Abstract
Background
Phramongkutklao Hospital is one of the largest military hospitals in Thailand. Beginning in 2016, an institutional policy was implemented in which medication prescription length was increased from 30 to 90 days. However, there have been no formal investigations into how this policy has impacted medication adherence among patients in hospitals. As such, this study evaluated how prescription length impacted medication adherence among dyslipidemia and type-2 diabetes patients who were treated at Phramongkutklao Hospital.
Methods
This pre-post implementation study compared patients who received prescription lengths of 30 and 90 days based on information recorded in the hospital database between 2014 and 2017. Therein, we used the medication possession ratio (MPR) to estimate patient adherence. Focusing on patients with universal coverage insurance, we employed the difference-in-difference method to examine changes in adherence from before and after policy implementation, then conducted a logistic regression to test for associations between the predictors and adherence.
Results
We analyzed data from a total of 2,046 patients, with equal amounts of 1,023 placed into the control group (no change to 90-day prescription length) and intervention group (change from 30 to 90-day prescription length). First, we found that increased prescription length was associated with 4% and 5% higher MPRs among dyslipidemia and diabetes patients in the intervention group, respectively. Second, we found that medication adherence was correlated with sex, comorbidities, history of hospitalization, and the number of prescribed medications.
Conclusion
Increasing the prescription length from 30 to 90 days improved medication adherence in both the dyslipidemia and type-2 diabetes patients. This shows that the policy change was successful for patients in the hospital considered for this study.
Similar content being viewed by others
Background
Over the last few decades, there has been an unprecedented rise in healthcare expenditures across the globe, [1, 2] with estimates projecting an increase of more than 200% from 2013 to 2040 [3]. Policymakers have thus employed a wide range of approaches to contain these climbing costs, including increased patient cost-sharing, switching from innovative brands to lower-priced generic alternatives, and reducing the length of time between prescription refills [1, 4, 5]. Although many such efforts have been effective, [6] they have also had unexpected spillover impacts on patients, thus increasing hospitalization and mortality rates while decreasing medication adherence [6, 7].
In 2016, Phramongkutklao Hospital implemented a measure known as the Extended Dispensing Policy (EDP), which aims to improve convenience and adherence among patients. Prior to implementation, patients with universal coverage (UC) were prescribed 30 days medication supplies, while those covered by the Civil Servant Medical Benefit (CSMB) scheme were given longer prescription lengths, specifically three-month treatments. Under the EDP, all patients with stable chronic diseases can now acquire up to three months of their prescribed medications, regardless of the provision type. While this allowance is expected to help patients, there is still a lack of evidence on the EDP’s specific impacts. Furthermore, the current situation of the national health policy of Thailand in 2023 which recommends the certain amount of prescription length supply is still unclear. As such, this study investigated how the 30-to-90-day increase in maximum prescription refill length has impacted medication adherence which is one of the key predictors of patient’s health outcome among patients with chronic disease who were treated at Phramongkutklao Hospital.
Methods
Data source
This study used hospital claims data from the Phramongkutklao Hospital Management System (PMKHMS) provided by Phramongkutklao Hospital, which is a quaternary care center and one of the largest military hospitals in Thailand. The database covered three main areas of necessary information, including demographic, clinical, and prescription data.
The demographic database covered a variety of patient characteristics, including sex, age, and the type of insurance coverage. Meanwhile, the clinical database contained details such as disease diagnostic data from the International Classification of Diseases, Tenth Revision (ICD-10), visit date, hospitalization date, and prescribed medications. Finally, the prescription database covered information on dispensed medications, dispensing date, dosing regimen, and medication quantities for each prescription.
Study design and population
In this study, we employed a pre-post implementation study design to compare changes in medication adherence following EDP implementation.
As the EDP was enacted on February 1, 2016, our investigation covered both a 12-month pre-implementation period (February 1, 2015, through January 31, 2016) and 12-month post-implementation period (February 1, 2016, through January 31, 2017). For both periods, the first occurrences of dispensing were set as index dates. Patients included in this analysis had been on stable regimens for at least six months prior to the investigated period; that is, between August 1, 2014, and January 31, 2015, which was thus defined as the identification period. Patients were followed-up from the day of their index date until the day of their last dose of medication during the investigated period (Fig. 1).
