Abstract
Introduction
Kenya’s maternal mortality ratio is relatively high at 342/100,000 live births. Confidential enquiry into maternal deaths showed that 90% of the maternal deaths received substandard care with health workforce related factors identified in 75% of 2015/2016 maternal deaths. Competent Skilled Health Personnel (SHP) providing emergency obstetric and newborn care (EmONC) in an enabling environment reduces the risk of adverse maternal and newborn outcomes. The study objective was to identify factors that determine the retention of SHP 1 – 5 years after EmONC training in Kenya.
Methods
A cross-sectional review of EmONC SHP in five counties (Kilifi, Taita Taveta, Garissa, Vihiga and Uasin Gishu) was conducted between January–February 2020. Data was extracted from a training database. Verification of current health facilities where trained SHP were deployed and reasons for non-retention were collected. Descriptive data analysis, transfer rate by county and logistic regression for SHP retention determinants was performed.
Results
A total of 927 SHP were trained from 2014–2019. Most SHP trained were nurse/midwives (677, 73%) followed by clinical officers (151, 16%) and doctors (99, 11%). Half (500, 54%) of trained SHP were retained in the same facility. Average trained staff transfer rate was 43%, with Uasin Gishu lowest at 24% and Garissa highest at 50%. Considering a subset of trained staff from level 4/5 facilities with distinct hospital departments, only a third (36%) of them are still working in relevant maternity/newborn/gynaecology departments. There was a statistically significant difference in transfer rate by gender in Garissa, Vihiga and the combined 5 counties (p < 0.05). Interval from training in years (1 year, AOR = 4.2 (2.1–8.4); cadre (nurse/midwives, AOR = 2.5 (1.4–4.5); and county (Uasin Gishu AOR = 9.5 (4.6- 19.5), Kilifi AOR = 4.0 (2.1–7.7) and Taita Taveta AOR = 1.9 (1.1–3.5), p < 0.05, were significant determinants of staff retention in the maternity departments.
Conclusion
Retention of EmONC trained SHP in the relevant maternity departments was low at 36 percent. SHP were more likely to be retained by 1-year after training compared to the subsequent years and this varied from county to county. County policies and guidelines on SHP deployment, transfers and retention should be strengthened to optimise the benefits of EmONC training.
Similar content being viewed by others
Introduction
Globally, estimated 295,000 maternal deaths occurred in 2017, 2.5 million newborns died in 2018, and 2.6 million stillbirths occurred in 2015 with 99 percent, 77 percent and 98 percent of them occurring in low- and middle-income countries (LMICs) respectively [1,2,3]. The majority of these deaths occurred around the time of childbirth [4]. Kenya continues to experience a high burden of maternal and newborn deaths above the global sustainable development goal (SDG) targets of less than 70/100,000 live births for maternal mortality and 12/1000 live births for newborn mortality respectively [5]. In Kenya, the maternal mortality ratio was estimated at 342/100,000 live births in 2017 [6], perinatal mortality (stillbirths and early neonatal deaths) rate at 29/1000 in 2014 and neonatal mortality rate reduced to 22/1000 live births in 2014 [7]. The first Kenya Confidential Enquiry into Maternal Deaths report (2017) showed that substandard care was identified in 9 out of 10 maternal deaths with three quarters of the deaths associated with health workforce related deficiencies in knowledge and skills in emergency obstetric care (EmOC). The most frequently identified health workforce related factors were delay in starting treatment (32.9%), inadequate clinical skills (28.1%) and inadequate monitoring (26.9%) [8].
The Lancet Every Newborn Series report shows that three million lives can be saved by 2025 if achievable interventions are scaled up to nearly universal coverage, and improving care at the time of birth gives a triple return on investment saving mothers, newborns and stillbirths [9]. Increased coverage and quality of preconception, antenatal, intrapartum, and postnatal interventions by 2025 could avert 71% of neonatal deaths (1·9 million), 33% of stillbirths (0·82 million), and 54% of maternal deaths (0·16 million) per year. Evidence has shown that the day of birth is the most dangerous for mothers and their babies, resulting in nearly half of maternal and newborn deaths and stillbirths and therefore priority and urgent attention should be paid to this birth day. Preterm birth, intrapartum complications, and infections are the leading causes of neonatal death. Interventions delivered around the time of birth – skilled care during labor and childbirth, emergency obstetrics and newborn care for obstetric complications plus immediate newborn care – have the greatest potential to avert 41% of neonatal deaths [10,11,12]. However, barriers to scale-up of skilled care at birth with the highest effect on mortality outcome exist especially in LMICs including finance (only four percent of donor funding allocated to newborn health) and workforce, especially midwives and nurses – insufficient numbers, inefficient skill mix, inequitable distribution, varying levels and quality of education and training programmes [13, 14]. The Every Newborn Series recommends urgent attention to reach every woman and every newborn baby, close gaps in coverage, and improve equity and quality for antenatal, intrapartum, and postnatal care, especially in the poorest countries and for underserved populations for a triple return on investment around the time of birth: averting maternal and newborn deaths and preventing stillbirths [13]. This is also emphasized in the State of the World Midwifery (SoWMy) report 2021 which indicates that for midwives to achieve their potential, urgent investments are needed in the midwifery workforce planning, management and regulation and the work environment. This includes their production and deployment [14].
