Abstract
Background
Stroke has one of the biggest burden of disease in Thailand and all health regions have been tasked to develop their service delivery to achieve the national key performance indicators set out by the Thai service plan strategy 2018–2022. Our aim was to characterise stroke services and hospital facilities by investigating differences in facilities across different hospital levels in Thailand.
Methods
Self-complete questionnaires were distributed to 119 hospitals in 12 health regions between November–December 2019. Participants were health professionals whose main responsibilities are related to stroke service provision in their hospital. Descriptive statistics were used to report differences of stroke service provision between advanced-level, standard-level and mid-level referral hospitals.
Results
Thirty-eight (32% response rate) completed questionnaires were returned. All advanced-level, standard-level (100%) and 55% of mid-level referral hospitals provided stroke units. Neurologists were available in advanced-level (100%) and standard-level referral hospitals (50%). Standard-level and mid-level referral hospitals only had a quarter of rehabilitation physicians compared to advanced-level referral hospital. Home-based rehabilitation was provided at 100% in mid-level but only at 16% and 50% in advanced-level and standard-level referral hospitals.
Conclusions
Setting up a stroke unit, as a national goal that was set out in the service plan strategy 2018–2022, was achieved fully (100%) in advanced-level and standard-level referral hospitals including key essential supportive components. However, capacity in hospitals was found to be limited and stroke service delivery needs to be improved especially at mid-level referral hospitals. This should include regular organisational surveys and the use of electronic records to facilitate monitoring of clinical/health outcomes of patients.
Similar content being viewed by others
Background
In Thailand, stroke is ranked second among the top ten causes of disability-adjusted life years [1] and stroke mortality rates (per 100,000 population) increased from 38.7 to 47.1 between 2014 and 2018 [2]. The stroke mortality rate in Thailand remains above the national key performance indicators (KPIs) [3]. To reduce the burden of stroke, the Thai ministry of public health (MOPH) developed national KPIs of stroke service delivery through their service plan strategy 2018–2022 according to hospital level.
The service plan strategy classifies the provinces in Thailand into 12 health regions (Additional file-Fig. S1). Each health region comprises of 4–8 provinces and serves 3–5 million people. Every health region has an authority to design their service delivery systems. As the MOPH considers the improvement of service provision in terms of health regions, hospitals in the same health region have to work together under the concept of a seamless health service network, self-contain and referral hospital cascade [3, 4]. Hospitals in all heath regions are grouped into different levels. A classification and numbers of referral hospitals is provided in supplementary materials (Additional file-Table S1 and Table S2).
Stroke care included stroke service delivery via the stroke fast track system which can include emergency medical services [5] or a ‘drip-and-ship’ model from spoke to hub hospital for thrombolytic treatment [6]. Spoke hospitals can be mid-level referral hospitals depending on capacity, while hub hospitals are mostly mid-level to advanced-level referral hospitals [7, 8]. For in-hospital care, thrombolysis treatment can be prescribed under supervision of a hub network. Some hospitals do not have a stroke unit (SU) but a stroke corner (SC) - a specialised area in in-patient wards, where healthcare professionals are able to provide more intensive treatments. Some hospitals provide in-patient rehabilitation services after the acute-phase or refer patients back to their contracted hospital for either outpatient rehabilitation or home visits. Village health volunteers (VHVs) from local communities play an important role in offering home visits as well as promoting primary health care [9, 10].
In terms of KPIs, the strategy stipulates that, in 2018, SU should be the standard of care and should be available in all advanced-level, and in 80% of standard-level referral hospitals within each health region [11]. All mid-level referral hospitals should establish rehabilitation units to reduce over-crowding of stroke care in advanced-level and standard-level referral hospitals and to increase capacity and accessibility of rehabilitation in rural areas [9, 10].
Following regular reviews, this was updated in 2019, and the service plan strategy stipulated that all advanced-level and standard-level referral hospitals have to set up SU while for mid-level referral hospitals this would be based on their performance (Table 1) [12].