Patient’s population and patient’s medical condition
Here, patients with UC were set as the intervention group, as they had experienced an increase in prescription length from 30 to 90 days, while patients under the CSMB scheme were set as the control group, as they were always allowed prescription lengths of 90 days.
We aimed an attention on the cardiovascular disease (CVD) which is the predominant cause of global death from non-communicable diseases (NCDs), especially ischemic heart disease and stroke [8]. Additionally, both of two diseases are correlated with alteration of lipid and glucose metabolism and primarily caused by dyslipidemia and diabetes mellitus (DM) [9, 10]. Moreover, we focused on patients with type 2 diabetes and dyslipidemia, since adherence to medication therapy is an important part of patient management in such cases. [11, 12]. Patients were diagnosed with diabetes mellitus and/or dyslipidemia using the ICD-10 diagnosis codes from their claims. For diabetes mellitus, we searched for codes E11, E13, and E14, which refer to non-insulin-dependent diabetes mellitus, other specific diabetes mellitus, and unspecified diabetes mellitus, respectively [13]. Meanwhile, patients with dyslipidemia were identified using code E78, which refers to disorders of lipoprotein metabolism and other types of lipidaemia. Based on recent clinical practice guidelines, we selected statins to represent medications for treating patients with dyslipidemia [14]. For patients with diabetes mellitus, we selected seven classes of antihyperglycemic medications, including sulfonylureas, non-sulfonylureas, biguanides, thiazolidinediones (TZDs), alpha-glucosidase inhibitors (AGIs), dipeptidyl peptidase-4 inhibitors (DPP-4 inhibitors), and sodium-glucose co-transporter-2 inhibitors (SGLT-2 inhibitors) [15].
Role of eligibility
Patients were subjected to the following inclusion criteria: (1) 18 years or older on their index date, (2) had at least one prescription in any class of antihyperglycemic medication or statins refilled between February 1, 2015, and January 31, 2016, and (3) had at least one prescription refilled from February 1, 2016, to February 1, 2017. By contrast, we excluded patients if they only received insulin prescriptions or glucagon-like peptide-1 receptor agonists (GLP-1 receptor agonists) for the treatment of diabetes mellitus at any time during the investigated period. Owing to the inadequacy of data on insulin dosing and GLP-1 receptor agonists, we could not accurately examine the amount of daily doses for injectable medication utilization [12].
Drug and dosage forms
Only adherence from tablets or capsules was assessed due to their dosage form can be measured accurately.
Propensity score matching
The propensity scores were evaluated with a caliper of 0.001 via logistic regression using the following factors: age, sex, number of medications, Charlson Comorbidity Index (CCI) score, history of hospitalization, comorbidities, and class of medication. After generating weights, all patients in the intervention group were respectively matched with patients in the control group at a one-to-one ratio.
Outcome variables
Medication adherence
This study used administrative prescription refills database; therefore, the medication possession ratio (MPR) was used as a proxy to verify medication adherence. MPR is a typical method, both in outcome research and standard procedure, for calculating adherence via claim databases [16, 17]. In this study, individual MPR assessments were computed from the database using the following formula:
Medication adherence was assessed twice for each patient for both investigated periods; that is, pre- and post-EDP implementation with fixed duration of total days of follow-up. The pre-implementation period started from February 1st, 2015 through January 31st, 2016 (365 days), and the post-implementation started from February 1st, 2016 through January 31st, 2017 (366 days).
Computed MPR values were considered acceptable at ≥ 0.8, while values below 0.8 indicated nonadherence to medication [18, 19]. For patients receiving multiple therapies, MPR was calculated for each medication class, then a mean value was calculated [20, 21].
