Abstract
Background
Increasing spending and use of prescription drugs pose an important challenge to governments that seek to expand health insurance coverage to improve population health while controlling public expenditures. Patient cost-sharing such as deductibles and coinsurance is widely used with aim to control healthcare expenditures without adversely affecting health.
Methods
We conducted a systematic umbrella review with a quality assessment of included studies to examine the association of prescription drug insurance and cost-sharing with drug use, health services use, and health. We searched five electronic bibliographic databases, hand-searched eight specialty journals and two working paper repositories, and examined references of relevant reviews. At least two reviewers independently screened the articles, extracted the characteristics, methods, and main results, and assessed the quality of each included study.
Results
We identified 38 reviews. We found consistent evidence that having drug insurance and lower cost-sharing among the insured were associated with increased drug use while the lack or loss of drug insurance and higher drug cost-sharing were associated with decreased drug use. We also found consistent evidence that the poor, the chronically ill, seniors and children were similarly responsive to changes in insurance and cost-sharing. We found that drug insurance and lower drug cost-sharing were associated with lower healthcare services utilization including emergency room visits, hospitalizations, and outpatient visits. We did not find consistent evidence of an association between drug insurance or cost-sharing and health. Lastly, we did not find any evidence that the association between drug insurance or cost-sharing and drug use, health services use or health differed by socioeconomic status, health status, age or sex.
Conclusions
Given that the poor or near-poor often report substantially lower drug insurance coverage, universal pharmacare would likely increase drug use among lower-income populations relative to higher-income populations. On net, it is probable that health services use could decrease with universal pharmacare among those who gain drug insurance. Such cross-price effects of extending drug coverage should be included in costing simulations.
Similar content being viewed by others
Background
As the US strives to reduce its uninsurance rate, it faces an intensifying challenge of increasing out-of-pocket costs in employer-sponsored health insurance [1, 2]. All the while Canada is debating how best to provide drug insurance to all its residents [3]. Canada is often cited as the only high-income country with universal health insurance coverage lacking universal coverage for prescription drugs [4]. Increasing spending and use of prescription drugs pose an important challenge to governments that seek to expand health insurance coverage to improve population health while controlling public expenditures. Patient cost-sharing such as deductibles and coinsurance is widely used with aim to control healthcare expenditures without adversely affecting health [5].
Since the seminal RAND Health Insurance Experiment [6], numerous studies have examined, at various times and across diverse settings, the impact of health insurance generally, and drug insurance in particular, on utilization and health outcomes. For example, in the US, the introduction of Medicare Part D in 2003 and the Affordable Care Act in 2010 have generated a wealth of new research [7, 8]. Likewise in Canada, the prospect of universal pharmacare and important changes to provincial drug programs such as the 1997 public/private prescription drug program that covered all Québec residents and British Columbia’s adoption of income-based Pharmacare in 2003 in place of an age-based drug benefits program have resulted in an abundance of new analyses [3, 9, 10]. Countless reviews have examined the impact of prescription drug insurance and drug cost-sharing on an array of outcomes such as drug use, health services use, and health, in varied settings and among heterogenous populations. To our knowledge, there has not been an attempt to assess the quality and synthesize evidence from existing reviews. In addition to identifying the strength/credibility of combined associations from reviews to present an objective and comprehensive synthesis of the evidence, such a review of reviews can identify knowledge gaps in the literature, provide useful guidance for future reviews, and have greater implications for policy and practice.
We conducted a systematic umbrella review in order to provide a closer examination of what policy introductions of prescription drug coverage (with and without cost-sharing) would mean for both individuals and governments financing this coverage. We examined reviews that studied the association between having prescription drug coverage (primary and supplementary), as well as varying types and levels of cost-sharing, and:
-
1.
the utilization of prescription drugs (i.e., own-price effects on drug use);
-
2.
the utilization of healthcare services (i.e., cross-price effects on the use of health services such as physician, emergency department, and inpatient services);
-
3.
health outcomes (i.e., own-price effects on health outcomes);
We also examined the degree to which the associations identified in 1–3 above differed across levels of socioeconomic status (SES, e.g., income, education), populations of differing health status such as the chronically ill, age, and sex.
Methods
A review protocol was prepared in advance and registered with PROSPERO (CRD42017052018). We searched five electronic bibliographic databases: MEDLINE, Embase, Scopus, EconLit, and Health Systems Evidence. Grey literature was searched via the New York Academy of Medicine Grey Literature Report, Open Grey, Google, and Google Scholar. Eight specialty journals (BMC Health Services Research, Health Affairs, Healthcare Policy, Health Economics, Journal of Health Economics, Health Economics, Policy and Law, Health Services Research, and Medical Care Research and Review) and two working paper repositories (RePEc, Research Papers in Economics and the National Bureau of Economic Research working paper series) were ‘hand-searched.’ We examined references of included reviews and of reviews that cited key studies using Web of Science and Google Scholar. The database search was last updated on September 15, 2020. At least two reviewers, using distillerSR, screened titles and abstracts of citations to determine relevance, then full text if relevance was unclear.
