Abstract
Background
Routine program data indicates positivity rates under 2% from HIV testing services (HTS) at sites supported by Centre for Health Solutions-Kenya in Central Kenya. Achieving the UNAIDS 95:95:95 goals requires continuous identification of people living with HIV in an environment of diminishing resources. We assessed non-clinical and clinical characteristics of persons who tested HIV-positive aimed at improving the process of HTS through Provider-Initiated HIV Testing & Counseling (PITC).
Methods
We conducted a retrospective analysis of routine PITC program data collected between October 2018 and September 2019 from six health facilities located in three counties in central Kenya. Stratification was based on county and facility volume. A multivariable logistic regression model, clustered adjusted for facility using robust standard errors, was used to determine predictors of a positive HIV result.
Results
The total sample was 80,693 with an overall positivity rate of 1.2%. Most, (65.5%), were female and 6.1% were < 15 years. Most clients, 55,464 (68.7%), had previously tested for HIV. Client characteristics associated with a higher odds of positivity on multivariable analysis included: being female (adjusted odds ratio [aOR] 1.27, 95% confidence interval [CI] (1.03–1.57); adults 15 years and above compared to children < 15 years, divorced and married polygamous compared to married monogamous [aOR 3.98, 95% CI (2.12–7.29) and aOR 2.41 95% CI (1.48–3.94) respectively]; clients testing for the first time compared to repeat testers in less than 12 months [aOR 1.39, 95% CI (1.27–1.51)]. Similarly, repeat testers in more than 12 months compared to repeat testers in less than 12 months [aOR 1.90, 95% CI (1.55–2.32)]; presumptive TB clients compared to those without signs of TB [aOR 16.25, 95% CI (10.63–24.84)]. Clients tested at inpatient departments (IPD) were more likely to get a positive HIV result compared to those tested at outpatient departments (OPD), and other departments.
Conclusions
The study findings highlight client characteristics such as age, marital status, HIV test entry point, first-time test, repeat test after 12 months, and TB status as factors that could influence PITC results and could be used to develop a screening tool to target eligible clients for HTS in low HIV prevalence settings.
Similar content being viewed by others
Introduction
An estimated 1.5 million Kenyans are living with HIV of whom 79.5% are aware of their status [1]. The 2018 Kenya HIV prevalence survey (KENPHIA), estimated a national HIV prevalence of 4.9% among adults and 0.7% among children. In three counties of central Kenya, HIV prevalence was estimated at 4.2% in Murang’a County, 2.2% in Nyandarua, and 5.1% in Nyeri County [1]. Compared to the high HIV burden regions such as Homa Bay County with a prevalence rate of 19.6%, these are low HIV-burden counties and also categorized as middle antiretroviral treatment (ART) coverage counties ranging between 70 to 79% [2]. Routine program data indicates continued low positivity rates from HIV testing services (HTS) with the three counties reporting positivity rates below 2% (male 1.8% and female 1.5%). In 2021, the highest positivity was reported among adults above 25 years (2%) and children aged 0 to 4 years (1.4%) [3].
Achieving the UNAIDS first and second 95 goals requires identifying people living with HIV (PLHIV) and linking them to treatment [4]. Getting to the 95% target remains an uphill task as factors associated with HIV infection continue to change and therefore the need to continuously improve our understanding of the HIV epidemic by region and population. These constant changes suggest the need to continually review program implementation strategies for HTS approaches toward meeting the UNAIDS goals [5]. To this end, the United States President’s Emergency Fund for AIDS Relief (PEPFAR) Country Operation Plan 21 required implementing partners to optimize the limited resources by adopting efficient interventions for HIV case identification. Self-test, social network strategies (SNS), and assisted partner notification services (aPNS) are recommended as efficient HTS approaches in Kenya [2, 6]. The 2020 PEPFAR report recognized the need to advance provider-initiated testing and counseling (PITC) as a strategy that contributes the highest number of HIV positives identified compared to other HTS modalities and remains one of the least costly case-finding strategies available [7]. The WHO HIV testing guidelines of 2019 also recommend targeted HIV testing through the use of a symptom screening approach in low HIV burden settings with a national HIV prevalence of below 5% [8].