The medical and surgical interventions necessary to prevent this loss of life are known, and most maternal and newborn deaths are in principle preventable. The SoWMy 2021 report indicates that fully educated, licensed and integrated midwives supported by interdisciplinary teams and an enabling environment can deliver about 90% of essential sexual, reproductive, maternal, newborn and adolescent health (SRMNAH) interventions across the life course, even though they account for less than 10% of the global SRMNAH workforce [14]. Improving access to midwifery (including family planning & interventions for maternal and newborn health), could avert 83 percent of all maternal deaths, stillbirths and neonatal deaths [15]. Evidence shows that availability and utilisation of EmONC reduces maternal and newborn mortality [12, 16]. Skilled health personnel (SHP), commonly referred to as skilled birth attendants, should be trained to have the required competencies [17], and should work as part of an integrated team of maternal and newborn professionals (including midwives, nurses, obstetricians paediatricians and anaesthetists) performing all the signal functions of emergency obstetric and newborn care (EmONC). Such care provided within an ‘enabling environment’ that includes drugs, supplies, appropriate policies and a functional referral system is likely to result in optimisation of the health and well-being of women and newborns [18, 19]. In addition to competent, well resourced, multi-disciplinary maternal and newborn health (MNH) teams, country-level workforce management is required to ensure optimal recruitment, distribution and retention of and supervision of health workers is essential to improve access to high-quality care [20].
Kenya is committed to reducing preventable maternal and newborn deaths through the inclusion of EmONC training in its national health sector strategic and investment development plans [21, 22] and Vision 2030 [23] in the attainment of universal health coverage (UHC) targets. It developed its first emergency obstetric care training curriculum in 2006 and this was rolled-out in 2009 in 10 level 5 hospitals in the country in 2009 under the Making it Happen (MiH) I program supported by Liverpool School of Tropical Medicine (LSTM). In 2012, a revised Ministry of Health Kenya emergency obstetric and newborn care curriculum was implemented by LSTM to cover 15 additional counties located in the former Nyanza, Western and Central provinces. In 2014, the MiH program expanded the coverage of the trainings across all the 47 counties of Kenya. The MiH program had the objective to build the capacity of at least 80 percent of a multi-professional team of skilled health personnel (nurse/midwives, clinical officers and medical doctors including specialist obstetricians and paediatricians) working in the maternity units of health facilities to improve the availability and utilisation of EmONC and quality of maternal and newborn health outcomes.
Human resources for health, also known as the health workforce, is one of the building blocks proposed by the World Health Organization (WHO) Health Systems Framework and is central to achieving UHC and enhancing the achievement of the SDGs [24]. The proportion of births attended by SHP increased from 42% in 2003 to 62% in 2014 [7]. Despite this increase and the in-service EmONC trainings, the quality of maternal and newborn care provision is still sub-optimal [8]. Evidence on the status of EmONC services in Kenya has largely concentrated on the readiness and availability of these in health facilities, specifically focusing on equipment and supplies [25,26,27,28]. The results of three annual health facility assessments on availability and quality of EmONC services in Kenya between 2014 and 2016 in 18 counties showed that availability of equipment to perform all seven basic EmOC (BEmOC) signal functions (Table 1) increased progressively over the three annual assessments. In 2016, essential items for performing all seven BEmOC signal functions were available in 28 percent of health centres and dispensaries (a 14-fold increase from 2014) and 54 percent of hospitals (a two-fold increase from 2014) [26]. Little is documented on the availability of the trained SHP to provide essential EmONC services in the health facilities and poor staff retention after training may be reducing the optimal effect of the SHP strategy under the Ending Preventable Maternal Mortality global strategy and the Kenya strategic health sector development plan. For progress towards achievement of SDG targets, high quality health systems should focus on the population’s health needs and expectations, governance of the health sector and partnerships across sectors, platforms for care delivery, workforce numbers and skills, and tools and resources, from medicines to data [29].
