Abstract
Background
Traditional cardiac rehabilitation programs are centre-based and clinically supervised, with their safety and effectiveness well established. Notwithstanding the established benefits, cardiac rehabilitation remains underutilised. A possible alternative would be a hybrid approach where both centre-based and tele-based methods are combined to deliver cardiac rehabilitation to eligible patients. The objective of this study was to determine the long-term cost-effectiveness of a hybrid cardiac telerehabilitation and if it should be recommended to be implemented in the Australian context.
Methods
Following a comprehensive literature search, we chose the Telerehab III trial intervention that investigated the effectiveness of a long-term hybrid cardiac telerehabilitation program. We developed a decision analytic model to estimate the cost-effectiveness of the Telerehab III trial using a Markov process. The model included stable cardiac disease and hospitalisation health states and simulations were run using one-month cycles over a five-year time horizon. The threshold for cost-effectiveness was set at $AU 28,000 per quality-adjusted life-year (QALY). For the base analysis, we assumed that 80% completed the programme. We tested the robustness of the results using probabilistic sensitivity and scenario analyses.
Results
Telerehab III intervention was more effective but more costly and was not cost-effective, at a threshold of $28,000 per QALY. For every 1,000 patients who undergo cardiac rehabilitation, employing the telerehabilitation intervention would cost $650,000 more, and 5.7 QALYs would be gained, over five years, compared to current practice. Under probabilistic sensitivity analysis, the intervention was cost-effective in only 18% of simulations. Similarly, if the intervention compliance was increased to 90%, it was still unlikely to be cost-effective.
Conclusion
Hybrid cardiac telerehabilitation is highly unlikely to be cost-effective compared to the current practice in Australia. Exploration of alternative models of delivering cardiac telerehabilitation is still required. The results presented in this study are useful for policymakers wanting to make informed decisions about investment in hybrid cardiac telerehabilitation programs.
Similar content being viewed by others
Introduction
Cardiac rehabilitation is a holistic multidisciplinary program tailored to provide patients with cardiovascular disease a range of supports including education, risk factor management, psychosocial care, eating healthy and exercise training [1]. Conventional cardiac rehabilitation programs are centre-based under clinical supervision, with their safety and effectiveness well established. For example, cardiac rehabilitation significantly improves quality of life, reduces cardiac hospitalisations and mortality, and in turn reduces costs to the healthcare system [2]. Given these benefits, referral to cardiac rehabilitation is a Class 1A recommendation for secondary prevention of cardiovascular disease [3]. However, current programs remain underutilised world-wide [4] with reported attendance rates as low as 18–40% [5]. Two Australian studies reported that only 30% of patients eligible for cardiac rehabilitation were referred and fewer than one-third of those referred attended the program [6, 7].
Low referral and participation rates can be attributed to several issues that occur across patient, provider, program and system levels. These include gender, socio-economic factors [8], travel time and distance to centre-based cardiac rehabilitation facilities [9], poor referral systems [10], fragmented care [11], and out-of-pocket costs of attending programs [12]. Low referral and attendance rates indicate that the benefits cardiac rehabilitation provides in the secondary prevention of cardiovascular disease are underutilised in Australia. As such, alternative models of care are required to supplement centre-based programs to encourage increased participation, adherence and completion.
A number of different cardiac rehabilitation models have been trialled to improve uptake. In particular, telerehabilitation, or the delivery of services via telecommunication networks or the internet, has garnered much attention for its potential to overcome some of the barriers of conventional centre-based cardiac rehabilitation. Additionally, telerehabilitation has demonstrated effectiveness [13], may reduce healthcare costs associated with rehospitalisation and absenteeism from work [14], and can be delivered in convenient ways for patients. Despite the increasing availability of such approaches, few were implemented before the pandemic. However, the rapid transition of services to virtual cardiac rehabilitation across Australia in 2020 highlighted the feasibility and acceptability of remote program delivery [15]. Implementation of fully tele-based cardiac rehabilitation programs however, comes with its own set of challenges including increased staff workload, as well as requirements for digital literacy, access to equipment, system infrastructure, and technological support [16]. A possible alternative would be a hybrid approach where both centre-based and tele-based methods are combined to deliver cardiac rehabilitation to eligible patients. When the willingness to participate in a cardiac telerehabilitation program was assessed amongst cardiac rehabilitation participants, the majority (70%) indicated that they would be interested in a hybrid cardiac rehabilitation program [17]. Additionally, delivering telehealth alongside centre-based programs has been reported to be the preference of Australian cardiac rehabilitation providers [16]. Moreover, adding independent home-based rehabilitation to supervised centre-based care may encourage patients to improve self-management of their condition and promote long-term behaviour change. However, trials of such hybrid programs have reported mixed results, and none have evaluated if hybrid cardiac telerehabilitation programs sustain benefits beyond the study period [18, 19].
In the absence of randomised controlled trials with sustained follow-up, there has been increasing use of decision analytic models to determine the long-term costs and benefits of a health intervention. Decision analytic models integrate information from various sources into a single analytical framework and capture the variation of economic outcomes over a long period of time. Consequently, model-based economic evaluations provide better evidence for decision making than trial-based economic evaluations. Even though model-based economic evaluations are vital in identifying cost-effective interventions, none of the systematic reviews to date have assessed the long-term cost-effectiveness of a hybrid cardiac telerehabilitation program. Therefore, the objective of this study was to determine the long-term cost-effectiveness of a hybrid cardiac telerehabilitation in the context of implementation in the Australian setting.