Research evidence suggests that the implementation of risk prediction algorithms based on patient characteristics could be used to strengthen risk screening and improve case identification and thus introduce moderate efficiencies to HIV testing services offered in health facilities [9]. The 2016 Kenya HIV testing services guidelines which recommended a routine opt-out PITC approach also provided generalized categories of high-risk persons to be prioritized for a test. The national program further proposed the integration of HTS in all service delivery points for national implementation [10]. However, to achieve efficiency in PITC there is a need for deeper analysis to further understand program outcomes based on non-routine parameters and their impact in a sub-national context. Since 2017, the Centre for Health Solutions – Kenya (CHS) has implemented aPNS in central Kenya alongside other effective strategies that continue to yield good results measured by the number needed to test to get one HIV-positive case. The program data however shows that PITC contributes over 60% of cases identified in the region. Our study aimed to describe the demographic and clinical characteristics of persons who tested HIV positive to improve the efficiency of HTS to test less and identify more through PITC in Murang’a, Nyandarua, and Nyeri counties of central Kenya.
Study methods
Study population
The study population was all persons tested for HIV through routine provider-initiated testing and counselling interventions. Persons who tested through community testing or partner notification services were excluded from the analysis.
Study design and setting
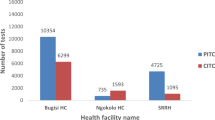
This was a cross-sectional retrospective study utilizing routine HTS data from October 2018 to September 2019. Six facilities located across 3 counties in central Kenya including Murang’a (Population 1,056,640; HIV prevalence 3%, ART coverage 91%), Nyandarua (Population 638,289; HIV prevalence 2.2%, ART coverage 90%), and Nyeri counties (Population 759,164; HIV prevalence 5.1%, ART coverage 91%) were included in the study [1, 11]. These are Ministry of Health (MOH) owned county referral and primary healthcare hospitals that are supported by the Centre for Health Solutions – Kenya (CHS) to provide HTS services through the Tegemeza Plus project, with funding and technical assistance from the US Centers for Disease Control and Prevention (CDC). Other details, including outcomes of this project setting, have been described elsewhere [12,13,14,15,16]). The facilities were purposively sampled to include a mix of high volume (facility 1—County, facility 2—County, facility 3—County) and low volume (facility 1—County, facility 2- County, facility 3—County). Facility categorization was based on the monthly outpatient department (OPD) workload with high volume being > 10,000 patients seen in a month and low volume being < 10,000 patients seen in a month. A census of all clients was done and included a total of 80,683 clients (35,018 – Murang’a county, 21,909 – Nyandarua county, and 23,756 – Nyeri county).
Data collection and management
Routine data were collected by data officers who abstracted data from the laboratory HIV testing services registers (MOH 362) covering the period between October 2018 to September 2019. The outcome variable was the HIV test result while predictors variables included the date of the HIV test, age, sex, marital status, population type (key population [men who have sex with men (MSM), people who inject drugs (PWID), female sex workers (FSW)] versus general population), department (outpatient department [OPD] vs inpatient department [IPD], integrated management of childhood illnesses (IMCI), others [Medical outpatient clinics for dermatology, dental, diabetes]), new (never tested before) or repeat HIV test (tested in the last 12 months), duration since last HIV test, history of HIV test, history of sexually transmitted infections (STI), tuberculosis (TB) screening results, pre-exposure prophylaxis (PrEP) screening results (answering ‘Yes’ to any question in the PrEP RAST tool) and GBV screening result (answering ‘Yes’ to any question in the National GBV screening criteria). Data were entered into a MySQL database and cleaned by data officers, and the final dataset was exported in a Microsoft Excel format for analysis.
Statistical analysis
Routine HIV individual testing data collected at health facilities were used. Descriptive statistics included mean (standard deviation) and counts (proportions). Univariable and multivariable logistic regression models, clustered adjusted for facility-level variations, were used to determine predictors of a positive HIV result. The final multivariable model used was developed using a backward stepwise approach with the probability of inclusion set at 0.20. The univariable and multivariable odds ratios (aOR) and corresponding 95% confidence intervals (CIs) were presented. All the statistical tests were evaluated at the 5% level of significance. All the analyses were done in Stata version 15.1 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.).