Challenges in the provision of stroke services in Thailand remain, namely, a low rate of thrombolytic therapy with huge variation between health regions in terms of patterns of care and prescribing [13], limited stroke rehabilitation services in several regions, limited resources and infrastructure in provincial and rural areas [8, 14], A global observational study across 28 countries, included Thailand, (the INTERSTROKE study) [15] emphasised that poorer access to investigations, treatments, and services was found in low- and middle-income countries compared to high-income countries. Our aim was to characterise stroke services and hospital facilities by investigating differences in facilities across different hospital levels in Thailand. Findings from our study will help to address gaps in or barriers to stroke service provision and improve implementation and ultimately patient care.
Methods
The study design was a cross-sectional survey study and reported according to the Checklist for Reporting Of Survey Studies (CROSS) (Additional file-Table S3).
Questionnaire development
The questionnaire developed for this study (Additional File-Fig. S2) was adapted from the INTERSTROKE study [15] and contained six parts namely, hospital characteristics (e.g. hospital level, beds, number of staff), funding (e.g. sources of fund), SU characteristics (e.g. beds in SU, type and the number of staff providing care, proportion of stroke patients, multidisciplinary team meetings), other facilities and services related to stroke services (e.g. their own written guidance, type of clinical assessment scores, systems of complication prevention), post-stroke care (e.g. type of rehabilitation provided, type of staff), and suggestions and feedback for services improvement.
Before circulating the questionnaire, it was reviewed by two non-academic healthcare staff from hospitals (neurologists) and one academic staff member. After revision, a pilot questionnaire was sent to four secondary hospitals.
Study sites and participants
Questionnaires were distributed to 119 hospitals under the MOPH service plan strategy which does not include hospitals within Bangkok and other university hospitals (one questionnaire per hospital). Hospitals are classified into: (1) 34 advanced-level, (2) 49 standard-level and (3) 36 mid-level referral hospitals. Questionnaires were sent to health professionals whose main responsibilities are related to stroke service provision in their hospital.
Ethics approval
Ethical approval was sought by the first author and granted by the Ethical Review Committee of the Institute for Development of Human Research Protection, MOPH (No.IHRP722/2562). All research was performed in accordance with the declaration of Helsinki ethical principles. Ethical approval was granted for public hospitals under the Thai MOPH (12 health regions).
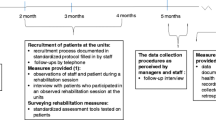
Data collection
The questionnaire was distributed via post, online and e-mail (pdf file) to all hospitals between November–December 2019 (Additional file-Table S4). All hospitals received the questionnaire via post with a link to the online questionnaire. Telephone calls were offered if clarification was required by respondents. A follow-up email was sent 4 weeks after distribution, followed by telephone reminders every 2 weeks. The survey was closed at month seven. Data were collected for the fiscal year 2018 (1 October 2017–30 September 2018). Data were entered or exported into Microsoft Excel spreadsheets before being transferred to R for analysis.
Statistical analysis
Data were analysed by comparing service availability, healthcare staffing, stroke service characteristics and rehabilitation. Comparisons were made between hospital levels. All analyses were undertaken using R software. Descriptive statistics were used to compare differences in the services provided.
Results
We received responses from 38 hospitals (response rate 32%). The majority was returned by post (66%, N = 25), followed by online questionnaires (24%, N = 9) and email (11%, N = 4). Respondents who provided the information were nurses (98%, N = 37) and physicians (2%, N = 1). Eight (21%) of these were advanced-level, 19 (50%) standard-level and 11 (29%) mid-level referral hospitals, representing all health regions except regions 7 and 13 (Bangkok). The highest proportion of respondents (18%) came from health regions 5 and 11 (Additional file-Fig. S3 and Fig. S4).