Methods
Intervention selection
As cost-effectiveness studies require detailed costing information such as the intervention cost, cost of the health service utilisation, and long-term effectiveness measures, the first aim was to find a study that met the above requirements. To do this, previously published systematic reviews examining the cost-effectiveness of cardiac rehabilitation were used [20, 21] to identify a trial which had used a hybrid cardiac telerehabilitation program as the intervention. An electronic database search was conducted for the time period 2017 to January 2022 using the same terms as in Scherrenberg et al. [20], to identify new studies relevant to these reviews.
This process identified several potential randomised controlled trials which measured costs of telerehabilitation for cardiovascular disease (Supplementary table 1). Three of these studies [22,23,24] reported on cardiac telerehabilitation in the Australian/New Zealand context. All aimed to determine the effectiveness of home-based remotely monitored telerehabilitation programs compared to conventional centre-based care. While these studies could have provided contextually relevant interventions for our analytical model, none reported on the probability of cardiac related hospitalisation after cardiac rehabilitation which is an important health service outcome in determining the cost-effectiveness of an intervention. Most other international trials identified also failed to report enough information for developing a decision analytic model. For example, they lacked information that could be used to determine health state transition probabilities or information on health service utilisation. Other potential studies were ruled out as they focussed mostly on patients with heart failure or were conducted too long ago to be applicable to current practice.
Consequently, based on these results and expert opinion of clinical members of the team, the Belgium Telerehab III [25] was the only suitable intervention to model in our analysis. Telerehab III was a multicentred randomised control trial, that investigated the effectiveness of a long-term hybrid cardiac telerehabilitation program. The trial based economic evaluation of the Telerehab III study reported that hybrid cardiac telerehabilitation was more effective in reducing cardiac related hospitalisations compared to conventional centre-based cardiac rehabilitation alone. Furthermore, health benefits persisted when the Telerehab III outcomes were reported after 2 years follow up [26].
Therefore, a Markov model was developed to assess the cost-effectiveness of Australians who undergo hybrid cardiac telerehabilitation (Telerehab III trial) compared to those attending centre-based cardiac rehabilitation.
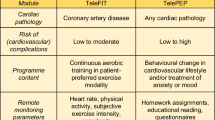
Telerehab III trial
The Telerehab III trial comprised of 140 patients, who had (i) coronary heart disease (94% in the intervention group and 93% in the control group), treated with coronary artery bypass grafting or percutaneous coronary intervention or (ii) chronic heart failure (6% in the intervention group and 7% in the control group) with reduced or preserved ejection fraction and defined by the New York Heart Association (NYHA) functional class system I to III only [25].
The intervention group (n = 70) were enrolled in a 24-week cardiac telerehabilitation program after receiving the first 6 weeks of a standard 12-week centre-based cardiac rehabilitation program. During the first 6 weeks of the cardiac telerehabilitation program, the intervention group continued to receive centre-based cardiac rehabilitation but were also taught how to use the computer-based software and accelerometer. Upon initiation of the telerehabilitation only phase, they were provided with customised exercise programs and were asked to self-monitor their activities using an accelerometer. They were asked to upload their activity data to a secure webpage every two weeks. A semi-automatic tele-coaching system provided feedback on their physical activity performance, and smoking and dietary modification advice weekly via email or text message. In essence, while utilising a hybrid cardiac rehabilitation format, the intervention focussed more on sustaining behaviour change beyond attendance at a centre-based program.
Centre-based cardiac rehabilitation in Australia
Our model’s control group aimed to reflect current Australian practice for centre-based cardiac rehabilitation. We used a recently conducted study to determine the length and number of sessions per week in Australian practice [27]. The study reported that patients had, on average, ten cardiac rehabilitation sessions. Therefore, the control group of our study were assumed to receive ten sessions of conventional centre-based cardiac rehabilitation. In the economic evaluation, we compared cost and effectiveness of the hybrid cardiac telerehabilitation program to the current centre-based cardiac rehabilitation care in Australia.
Target population
The target population was people who are eligible, referred and compliant with attending cardiac rehabilitation in Australia. As the Telerehab III study was used as a basis for our model, we assumed that our target population had similar eligibility criteria for cardiac rehabilitation i.e. had coronary heart disease or chronic heart failure (NYHA I, II, and III). This is consistent with cardiac rehabilitation eligibility criteria reported by Australian programs [27].
Several studies, such as an audit of South Australian cardiac rehabilitation programs, have reported a high percentage of participants successfully completing telerehabilitation programs, with proportions exceeding 85% [28, 29]. However, we assumed a more conservative completion rate of 80%, for the base analysis. Furthermore, we performed a scenario analysis to assess the cost and outcome implications if 90% of participants successfully complete telerehabilitation.
Model structure
A Markov model was developed on Tree Age Pro 2022 to estimate the costs and quality-adjusted life-years (QALYs) of people who had undergone hybrid cardiac telerehabilitation compared to those who underwent centre-based cardiac rehabilitation. The Markov model has four health states (Fig. 1): stable after the initial cardiac event, hospitalised due to cardiac event, hospitalised due to non-cardiac event, and death. The model starts at the "stable" health state, and the patients remain in this state until they have a cardiac-related hospitalisation, non-cardiac-related hospitalisation or die over the course of time. If they transit from “stable” to either of the hospitalised health states, they can die while being hospitalised or return to the "stable" health state.
The data used for the model was from the Telerehab III study [25] and was supplemented with inputs from other published studies [27, 30] and the Victorian Cardiac Outcomes Registry [31]. To be consistent in our study, parameter data were collected from an Australian setting wherever possible. We used a pre-COVID-19 pandemic data baseline period, as hospitalisations for non-COVID diseases decreased after 2020, and the mortality rate was higher than expected.
