Abstract
Background
Preconception care (PCC) is recommended for optimizing a woman’s health prior to pregnancy to minimize the risk of adverse pregnancy and birth outcomes. We aimed to evaluate the impact of strategy and a novel risk classification model of China´s “National Preconception Health Care Project” (NPHCP) in identifying risk factors and stratifying couples’ preconception health status.
Methods
We performed a secondary analysis of data collected by NPHCP during April 2010 to December 2012 in 220 selected counties in China. All couples enrolled in the project accepted free preconception health examination, risk evaluation, health education and medical advice. Risk factors were categorized into five preconception risk classes based on their amenability to prevention and treatment: A-avoidable risk factors, B- benefiting from targeted medical intervention, C-controllable but requiring close monitoring and treatment during pregnancy, D-diagnosable prenatally but not modifiable preconceptionally, X-pregnancy not advisable. Information on each couple´s socio-demographic and health status was recorded and further analyzed.
Results
Among the 2,142,849 couples who were enrolled to this study, the majority (92.36%) were from rural areas with low education levels (89.2% women and 88.3% men had education below university level). A total of 1463266 (68.29%) couples had one or more preconception risk factors mainly of category A, B and C, among which 46.25% were women and 51.92% were men. Category A risk factors were more common among men compared with women (38.13% versus 11.24%; P = 0.000).
Conclusions
This project provided new insights into preconception health of Chinese couples of reproductive age. More than half of the male partners planning to father a child, were exposed to risk factors during the preconception period, suggesting that an integrated approach to PCC including both women and men is justified. Stratification based on the new risk classification model demonstrated that a majority of the risk factors are avoidable, or preventable by medical intervention. Therefore, universal free PCC can be expected to improve pregnancy outcomes in rural China.
Similar content being viewed by others
Background
Preconception care (PCC) is defined as interventions that aim to identify and, when possible, modify the biomedical, behavioral, and social risks to optimize woman’s health before pregnancy with the aim of improving pregnancy outcomes [1]; In 2014, Centers for Disease Control and Prevention (CDC) and the Office of Population Affairs published clinical recommendations, “Providing Quality Family Planning Services” (QFP), and recognized PCC as a critical component of health care for women of reproductive age [2].
The purpose of PCC is to optimize a woman’s health prior to pregnancy and promote healthy behavior during pregnancy to reduce the incidence of adverse birth outcomes [3]. It is reported that an estimated 300,000 women die globally as a result of pregnancy-related conditions [4]. The prevalence of birth defects in China is around 5.6%, and there are nearly 900 000 new cases annually according to the official Report on Prevention of Birth Defects in China published in 2012 [5]. Health services provided to the couples of reproductive age, such as family planning, folic acid supplementation [6], genetic counseling, chronic disease management, immunizations, treatment of sexually transmitted infections, and interventions promoting healthier lifestyle, including those directed against alcohol, tobacco, and substance abuse [7] seem to have a positive effect. There is growing evidence that effective treatment of maternal diabetes and hypertension during the preconception period reduces adverse maternal and neonatal outcomes [8–10]. Avoiding unintended pregnancy through PCC could avert 44% maternal mortality [11]. Moreover, the effect of PCC on women with a history of previous adverse infant outcome, such as preterm birth, low birth weight, stillbirth or major birth defect, appears to be meaningful [12].
Even though the benefits of PCC have been well established [13, 14], integrating PCC into regular family planning services still remains a challenge for some providers [15]. Poor organization of health services’ delivery systems, lack of comprehensive PCC programs, limited awareness among future parents about the availability and benefits of PCC and that of physicians about the necessity and effectiveness of PCC are apparent barriers affecting delivery and uptake of PCC [16, 17].
PCC in China has been insufficient and inadequate, especially in rural areas, despite the fact that facility-based strategy on reducing neonatal mortality had a significant impact on the Millennium Development Goal 4, and with a rapid economic development there have been improvements in population health in recent decades [18]. Therefore, the National Health and Family Planning Commission of the People’s Republic of China(NHFPC)launched the “National Preconception Health Care Project” (NPHCP) in 2010, focusing on rural areas and providing free PCC for the couples of reproductive age [19]. In this project, relevant preconception risk factors were classified according to their amenability to prevention and treatment. The objective of our study was to evaluate the impact of strategy and risk classification model of China’s NPHCP in identifying risk factors and stratifying the preconception health status of men and women of reproductive age.
Methods
Data source and study design
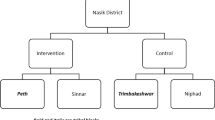
We conducted a secondary analysis of data collected within the framework of NPHCP during April 2010 to December 2012 to investigate the characteristics of preconception risk factors among married Chinese women and men of reproductive age. Methodological details of the project have been described previously [20–22]. Briefly, the study covered 220 counties in China. Selected rural counties in all provinces and the urban counties that wanted to participate in this project were included in this population-based prospective cohort study.
