Abstract
Background
Economic disparities affect access to assisted reproductive technology (ART) treatment in many countries. At the time of this survey, Japan provided partial reimbursement for ART treatment only for those in low- or middle-income classes due to limited governmental budgets. However, the optimal level of financial support by income class remains unclear.
Methods
We conducted a conjoint analysis of ART in Japan in January 2020. We recruited 824 women with fertility problems aged 25 to 44 years via an online social research panel. They completed a questionnaire of 16 hypothetical scenarios measuring six relevant ART attributes (i.e., out-of-pocket payment, pregnancy rate, risk of adverse effects, number of visits to outpatient clinics, consultation hours and kindness of staff) and their relations to treatment choice.
Results
Mixed-effect logistic regression models showed that all six attributes significantly influenced treatment preferences, with participants valuing out-of-pocket payment the most, followed by pregnancy rates and kindness of staff. Significant interactions occurred between high household income (≥ 8 million JPY) and high out-of-pocket payment (≥ 500,000 JPY). However, the average marginal probability of the highest-income patients (i.e., ≥ 10 million JPY, ineligible for the subsidy) receiving ART treatment at the average cost of 400,000 JPY was 47%, compared to 56 − 61% of other income participants, who opted to receive ART at an average cost of 100,000 JPY after a 300,000 JPY subsidy.
Conclusion
Our results suggest that out-of-pocket payment is the primary determinant in patients’ decision to opt for ART treatment. High-income patients were more likely to choose treatment, even at a high cost, but their income-based ineligibility for government financial support might discourage some from receiving treatment.
Similar content being viewed by others
Introduction
As more people postpone parenthood [1, 2], the use of assisted reproductive technology (ART) is increasing worldwide [3]. Despite the growing need and effectiveness of this treatment, economic factors have contributed to huge disparities in access to ART within and between countries [4,5,6]. To improve financial accessibility to ART treatments, governments of many countries provide various types of public funding, such as health insurance coverage, subsidies and tax refunds [7]. The proportions of reimbursement (i.e. full or partial) and eligibility criteria (e.g. clinical or demographical) vary substantially depending on regional and financial factors [7].
Japan provides universal health insurance coverage to the entire population [8]. In response to prolonged low fertility rates in Japan, ART treatments have been covered since April 2022 [9]. Prior to that date, only eligible couples received partial subsidies for ART treatment [10, 11]. Specifically, at the time of this survey in 2020, ART subsidies were available only to low- or middle-income patients. For high-income couples, the out-of-pocket payment for ART was approximately 400,000 − 500,000 JPY per cycle, or 3,300 − 4,200 euros using the 2020 exchange rate of 1 euro = 120 JPY [10, 11].
In Japan, eligibility rules for this and other subsidies (e.g. child allowance) often prioritize lower-income citizens [12]. Similar criteria were set up for ART subsidies in other East Asian countries, such as Korea [13] and Taiwan [14]. Yet, ART treatment is generally highly used among older and higher-income couples [15]. If these couples delay fertility treatment until they can better afford the associated cost, then the lack of subsidization for high-income couples could contribute to decreased rates of pregnancy [16]. In consideration of such potential adverse effects, the rationale for the eligibility criteria based on annual household income should be discussed.
Previous research has assessed the relationship between price and demand for ART [17], but few studies have assessed the quantitative association between demand and uptake of ART treatment and out-of-pocket payments by income level [4, 5]. The optimal amount of financial support by income class is unknown. We thus aimed to evaluate the probability of patients receiving ART treatment based on out-of-pocket payment and income class, using a conjoint analysis (CA).
Methods
Study setting
At the time of this survey in Japan, January 2020, the average cost per cycle of ART treatment was 380,000 JPY (i.e. 3,170 euros) for a fresh cycle and 510,000 JPY (i.e. 4,250 euros) for a freeze-all cycle, and these averages varied greatly across regions and institutions [18]. In lieu of health insurance coverage for ART treatment, the government offered partial reimbursement in the form of subsidies. The governmental subsidy was 300,000 JPY (i.e. 2,500 euros) for the first ART treatment cycle and 150,000 JPY (i.e. 1,250 euros) per cycle for the second to sixth cycles for legally married women younger than 40 (women aged 40–42 were limited to three cycles). Eligibility was income-based: annual household income after deducting predefined items could not exceed 7,300,000 JPY, corresponding to a gross income of 9,530,000 JPY (i.e. 79,400 euros).