Inclusion and exclusion criteria
Types of studies: all reviews (e.g., narrative, rapid, scoping, systematic, meta-analysis, meta-regression). Types of interventions: (1) insurance: all studies that examined the expansion of prescription drug insurance, irrespective of the insurance provider (e.g., government, employers, professional associations) and studies that examined partial or full-delisting of prescription drugs from insurance coverage; (2) cost-sharing: all studies that examined any form of direct patient payment for prescription drugs including, but not limited to, fixed copayment, coinsurance, ceilings, and caps. Types of outcomes: all reviews that included as an outcome any of drug utilization, health services utilization, or health outcomes. Time period: all reviews published since January 2000. Languages: we included only studies written in English and French. We excluded reviews that focused solely on low- and middle-income countries.
Quality assessment and data extraction
We used the Assessment of Multiple Systematic Reviews (AMSTAR) measurement tool as a methodological guide [11]. Although AMSTAR’s focus is primarily on the reporting quality of reviews, we paid particular attention to the quality assessment conducted in each review. At least two reviewers independently extracted detailed study characteristics for each included review using a standardized form, including all AMSTAR 2 items (see Additional file 1). The following study characteristics were extracted, where possible: citation, type of review, population investigated, research question, outcomes studied, whether there was an ‘a priori design’ and duplicate study selection and data extraction, the comprehensiveness of the search including if grey literature was searched, year/month of last search, whether the keywords/search strategy were reported, total number of studies included, total number of studies included that focused on drug insurance and/or cost-sharing, whether a list of included and excluded studies were provided, whether the characteristics of the included studies were provided, whether the scientific quality of the included studies was assessed, documented, and used appropriately in formulating conclusions, whether the methods used to combine the findings of studies were appropriate, whether the likelihood of publication bias was assessed, whether funding and competing of interests were clearly reported, key results for each of drug use, healthcare services utilization, and health, and reviews’ conclusion (as stated by the authors). In assessing the quality of the included studies, we paid particular attention to the following components: ‘a priori’ design; duplicate study selection and data extraction; systematic search strategy; presentation of characteristics of included studies and list of excluded studies and reasons for exclusion; quality assessment of included studies; and the generalizability of the findings. We did not compute total scores as empirical evidence does not support their use [12,13,14]. We created summary tables, organized by outcome and subgroup, using our completed standardized forms. For each study, we highlighted the direction and magnitude of the associations. In our descriptive table, we present the study citations, research question, outcomes studied, study selection and extraction process, quality assessment, and limitations/risk of bias. Lastly, given the current policy debate surrounding universal pharmacare in Canada, we also reported the total number of Canadian studies included that focused on drug insurance and/or cost-sharing [3].
Results
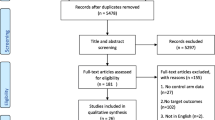
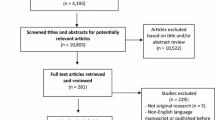
The database search produced 5567 records after the removal of duplicate citations, from which 5261 were excluded based on the title/abstract screen and 268 were subsequently removed after a full-text screen, yielding 38 reviews that met all inclusion criteria (Fig. 1). Selected study characteristics and our assessment of study’s limitations are presented in Table 1. Detailed characteristics of included studies are presented in the Additional file 1. Of 38 reviews, 16 focused on the general population of which eight also commented on subgroups (e.g., seniors, the poor, and chronically ill), nine focused on seniors (most often on the US Medicare population), and 11 focused on the poor and/or chronically ill. A further two reviews examined drug insurance and cost-sharing among Canadians and one review examined publicly insured populations. Most included reviews were narrative reviews. We included six meta-analyses and one meta-regression. A list of excluded studies and reasons for exclusion is provided in the Additional file 1. We present a synthesis of results in Table 2 and more detailed findings for each reviews in Tables 3, 4, 5, 6, 7, and 8.
