Abstract
Background
Uganda’s under-five mortality is high, currently estimated at 66/1000 live births. Poor referral of sick children that seek care from the private sector is one of the contributory factors. The proposed intervention aims to improve referral and uptake of referral advice for children that seek care from private facilities (registered drug shops/private clinics).
Methods/Design
A cluster randomized design will be applied to test the intervention in Mukono District, central Uganda. A sample of study clusters will implement the intervention. The intervention will consist of three components: i) raising awareness in the community: village health teams will discuss the importance of referral and encourage households to save money, ii) training and supervision of providers in the private sector to diagnose, treat and refer sick children, iii) regular meetings between the public and private providers (convened by the district health team) to discuss the referral system. Twenty clusters will be included in the study, randomized in the ratio of 1:1. A minimum of 319 sick children per cluster and the total number of sick children to be recruited from all clusters will be 8910; adjusting for a 10 % loss to follow up and possible withdrawal of private outlets.
Discussion
The immediate sustainable impact will be appropriate treatment of sick children. The intervention is likely to impact on private sector practices since the scope of the services they provide will have expanded. The proposed study is also likely to have an impact on families as; i) they may appreciate the importance of timely referral on child illness management, ii) the cost savings related to reduced morbidity will be used by household to access other social services. The linkage between the private and public sectors will create a potential avenue for delivery of other public health interventions and improved working relations in the two sectors. Further, improved quality of services in the private sector will improve provider confidence and hopefully more clientelle to the private practices.
Trial registration
NCT02450630 Registration date: May/9th/2015
Similar content being viewed by others
Background
About half of mortality in children under five years of age in sub-Saharan Africa is caused by malaria, pneumonia and diarrhea [1]. Almost 60 % of parents with febrile children in Uganda first seek care in the private sector, especially at drug shops [2], however they provide sub-standard care [3, 4]. A functioning referral system is a critical part of an appropriate health care delivery system [5]. Referral systems have been given particular emphasis in the integrated community case management (iCCM), which is the recommended strategy for management of childhood illness in Africa [6]. In many developing countries, referral is an essential part of preventing unnecessary deaths: primary health care workers should refer children with life threatening illnesses which they are unable to treat properly [7]. In Uganda, the Ministry of Health encourages referrals from dispensaries and health centres to district hospitals, from district hospitals to regional and the National Referral hospitals [8]. Uganda’s under-five mortality is high, currently estimated at 66/1000 live births [9]. Low referral rates of sick children is one of the contributory factors [7, 8], particularly in those who seek care from the private sector.
Previous research in Uganda and elsewhere in Africa has found that referral rates of sick children from lower levels to higher levels of care are extremely low [7, 10–13]. Several factors have been attributed to poor referral rates including; lack of money and high costs involved in referral, long distances to the referral health facilities, poor attitudes of health workers, lack of drugs at the referral health facilities, lack of involvement of fathers in the referral process and waiting for malaria drugs provided at the lower level of care to finish [7, 11, 13, 14]. We propose an intervention designed to strengthen referral from private providers to higher level facilities with the aim of improving child survival by getting sick children to an appropriate level of care in a timely manner. The study targets children aged less than five years, especially in rural areas who have poor access to health interventions. The proposed intervention aims to improve uptake of referral advice for children that seek care from private facilities (registered drug shops/private clinics). We describe the trial management structure, interventions, design, and analysis plan, as well as expected contributions that this study can make.
Aim of the study
The aim of the study is to assess the effect of a strengthened referral system from the private sector on uptake of referral advice. The project addresses poor referral of children as one of the challenges in the reduction of under-five mortality in Uganda. The proposed intervention aims to improve uptake of referral advice for children who’s parents seek care from private facilities (registered drug shops/private clinics), by i) training VHTs to do community sensitization and raise awareness about saving money for referral at a household level, ii) training and supervision of providers in the private sector to diagnose, treat and refer sick children- training the private providers in iCCM and iii) regular meetings between the public and private providers (convened by the district health team) to discuss the referral system.
Objectives
The protocol focuses on one primary and two secondary objectives:
Primary objective
-
1.