The objectives of this study were to determine the availability and staff transfer rates of SHP trained in EmOC, and to identify the determinants of their retention within maternity units up to five years after the training to inform local and national solutions to optimise the impact of EmONC trainings.
Methods
Study Design
This was a cross-sectional review of EmONC trained SHP in five counties (Kilifi, Taita Taveta, Garissa, Vihiga and Uasin Gishu) supported by LSTM for a 5-year period from 2014 to 2019. Data collection was conducted between January–February 2020. Secondary data was extracted from an LSTM maintained in-service EmONC training database. The original data was not collected for research purposes but part of routine EmONC training administrative and registration purposes. No primary data was collected.
Study Setting
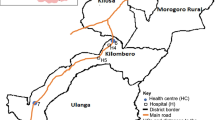
The assessment was conducted in the five counties (Kilifi and Taita Taveta from the coast, Garissa from the North Eastern Kenya, Vihiga from Western Kenya and Uasin Gishu from Rift Valley) supported by LSTM (Fig. 1). These counties in collaboration with LSTM conduct in-service EmONC trainings and other capacity building initiatives using a sustainable cost-sharing model. In this model, counties budget for and implement EmONC capacity building activities in their annual workplans. Multidisciplinary hands-on training within existing training facilities were organised without compromising the provision of services. Training and capacity building initiatives in EmONC target SHP working in maternity departments (mother and child health (MCH) clinics, maternity units, newborn units & gynecology units. Garissa and Kilifi were two of the 15 counties in Kenya with the highest burden of maternal mortality in 2014 [30]. Each of the counties has a single county referral hospital (except Uasin Gishu that has the national Moi Teaching and Referral Hospital) in addition to subcounty hospitals/faith-based/private hospitals, health centres and dispensaries providing basic and comprehensive emergency obstetrics and newborn care as appropriate according to the level, infrastructure and staffing levels of the facilities as per the minimum package of MNH services at different levels [31].
Data collection
Data was extracted from an LSTM maintained in-service training database (staff gender, cadre, year trained, hospital level, and hospital location-sub-county or county). Verification of current health facility in which trained SHP were deployed was confirmed using a specifically designed data collection tool by the respective county reproductive health departments (in collaboration with the subcounty reproductive health coordinators and the facility in-charges) and the study team. The data collection tool captured information about whether the SHP was still working at the same facility they were working in when they were trained in EmONC during the study period and still working in maternity department. If they were not still working in the training facility, the reasons for this (transferred, resigned, went for further education, retired or died) were documented.
Variables and measurements
The dependent variable was retention in maternity department, which was a binary outcome (yes or no). Retention in maternity department referred to a staff working in any of the following sections: mother and child health (MCH) clinics, maternity units (antenatal, intrapartum and postpartum), newborn units & gynecology units where they provide at least one EmONC signal function. The independent variables were: gender (male, female), cadre (nurse/midwife, medical doctor or clinical officer), interval from training in years (1, 2, 3, 4, 5 years), type of facility (dispensary, health centre, subcounty/county hospital) and county (Kilifi, Uasin Gishu, Taita Taveta, Garissa and Vihiga). Other variables (binary response; yes/no) included – staff still working at training facility, still working in maternity department, transferred, resigned, retired, died or unknown.
Data analysis
Data was entered in Microsoft Excel 2016, cleaned and responses coded as binary (yes = 1 and no = 0). This was then exported to StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP. for statistical analysis. Descriptive data analysis – frequencies and proportions of EmONC trained SHP and transfer rate by county were calculated. The association between staff transfers and gender in the counties was tested through two-sample test of proportions and p-values less than 0.05 were considered statistically significant. Associations between independent variables (gender, cadre, hospital level, county and interval from training in years) and the dependent/outcome variable (retention in maternity department) were tested using binary logistic regression to identify the determinants of EmONC trained SHP retention. Odds ratios, 95% confidence intervals and p-values were reported. Independent variables with p-values less than 0.05 were considered statistically significant as determinants of EmONC trained SHP retention.
Results
Distribution of EmONC trained healthcare workers
A total of 927 SHP were trained in the five counties between 2014 and 2019. Most trained SHP were nurse/midwives (677, 73%) followed by clinical officers (151, 16%) and medical doctors (91, 11%). At the level of facility, the majority of the SHP (621, 67%) were from the hospitals, followed by health centres (219, 24%) and dispensaries (87, 9%) (Table 2).
