Abstract
Background
Mobile HIV testing approaches are a key to reaching the global targets of halting the HIV epidemic by 2030. Importantly, the number of clients reached through mobile HIV testing approaches, need to remain high to maintain the cost-effectiveness of these approaches. Advances in rapid in-vitro tests such as INSTI® HIV-1/HIV-2 (INSTI) which uses flow-through technologies, offer opportunities to reduce the HIV testing time to about one minute. Using data from a routine mobile HTS programme which piloted the use of the INSTI point-of-care (POC) test, we sought to estimate the effect of using a faster test on client testing volumes and the number of people identified to be living with HIV, in comparison with standard of care HIV rapid tests.
Methods
In November 2019, one out of four mobile HTS teams operating in Ekurhuleni District (South Africa) was randomly selected to pilot the field use of INSTI-POC test as an HIV screening test (i.e., the intervention team). We compared the median number of clients tested for HIV and the number of HIV-positive clients by the intervention team with another mobile HTS team (matched on performance and area of operation) which used the standard of care (SOC) HIV screening test (i.e., SOC team).
Results
From 19 November 2019 to 20 December 2019, the intervention team tested 7,403 clients, and the SOC team tested 2,426 clients. The intervention team tested a median of 442 (IQR: 288–522) clients/day; SOC team tested a median of 97 (IQR: 40–187) clients/day (p<0.0001). The intervention team tested about 180 more males/day compared to the SOC team, and the median number of adolescents and young adults tested/day by the intervention team were almost four times the number tested by the SOC team. The intervention team identified a higher number of HIV-positive clients compared to the SOC team (142 vs. 88), although the proportion of HIV-positive clients was lower in the intervention team due to the higher number of clients tested.
Conclusions
This pilot programme provides evidence of high performance and high reach, for men and young people through the use of faster HIV rapid tests, by trained lay counsellors in mobile HTS units.
Similar content being viewed by others
Background
Community-based HIV testing services are a key to reaching the global targets of halting the HIV epidemic by 2030 [1]. In particular, the delivery of HIV testing services (HTS) through mobile units has been shown to be cost-effective and successful in reaching people who are less likely to undergo testing in health care facilities [2,3,4]. Mobile units provide HTS through outreach teams and fully contained medical mobile units within community settings in order to access underserved or hard to reach populations, such as men, key populations, rural communities, or migrant populations [5]. This includes people who have a low perceived risk of being infected with HIV, are uncomfortable with or unable to frequent available health care facilities, or lack clinical reasons to seek services in health care facilities [6,7,8].
Although mobile HTS approaches have been shown to be cost-effective, they are not necessarily inexpensive [3]. Compared with facility-based or stand-alone HTS approaches, mobile HTS approaches incur higher costs for capital and recurring expenses as a proportion of totals costs [9]. However, costing studies of community-based HTS approaches in South Africa and similar settings, have shown that the mean cost per HTS client is reduced when client testing volumes are high [3, 9, 10]. As such, the number of clients reached through mobile HTS approaches, needs to remain sufficiently high to maintain the cost-effectiveness of these approaches. However, the turnaround time for obtaining results from current HIV rapid point-of-care tests, means that counsellors are often near capacity with the numbers of clients they can test a day. The standard HIV rapid tests take 10-20 min to produce a result, during which the counsellor and client are occupied, and the service is unavailable for the next client. In South Africa, a negative test is followed by brief post-test counselling, and a positive test is followed by a confirmatory test and post-test counselling [11]. The full process is time consuming with much of the time spent waiting for test results. This constrains the volume of HTS because a single counsellor is limited to testing 2-3 clients per hour and the lack of private spaces in a mobile setup limits the number of counsellors that can provide HTS at any given time [12].
In some mobile HTS settings, onsite HIV self-screening (HIVSS) has been implemented as an approach to increase the reach of HTS [13]. However, despite HIVSS shifting the locus of control to the client, the turnaround time of 15–20 min for test results remains a bottleneck for optimising daily HTS reach. Recent advances in rapid in-vitro tests such as INSTI® HIV-1/HIV-2 (INSTI) which uses faster flow-through technologies (compared with widely available lateral flow-based tests), offer opportunities to reduce the HIV testing time to about one minute of starting the test [14]. The reduced testing times of the INSTI point-of care (POC) test have also been shown to result in high levels of satisfaction by both clients and HTS providers [15, 16]. However, despite the prequalification of the INSTI-POC test by the World Health Organisation (WHO) in 2013, and its transformative potential to increase the volume of HTS in high burden settings; there are few published findings on the implementation outcomes from using INSTI in routine programmes or research settings [15, 17].