Participants and procedures
Participants were recruited via an online social research panel from the market research company Macromill (Tokyo, Japan), which manages a nationwide panel of more than 1 million registrants. To be considered for inclusion, participants had to be female, married, aged 25–44 years, currently experiencing infertility, and have a history of fertility tests or treatment. Macromill sent a pre-screening questionnaire to 210,212 randomly selected female registrants aged 25–44 years, then accepted pre-screening responses until reaching 20,000 respondents. Of those 20,000 respondents, 1,346 met the previously mentioned eligibility criteria. Macromill then sent recruitment emails to 1,247 who were randomly selected from the 1,346 eligible participants. Finally, 824 completed the survey and received a coupon (usually worth less than 1 Euro), consistent with Macromill’s procedures. All procedures were conducted from January 16 to 21, 2020. Participant responses were anonymous.
Measures
CA questionnaire
Participants were presented with brief material explaining ART treatments, such as procedures, average pregnancy rates, possible adverse events due to medication and procedures, costs and subsidies and visits to outpatient clinics. We then presented hypothetical and realistic scenarios of ART treatment (see Fig. 1 for an example). As described in Table 1, scenarios comprised six relevant ART attributes (out-of-pocket payment, pregnancy rate, risk of adverse effects, number of monthly visits to outpatient clinics, consultation hours and kindness of staff). We selected these attributes based on literature about patient preferences in fertility care [19, 20], previous surveys conducted by a patient group in Japan [21], interviews with colleagues who experienced fertility care and a discussion with fertility specialists (SCJ, YKumazawa and OI) and public health researchers (EM, YKobayashi and TF). We divided each attribute into two to four levels covering a realistic range of Japanese fertility care settings. We established a range of out-of-pocket payments from 0 JPY (i.e. fully subsidised) to 800,000 JPY, or 6,700 euros (i.e. ineligible for subsidy). We used an orthogonal fractional factorial design to generate combinations of attribute levels, yielding 16 scenarios. Patients were asked to make ART treatment decisions in each of the 16 scenarios (see Fig. 1 for an example), which were presented in random order. To ensure that the questionnaire was understandable, we conducted a pilot survey on a small group of our colleagues, including those who experienced fertility problems.
Socioeconomic and fertility status
Participant were grouped by age (25–29, 30–34, 35–39, or 40–44 years). They reported their annual household incomes (before deductions), educational backgrounds (university education, yes/no), average paid working hours per week (none, < 40 h, ≥ 40 h) and whether they had ever given birth (yes/no). We categorised annual household income into five groups (Low, < 4 million JPY; Lower-middle, 4–6 million JPY; Middle, 6–8 million JPY; Upper-middle, 8–10 million JPY; or High, ≥ 10 million JPY). The High-income group was assumed to be ineligible for governmental subsidy of ART treatments because only those with a gross household income of approximately 9.5 million JPY or lower were eligible. Participants reported their fertility information, including history (i.e., tests, timing methods, ovulation induction, intrauterine insemination, ART) and primary diagnosis (i.e., female factor, male factor, male and female factor, unknown, under investigation).
Statistical analyses
Characteristics of the study participants were described and compared by household income class using Cuzick’s tests for trend. Using mixed-effects logistic regression models, we assessed 13,184 choices among 824 participants for the 16 ART treatment scenarios. Explanatory variables included the six previously described attributes of ART treatment (Model 1) and socioeconomic and fertility status (Model 2). In addition, we added to Model 2 an interaction term between household income and “out-of-pocket payment” and an interaction term between average working hours per week and “consultation hours” (Model 3).
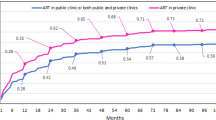
To visualise all attribute effects, in Model 1, we calculated part-worth utility estimates using effect code (zero-centred) dummy variables, taking the value of -1 for the reference level [22]. To graph the relationships between treatment choice, out-of-pocket payment and income, we calculated in Model 1 the average marginal predicted probabilities by household income when the attribute “out-of-pocket payment” changed continuously. A two-sided p-value of < 0.05 indicated statistical significance. All analyses were performed using STATA14-MP (StataCorp LP, College Station, TX, USA) and R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).
