy–video-assisted thoracic surgery versus muscle-sparing thoracotomy. A randomized trial. J Thorac Cardiovasc Surg. 1995;109:997–1002. https://doi.org/10.1016/S0022-5223(95)70326-8.
Sugi K, Kaneda Y, Esato K. Video-assisted thoracoscopic lobectomy achieves a satisfactory long-term prognosis in patients with clinical stage IA lung cancer. World J Surg. 2000;24:27–31. https://doi.org/10.1007/s002689910006.
Palade E, Passlick B, Osei-Agyemang T, et al. Video-assisted vs open mediastinal lymphadenectomy for Stage I non-small-cell lung cancer: results of a prospective randomized trial. Eur J Cardiothorac Surg. 2013;44:244–9. https://doi.org/10.1093/ejcts/ezs668.
Long H, Tan Q, Luo Q, Wang Z, Jiang G, Situ D, et al. Thoracoscopic surgery versus thoracotomy for lung cancer: short-term outcomes of a randomized trial. Ann Thorac Surg. 2018;105:386–92.
Bendixen M, Kronborg C, Jørgensen O, Andersen C, Licht P. Cost-utility analysis of minimally invasive surgery for lung cancer: a randomized controlled trial. Eur J Cardiothorac Surg. 2019;56:754–61.
Pagès P-B, Abou Hanna A, Bertaux A-C, Aho LSS, Magdaleinat P, Baste J-M, et al. Medicoeconomic analysis of lobectomy using thoracoscopy versus thoracotomy for lung cancer: a study protocol for a multicentre randomised controlled trial (Lungsco01). BMJ Open 2017:e012963. https://doi.org/10.1136/bmjopen-2016-012963.
Briggs A, O’Brien B. The death of cost-minimization analysis? Health Econ. 2001;10:179–84.
ScanSanté. ENC MCO. https://www.scansante.fr/applications/enc-mco - Accessed 14 Feb 2022.
ScanSanté. ENC SSR. https://www.scansante.fr/enc-ssr - Accessed 14 Feb 2022.
Launois R, Vergnenègre A, Garrigues B. Notions et mesure des coûts en fonction de la perspective choisie. Costs, costs and more costs: which one should we use? Bull Cancer. 2003;90:946–54.
Charvin M, Späth HM, Bernard A, Bertaux A-C. A micro-costing evaluation of lobectomy by thoracotomy versus thoracoscopy. J thorac Dis. 2019;11:1233–42. https://doi.org/10.21037/jtd.2019.03.67.
Institut national de la statistique et des études économiques (INSEE). Indice des prix à la consommation harmonisé annuel - Base 2015 - Ensemble des ménages - France - Nomenclature Coicop: 03.3.0.0 - Services hospitaliers. Identifiant 001763348 2022. 2022. https://www.insee.fr/fr/statistiques/serie/001763348#Tableau - Accessed 17 Feb 2022.
Haute Autorité de Santé. Choix méthodologiques pour l’évaluation économique à la HAS. Guide méthodologique. Juillet 2020. Haute Autorité de Santé - 5 avenue du Stade de France - 93218 Saint-Denis la Plaine Cedex. France. https://www.has-sante.fr/upload/docs/application/pdf/2020-07/guide_methodologique_evaluation_economique_has_2020_vf.pdf.
EuroQol Group. EQ-5D. https://euroqol.org/eq-5d-instruments/ - Accessed 17 Feb 2022.
Drummond M, O’Brien B, Stoddart G, Torrance G. Méthodes d’Evaluation Economique des Programmes de Santé (version française). Paris: ECONOMICA (2ème édition); 1998.
Morelle M, Plantier M, Dervaux B, Pagès A, Deniès F, Havet N, et al. Méthodes d’analyse et de traitement des données de coût: approches par “micro-costing” et “gross-costing.” Revue d’epidémiologie et de Santé Publique. 2018;66:S101–18.
Veronesi G, Navone N, Novellis P, Dieci E, Toschi L, Velutti L, et al. Favorable incremental cost-effectiveness ratio for lung cancer screennig in Italy. Lung Cancer. 2020;143:73–9.
Fiorelli A, Forte S, Caronia FP, Ferrigno F, Santini M, Horsleben Petersen rené, et al. Is video-assisted thoracoscopic lobectomy associated with higher overall costs compared with open surgery? Results of best evidence topic analysis. Thoracic Cancer. 2021;12:567–79.
Mercier G, Costa N, Riche V-P. Calcul et analyse des coûts hospitaliers: guide méthodologique. Sources de données, données utilisées et modalité de recueil. Revue d’Epidémiologie et de Santé Publique. 2018;66:S73-91.