Associations of prescription drug insurance and cost-sharing with drug utilization
Examining the 20 reviews that investigated, with a focus on the general population, the association between having prescription drug coverage or varying levels of cost-sharing on drug use, there was a clear inverse association, but the magnitude of the association was unclear (Tables 2 and 3). Across the literature, the outcomes were reported in elasticities, changes in drug use, and changes in medication adherence, with reviews published between 2004 and 2019. Reviews assessing medication adherence generally found that the absence of prescription drug insurance, or having copayments, reduced medication adherence [21, 32, 36, 41, 46] with specific estimates ranging as low as a 0.4% decrease in adherence for each dollar increase in copays, and an average reduction of 3% after 1 year of copayment reductions [32]. Another review reported that publicly insured patients who were required to pay copays for their prescription medicines had 11% higher odds of reporting nonadherence relative to those who faced no copayments [36]. However, not all associations were statistically significant, with variations in adherence reported depending on the drug class. Reviews reporting on drug use also generally found consistent results, reporting that increasing cost-sharing or not having drug insurance decreased drug use, but with varying impacts by drug class or type, and some not reporting clear effect sizes or very small to moderate impacts [16, 26, 27, 37, 39, 40, 51]. Own-price elasticities reported in seven older reviews, published in 2011 or earlier, generally found that the demand for prescription drugs was inelastic, with most estimates ranging from − 0.2 to − 0.6 depending on the drug class and essentiality, suggesting that a 10% increase in price resulted in a 2 to 6% decrease in use [19, 22,23,24,25, 29, 30].
Differences between subgroups: SES, health status, age, and sex/gender
These results varied when assessing vulnerable population subgroups including the elderly, children, the poor, and the chronically ill (Tables 2 and 4). We identified two reviews that focused specifically on low-income groups [17, 44] and six that generally commented on low-SES populations [23,24,25, 27, 29, 37]. One older review focusing on low-income populations reported price elasticities ranging from − 0.3 and − 0.5 and argued there was unequivocal evidence that increasing cost-sharing decreased drug use among the poor [17]. This conclusion was supported by all other reviews except one [25]. However, when comparing price responsiveness between the poor and non-poor, four reviews provided mixed or no evidence that individuals with lower income were more price sensitive than those with higher income [23,24,25, 27]. Although one review concluded that higher copayments led to a greater reduction in drug use in vulnerable populations (low socioeconomic status measured by income, education, or social status) than the non-vulnerable population) [37].
With respect to the chronically ill, reviews generally concluded that higher copayments or the absence of drug insurance were associated with increased medication nonadherence for a range of illnesses and drug classes [17, 23, 25, 27, 33, 34, 38, 42,43,44,45,46,47,48,49]. However, the magnitude of effects was often unclear and difficult to synthesize given the diverse outcome measures employed in each review. A recent meta-analysis focusing on individuals with chronic cardiovascular diseases found that access to insurance or other programs that assisted with medication costs resulted in a 37% decrease in the risk of medication nonadherence [48]. Another recent review examined the association between cost-sharing on specialty drugs for rheumatoid arthritis, multiple sclerosis, and cancer, and the use of specialty drugs and nondrug medical services, and health outcomes [43]. Although no research was found that pertained to the use of nondrug medical services and health outcomes, the review found that higher cost-sharing was associated with higher prescription abandonment and discontinuation/persistence, and lower initiation and adherence. Findings varied by diseases but generally indicated stronger effects for noninitiation or abandonment of a prescription at the pharmacy and somewhat smaller effects for refill behaviour once patients initiated therapy [43]. Lastly, we are unable to comment on how the impact of cost-sharing or drug insurance on drug use compared to drug use by the healthy population as such comparisons were not drawn in the literature.
The elderly was the most studied group apart from the chronically ill, with 14 reviews focusing on this particular population. Of the 14 reviews, 11 concluded that seniors were sensitive to price changes [7, 15, 18, 21, 27,28,29,30,31, 47, 51]; drug use decreased with increasing cost-sharing or the lack of drug insurance, with the others finding mixed or no evidence for price responsiveness among older adults [20, 24, 35]. Again, the magnitude of effect was difficult to evaluate, and we are unable to comment on age differences (elderly vs non-elderly) in price responsiveness.
Only two reviews mentioned potential sex/gender differences in responsiveness to changes in cost-sharing or insurance. One review reported that one study had found that a drug policy change had not reduced the use of essential cardiac medications among Québec elderly who experienced acute myocardial infarction and that this finding did not vary by sex [23]. Another review reported that one study had found that low-income single elderly women were much less price responsive to drug fees than low-income single elderly men in British Columbia [17].
Associations of prescription drug insurance and cost-sharing with health services use
On the whole, most reviews concluded that increasing prescription drug cost-sharing or limiting drug insurance were associated with higher healthcare services utilization, such as emergency room visits, hospitalizations, and outpatient visits in the general population, although the magnitudes of associations were unclear (Tables 2 and 5) [24, 25, 30, 32, 37, 39, 50]. Two older reviews (published in 2005 and 2007) found no evidence of associations between prescription drug cost-sharing and changes in the use of healthcare services such as outpatient visits or hospitalizations [19, 23] while three relatively more recent reviews from 2010, 2015, and 2018 concluded the evidence was mixed or uncertain [26, 40, 46].