Patients who were prescribed with new medication or switch to other medication in the different medication class but still in the same therapeutic were identified as add-on and switch therapy, respectively. We assumed that patients who were switched their medication were stop taking their prior medication, then total days of follow-up were not fixed but calculated from the first date of their medication prescribed to the date of switching medication. Hospitalized patients were divided calculation into three parts which are before admission period, during admission period, and after discharged to the end of study period. Then average value of each medication class was assessed.
Independent variables and covariates
We adjusted for numerous confounding variables via regression model, including age, sex, number of medications prescribed, history of hospitalization, and CCI scores. We also incorporated time dummy variables to adjust for the time of the policy change, from 2015 to 2017.
Data Analysis
To allow a baseline comparison, we conducted a chi-square test and t-test for the categorical and continuous variables, respectively. According to the natural experimental study design, we applied the difference-in-difference method. We identified an intervention and control group as well as a post-period and pre-period, then measured the differences based on the following two aspects: intervention/control group change and pre-/post-period change. We also conducted a multivariable logistic regression analysis using the data in both intervention and control groups to demonstrate the relationship between prescription length and medication adherence by adjusting for patient characteristics and disease-related variables.
Sensitivity analysis
Owing to the lack of the standard value for MPR that used to identify medication adherence of the patients. We performed sensitivity analysis, applying various medication adherence thresholds of 0.50, 0.60, 0.70, and 0.90, included to pre-implementation and post-implementation in the study. Additionally, adjusted multivariable logistic regression was also conducted with these thresholds.
Results
Baseline characteristics
Initially, we obtained data on a total of 16,144 patients. Most descriptive characteristics showed differences between the intervention and control groups. After a propensity score adjustment, the final sample consisted of 2,046 patients, with 1,023 patients in each group. None of the demographic variables showed significant differences between these two final groups. An additional table file shows this in more detail [see Additional file 1].
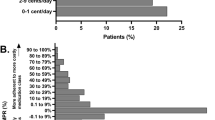
Change in medication adherence
Comparing the pre- and post-EDP periods, significant increases was identified in mean adherence (MPR) for patients with diabetes mellitus and dyslipidemia across the intervention and control groups. Looking only at those with diabetes mellitus, MPR increased by 14% and 9% in the intervention and control groups, respectively. Looking only at those with dyslipidemia, MPR increased by 22% and 18% the intervention and control groups, respectively. After propensity score matching, the tendency for pre-post changes in adherent patients for diabetes increased in both the control and intervention groups. For dyslipidemia, the intervention group reported a marked increase of 24.4%, while the control group showed a statistically significant increase of 23.1% (Table 1). Patients in the intervention group showed medication adherence nearly two times higher than those in the control group (adjusted OR than the patients in the control group) (Table 2). Women were less likely to adhere to their medications than men. Patients with histories of hospitalization during the study period were 14% less likely to adhere to their medications than those without such histories. The total number of prescribed medications was strongly correlated with medication adherence. Most comorbidities were significantly associated with medication adherence. Finally, CCI scores had positive effects on adherence.
Discussion
To the best of our knowledge, this was the first pre-post implementation study analysis to investigate the impacts of a policy designed to increase medication adherence based on administrative data from a quaternary care hospital in Thailand. Remarkably, the EDP provision was found to improve medication adherence in patients with dyslipidemia and type-2 diabetes, especially among those with UC insurance. Moreover, the EDP substantially increased the overall number of adherent patients, which is known to decrease healthcare costs and lower the risk of hospitalization [22,23,24]. These findings suggest that increasing prescription lengths from 30 to 90 days helps patients concentrate on their affiliated hospitals, thus producing continuity of care. In turn, healthcare professionals have more time to routinely take care of their patients.
Our findings are similar to those from previous studies showing increased medication adherence following measures to increase daily supplies [25,26,27]. Specifically, researchers found higher adherence due to increased prescription sizes for patients undergoing statin therapy, in which the refill period was raised from 30 to 60 days [25]. Further, a retrospective study showed that patients who received medication in four groups (antihypertensive, statins, oral hypoglycemic, and selective serotonin reuptake inhibitors) were more likely to adhere when given 90-day (vs. 30-day) prescription supplies [26]. In similar research, a study that extended the prescription length of statin medication from 30 days to 60 days or 90 days found correlations with increased medication adherence [27].