Ethical approval
This study was approved by the Kenyatta National Hospital Ethics and Scientific Research Committee. The protocol was also reviewed in accordance with the U.S. Center for Disease Control and Prevention (CDC) human research protection procedures and was determined to be research, but the CDC investigators did not interact with human subjects or have access to identifiable data or specimens for research purposes. We received a waiver of informed consent for the use of retrospective data. All data were kept confidential and only the CHS team had access to identifiable patient data.
Results
Socio-demographic characteristics of clients
A total of 80,683 clients had an HIV test done between October 2018 to September 2019 as shown in Table 1. Of these, 52,878 (65.5%) were female, 4,894 (6.1%) were less than 15 years old, and 50,016 (62.0%) were in a married monogamous relationship. More than two-thirds 55,464 (68.7%) had previously tested for HIV.
HIV testing outcome
The overall HIV positivity rate among the clients tested was 1.2% (982/80,683). HIV positivity rate was 1.4% (n = 342) among the 25,219 first-time testers, 1.0% (n = 482) among those who had previously tested (‘repeat testers’) for HIV within 12 months, and 1.9% (n = 158) among the repeat testers in over 12 months. The highest positivity rates were among ages 25–34 [286 (1.3%)], 35–44 [269 (1.6%)], and 45–54 [164 (1.6%)] as shown in Table 1.
Client characteristics associated with a positive test
Univariable analysis
On univariable analysis, adults aged 25 to 29, 30 to 34, 35 to 39, and 40 to 49 years compared to children less than 15 years were associated with significantly higher odds of having a positive HIV test result (Table 2). Divorced and married polygamous clients compared to married monogamous ones had higher odds of having a positive HIV result, OR 2.41, 95% CI (1.48–3.94) and OR 3.98, 95% (2.12–7.29) respectively. Female clients compared to males also had higher odds of having a positive HIV test result, OR 1.27, 95% CI (1.03–1.57). Clients tested at IMCI, outpatient, or other departments compared to IPD were less likely to have a positive HIV test result [OR 0.14 95% CI (0.12–0.17), OR 0.33 95% CI (0.20–0.55), and OR 0.22 (0.19–0.26) respectively] (Table 2).
Newly tested clients and those having a repeat test after 12 months compared to < 12 months had significantly higher odds of having a positive HIV test result (OR 1.33, 95% CI (1.09–1.62) and (OR 1.82, 95% CI (1.32–2.52) respectively as shown in Table 2. The presumptive TB clients compared to clients with no signs of TB had significantly higher odds of having a positive HIV test result, (OR 16.21, 95% CI (8.32–31.57) (Table 2).
Multivariable analysis
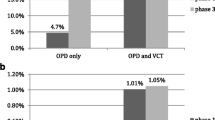
On multivariable analysis, being an adult (15 years plus) aged, 20 to 24, 25 to 29, 30 to 34, 35 to 39, 40 to 49, and 50 plus years compared to children less than 15 years was associated with significantly higher odds of having a positive HIV test result, [aOR 1.65 95% CI (1.01–2.69), aOR 2.45 95% CI (1.61–3.74), aOR 3.40 95% CI (1.54–7.51), aOR 3.75 95% CI (1.79–7.83), aOR 3.16 95% CI (1.56–6.43), aOR 3.06 95% CI (1.64–5.70), and aOR 2.57 (1.27–5.17) respectively] as shown in Table 2. Female clients had significantly higher odds of having a positive HIV test result compared to males (aOR 1.27, 95% CI (1.03–1.57). Divorced clients and married polygamous compared to married monogamous ones also had significantly higher odds of having a positive HIV result [aOR 3.98, 95% CI (2.12–7.29) and aOR 2.41 95% CI (1.48–3.94)] respectively. Those clients tested in IMCI, OPD, or other departments were still less likely to have a positive HIV test result using IPD as a reference, [aOR 0.15 95% CI (0.10–0.24), aOR 0.26 95% CI (0.13–0.54), and aOR 0.26 (0.14–0.46)] respectively as shown in Table 2.
