Abstract
Background
Clinical activity accounts for 70–80% of the carbon footprint of healthcare. A critical component of reducing emissions is shifting clinical behaviour towards reducing, avoiding, or replacing carbon-intensive healthcare. The objective of this systematic review was to find, map and assess behaviour change interventions that have been implemented in healthcare settings to encourage clinicians to reduce greenhouse gas emissions from their clinical activity.
Methods
Studies eligible for inclusion were those reporting on a behaviour change intervention to reduce carbon emissions via changes in healthcare workplace behaviour. Six databases were searched in November 2021 (updated February 2022). A pre-determined template was used to extract data from the studies, and risk of bias was assessed. The behaviour change techniques (BCTs) used in the interventions were coded using the BCT Taxonomy.
Results
Six full-text studies were included in this review, and 14 conference abstracts. All studies used a before-after intervention design. The majority were UK studies (n = 15), followed by US (n = 3) and Australia (n = 2). Of the full-text studies, four focused on reducing the emissions associated with anaesthesia, and two aimed at reducing unnecessary test ordering. Of the conference abstracts, 13 focused on anaesthetic gas usage, and one on respiratory inhalers. The most common BCTs used were social support, salience of consequences, restructuring the physical environment, prompts and cues, feedback on outcome of behaviour, and information about environmental consequences. All studies reported success of their interventions in reducing carbon emissions, prescribing, ordering, and financial costs; however, only two studies reported the magnitude and significance of their intervention’s success. All studies scored at least one item as unclear or at risk of bias.
Conclusion
Most interventions to date have targeted anaesthesia or pathology test ordering in hospital settings. Due to the diverse study outcomes and consequent inability to pool the results, this review is descriptive only, limiting our ability to conclude the effectiveness of interventions. Multiple BCTs were used in each study but these were not compared, evaluated, or used systematically. All studies lacked rigour in study design and measurement of outcomes.
Review registration
The study was registered on Prospero (ID number CRD42021272526) (Breth-Petersen et al., Prospero 2021: CRD42021272526).
Similar content being viewed by others
Cutting carbon emissions as a first step toward reducing greenhouse gas (GHG) levels in the atmosphere is the most urgent goal in the climate emergency. Climate change is the ‘single biggest health threat facing humanity’ and is already negatively impacting public health and health systems globally [1]. Paradoxically, the global health sector – hospitals, health services, and its medical supply chain – is responsible for around 5% of global net carbon emissions [2,3,4], thus inadvertently contributing to irreversible environmental changes and threatening human health and future generations. This carbon footprint is equivalent to the total CO2 emissions of entire countries such as India (7.1%) and Russia (4.7%) [5]. To fulfil international commitments to the Paris Climate Change Agreement and decarbonisation of healthcare systems around the world [6], the health sector must take a lead role in reaching net-zero emissions [1].
Carbon footprint modelling has been applied to health systems internationally to quantify the environmental impacts of healthcare services and activities [7]. This has helped determine the areas in which the most carbon emissions are produced and identify priority areas for strategic intervention [7]. For example, 62% of total health service emissions in the UK were from the supply chain, with 24% (of the total) from the direct delivery of care (e.g. on-site fossil fuel use, anaesthetics, inhalers). Life cycle assessments have identified emissions involved in different hospital departments or operations [8,9,10] that could be reduced simply and cheaply through, for example, reducing waste [11, 12], changing anaesthetic gases used [13], and reducing unnecessary testing [14] and imaging [15].
Since clinical activity itself accounts for 70–80% of the total carbon footprint of healthcare (not buildings, water, and waste) [16, 17] optimising how clinical care is delivered is a key component to decarbonising the health sector. Therefore, a crucial component to reducing the emissions of clinical care is individual behaviour change [18]. Encouraging a shift in clinical behaviour to avoid or replace carbon-intensive healthcare could result in significant health, carbon, and cost savings for the health system. For example, an existing NHS initiative that used prompt cards to ‘nudge’ anaesthetists away from using a potent anaesthetic agent (desflurane) and towards a lower carbon alternative (e.g., sevoflurane) resulted in the equivalent of 30,000 kg less CO2 per month for the hospital [19]. A Trainee-Led Research and Audit in Anaesthesia (TRA2SH) group have campaigned for hospitals in Australia and New Zealand to pledge to #DitchTheDes and remove desflurane from their formularies by 2025 (or sooner) [20]. In Australia, unnecessary Vitamin D testing (> 3 million tests per year) cost Medicare more than $87 million in 2020 and a carbon burden equivalent to 28,000–42,000 kg CO2e or driving approximately 160,000–230,000 km in a standard, petrol-fueled, passenger car, yet provided no net health benefit for patients [21]. Lastly, pathology and diagnostic imaging account for approximately 9% of healthcare’s carbon footprint in Australia [22]. Opportunities for intervening in this context include turning off scanners to reduce emissions from standby power and reducing ordering of unnecessary imaging or substituting high-impact imaging (e.g., MRI and CT) with lower-impact imaging (e.g., X-Ray and ultrasound) to reduce carbon and costs [15].