To assess the effect of strengthening the referral system on uptake of referral of sick children who initially seek care in the private sector.
Secondary objectives
-
1.
To explore factors which influence the referral or non-referral of sick children from the private sector.
-
2.
To assess the effect of training private providers on appropriate case management for malaria, pneumonia and diarrhea.
Methods
Referral is defined here as any child under 5 years of age who has been seen at a private practitioner and recommended for higher level care. The private sector providers participating in this project will include private clinics and registered drug shops.
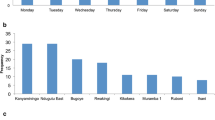
Setting
The study will be conducted in Mukono, central Uganda. The total population of the district is 583,600 and the majority, 88 % live in the rural areas. The district has an annual population growth rate of 2.3 % per annum and is inhabited by mainly the Baganda an indigenous ethnic group whose main occupation is subsistence agriculture [15]. The district was selected to implement the study because it is endemic for malaria. Mukono district is served by a network of health providers, including public, private not-for-profit and private for profit health care services, which makes the referral from private to public sector easy. The health policy in Uganda supports public-private partnerships to improve health outcomes [8].
Design
This study is a cluster randomized trial with two arms. Twenty clusters in Mukono district, central Uganda will be assigned to a control or intervention in the ratio 1:1, Fig. 1. A cluster was defined as a parish or neighbouring parishes if the distance between any two private health facilities located in each of the parishes is <1 km (to minimize possible spill over). The intervention consists of three components; i) VHTs will be trained to do community sensitization and raise awareness about saving money at a household level for to pay for future referral if care is needed, ii) training of the private providers in iCCM and provide with them with subsidized drugs, i.e., Artemesinin Combination Therapy (Coartem®) for malaria, amoxicillin for pneumonia, RDTs, Zinc and Oral Rehydration Salts (ORS) to treat diarrhea among children aged less than 5 years. They will also be trained in the use rapid diagnostic tests (RDTs) and how to recognize and distinguish uncomplicated and severe malaria, diarrhea and pneumonia; supply unit-dose packaged Coartem® for children with uncomplicated malaria and then administer rectal artesunate prior to referring children with severe and complicated malaria to a higher level of care (i.e., a health centre II and above), Fig. 2. These private providers will be supervised on how they diagnose, treat and refer sick children, iii) regular meetings between the public and private providers (convened by the district health team) will be held to discuss the referral system. In the control arm there will be standard of care (no training of private providers in iCCM, no community sensitization and no meetings between the public and private providers).
Study hypothesis
Clusters (private providers) implementing a strengthened referral system from the private sector (through community sensitization, training of private providers in iCCM, supervision on how they diagnose, treat and refer sick children, regular meeting between the public and private providers on referral of sick children and provision of subsized drugs) will have more referral uptakes of sick children compared to those clusters that do not receive the study interventions.
Principles for recruitment
Inclusion criteria
Cluster inclusion criteria
-
i)
Contain more than 200 households to ensure a sufficient number of sick children visiting the private outlets
-
ii)
Contained at least one registered drug shop/private clinic
-
iii)
Contain a health centre II, the lowest public health facility where referral for early treatment is recommended.
Cluster exclusion criteria
-
i)
Unregistered drug shop/private clinic
-
ii)
Non-government health facility located within the same parish
-
iii)
Fewer than 200 households in the parish where drug shop/private clinic is located
-
iv)
Health centre II facility does not have a qualified health worker. Some government health HCIIs in Uganda are run by nursing aides.
Clinic/drug shop inclusion criteria
If they are registered and consent to participate in the study.
Clinic/drug shop exclusion criteria
If they have just been established within one year, because such newly established units may not have created a clientele of customers.
Patient inclusion criteria
i) Children aged <5 years with a fever, cough or diarrhea or had a history of any of the above when presenting at the private outlet or; ii) Axillary temperature ≥ 37.5 °C).
Patient exclusion criteria
i) Sick children with no fever, cough, diarrhoea or any symptom and ii) If they are visitors in the area and have not spent 2 weeks in the village.