Hospital characteristics
The number of dedicated stroke beds (Table 2) was similar at each hospital level. Eight (1.1%, N = 705), six (1.5%, N = 400) and four beds (1.6%, n = 252) were dedicated to stroke patients in advanced-level, standard-level and mid-level referral hospitals, respectively.
In terms of number of patient admissions and referrals, a higher mean percentage of stroke patient admissions was observed for ischemic stroke for all hospital levels. However, haemorrhagic stroke patient admissions in advanced-level hospitals was 1.7 times higher than in mid-level referral hospitals. In addition, mainly patients with ischemic stroke were transferred to other hospitals (standard-level 47%, mid-level 75%). In contrast, mainly patients with haemorrhagic stroke were transferred from advanced-level referral hospitals (51%).
The main type of physician at all three hospital levels was similar, including general practice, internal medicine and surgeons. Neurologists were available in advanced-level (100%) and standard-level (42%), but not in mid-level referral hospitals. Rehabilitation physicians were available in all advanced-level and standard-level, and in 50% of mid-level referral hospitals.
Additionally, the median percentage of stroke patients who were reported to be looked after by specialist doctors with training in stroke was highest in mid-level referral hospital (advanced-level: 80%, standard-level: 80%, mid-level: 100%). However, 10 hospitals (three standard-level and seven mid-level referral hospitals) reported 0% as they did not have a specialist in their hospitals.
Lastly, five out of eight (63%) advanced-level referral hospitals served as a stroke-fast-track hub for lower-level hospitals, while only four (21%) standard-level referral hospitals had the capacity to be a hub/node for mid-level referral hospitals.
Healthcare service funding
The funding sources did not differ between hospitals (N = 34), with most hospitals reporting that nearly 100% of funding came from government. There is generally no requirement for out-of-pocket payments from patients.
Stroke unit (SU) services
Overall, 33 hospitals (87%) reported having SUs (Table 3). This included all advanced-level and standard-level and six mid-level (54%) referral hospitals. While four mid-level referral hospitals reported to provide SC. Only one mid-level referral hospitals reported not to have either SU or SC.
The proportion of stroke patients admitted to SU/SC was evaluated. The highest average percentage reported was found in mid-level referral hospitals at 77% (N = 8), while in advanced-level and standard-level referral hospitals proportions were 64% (N = 8), and 67% (N = 19), respectively. However, there were wide variations between health regions in advanced-level referral hospitals with four hospitals reporting that the proportion of stroke patients admitted to SU/SC was ≤50%. Similar proportions were reported at four standard-level and one mid-level referral hospitals.
Results of supportive features for SU/SC showed that 28 hospitals (76%) were able to provide all six features. All features were provided by all advanced-level referral hospitals except for special education programmes for staff (75%). Only three features were provided at all standard-level (feature 3, 4 and 6) and mid-level referral hospitals (feature 2, 5 and 6). In addition, 75% of advanced-level, 79% of standard-level, and 33% of mid-level referral hospitals passed the criteria for stroke centre certification recommended by Thai MOPH.
Neurologists, neurosurgeons, rehabilitation physicians, nurses, physiotherapists and occupational therapists were usually involved in providing care in SU/SC in all advanced-level referral hospitals. In standard-level referral hospitals, the main type of staff was similar but the number of staff was lower compared to advanced-level referral hospitals. In mid-level referral hospitals, there was no neurologists at SU/SC and the number of overall staff being lower except for physiotherapists. The type and number of staff providing care in SU/SC, either full-time or part-time is presented in Additional file-Table S5.
All advanced-level and standard-level referral hospitals reported to provide rehabilitation in SU/SC, but only 73% in mid-level referral hospitals. For all hospital levels, the key staff delivering rehabilitation after patients were discharged from hospital comprised physiotherapists, nurses, occupational therapists and VHVs. Most VHV provided rehabilitation services in mid-level referral hospitals.