Effectiveness of the Telerehab III intervention was only available for two years after the intervention ended and there was a lack of data supporting longer term effectiveness. Therefore, the decision-analytic model was simulated only for a 5-year time horizon, transitioning in 1-month cycles through the health states described earlier. Quality-adjusted life-years were used to evaluate effectiveness where one QALY is equivalent to one year in perfect health. A healthcare payer perspective was taken for this analysis. An annual rate of 5% was used to discount costs and QALYs in the base case and probabilistic sensitivity analyses.
Data sources
Cost information
All costs are reported in 2022 Australian dollars for the current analysis. The Campbell & Cochrane Economics Methods Group—Evidence for Policy and Practice Information—Centre (CCEMG-EPPI) Cost Converter was used when required [32]. The cost of standard centre-based cardiac rehabilitation in Australia was calculated using the National Efficient Price (NEP) Determination 2022–23-Price Weight Tables [33]. We used Appendix K, price weights for non-admitted patients—Tier 2 V7.0, to estimate the cost of cardiac rehabilitation in the model. Clinic 40.21 is Cardiac Rehabilitation and has a price weight of 0.0407. (Cost of one session is 0.0407 X NEP ($5,797) = $235.94). Therefore, assuming that the mean length of standard cardiac rehabilitation is 10 sessions [27], the cost of completing a course of centre-based cardiac rehabilitation in Australia is estimated to be about $2,359 per patient.
The cost of the resources used in the cardiac telerehabilitation program was based on the Telerehab III study [25] and included the cost of accelerometers, software, the web-page service, and information brochures (Table 1). The cost of the web-page service and information brochures was obtained from data provided in the Telerehab III study [25]. Since the accelerometer used in the Telerehab study (YorBody accelerometer) is not available in Australia, we used the Actigraph Monitor, a device with similar physical activity measurement features. The Actigraph monitor, software, and wearable accessory costs were obtained directly from the Actigraph Sales Team in March 2022.
To estimate the cost of managing a stable cardiac patient in Australia, we assumed that a patient with cardiovascular disease has four visits to the general practitioner and one specialist visit per year, based on expert opinion of the clinician members from the study team. The cost of a general practitioner visit was estimated using Medical Benefit Schedule (MBS) Item 23 and the cost of an annual specialist visit using MBS Item 116 [38]. A cardiac patient's average yearly medical cost was obtained from a published source [30]. The cost of hospitalisation from a cardiac-related or a non-cardiac cause was derived from a linked dataset [39]. This dataset has cost information of routinely collected and linked hospital admission, emergency presentation and death registry data of patients with cardiac disease in Queensland, Australia. The following four registries were linked in the dataset: Government Death Registration Data collection, Queensland Hospital Admitted Patient Data Collection (QHAPDC), Queensland Health Emergency Department Data Collection (QHEDDC), and National Hospital Costing Data Collection (NHCDC).
Utility information
The utility weights used in the model were sourced from previously published information [30]. This study utilised data from the Victorian Cardiac Outcomes Registry (VCOR), 30-day follow-up questionnaire given to patients following treatment for coronary artery disease in Victorian hospitals. The responses were used to generate 30-day utility scores, where a maximum value of 1 is indicative of being in full health, a score of 0 represents death, and less than 0 indicates a health state worse than death (rare).
Transition probabilities
We calculated five transition probabilities in the model. Monthly probability of:
-
1.
Hospitalisation for a cardiac event (Fig. 1; P1)
-
2.
Hospitalisation for a non-cardiac event (Fig. 1; P2)
-
3.
Death after a cardiac-related hospitalisation (Fig. 1; P3)
-
4.
Death after a non-cardiac-related hospitalisation (Fig. 1; P4)
-
5.
Death among stable cardiac patients (Fig. 1; P5)
Hospitalisation probabilities
The probability of hospitalisation for a cardiac event was based on the Telerehab III study [25], which was obtained at one year follow-up. The annual probabilities of hospitalisation due to a cardiac event in the intervention and control groups were 0.1014 and 0.2285, respectively (Fig. 1; P1) [25]. In the absence of long-term evidence, we assumed that these probabilities would reduce annually by 10%.
We used the VCOR-30-day rehospitalisation data to estimate the probability of hospitalisation for a non-cardiac event (Fig. 1; P2) [37]. We assumed the rate of non-cardiac hospitalisations would remain constant over time.
Probability of death
In 2018–2019, there were 11.5 million hospitalisations in Australia where 10,372,469 were for people aged 20 years and over [35] and 160,787 hospitalisations were related to coronary heart disease [36]. Mortality data was sourced from the Australian Bureau of Statistics [34], where it is reported that 6,051 ischaemic heart disease (ICD-10 CM Codes I20-I25) related deaths occurred in hospitals. Therefore, we used the probability of in-hospital death related to coronary heart disease to be 0.038 (6,051/160,787) annually (monthly probability 0.0032 (Fig. 1; P3)).
We used a similar approach to estimate the probability of death during a non-coronary heart disease related hospitalisation using data from the Australian Institute of Health and Welfare and the Australian Bureau of Statistics. We deducted the age specific coronary heart disease related hospitalisations (160,787) from age-specific total hospitalisations (10,372,469) to estimate the number of non-coronary heart disease related hospitalisations. Mortality data was sourced from the Australian Bureau of Statistics [34], where it is reported that there were 78,688 non-coronary heart disease related age-specific (> 25 years) in-hospital deaths. The probability of death after a non-coronary heart disease hospitalisation, 0.0071 (Fig. 1; P4), was calculated by dividing the number of non-coronary heart disease deaths (78,688) by the total number of age-specific non-coronary heart disease hospitalisations (10,372,469).