Overall, 427 (46.0%) were still working in the facility where they worked when they received the EmONC training, 394 (42.5%) had been transferred to other health facilities, 63 (6.8%) had resigned and the reason for non-retention was not known for 32 (3.5%) EmONC trained SHP. Uasin Gishu county had the highest proportion of trained SHP still working in the same facility as when they were trained in EmONC, (72.4%) with Vihiga county having the lowest at 28.7%. Regarding staff transferred, in Garissa county half (50.3%) of its trained SHP had been transferred to other facilities while Vihiga had the highest proportion of trained SHP resigning (28%). Kilifi and Taita Taveta counties had 7.7% and 13.2% of the trained SHP with unknown status as their availability could not be accounted for by the health facilities (Table 3). A total of 26 SHP were in school for further education with the majority (16, 62%) being doctors followed by nurse/midwives (8, 31%) and clinical officers (2, 8%). Overall, 18% (16 of 91) of the doctors, one percent each for nurse/midwives (8 of 677) and clinical officers (2 of 151) trained were pursuing further education at the time of the assessment.
Period of training
Overall, the distribution of SHP per year of EmONC training was highest in 2019 (207) and lowest in 2015 (161) with no major differences between the years for the combined counties. However, variations existed across the counties with Garissa receiving at least one training course in each of the five years while Kilifi, Uasin Gishu and Vihiga received three training courses each in the 5-year period. No EmONC training course was supported in 2018 across any of the five counties (Table 4).
Association between staff transfers and gender per county
There was a statistically significant difference in staff transfer rate by gender in Garissa and Vihiga counties with more male SHP (58%) transferred in Garissa compared to females (42%), P = 0.0015 with the reverse for Vihiga with more females (47%) compared to males (27%), P = 0.0109. There were no statistically significant differences in the transfers by gender for Kilifi, Uasin Gishu and Taita Taveta counties (P > 0.05) (Table 5).
Retention of SHP in maternity departments
Data from hospitals was analysed as SHP in these are facilities are deployed to serve in distinct service departments (e.g. maternity department, medical/surgical department etc.), as opposed to health centres and dispensaries where there are no distinct departments and SHP work across all the departments in most cases, usually under one roof. Overall, only 223 (36%) of the trained SHP were still working in maternity departments. This varies significantly across counties with Uasin Gishu county having the highest staff retention rate of 73% while Garissa had the lowest retention rate of 19% (Table 6).
Determinants of staff retention for EmONC trained SHP in maternity departments
County, cadre of staff and interval period from training were statistically significant determinants for staff retention in maternity departments. Compared to clinical officers and doctors, nurse/midwives were 3 times more likely to be retained in maternity departments (AOR 2.5, 95%CI 1.4—4.5, P < 0.0001). Compared to Garissa and Vihiga counties, EmONC trained SHP were 10 times in Uasin Gishu (AOR 9.5, 95%CI 4.6—19.5, P < 0.0001), four times in Kilifi (AOR 4.0, 95%CI 2.1—7.7, P < 0.0001) and twice in Taita Taveta (AOR 1.9, 95%CI 1.1—3.5, P = 0.032) more likely to be retained in maternity departments. Skilled health personnel were four times more likely to be retained in maternity departments during the first year after EmONC training (AOR 4.2, 95%CI 2.1—8.4, P < 0.0001). However, there was no association between 2 – 5 years interval since EmONC training and staff retention in maternity departments in the five counties (P > 0.05). Besides, there was no association between gender and staff retention in maternity departments (P > 0.05) (Table 7).
Discussion
The purpose of this study was to identify the determinants of staff retention after EmONC training in Kenya. The findings will be useful to improve the availability and performance of all the EmONC signal functions and improve the quality of maternal and newborn health services and outcomes at health facilities.
Overall, our findings demonstrate that although practices on staff deployment and transfers varied across counties, overall retention of EmONC trained SHP in maternity departments was low (36%) in the five counties. Nurse/midwives had the highest odds of being retained in the maternity departments five years after the EmONC training compared to clinical officers and doctors. Besides, only SHP trained within the last year had a higher chance of retention in maternity departments compared with those trained 2 – 5 years ago.