Other healthcare facilities and services to support stroke service provision
The main types of clinical assessment (Table 4) included the Glasgow coma scale, Barthel Index (BI) and swallowing impairment at all hospital levels. Not all standard-level and mid-level referral hospitals used the modified Rankin Score (mRS) at admission. The type of assessment differed in standard-level referral hospitals with some noticeable variations in using the mRS with one hospital not conducting mRS. BI assessment was conducted at all hospital levels at admission, however, not all standard-level and mid-level referral hospitals measured BI at discharge. A less frequent test was malnutrition.
The proportion of thrombolytic therapy (Table 5) was less than 10%. There were notable differences in the proportion of prescribing thrombolysis between hospitals within the same health region at all hospital levels. It should be noted that two mid-level referral hospitals did not provide thrombolysis although they provided SC. Furthermore, 58% (N = 22) of hospitals provided only two investigations within 24 hours after admission including electrocardiogram monitoring and computerized tomography (CT) of the brain.
Post-stroke care services
There was considerable variation in the proportion of stroke patients receiving rehabilitation (Table 6). This was found for all types of services available and was not only observed between health regions but also between different hospital levels, and within hospital levels.
Suggestions for stroke service improvement from respondents
Respondents were also asked to provide comments with regards to improving stroke services. In advanced-level referral hospitals, these suggestions comprised: a clear policy and direction in order to respond to the MOPH policy, government funding to support human resource development, and an efficient system of health data records and linkage between hospitals along with monitoring and data analysis teams. Staff from standard-level and mid-level referral hospitals, commented on the need for materials and facilities to be able to care for patients at their own home and the need for a budget and manpower to be able to provide appropriate care post-discharge. Moreover, staff at some mid-level referral hospitals reported they would require ongoing teaching support from the higher-level hospitals to improve patient care in SUs.
Discussion
This is the first study to provide a detailed picture of healthcare facilities and services available to stroke patients in Thailand. The number of dedicated beds for stroke patients was similar between health regions at all hospital levels. In terms of KPIs from MOPH inspection report, stroke mortality in fiscal year 2019 and 2020 decreased in some health regions, although the national stroke mortality rate remains at 8% (2019: 7.97% and 2020: 7.99%), not reaching the national target of less than 7% per year [16]. Many patients were transferred from advanced-level referral hospitals, this result may be explained by the fact that patients might need to receive specialist care during the acute phase, such as surgery for haemorrhagic stroke. Patients are referred back to their registered hospitals when they are clinically stable.
The available specialties were different between hospital levels, especially neurologists were available in advanced-level and standard-level referral hospitals due to the scarcity of neurologists. The service plan strategy [3] sets out that, at SU, at least one neurologist and/or neurosurgeon and/or internal medicine practitioner should be available as a minimum standard requirement. The availability of these specialists therefore very much determines whether standard-level referral hospitals are able to provide SUs. Moreover, approximately 50% of neurologists practice in the Bangkok area [17] with the remaining neurologists ranging from 3 to 27 per health region which could contribute to the shortage of professionals in rural areas [5, 10]. Nurses were the main group providing stroke care at all hospital levels. The service plan strategy indicates that at least four nurses should be available at SUs as a minimum standard requirement, and results from our survey confirmed an adequate number of nursing staff.
Our findings also highlight that all advanced-level and standard-level referral hospitals had a SU, thus achieving the goal set by the service plan strategy (100% at advanced-level and standard-level referral hospitals). Some mid-level referral hospitals were also able to set up SU/SC. Despite some hospitals with SU being eligible to apply for stroke centre certification, not all have had the certification. The stroke centre certification assessment was recommended by the Department of Medical Services, MOPH, Thailand. They recommended that hospitals should improve SU and should obtain certification to provide standard of stroke care for acute stroke patients and hospitals should be accredited or re-accredited every 3 years [18]. In addition to the lowest percentage of access to SU in advanced-level referral hospitals, we found that one hospital reported their SU had just been set up a few months before answering our questionnaire; thus, the percentage of access to SU at this hospital was less than 30%. Although, the percentage of access to SU was almost 70%, the percentage of stroke patients admitted to SU/SC was quite low compared to some developed countries [19, 20].