The Australian Institute of Health and Welfare reports that in Australia an estimated 571,000 Australians aged 18 and over (2.9% of the adult population) have coronary heart disease [36]. In 2019, there were 12,193 non-hospitalised ischemic heart disease deaths reported in the Australian Bureau of Statistics data set [34]. Therefore, the annual probability of death among stable cardiac patients (Fig. 1; P5) was estimated to be 0.0214 (12,193 / 571,000).
Model evaluation
The model was run over a 5-year period with monthly cycles. The transition probabilities dictate the proportion of patients who move between the health states during each cycle. As patients transition between health states, they accumulate costs and utilities (QALYs). The accumulated costs and utilities of the Telerehab III intervention and the current centre-based cardiac rehabilitation were compared, and an Incremental Cost-Effectiveness Ratio (ICER) was estimated using marginal QALYs and costs. The study used a cost-effectiveness threshold of AU$28,000 per QALY gained, suggested by Edney et al., which reflects the opportunity cost of introducing new health system investment into a constrained budget in Australia [40]. This threshold represents the maximum amount the Australian health system should pay for one additional unit of health benefit (QALY).
Sensitivity analysis
Scenario analysis is critical in the economic evaluation of healthcare interventions to aid decision-makers in understanding the impact of uncertainty parameter estimates. An alternative scenario of 90% completion rate of the intervention was considered in the scenario analysis.
Probabilistic sensitivity analysis (PSA) was used to assess the uncertainty across all relevant parameters used in the model, and their effect on the cost-effectiveness results. To reflect the full range of uncertainty in the input parameters, each parameter for which there is uncertainty is assigned an appropriate probability distribution. In this study, the transition probabilities were assigned beta distributions as they are most suitable for binomial parameters. Costs parameters were assigned gamma distributions as they are able to reflect the skew that is often associated with healthcare costs. We performed Monte Carlo simulations with 10,000 iterations, sampling from the distributions described in Table 1.
To avoid the problems associated with interpreting negative ICERs, we used Incremental Net monetary benefit (iNMB) to evaluate the probabilistic sensitivity analyses.
The equation is:
Incremental net monetary benefit (INMB) was used to summarise uncertainty in the cost-effectiveness results in this study. The expected maximum and minimum cost-saving, QALY gain, and net monetary benefit were estimated from the 10,000 iterations of the probabilistic sensitivity analyses.
Results
Base case analysis found the telerehabilitation intervention was more effective but more costly than centre-based cardiac rehabilitation and was not cost-effective at a cost-effectiveness threshold of $28,000 per QALY (Table 2). For every 1,000 patients who undergo cardiac rehabilitation, employing the telerehabilitation intervention would cost $650,000 more, and 5.7 QALYs would be gained, over the five-year time horizon, compared to current practice.
Figure 2 illustrates the cumulative cardiac related hospital cost, non-cardiac related hospital cost and stable cardiac management cost that includes the rehabilitation costs as well. If a cohort of 1,000 patients undergoes cardiac rehabilitation, the intervention will reduce the cardiac-related hospital admission costs by $0.7 million alone in the first year and $3.4 million over five years. Since telerehabilitation has a substantial initial cost, the stable cardiac management cost, which includes rehabilitation expenses, remains high throughout the time horizon.
Results of the probabilistic sensitivity analysis are presented in Fig. 3. If a cohort of 1,000 patients undergoes cardiac rehabilitation with an 80% completion rate, over a five-year time horizon, implementing the new intervention would have 15% probability of being cost saving, 100% probability of being effective (QALY gain) and 18% probability of being cost-effective (positive incremental net monetary benefit) (Fig. 3). Across the 10,000 simulations, the intervention generated a maximum cost saving of $5.3 million (minimum -$5.1 million), maximum 7.1 QALY gain (minimum 2.8) and maximum $5.2 million gain (minimum -$5.2 million) in net monetary benefit over the five-year time horizon.
Incremental cost, QALY and net monetary benefit (iNMB) for the telerehabilitation intervention compared to the current centre-based practice. Each dot in all three graphs indicates the values generated from the 10,000 iterations in the probabilistic sensitivity analysis. Negative incremental cost indicates a cost-saving compared to current practice, and positive incremental QALY indicates more effectiveness compared to the current practice. Positive incremental NMB indicates the intervention is cost-effective compared to current practice. The solid line in the graph indicates the mean estimation
The results of the scenario analyses are in Table 3. This shows that even if the completion rate of the intervention is 90%, the telerehabilitation intervention is still unlikely to be cost-effective. Under PSA, the likelihood of the intervention being cost-effective, with 90% completion rate, is only 30%.
Discussion
We used a decision analytic model to assess the long-term cost-effectiveness of using a hybrid cardiac telerehabilitation program in the Australian setting. Our modelling indicates that the hybrid intervention delivered in the trial is very unlikely to be cost-effective compared to current cardiac rehabilitation practice in Australia, using a cost-effectiveness threshold of $28,000 per QALY. However, these findings should be interpreted with caution, and more research about the cost-effectiveness of context-relevant implementable hybrid models of cardiac rehabilitation is required for the reasons described below.
Various standalone cardiac telerehabilitation programs have been examined previously, with some finding the approach to be cost-effective, particularly for patients with heart failure. In the TELE-HF study in Poland where patients with heart failure underwent 8 weeks of telerehabilitation, the approach was found to be cost-effective compared to a centre-based program and the incremental cost of gaining a healthy life year ranged between US$49,832 and US$82,480 [41]. Additionally, an Australian study which investigated the cost-utility of a 12-week home-based telerehabilitation program for patients with heart failure, delivered via video conferencing, reported that the intervention had lower costs compared to a traditional centre-based program but demonstrated no significant difference in QALYs between the groups at 6-months [22]. For patients with coronary heart disease, findings about cost-effectiveness are less clear. A remotely-monitored and real-time coaching telerehabilitation approach was investigated in a New Zealand study where patients’ physical activity was monitored for 12 weeks [23]. However, no statistically significant differences in outcomes or health service utilisation were observed despite lower program and medication costs for remote cardiac rehabilitation. Unfortunately, none of the above trials provided data to model the long-term cost-effectiveness of such standalone telerehabilitation approaches.