Using data from a routine mobile HTS programme which piloted the use of the INSTI-POC test to reduce HIV testing times, we sought to estimate the effect of INSTI-POC on client testing volumes and the number of people identified to be living with HIV, in comparison with standard of care rapid HIV testing approaches.
Methods
Programme setting
The mobile HTS programme operated in the Ekurhuleni District (Gauteng Province) of South Africa. Ekurhuleni District is a key district for South Africa’s National Strategic Plan to control the HIV epidemic [18]. In 2019, about 19 % of the estimated 3.7 million people who resided in the district, were living with HIV [19, 20]. The district is characterised by high levels of unemployment and poverty, coupled with increasing numbers of in-migrants who dwell in informal settlements mostly comprising of informal structures not approved for a permanent dwelling [21]. Four mobile HTS teams were deployed across the district in communities, workplaces, commercial shopping areas, and at special events as part of routine service delivery. All counsellors were trained and certified to provide HTS. HIV testing was provided in small private tents/gazebos and in private spaces within the repurposed fully contained medical mobile vans. Further, all HIV testing was offered as an opt-in service requiring informed consent, using finger-prick blood samples, and was accompanied by pre- and post-test counselling in a confidential private setting.
Piloting use of INSTI-POC as an HIV screening test
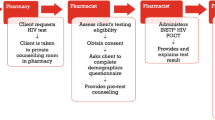
The South Africa HTS guidelines require counsellors to follow a serial testing algorithm, where a first rapid HIV test is performed as a screening test. If the screening test is non-reactive, the client is issued with a HIV-negative result. If the screening test is reactive, the HIV test is repeated with a different rapid HIV test to confirm the result of the screening test.
In November 2019, one out of four mobile HTS teams (hereafter referred to as the intervention team) operating in Ekurhuleni District was randomly selected to pilot the field use of INSTI-POC test as an HIV screening test. Prior to commencing the pilot programme, counsellors in the intervention team received additional three-day training on INTSI-POC tests which covered the principles of the test, conducting the test, interpretation of test results, storage of test kits, and quality control of the testing process. Of the remaining three mobile HTS teams, one team with similar number of counsellors and performance to the intervention team in terms of client testing volumes and the yield of HIV-positive diagnoses (i.e., in the 12-month period prior to study commencement), was selected to serve as the comparison for the intervention team (hereafter referred to as the standard of care (SOC) team). In contrast to the INSTI-POC team, the SOC team used the AbonTM HIV (Abon) rapid diagnostic test, which is the approved standard-of-care HIV screening test in public sector HIV testing programs in South Africa. Both INSTI-POC and Abon tests detect HIV Type 1 and/or Type 2 (HIV-1/HIV-2) and have similar sensitivity and specificity performance characteristics (i.e., >99 % sensitivity and specificity for both tests) [22, 23]. For both the intervention team and SOC team, all screening tests with reactive results were repeated using the First ResponseTM HIV (First Response) rapid diagnostic test to confirm the screening test result. Therefore, we hypothesise that the INSTI-POC and First Response testing algorithm compared to the Abon and First Response algorithm, had similar theoretical sensitivity and specificity. The Abon test required at least 10 min to read the result, compared with INSTI-POC test which required at least one minute to read the result. All HIV-positive clients were assigned to linkage officers who facilitated linkage to HIV medical care at referral clinics.
Quality control of test kits
Prior to commencement of the INSTI-POC pilot programme, a batch of INSTI-POC test kits were submitted for post-market surveillance testing at a national reference laboratory. The quality control (QC) process included tests for: (1) known negative and positive samples, (2) analytic sensitivity using a dilution series of reference material, and (3) intra-assay precision testing. Overall, the batch of INSTI-POC kits passed all QC tests. Similar additional QC processes were not conducted for Abon and First Response test kits since they are the approved SOC tests for use in the public sector HIV program with a routine QC process. As per routine standard operating procedures, each counsellor performed weekly internal QC tests on HIV test kits in use and additional QC tests on new shipments of HIV test kits. QC measures were used to assess the stability of the test devices and other reagents used for testing as well as adherence to test standard procedure and requirements. All QC results were recorded and reviewed by team leaders on a weekly basis.