New clients testing for the first time compared to repeat testers in less than 12 months had significantly higher odds of having a positive HIV test result (aOR 1.39, 95% CI (1.27–1.51). Similarly, repeat testers in more than 12 months compared to repeat testers in less than 12 months also had significantly higher odds of having a positive HIV test result (aOR 1.90, 95% CI (1.55–2.32). Presumptive TB clients compared to those with no signs of TB had significantly higher odds of having a positive HIV test result (aOR 16.25, 95% CI (10.63–24.84)), as shown in Table 2.
Key populations (MSM, PWID, FSW) and GBV status did not meet the model probability inclusion criteria and were therefore not included in the final multivariable model.
Discussion
Our study looked at the demographic and clinical characteristics of persons who tested HIV positive in central Kenya. Older clients aged over 20 years and above had significantly higher odds of testing HIV positive compared to those below 15 years. Among all age groups, this study showed that clients aged 35–39 years had the highest odds of testing HIV positive as compared to clients below 15 years. This finding differs from a study carried out in rural Kenya and Uganda which showed that more HIV infections were among persons aged 15–34 years [1, 13] and the KENPHIA 2018 report which showed that prevalence peaked among adults aged 45 to 49 years. The reason for this difference may be explained by the geographical differences in the HIV epidemic between Kenya and Uganda, with Uganda being classified under countries with > 10% adult prevalence as compared to Kenya which is classified under countries with adult prevalence of between 1–5% [5]. Another reason for the differences could be that the KENPHIA assessment covered the entire country whereas this study was only conducted in three counties in central Kenya.
Our study showed that the divorced and married polygamous were more likely to test HIV-positive compared to the married monogamous. This is consistent with a systematic review done in seven sub-Saharan African countries and three other studies carried out in Kenya [11, 17,18,19,20,21] which reported that the divorced/separated were significantly more likely to be HIV-positive compared to the married. While marital status may not be a prominent indicator in HIV eligibility screening tools, our study suggests its potentially important role in improving yield and should be incorporated in risk assessment for testing in Kenya and similar settings.
Female clients seeking health services were more likely to test HIV-positive as compared to male clients. This corroborates a finding of a study carried out in rural Kenya and Uganda and population-based HIV impact assessments done in Kenya, Uganda, and Tanzania which reported that women comprised of a majority of those likely to test HIV-positive [17]. This further corroborates population-based HIV impact assessments (PHIAs) done in Kenya, Uganda, Tanzania, and Rwanda that indicated that more females were HIV infected than males [1, 21,22,23]. This could be because of better health-seeking behavior among females than males, coupled with female biological and socio-cultural vulnerabilities, such as a lack of power to bargain for condom use during sex [24]. For this reason, service delivery points visited by female clients could be strengthened by including an HTS provider offering testing services to maximize testing and yield.
Patients tested at IPD were more likely to test HIV positive as compared to those tested at IMCI and other departments. This is consistent with a finding of a study carried out in several sub-Saharan countries which reported that PITC among inpatients had the highest positivity rate compared to other testing departments [25]. This is because clients already admitted in hospitals (if HIV infected) would likely show symptoms of HIV infection and be easy to reach hence the explanation for the high positivity rate compared to other departments. This means that for effective yield in inpatient departments, strategies could be put in place to screen all admitted patients for HTS eligibility and offer ‘opt-out’ HIV testing to all those eligible while addressing concerns about privacy and stigma in crowded spaces [25]. Patient education on the need to test for those admitted for other illnesses could be encouraged to reduce the chances of opting out of the HIV test.
Clients testing for the first time were more likely to test HIV-positive as compared to repeat testers. This reflects similar findings from two studies done in Kenya which showed that HIV-positive results were more common among first-time testers [18, 26]. This is explained by some factors such as the client’s location far from the testing facility, lower age bracket of 18–24, and low education level [27]. Including questions in HIV screening tools that explore why first-time testers do not test when they visit a health facility could help to improve access.