Differences between subgroups: SES, health status, age, and sex/gender
When assessing results by subgroups, the findings were generally the same as those reported in the general population (Tables 2 and 6). Three reviews that focused on both the poor and chronically ill found that, in most studies reviewed, drug cost-sharing was associated with increased emergency department visits, hospitalizations, and nursing home admissions [17, 29, 44]. The magnitude of these associations was, however, unclear. A more recent review of cost-related nonadherence to prescription medications in Canada provides further support and reported that, among the elderly and individuals on social assistance, the introduction of cost-sharing was associated with increased rates of emergency department and physician visits [46]. It was unclear, however, if any of these associations differed in magnitude when compared to healthier or higher-income populations.
Five reviews specifically discussed the association between prescription drug cost-sharing and healthcare services utilization in the chronically ill [23, 25, 27, 45, 46]. Four of these reviews found evidence that prescription drug cost-sharing was associated with increased use of health services including greater hospitalizations, emergency room visits, and nursing home admissions [23, 25, 27, 46]. The magnitude of these associations was, however, unclear. One review concluded that there was ‘no strong’ evidence showing a direct association between drug cost-sharing and healthcare services use among patients with diabetes mellitus, although there was limited evidence that higher drug copayments were associated with an increased risk of hospitalization among patients with heart failure [45]. Nonetheless, it was unclear how chronically ill patients compared to the healthier population in terms of the association between drug-cost sharing and healthcare services use.
Five reviews examined the association between drug cost-sharing or drug insurance and healthcare services utilization in older adults [15, 18, 20, 29, 46]. Four of these reviews concluded that there was some evidence that higher drug cost-sharing and lack of insurance were associated with greater hospitalizations or nursing home admissions in seniors, although the magnitude was unclear, whereas one older review reported inconclusive findings [18]. It was also unclear how seniors compared to non-seniors with respect to healthcare service utilization when faced with drug cost-sharing. Lastly, one recent review reporting on the association between drug cost-sharing and health services use found that government insurance plans with high-cost sharing on generic drugs were associated with lower use of health services among children. Again, the magnitude of effect was unclear and no comparison was drawn with older individuals [51].
Only one review mentioned potential sex/gender differences in responsiveness to changes in cost-sharing or insurance. One review reported that one study had found that a drug policy change had not reduced the use of medical services among Québec elderly who experienced acute myocardial infarction and that this finding did not vary by sex [23].
Associations of prescription drug insurance and cost-sharing with health
A total of 21 reviews reported on the association between prescription drug insurance or cost-sharing and health outcomes (Tables 2 and 7). Eleven of these reviews explored the association in the general population [19, 23,24,25,26, 29, 30, 32, 37, 39, 50] of which two focused specifically on the Canadian population [16, 46]. Six reviews examined health generally [23, 25, 26, 29, 30, 46], five all-cause mortality [16, 24, 37, 39, 50], four self-reported health [19, 32, 39, 50] and one review investigated cardiovascular-related mortality [50], adverse events [32] and vascular events [50].
Overall, there was limited evidence of a clear relationship between prescription drug insurance or cost-sharing and health outcomes. With one exception [32], several older reviews reported that very few empirical studies had examined the association between drug insurance/cost-sharing and health, and concluded that, on the whole, existing studies provided mixed or unclear evidence [19, 23, 25, 26, 29, 30, 37]. More recent reviews (published in 2015 and 2019) tended to conclude that drug insurance and lower cost-sharing were associated with better health. One review found that individuals with drug insurance had better health outcomes than those without, that drug insurance restrictions led to a decline in health status, and that extending drug coverage yielded mixed results [39]. Another review found that in all included studies, there was an inverse association between higher drug cost-sharing and health outcomes such as self-assessed health, major vascular events, cardiovascular-related mortality and all-cause mortality [50]. The above conclusions were, however, all based on very few primary studies.
Differences between subgroups: SES, health status, age and sex/gender
Reviews highlighted a paucity of studies that examined the associations of prescription drug insurance and cost-sharing with health among the poor and the chronically ill (Tables 2 and 8). Two older reviews found some evidence that drug cost-sharing was associated with adverse health outcomes in lower-income populations and another suggested that low-income individuals were at greater risk of poor health outcomes due to increased cost-sharing than higher-income individuals [17, 23, 29]. Three of four reviews that specifically discussed the chronically ill found that cost-sharing was associated with adverse health outcomes in patients with heart disease, hypertension, lipid disorders, and diabetes [30, 34, 45]. Two of the three reviews, however, discussed the association between health insurance generally (i.e., including but not limited to drug insurance) and health outcomes [30, 34]. One review found no evidence of an association between drug cost-sharing and clinical outcomes among patients with cardiovascular-related chronic disease [38]. Four older reviews specifically focused on the association between insurance and cost-sharing and health among seniors [15, 18, 20, 35]. Two reviews reported mixed findings [20, 35] while two reviews reported that higher cost-sharing was associated with worse health outcomes, including higher mortality and morbidity among seniors [15, 18]. One review pointed out that this association did not remain when there were generous provisions in place to protect vulnerable populations from incurring undue financial risk as a result of cost-sharing [18]. However, similar to previous reported outcomes, no comparisons were drawn between the poor and non-poor, the chronically ill and non-chronically ill, and the elderly and non-elderly and how health outcomes may have differed between them. We did not identify a single review that discussed potential differences between sex/gender in the association of prescription drug insurance and cost-sharing with health.