For a return on investment, in-service trained SHP can demonstrate greatest impact in performance and health outcomes by utilising the acquired knowledge and skills when retained in related departments/wards/units where they can apply the skills. High levels of attrition—defined broadly as exits from the workforce, which may be due to emigration, voluntary exits (e.g. to other sectors of employment), illness, death or retirement – lead to a large loss of public resources spent on in-service training of a health worker [32]. To plan effectively for the future, more focus needs to be dedicated to the issue of workforce retention and attrition following in-service training.
Midwives educated and regulated to international standards and working in well-equipped enabling environments are able to provide the full scope of interventions needed when they are fully integrated into a well-functioning health system within a multidisciplinary team to ensure availability of quality MNH and referral services when required for pregnancy and childbirth complications and emergencies [33, 34]. Following the skilled health personnel definition by WHO and others, it is critical for trained competent integrated teams working within an enabling environment to be available in maternity departments for pregnancy and childbirth services [35]. Our study shows that midwives are better retained compared to other cadres. While retention of nurse/midwives can be improved, retention of all the team is essential. Redeployments and staff movements or rotations may be inevitable due to shortages and inequitable distribution in these low resourced settings and so a system to ensure that those available are trained to maintain competency is required.
The overall average staff transfer rate of 43% compares with the overall annual attrition rate of between 3 and 44% from a rapid review of attrition rates of health workers from the workforce in different regions and settings by Lopes and colleagues [36]. This high transfer rate is not beneficial as the investments made for in-service training a SHP in key skills relevant to improving practice and outcomes in a distinct department is likely not to result in the desired impact. As a result, there is need for harmonised local practices and interventions including local staff deployment policies and guidelines at county and facility level to ensure that trained SHP with key skills are retained in departments they can utilise their competencies for improved health outcomes.
Our study showed that a significant proportion of doctors were pursuing further education compared to the other cadres. This could pose short to medium term challenges to the health facilities but represents a good long term investment in pursuing specialist training especially in these low resourced and inequitably distributed human resources for health settings [37, 38]. Evidence has also shown that attrition contributes to increased workload and worse working conditions for the remaining workforce, which in turn contributes to lower quality of care and worse health outcomes [39]. This calls for a robust capacity building approach to strengthen the skills of the remaining SHP serving in the health facilities at any given time to allow for a seamless transition when personnel leave for specialist training. This may include a mandatory and periodic EmOC training, including as part of induction of new members of the maternity care team, mentoring of all staff in order to maintain good quality of care.
Our study had strengths and limitations. To the best of our knowledge, this is the first study in Kenya to identify the determinants of in-service staff retention in maternity departments after EmONC training. Our study catalysed the funding and implementation of a project to improve the capacity of sub national health managers to monitor and improve staff retention after EmONC training. Specifically, the goal was to improve the capacity of County Health Management Teams (CHMT)/ government health facilities’ managers to manage retention of trained SHP in relevant departments for enhanced return on training investment and for improved maternal and newborn health outcomes. The project interventions were (1) a review of human resource management practices including maintaining a skills training database and development of healthcare workers’ dashboard at the health facilities, sub-counties and counties included in this study for future planning for deployment, capacity building and transfers/rotations based on specific skillset for greatest impact on quality of care and (2) the drafting and implementation of a declaration of intent – a signed agreement between health facilities and county health managers whose goal was to improve MNH health outcomes by committing to intentional transfer of EmONC trained staff and a sustainable training approach supported by facility and county health management. The intended outcome of the project was that policy makers and health facility managers have capacity to ensure that all maternity care staff are trained in EmONC at any given time, supported by at least one trained mentor per facility. Our study did not examine annual trends in retention/transfers and whether the transfers are to relevant departments where healthcare workers can demonstrate the greatest impact either intra-facility, intra-county or inter-facility and intercounty. As time goes by after training, more staff moving either within or between health facilities or departments is not surprising – whether due to personal, higher education, logistical reasons or career advancement/promotion. However, our study did not establish who decides the movement of the trained staff – whether by staff choice or by authorities. Use of secondary data – the training registration data captured misses out on other important determinants for staff turnover and transfers such as healthcare worker’s personal (physical, mental – emotional and social including marital status and other family responsibilities), job satisfaction at the current position, social support – opportunities for career development, stress at the current position and organisational factors (reward, salary and other benefits) which would have provided a deeper understanding of the key determinants for staff turnover in the maternity departments and health facilities [40,41,42]. Future research focusing on primary data collected from healthcare workers, health facility and county health managers should integrate this data to establish salient factors contributing to poor staff retention following investments in building the capacity of in-service health workforce.