Clients having a repeat test after 12 months were more likely to test HIV-positive compared to those having a repeat test in less than 12 months. This concurs with two studies done in Kenya which showed that HIV-positive test results were most common among first-time testers and late re-testers [24]- 27. With frequent testing, clients receive prevention messages during the testing and counseling session and are likely to follow the prevention measures given. This could be a possible reason why repeat testers after 12 months are likely to test HIV-positive as compared to those who repeat tests in less than 12 months. Programs in Kenya and similar settings should optimize HTS eligibility screening to identify first-time testers and late retesters to be prioritised for HIV testing to improve yield. Stakeholders could also educate clients to increase awareness of the need for HIV testing for those never tested and at risk and among late retesters.
Presumptive TB clients were more likely to test HIV-positive compared to those with no signs of TB. This finding is consistent with studies done in Nairobi, Kenya, and India which showed that persons with symptoms of TB had an HIV prevalence of 61% [28] and a 12% yield respectively among patients with presumptive TB [29]. This is because TB is among the major opportunistic infections in HIV-infected persons [18, 19]. This means that all clients presenting at the health facilities with signs suggestive of TB need to be screened for HTS eligibility with fidelity and tested. This also calls for streamlining patient flows in TB clinics to ensure all patients in such departments are tested for HIV, reducing missed opportunities. Programs in Kenya and similar settings should optimize presumptive TB screening as an important opportunity to increase yield from HIV testing.
GBV status was not significantly associated with HIV positivity in this study. This however contrasts with a study carried out in the South Wollo zone, Ethiopia which reported that partner sexual violence by another perpetrator was strongly associated with HIV infection [30]. There is a need to tailor-make the eligibility screening process for individuals undergoing GBV, who are at ongoing risk for HIV infection in the central region of Kenya.
PrEP eligibility was not significantly associated with HIV positivity in this study. This is central to the WHO recommendation that PrEP be offered to populations at substantial ongoing risk. This calls for further study on PrEP eligibility and HIV positivity in different settings.
Key populations (MSM, FSW, PWID) did not show any significant association with HIV positivity. The limitation in measurement of this particular variable is that this study was carried out in a general population setting with only 57 clients identified as key population, and only one turning out to be HIV-positive; hence, could give a misleading picture because of the low numbers used. This differs from a report by UNAIDS that reported the rate of new adult infections among the key population and their sexual partners was 62%. Key populations are disproportionately affected by HIV and have higher morbidity and mortality rates than the general population [5]. This calls for the development of screening tools that look out for key population individuals seeking hospital services and offer them HIV testing services.
Study limitations
This study had some limitations. First, the use of cross-sectional and routine program data that is captured in paper-based registers would not allow us to examine cause and effect. Secondly, transcription errors may have occurred during the process of data abstraction from registers to the electronic system and could lead to study biases. Another limitation was on variables used in the analysis in that some key HIV-positive predictor variables, like lifestyle, and education level, among others, were not evaluated because the study was limited to variables available in the HTS laboratory register. Lastly, the study included a limited number of key populations thereby affecting the generalizability of the results to them.
Conclusion
We found that client characteristics such as age, marital status, HIV test entry point, first-time test, repeat test after 12 months, and TB status are potentially predictive of the outcome of HIV case finding in PITC settings in central Kenya. The factors highlighted as determinants of a positive HIV test in this study can be used to develop a screening tool to target high-risk clients for HTS in similar settings. To the best of our knowledge, no similar study using a large dataset from the three central Kenya counties has been done. The researchers intend to build a prognostic risk model based on the multivariate model that will be trained, tested, calibrated, and validated to have a predictive capability to classify HTS clients as either low, medium, or high risk in low HIV prevalence settings.
Availability of data and materials
The dataset used is a deidentified dataset with individual-level routine HIV testing data and is not currently publically available as it is the property of the Ministry of Health and the Government of Kenya. The dataset can be obtained from the corresponding author based on a reasonable request.