Ethical approval
The ethics committee at Akita University Graduate School of Medicine approved the study protocol (no. 2343) on December 20, 2019.
Results
Socioeconomic and clinical status of participants
Table 2 shows the background characteristics of the 824 female participants. Overall, most were in their thirties with middle-level household incomes, and 46% had a university education. About 36% had a child, and about 60% had paid work. Regarding fertility status, 31% had received ART treatments, but most (68%) were in early treatment stages (e.g. fertility tests, intrauterine insemination). The most frequent diagnosis of infertility was unknown (45%), followed by female factor (28%) and male and female factor (12%).
The proportions of those having a university education and paid work were higher among higher income classes (Ps for trend < 0.001). The other demographic and fertility status traits were not significantly different by income class, except for the small number of participants aged 25–29 in the High-income group.
Relationships between attributes of treatment and choice of treatment
The mixed-effects logistic regression model showed that all six attributes were significantly associated with the choice to receive ART treatment (Model 1, Table 3 and Fig. 2). Participants were less likely to choose ART treatment when the out-of-pocket payment was high, when adverse events might happen, or when the monthly number of visits to the clinic was 12 (versus four) times. They were more likely to choose ART treatment when its associated pregnancy rates were high, when clinics were available at night and on weekends, or when staff were perceived as kind. Part-worth utility estimates suggested that participants valued out-of-pocket payment the most, followed by treatment pregnancy rates and kindness of staff (Fig. 2). The results were similar after adjusting for socioeconomic and clinical statuses of the participants (Model 2, Table 3). Those who had High household income, who worked 40 h per week, or who received more advanced treatments were more likely to choose ART treatments.
In Model 3, we observed significant interactions between the Upper-middle income class and an out-of-pocket payment of 500,000 JPY (P for interaction = 0.042) and between the High-income class and out-of-pocket payments of 500,000 JPY or 800,000 JPY (both Ps for interaction < 0.001), as shown in Table 4. We also observed a significant interaction between working more than 40 h per week and clinic consultation availability on nights and weekends (P for interaction = 0.005).
Figure 3 shows the average marginal probabilities of opting for ART treatment across the income groups in Model 1, when the out-of-pocket payment changed continuously. The probability of opting for ART was consistently higher among the High-income group, compared to other income groups. For example, for the scenario in which an initial ART cycle cost 400,000 JPY, the average marginal probability of High-income participants choosing treatment was 47%. In the same scenario but including an income-based subsidy of 300,000 JPY (reducing the out-of-pocket cost to 100,000 JPY) the average marginal probability of opting for ART treatment was 56% among Low-income participants and 61% for Upper-middle-income participants. These probabilities decreased to 43% for Low-income participants and 50% for Upper-middle-income participants for the second through sixth treatments, for which subsidies decreased to 150,000 JPY (i.e. 250,000 JPY out-of-pocket) each.
Discussion
In our CA study, we found that the out-of-pocket payment was the most influential determinant of ART treatment choice among participants, though all six attributes (e.g. pregnancy rates and kindness of staff) significantly influenced treatment preference. Higher-income patients were more likely to receive ART treatment even at a high cost, but their ineligibility for financial support due to their high income might discourage some from receiving treatment. This quantitative evaluation suggested that patients’ willingness to receive ART treatment could change substantially according to public funding of ART treatment. Many countries have sought to improve treatment accessibility in the context of limited financial resources, leading to enormous fluctuations in the number of treatments that patients opt to receive [4, 23, 24]. CA could be a feasible way to help policymakers identify the most appropriate programs for public funding under fiscal constraints.