Our findings have implications for practice and policy. For a return on investments and impact, counties and health facilities should strengthen capacity building and retention strategies of all skilled health personnel with EmONC skills in maternal and newborn health. Health managers should develop and implement local strategies, policies and protocols for staff deployment/transfers/replacement and retention based on key competencies by SHP and maintain a skills training database as well as provide an enabling working environment and motivation for SHP to apply the acquired competencies to prevent unnecessary attrition as well as preventing occupational stress [43,44,45,46]. Further research is needed to examine the annual trends in SHP transfers and retention in relevant departments. In addition, a system should be in place to monitor and investigate the SHP transfer or retention, maintain a staff training database, utilize and implement a staff training dashboard and the association between trained staff retention and MNH outcomes should be monitored regularly by facility managers.
Conclusion
Retention of EmONC trained SHP in the relevant maternity departments where they can demonstrate the greatest impact was low at 36 percent. Two out of five (42.5%) EmONC trained SHP were transferred to other health facilities post-training. SHP were more likely to be retained during the first year after training compared to the subsequent years and varied from county to county. County policies and guidelines on SHP deployment and transfers/retention should be strengthened to optimise the benefits of EmONC training. The study improved the capacity of sub national health managers to monitor and improve staff retention after EmONC training through a skills training database, development of healthcare workers’ dashboard to monitor training needs and deployments/transfers and declaration of intents between health facilities and counties advocating for and committing to a sustainable staff training and retention in areas where they can demonstrate greatest impact. Future studies to examine the effect of staff transfers or retention on the maternal and newborn health practices and outcomes in the health facilities as well as whether the staff movement is by choice or by the authorities, and other individual or institutional factors through participant interviews are needed.
Availability of data and materials
The datasets used and/or analysed during the study are available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odds ratio
- BEmONC:
-
Basic emergency obstetrics and newborn care
- CEmONC:
-
Comprehensive emergency obstetrics and newborn care
- CI:
-
Confidence Interval
- EmONC:
-
Emergency Obstetrics and Newborn Care
- EOC:
-
Emergency obstetrics care
- LSTM:
-
Liverpool School of Tropical Medicine
- MiH:
-
Making it Happen
- MNH:
-
Maternal and newborn health
- MOH:
-
Ministry of Health
- SDG:
-
Sustainable development goal
- SHP:
-
Skilled health personnel
- SoWMy:
-
State of the World Midwifery
- WHO:
-
World Health Organization
References
WHO. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF: UNFPA, World Bank Group and the United Nations Population Division; 2019. Available from: https://apps.who.int/iris/bitstream/handle/10665/327596/WHO-RHR-19.23-eng.pdf?sequence=13&isAllowed=y.
UN Inter-agency Group for Child Mortality Estimation (UN-IGME). Levels & Trends in Child Mortality: Report 2019 - Estimates developed by the UN Inter-agency Group for Child Mortality Estimation. New York, USA: United Nations Children's Fund; 2019. Available from: https://www.unicef.org/media/60561/file/UN-IGME-child-mortality-report-2019.pdf.
Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2016;4(2):e98–108.
Chou D, Daelmans B, Jolivet RR, Kinney M, Say L. Ending preventable maternal and newborn mortality and stillbirths. BMJ. 2015;351: h4255.
United Nations. Transforming our World: The 2030 Agenda for Sustainable Development Goals 2015. Available from: https://sustainabledevelopment.un.org/post2015/transformingourworld.
WHO. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, . Geneva: World Health Organization; 2019. Available from: https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/.
Kenya National Bureau of Statistics (KNBS) and ICF International. Kenya Demographic and Health Survey (KDHS) 2014 2015. Available from: https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf.
MOH (Kenya). Saving Mothers Lives 2017, First Confidential Report into Maternal Deaths in Kenya. 2017. Available from: https://cmnh.lstmed.ac.uk/sites/default/files/content/centre-news-articles/attachments/CEMD%20Main%20Report%20Sept%203%20FINAL-%20Full%20Report.pdf.
Healthy Newborn Network. The Lancet Every Newborn Series. Lancet [Internet]. 2014 15th May 2022. Available from: https://www.healthynewbornnetwork.org/resource/the-lancet-every-newborn-series/.
Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? The Lancet. 2014;384(9940):347–70.
Ameh CA, van den Broek N. Making It Happen: Training health-care providers in emergency obstetric and newborn care. Best Pract Res Clin Obstet Gynaecol. 2015;29(8):1077–91.