Guerre P, Hayes N, Bertaux A-C, on behalfof the French Costing group. Calcul et analyse des coûts hosiptaliers: Guide méthodologique. Estimation du coût hospitalier: approches par “micro-costing” et “gross-costing.” Revue d’Epidémiologie et de Santé Publique. 2018;66:S65-72.
Faria R, Gomes M, Epstein D, White IR. A Guide to Handling Missing Data in Cost-Effectiveness Analysis Conducted Within Randomised Controlled Trials. PharmacoEconomics. 2014;32(12):1157–70.
Villanti AC, Jiang Y, Abrams DB, Pyenson B. A cost-utility analusis of lung cancer screening and the additional benefits of incorporing smoking cessation interventions. PLoS One. 2013;8:e71379.
Ngo PJ, Cressman S, Behar-Harpaz S, Karikios DJ, Canfell K, Weber marianne F. Applying utility values in cost-effectiveness analyses of lung cancer screening: a review of methods. Lung Cancer. 2022;166:122–31.
McMahon PM, Kong CY, Bouzan C, Weinstein MC, Cipriano LE, Tramontano AC, et al. Cost-effectiveness of computed tomography screening for lung cancer in the United States. J Thorac Oncol. 2011;6(11):1841–8.
Lim E, Batchelor T, Shackcloth M, Dunning J, McGonigle N, Brush T, et al. Study protocol for VIdeo assisted thoracoscopic lobectomy versus conventional Open LobEcTomy for lung cancer, a UK multi-centre randomised controlled trial with an internal pilot (the VIOLET study). BMJ Open. 2019;9:e029507. https://doi.org/10.1136/bmjopen-2019-029507.
Van den Bogaart EHA, Kroese MEAL, Spreeuwenberg MD, Ruwaard D, Tsiachristas A. Economic evaluation of new models of care: does the decision change between cost-utility analysis and multi-criteria decision analysis? Value Health. 2021;24:795–803.
Acknowledgements
The authors thank the 10 centres that participated in the inclusion of patients and the collection of data for this study: CH Victor Dupouy (ARGENTEUIL), CH Henri Duffaut (AVIGNON), HCL—Louis Pradel (BRON), Centre Jean Perrin (CLERMONT-FERRAND), CHU Dijon – Hôpital du Bocage (DIJON), APHM—Hôpital Nord (MARSEILLE), CHU de Montpellier – Hôpital Arnaud de Villeneuve (MONTPELLIER), APHP—Hôpital Cochin (PARIS), CHU de Rennes – Hôpital Pontchaillou (RENNES), CHU de Rouen – Hôpital Charles Nicolle (ROUEN). The authors thank the Direction of Clinical Research and Innovation (DRCI) of the Dijon University Hospital, particularly the Clinical Research Unit and the Internal Promotion Unit. The authors also thank Ms. Aline JAZAYERI, phD (Cardiovascular and thoracic surgery unit) for logistic coordination; the Medical Information Department of the Dijon University Hospital for identification of the DRGs. They are grateful to the French Ministry of Health for funding and to all the patients for their participation. The authors thank Suzanne Rankin for editing the English manuscript.
Funding
This study was funded by the French Ministry of Health as part of the 2014 Medico-Economic Research Program.
Author information
Authors and Affiliations
Contributions
A-LS realized medico-economic literature review, conducted the medico-economic analyses and wrote the manuscript (Abstract, Material and Methods, Results, Discussion, Conclusion, Tables and Figures). SA conducted the statistical analyses. AB was the chief investigator and led the project. P-BP realized clinical literature review and wrote the introduction of the manuscript. A-LS, LSAG, AB and P-BP reviewed the manuscript. AB, HA-H, MF, PM, CM-A, FT, RG, J-MB, P-AT, BR-D-L–T, AP and P-BP contributed to the inclusions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. The protocol of this study was approved by an Ethics Committee (Comité de Protection des Personnes Est III) on the 8th of February 2015, and the French Medicines Agency (Agence Nationale de Sécurité du Médicament et des produits de santé) on the 9th of June 2015—Identification number: 2015-A00339-40. Written informed consent to participate in this study was provided by the patients.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Soilly, AL., Aho Glélé, L.S., Bernard, A. et al. Medico-economic impact of thoracoscopy versus thoracotomy in lung cancer: multicentre randomised controlled trial (Lungsco01). BMC Health Serv Res 23, 1004 (2023). https://doi.org/10.1186/s12913-023-09962-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09962-y