An inadequate baseline adherence rate was also noticed for diabetes and dyslipidemia patients, at only 11.2% and 13.9% for the one-year investigated period in the intervention group, respectively. This was mainly due to the limited prescription day supply up to 30 days before the policy was implemented. However, the proportions of adherent patients increased to 28.0% and 38.3% after the EDP was enacted, respectively. This was comparable to the overall adherence rate of 42.4% found in a study among patients who were prescribed antihyperglycemic medications [28]. Further, the rate of adherence found in this study was similar those reported in other studies that investigated medical and pharmacy claims databases [29, 30].
Although the clinical outcomes, such as HbA1c level, fasting plasma glucose (FPG), and lipid profiles, were not determined in this study, the literature reported their association with medication adherence. Andrew et al. [12] described that patients who do not adhere to oral glucose-lowering medications would have lower HbA1c decrease compared with adherence patients. Iloh et al. [31] explained that patients who adhere to their treatment were associated with plasma glucose controlled. Additionally, if patient adherence level to antidiabetic medication increased by 10%, level of HbA1c reduced by 0.16% as reported by Schectman [32]. Moreover, So-yeon et al. [33] concluded that adherent patients not only associated with better HbA1c level but also reduced fasting plasma glucose. For patients with dyslipidemia, increased length of statins from 30-day to 60-day at each prescription refill leads to better medication adherence and improved effectiveness of medication [25]. Another study that investigated the effects of expanding prescription length of statin from 30-day to 60-day and from 30-day to 90-day contributed to improvement in cholesterol level [27].
Factor-affecting MPR
Patient-related factors
As for other factors, we observed a non-significant relationship between patient age and medication adherence. Specifically, patients aged 26 to 50 years were less likely to adhere to their medications than those aged 18 to 25. While older groups were more likely to be adherent, this trend was not significant. These findings support a previous systematic review that demonstrated an inverted U-shaped association between patient age and medication adherence [34]. In this study, we also found that being male was related to medication adherence, but a previous systematic review found inconsistent results on the relationship between this factor and the participants’ sex [35].
Therapy-related factors
There were also interesting findings on the quantity and type of medication. Here, patients who were prescribed only one medication were 3.20 times more likely to present adherence than those who were prescribed more than one. By contrast, some studies have shown that the number of prescription medications is not associated with medication adherence, [36] although there is evidence that the frequency of drug administration imposes an influence [37]. In this latter regard, a meta-regression analysis reported that patients who took cardiovascular disease drugs once daily were significantly more adherent than patients who took medications twice daily [38]. In this way, adjusting the frequency and quantity of medication could substantially promote adherence. We also found that all medication classes (especially AGIs, SGLT-2 inhibitors, biguanides, and statins) largely influenced lower medication adherence. This may be due to unique mechanisms of action. For example, AGIs that prevent digestion and delay the absorption of carbohydrates through the intestine may produce side effects such as flatulence, nausea, and diarrhea [39, 40]. Further, the remarkable glycosuric effect of SGLT-2 inhibitors promotes the excretion of glucose via urine, meaning that patients may experience frequent urination, dry mouth, and urinary tract infections [41, 42]. Moreover, common adverse effects are present when taking metformin, including abdominal bloating, vomiting, and metallic taste, [43] while statins may result in myalgia, abdominal discomfort, and joint pain [44]. Our findings support Bubalo et al., who found that patients were less likely to comply with therapy plans when there were frequent adverse events [45]. Therefore, to promote medication adherence, healthcare providers are not only responsible for counseling about the advantages of using the medication, but also providing appropriate recommendations through adverse events.