Risk of bias assessment
In our umbrella review, we found that the most common limitations were the lack of an a priori study design and issues with clarity in reporting search strategies and results. Reviews often did not clearly report data screening and extraction procedures including exclusion and inclusion criteria, had poorly described search strategies or non-systematic search strategies, failed to provide or clearly synthesize study characteristics and, most often than not, did not provide a list of excluded studies. The most important limitation was, however, the lack of attention given to quality assessments. About half of the included reviews did not conduct any formal quality assessments and many that did often failed to appropriately describe and justify their quality assessment.
Discussion
Main findings
We found consistent evidence that changes in drug cost-sharing and/or drug insurance were associated with drug use. Lower cost-sharing and having drug insurance were associated with increased drug use while higher drug cost-sharing and the lack or loss of drug insurance were associated with decreased drug use. We also found consistent evidence that the poor, the chronically ill, seniors and children were similarly responsive to changes in insurance and cost-sharing. Although the direction of the associations between changes in drug insurance and cost-sharing was clear, the magnitude of these associations was difficult to ascertain. The demand for prescription drugs is most certainly inelastic (i.e., a percentage change in price is associated with a smaller percentage change in demand) with an own-price elasticity ranging from about − 0.2 to − 0.6, depending on drug class, intervention, disease, and population studied. We found that lower drug cost-sharing and drug insurance were associated with lower healthcare services utilization including emergency room visits, hospitalizations, and outpatient visits. Similar results were found in all population subgroups aside from children, although the literature on the poor and children was very limited. We did not find consistent evidence of an association between cost-sharing and insurance and health. While several reviews reported mixed or no evidence, more recent reviews tended to conclude that there was some evidence that increased cost-sharing led to poorer health outcomes because of reduced drug adherence. Again, the magnitude of effect was unclear and evidence on the elderly, chronically, ill, and poor was limited and mixed. Lastly, we did not find any evidence that the association between drug insurance or cost-sharing and drug use, health services use, or health differed by SES, health status, age or sex.
We found two reviews that specifically studied the Canadian population. An older review examined Canadian evidence of the effects of cost-sharing mechanisms of provincial drug benefit programs on drug utilization and health [16]. A more recent scoping review examined the extent, determinants, and consequences of cost-related nonadherence to prescription medications in Canada [46]. The two reviews generally found that higher drug cost-sharing reduced drug use. There was, however, little discussion of the magnitude of associations or subgroup differences in price responsiveness [16, 46]. The review of cost-related nonadherence to prescription medications found limited and mixed evidence that cost-sharing increased health services use [46]. A more recent review examined the prevalence, predictors, and clinical impact of cost-related medication nonadherence in Canada [52]. Along with lower income, younger age, and poorer health, high out-of-pocket spending and drug insurance were found to be associated with medication cost-related nonadherence [52].
Limitations
Our review has some inherent limitations. Although we identified 38 relevant reviews, this does not equate to 38 independent reviews because there was considerable overlap between the studies that were included in the reviews. Although we are confident about the direction of the associations we examined, we had difficulties commenting on the precise magnitude of associations as these were often not clearly identified and reported in the reviews themselves, and could not be easily extracted and synthesized. Lastly, our review did not examine reviews that focused specifically on an alternative cost-sharing design called “value-based cost-sharing” or more generally “value-based insurance design.” The key feature of value-based insurance design is to link the amount of cost-sharing across services with the documented effectiveness and cost-effectiveness of a service, drug or device. A list of reviews that focused specifically on value-based designs is provided in the Additional file 1.
Implications for research
Our umbrella review highlights a paucity of research focused on children and youth. We identified no reviews that specifically focused on children and youth. The reviews we included generally sparingly discussed the potential impact of drug insurance and cost-sharing among youth. In our search, we identified a single review that focused specifically on children, which we excluded because it focused primarily on access and not on drug use. Unger and Ariely, identified two studies that compared insured and uninsured paediatric populations which showed increased access to healthcare services and medications for insured children [53]. The review noted that access to prescription drugs frequently differed by the type of health insurance provider and the type of cost-sharing arrangement and that more research was needed. The lack of discussion of potential sex/gender differences in the associations of prescription drug insurance and cost-sharing with drug use, health services use, and health is of concern. Only two reviews discussed this issue and reported on just two primary studies. It is unclear if the lack of discussion of potential sex/gender differences is due to reviews or primary studies not investigating it.