NHFPC established the implementation and quality control standards for this program [20, 21]. Local community staff investigated the conception plans of the couples, and those planning to conceive within the next six months were enrolled and invited to attend a free health examination. Professional doctors specially trained in obstetrics, genetic and other related specialties provided necessary medical advice to the couples. NHFPC has drafted and published the consultation guide for common preconception health problems. All couples enrolled accepted a free preconception health examination, risk evaluation, health education and medical advice based on the risk factors. A written informed consent was obtained from each participant, and this study was approved by the Institutional Review Board of the Chinese Association of Maternal and Child Health Studies [20, 21].
Preconception examination included (1) a medical history: current medical illness and use of any medication, family history of hypertension, diabetes, congenital or genetic diseases in the first-degree relatives, life style, dietary habits and exposure to environmental and occupational hazards; (2) physical examination: height, weight, blood pressure, heart rate, palpation of thyroid gland, auscultation of the heart and lungs, abdominal palpation, examination of the limbs and the spine; (3) clinical laboratory tests: genital swabs for microbiological culture and sensitivity, gonococcus and chlamydia test, hemoglobin and full blood count, urine for bacteriology and culture, blood type, serum glucose, liver, renal function and thyroid function tests, hepatitis B serology, syphilis test, TORCH (toxopasma, rubella virus, cytomegalovirus, and herpes simplex virus) screen, and gynecological ultrasound; (4) past medical history: hypertension, diabetes, cardiac diseases, immune system diseases, renal diseases and other chronic diseases; (5) past obstetric history including history of induced abortion, spontaneous abortion, live birth, stillbirth, neonatal death, fetal abnormality, preterm birth and multiple pregnancy. Trained staff regularly recorded and entered the information into the NHFPC database.
Preconception risk evaluation and classification model
The aim of the preconception health examination was to identify all the risk factors as far as possible, and treat accordingly. Therefore, instead of assessing the degree of exposure, we developed a preconception risk classification system based on their amenability to prevention and treatment according to Preconception Health Examination and Risk Evaluation Guides (Science and Technology Division of NHFPC) (Table 1). Risk factors were categorized into five preconception risk classes: A-avoidable risk factors, B-benefiting from targeted medical intervention before conception, C-controllable but requiring close monitoring and treatment during pregnancy, D-diagnosable prenatally but the risk factor not modifiable preconceptionally, X-pregnancy not advisable. The couples with category X risk factor were advised to use appropriate contraception and were considered in further analysis. Participants with missing or incomplete records were excluded from analysis.
Statistical analysis
Statistical analysis was performed using SPSS statistical software version 15.0 (SPSS, System for Windows, Chicago, USA). Data are presented as number (%) and mean ± standard deviation (SD). For comparing groups, we used independent samples t-test for continuous variable and χ2 test for categorical variables. All P-values were two-tailed, and a P < 0.05 was considered to be statistically significant.
Results
General characteristics of the study population
During April 2010 to December 2012, a total of 22.42 million married Chinese couples planning to conceive within the six months were recruited to the study from 220 different counties. After excluding those with incomplete medical records and lost to follow-up, data from 2,142,849 couples were available for analysis. NPHCP targeted couples of reproductive age mainly from rural areas, and covered most areas, regions, and ethnicities from all provinces of mainland China. 92.36% couples were from rural areas and 89.2% women and 88.3% men had education below university level. Other socio-demographic details of the participants are presented in Tables 2 and 3.
Preconception risk factor classification
As demonstrated in Tables 2 and 3, category D risk was more common among couples in the age group 30–35 years and >35 years (P < 0.05). There were no significant differences between rural areas and cities in both couples in terms of risk factor categories. Proportionally, more women of non-Han ethnicity were classified in category D and X compared to those with no risk factors, while there was no difference in that ratio among men. Women with category A, and men with category B and D risk factors had higher education levels (P < 0.05).
Distribution preconception risk factors
Distribution of the participants in different preconception risk categories is presented in Table 4. Among 2,142,849 couples, 46.25% women had preconception risks, mainly of category A, B and C. 9.80% women had category A risks including alcohol consumption (3.4%), inadequate protein intake (1.36%) and exposure to noise (1.18%). 14.83% women were had category B risks, such as anemia (8.40%), gingival hemorrhage (3.57%) and vaginitis (2.29%). Moreover, 23.5% of women had category C risks, such as thyroid dysfunction (6.34%), HBV infection (4.76%), history of gynecological diseases (3.41%) and/or category D risks, such as history of spontaneous abortion (2.66%) and adverse pregnancy history (1.12%). On the other hand, 51.92% of couples had paternal risks, and 38.13% of them had category A risk factors including alcohol (29.61%) and smoking (29.07%) (Table 4).