There is evidence that a hybrid telerehabilitation approach may to be better than both stand-alone telerehabilitation or centre-based cardiac rehabilitation in preventing cardiac related hospitalisations and reducing healthcare and non-healthcare costs [42, 43]. However, it is difficult to make this argument with certainty due to the variation in the target population, type of tele-intervention, duration of monitoring and frequency of data transfer and evaluation. Additionally, the largely head-to-head comparisons of these different models seen in previous research limits understanding of how each telerehabilitation model may compare to usual care. Importantly, the two hybrid cardiac rehabilitation studies which have demonstrated benefits at one year both had extended intervention periods [25, 42]. The first was the Telerehab-III study, modelled in this paper, which comprised 12 weeks of centre-based cardiac rehabilitation (6 of which were hybrid), followed by an 18-week telerehabilitation program. This intervention was shown to reduce hospital admissions and have better health outcomes compared to 12 weeks of centre-based cardiac rehabilitation [25]. The second study, SmartCare-CAD from the Netherlands [42], used a similar approach with 6 weeks of centre-based cardiac rehabilitation and 12 weeks of virtual cardiac rehabilitation using accelerometers, data monitoring and video consultation. This was followed by 9 months of self-directed extended participation in the program at home with on-demand video coaching to maintain adherence. While there was no difference in quality of life between patients participating in centre-based and hybrid cardiac rehabilitation after one year, a hybrid model was likely to be cost-effective compared with centre-based care at a cost-effectiveness threshold of €20 000, although uncertainty remained [42].
Careful consideration of the applicability of European trialled hybrid programs to the Australian setting is also required. While there is Australian evidence to support the acceptability, adoption, and effectiveness of similar home-based coaching programs[44], this is not the case for the delivery of the centre-based component. Despite similarities in the overall core components and providers of centre-based cardiac rehabilitation in both regions, European programs generally provide a higher “dose” of intervention due to the greater number of sessions conducted[45]. For example, the centre-based component of the Telerehab III intervention (45 sessions over 12 weeks) is not indicative of the delivery of Australian centre-based cardiac rehabilitation (10–11 sessions over 7 weeks) [46, 47]. Consequently, this has implications for how we would feasibly implement this more resource intensive model into current practice, and also how the costs and effectiveness of the hybrid intervention should be interpreted in the Australian context.
These findings are important in the context of research demonstrating the relationship between the duration of cardiac rehabilitation and positive health and clinical outcomes. Longer durations of participation in centre-based or community-based cardiac rehabilitation have been shown to lead to decreased mortality, increased physical activity and sustained behaviour change after program completion [48]. Additionally, recent research has highlighted the importance of the total number of centre-based sessions attended on clinical outcomes, including a linear relationship between sessions completed and major adverse cardiac events [49]. While no research yet exists about the relationship between the frequency or duration of home-based exercise sessions and outcomes, it may be likely that it is the extended nature of these hybrid programs (rather than the delivery format) that is contributing to their comparative effectiveness. If these extended programs could however, be delivered in a cost-effective manner compared to shorter, centre-based programs, they may have an important role to play in the in the delivery of the maintenance phase of cardiac rehabilitation. Unfortunately, this does not yet appear to be the case for these models in the Australian setting. Consequently, more work needs to be done capturing cost and health utilisation data and evaluating hybrid telerehabilitation programs of shorter durations to determine if benefits remain. Most of the costs of the hybrid telerehabilitation program in our model came from the 12 weeks of centre-based sessions rather than the virtual components. If some of these in-person sessions could be reduced and replaced with virtual sessions (as in the SmartCare-CAD trial) the intervention may become cost-effective.
How program completion is defined and modelled can have substantial effects on the cost-effectiveness results. Our base case analysis assumed that the proportion of patients completing a program was 80%, yet even with a higher proportion completing (90%), the probability of the hybrid option being cost-effective was low (30%). While it would be unrealistic to assume a higher than 90% completion rate, a recent systematic review and a meta-analysis did indicate that exercise adherence is significantly higher in telerehabilitation compared to centre-based cardiac rehabilitation (standard mean difference 0.75; 95% CI 0.52 to 0.98) [13]. Several studies (including an audit of South Australian cardiac rehabilitation programs) have also reported very high percentage of participants successfully completing telerehabilitation, where the proportions have been more than 85% [28, 29].
The COVID-19 pandemic necessitated the delivery of cardiac rehabilitation by entirely virtual means for many programs, providing a potential catalyst for the adoption of such models in practice. However, uptake of telerehabilitation during this time was largely confined to phone and email modalities. A shift towards telerehabilitation interventions as described in successful trials will require significant organisational, clinical, and cultural change, particularly as issues remain around technological equity and literacy, reimbursement models, patient privacy and safety, quality of social interactions and staff capacity [16].
Additionally, recent research suggests that ongoing implementation of stand-alone cardiac telerehabilitation programs is not the preferred model of care. Rather, clinicians both in Australia and abroad have reported a desire to deliver hybrid cardiac rehabilitation programs combining in-person visits for assessments, provider consultation and initial exercise sessions with virtually delivered exercise training and education [16]. This enables a centre-based program and telerehabilitation to be run within the same site, providing patients with greater choice of modality, while allowing closer supervision of high-risk patients. The intervention we modelled in this analysis does not reflect this type of hybrid model. In fact, there is limited published evidence of any type about the effectiveness of such a model of cardiac rehabilitation, particularly the delivery of exercise and education via real-time videoconferencing [18]. Moreover, there is a paucity of research examining the ability of telerehabilitation of any type to increase the proportion of patients who enrol in cardiac rehabilitation programs.