Disease-related factors
We also found that comorbidities were significantly associated with medication adherence. Patients diagnosed with congestive heart failure, cerebrovascular disease, chronic pulmonary disease, mild liver disease, hemiplegia, and cancer were less likely to adhere, while those with other diseases were more likely to adhere. In this regard, the literature offers some conflicting findings, with some studies showing higher adherence levels as the number of comorbid conditions increases, [46, 47] and others reporting lower medication adherence with complex comorbid conditions [48, 49]. There may be several explanations for these discrepancies. First, patients with many comorbidities may require complicated medical procedures. This may negatively affect how patients perceive their care plans, thus decreasing medication adherence [50]. Moreover, complicated treatments are highly associated with an accumulating number of medications, which may lead to omissions and reduced adherence [38, 51]. Adherence to therapy regimens also decreases substantially with time, especially in cases where medications are used to treat long-term chronic diseases [52]. This generally occurs when patients lack symptoms; for example, hypertension treatments may be associated with unfavorable adherence. As comorbidities and other factors may substantially influence medication adherence, it is important for health care providers to consider specific factors pertaining to each case, which entails targeted educational provisions and patient-centered care [29].
Our findings suggest that increased prescription lengths may enhance and maintain medication adherence for patients with chronic diseases, especially type-2 diabetes mellitus and dyslipidemia. This may point to the need for relevant policy changes at public hospitals in Thailand and elsewhere due to lack of up-to-date visible national policy direction. However, caution should be taken when generalizing these results, as they are based on a single-source database. Other important considerations when attempting to apply these results to other settings include the hospital type, patient demographics, medication class, and specific measure used to represent medication adherence.
Limitations
It is worth noting that this study presents certain limitations. First, we examined administrative pharmacy claims from the Phramongkutklao Hospital database, which may not reflect the nature of all databases used in Thailand. This should be considered when comparing the results of policy changes in other hospitals. Second, the database was primarily operated for reimbursements, and did not include several predictors that have previously been associated with adherence, including education level, [53] race and ethnicity, [54] socioeconomic status, [55] adverse events with medications, [56] the relationship between healthcare providers and patients, [57] and social support [58]. Third, we used MPR as a proxy for medication adherence based on administrative prescription refills, but patients may not actually use the medications prescribed by their healthcare providers. Still, previous studies have shown that calculating adherence based on administrative data produces results that are consistent with those found in other approaches, including self-reported adherence, [59, 60] pill counts, [61] and direct measurements of serum drug concentrations [62]. In sum, this suggests that medication refill numbers reflect the amounts consumed by patients. Fourth, no data on any medications that patients may have acquired from other pharmacies or hospitals was considered in this study, which may have resulted in the underestimation of medication adherence. Finally, according to our study design was not randomized controlled, regression to mean (RTM) phenomenon was occurred and partially controlled. This determines the significance of further research to identify, reduce and handled RTM when possible [63].
Conclusion
The EDP substantially promoted medication adherence in patients with dyslipidemia and type-2 diabetes. However, several other variables also affected adherence, some of which were related to specific therapies and the patients themselves. Efforts to determine clearly changeable variables that are correlated with both would benefit healthcare providers, patients, and national health services. Still, the current findings should aid in the development of new hospital policies, especially those aimed at ensuring that patients are consistent with their prescribed medications.
Data Availability
The data that support the findings of this study are available from Phramongkutklao Hospital, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Phramongkutklao Hospital.
Abbreviations
- MPR:
-
Medication Possession Ratio
- EDP:
-
Extended Dispensing Policy
- UC:
-
Universal Coverage
- CSMB:
-
Civil Servant Medical Benefit
- PMKHMS:
-
Phramongkutklao Hospital Management System
- ICD-10:
-
International Classification of Diseases, Tenth Revision
- TZDs:
-
Thiazolidinediones
- AGIs:
-
Alpha-Glucosidase Inhibitors
- DPP4:
-
Dipeptidyl Peptidase-4
- SGLT2:
-
Sodium-Glucose co-transporter-2
- GLP-1:
-
Glucagon-Like Peptide-1
- CCI:
-
Charlson Comorbidity Index
- OR:
-
Odds Ratio
References
Ess SM, Schneeweiss S, Szucs TD. European healthcare policies for controlling drug expenditure. PharmacoEconomics. 2003;21(2):89–103.