Discussion
This nation-wide free preconception care project targeting rural areas in China used an integrated model of PCC including both women and men. A novel classification system was used to classify risk factors based on their amenability to prevention and treatment, which stratified couples in five different risk categories. More than 68% of couples with conception plans within the next six months had one or more risk factors, and nearly 40% of these risk factors could be potentially modified by intervention before or during pregnancy. Approximately 23% of risk factors among women were in category A and B, whereas among men the figure was 45%. Avoidable risk factors were more common among men compared with women suggesting that men may have riskier behavior than women, with almost 30% of men reporting consumption of alcohol and smoking.
Our study revealed that preconception risk evaluation in couples with plans to conceive within six months could be meaningful as nearly two-thirds of the recruited couples had preconception risk factors, and 23% maternal risk factors were in category A and B, and thereby potentially avoidable or modifiable preconceptionally by health education, medical intervention and life style changes. More importantly, a similar situation was observed regarding paternal risk factors. Almost 45% of the male partners consumed alcohol or smoked, which may lead to passive smoking by women, a fact often ignored in preconception care. Some European countries have preconception care recommendations for women with chronic diseases, such as diabetes and epilepsy, but guidelines are heterogeneous and recommendations for healthy women and men are fragmented and inconsistent [22]. Our results further enforce the need for an integrated approach to PCC that includes both women and men.
A more innovative and integrated approach to PCC for both women and men is needed for achieving optimal reproductive health status before pregnancy and better pregnancy outcomes [23, 24]. Preconception health promotion may be useful in eliminating some of the Category A and B risk factors before pregnancy. However, some risk factors, such as smoking, alcohol and substance abuse, would require longer term strategies to achieve sustained amelioration. A more comprehensive health promotion strategy during pregnancy would be required for managing other risk categories to achieve better pregnancy outcomes.
The preconception risk classification system used in this big population-based study was practical for stratifying preconception health status of the couples, and helpful in organizing targeted educational and health care interventions, and identifying need for referral. The risk classification was based on existing risk factors during the preconception period and categorized by whether it could be prenatally avoided or modified during the preconception period or prenatally. As preconception risks may vary from prenatal risks, Considering different methods and timing of intervention is important. Nearly half of the risk factors identified were avoidable or preventable by medical intervention during the preconception period in this study, allowing for a window of opportunity for personalized lifestyle modification and health care to achieve better pregnancy outcome. Despite the evidence supporting the value and importance of PCC [25], it is reported that there is lack of sufficient research attention to clinical PCC service delivery, and a more detailed consideration of the practicalities of implementing PCC within contemporary women’s health care is required [26]. This integrated universal free PCC service provided in rural China could be a promising model if its positive impact on pregnancy outcomes could be demonstrated in future.
Our study does have some limitations. Follow-up of risk modifications was not included in this study, so the impact of preconception risk classification on the health status of the couple could not be assessed. Prevalence of adverse pregnancy history and chronic disease history in couples planning pregnancy might have been underestimated as this was based on self-reporting and recall bias cannot be excluded.
Conclusions
This project provided new insights into preconception health of Chinese couples of reproductive age. More than half of the male partners planning to father a child were exposed to risk factors during the preconception period, suggesting that an integrated approach to PCC including both women and men is justified. Stratification based on the new risk classification model demonstrated that a majority of the risk factors are avoidable or preventable by medical intervention. Therefore, universal free PCC can be expected to improve pregnancy outcomes in rural China.
Abbreviations
- LBW:
-
Low birth weight
- NHFPC:
-
The National Health and Family Planning Commission of the People’s Republic of China
- NPHCP:
-
National Preconception Health Care Project
- PCC:
-
Preconception care
References
Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, et al. Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55(6):1–23.
Robbins CL, Loretta G, Zapata LB, Carter MW, Christina L, Nancy M-S, et al. Preconception Care in Publicly Funded U.S. Clinics That Provide Family Planning Services. Am J Prev Med. 2016;51(3):336–43.
Inskip HM, Crozier SR, Godfrey KM, Borland SE, Cooper C, Robinson SM, et al. Women's compliance with nutrition and lifestyle recommendations before pregnancy: general population cohort study. BMJ. 2009;338:b481.
Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387:462–74.
Ministry of Health of People’s Republic of China. The report on the prevention of birth defects in China. 2012. Available online at: www.gov.cn/gzdt/2012-09/12/content_2223371.htm. Accessed 17 Jan 2016.
De-Regil LM, Fernández-Gaxiola AC, Dowswell T, Peña-Rosas JP. Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Database Syst Rev. 2010;6(10):CD007950.