Future reviews need to give more consideration to appropriately synthesizing and discussing magnitudes of effect for given associations as solely presenting the direction or significance of a relationship provides minimal information. A stronger emphasis also needs to be placed on improving the methodological rigour of reviews by employing systematic and transparent methods to develop and execute search strategies as well as conducting quality assessment that is applicable to the literature being reviewed and ensuring that it is adequately discussed. Lastly, our umbrella review highlights the importance of searching systematically both peer-reviewed and grey literature, and not to overly rely on a single repository of research evidence. For example, only 11 reviews are included in Health Systems Evidence, which is perhaps the most comprehensive repository of reviews relevant to health systems.
Conclusions
Implications for health equity
Socioeconomic, racial and ethnic inequities in health care and drug coverage are well documented in the US and Canada [1, 54, 55]. For example, in 2015–16 in Canada, relative to adults in the lowest income decile, those in the 10th decile had odds of reporting drug insurance coverage that were more than five times higher [54]. In the US, Black and Latinx/Hispanic adults have historically reported substantially higher uninsured rates than white adults. In 2019, while the uninsured rate among white adults was only 9%, the uninsured rates among Black and Latinx/Hispanic adults stood at 14 and 26%, respectively. Consequently, universal pharmacare would likely increase drug use among lower-income populations relative to higher-income populations, and potentially reduce health inequities.
Implications for policy
Although cost-sharing can be used as a mechanism to reduce pharmaceutical expenditures, the associated impacts on health service use may offset those benefits. These cross-price effects of extending drug coverage are, however, often ignored in costing simulation, [56, 57] and need to be taken into consideration by policymakers. Lastly, current Canadian universal pharmacare proposed designs most often include cost-sharing for all but the most vulnerable despite evidence that cost-sharing reduces drug use and treatment adherence, and likely results in increases in health services use [3, 58].
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitors
- AMSTAR:
-
Assessment of Multiple Systematic Reviews
- ARB:
-
Angiotensin-receptor blockers
- CI:
-
Confidence Intervals
- ED:
-
Emergency Department
- EPHPP:
-
Effective Public Health Practice Project
- EPOC:
-
Effective Practice and Organisation of Care
- GRADE:
-
Grading of Recommendations, Assessment, Development and Evaluations
- HR:
-
Hazard Ratio
- ITS:
-
Interrupted Time Series
- NIH:
-
National Institute of Health
- OR:
-
Odds Ratio
- RCT:
-
Randomized Controlled Trial
- RePEc:
-
Research Papers in Economics
- RM:
-
Repeated Measures
- RR:
-
Relative Risk
- SES:
-
Socioeconomic Status
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- US:
-
United States
References
Sommers BD. Health insurance coverage: what comes after the ACA? Health Aff (Millwood). 2020;39(3):502–8.
Rosenthal MB. The growing problem of out-of-pocket costs and affordability in employer-sponsored insurance. JAMA. 2021;326(4):305–6.
Health Canada. A prescription for Canada: achieving pharmacare for all. Final report of the Advisory Council on the Implementation of National Pharmacare. Ottawa: Government of Canada; 2019.
Marchildon GP. Canada: health system review. Copenhagen: WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies; 2013.
OECD. Health at a glance 2019: OECD indicators. Paris: Organization for Economic Cooperation and Development; 2019.
Newhouse JP, The Insurance Experiment G. Free for all? Lessons from the RAND health insurance experiment: a RAND study. Cambridge and London: Harvard University Press; 1993.
Park YJ, Martin EG. Medicare part D’s effects on drug utilization and out-of-pocket costs: a systematic review. Health Serv Res. 2017;52(5):1685–728.
Glied SA, Collins SR, Lin S. Did the ACA lower Americans’ financial barriers to health care? Health Aff (Millwood). 2020;39(3):379–86.
Morgan S, Coombes M. Income-based drug coverage in British Columbia: towards an understanding of the policy. Healthc Policy. 2006;2(2):92–108.
Morgan SG, Gagnon M-A, Charbonneau M, Vadeboncoeur A. Evaluating the effects of Quebec’s private-public drug insurance system. CMAJ. 2017;189(40):E1259–E63.
Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Greenland S, O'Rourke K. On the bias produced by quality scores in meta-analysis, and a hierarchical view of proposed solutions. Biostatistics. 2001;2(4):463–71.
Lundh A, Gotzsche PC. Recommendations by Cochrane review groups for assessment of the risk of bias in studies. BMC Med Res Methodol. 2008;8:22.
Higgins J, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of Interventions version 6.0 (updated July 2019): Cochrane; 2019. Available from www.training.cochrane.org/handbook
Adams AS, Soumerai SB, Ross-Degnan D. The case for a medicare drug coverage benefit: a critical review of the empirical evidence. Annu Rev Public Health. 2001;22:49–61.
Harten C, Ballantyne P. The impact of cost-sharing within Canadian provincial drug benefit programs: a review. J Pharm Finance Econ Policy. 2004;13(1):35–53.