Furthermore, this study supports evidence from the INTERSTROKE study that CT scans and antiplatelet drugs given were nearly 100%, while provision of MRI scans, carotid doppler ultrasound and thrombolytic therapy was extremely low.
The type and number of staff involved in providing care in SU/SC differed between hospital levels. One possible explanation could be the limited number of staff based at these hospitals and the scarcity of specialists in standard-level referral hospitals [5]. This is consistent with previous studies [21, 22] indicating that mid-level not only had fewer health professionals than advanced-level or standard-level referral hospitals but also that there was maldistribution of healthcare workers.
Furthermore, our finding shows that standard-level had greater provision of thrombolysis compared to advanced-level referral hospitals. It seems possible that stroke service delivery was improved due to the improvement of stroke fast track and thrombolytic treatment in mid-level and standard-level referral hospitals. Thrombolysis treatment can be provided at mid-level referral hospitals by non-neurologist, such as internists or emergency physicians, under the supervision of a neurologist from advanced-level or standard-level referral hospitals [23]. It should be noted that there could be regional differences which ranging from 5 to 22%. These results are supported by a Thai study using national stroke data [23] which showed that the percentage of acute ischemic stroke patients who were treated with thrombolysis varied widely across the country.
Although, there is no agreed benchmark for thrombolysis rates, the utilization rate remains low compared to other countries, especially developed countries [24,25,26]. Possible explanations include the onset of symptoms was more than 4.5 hours [5, 14], or patients may have had contraindications or a poor prognosis, which could affect the rate of thrombolysis initiation.
One interesting finding relates to the clinical assessment scores. Not all hospitals, especially standard-level and mid-level referral hospitals, evaluated patients at both admission and discharge. While the intermediate care guidelines [27], focussing on the recovery phase, recommended to measure the need for rehabilitation using the BI scores. This will affect health outcome assessments in the post-acute period. Further, the proportion and type of rehabilitation differed between hospital levels. Advanced-level and standard-level referral hospitals focused on inpatient rehabilitation, while most home-based and community rehabilitation were provided by mid-level referral hospitals. Indeed, these findings reflect the real-world service delivery in Thailand with the higher-level hospitals having the capacity to provide specialised care, while lower-level hospitals having fewer resources offering basic care [9, 10],
Thailand has introduced VHVs [9, 10] based in the community and VHVs play an important role in supporting healthcare providers such as follow-up care and acting as a link between providers and community resources. A previous study indicated that well-trained VHVs could help improve quality of life for stroke survivors [21]. However, VHVs seem to be unique to a Thai context and no international comparison can be made here.
Our study offers novel insights into stroke care in Thailand. Our questionnaire was adapted from the INTERSTROKE study [15], allowing us to draw comparisons. Despite low response rates, we were able to include representatives of almost all geographical areas in Thailand. Our results seem consistent with the INTERSTROKE study but should be interpreted with caution. Some limitations arise due to the nature of the survey method. Our study does not cover all hospital types, such as Bangkok area and university hospitals which mostly serve as excellence centres. This will have led to limitations in terms of comparability between health regions. Another limitation arises due to a lack of information on secondary prevention medication.
Moving forward we suggest that the stroke organisational survey should be reviewed and updated regularly in the MOPH annual reports and audit systems. The ability to track changes over time in stroke service quality should be the cornerstone of stroke provision. The use of patient-level data could help to improve information that is fed back to health facilities. Developing a system of national health data records and linkage between hospitals would be valuable for collecting data on clinical assessments and continuous stroke care between hospitals. Moreover, the national data should not be a fragmented database, rather, it should be in co-operation between heath schemes and MOPH.