Data collection
All screening and confirmatory (where applicable) test results were captured by counsellors using an electronic HIV testing register. The HIV testing register included information on the date of HIV test, a unique system-generated client identifier, client’s name, locator details, client’s age, client’s sex, final HIV test result, and a unique counsellor code used to identify the counsellor and the mobile HTS unit in which the client was tested.
Data analysis
Our analyses had two primary outcomes that served as proxies of HTS performance in the study period, (1) the number of clients tested for HIV and (2) the number of clients identified to be living with HIV (i.e., final HIV test results). To explore the effect of using INSTI-POC on these outcomes, we restricted comparisons to the SOC team on days when both the intervention team and SOC team delivered HTS. Further, we excluded days when one team worked beyond the average 8-hour workday, which occurred when mobile HTS teams were invited to, or hosted special events to provide HTS.
We used the median and interquartile range (IQR) to summarise the number of clients tested per day, and performed nonparametric tests for equality of the median number of clients tested between the two teams, using the Wilcoxon rank sum test [24]. We further compared the median number of clients tested per day among two priority groups for HTS in South Africa: men and adolescents and young adults (15–24 years) [25].
We summarised the final HIV test results (i.e., HIV-negative, or HIV-positive) using number (n) and proportion (%), and further stratified final HIV test results by client’s sex and age group. We explored differences in final HIV test results between the two teams using the Chi-Squared test at 5 % significance level. Data were analysed using STATA ® (Version 16, Stata Corporation, College Station, TX, USA). All data were de-identified for the purposes of this analysis.
Results
Comparison of HTS reach between the Intervention and SOC teams
From 19 November 2019 to 20 December 2019 (i.e., study period), both the intervention team and SOC team delivered mobile HTS services for 18 days. On these days, the intervention team tested 7,403 clients compared with 2,426 clients tested by the SOC team. The age and sex distribution of HTS clients was similar between the two teams (Table 1). Both teams mostly reached males, and clients aged 25–49-years. The intervention team tested a median of 442 (IQR: 288–522) clients/day compared with the SOC team which tested a median of 97 (IQR: 40–187) clients/day. Based on 9 counsellors per team, this translated to approximately each counsellor in the intervention team testing about 49 clients/day compared with a counsellor in the SOC team testing about 11 clients/day. The intervention team tested about 180 more males/day compared to the SOC team, and the median number of adolescents and young adults (15-24 years) tested/day by the intervention team (112, IQR: 72–141) were almost four times the number tested by the SOC team (29, IQR: 10–47) (Table 2).
Final HIV testing outcomes
Over the same number of days, the intervention team identified a total of 142 HIV-positive clients compared with the SOC team which identified 88 HIV-positive clients. Relative to the number of clients tested, the SOC team identified a higher proportion of HIV-positive clients (3.6 %) compared with the intervention team (1.9 %). Also, the HIV-positivity yield was higher among men tested by the SOC team compared with the intervention team (Table 3).
Discussion
Identifying ways to increase the reach of HTS is essential to reach the goals set globally for reducing the number of new infections and AIDS-related deaths. In this retrospective analysis of data from a routine mobile HTS programme, we identified the transformative potential of a faster HIV screening test to increase the reach of mobile HTS services. The large differences in the number of HTS clients reached between the intervention team and SOC team point to the potential benefit of faster HIV rapid testing technologies to increasing the productivity of healthcare workers providing HTS.
Achieving the balance in increasing the volume of HTS, while maintaining the quality of HIV test results is essential for increasing the number of people aware of their HIV status without causing unintended harm due to poor quality of HIV testing procedures. This is of particular concern in South Africa where about 10 million HIV tests are performed annually using rapid HIV diagnostic tests [19], and up to about 2.4 % and 8.9 % of the test results are false positive and false negative results, respectively [26, 27]. While the country has intensified efforts of training and quality assurance programmes to improve the quality control and adherence to testing algorithms [28], little has been documented about the malpractices by HTS providers in prematurely reading test results before the recommended minimum time [29]. It is plausible that poor fidelity to result waiting times is a result of HTS providers’ efforts to reduce patient waiting times or an attempt to meet daily performance targets. concordance test. Our findings of high HTS reach from the intervention team, suggest that with faster HIV screening tests, HTS providers may be able to increase the number of clients tested without the need to prematurely read the test results in an effort to save time.