Further research about the feasibility, effectiveness, equitability, service-level impacts and costs of telerehabilitation in Australian practice is warranted to understand the potential benefits of implementing hybrid models. Importantly, consideration of how these virtual models of care may impact underserved populations is required. While telerehabilitation may benefit those living in regional areas by improving access, it can also increase disparity for those with poor digital or health literacy, limited English proficiency, or from low socio-economic backgrounds [50]. Moreover, data is currently lacking to model the cost-effectiveness of hybrid cardiac rehabilitation programs for traditionally underserved groups such as First Nations people, culturally diverse communities or rural populations. However, if such models could increase cardiac rehabilitation program uptake amongst these groups, as well as those who decline participation in traditional centre-based programs, they may be worth implementing. Additionally, research about the preferences of patients for a hybrid telerehabilitation programme in the Australian context is lacking. These are important prerequisites to address before hybrid telerehabilitation programs have wide-spread implementation in Australia.
The current study has several limitations. Firstly, as we were not able to find trial data for an Australian cohort, the transition probabilities used in the model were derived from a range of published data sources. However, we believe that our study uses the best currently available information from published data sources representing the Australian population. Additionally, our analysis only applies to a specific application of telerehabilitation that we modelled in the study and does not imply that hybrid telerehabilitation will not be cost-effective with a different intervention or in a different context. It is hoped that two Australian telerehabilitation studies currently underway [51, 52] may soon provide additional models of hybrid telerehabilitation and/or Australian data to use in future decision analytic modelling. Secondly, a time horizon of 5 years was chosen in our model as long-term evidence of effectiveness is unavailable. The lack of long-term effectiveness data in hybrid telerehabilitation studies has a significant impact on evaluating the overall efficacy of the intervention. Thirdly, the diversity of both programs and participants across the Australian cardiac rehabilitation landscape must be acknowledged. While a standardised content outline for cardiac rehabilitation programs has been developed, there are currently no criteria for what constitutes a face-to-face program in Australia [53], and much heterogeneity exists. While we modelled an “average face-to-face program”, this is not representative of all cardiac rehabilitation services delivered and may limit generalisability of the findings across different approaches to in-person delivery. Additionally, participants attending programs have various levels of cardiac disease and risk, which is not easily captured in our utility values, effectiveness estimates and modelling. For example, we only modelled for patients with coronary artery disease because this reflects the underlying disease in the vast majority (~ 95%) of patient included in the original clinical trial. We cannot exclude that in other selected cohorts (such as those with heart failure) who may have higher risks of adverse outcomes and greater benefits from hybrid telerehabilitation that our findings may have differed.
Conclusion
Our study is the first to evaluate long-term cost-effectiveness of a hybrid cardiac telerehabilitation intervention in the Australian context. The results indicate that over the long-term, the Telerehab III model of hybrid cardiac telerehabilitation is highly unlikely to be cost-effective compared to current centre-based cardiac rehabilitation practice in Australia. Exploration of other models of delivering cardiac telerehabilitation and their implications for the diverse population groups they are intended to serve is still required. Our findings will assist policymakers and researchers to make informed decisions when designing future trials and planning for implementation of hybrid cardiac telerehabilitation programs.
Availability of data and materials
This is an economic analysis based on published literature and no databases were used for analysis. The data underlying this article are available in the article. The economic analysis was performed according to the Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS2022) Statement.
References
Mehra VM, Gaalema DE, Pakosh M, Grace SL. Systematic review of cardiac rehabilitation guidelines: Quality and scope. Eur J Prev Cardiol. 2020;27:912–28. https://doi.org/10.1177/2047487319878958.
Dibben G, Faulkner J, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2021. https://doi.org/10.1002/14651858.CD001800.pub4.
Visseren FL, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J. 2021;42:3227–337. https://doi.org/10.1093/eurheartj/ehab484.
Grace SL, Kotseva K, Whooley MA. Cardiac rehabilitation: Under-utilized globally. Curr Cardiol Rep. 2021;23:1–8. https://doi.org/10.1007/s11886-021-01543-x.
Beatty AL, Truong M, Schopfer DW, et al. Geographic variation in cardiac rehabilitation participation in Medicare and Veterans Affairs populations: opportunity for improvement. Circulation. 2018;137:1899–908. https://doi.org/10.1161/CIRCULATIONAHA.117.029471.
Astley CM, Chew DP, Keech W, et al. The impact of cardiac rehabilitation and secondary prevention programs on 12-month clinical outcomes: a linked data analysis. Heart Lung Circ. 2020;29:475–82. https://doi.org/10.1016/j.hlc.2019.03.015.
Scott IA, Lindsay KA, Harden HE. Utilisation of outpatient cardiac rehabilitation in Queensland. Med J Aust. 2003;179:341–5. https://doi.org/10.5694/j.1326-5377.2003.tb05588.x.
Resurreccion DM, Motrico E, Rigabert A, et al. Barriers for nonparticipation and dropout of women in cardiac rehabilitation programs: a systematic review. J Womens Health. 2017;26:849–59. https://doi.org/10.1089/jwh.2016.6249.
Bakhshayeh S, Sarbaz M, Kimiafar K, Vakilian F, Eslami S. Barriers to participation in center-based cardiac rehabilitation programs and patients’ attitude toward home-based cardiac rehabilitation programs. Physiother Theory Pract. 2019. https://doi.org/10.1080/09593985.2019.1620388.