Conclusions
The present study highlights that hospitals at all levels are likely to have shown improvement in service delivery, achieving the goals set by the service plan strategy in terms of setting up SUs with essential supportive features. Although, mid-level referral hospitals have potential to provide stoke service delivery similar to standard-level or advanced-level referral hospitals, improvements still need to be made in areas of health care workforce. Data linkage and health record systems for clinical or health outcomes in order to follow-up and monitor health outcomes of patients should be developed between hospitals and at national levels. Further, the limited capacity of service delivery should encourage policy makers to further improve stroke care at mid-level referral hospitals in Thailand.
Availability of data and materials
The data that support the findings of this study are available upon request from the corresponding author, [SK]. The data are not publicly available due to containing information that could compromise the privacy of research participants. Data are available from the authors upon reasonable request and with permission of each hospital that may require an additional document.
Abbreviations
- BI:
-
Barthel index
- CT:
-
Computerized tomography
- KPIs:
-
Key performance indicators
- mRS:
-
Modified Rankin Score
- MOPH:
-
Ministry of public health
- SC:
-
Stroke corner
- SU:
-
Stroke unit
- VHV:
-
Village health volunteers
References
Burden of Disease Research Program. Burden of diseases and injuries of Thai population in 2014. Nonthaburi: International Health Policy Program; 2017.
Strategy and Planning Division. Public health statistics 2018. Nonthaburi: Ministry of Public Health; 2019.
Bureau of Health Administration. Service plan strategies 2018–2022. Nonthaburi: Ministry of Public Health; 2016.
Bureau of Health Administration. Operating the service plan policies, 2017–2021. Nonthaburi: Office of the Permanent Secretary, Ministry of Public Health; 2017.
Suwanwela NC, Chutinet A, Kijpaisalratana N. Thrombolytic treatment in Thailand. J Stroke Med. 2018;1(1):41–4.
Kijpaisalratana N, Chutinet A, Akarathanawat W, Vongvasinkul P, Suwanwela NC. Outcomes of thrombolytic therapy in acute ischemic stroke: mothership, drip-and-ship, and ship-and-drip paradigms. BMC Neurol. 2020;20(1):45.
Suwanwela NC. Stroke epidemiology in Thailand. J Stroke. 2014;16(1):1–7.
Tiamkao S. Development of the stroke service system in the 7th health zone. J Med Assoc Thail. 2019;18(1):25–41.
Jongudomsuk P, Srithamrongsawat S, Patcharanarumol W, Limwattananon S, Pannarunothai S, Vapatanavong P, et al. The kingdom of Thailand health system review. Regional Office for the Western Pacific: World Health Organization; 2015.
Woratanarat T, Woratanarat P, Lekthipa C. Primary health care systems (PRIMASYS): case study from Thailand. Geneva: World Health Organization; 2017. p. 36.
Bureau of inspection and evaluation. Results of first round inspection and evaluation fiscal year 2018: group 2 service excellence. Nonthaburi: The Office of Permanent Secretary, Ministry of Public Health; 2018.
Bureau of inspection and evaluation. Results of inspection and evaluation fiscal year 2019. Nonthaburi: Ministry of Public Health; 2019.
Bureau of inspection and evaluation. Results of second round inspection and evaluation fiscal year 2018. Nonthaburi: Ministry of Public Health; 2018.
Rajborirug K, Tumviriyakul H, Suwanno J. Effects of stroke unit care in acute ischemic stroke patient ineligible for thrombolytic treatment. J Med Assoc Thail. 2017;100(4):410–7.
Langhorne P, O'Donnell MJ, Chin SL, Zhang H, Xavier D, Avezum A, et al. Practice patterns and outcomes after stroke across countries at different economic levels (INTERSTROKE): an international observational study. Lancet. 2018;391(10134):2019–27.
Bureau of inspection and evaluation. Results of inspection and evaluation fiscal year 2020. Nonthaburi: Ministry of Public Health; 2020.
Strategy and Planning Division. Public health resource 2018. Nonthaburi: Ministry of Public Health; 2018.