Over the past decade, the reach of HTS to adolescents and young adults and men in South Africa has been suboptimal to meet the country’s goal of reducing the proportion of people with undiagnosed HIV infection to at least 5% [25, 30]. While community-based HTS has been shown to reach these hard-to-reach population groups [8], the number needed to test to identify people living with HIV is set to increase as the proportion of people aware of their HIV status increases. Our findings show that the intervention team reached more than triple the number of clients compared with the SOC team. We hypothesise that shorter queues and faster service times at the intervention team’s mobile HTS sites may have increased demand of services by reducing the perceived opportunity costs of undergoing HTS or reduced the potential of loss in privacy by being seen in HIV testing queues [31, 32]. These are particularly important factors for mobile HTS units that offer services to people in public places, and to people who may have competing priorities at the time they are invited for HTS (e.g., shopping or attending an event). With the advent and high uptake of HIV self-screening strategies in South Africa, faster HIV self-screening test may also increase the throughput of community-based HTS [13, 33, 34].
Our findings of high reach and low HIV-positivity yield from the intervention team, compared with low reach and marginally higher HIV-positivity yield from the SOC team, contribute to ongoing discussions on how to best measure the cost efficiency of HTS programmes (i.e., absolute numbers vs. yield) [35]. Achieving universal health coverage for people living with HIV, requires identifying more people unaware of their HIV diagnosis, and our findings show that this can be achieved through faster rapid HIV diagnostic tests. Further, achieving HIV epidemic control also requires identifying HIV-negative persons and linking them to HIV prevention programmes to reduce the number of new HIV infections, which is a frequently overlooked aspect in evaluating the cost-effectiveness of mobile HTS approaches.
Our study highlights the field performance of counsellors using a fast HIV screening test and the potential benefit in increasing HTS reach, but it is not without limitations. Our comparison of HTS reach between the Intervention and SOC teams, was conducted within a pragmatic setting where teams identified target areas for HTS, as per routine practice. While it is plausible that the teams served areas with different HTS demand, it is noteworthy that these teams were selected because of similar performance over a period of 12 months, and the team composition did not change during the study period. Therefore, to a large extent, the observed differences in HTS reach between the two teams may be attributed to the potential influence of using a faster HIV screening test. One of the goals of HTS is to ensure that people with an HIV-positive diagnosis are linked to HIV care services. Data on linkage-to-care outcomes from clinic records could not be readily linked to unique identifiers in the de-identified data set and was excluded from this analysis. Further, we were unable to quantify the number of clients who were previously unaware of their HIV-positive. However, emerging evidence suggests that clients who have never entered care or those who have disengaged from care, use HTS as a gateway for first entry or re-entry into HIV care and treatment services [36, 37]. Lastly, we report findings from a routine mobile HTS programme in an urban high HIV-burden district, using data collected over an 18-day period. In this regard, our findings need to be interpreted cautiously beyond the program’s implementation context.
Conclusions
This pilot programme provides preliminary evidence of high HTS reach through the use of a faster HIV screening test by trained lay counsellors in mobile HTS units. As South Africa continues its investments in HIV prevention and treatment programmes, innovations such as INSTI-POC that reduce the time spent utilising HIV services will be key to success. We hypothesize that the gains in productivity outweigh the increase in test kit costs, but this needs further study. Our work sets a platform for further research exploring implementation and health economics outcomes to assess the benefits of faster HIV screening in community-based HTS models.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available as they pertain to routine programme data but are available from the corresponding author on reasonable request and upon receipt of relevant approvals by local authorities in South Africa.
Change history
22 November 2021
A Correction to this paper has been published: https://doi.org/10.1186/s12913-021-07271-w
Abbreviations
- CI:
-
Confidence Interval
- HTS:
-
HIV testing services
- IQR:
-
Interquartile range
- POC:
-
Point-of-care
- QC:
-
Quality Control
- SOC:
-
Standard of care
- WHO:
-
World Health Organisation
References
World Health Organization. Consolidated guidelines on HIV testing services for a changing epidemic: policy brief 2019. 2019. Available from: https://www.who.int/publications-detail/consolidated-guidelines-on-hiv-testing-services-for-a-changing-epidemic.
Mabuto T, Latka MH, Kuwane B, Churchyard GJ, Charalambous S, Hoffmann CJ. Four models of HIV counseling and testing: utilization and test results in South Africa. PLoS One. 2014;9(7):e102267.
Bassett IV, Govindasamy D, Erlwanger AS, Hyle EP, Kranzer K, van Schaik N, et al. Mobile HIV screening in Cape Town, South Africa: clinical impact, cost and cost-effectiveness. PloS One. 2014;9(1):e85197. PubMed PMID: 24465503. Pubmed Central PMCID: 3898963.