Schumock GT, Li EC, Suda KJ, et al. National trends in prescription drug expenditures and projections for 2016. Am J Health-Syst Pharm. 2016;73(14):1058–75.
Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521–35.
Acosta A, Ciapponi A, Aaserud M et al. Pharmaceutical policies: Effects of reference pricing, other pricing, and purchasing policies. Cochrane Database Syst Rev. 2014(10).
Shirneshan E, Kyrychenko P, Matlin OS, Avila JP, Brennan TA, Shrank WH. Impact of a transition to more restrictive drug formulary on therapy discontinuation and medication adherence. J Clin Pharm Ther. 2016;41(1):64–9.
Soumerai SB. Benefits and risks of increasing restrictions on access to costly drugs in medicaid. Health Aff. 2004;23(1):135–46.
Lyles CR, Seligman HK, Parker MM, et al. Financial strain and medication adherence among diabetes patients in an integrated health care delivery system: the diabetes study of northern california (DISTANCE). Health Serv Res. 2016;51(2):610–24.
Non communicable diseases [Internet]. World Health Organization., World Health Organization; [cited 2022Dec5]. Available from:https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
Barquera S, Pedroza-Tobías A, Medina C, Hernández-Barrera L, Bibbins-Domingo K, Lozano R, et al. Global overview of the Epidemiology of Atherosclerotic Cardiovascular Disease. Arch Med Res. 2015;46(5):328–38.
Yeates K, Lohfeld L, Sleeth J, Morales F, Rajkotia Y, Ogedegbe O. A Global Perspective on Cardiovascular Disease in vulnerable populations. Can J Cardiol. 2015;31(9):1081–93.
Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14.
Farmer AJ, Rodgers LR, Lonergan M, et al. Adherence to oral glucose-lowering therapies and associations with 1-year HbA1c: a retrospective cohort analysis in a large primary care database. Diabetes Care. 2016;39(2):258–63.
International statistical classification of diseases and related health problems 10th revision: the World Health Organization. ; 2017 [cited 2017 May 19]. Available from: http://apps.who.int/classifications/icd10/browse/2016/en#/E10-E14.
Anderson TJ, Grégoire J, Hegele RA, et al. 2012 update of the canadian Cardiovascular Society Guidelines for the diagnosis and treatment of Dyslipidemia for the Prevention of Cardiovascular Disease in the adult. Can J Cardiol. 2013;29(2):151–67.
Pablo Aschner M, Oscar Mauricio Muñoz V, Girón D, et al. Clinical practice guideline for the prevention, early detection, diagnosis, management and follow up of type 2 diabetes mellitus in adults. Colombia Med. 2016;47(2):109–31.
Andrade SE, Kahler KH, Frech F, Chan KA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15(8):565–74.
Hess LM, Raebel MA, Conner DA, Malone DC. Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother. 2006;40(7–8):1280–88.
Jacobs K, Julyan M, Lubbe MS, Burger JR, Cockeran M. Medicine possession ratio as proxy for adherence to antiepileptic drugs: prevalence, associations, and cost implications. Patient Prefer Adherence. 2016;10:539–47.
Schulz M, Krueger K, Schuessel K, et al. Medication adherence and persistence according to different antihypertensive drug classes: a retrospective cohort study of 255,500 patients. Int J Cardiol. 2016;220:668–76.
Choudhry NK, Shrank WH, Levin RL, et al. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15(7):457–64.
Oladapo AO, Barner JC, Rascati KL, Strassels SA. A retrospective database analysis of neuropathic pain and oral antidiabetic medication use and adherence among Texas adults with type 2 diabetes enrolled in medicaid. Clin Ther. 2012;34(3):605–13.
Asche C, LaFleur J, Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther. 2011;33(1):74–109.
Dilokthornsakul P, Chaiyakunapruk N, Nimpitakpong P, Jeanpeerapong N, Sruamsiri R. The effects of medication supply on hospitalizations and health-care costs in patients with chronic heart failure. Value Health. 2012;15(1, Supplement):9–S14.