Behaviour change interventions are ‘coordinated sets of activities designed to change specified behaviour patterns’ [23]. Systematic reviews of behavioural interventions to reduce carbon emissions in office workplaces [24] and residential buildings [25] have shown that incentives given to individuals (both financial and non-financial) can be very successful, as well as interventions which change the physical environment in some way (such as fitting technologies) and social influences. However, these are lacking in the healthcare sector. It is widely recognised that interventions targeting clinicians are the most effective when implementing changes in the health setting [26], and that behaviour change interventions have demonstrated effectiveness in multiple areas of healthcare [27,28,29]. These types of interventions aim to change individual clinicians’ behaviour through a variety of methods. One framework for designing behaviour change interventions is the Behaviour Change Wheel (BCW) [23, 30] which has been used extensively in this setting [31, 32]. It characterises interventions and policies aiming to change behaviour and categorises barriers and facilitators to a particular behaviour change into three areas: capability, motivation, and opportunity (COM-B).
Despite the recent emergence of multiple studies estimating the carbon footprint of clinical activity and suggesting emissions reduction strategies via behaviour change [22, 33, 34], no reviews, to our knowledge, have explored the effectiveness of implemented behavioural change interventions, targeting clinicians, to reduce carbon emissions in health settings. To design and implement effective carbon reduction interventions in clinical care in the future, it is essential to identify and understand the nature and scope of existing initiatives internationally and the impact of those interventions have had on healthcare emissions.
This systematic review sought to answer the question: ‘What behaviour change interventions have been implemented in healthcare settings to encourage clinicians to reduce greenhouse gas emissions from their clinical activity?’ We will achieve this by identifying and synthesising global empirical evidence on behavioural change interventions implemented to reduce carbon emissions arising from clinical care provision. The findings of this review will inform the design and development of emissions-reduction interventions in healthcare settings – and ultimately support a shift towards more sustainable healthcare at this critical time for the environment, the future medical workforce, and the global population.
Methods
The study was registered on Prospero (ID number CRD42021272526) [35]. Study procedures are reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance [36].
Types of studies
See Table 1 for inclusion and exclusion criteria. Eligible study types included randomised and non-randomised controlled trials, controlled or uncontrolled before-and-after studies, case series, case studies, and audit. Conference proceedings were excluded initially before being re-introduced due to a limited number of full-text papers identified. No language restrictions were applied.
Types of interventions
Studies were included if they reported on a behaviour change intervention/s implemented in any clinical setting aimed at decreasing greenhouse gas emissions through changing the behaviour (clinical activity) of individual clinicians at their workplace. Interventions could have been initiated by clinicians or healthcare services and implemented in any healthcare setting including primary care clinics, hospitals, health clinics, allied health centres, or online.
Studies were excluded if they described interventions targeting supply chains/procurement (beyond individual clinician behavioural change) or interventions to reduce emissions outside of clinical activity in the healthcare setting. Studies that evaluated interventions designed primarily to address waste/recycling or water and/or energy use were also excluded. Comparisons of the intervention versus no intervention (usual practice) or another intervention were acceptable.
Outcomes
Our primary outcome was environmental impact (specifically, greenhouse gas emissions/carbon footprint) of clinical activity, measured or modelled directly or indirectly (e.g. estimated from costs, waste and/or energy consumption). Secondary outcomes included financial costs and change in clinical activity (e.g. reduction in anaesthetic gas use or pathology test ordering).
Search strategy
Six databases were searched (Medline (via OvidSP), Scopus, EMBASE (via OvidSP), Cinahl, Web of Science (Core Collection), and ABI-Inform) for all studies up to November 4, 2021. The search was repeated to update the results on February 7, 2022. The search terms were based on a previous similar review [24], with additional terms based on known relevant papers and librarian suggestions [from the Faculty of Medicine and Health at the University of Sydney]. The complete list of search terms is included in Table 2 below, and the search strategy is shown in Additional file 1: Appendix 1. The terms were searched within article title, abstract, and keywords. Once the final selection was complete, references and citations of full-text papers were also searched, and potentially relevant articles were reviewed.
Study selection
We downloaded references identified in searches and uploaded them to Covidence, an online software platform and primary screening and data extraction tool. Two reviewers (CB, MBP) independently conducted title and abstract screening using the inclusion and exclusion criteria to determine suitability. Any conflicts were resolved by discussion with two additional reviewers (KP and TD). All reviewers assessed the full text of the remaining papers.
Once this process was completed, a small number (n = 6) of studies were found to be relevant to the review. After a discussion amongst the reviewers, it was decided that we would also include conference abstracts of relevant studies that may be published in the future because of the limited pool of studies. Attempts were made to contact authors of all included conference abstracts to confirm that the study had not (yet) been published.
Data extraction
Three reviewers (MP, TD, CB) used a pre-determined data extraction template on Excel to extract data from the included full-text papers and conference abstracts. The data extracted from the included studies were: year, country, study design, study population, research question/aim, description of the intervention, measured outcomes (change in CO2e, change in clinical activity e.g. anaesthetic gas usage, change in cost), and behaviour change techniques used.
One reviewer (CB), with training in applying Michie et al.’s behaviour change technique taxonomy [37] to published methods, extracted the behaviour change techniques from the methods section of the full-text papers and as much as possible from methods described in the conference abstracts. We used this taxonomy as it relates to a model of behaviour change commonly used when designing interventions, the Capability-Opportunity-Motivation-Behaviour (COM-B) model [23]. Figure 1 demonstrates how some of the behaviour change techniques, from the taxonomy of 93 techniques, are situated in the COM-B model.