Lexchin J, Grootendorst P. Effects of prescription drug user fees on drug and health services use and on health status in vulnerable populations: a systematic review of the evidence. Int J Health Serv. 2004;34(1):101–22.
Rice T, Matsuoka KY. The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med Care Res Rev. 2004;61(4):415–52.
Gibson TB, Ozminkowski RJ, Goetzel RZ. The effects of prescription drug cost sharing: a review of the evidence. Am J Manag Care. 2005;11(11):730–40.
Maio V, Pizzi L, Roumm AR, et al. Pharmacy utilization and the Medicare modernization act. Milbank Q. 2005;83(1):101–30.
Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22(6):864–71.
Gemmill MC, Costa-Font J, McGuire A. In search of a corrected prescription drug elasticity estimate: a meta-regression approach. Health Econ. 2007;16(6):627–43.
Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61–9.
Gemmill MC, Thomson S, Mossialos E. What impact do prescription drug charges have on efficiency and equity? Evidence from high-income countries. Int J Equity Health. 2008;7:12.
Remler DK, Greene J. Cost-sharing: a blunt instrument. Annu Rev Public Health. 2009;30:293–311.
Green CJ, Maclure M, Fortin PM, Ramsay CR, Aaserud M, Bardal S. Pharmaceutical policies: effects of restrictions on reimbursement. Cochrane Database Syst Rev. 2010;(8):CD008654. https://doi.org/10.1002/14651858.CD008654.
Holst J. Patient cost sharing: reforms without evidence, Theoretical considerations and empirical findings from industrialized countries, WZB discussion paper, no. SP I 2010–303. Berlin: Wissenschaftszentrum Berlin für Sozialforschung (WZB); 2010.
Polinski JM, Kilabuk E, Schneeweiss S, Brennan T, Shrank WH. Changes in drug use and out-of-pocket costs associated with Medicare part D implementation: a systematic review. J Am Geriatr Soc. 2010;58(9):1764–79.
Swartz K. Cost-sharing: effects on spending and outcomes. The synthesis project. Research synthesis report no. 20. Princeton: Robert Wood Johnson Foundation; 2010.
Baicker K, Goldman D. Patient cost-sharing and healthcare spending growth. J Econ Perspect. 2011;25(2):47–68.
Polinski JM, Donohue JM, Kilabuk E, Shrank WH. Medicare part D’s effect on the under- and overuse of medications: a systematic review. J Am Geriatr Soc. 2011;59(10):1922–33.
Eaddy MT, Cook CL, O'Day K, Burch SP, Cantrell CR. How patient cost-sharing trends affect adherence and outcomes: a literature review. P T. 2012;37(1):45–55.
Lemstra M, Blackburn D, Crawley A, Fung R. Proportion and risk indicators of nonadherence to statin therapy: a meta-analysis. Can J Cardiol. 2012;28(5):574–80.
Maimaris W, Paty J, Perel P, et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med. 2013;10(7):e1001490.
Pimentel CB, Lapane KL, Briesacher BA. Medicare part D and long-term care: a systematic review of quantitative and qualitative evidence. Drugs Aging. 2013;30(9):701–20.
Sinnott S-J, Buckley C, O'Riordan D, Bradley C, Whelton H. The effect of copayments for prescriptions on adherence to prescription medicines in publicly insured populations; a systematic review and meta-analysis. PLoS One. 2013;8(5):e64914.
Kiil A, Houlberg K. How does copayment for health care services affect demand, health and redistribution? A systematic review of the empirical evidence from 1990 to 2011. Eur J Health Econ. 2014;15(8):813–28.
Mann BS, Barnieh L, Tang K, et al. Association between drug insurance cost sharing strategies and outcomes in patients with chronic diseases: a systematic review. PLoS One. 2014;9(3):e89168.
Kesselheim AS, Huybrechts KF, Choudhry NK, et al. Prescription drug insurance coverage and patient health outcomes: a systematic review. Am J Public Health. 2015;105(2):E17–30.
Luiza VL, Chaves LA, Silva RM, et al. Pharmaceutical policies: effects of cap and co-payment on rational use of medicines. Cochrane Database Syst Rev. 2015;5:CD007017.
Aziz H, Hatah E, Makmor Bakry M, Islahudin F. How payment scheme affects patients’ adherence to medications? A systematic review. Patient Prefer Adherence. 2016;10:837–50.
Banerjee A, Khandelwal S, Nambiar L, et al. Health system barriers and facilitators to medication adherence for the secondary prevention of cardiovascular disease: a systematic review. Open Heart. 2016;3(2):e000438.
Doshi JA, Li P, Ladage VP, Pettit AR, Taylor EA. Impact of cost sharing on specialty drug utilization and outcomes: a review of the evidence and future directions. Am J Manag Care. 2016;22(3):188–97.