Abbreviations
- aPNS:
-
Assisted partner notification services
- ART:
-
Antiretroviral therapy
- CDC:
-
Centers for Disease Control and Prevention
- CHS:
-
Centre for Health Solutions - Kenya
- CI:
-
Confidence Interval
- FSW:
-
Female sex workers
- GBV:
-
Gender based violence
- IMCI:
-
Integrated management of childhood illnesses
- IPD:
-
Inpatient department
- MOH:
-
Ministry of Health
- KENPHIA:
-
The Kenya Population-based HIV Impact Assessment
- MSM:
-
Men who have sex with men
- NASCOP:
-
National AIDS and STI Control Program
- OPD:
-
Outpatient department
- OR:
-
Odds Ratio
- PEPFAR:
-
President’s Emergency Plan for AIDS Relief
- PLHIV:
-
People living with HIV
- PMTCT:
-
Prevention of mother-to-child transmission of HIV
- PITC:
-
Provider initiated testing and counselling
- PrEP:
-
Pre-exposure prophylaxis
- PWID:
-
People who inject drugs
- SNS:
-
Social network strategies
- SSA:
-
Sub-Saharan Africa
- STI:
-
Sexually transmitted infections
- SQL:
-
Structured Query Language
- TB:
-
Tuberculosis
- UNAIDS:
-
The Joint United Nations Programme on HIV/AIDS
- WHO:
-
World Health Organization
References
NASCOP. “KENPHIA 2018 Preliminary Report,.” 2020.
PEPFAR. “PEPFAR 2021 Country and Regional Operational Plan ( COP / ROP ) Guidance for all PEPFAR Countries,.” USA: WHo; 2020. p. 2020.
PEPFAR, “PEPFAR DATIM database.” [Online]. Available: https://www.datim.org/. [Accessed: 09-Aug-2022].
UNAIDS. “Understanding Fast-Track Targets. Accelerating action to end the AIDS epidemic by 2030,.” 2015.
UNAIDS. Programme on HIV/AIDS: Data 2020. 2020.
Wekesa P. et al., “Time to HIV testing of sexual contacts identified by HIV-positive index clients in Siaya County, Kenya,” PLoS One, vol. 15, no. 9 September, pp. 1–11, 2020.
PEPFAR. 2020 Annual Report to Congress. 2020.
M. D. Quigless. Consolidated Guidelines on HIV Testing Services. 2019.
G. Antelman et al., “Balancing HIV testing efficiency with HIV caseidentification among children and adolescents (2–19 years) using an HIV risk screening approach in Tanzania,” PLoS One, vol. 16, no. 5 May, pp. 1–16, 2021.
NASCOP. The Kenya HIV Testing Services Guidelines. 2015. p. 1–78.
K. N. B. of Statistics, Kenya population and housing census volume 1: Population by County and sub-County, vol. I, no. November. 2019.
Wekesa P, McLigeyo A, Owuor K, Mwangi J, Nganga E, Masamaro K. Factors associated with 36-month loss to follow-up and mortality outcomes among HIV-infected adults on antiretroviral therapy in Central Kenya. BMC Public Health. 2020;20(1):1–11.
Wekesa P, McLigeyo A, Owuor K, Mwangi J, Isavwa L, Katana A. Temporal trends in pre-ART patient characteristics and outcomes before the test and treat era in Central Kenya. BMC Infect Dis. 2021;21(1):1–10.
McLigeyo A, Wekesa P, Owuor K, Mwangi J, Isavwa L, Mutisya I. Factors Associated with Treatment Outcomes among Children and Adolescents Living with HIV Receiving Antiretroviral Therapy in Central Kenya. AIDS Res Hum Retroviruses. 2022;38(6):480–90.
Wekesa P, McLigeyo A, Owuor K, Mwangi J, Ngugi E. Survival probability and factors associated with time to loss to follow-up and mortality among patients on antiretroviral treatment in central Kenya. BMC Infect Dis. 2022;22(1):1–10.
McLigeyo A, Owuor K, Ng’ang’a E, Mwangi J, Wekesa P. Characteristics and Treatment Response of Patients with HIV Associated Kaposi’s Sarcoma in Central Kenya,”. HIV/AIDS – Res Palliat Care. 2022;14:207–15.
Nyabuti MN, et al. Characteristics of HIV seroconverters in the setting of universal test and treat: Results from the SEARCH trial in rural Uganda and Kenya. PLoS One. 2021;16(2):1–13.
Tenkorang EY. Marriage, widowhood, divorce and HIV risks among women in sub-Saharan Africa. Int Health. 2014;6(1):46–53.
Kimanga DO, et al. Prevalence and Incidence of HIV Infection, Trends, and Risk Factors Among Persons Aged 15–64 Years in Kenya. JAIDS J Acquir Immune Defic Syndr. 2014;66(Supplement 1):S13–26.