Assessing the quality of the included studies
For the full-text papers, we used a risk of bias tool for single-arm observational studies of interventions using a modified checklist based on previously-published checklists and evidence-based medicine criteria [38, 39], adapted from [40] (see Additional file 1: Appendix 4 for the tool used). Two reviewers independently rated each study for risk of bias (CB, MBP) and conflicts that arose were discussed with two further reviewers (KP, TD) until consensus was reached. The Template for Intervention Description and Replication (TIDieR) checklist [41] was completed for each study (TD, CB).
Data synthesis
We anticipated that meta-analysis to calculate the pooled effects of the interventions would not be possible because of heterogenous data reported across the studies and measurement of outcomes. Study findings were therefore synthesised thematically in tabular form.
Results
Description of studies
Search results
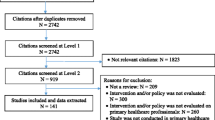
The PRISMA diagram (Fig. 2) shows the search process and results. In November 2021, 5,956 database results were assessed for eligibility. In February 2022, the search was repeated, and an additional 1,006 database results were assessed. The 144 citations and references from the full-text papers included were also reviewed. We identified a total of 4,675 papers (after duplicates were removed). After excluding irrelevant papers based on abstract screening, the full texts of 10 studies were assessed, with six eligible studies identified. Of 309 conference abstracts identified in the search, 14 were found to be eligible for inclusion. The study team emailed lead authors from the conference abstracts to request whether they had progressed to full-text papers. 3 out of the 14 replied and confirmed that they had not. Study details and outcomes are summarised in Tables 3, 4, 5, 6 and 7.
Full text papers
Characteristics of included studies
All studies described interventions in hospital settings. Four of the six included studies were undertaken in hospital anaesthesia departments in the USA [42, 45, 46] (3/6), and UK [44] (1/6). These studies (4/6) focused on reducing emissions of volatile anaesthetic agents, for example by encouraging anaesthetists to use a low flow anaesthesia technique or reducing the use of specific anaesthetic gases – such as desflurane—that have a particularly potent global warming potential. The remaining two studies (2/6) aimed to reduce unnecessary test ordering in a paediatric cardiology ward in the UK and a hospital in Australia (Regan et al. focused on biochemistry [43] and McAlister et al. on pathology [47]).
All included studies used a before-after (pre-post) intervention study design. The main outcome was most commonly measured at baseline for the whole hospital department, followed by an intervention administered to the staff in the department, and the outcome measured again, often many times over a period of months (range of 2 months to 4 years). However, one study [47] measured the effect of the intervention retrospectively, rather than designing the intervention and following its outcomes over time.
The interventions themselves included many different facets. Some common themes were: adding reminders onto machines for which/how much gas to use, sending personalised feedback to individuals based on performance (e.g. how much gas had been used in the last month, and the target), physically changing the canisters in the rooms so that it is more difficult to use the unwanted gas, gathering the team regularly for updates in person, and putting up educational posters. For more detail of the characteristics of included studies’ interventions, the completed TIDieR checklist [41] for each study is in Additional file 1: Appendix 6.
Behaviour change techniques (BCTs) used in interventions
The studies in this review used very similar methods to change behaviour. Table 5 shows the BCTs coded from the full-text papers (see Additional file 1: Appendix 2 for more detail, and Table 7 for definitions of the techniques included). Five to 10 BCTs were used in each study; all included papers used the techniques of (1) credible source, as they all took place in a hospital setting and interventions were run by colleagues of participants, and (2) instruction on how to perform a behaviour, such as a guide to using new machines to deliver anaesthesia.
Most of the studies included the BCTs of social support (5/6; e.g. encouraging staff), salience of consequences (5/6; e.g. showing carbon emissions reductions as equivalent miles driven by a car), adding objects to the environment (5/6; e.g. posters put up), prompts or cues (5/6; e.g. reminder labels on machines), feedback on outcome of behaviour (4/6; e.g. by sending email updates on progress), and information about environmental consequences (4/6; e.g. describing environmental impacts of the emissions). For a more detailed table of the BCT coding, see Additional file 1: Appendix 2.
Outcomes from the interventions
Table 3 summarises primary and secondary outcomes measured across the studies, which were change in CO2e (both percentage and absolute difference), change in cost, and change in clinical activity (e.g., anaesthetic gas use or pathology test ordering). All studies reported success in their interventions; however, only two reported any statistical analysis to measure the size and significance of the effect [42, 47].
In terms of the primary outcome of CO2e reduction, four studies calculated a reduction in emissions as a result of their intervention. Zuegge et al. reported a reduction of 2,865,430 kg CO2e per year, calculating CO2e using the global warming potential (GWP) of the gas and the mass emitted [45]. They also reported a CO2e per case of 163 kg before their intervention, versus 58 kg 3 years later, in 2015 [45]. Glenski & Levine calculated a reduction of 28.5 MT CO2e per year compared to before their intervention, using a formula based on number of Sevoflurane bottles, their density and the GWP [46]. McAlister et al. reported a reduction of 53 g CO2e (P < 0.001) per admission using an analysis which included many factors (e.g., current energy suppliers, differences in power when a test is taken) [47]. Regan et al. [43] estimated a 10,042 kg CO2e reduction per year attributable to a reduction in test ordering after their intervention, using estimates from the UK government’s carbon emissions indicator [62], which convert price to CO2.