Smith JA, Sharma M, Levin C, Baeten JM, van Rooyen H, Celum C, et al. Cost-effectiveness of community-based strategies to strengthen the continuum of HIV care in rural South Africa: a health economic modelling analysis. Lancet HIV 2015;2(4):e159-68. PubMed PMID: 25844394. Pubmed Central PMCID: 4384819.
World Health Organization. Increasing access to HIV testing and counselling 2014. 2019. Available from: https://apps.who.int/iris/bitstream/handle/10665/42757/9241590904.pdf?sequence=1.
Bassett IV, Regan S, Mbonambi H, Blossom J, Bogan S, Bearnot B, et al. Finding HIV in hard to reach populations: mobile HIV testing and geospatial mapping in Umlazi township, Durban, South Africa. AIDS Behav. 2015;19(10):1888–95. PubMed PMID: 25874754. Pubmed Central PMCID: 4531102.
Grabbe KL, Menzies N, Taegtmeyer M, Emukule G, Angala P, Mwega I, et al. Increasing access to HIV counseling and testing through mobile services in Kenya: strategies, utilization, and cost-effectiveness. J Acquir Immune Defic Syndr. 2010;54(3):317–23. PubMed PMID: 20453819. Pubmed Central PMCID: 3225204.
Meehan SA, Naidoo P, Claassens MM, Lombard C, Beyers N. Characteristics of clients who access mobile compared to clinic HIV counselling and testing services: a matched study from Cape Town, South Africa. BMC Health Serv Res. 2014;14:658. PubMed PMID: 25526815. Pubmed Central PMCID: 4280046.
Meehan S-A, Beyers N, Burger R. Cost analysis of two community-based HIV testing service modalities led by a Non-Governmental Organization in Cape Town, South Africa. BMC Health Serv Res. 2017;17(1):1–9.
Parker LA, Jobanputra K, Rusike L, Mazibuko S, Okello V, Kerschberger B, et al. Feasibility and effectiveness of two community-based HIV testing models in rural Swaziland. Trop Med Int Health. 2015;20(7):893–902. PubMed PMID: 25753897. Pubmed Central PMCID: 4672714.
South Africa National Department of Health. NATIONAL HIV TESTING SERVICES: POLICY. Preoria; 2016
Mabuto T, Hansoti B, Kerrigan D, Mshweshwe-Pakela N, Kubeka G, Charalambous S, et al. HIV testing services in healthcare facilities in South Africa: a missed opportunity. J Int AIDS Soc. 2019;19(1):898. PubMed PMID: 31599495. Pubmed Central PMCID: 6785782.
Lebina L, Seatlholo N, Taruberekera N, Radebe M, Kinghorn A, Meyer T, et al. Feasibility of community-based HIV self-screening in South Africa: a demonstration project. BMC Public Health. 2019 2019/07/08;19(1):898.
Adams S, Luo W, Wesolowski L, Cohen SE, Peters PJ, Owen SM, et al. Performance evaluation of the point-of-care INSTI HIV-1/2 antibody test in early and established HIV infections. J Clin Virol. 2017;91:90–4. PubMed PMID: 28372890.
Bwana P, Ochieng’ L, Mwau M. Performance and usability evaluation of the INSTI HIV self-test in Kenya for qualitative detection of antibodies to HIV. PLoS One. 2018;13(9):e0202491.
Galli RA, Green KF, La Marca A, Waldman LF, Powers RE, Daly AC, et al. Evaluation of the accuracy and ease of use of a rapid HIV-1 Antibody Test performed by untrained operators at the point of care. J Clin Virol. 2013;58:e65-e9.
Lau L, Wudel B, Lee E, Darraj M, Richert Q, Trajtman A, et al. Evaluation of the utility of point-of-care HIV testing on a Canadian internal medicine inpatient unit. Can J Infect Dis Med Microbiol. 2017;2017:8495307.
Relief UPsEPfA. South Africa Country Operational Plan (COP/ROP) 2020 Strategic Direction Summary 2020. 2021. Available from: https://www.state.gov/wp-content/uploads/2020/07/COP-2020-South-Africa-SDS-FINAL.pdf.
Massyn N, Barron P, Day C, Ndlovu N, Padarath A District Health Barometer 2018/19. Durban: Health Systems Trust; 2020.
Statistics South Africa. District Popultion Estimates 2017-2021.
City of Ekurhuleni. City of Ekurhuleni Annual Report 2017/18 2016. 2020. Available from: https://www.ekurhuleni.gov.za/annual-report/2017-18-annual-report/3924-annual-report-2017-18-1/file.html.