Ameh CA, Mdegela M, White S, van den Broek N. The effectiveness of training in emergency obstetric care: a systematic literature review. Health Policy Plan. 2019;34(4):257–70.
Mason E, McDougall L, Lawn JE, Gupta A, Claeson M, Pillay Y, et al. From evidence to action to deliver a healthy start for the next generation. The Lancet. 2014;384(9941):455–67.
World Health Organization, United Nations Population Fund, International Confederation of Midwives. The State of the World’s Midwifery 2021: Building a health workforce to meet the needs of women, newborns and adolescents everywhere 2021. Available from: https://www.unfpa.org/publications/sowmy-2021.
ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. The Lancet. 2014;384(9949):1226–35.
Ameh C, van den Broek N. Making it happen: training health-care providers in emergency obstetric and newborn care. Best Pract Res Clin Obstet Gynaecol. 2015;29(8):1077–91.
World Health Organization. Defining competent maternal and newborn health professionals. Geneva: World Health Organization; 2018. Available from: https://apps.who.int/iris/bitstream/handle/10665/272817/9789241514200-eng.pdf?ua=1.
Graham WJ, Bell JS, Bullough CH. Can skilled attendance at delivery reduce maternal mortality in developing countries? Safe motherhood strategies: a review of the evidence. 2001.
Adegoke A, Van Den Broek N. Skilled birth attendance-lessons learnt. BJOG. 2009;116:33–40.
WHO. Strategies towards ending preventable maternal mortality (EPMM) 2015 2nd March 2021]. Available from: https://apps.who.int/iris/handle/10665/153544.
Ministry of Health. Kenya Health Sector Strategic Plan (KHSSP) July 2018–June 2023: Transforming Health Systems: Attainment of Universal Health Coverage by 2022 2020. Available from: https://www.health.go.ke/wp-content/uploads/2020/11/Kenya-Health-Sector-Strategic-Plan-2018-231.pdf.
MOH. The Kenya Health Sector Strategic and Investment Plan - KHSSP July 2012-June 2017.: Government of Kenya; 2013. Available from: http://www.nationalplanningcycles.org/sites/default/files/country_docs/Kenya/draft_khssp_-_14_november_5_.pdf.
Kenya Ro. Kenya Vision 2030 2007. Available from: http://vision2030.go.ke/inc/uploads/2018/05/Vision-2030-Popular-Version.pdf.
World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies: World Health Organization; 2010. Available from: https://apps.who.int/iris/bitstream/handle/10665/258734/9789241564052-eng.pdf.
Ziraba AK, Mills S, Madise N, Saliku T, Fotso J-C. The state of emergency obstetric care services in Nairobi informal settlements and environs: results from a maternity health facility survey. BMC Health Serv Res. 2009;9(1):46.
MEASURE Evaluation PIMA. Availability and Quality of Emergency Obstetrical and Newborn Care Services in Kenya: Results of Three Annual Health Facility Assessments. 2017.
Echoka E, Kombe Y, Dubourg D, Makokha A, Evjen-Olsen B, Mwangi M, et al. Existence and functionality of emergency obstetric care services at district level in Kenya: theoretical coverage versus reality. BMC Health Serv Res. 2013;13(1):1–9.
MOH (Kenya). Kenya Service Availability and Readiness Assessment Mapping (SARAM) Report. Nairobi: Ministry of Health; 2013. Available from: http://guidelines.health.go.ke:8000/media/Kenya_Saram_Report.pdf.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–252.
United Nations Population Fund (UNFPA Kenya). Counties with the Highest Burden of Maternal Mortality. Kenya: United Nations Population Fund (Kenya Country Office); 2014. Available from: http://countryoffice.unfpa.org/kenya/2014/08/13/10333/counties_with_the_highest_burden_of_maternal_mortality/.
MOH (Kenya). National Guidelines for Quality Obstetrics and Perinatal Care: Kenya [MNH Reference Manual]. Nairobi: Ministry of Health, Department of Health; 2012. Available from: https://www.k4health.org/sites/default/files/National%20Guidelines%20for%20Quality%20Obstetrics%20and%20Perinatal%20Care.pdf.
Kollar E, Buyx A. Ethics and policy of medical brain drain: a review. Swiss Med Wkly. 2013;143:1–8.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience: World Health Organization; 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf.
Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. The Lancet. 2014;384:1129–45.