Of those studies that aimed to change anaesthetic gas use [42, 44,45,46], all four reported a reduction in emissions after the intervention, through for example, increasing uptake of low flow anaesthesia or replacing more potent inhalational anaesthesia with lower emissions alternatives. Epstein et al. [42] reported a statistically significant reduction in Sevoflurane use (P < 0.001) and a non-significant decrease in the number of gas bottles purchased (P = 0.81), when comparing 8-week periods before and after their intervention. Carter et al. [44] reported an 18% reduction in volatile gas bottles ordered in the year after their intervention compared to the year before; Zuegge et al. [45] a 55% reduction in Desflurane use (and a 16% increase in Sevoflurane use) in the yearly totals before and after their intervention; and Glenski & Levine [46] reported a 20% decrease in Sevoflurane bottles used per month (and a 25% decrease in the amount of Sevoflurane used per anaesthetic performed) before their intervention compared to 9 months later.
Two studies described the effect of interventions that aimed to reduce the cost and environmental impact of unnecessary test ordering. Regan et al. [43] reported a significant reduction in percentage of biochemical tests ordered, as well as an increase in use of more efficient C005 tests as a percentage of total biochemistry tests ordered, from 13 to 45%. McAlister et al. [47] found a 10% reduction in rate of pathology collections (P < 0.001) after the intervention.
Five of six studies also found a reduction in financial cost. Epstein et al. [42] reported a non-significant decrease in the cost of absorbent purchases (P = 0.81). Carter et al. [44] reported a 25% decrease in spending on volatile agents compared with the same period the previous year. Zuegge et al. [45] calculated savings of $25,000 per month after their intervention. McAlister et al. [47] also found that fees per admission were $22 lower (P = 0.001) after their intervention, and for Regan et al. [43] biochemistry test cost fell by £533 (23%) per month after their intervention.
Conference abstracts
Characteristics of included studies
Almost all the studies (13/14) described in the conference abstracts were conducted in the UK, with the remaining one from Australia [55]. Most of the studies (13/14) were focused on anaesthetic gas usage, with only one aiming to reduce emissions of respiratory inhalers [60]. In terms of methodology, all abstracts described before-after (pre-post) study design. One of the studies [60] was aimed at GPs; the rest targeted anaesthetists in hospitals (13/14).
As limited detail was included in the abstracts, interventions were not described as thoroughly as in the full-text papers. However, some common characteristics of the interventions described were: participant feedback on progress via, for example, email updates, visual prompts such as stickers on machines, education provided through presentations and posters, and physically removing the unwanted gas (usually Desflurane) from anaesthetic machines. The one intervention that focused on inhalers was slightly different [60]. Here, GPs were provided with educational materials on the environmental benefits of using less carbon intensive inhalers, as well as a decision support tool to use with patients and prompts when prescribing inhalers.
Behaviour change techniques (BCTs) used in interventions
Table 6 includes as many BCTs as possible from the abstracts (see Additional file 1: Appendix 3 for more detail, and Table 7 for definitions of the techniques included). Like the full text papers, the conference abstracts also all included the technique of ‘credible source’. Most also included information about environmental consequences (8/14; e.g., presentation on environmental impacts). Also common were instruction on how to perform a behaviour (7/14; e.g., a website with education and instructions), and prompts or cues (7/14; e.g., reminders on machines). For a more detailed summary, see Additional file 1: Appendix 3.
Outcomes from the interventions
Primary and secondary outcomes of the conference abstracts are summarised in Table 4, where detail was available. Only one study reported statistical analyses as a measure of effect [58]. All reported an effect on outcomes following the intervention. Nine of the 13 anaesthetic gas studies found a reduction in gas use, and the study aiming to reduce Ventolin inhaler prescribing [60] achieved a 31% reduction in inhalers being prescribed after their intervention, and improved patient satisfaction. Similar to the full-text papers, 7/14 abstracts also reported a reduction in financial cost and 8/14 a reduction in CO2e emissions.
Quality of the evidence
Risk of bias assessment for the 6 included studies is reported in Table 8; definitions of the risk of bias criteria and detailed rationale per study are provided in Additional file 1: Appendices 4 and 5. Overall, all studies scored at least one item as unclear or at risk of bias.
Internal validity
Selection bias was assessed as low risk for all studies, as the total eligible population (e.g., entire hospital department) was included in the intervention (although none explored how many individuals within the departments were engaged with the intervention). Study outcomes were also assessed in > 95% of the study group of interest, meaning that risk of attrition bias was judged to be low for the included studies. All 6 studies were judged to be at high risk of detection bias because all studies did not have blinded outcome assessors (except McAlister et al., however, in this study, they also were not blinded to the investigated determinant [47]). Regarding adjustment for confounding factors, four of the six studies [43,44,45,46] did not report adjusting for any confounders. The remaining two did account for some but not fully. McAlister et al. included sensitivity analyses adjusting for age, sex, NWAU19 and type of admission but reported in their limitations that they did not capture all confounding factors due to a lack of control in the study [47]. Epstein et al. conducted a sensitivity analysis on the financial implications of changing gases, however not for any other of their hypotheses [42].
External validity
Reporting bias was not well defined for three studies: Carter et al. [44] and Zuegge et al. [45] did not adequately define the number of participants or the intervention. Glenski & Levine defined the number of participants (number of people in the anaesthesiology department) but did not define the intervention adequately enough [46]. Epstein et al. [42], Regan et al. [43] and McAlister et al. defined the intervention but not the number of participants, as they did not include the number of people in the department being targeted by the intervention [47]. All studies defined the follow up and outcome adequately. Despite four of the studies also defining the method of analysis and quantifying the effect of the intervention [42, 45,46,47], two studies [43, 44] did not perform any kind of rigorous statistical analyses.