Randomization
Eligible clusters (20) will be randomly assigned as intervention or control arms. A process of restricted randomization will be utilised to balance cluster-level factors strongly associated with the primary outcome, or those expected to influence the effect of the intervention, between the study arms to ensure the credibility of the study and improve precision. The intervention is designed to address key barriers to effective treatment in the private sector; poor quality of care in the private sector, delay or no referral, and uptake of referral advice at a community level. Poor quality of care in the private sector may be attributed to inadequate training of providers in the private sector (in diagnosis and management of childhood illnesses); inadequate supervision and regulation; poor linkages and collaboration between the public and private sectors. Poor uptake of referral advice may be due to lack of awareness of severe signs for childhood illnesses and their consequences; and poor preparation of households in terms having finances for referral; and non-existent linkages between community structures and the public-private sectors. The intervention clusters will receive community awareness on referral, training of private providers in using RDTs/ICCM to treat and refer sick children, and supervision and regular meetings between the private and public sector, while the private providers in the control arm will only be trained in completing study tools i.e., filling in register and referral forms.
Blinding
There will be no blinding put in place i.e., for the participants (private providers), investigators and data collectors. However, the person who will analyse the data will be blinded.
Procedures
Baseline survey
Prior to randomization, a baseline survey will be done to guide the randomization process. GPS coordinates for the private premises will be taken and these will be used to define the boundaries of a cluster. This is because we defined a cluster as a parish or group of neighbouring parishes if the distance between any two private outlets located in these parishes is <1 km. This was done to avoid contamination.
Community sensitization
In the intervention arm, community consultation and sensitization will take place before implementing the intervention, to increase awareness about the need for referral within the community as summarized below;
-
A meeting will be held with the district heath team to share the project objectives and focus on improving management of sick children in the district.
-
Training of VHTs will take place in each of the study clusters. The village health teams will be mobilized at the village level before the start of recruitment, to inform communities within the study area of the trial, its purpose and what to expect.
Training of private providers
Private providers in the intervention arm will be convened in a central place and trained in iCCM and using RDTs. This will be after they have consented to participate in the study. They will be trained in diagnosis, treatment and referral according to iCCM guidelines. The training will be carried out by experts in iCCM, together with the study team. In addition, the providers will be trained in filling registers and referral forms. They will be awarded training certificates that are to be displayed on their premises, as well as pictorial job aids that will be used to explain diagnosis, treatment and referral to sick children. Furthermore, they will be supplied with a placard identifying them as an approved provider of sick children with diagnostic tests.
Private providers in the control arm will be only trained in filling of registers and referral forms and not in iCCM. They will not be given certificates or job aids. All private providers in both arms will be trained to record data on sick children aged less than 5 years who seek care at private outlets for a period of 12 months/years after enrolment.
The following data will be captured in patient registers and treatment forms distributed in both the intervention and control clusters:
-
a)
Demographic (age, sex, relationship to caretaker, marital status of caretaker, education levels, rural/urban residence)
-
b)
Social-economic data (household income, ownership of household items that determine expenditure and consumption levels, address and telephone contacts of caretakers);
-
c)
Type of illnesses, treatment given, prescription of drugs, referral advice, children referred and where referred.
Support supervision
Meetings between in-charges of health units and the private units in the intervention clusters will be convened at public health facilities on a quarterly basis to discuss the referral system. The VHTs and the private providers in the intervention arm will be supervised by the study team, the DHT and in-charges of health facilities. The supervision will be on a weekly basis in the first three months of the interventions and will be scaled down to monthly for the remaining nine months of the study period.
Interventions
The barriers to referral from the private sector to higher level facilities will be addressed through an intervention with three components; i) VHTs to do community awareness on referral and initiate discussions on saving schemes for referral costs; ii) training and supervision of providers in the private sector to diagnose, treat and refer sick children, and iii) regular meetings between the public and private providers (convened by the district health team) to discuss the referral system.
-
Intervention Arm – Community awareness on referral and training private providers in using RDTs/iCCM to treat and refer sick children and supervision and regular meetings between the private and public sector.