Among the various factors affecting fertility care utilisation (e.g. sociocultural acceptability, availability), financial accessibility is a dominant one [6, 11]. Our findings corroborate that patients consider their out-of-pocket payment to be the most important attribute in their fertility decisions (Fig. 2). In addition, our prediction is consistent with previous findings on the relationship between cost and utilisation of ART treatment. For example, in an ecological study of 30 high- and upper-middle-income countries, Chambers et al. [5] find that a 1 percentage point decrease (based on annual disposable income for a single person with no dependents) in the cost of a treatment cycle predicts a 3.2% increase in utilisation. In our study, the probability of participants choosing ART treatment increased by 54% when the out-of-pocket payment decreased by 800,000 JPY (Fig. 3), corresponding with a 2.3% increase in demand per 1 percentage point decrease (based on disposable household income) in cost [25]. However, the slope differed depending on both income and out-of-pocket payment.
A study on ART treatment copayments in Germany demonstrated arc price elasticity of demand of -0.36 [17]: in other words, when the copayment for fertility treatment increased from free to 50% (1,500–2,000 euros), ART treatments dropped by 53% [23]. We observe a smaller elasticity (-0.13) but comparable inelasticity when the cost of ART treatment increases from 0 (free) to 200,000 JPY (1,670 euros), which is similar to results for other medical services, generally in the range of -0.1 to -0.3 [26]. Although the choices made in a CA would not completely match actual treatment choices, we confirmed that the CA could reasonably predict treatment choices based on arbitrary treatment costs.
As shown in Fig. 3, higher-income participants consistently opted for ART even at a higher cost: 27% of those in the High-income group were willing to pay up to 800,000 JPY (6,770 euros). For out-of-pocket payments exceeding 500,000 JPY (4,170 euros), we observed significant interactions between out-of-pocket payments and the Upper-middle- or High-household income groups (Table 4), suggesting an important effect of income: The negative impact of cost on ART demand was lower among higher-income populations, compared to lower-income populations.
Yet, the probability of receiving ART treatment among High-income group could fall below that of other income groups, depending on their subsidy eligibility. Among all five income groups, to attain a 47% probability of opting for ART treatment costing 400,000 JPY (as we observed for the High-income group), the ideal subsidy amounts are 200,000 JPY for Low-, 180,000 JPY for Lower-middle, 140,000 JPY for Middle- and 120,000 JPY for Upper-middle income groups. In 2020, the Japanese government provided a 150,000 JPY income-based subsidy for each of the second through sixth ART treatments, which was close to our suggested ideal amount. In contrast, the 300,000 JPY subsidy for the first application may induce a sense of “unfairness” among High-income patients.
In response to the country’s prolonged low fertility rate, the Japanese government removed the income eligibility criteria at the end of 2020 [10]. Since April 2022, up to six (three) cycles of ART treatments have been covered by health insurance for all legally or virtually married women aged < 40 years (40–42 years). Under the health insurance scheme, out-of-pocket payment for a fresh ART treatment cycle is estimated to be approximately 150,000 JPY (e.g., when six to nine eggs are retrieved, and two to five embryos are cultured and cryopreserved) [9]. This policy change helps to eliminate the perceived “unfairness” among High-income couples and to increase the total number of fertility treatments that women receive. Our model calculated that the probability of High-income couples opting for a fresh ART treatment cycle would increase nearly 1.3 times, from 47 to 61%, if the out-of-pocket payment decreased from 400,000 JPY(i.e., without a subsidy) to 150,000 JPY(i.e., covered by health insurance). This potentially large fiscal impact should be monitored to ensure that public funding for ART remains sustainable.
Interestingly, we found that Japanese patients preferred to seek ART treatment when the clinic staff was perceived as friendly (Fig. 2). Our findings agree with studies in China [19] and Europe [27] indicating that patients value physician’s attitude toward patients as much as they value the treatment’s success rate, whereas physicians underestimate the importance of patient-centred care. Although we could not assess a variety of aspects of patient-centredness, such as physician continuity or information provision of treatment [28], this is the first study to quantify the effects of patient-centred fertility care on treatment choice of patients in Japan. The fact that patients attached great importance to staff attitudes should promote clinicians’ understanding of the care they seek.
Another important finding of this study relates to women engaged in paid work for 40 h or more per week, who were more likely to choose treatment if they could visit outpatient clinics at night or on weekends. Aligned with rises in parental age and women’s labour force participation [2], 60% of women receiving fertility care have concerns about missing work [29], and about 17% of women in Japan resign from their jobs after starting fertility treatment [30]. We found that medical institutions offering consultation during nights and weekends were preferred by participants working outside the home. Since ART procedures require frequent and sometimes unpredictable visits based on the menstrual cycle [30], providing flexible clinic hours and a supportive work environment would help employees balance their fertility treatments with their work schedules [31].