Clark B, DuChane J, Hou J, Rubinstein E, McMurray J, Duncan I. Evaluation of increased adherence and cost savings of an employer value-based benefits program targeting generic antihyperlipidemic and antidiabetic medications. J Manag Care Pharm.20(2):141–50.
Batal HA, Krantz MJ, Dale RA, Mehler PS, Steiner JF. Impact of prescription size on statin adherence and cholesterol levels. BMC Health Serv Res. 2007;7:175.
Taitel M, Fensterheim L, Kirkham H, Sekula R, Duncan I. Medication days’ supply, adherence, wastage, and cost among chronic patients in medicaid. Medicare & Medicaid Res Rev. 2012;2(3).
Gaziano T, Cho S, Sy S, Pandya A, Levitt N, Steyn K. Increasing prescription length could cut cardiovascular disease burden and produce savings in South Africa. Health Aff. 2015;34(9):1578–85.
Huber CA, Rapold R, Brüngger B, Reich O, Rosemann T. One-year adherence to oral antihyperglycemic medication and risk prediction of patient outcomes for adults with diabetes mellitus. Medicine. 2016;95(26):e3994.
Munsell M, Frean M, Menzin J, Phillips AL. An evaluation of adherence in patients with multiple sclerosis newly initiating treatment with a self-injectable or an oral disease-modifying drug. Patient Prefer Adherence. 2017;11:55–62.
Cindolo L, Pirozzi L, Fanizza C, et al. Drug adherence and clinical outcomes for patients under pharmacological therapy for lower urinary tract symptoms related to benign prostatic hyperplasia: Population-based cohort study. Eur Urol. 2015;68(3):418–25.
Pascal I, Ofoedu J, Uchenna N, Nkwa A, Uchamma G-U. Blood glucose control and medication adherence among adult type 2 diabetic Nigerians attending a primary care clinic in under-resourced environment of eastern Nigeria. North Am J Med Sci. 2012;4(7):310–5.
Schectman JM, Nadkarni MM, Voss JD. The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care. 2002;25(6):1015–21.
An S-Y, Kim HJ, Chun KH, Kim TH, Jeon JY, Kim DJ, et al. Clinical and economic outcomes in medication-adherent and -nonadherent patients with type 2 diabetes Mellitus in the Republic of Korea. Clin Ther. 2014;36(2):245–54.
Mann DM, Woodward M, Muntner P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44(9):1410–21.
Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–86.
Hyekyung J, Sandy Jeong R, Yeonhee K. Factors affecting medication adherence in elderly people. Patient Prefer Adherence. 2016;10:2117–25.
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. ClinTher. 2001;23:1296–310.
Weeda ER, Coleman CI, McHorney CA, Crivera C, Schein JR, Sobieraj DM. Impact of once- or twice-daily dosing frequency on adherence to chronic cardiovascular disease medications: a meta-regression analysis. Int J Cardiol. 2016;216:104–9.
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M. Acarbose for prevention of type 2 diabetes mellitus: the stop-niddm randomised trial. Lancet. 2002;359(9323):2072–7.
Kim HS, Oh M, Kim EJ, Song GS, Kim EY, Shin JG. Pharmacodynamic effects of voglibose administered alone, administered with metformin, and administered with metformin in a fixed-dose combination in healthy korean subjects. Int J Clin Pharmacol Ther. 2018;56(11):544–50.
Giugliano D, Esposito K. Class effect for SGLT-2 inhibitors: a tale of 9 drugs. Cardiovasc Diabetol. 2019;18(1):94.
Hsia DS, Grove O, Cefalu WT. An update on sodium-glucose co-transporter-2 inhibitors for the treatment of diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2017;24(1):73–9.
Nasri H, Rafieian-Kopaei M. Metformin: current knowledge. J Res Med Sci. 2014;19(7):658–64.
Ward NC, Watts GF, Eckel RH. Statin toxicity. Circ Res. 2019;124(2):328–50.