Crawford C. AAFP urges family physicians to integrate preconception care into patient visits. Ann Fam Med. 2016;14:180–1.
Seely EW, Ecker J. Clinical practice. Chronic hypertension in pregnancy. N Engl J Med. 2011;365(5):439–46.
Bentley-Lewis R. Gestational diabetes mellitus: an opportunity of a lifetime. Lancet. 2009;373(9677):1738–40.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51.
Saifuddin A, Qingfeng L, Li L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet. 2012;380:111–25.
Wahabi HA, Alzeidan RA, Bawazeer GA, Alansari LA, Esmaeil SA. Preconception care for diabetic women for improving maternal and fetal outcomes: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2010;10:63.
Beckmann MM, Widmer T, Bolton E. Does preconception care work? Aust N Z J Obstet Gynaecol. 2014;54(6):510–4.
Luton D, Forestier A, Courau S, Ceccaldi PF. Preconception care in France. Int J Gynaecol Obstet. 2014;125(2):144–5.
M'hamdi HI, Voorst SF, Pinxten W, Hilhorst MT, Steegars EA. Barriers in the uptake and delivery of preconception care exploring the views of care providers. Matern Child Health J. 2016. Epub ahead of print.
M’hamdi HI, van Voorst SF, Wim P, Hilhorst MT, Eric AP. Steegers. Barriers in the uptake and delivery of preconception care: exploring the views of care providers. Matern Child Health J. 2016. Epub ahead of print.
Poels M, Koster MP, Boeije HR, Franx A, van Stel HF. Why do women not use preconception care? A systematic review on barriers and Facilitators. Obstet Gynecol Surv. 2016;71(10):603–12.
Feng XL, Guo GF, Hipgrave D, Zhu J, Zhang L, Song L, et al. China’s facility-based birth strategy and neonatal mortality: a population-based epidemiological study. Lancet. 2011;378:1493–500.
Zhou Q, Acharya G, Zhang S, Wang Q, Shen H, Li X. New perspective on universal preconception care in China. Acta Obstet Gynecol Scand. 2016;95(4):377–81.
Zhang SK, Wang QM, Shen HP. Design, implementation and objective of free “National Preconception Health Care Project in China. Natl Med J China. 2015;95(3):162–5.
Wang QM, Zhang M, Zhang SK, Hu M, Liu N, Kang XX, et al. Establishment of quality control system of free “National Preconception Health Care Project in China. Natl Med J China. 2015;95(3):166–8.
Jill Shawe ID, Maria E, Hanne Kristine H, Margareta L, Pierpaolo M, et al. Preconception care policy, guidelines, recommendations and services across six European countries: Belgium (Flanders), Denmark, Italy, the Netherlands, Sweden and the United Kingdom. Eur J Contracept Reprod Health Care. 2015;20:77–87.
Michelle SF, Karla D, Brian J. The future of preconception care in the United States: multigenerational impact on reproductive outcomes. Ups J Med Sci. 2016;19:1–5.
Anna B, Gunilla L. Preconception health and care (PHC)—a strategy for improved maternal and child health. Ups J Med Sci. 2016;20:1–6.
Braspenningx S, Haagdorens M, Blaumeiser B, Jacquemyn Y, Mortier G. Preconceptional care: a systematic review of the current situation and recommendations for the future. Facts Views Vis Obgyn. 2013;5(1):13–25.
Steel A, Luckec J, Reida R, Adams J. A systematic review of women’s and health professional’s attitudes and experience of preconception care service delivery. Fam Pract. 2016; Epub ahead of print.
Acknowledgments
The views expressed in the report are those of the authors and do not necessarily reflect the official policy or position of the Department of Maternal and Child Health of National Health and Family Planning Commission (NHFPC) in China. We thank health workers in 220 counties of 31 provinces for their strong collaboration and contributions made in the NFPHEP.
Funding
This study was funded by the Chinese Association of Maternal and Child Health Studies (AMCHS-2014-4).
Availability of data and materials
Dataset analyzed in this study was based on the national database and public access to the database is closed. Zhang Shikun gave the administrative permission to access the database on behalf of National Health and Family Planning Commission of the People’s Republic of China (NHFPC).
Authors’ contributions
ZQ and LX carried out the statistical analysis and drafted the manuscript. GA interpreted data and drafted the manuscript. ZS, WQ, SH and LX participated in the design of the study and coordination. TW and CJ performed the statistical analysis. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Chinese Association of Maternal and Child Health Studies. A written informed consent was obtained from each participant, as consent to participate.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhou, Q., Zhang, S., Wang, Q. et al. China’s community-based strategy of universal preconception care in rural areas at a population level using a novel risk classification system for stratifying couples´ preconception health status. BMC Health Serv Res 16, 689 (2016). https://doi.org/10.1186/s12913-016-1930-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-016-1930-4