Gurewich D, Prottas J, Bhalotra S, Suaya JA, Shepard DS. System-level factors and use of cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2008;28:380–5. https://doi.org/10.1097/HCR.0b013e31818c3b5b.
Giuliano C, Parmenter BJ, Baker MK, et al. Cardiac Rehabilitation for Patients With Coronary Artery Disease: A Practical Guide to Enhance Patient Outcomes Through Continuity of Care. Clin Med Insights. 2017;11:1179546817710028. https://doi.org/10.1177/1179546817710028.
Dunlay SM, Witt BJ, Allison TG, et al. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–9. https://doi.org/10.1016/j.ahj.2009.08.010.
Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102:1183–92. https://doi.org/10.1136/heartjnl-2015-308966.
Brouwers RWM, van Exel HJ, van Hal JMC, et al. Cardiac telerehabilitation as an alternative to centre-based cardiac rehabilitation. Neth Hear J. 2020;28:443–51. https://doi.org/10.1007/s12471-020-01432-y.
Cartledge S, Thomas E, Abell B, et al. COVID-19 Impact on Australian Cardiac Rehabilitation Programs: Results From a National Survey. Heart Lung Circ. 2022;31:S290–1. https://doi.org/10.1016/j.hlc.2022.06.493.
Cartledge S, Rawstorn JC, Tran M, et al. Telehealth is here to stay but not without challenges: a consultation of cardiac rehabilitation clinicians during COVID-19 in Victoria Australia. Eur J Cardiovasc Nurs. 2022;21:548–58. https://doi.org/10.1093/eurjcn/zvab118.
Falter M, Scherrenberg M, Kindermans H, et al. Willingness to participate in cardiac telerehabilitation: results from semi-structured interviews. Eur Heart J. 2021;3:67–76. https://doi.org/10.1093/ehjdh/ztab091.
Jin K, Khonsari S, Gallagher R, et al. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2019;18:260–71. https://doi.org/10.1177/1474515119826510.
Heindl B, Ramirez L, Joseph L, et al. Hybrid cardiac rehabilitation–The state of the science and the way forward. Prog Cardiovasc Dis. 2021. https://doi.org/10.1016/j.pcad.2021.12.004.
Shields GE, Wells A, Doherty P, et al. Cost-effectiveness of cardiac rehabilitation: a systematic review. Heart. 2018;104:1403–10. https://doi.org/10.1136/heartjnl-2017-312809.
Scherrenberg M, Falter M, Dendale P. Cost-effectiveness of cardiac telerehabilitation in coronary artery disease and heart failure patients: systematic review of randomized controlled trials. Eur Heart J Digit Health. 2020;1:20–9. https://doi.org/10.1093/ehjdh/ztaa005.
Hwang R, Morris NR, Mandrusiak A, et al. Cost-utility analysis of home-based telerehabilitation compared with centre-based rehabilitation in patients with heart failure. Heart Lung Circ. 2019;28:1795–803. https://doi.org/10.1016/j.hlc.2018.11.010.
Maddison R, Rawstorn JC, Stewart RAH, et al. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart. 2019;105:122–9. https://doi.org/10.1136/heartjnl-2018-313189.
Maddison R, Pfaeffli L, Whittaker R, et al. A mobile phone intervention increases physical activity in people with cardiovascular disease: Results from the HEART randomized controlled trial. Eur J Prev Cardiol. 2015;22:701–9. https://doi.org/10.1177/2047487314535076.
Frederix I, Hansen D, Coninx K, et al. Effect of comprehensive cardiac telerehabilitation on one-year cardiovascular rehospitalization rate, medical costs and quality of life: a cost-effectiveness analysis. Eur J Prev Cardiol. 2016;23:674–82. https://doi.org/10.1177/2047487315602257.
Frederix I, Solmi F, Piepoli MF, Dendale P. Cardiac telerehabilitation: a novel cost-efficient care delivery strategy that can induce long-term health benefits. Eur J Prev Cardiol. 2020;24:1708–17. https://doi.org/10.1177/2047487317732274.
Astley CM, Beleigoli A, Tavella R, et al. Assessing the quality of cardiac rehabilitation programs by measuring adherence to the Australian quality indicators. BMC Health Serv Res. 2022;22:267. https://doi.org/10.1186/s12913-022-07667-2.
Varnfield M, Karunanithi M, Lee C-K, et al. Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomised controlled trial. Heart. 2014;100:1770–9. https://doi.org/10.1136/heartjnl-2014-305783.
Champion S, Clark RA, Tirimacco R, et al. The Impact of the SARS-CoV-2 Virus (COVID-19) Pandemic and the Rapid Adoption of Telehealth for Cardiac Rehabilitation and Secondary Prevention Programs in Rural and Remote Australia: a multi-method study. Heart Lung Circ 2022. https://doi.org/10.1016/j.hlc.2022.07.006
McCreanor VHR. Identifying high-value care for coronary artery disease in Australia. Doctoral thesis. Brisbane: Queensland University of Technology; 2019.
Lefkovits J BA, Dinh D, Carruthers H, Doyle J, Lucas M, Stub D, Reid C.M. The Victorian Cardiac Outcomes Registry Annual Report 2021. Melbourne: Monash University- School of Public Health and Preventive Medicine; 2021.
Shemilt I, James T, Marcello M. A web-based tool for adjusting costs to a specific target currency and price year. Evid Policy. 2010;6:51–9.
Independent Hospital Pricing Authority. National Efficient Price Determination 2022–2023- Price Weight Tables. 2022.
Australian Bureau of Statistics. Classifying Place of Death in Australian Mortality Statistics. 2022. https://www.abs.gov.au/statistics/research/classifying-place-death-australian-mortality-statistics .