Prasat Neurological Institute, Department of Medical Services. Standard Stroke Center. Bangkok: Ministry of Public Health, Thailand; 2018. p. 54.
NHS National Services Scotland. Scottish stroke care audit, 2011 National Report: Scottish stroke improvement Programme Report-2019. Edinburgh; 2019.
Ringelstein E, Busse O, Ritter M. Current concepts of stroke units in Germany and Europe. Schweizer archiv fur Neurologie und Psychiatrie. 2011;162(4):155–60.
Dwyer M, Peterson GM, Gall S, Francis K, Ford KM. Health care providers’ perceptions of factors that influence the provision of acute stroke care in urban and rural settings: a qualitative study. SAGE Open Med. 2020:8.
Witthayapipopsakul W, Cetthakrikul N, Suphanchaimat R, Noree T, Sawaengdee K. Equity of health workforce distribution in Thailand: an implication of concentration index. Risk Manag Healthc Policy. 2019;12:13–22.
Tiamkao S, Ienghong K, Cheung LW, Celebi I, Suzuki T, Apiratwarakul K. Stroke incidence, rate of thrombolytic therapy, mortality in Thailand from 2009 to 2021. Open Access Maced J Med Sci. 2022;10(E):110–5.
Stolz E, Hamann GF, Kaps M, Misselwitz B. Regional differences in acute stroke admission and thrombolysis rates in the German federal state of Hesse. Deutsches Arzteblatt international. 2011;108(36):607–11.
Addo J, Bhalla A, Crichton S, Rudd AG, McKevitt C, Wolfe CDA. Provision of acute stroke care and associated factors in a multiethnic population: prospective study with the South London stroke register. BMJ. 2011;342:d744.
Quain Debbie A, Parsons MW, Loudfoot AR, Spratt NJ, Evans MK, Russell ML, et al. Improving access to acute stroke therapies: a controlled trial of organised pre-hospital and emergency care. Med J Aust. 2008;189(8):429–33.
Intermediate care service plan board. Guideline for intermediate care: Ministry of Public Health; 2019.
Acknowledgements
The authors would like to express deep gratitude and sincere appreciation to the healthcare staff from all study sites for their valuable support.
We are also grateful to the BMC Health Services Research reviewers for their helpful suggestions.
Funding
International Health Policy Program Foundation.
Author information
Authors and Affiliations
Contributions
The conceptualisation of this study was initiated by OW, PL and CG. All authors contributed to the development of the study design and protocol. SK coordinated the ethical approval, distribution of questionnaire, reminders, designed the system to monitor and follow up response rates and record questionnaire responses. SK conducted the data management and analysis with supervision by CG, OW and PL. SK and CG led the drafting of the paper supported and validated by OW and PL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Review Committee of the Institute for Development of Human Research Protection, MOPH (No.IHRP722/2562). All methods were performed in accordance with the declaration of Helsinki ethical principles. Healthcare staff, who decided to participate provided written informed consent by sending back the consent with questionnaire or in case of the online questionnaire by clicking a designated check box.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
Map of health regions in Thailand. Table S1. Classification of referral hospitals and goal of stroke service delivery under Thai service plan strategy [1,2,3]. Table S2. Number of hospitals by health region at year 2019 [4]. Table S3. Checklist for Reporting Of Survey Studies (CROSS). Questionnaire administration. Fig. S2. Stroke questionnaire adapted from the INTERSTROKE study. Table S4. Data collection timeline. Fig. S3. Number of questionnaires received and proportion of questionnaires (N = 38). Fig. S4. Response rate, by health region (N = 38). Table S5. Type and number of staff providing care for stroke patients in stroke unit/stroke corner.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kumluang, S., Geue, C., Langhorne, P. et al. Availability of stroke services and hospital facilities at different hospital levels in Thailand: a cross-sectional survey study. BMC Health Serv Res 22, 1558 (2022). https://doi.org/10.1186/s12913-022-08922-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08922-2