Bubalo J, Clark RK Jr, Jiing SS, et al. Medication adherence: pharmacist perspective. J Am Pharm Assoc. 2010;50(3):394–406.
Kim S, Bennett K, Wallace E, Fahey T, Cahir C. Measuring medication adherence in older community-dwelling patients with multimorbidity. Eur J Clin Pharmacol. 2018;74(3):357–64.
Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy. 2008;28(4):437–43.
Chapman RH, Petrilla AA, Benner JS, Schwartz JS, Tang SSK. Predictors of adherence to concomitant antihypertensive and lipid-lowering medications in older adults: a retrospective, cohort study. Drugs Aging. 2008;25(10):885–92.
Saadat Z, Nikdoust F, Aerab-Sheibani H, et al. Adherence to antihypertensives in patients with comorbid condition. Nephro-Urol Mon. 2015;7(4):e29863.
McAuley JW, McFadden LS, Elliott JO, Shneker BF. An evaluation of self-management behaviors and medication adherence in patients with epilepsy. Epilepsy Behav. 2008;13(4):637–41.
Obi Y, Ichimaru N, Kato T, et al. A single daily dose enhances the adherence to immunosuppressive treatment in kidney transplant recipients: a cross-sectional study. Clin Exp Nephrol. 2013;17(2):310–5.
Movahedinejad T, Adib-Hajbaghery M. Adherence to treatment in patients with open-angle glaucoma and its related factors. Electron Physician. 2016;8(9):2954–61.
Cho S-J, Kim J. Factors associated with nonadherence to antihypertensive medication. Nurs Health Sci. 2014;16(4):461.
Zhang Y, Baik SH. Race/ethnicity, disability, and medication adherence among medicare beneficiaries with heart failure. J Gen Intern Med. 2014;29(4):602–7.
Ma C. A cross-sectional survey of medication adherence and associated factors for rural patients with hypertension. Appl Nurs Res. 2016;31:94–9.
Dibonaventura M, Gabriel S, Dupclay L, Gupta S, Kim E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry. 2012;12(1):20–6.
Al-Hajje A, Awada S, Rachidi S, et al. Factors affecting medication adherence in lebanese patients with chronic diseases. Pharm Pract. 2015;13(3):1–9.
Magrin ME, D’Addario M, Greco A, et al. Social support and adherence to treatment in hypertensive patients: a meta-analysis. Ann Behav Med. 2015;49(3):307–18.
Rijcken CAW, Tobi H, Vergouwen ACM, de Jong-van LTW. Refill rate of antipsychotic drugs: an easy and inexpensive method to monitor patients’ compliance by using computerised pharmacy data. Pharmacoepidemiol Drug Saf. 2004;13(6):365–7.
Cook WCLWE, Martin BC, Perri IIIM. Concordance among three self-reported measures of medication adherence and pharmacy refill records. J Am Pharm Assoc. 2005;45(2):151–9.
Grymonpre R, Cheang M, Fraser M, Metge C, Sitar DS. Validity of a prescription claims database to estimate medication adherence in older persons. Med Care. 2006;44(5):471–7.
Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;50(1):105–16.
Barnett A, van der Pols J, Dobson A. Regression to the mean: what it is and how to deal with it. Int J Epidemiol. 2005;34:215–20.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
I.J. contributed to the study conception and design, data collection, analysis and interpretation of results, and manuscript preparation. S.T. is a corresponding author. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors confirm that all methods were carried out in accordance with relevant guidelines and regulations. The Institutional Review Board of the Royal Thai Army Medical Department (IRB-RTA) waived the requirement to obtain informed consent due to the type of the research which could not practicably be carried out without the waiver and data were de-identified before used in the analysis. The institutional review board of the Institutional Review Board of the Royal Thai Army Medical Department (IRB-RTA) (S048h/60_Exp) provided ethical approval for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jarujumrus, I., Taychakhoonavudh, S. Impact of prescription length supply policy on patient medication adherence in Thailand. BMC Health Serv Res 23, 533 (2023). https://doi.org/10.1186/s12913-023-09530-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09530-4