This study has some limitations. First, attributes not included in our CA scenarios might be relevant in real-life settings. We selected six attributes based on surveys in Japan [21] and abroad [19, 20] and on our interviews of patients and clinicians. To maintain a reasonable number of scenarios presented to participants, we did not include all possible attributes (e.g. geographical access to the institution, amount of time required to see doctors). However, we ensured through the pilot survey that the questionnaire was understandable and that no vital information was missing from the scenarios. A future qualitative study including in-depth interviews in Japan might help construct a CA questionnaire. Second, decisions in a CA may not exactly match those during actual treatment. Empirical studies on patients’ actual behaviours before and after the subsidy policy revision and based on health insurance coverage could help confirm the validity of this study. Third, the use of social research panels could have caused selection bias associated with higher education [32, 33]. To recruit eligible samples efficiently, the market research company invited a large sample to the pre-screening, accepted responses in order of arrival and invited randomly selected participants to the survey. However, the sociodemographic distribution of our participants was similar to that of previous clinical settings in Japan [30], and patients with fertility problems tend to have higher education levels. Thus, our data should not be heavily influenced by potential selection bias. Finally, this study focused on ART treatment in Japan. However, CA is a generic approach that can be used widely. Future research should assess cultural relevance in perceptions of fertility information.
Conclusions
We found that out-of-pocket payments were the most influential determinant for patients in Japan seeking ART treatment. Higher-income patients opted for treatment even at a higher cost, but their income-based ineligibility for government financial support discouraged some from receiving treatment. Although the setting of the present study was in Japan, CA could be a feasible way to discuss appropriate programs for public funding in many countries.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to participant privacy, but they are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Assisted reproductive technology
- CA:
-
Conjoint analysis
- JPY:
-
Japanese Yen
References
Organisation for Economic Co-operation and Development (OECD). OECD Family Database, Indicator SF2.3, “Age of mothers at childbirth and age-specific fertility”, 2017. https://www.oecd.org/els/soc/SF_2_3_Age_mothers_childbirth.pdf Accessed 18 Jun 2021
Mills M, Rindfuss RR, McDonald P, te Velde E. Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod. 2011;17:848–60.
de Mouzon J, Chambers GM, Zegers-Hochschild F, Mansour R, Ishihara O, Banker M, Dyer S, Kupka M, Adamson GD. International committee for monitoring assisted reproductive technologies world report: assisted reproductive technology 2012. Hum Reprod. 2020;35:1900–13.
Chambers GM, Hoang VP, Illingworth PJ. Socioeconomic disparities in access to ART treatment and the differential impact of a policy that increased consumer costs. Hum Reprod. 2013;28:3111–7.
Chambers GM, Hoang VP, Sullivan EA, Chapman MG, Ishihara O, Zegers-Hochschild F, Nygren KG, Adamson GD. The impact of consumer affordability on access to assisted reproductive technologies and embryo transfer practices: an international analysis. Fertil Steril. 2014;101:191–8.
Dyer S, Chambers GM, Adamson GD, Banker M, de Mouzon J, Ishihara O, Kupka M, Mansour R, Zegers-Hochschild F. ART utilization: an indicator of access to infertility care. Reprod Biomed Online. 2020;41:6–9.
Keane M, Long J, O’Nolan G, Faragher L. Assisted reproductive technologies: International approaches to public funding mechanisms and criteria an evidence review. Ireland: Health Research Board; 2017.
Ikegami N, Yoo BK, Hashimoto H, Matsumoto M, Ogata H, Babazono A, Watanabe R, Shibuya K, Yang BM, Reich MR, Kobayashi Y. Japanese universal health coverage: evolution, achievements, and challenges. Lancet. 2011;378:1106–15.
Ministry of Health, Labour and Welfare. Health insurance coverage of infertility treatments (in Japanese), 2022. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kodomo/kodomo_kosodate/boshi-hoken/funin-01.html Accessed 6 Jun 2022
Jwa SC, Ishihara O, Kuwahara A, Saito K, Saito H, Terada Y, Kobayashi Y, Maeda E. Cumulative live birth rate according to the number of receiving governmental subsidies for assisted reproductive technology in Saitama Prefecture, Japan: a retrospective study using individual data for governmental subsidies. Reprod Med Biol. 2021;20:451–9.