Training of the private providers in iCCM and provide them with subsidized drugs i.e., Coartem® for malaria, amoxicillin for pneumonia, RDTs, Zinc and Oral Rehydration Salts (ORS) to treat diarrhea among children aged less than 5 years. They were also be trained in the use of RDTs and how to recognize and distinguish uncomplicated and severe malaria, diarrhea and pneumonia; supply unit-dose packaged Coartem® for children with uncomplicated malaria and then administer rectal artesunate prior to referring these children with severe and complicated malaria to higher level facilities for care. Private providers will be given subsidized drugs. These private providers will be supervised on how they diagnose, treat and refer sick children.
Training on referral
Health workers in the intervention arm will be trained on how to recognize and distinguish uncomplicated & severe malaria, supplying unit-dose packaged Coartem® to customers with uncomplicated malaria, and administration of rectal artesunate prior to referral for higher level treatment of sick children with severe and complicated malaria, diarrhoea and pneumonia. Private health facilities will be provided with low literacy visual aids (job aids) to help explain the symptoms, diagnosis, correct treatment of malaria and danger signs for severe disease. The private outlets will be expected to explain the pictorial instructions to customers, as well as give instructions on dosing and how to give the drug to the patient. The age and sex of sick children, onset of symptoms and promptness of treatment-seeking, diagnosis (including RDT result, where appropriate), tablets supplied and outcome (treatment and/or referral) will be routinely recorded by private outlets for all sick children seeking treatment for fever, cough or diarrhea.
All private outlets in the intervention arm will be trained to give pre-referral treatment using a rectal artesunate suppository to children with danger signs consistent with severe malaria [16] and to refer these cases immediately to the nearest health unit for further treatment. Private outlets will also be trained to refer any RDT-negative sick children with danger signs and/or a temperature >38.5 °C to the nearest health unit as an urgent case. This additional temperature criterion is based on the WHO definition of hyperthermia and is intended to help ensure that those with severe bacterial infections are seen at a health unit. The sick children will be referred using an emergency referral form, including details of symptoms and the use of pre-referral treatment.
For patients who are RDT negative with no serious symptoms, private providers will be trained to advise caretakers on tepid sponging, but to return for further assessment at the facility or a health facility should the symptoms persist or worsen.
In the control arm, private providers will be trained in completing study tools i.e., filling in referral forms and the rest will be business as usual (no training of private providers in iCCM, no community sensitization and no meetings between the public and private providers, Table 1.
-
Control Arm – Training of private providers in completing study tools i.e., filling in register and referral forms. No community awareness on referral
Study outcomes and analytic methods
The primary analytic approach is intention to treat with children in the clusters in the intervention arm considered exposed to the intervention. Data for all of the primary and secondary outcome variables will be captured on the routine treatment recording forms and all consultations for fever, pneumonia and diarrhea routinely completed by drug shop vendors/private clinics. The outcome of referral will be recorded on the referral forms by health staff for referred sick children presenting to health facilities with a referral form. The primary trial outcome is the proportion of sick children referred from a private outlet that complete referral (seen at higher level facilities). The denominator includes all referrals of sick children with a history of fever, pneumonia and diarrhoea. Through review of records at the private health facilities, care takers whose children are referred in a specific period of time will be followed up in their respective communities to verify whether they took up referral. Secondary outcomes are; appropriate case management for malaria, pneumonia and diarrhea among children and factors which influence referral or non-referral of sick children from the private sector. Other outcomes include the proportion of sick children seeking care at private outlets within 24 h of onset of symptoms, and time between consultations at private outlets and uptake of referral at health facilities (referral facilities).