World Health Organisation. WHO Prequalification of Diagnostics Programme: ABON HIV 1/2/O Tri-Line Human. Geneva; 2019.
World Health Organisation. WHO Prequalification of Diagnostics Programme: INSTI HIV-1/HIV-2 Antibody Test. 2013.
Wilcoxon F. Individual comparisons by ranking methods. Biom Bull. 1945;1:80–3.
Simbayi L, Zuma K, Moyo S, Marinda E, Mabaso M, Ramlagan S, et al. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017. 2019.
Johnson CC, Fonner V, Sands A, Ford N, Obermeyer CM, Tsui S, et al. To err is human, to correct is public health: a systematic review examining poor quality testing and misdiagnosis of HIV status. J Int AIDS Soc. 2017;20:21755.
Moodley D, Moodley P, Ndabandaba T, Esterhuizen T. Reliability of HIV rapid tests is user dependent. S Afr Med J. 2008;98(9):707–9.
Woldesenbet SA, Kalou M, Mhlongo D, Kufa T, Makhanya M, Adelekan A, et al. An overview of the quality assurance programme for HIV rapid testing in South Africa: Outcome of a 2-year phased implementation of quality assurance program. PLoS One. 2019;14(9):e0221906.
Mwisongo A, Peltzer K, Mohlabane N, Tutshana B. The quality of rapid HIV testing in South Africa: an assessment of testers’ compliance. Afr Health Sci. 2016;16(3):646–54.
Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Capetown: HSRC Press; 2014.
Mohlabane N, Tutshana B, Peltzer K, Mwisongo A. Barriers and facilitators associated with HIV testing uptake in South African health facilities offering HIV Counselling and Testing. Health SA Gesondheid. 2016;21:86–95.
Mambanga P, Sirwali RN, Tshitangano T. Factors contributing to men’s reluctance to seek HIV counselling and testing at Primary Health Care facilities in Vhembe District of South Africa. Afr J Prim Health Care Fam Med. 2016;8(2)e1-7.
Krause J, Subklew-Sehume F, Kenyon C, Colebunders R. Acceptability of HIV self-testing: a systematic literature review. BMC Public Health. 2013;13(1):735.
Njau B, Covin C, Lisasi E, Damian D, Mushi D, Boulle A, et al. A systematic review of qualitative evidence on factors enabling and deterring uptake of HIV self-testing in Africa. BMC Public Health. 2019;19(1):1289.
De Cock KM, Barker JL, Baggaley R, El Sadr WM. Where are the positives? HIV testing in sub-Saharan Africa in the era of test and treat. Aids. 2019;33(2):349–52.
Grimsrud A, Wilkinson L, Eshun-Wilson I, Holmes C, Sikazwe I, Katz IT. Understanding Engagement in HIV Programmes: How Health Services Can Adapt to Ensure No One Is Left Behind. Curr HIV/AIDS Rep. 2020;17(5):458–66.
Wringe A, Moshabela M, Nyamukapa C, Bukenya D, Ondenge K, Ddaaki W, et al. HIV testing experiences and their implications for patient engagement with HIV care and treatment on the eve of ‘test and treat’: findings from a multicountry qualitative study. Sex Transm Infect. 2017;93(Suppl 3):e052969.
Acknowledgements
We would like to acknowledge the mobile HIV testing teams who were involved in collecting high quality routine programme data that was used to conduct this study.
Funding
The study was funded by the Foundation of Professional Development, South Africa. The funder had no role in the design of the study and collection, analysis, interpretation of data, nor in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
JP, SD, LM, and DC designed the pilot programme, developed the data collection, and contributed to manuscript writing. TM, GS, and NM performed data analysis, interpreted analysis findings, and contributed to manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval to conduct the study was provided by the University of Witwatersrand Human Research Ethics Committee (Reference number: 190702). The study was also approved by the Ekurhuleni Health District Department of Health and City of Ekurhuleni Health and Social Development. Informed consent to participate was obtained from all participants aged 18 years and above, and from legal guardian(s) for participants below 18 years of age. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: some content is corrected in the Results section of the Abstract.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mabuto, T., Setswe, G., Mshweshwe-Pakela, N. et al. Findings from a novel and scalable community-based HIV testing approach to reduce the time required to complete point-of-care HIV testing in South Africa. BMC Health Serv Res 21, 1176 (2021). https://doi.org/10.1186/s12913-021-07173-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-07173-x