Iba A, Maeda E, Jwa SC, Yanagisawa-Sugita A, Saito K, Kuwahara A, Saito H, Terada Y, Ishihara O, Kobayashi Y. Household income and medical help-seeking for fertility problems among a representative population in Japan. Reprod Health. 2021;18:165.
Kuroda A. Significance and issue of social allowances: Implications from the child allowance system and child-rearing allowance system (in Japanese). Shakaihoshokenkyu. 2016;1:370–81.
Shin J, Lee SG, Park EC, Nam JY. Socioeconomic status and successful delivery after an infertility diagnosis: a nationwide health insurance cohort study in Korea conducted from 2005 to 2013. J Korean Med Sci. 2020;35(39):e341.
Wu CL, Huang YL, Ha JO, Chen WH, Huang YH. Equal access, risk prevention, or pronatalism? public financing of in vitro fertilization in Japan, South Korea, and Taiwan. Taiwan Democracy Quarterly. 2020;17:49–104.
Goisis A, Håberg SE, Hanevik HI, Magnus MC, Kravdal Ø. The demographics of assisted reproductive technology births in a Nordic country. Hum Reprod. 2020;35:1441–50.
Katagiri Y, Jwa SC, Kuwahara A, Iwasa T, Ono M, Kato K, Kishi H, Kuwabara Y, Harada M, Hamatani T, Osuga Y. Assisted reproductive technology in Japan: a summary report for 2019 by the ethics committee of the japan society of obstetrics and gynecology. Reprod Med Biol. 2021;21:e12434.
Connolly MP, Griesinger G, Ledger W, Postma MJ. The impact of introducing patient co-payments in Germany on the use of IVF and ICSI: a price-elasticity of demand assessment. Hum Reprod. 2009;24:2796–800.
Maeda E. Health and Labour Sciences Research Grants (H30‑Sukoyaka‑Ippan‑002) Summary Research Report (in Japanese). 2018. https://mhlw-grants.niph.go.jp/project/27041 Accessed 2 Nov 2021
Cai QF, Wan F, Dong XY, Liao XH, Zheng J, Wang R, Wang L, Ji LC, Zhang HW. Fertility clinicians and infertile patients in China have different preferences in fertility care. Hum Reprod. 2014;29:712–9.
Palumbo A, De La Fuente P, Rodríguez M, Sánchez F, Martínez-Salazar J, Muñoz M, Marqueta J, Hernández J, Espallardo O, Polanco C, Paz S, Lizán L. Willingness to pay and conjoint analysis to determine women’s preferences for ovarian stimulating hormones in the treatment of infertility in Spain. Hum Reprod. 2011;26:1790–8.
Fine (non-profit organization). Questionnaire and results for “How do you choose your medical institution?” (in Japanese) August, 2012. https://j-fine.jp/prs/prs/Fine_press_1208_byoin_ank.pdf Accessed 11 Oct 2021
Rao VR. Applied conjoint analysis. New York: Springer; 2014.
Griesinger G, Diedrich K, Altgassen C. Stronger reduction of assisted reproduction technique treatment cycle numbers in economically weak geographical regions following the German healthcare modernization law in 2004. Hum Reprod. 2007;22:3027–30.
Bissonnette F, Phillips S, Sampalis J, Dahdouh EM, St-Michel P, Buckett W, Kadoch IJ, Mahutte N. Impact of government health coverage for ART: the results of a 5-year experience in Quebec. Reprod Biomed Soc Online. 2019;8:32–7.
Statistics Bureau of Japan. National Survey of Family Income and Expenditure. Workers’s household of one-person households 2020. https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00200561&tstat=000000330001&cycle=7&year=20200&month=0&tclass1=000000330001&tclass2=000000330022&tclass3=000000330024&result_back=1&cycle_facet=tclass1%3Atclass2%3Atclass3%3Acycle&tclass4val=0 Accessed 12 Jun 2022
Phelps CE. Health economics. Boston: Pearson Education Inc; 2010.
van Empel IW, Dancet EA, Koolman XH, Nelen WL, Stolk EA, Sermeus W, D’Hooghe TM, Kremer JA. Physicians underestimate the importance of patient-centredness to patients: a discrete choice experiment in fertility care. Hum Reprod. 2011;26:584–93.