Discussion
Principal results
Six studies that described behaviour change interventions to reduce greenhouse gas emissions in healthcare settings were identified for inclusion in this review. 14 conference abstracts were also identified that met eligibility criteria. All studies took place in hospitals. The most common techniques included in the behaviour change interventions were: credible source, social support, salience of consequences, adding objects to the environment, and prompts or cues. Four looked at changing or reducing anaesthetic agents, a key carbon emitter, with their interventions resulting in 16–55% reduction in gas used. The other two aimed to reduce unnecessary test ordering to lower emissions; these two interventions were also successful in their aims.
However, not all studies measured or calculated CO2e, despite a reduction in emissions being their goal. Those studies that did report a reduction, for example Regan et al.’s calculated reduction of 10,042kg [43], were not necessarily reporting an accurate estimate of carbon emissions saved because their estimate is based on a conversion of cost to carbon emissions. While cost-based estimates of carbon emissions are widely used, they are less accurate than emissions estimate from life cycle assessment for a range of reasons including some components of the life cycle of the product/service may be omitted, and the assumption of a linear relationship between costs and carbon emissions may not always hold. One study [47] used rigorous methodology (i.e., environmental impact was based on previous LCA), however others used simple calculations which may not account for all CO2e emissions. Therefore, the quantifiable reductions in number of tests ordered and amount of harmful gases (e.g. desflurane) used may be a better indicator of reduced environmental impact.
Strengths and limitations
As far as the authors are aware, this review is the first to look at behaviour change interventions to reduce carbon emissions in healthcare settings. It provides a valuable starting point for others to design interventions in similar contexts as it demonstrates the type and scope of behavioural change interventions implemented internationally to address the carbon footprint of clinical care. It shows interventions to date have targeted anaesthetic gas use or unnecessary pathology test ordering in hospital settings only. A strength of this study is our systematic mapping of behavioural change techniques used in each study. Other strengths include the extensive search strategy and large number of titles and abstracts screened and having multiple assessors to extract data and conduct risk of bias assessments independently.
However, only 6 studies were eligible to be included in this review, and eligible conference abstracts (which were included to illustrate some local initiatives that have been undertaken by clinicians in their clinical settings) are unlikely to be published in academic journals in the future. Furthermore, the 6 included studies were very similar in methodology and interventions. None of the studies randomised groups to different interventions or had a control group. The only study design was uncontrolled before-after. In order to conclude that the interventions were indeed effective, we need gold standard RCTs to truly measure their effectiveness. As statistical analyses was not performed in most of the included full-text papers, we cannot be sure of how much of an improvement the interventions caused and whether this was statistically significant.
Another limitation is that the studies introduced new aspects of the intervention as it progressed, with limited or no effort made to evaluate the effects of each component, so it remains unclear which aspect of the intervention produced the largest effect on the outcomes measured. The studies used multiple behavioural change techniques, for example adding objects to the environment and providing tailored feedback, but did not compare any, or use them systematically or strategically. Therefore, it is not clear which techniques were the most effective, or indeed if any were counter-intuitive.
None of the studies appear to have designed their intervention using a model, theory or framework which is recommended when designing successful behaviour change interventions [63, 64]. All included studies did not reference or define the barriers and facilitators involved in the behaviour they were attempting to change. This is best practice when aiming to change behaviour, so as to ensure the intervention is targeting the barriers to behaviour change [23].
Comparison to prior work
Previous work in other areas has also found that the behaviour change techniques of incentives and social influences work well, as well as changing the environment [24, 25]. This review demonstrates success using social support and adding or removing objects in the environment in the healthcare setting too. However, incentives were only used in one of the studies [43], and this was in combination with 9 other BCTs [43], so it isn’t clear how effective this specific technique is in this setting.
This review shows that very little work has been done to date to develop and evaluate behaviour change interventions to reduce the carbon footprint of healthcare. Yet this area is in urgent need of attention if commitments by countries at the COP26 meeting to move towards low carbon healthcare systems are to be met [65]. Measuring carbon emissions from healthcare is challenging, and methods for doing this work accurately, while well developed in other sectors, are only now being applied to healthcare (e.g., [14, 15, 66, 67]). The gold standard method is the Life Cycle Assessment (LCA), as described by ISO 14040 and ISO 14044. Most of the studies in our systematic review did not measure carbon emissions directly based on LCA, but estimated them, for example from changes in anaesthetic gas usage. This approach is likely to be valid, as in turn those anaesthetic gases have been thoroughly studied in previous LCAs. One study [47] was able to estimate carbon emissions from a previous LCA of common pathology tests. Such studies are currently rare in healthcare. Other studies in our review, which estimated carbon emissions from costs data, are likely less accurate in their estimates of CO2e emissions. This highlights the urgent need for LCAs of more healthcare products and services. This work will be needed for better measurement of the outcomes of behavioural interventions to reduce the carbon footprint of healthcare.