A cluster-level approach to the analysis will be used due to the small number of clusters per arm [17]. The proportion relating to this primary outcome will be calculated in each cluster. If the distribution of the proportions in each study arm is skewed a logarithmic transformation will be applied and the geometric mean proportions computed. To compare the intervention with the control arm point estimates based on these cluster summaries will be used to derive risk differences; using a weighted average of the cluster proportions, with weights proportional to the sample size for each cluster, since consultation rates differ between drug shops/private clinics and clusters. If the data have been log transformed, this will be the ratios of the geometric means. Corresponding 95 % confidence intervals will be computed assuming separate estimates of the variances in the two study arms, or if log transformed using an estimate of the pooled standard deviation of the log-transformed cluster summaries. The null hypothesis that there is no intervention effect will be tested using an unpaired t-test. Finally, an estimate of the coefficient of variation, k, will be provided. The overall mean proportion of sick children referred in the intervention arm, with 95 % confidence interval, will be computed using a random effects model to account for cluster sample. This analysis will be restricted to data from the treatment records of registered drug shop/private clinics enrolled in the intervention arm of the trial. A two-stage process will be carried out to adjust for covariates. At the first stage a regression model will be fitted incorporating the covariate(s) of interest, except the study arm. Expected values from this model will be compared with observed values by computing a residual, based on the difference between observed and expected, for each cluster. In the second stage, adjusted risk differences and 95 % CIs will be estimated as described above, replacing the cluster-level proportions with the covariate adjusted residuals. The covariates that will be adjusted for include balance criteria used in randomization at cluster level (primary endpoint at baseline); level of qualification, number of years working as a drug shop vendor/private clinic and/or health worker; age of sick child, education level of caretaker, and occupation of caretaker. A test for interaction will be carried out, and a 95 % confidence interval computed, using the methods of [18]. The above methods will also be used to analyse the other secondary outcomes; appropriate case management for malaria, pneumonia and diarrhea among children in the private sector and time between consultations at private outlets and uptake of referral at health facilities (referral facilities).
Factors which influence the referral or non-referral of sick children from the private sector will be explored through focus group discussions and key informant interviews. Coding of the transcripts will take place through an iterative process, with data being grouped into themes drawn from idea codes to generate a ‘node tree of ideas’.
Primary outcome:
-
The proportion of sick children referred from the private sector that completes the referral process (seen at higher health facilities), Table 2.
Secondary outcomes:
-
Appropriate case management for malaria, pneumonia and diarrhea among children in the private sector.
-
Factors which influence the referral or non-referral of sick children from the private sector.
Sample size estimation
The study will recruit 319 sick children per cluster and the total number of sick children to be recruited from all clusters will be 8910; adjusting for a 10 % loss to follow up and possible withdrawal of private outlets. This was based on assumption that the intervention will increase the primary outcome from 28 to 40 %, at a study power of 80 %, 5 % level of significance and a cluster correlation k, of 0.15; 20 clusters will be required. Ten (10) of them will be randomly allocated to the intervention and 10 to the control arm.
Study status
The intervention will last one year and 4 months have elapsed since we implemented.
Discussion
Critical barriers in the implementation of child survival interventions are poor quality of care in the private sector and timely referral and uptake of referral advice at community level. Poor referral of sick children, particularly those that seek care from the private sector is one of the contributory factors to Uganda’s high under-five mortality. The proposed intervention aims to improve referral and uptake of referral advice for children that seek care from private facilities. The barriers to referral may be attributed to inadequate training of providers in the private sector (in diagnosis and management of childhood illnesses); inadequate supervision and regulation; poor linkages and collaboration between the public and private sectors; and non-existent linkages between community structures and the private sector. These barriers will be addressed through an intervention with three components; i) VHTs to raise community awareness on the importance of referral and encouraging families to save money for referral, ii) training and supervision of providers in the private sector to diagnose, treat and refer sick children, iii) regular meetings between the public and private providers to discuss the referral system.
Studies in Uganda and elsewhere have shown that drug shop attendants can be trained to offer appropriate treatement for fever, cough or diarrhea, can procure and store ACTs and RDTs and dispose them off safely [19]. What is currently lacking is the evidence on how to link the private and public sectors. This study will add to ongoing research to demonstrate that such collaboration to improve referral of sick children may be succesful. The immediate impact will be appropriate treatment of sick children. The linkage between the private and public sectors will create a potential avenue for delivery of other public health interventions and improved working relations in the two sectors. Further, improved quality of services in the private sector will improve provider confidence and hopefully more clientelle to the private practices. The long term effect will be reduction in child mortality.
Conclusions
The data generated from this study will contribute to an understanding of factors of importance for strengthening the referral system, including optimal training required, supervision activities, and community participation. The lessons learned are likely to inform programming at a national and district level to improve referral of children from the private sector.