WHO. Definition of skilled health personnel providing care during childbirth: the 2018 joint statement by WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA. Geneva: World Health Organization; 2018. Available from: https://apps.who.int/iris/bitstream/handle/10665/272818/WHO-RHR-18.14-eng.pdf?ua=1
Castro Lopes S, Guerra-Arias M, Buchan J, Pozo-Martin F, Nove A. A rapid review of the rate of attrition from the health workforce. Hum Resour Health. 2017;15(1):21.
Adegoke A, Utz B, Msuya SE, Van Den Broek N. Skilled Birth Attendants: who is who? A descriptive study of definitions and roles from nine Sub Saharan African countries. PLoS ONE. 2012;7(7): e40220.
WHO. World Health Statistics. 2014.
Serour GI. Healthcare workers and the brain drain. Int J Gynecol Obstet. 2009;106(2):175–8.
Darkwa EK, Newman MS, Kawkab M, Chowdhury ME. A qualitative study of factors influencing retention of doctors and nurses at rural healthcare facilities in Bangladesh. BMC Health Serv Res. 2015;15(1):1–12.
Heidari M, Seifi B, Gharebagh Z. Nursing staff retention: Effective factors. Ann Trop Med Public Health. 2017;10(6):1467–73.
Chiao L-H, Wu C-F, Tzeng I, Teng A-N, Liao R-W, Yu LY, et al. Exploring factors influencing the retention of nurses in a religious hospital in Taiwan: a cross-sectional quantitative study. BMC Nurs. 2021;20(1):1–8.
Allen DG. RetainingTalent: A Guide to Analyzing and Managing Employee Turnover: SHRM Foundation. 2008.
Baba A, Martineau T, Theobald S, Sabuni P, Nobabo MM, Alitimango A, et al. Developing strategies to attract, retain and support midwives in rural fragile settings: participatory workshops with health system stakeholders in Ituri Province, Democratic Republic of Congo. Health Res Policy Syst. 2020;18(1):1–14.
Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. 2014(11):CD002892.pub4.
Brand SL, Thompson Coon J, Fleming LE, Carroll L, Bethel A, Wyatt K. Whole-system approaches to improving the health and wellbeing of healthcare workers: a systematic review. PLoS One. 2017;12(12): e0188418.
Acknowledgements
This paper has been developed under the Reducing Maternal and Newborn Deaths programme funded by the UK Government as part of efforts to improve access and utilisation of all the EmOC signal functions for quality maternal and newborn health services at health facilities and better maternal and perinatal outcomes in Kenya. We specially acknowledge the collaboration and support provided by Gladys Etemesi (Kilifi County Reproductive Health Coordinator), Margaret Chuya (Taita Taveta County Reproductive Health Coordinator), Veronica Musiega (Vihiga County Reproductive Health Coordinator) and Carolyne Chemoiywo (Uasin Gishu County Reproductive Health Coordinator) and the respective counties’ health departments through the reproductive health offices using the cost-shared model of health financing to improve the quality of MNH services. Lastly, the authors would like to acknowledge the special logistical support provided by the LSTM team in Kenya – Veneranda Kamanu, Roselynne Githinji, David Ndakalu, Esther Wekesa, Eunice Ngundo and Pamela Godia during the data collection.
Funding
None.
Author information
Authors and Affiliations
Contributions
DS and CA conceptualized the idea and designed the study. DS performed data extraction, cleaning, analysis and interpretation of the results, drafted the primary manuscript, reviewed and prepared it for publication. CA, HA, ET and IB interpreted the results and substantively reviewed the manuscript for publication. IN, OM, ME, SG, FI and LN participated in the design of the study procedures, data collection and reviewed the drafts and final manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Secondary data was used. The original data was not collected for research purposes and was a byproduct of routine EmONC training administrative and registration purposes. No institutional research and ethics review was sought. The Pre-service Task Force of the Kenya Ministry of Health approved the monitoring and evaluation plan for the project, in line with relevant guidelines and regulations. All data from the training database used was deidentified before analysis and this was part of the monitoring of implementation to strengthen capacity of the workforce through in-service EmONC training interventions, and all SHP consented/registered to participation in the trainings. Data was accessed from the internal LSTM maintained training database in Kenya and no administrative permissions were required to access the raw data.
Consent for publication
Not applicable (as our manuscript does not contain any personal information, or data in any form (including any individual details, images or videos).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shikuku, D.N., Nyaoke, I., Maina, O. et al. The determinants of staff retention after Emergency Obstetrics and Newborn Care training in Kenya: a cross-sectional study. BMC Health Serv Res 22, 872 (2022). https://doi.org/10.1186/s12913-022-08253-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08253-2