Powell V, Saloner B, Sabik LM. Cost sharing in Medicaid: assumptions, evidence, and future directions. Med Care Res Rev. 2016;73(4):383–409.
Gourzoulidis G, Kourlaba G, Stafylas P, Giamouzis G, Parissis J, Maniadakis N. Association between copayment, medication adherence and outcomes in the management of patients with diabetes and heart failure. Health Policy. 2017;121(4):363–77.
Gupta S, McColl MA, Guilcher SJ, Smith K. Cost-related nonadherence to prescription medications in Canada: a scoping review. Patient Prefer Adherence. 2018;12:1699–715.
Ofori-Asenso R, Jakhu A, Curtis AJ, et al. A systematic review and meta-analysis of the factors associated with nonadherence and discontinuation of statins among people aged ≥65 years. J Gerontol A Biol Sci Med Sci. 2018;73(6):798–805.
Schneider APH, Gaedke MA, Garcez A, Barcellos NT, Paniz VMV. Effect of characteristics of pharmacotherapy on non-adherence in chronic cardiovascular disease: a systematic review and meta-analysis of observational studies. Int J Clin Pract. 2018;72(1). https://doi.org/10.1111/ijcp.13044.
Cheen MHH, Tan YZ, Oh LF, Wee HL, Thumboo J. Prevalence of and factors associated with primary medication non-adherence in chronic disease: a systematic review and meta-analysis. Int J Clin Pract. 2019;73(6):e13350.
Kolasa K, Kowalczyk M. The effects of payments for pharmaceuticals: a systematic literature review. Health Econ Policy Law. 2019;14(3):337–54.
Mishuk AU, Fasina I, Qian J. Impact of U.S. federal and state generic drug policies on drug use, spending, and patient outcomes - a systematic review. Res Soc Adm Pharm. 2020;16(6):736-45. https://doi.org/10.1016/j.sapharm.2019.08.031.
Holbrook AM, Wang M, Lee M, et al. Cost-related medication nonadherence in Canada: a systematic review of prevalence, predictors, and clinical impact. Syst Rev. 2021;10(1):11.
Ungar WJ, Ariely R. Health insurance, access to prescription medicines and health outcomes in children. Expert Rev Pharmacoecon Outcomes Res. 2005;5(2):215–25.
Guo EX, Sweetman A, Guindon GE. Socioeconomic differences in prescription drug supplemental coverage in Canada: a repeated cross-sectional study. Health Policy. 2020;124(3):252–60.
Baumgartner JC, Collins SR, Radley DC. Racial and ethnic inequities in health care coverage and access, 2013–2019. Data brief, June 2021. New York: Commonwealth Fund; 2021.
Morgan SG, Law M, Daw JR, Abraham L, Martin D. Estimated cost of universal public coverage of prescription drugs in Canada. CMAJ. 2015;187(7):491–7.
Office of the Parliamentary Budget Officer. Federal cost of a national pharmacare program. Ottawa: Parliamentary Budget Officer (PBO); 2017.
Yeung K, Morgan SG. Should national pharmacare apply a value-based insurance design? CMAJ. 2019;191(29):E811–E5.
Acknowledgements
We thank our collaborator Carley Hay from the Ontario Ministry of Health, Umaima Abbas, Bria Barton, Gioia Buckley, Selene Miller, Erica Stone and Riya Trivedi for their research assistance, and Arthur Sweetman and Jeremiah Hurley for their comments and discussion.
Funding
Canadian Institutes for Health Research (grant # 378730). GEG holds the Centre for Health Economics and Policy Analysis (CHEPA)/Ontario Ministry of Health and Long-Term Care (MOHLTC) Chair in Health Equity, an endowed Chair funded in part by the MOHLTC. The funders had no role in the study design, analysis, interpretation, writing of the report, or in the decision to submit this article for publication.
Author information
Authors and Affiliations
Contributions
GEG conceptualized the study. SG and GEG designed the search strategy. GEG, TF, SG, and KK assessed studies for inclusion, extracted detailed study characteristics, identified study limitations, and contributed to the interpretation of the findings. GEG and TF led the writing of the article. SG and KK revised the article critically for important intellectual content. GEG obtained funding. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board approval was not needed because we reviewed and synthesized existing research.
Consent for publication
We confirm that all contributors agreed to submit this paper for publication.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix A.
Search strategy. Appendix B. Quality Assessment / Risk of Bias tools. Appendix C. Characteristics of included studies. Appendix D. Excluded studies. Appendix E. List of Canadian studies included in reviews. Appendix F. List of reviews that focused specifically on value-based cost-sharing/insurance design.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guindon, G.E., Fatima, T., Garasia, S. et al. A systematic umbrella review of the association of prescription drug insurance and cost-sharing with drug use, health services use, and health. BMC Health Serv Res 22, 297 (2022). https://doi.org/10.1186/s12913-022-07554-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-07554-w