Australian Institute of Health and Welfare. Admitted patient care 2016–17: Australian hospital statistics. Canberra: Australian Institute of Health and Welfare; 2018.
Australian Institute of Health Welfare. Heart, stroke and vascular disease—Australian facts. Canberra: AIHW, Australian Government; 2021.
Lefkovits J, Brennan A, Dinh D, et al. The Victorian Cardiac Outcomes Registry Annual Report 2020. Melbourne: In: Monash University; 2021.
Australian Government Department of Health. Medicare Benefits Schedule (MBS) Online. http://www9.health.gov.au/mbs/search.cfm. Accessed 26 Sept 2022.
Kularatna S, Wong J, Senanayake S, et al. Financial Costs of Emergency Department Presentations for Australian Patients With Heart Disease in the Last 3 Years of Life. Health Serv insights. 2022;15:11786329221091038. https://doi.org/10.1177/1178632922109103.
Edney LC, Afzali HHA, Cheng TC, Karnon JJP. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. Pharmacoeconomics. 2018;36:239–52. https://doi.org/10.1007/s40273-017-0585-2.
Niewada M, Tabor B, Piotrowicz E, et al. Cost-effectiveness of telerehabilitation in patients with heart failure in Poland: an analysis based on the results of Telerehabilitation in the Heart Failure Patients (TELEREH-HF) randomized clinical trial. Kardiol Pol. 2021;79:510–6. https://doi.org/10.33963/kp.15885.
Brouwers RW, Van Der Poort EK, Kemps HM, Van Den Akker-Van ME, Kraal JJ. Cost-effectiveness of cardiac telerehabilitation with relapse prevention for the treatment of patients with coronary artery disease in the Netherlands. JAMA Netw Open. 2021;4:e2136652–e2136652. https://doi.org/10.1001/jamanetworkopen.2021.36652.
Główczyńska R, Piotrowicz E, Szalewska D, et al. Effects of hybrid comprehensive telerehabilitation on cardiopulmonary capacity in heart failure patients depending on diabetes mellitus: subanalysis of the TELEREH-HF randomized clinical trial. Cardiovasc Diabetol. 2021;20:1–11. https://doi.org/10.1186/s12933-021-01292-9.
Vale MJ, Jelinek MV, Best JD, et al. Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Internal Med. 2003;163:2775–83.
Abreu A, Pesah E, Supervia M, et al. Cardiac rehabilitation availability and delivery in Europe: How does it differ by region and compare with other high-income countries? Endorsed by the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2019;26:1131–46.
Astley C, Beleigoli A, Tavella R, et al. Assessing the quality of cardiac rehabilitation programs by measuring adherence to the Australian quality indicators. BMC Health Serv Res. 2022;22:1–12.
Abell B, Glasziou P, Briffa T, Hoffmann T. Exercise training characteristics in cardiac rehabilitation programmes: a cross-sectional survey of Australian practice. Open Heart. 2016;3:e000374.
Taylor C, Tsakirides C, Moxon J, et al. Exercise dose and all-cause mortality within extended cardiac rehabilitation: a cohort study. Open Heart. 2017;4:e000623. https://doi.org/10.1136/openhrt-2017-000623.
Medina-Inojosa JR, Grace SL, Supervia M, et al. Dose of cardiac rehabilitation to reduce mortality and morbidity: a population-based study. J Am Heart Assoc. 2021;10:e021356. https://doi.org/10.1161/JAHA.120.021356.
Gergen Barnett K, Mishuris RG, Williams CT, et al. Telehealth’s Double-Edged Sword: Bridging or Perpetuating Health Inequities? J Gen Internal Med. 2022;37:2845–8.
Beleigoli A, Nicholls SJ, Brown A, et al. Implementation and prospective evaluation of the Country Heart Attack Prevention model of care to improve attendance and completion of cardiac rehabilitation for patients with cardiovascular diseases living in rural Australia: a study protocol. BMJ Open. 2022;12:e054558. https://doi.org/10.1136/bmjopen-2021-054558.
Gao L, Maddison R, Rawstorn J, et al. Economic evaluation protocol for a multicentre randomised controlled trial to compare Smartphone Cardiac Rehabilitation, Assisted self-Management (SCRAM) versus usual care cardiac rehabilitation among people with coronary heart disease. BMJ open. 2020;10:e038178. https://doi.org/10.1136/bmjopen-2020-038178.
Cartledge S, Thomas E, Hollier K, Maddison R. Development of standardised programme content for phase II cardiac rehabilitation programmes in Australia using a modified Delphi process. BMJ Open. 2019;9:e032279.
Acknowledgements
We thank all SOLVE-CHD Investigators and Julia Ning for their support of this project.
Funding
This research was supported by the SOLVE-CHD Australian Government National Health and Medical Research Council (NHMRC) Synergy Grant (GNT1182301). JR is funded by a NHMRC Investigator Grant (GNT1143538).
Author information
Authors and Affiliations
Contributions
SS, SK, VM, WP contributed to the conception or design of the work. SS, UH contributed to the data acquisition and analysis. SS, BA, SM, JR, TB, WP contributed to interpretation of data for the work. SS, UH, BA drafted the manuscript. SK, VM, WP, JR, TB, SM critically revised the manuscript. All gave final approval and agreed to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is an economic analysis based on published literature. Therefore, ethics approval and consent to participate are not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary table 1.
The studies which were considered for the economic evaluation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Senanayake, S., Halahakone, U., Abell, B. et al. Hybrid cardiac telerehabilitation for coronary artery disease in Australia: a cost-effectiveness analysis. BMC Health Serv Res 23, 512 (2023). https://doi.org/10.1186/s12913-023-09546-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09546-w