Future research
As most of the interventions of the included studies were designed and run by clinicians themselves, we suggest that there is strong clinician interest and engagement with this issue, which is promising for future research being implemented and maintained in hospitals. However, future research should aim to run these interventions in a systematic and evidence-based way. One method would be to use the COM-B model [23], a tool for designing interventions based on tackling the capability, opportunity and motivational barriers for individuals to perform a particular behaviour. Once the barriers are understood, the relevant BCTs can be applied which target those barriers. Future interventions should also test a select few techniques at a time only, with a control or comparison group, as doing so would give a clearer indication of which specific BCTs are effective, resulting in more practical outcomes that can be implemented in other contexts. High quality evidence is necessary to direct change in clinical behaviour, and close attention must be paid to local contexts (e.g. resources, culture and values, receptivity) for successful implementation of evidence-based interventions into practice, that best support healthcare decarbonisation [33, 68]. Clinicians could be supported to partner with researchers to improve research design, quality, and long-term evaluation.
We also found that most interventions to reduce emissions in healthcare have focused on anaesthesia. This is a priority area due to the high global warming potential of anaesthetic gases – prioritisation which has been made possible by previous LCA studies of these and other greenhouse gases. The behaviour changes observed in these studies represent big wins in terms of large-scale emissions reduction. However, rigorous studies with well-designed interventions are also needed in other areas of clinical practice both in and outside of hospital settings within health care. Future research should investigate what types of interventions could work in other settings, such as primary care or allied health, where there are likely to be different barriers and facilitators to behavioural change.
Conclusion
To conclude, this review demonstrates that there has been little published research on behaviour change interventions to reduce carbon emissions in healthcare. Those that do exist have all used a before-after design and have tested multiple interventions simultaneously, limiting the reliability of their findings, and have focused on either anaesthetic gas use or test ordering. Future research should be more systematic when designing interventions in this space, and test more rigorously their impact. More interventions should also be done in other areas of healthcare, such as in primary care or other hospital settings.
Availability of data and materials
The datasets supporting the conclusions of this article are included within this published article and its supplementary information files.
Abbreviations
- BCTs:
-
Behaviour Change Techniques
- CO2e:
-
Carbon dioxide equivalent
- COM-B model:
-
Capability, Opportunity, Motivation, Behaviour Model
- COP26:
-
Conference of the Parties 26
- LCA:
-
Life Cycle Assessment
- NWAU19:
-
National Weighted Activity Units, 2019
References
World Health Organization. Climate change and health. Available from: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health. Accessed 31 Aug 2022.
Pichler P-P, Jaccard IS, Weisz U, Weisz H. International comparison of health care carbon footprints. Environ Res Lett. 2019;14(6):064004.
Lenzen M, Malik A, Li M, Fry J, Weisz H, Pichler P-P, et al. The environmental footprint of health care: a global assessment. Lancet Planet Health. 2020;4(7):e271–9.
Health Care Without Harm in collaboration with ARUP. Health care’s climate footprint: how the health sector contributes to the global climate crisis and opportunities for action 2019. Available from: https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_090619.pdf. Accessed 31 Aug 2022.
Worldometers. CO2 emissions by country. Available from: https://www.worldometers.info/co2-emissions/co2-emissions-by-country/. Accessed 31 Aug 2022.
Department of Industry S, Energy and Resources. International climate change commitments. Available from: https://www.industry.gov.au/policies-and-initiatives/international-climate-change-commitments. Accessed 31 Aug 2022.
Booth A. Carbon footprint modelling of national health systems: opportunities, challenges and recommendations. Int J Health Plann Manage. 2022;37(4):1885–93.
McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth. 2020;125(5):680–92.
Tan E, Lim D. Carbon footprint of dermatologic surgery. Australas J Dermatol. 2021;62(2):e170–7.
Brown LH, Buettner PG, Canyon DV, Mac Crawford J, Judd J. Estimating the life cycle greenhouse gas emissions of Australian ambulance services. J Clean Prod. 2012;37:135–41.
Petre M-A, Malherbe S. Environmentally sustainable perioperative medicine: simple strategies for anesthetic practice. Can J Anesth. 2020;67(8):1044–63.
de Sa D, Stephens K, Kuang M, Simunovic N, Karlsson J, Ayeni OR. The direct environmental impact of hip arthroscopy for femoroacetabular impingement: a surgical waste audit of five cases. J Hip Preserv Surg. 2016;3(2):132–7.
Thiel CL, Woods NC, Bilec MM. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am J Public Health. 2018;108(S2):S158–64.
McAlister S, Barratt AL, Bell KJL, McGain F. The carbon footprint of pathology testing. Med J Aust. 2020;212(8):377–82.
McAlister S, McGain F, Petersen M, Story D, Charlesworth K, Ison G, et al. The carbon footprint of hospital diagnostic imaging in Australia. Lancet Reg Health West Pac. 2022;24:100459.
Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5(2):e84–92.
Malik A, Lenzen M, McAlister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health. 2018;2(1):e27–35.
Australian Medical Association and Doctors for the Environment Australia. AMA and DEA outline plan to reduce healthcare’s carbon footprint to top health bureaucrats 2022. Available from: https://www.ama.com.au/ama-rounds/25-february-2022/articles/ama-and-dea-outline-plan-reduce-healthcares-carbon-footprint. Accessed 31 Aug 2022.
Greener NHS. Putting anaesthetic-generated emissions to bed. Available from: https://www.england.nhs.uk/greenernhs/whats-already-happening/putting-anaesthetic-generated-emissions-to-bed/. Accessed 31 Aug 2022.
Trainee-Led Research and Audit in Anaesthesia for Sustainable Healthcare. Why are we still using desflurane? Available from: https://www.tra2sh.org/refuse-desflurane. Accessed 31 Aug 2022.