Kimani JK, Ettarh R, Ziraba AK, Yatich N. Marital status and risk of HIV infection in slum settlements of Nairobi, Kenya: results from a cross-sectional survey. Afr J Reprod Health. 2013;17(1):103–13.
MOH and RBC, “Rwanda Population-based HIV Impact Assessment. RPHIA 2018–2019,” Report, no. September, pp. 1–232, 2020.
TACAIDS. Tanzania HIV Impact Survey (THIS) 2016–2017. 2018.
Verloo M, Roggeband C. Gender impact assessment: The development of a new instrument in the netherlands. Impact Assess. 1996;14(1):3–20.
Sia D, Onadja Y, Nandi A, Foro A, Brewer T. What lies behind gender inequalities in HIV/AIDS in sub-Saharan African countries: Evidence from Kenya, Lesotho and Tanzania. Health Policy Plan. 2014;29(7):938–49.
Dougherty G, et al. Reaching the first 90: Improving inpatient pediatric provider-initiated HIV testing and counseling using a quality improvement collaborative strategy in Tanzania. J Assoc Nurses AIDS Care. 2019;30(6):682–90.
De Anda S, et al. Predictors of First-Time and Repeat HIV Testing Among HIV-Positive Individuals in Kenya. J Acquir Immune Defic Syndr. 2020;85(4):399–407.
Mugo PM, et al. Trends and predictors of HIV positivity and time since last test at voluntary counselling and testing encounters among adults in Kilifi, Kenya, 2006–2017. Wellcome Open Res. 2021;4:1–28.
Odhiambo J, et al. Provider-initiated HIV testing and counselling for TB patients and suspects in Nairobi, Kenya. Int J Tuberc Lung Dis. 2008;12(3 SUPPL. 1):63–8.
A. M. Kumar et al., “HIV testing among patients with presumptive Tuberculosis: How do we implement in a routine programmatic setting? Results of a large operational research from India,” PLoS One, 2016; 1(5):.
F. Hassen and N. Deyassa, “The relationship between sexual violence and human immunodeficiency virus (HIV) infection among women using voluntary counseling and testing services in South Wollo Zone, Ethiopia,” BMC Res. Notes, 2013:6(1);
Acknowledgements
We acknowledge the support of the county health management teams, and all health care workers for their work in providing HTS ensuring complete documentation, CHS leadership for guidance and direction, the health information systems team for developing the data collection application, and the monitoring and evaluation team for coordinating data collection at health facilities. We also thank all the amazing clients we served without whose data this study would not be possible.
Funding
This manuscript has been supported by funding from the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) under the terms of cooperative agreement GH002024. The funding body did not play any role in the study design and collection, analysis, and interpretation of data and in the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors (RM, KO, JMU, JMW, and PW) made significant contributions in interpretation of the data and also gave approval for the final paper. RM, JMU, KO, and PW developed the idea and were in charge of study implementation including data collection. KO, RM and PW were involved in data management, analysis, and results writeup. RM, JMU, PW, and KO contributed to drafting and revising the manuscript with guidance and intellectual input from co-authors (JMW). PW and KO have access to the data and take responsibility for the integrity and accuracy of the data. All authors contributed substantially to the interpretation of the data and approved the final manuscript.
Attribution of support
This study was supported by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the U.S. Centers for Disease Control and Prevention (CDC) under the terms of Cooperative Agreement No. GH002024 CHS Tegemeza+.
Disclaimer
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the funding agencies.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Kenyatta National Hospital—University of Nairobi Ethics Review Committee. The study was reviewed according to the Centers for Disease Control and Prevention (CDC) human research protection procedures and was determined to be and approved as research, but CDC was not engaged. As this research was retrospective, the Kenyatta National Hospital – University of Nairobi Ethics Review Committee waived the need for consent from study participants. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muinde, R., Owuor, K., Mutiso, J. et al. Optimizing HIV case identification: investigating client characteristics predictive of HIV positivity from provider-initiated testing (PITC) in central Kenya. BMC Health Serv Res 23, 1005 (2023). https://doi.org/10.1186/s12913-023-09876-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09876-9