Abbreviations
- ACTs:
-
Artemensin contain treatment/drugs
- iCCM:
-
Integrated community case management
- RDTs:
-
Rapid diagnostic test
- VHTs:
-
Village heath teams
References
Lozano R, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Rutebemberwa E, et al. Utilization of public or private health care providers by febrile children after user fee removal in Uganda. Malar J. 2009;8:45.
Awor P, et al. Private sector drug shops in integrated community case management of malaria, pneumonia, and diarrhea in children in Uganda. Am J Trop Med Hyg. 2012;87(5 Suppl):92–6.
Smith F. The quality of private pharmacy services in low and middle-income countries: a systematic review. Pharm World Sci. 2009;31(3):351–61.
WHO. Primary health care. “Health for all”. Geneva: World Health Organization; 1978.
Young M, et al. World health organization/united nations Children’s fund joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children. Am J Trop Med Hyg. 2012;87 Suppl 5:6–10.
Font F, et al. Paediatric referrals in rural Tanzania: the Kilombero district study- a case series. BMC Int Health Hum Rights. 2002;2(1):4.
MoH. Health sector strategic plan III 2010/11-2014/15. Kampala: Ministry of Health, Uganda; 2010.
UNICEF. Commiting to child survival: a promise renewed, in progress report 2014. New York: UNICEF; 2014.
Achan J, et al. Case management of severe malaria-a forgetten practice: experiences from health facilities in Uganda. Plos ONE. 2011;6(3):e17053.
Kallander K, et al. Community referral in home management of malaria in western Uganda: a case series study. BMC Int Health Hum Rights. 2006;6:2.
Oryema-Lalobo M. Community health seeking practices for the management of malaria of the under-five in Bugiri District, Uganda. East Afr J Public Health. 2009;6(2):191.
Peterson S, et al. Coping with paediatric referral--Ugandan parents’ experience. Lancet. 2004;363(9425):1955–6.
Mbonye AK. Prevalence of childhood illnesses and care-seeking practices in rural Uganda. ScientificWorldJournal. 2003;3:721–30.
Statistics, U.B.O. The statistical Abstract. Kampala: Uganda Bureau of Statistics; 2013.
WHO. Guidelines for the treatment of malaria. W.H. Organization, Editor. Geneva. 2015.
Hayes, R.J. and L.H. Moulton. Cluster randomized trials. Interdisciplinary statistic series. C. Hall/CRC, Editor. Florida. 2009.
Cheung YB, et al. A simple approach to test for interaction between intervention and an individual-level variable in community randomized trials. Trop Med Int Health. 2008;13(2):247–55.
Awor P, et al. Increased access to care and appropriateness of treatment at private sector drug shops with integrated management of malaria, pneumonia and diarrhoea: a quasi-experimental study in Uganda. PLoS One. 2014;9(12):e115440.
Acknowledgements
None.
Funding
The National Academy of Sciences peer reviewed and funded the study.
Availability of data and materials
Not applicable.
Authors’ contributions
AKM, EB and ER were the main contributors to the conceptualization of the study. PL made significant contribution to the study. All the authors read and approved the final draft.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the Higher Degrees, Research and Ethics Committee of Makerere University School of Public Health and the Uganda National Council for Science and Technology. All registered private outlets in the eligible study clusters will be asked to participate in the study. After a written consent, they will be enrolled in the study. Care takers participating in the assessment of uptake of referral will also provide a written informed consent, administered by the interviewers, including those aged 14–17 years as these are treated as emancipated minors. The Uganda National Council for Science and Technology defines emancipated minors as children who may independently provide informed consent to participate in research. They are individuals who are aged 14–17 years pregnant or married or have a child or cater for their own livelihood.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Buregyeya, E., Rutebemberwa, E., LaRussa, P. et al. Strengthening referral of sick children from the private health sector and its impact on referral uptake in Uganda: a cluster randomized controlled trial protocol. BMC Health Serv Res 16, 646 (2016). https://doi.org/10.1186/s12913-016-1885-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-016-1885-5