Breth-Petersen M, Bell K, Pickles K, McGain F, McAlister S, Barratt A. Health, financial and environmental impacts of unnecessary vitamin D testing: a triple bottom line assessment adapted for healthcare. BMJ Open. 2022;12(8):e056997.
Malik A, Padget M, Carter S, Wakiyama T, Maitland-Scott I, Vyas A, et al. Environmental impacts of Australia’s largest health system. Resour Conserv Recycl. 2021;169:105556.
Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):1–12.
Staddon SC, Cycil C, Goulden M, Leygue C, Spence A. Intervening to change behaviour and save energy in the workplace: a systematic review of available evidence. Energy Res Soc Sci. 2016;17:30–51.
Khanna TM, Baiocchi G, Callaghan M, Creutzig F, Guias H, Haddaway NR, et al. A multi-country meta-analysis on the role of behavioural change in reducing energy consumption and CO2 emissions in residential buildings. Nat Energy. 2021;6(9):925–32.
Cliff BQ, Avancena AL, Hirth RA, Lee SYD. The impact of Choosing Wisely interventions on low-value medical services: a systematic review. Milbank Q. 2021;99(4):1024–58.
Chauhan BF, Jeyaraman M, Mann AS, Lys J, Skidmore B, Sibley KM, et al. Behavior change interventions and policies influencing primary healthcare professionals’ practice—an overview of reviews. Implement Sci. 2017;12(1):1–16.
Gardner B, Whittington C, McAteer J, Eccles MP, Michie S. Using theory to synthesise evidence from behaviour change interventions: the example of audit and feedback. Soc Sci Med. 2010;70(10):1618–25.
Keyworth C, Epton T, Goldthorpe J, Calam R, Armitage CJ. Delivering opportunistic behavior change interventions: a systematic review of systematic reviews. Prev Sci. 2020;21(3):319–31.
Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions 1st ed, vol. 1003. Great Britain: Silverback Publishing; 2014. p. 1010.
Isenor JE, Bai I, Cormier R, Helwig M, Reeve E, Whelan AM, et al. Deprescribing interventions in primary health care mapped to the behaviour change wheel: a scoping review. Res Social Adm Pharm. 2021;17(7):1229–41.
Richardson M, Khouja CL, Sutcliffe K, Thomas J. Using the theoretical domains framework and the behavioural change wheel in an overarching synthesis of systematic reviews. BMJ Open. 2019;9(6):e024950.
McGain F, Naylor C. Environmental sustainability in hospitals–a systematic review and research agenda. J Health Serv Res Policy. 2014;19(4):245–52.
MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1(9):e381–8.
Breth-Petersen M, Batcup C, Dakin T, Pickles K, Barratt A, Newell B, et al. Behavioural change interventions for environmentally sustainable clinical activity: a systematic review of the available evidence. Prospero. 2021;2021:CRD42021272526.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. 2021;134:103–12.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Grimes DA, Schulz KF. Cohort studies: marching towards outcomes. Lancet. 2002;359(9303):341–5.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
van Deuren S, Boonstra A, van DulmendenBroeder E, Blijlevens N, Knoop H, Loonen J. Severe fatigue after treatment for childhood cancer. Cochrane Database Syst Rev. 2020;2020(3):CD012681.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:1687.
Epstein RH, Dexter F, Maguire DP, Agarwalla NK, Gratch DM. Economic and environmental considerations during low fresh gas flow volatile agent administration after change to a nonreactive carbon dioxide absorbent. Anesth Analg. 2016;122(4):996–1006.
Regan W, Hothi D, Jones K. Sustainable approach to reducing unnecessary combined biochemistry tests on a paediatric cardiology ward. BMJ Open Qual. 2018;7(4):e000372.
Carter LA, Oyewole M, Bates E, Sherratt K. Promoting low-flow anaesthesia and volatile anaesthetic agent choice. BMJ Open Qual. 2019;8(3):e000479.
Zuegge KL, Bunsen SK, Volz LM, Stromich AK, Ward RC, King AR, et al. Provider education and vaporizer labeling lead to reduced anesthetic agent purchasing with cost savings and reduced greenhouse gas emissions. Anesth Analg. 2019;128(6):e97–9.
Glenski TA, Levine L. The implementation of low-flow anesthesia at a tertiary pediatric center: a quality improvement initiative. Pediatr Anesth. 2020;30(10):1139–45.
McAlister S, Smyth B, Koprivic I, Luca Di Tanna G, McGain F, Charlesworth K, et al. Carbon emissions and hospital pathology stewardship: a retrospective cohort analysis. Int Med J. 2021. https://doi.org/10.1111/imj.15622. Accessed 31 Aug 2022.
Patel N, Maguire D, Dexter F, Epstein RH. Reduction of fresh gas flow during administration of volatile anesthetic agents via monthly individualized e-mail feedback. In: Anaesthesia and analgesia. Pennsylvania: Lippincott Williams & Wilkins. 2014;119(6S_Suppl):1–158. https://journals.lww.com/anesthesia-analgesia/Citation/2014/12001/Abstracts_of_Papers_Presented_at_the_2014_Annual.1.aspx.
Boyle A, Coleman A, Barker K, Baraclough D. A grassroots approach to the greenhouse effect: implementing recent guidance from the AAGBI and RCoA. In: Anaesthesia. New Jersey: Wiley; 2018. p. 22.
Danby J, Erringtonn T, Baxter I, Chishti A, Sweenie A. Lowering the carbon footprint of our anaesthetics-using a Golf GTI. In: Anaesthesia. New Jersey: Wiley; 2018. p. 41.