Huppelschoten AG, Verkerk EW, Appleby J, Groenewoud H, Adang EMM, Nelen WLDM, Kremer JAM. The monetary value of patient-centred care: results from a discrete choice experiment in Dutch fertility care. Hum Reprod. 2014;29:1712–20.
Klonoff-Cohen H, Natarajan L. The concerns during assisted reproductive technologies (CART) scale and pregnancy outcomes. Fertil Steril. 2004;81:982–8.
Imai Y, Endo M, Kuroda K, Tomooka K, Ikemoto Y, Sato S, Mitsui K, Ueda Y, Deshpande GA, Tanaka A, Sugiyama R, Nakagawa K, Sato Y, Kuribayashi Y, Itakura A, Takeda S, Tanigawa T. Risk factors for resignation from work after starting infertility treatment among Japanese women: Japan-female employment and mental health in assisted reproductive technology (J-FEMA) study. Occup Environ Med. 2021;78:426–32.
Ichikawa T, Ota I, Kuwabara Y, Tsushima R, Hamatani T, Hiraike O, Takeshita T, Osuga Y, Akira S. Infertility treatment hinders the careers of working women in Japan. J Obstet Gynaecol Res. 2020;46:1940–50.
Haagen EC, Tuil W, Hendriks J, de Bruijn RP, Braat DD, Kremer JA. Current internet use and preferences of IVF and ICSI patients. Hum Reprod. 2003;18:2073–8.
Takahashi Y, Ohura T, Ishizaki T, Okamoto S, Miki K, Naito M, Akamatsu R, Sugimori H, Yoshiike N, Miyaki K. Internet use for health-related information via personal computers and cell phones in Japan: a cross-sectional population-based survey. J Med Internet Res. 2011;13:e110.
Acknowledgements
This study was presented at the 37th annual meeting of the European Society of Human Reproduction and Embryology, June 27–July 1, 2021. We thank Ms. Sanae Taniguchi and Ms. Junko Hirayama for their assistance in data analyses and Ms. Jennifer Keane of Oxford Editing for editing the article.
Funding
This study was funded by the Health and Labour Sciences Research Grant (H30-Sukoyaka-Ippan-002) and the Japan Society for the Promotion of Science: KAKENHI (Grant Number 21H03193). The funders had no rules regarding the design or conduct of the study; collection, analyses, or interpretation of the data; or preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
EM contributed to the conception and design of the study; participated in the acquisition, analyses and interpretations of data; drafted all versions of the article; and approved the final version for publication. SCJ, Y. Kumazawa and OI contributed to the design of the study, the revisions of each version and the approval of the final version for publication. Y. Kobayashi and TF contributed to the conception and design of the study, data interpretation, manuscript revisions and approval of the final version for publication. All other co-authors contributed to the critical revision of the paper and final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee at Akita University Graduate School of Medicine approved the study protocol (no. 2343) on December 20, 2019. All methods were conducted in accordance with “Ethical Guidelines for Medical and Biological Research Involving Human Subjects (Ministry of Health, Labour and Welfare, Japan).”
Only those who agreed that participation was voluntary and that participants could withdraw from the survey at any time participated in this survey. The need for informed consent was waived by the ethics committee at Akita University Graduate School of Medicine according to the above-mentioned national guideline (Ministry of Health, Labour and Welfare, Japan). Collection of online data complied with the “Code of Conduct of Marketing Research” and “Requirements for Compliance Program on Personal Information Protection (JIS Q 15001)” of the Japan Marketing Research Association.
Consent for publication
Not applicable.
Competing interests
None declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Maeda, E., Jwa, S.C., Kumazawa, Y. et al. Out-of-pocket payment and patients’ treatment choice for assisted reproductive technology by household income: a conjoint analysis using an online social research panel in Japan. BMC Health Serv Res 22, 1093 (2022). https://doi.org/10.1186/s12913-022-08474-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08474-5