Jani S, Kalla A. Economy and ecology friendly anaesthesia. In: Anaesthesia. New Jersey: Wiley; 2018. p. 111.
Hickman J, Molyneux M. The EnVol (Environmental Volatile’s) project: reducing the impact of volatile anaesthetics at University Hospitals Bristol NHS Foundation Trust. In: Anaesthesia. New Jersey: Wiley; 2019. p. 11.
Lawson C, Baxter I. Transforming anaesthetic practices and reducing carbon emissions: how much of this can we achieve with behavioural nudges? In: Anaesthesia. New Jersey: Wiley; 2019. p. 58.
Self J, Eveleigh M. Ditching our desflurane addiction to reduce the environmental impact of anaesthesia-changing practice with minimal intervention. In: Anaesthesia. New Jersey: Wiley; 2019. p. 89.
Benness M, Doane M. Anesthetists are primed to leap into action on climate change. 2021 virtual Australian and New Zealand College of Anaesthestists annual scientific meeting; Melbourne, Australia. Anaesth Intensive Care. 2021;49(25).
Carta S, Biela C, Barr J. Cleaning up our act: volatile anaesthesia post-pandemic. In: Anaesthesia. 2021. p. 28.
Hirst J, Mangham T, Lie J. Greener anaesthesia. In: Anaesthesia and analgesia. Pennsylvania: Lippincott Williams & Wilkins; 2021. p. 1577–578.
Jameson R, Young S. Raising the standard: lowering the flow. Glasgow Royal Infirmary trainee group collaborative audit. Anaesthesia. 2021;76:45–45. NJ USA: Wiley.
Kirkman J, Mathur R, McHugh C, Whitaker M. Volatile anaesthesia: reducing the financial cost and environmental impact by reducing desflurane usage. In: Anaesthesia. New Jersey: Wiley; 2021. p. 21.
Roome C, Bush O, Steinback I, Langran T, Patel S. Reducing the environmental impact of inhaler use and disposal within paediatrics and the local community. Arch Dis Child. 2021;106(Suppl 1):A1–514.
Wilson M, Clark A. Continued reduction in volatile anaesthetic agent use after presentation of adjusted usage rates. In: Anaesthesia. New Jersey: Wiley; 2021. p. 106.
United Kingdom Government. UK and England’s carbon footprint to 2019. Available from: https://www.gov.uk/government/statistics/uks-carbon-footprint.
Bartholomew LK, Mullen PD. Five roles for using theory and evidence in the design and testing of behavior change interventions. J Public Health Dent. 2011;71:S20–33.
Michie S, Fixsen D, Grimshaw JM, Eccles MP. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement Sci. 2009;4:40. https://doi.org/10.1186/1748-5908-4-40.
Wise J. COP26: Fifty countries commit to climate resilient and low carbon health systems. BMJ. 2021;375:n2734. https://doi.org/10.1136/bmj.n2734. (Published 09 November 2021).
Sherman JD, Raibley LA IV, Eckelman MJ. Life cycle assessment and costing methods for device procurement: comparing reusable and single-use disposable laryngoscopes. Anesth Analg. 2018;127(2):434–43.
Hu X, Pierce JT, Taylor T, Morrissey K. The carbon footprint of general anaesthetics: a case study in the UK. Resour Conserv Recycl. 2021;167:105411.
Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci. 2008;3:1–2.
Acknowledgements
Not applicable.
Funding
This study was funded through the NHMRC Centre of Research Excellence, APP2006545.
Author information
Authors and Affiliations
Contributions
CB was involved with designing the review, developed and ran the literature search, uploaded literature to Covidence, conducted title and abstract screening, assessed full text of included literature, data extraction, BCT extraction, rated risk of bias for included literature, completed TIDieR checklist, lead the drafting of the manuscript. MBP conducted title and abstract screening, assessed full text of included literature, contacted conference abstract authors, extracted data, rated risk of bias for included literature, and drafted sections of the manuscript. TD attended discussions to resolve conflicts relating to title and abstract screening and risk of bias assessments, assessed full text of included literature, contacted conference abstract authors, extracted data, completed TIDieR checklist, and drafted sections of the manuscript. AB conceived and designed the review, obtained funding, approved the literature search, and critically revised the manuscript. FM approved the literature search, and critically revised the manuscript. BN contributed valuable suggestions throughout the project and critically revised the manuscript. KP conceived and designed the review, coordinated the running of the study, developed the literature search, led all discussions around resolving conflicts relating to title and abstract screening and risk of bias assessments, assessed full text of included literature, and drafted and critically revised the manuscript. All authors read and approved the final manuscript.
Authors’ information
All authors have training and experience in health services research (behavioural science, public health, psychology, clinical and public health epidemiology). FM is a currently employed anaesthetist/intensive care physician, and member of the ANZCA Environmental Sustainability Working Group and Doctors for the Environment Australia.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Full search strategy. Appendix 2. BCTs full codes from papers. Appendix 3. BCTs full codes from abstracts. Appendix 4. Risk of bias information. Appendix 5. Risk of bias more detailed table. Appendix 6. TiDIER table.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Batcup, C., Breth-Petersen, M., Dakin, T. et al. Behavioural change interventions encouraging clinicians to reduce carbon emissions in clinical activity: a systematic review. BMC Health Serv Res 23, 384 (2023). https://doi.org/10.1186/s12913-023-09370-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09370-2