Abstract
Background
The evidence of preferences for infection prevention and control (IPC) intervention from system perspective was lacked. This study aimed to elicit nurses’ preferences for the intervention designed to improve IPC behaviors based on the Systems Engineering Initiative to Patient Safety (SEIPS) model using Discrete Choice Experiment (DCE).
Methods
A DCE was conducted among nurses who were on active duty and willing to participate from July 5th to 10th, 2021 in a tertiary hospital in Ganzhou City, Jiangxi Province, using convenience sampling. A self-administered questionnaire included scenarios formed by six attributes with varying levels based on SEIPS model: person, organization, tools and technology, tasks, internal environment and external environment. A conditional logit and latent class logit model were performed to analyze the data.
Results
A total of 257 valid questionnaires were analyzed among nurses. The results from the latent class logit model show that nurses’ preferences can be divided into three classes. For nurses in multifaceted-aspect-preferred class (41.9%), positive coefficients were obtained in those six attributes. For person-preferred class (19.7%), only person was positively significant. For environment-preferred class (36.4%), the most important attribute were tasks, tools and technology, internal environment and external environment.
Conclusions
This finding suggest that nurses have three latent-class preferences for interventions. Multifaceted interventions to improve IPC behaviors based on the SEIPS model are preferred by most nurses. Moreover, relevant measured should be performed targeted the latent class of person-preferred and external-environment-preferred nurses.
Similar content being viewed by others
Background
Healthcare-associated infections (HCAI) have become a major threat to global health, leading to the spread of drug-resistant organisms, prolonged hospital stays, long-term disability, increased mortality rates, and additional costs [1]. It is estimated that HCAI resulted in an increase of 13.89 days of hospitalization, an increase of 24881.37 average medical cost and an increase of 9438.46 average drug cost [2]. By implementing infection prevention and control (IPC) behaviors such as physical distancing, mask-wearing, and eye protection, the risk of HCAI can be greatly reduced, potentially leading to 55–70% fewer cases of HCAI [3, 4].
Previous studies have investigated the factors that influence IPC behavior in healthcare workers, primarily from a person-centered perspective [5, 6]. For example, subjective norm, subjective norm and perceived behavioral control are associated with hand hygiene behaviors according to theory of planned behavior [7]. Nevertheless, IPC is a complex system that entails numerous system-related components, including the individuals, workload, and the tools used and environment, etc. [5, 8,9,10]. Each of these system-related elements may pose risks for HCAI acquisition, making it essential to take into account all the system-related factors with respect to improve IPC behaviors. Unfortunately, most studies fail to incorporate critical system-related factors in the analysis of IPC process simultaneously, leaving out the relevant analysis and resulting in incomplete findings [11]. Some studies have attempted theoretical explorations of IPC behaviors in healthcare workers from a systems-oriented perspective, such as normalization process theory and non-representational theory [12, 13]. However, there is a lack of an explicit definition of key components or pathway regarding IPC mechanism [14]. Consequently, a system-related pathway exploration to fully understand the mechanisms of IPC.
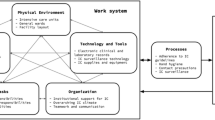
Systems Engineering Initiative to Patient Safety (SEIPS) model, developed specifically for healthcare to improve patient safety and medical quality through examining the mechanism in healthcare systems comprehensively [15]. An updated version of the SEIPS model, SEIPS 2.0, identifies specific structural components including person, organization, tools and technology, tasks, internal environment, and external environment and their contribution to the healthcare process and outcomes [16]. Our study chose the SEIPS 2.0 version as it is more appropriate for analyzing the impact of system-related factors on IPC behaviors among healthcare workers, while SEIPS 3.0 is more suitable for the exploration of healthcare transition [17]. The SEIPS model offers numerous benefits when applied to IPC. First, it has the potential to identify the principal contributors and barriers to IPC issues. Second, it provides a theoretical foundation for promoting IPC behavior from a system perspective, with its distinct elements and interrelatedness. Finally, it considers numerous broad outcomes and attaches equal importance to non-human factors, which constitutes a considerable advantage to solve system problem [18, 19]. However, there remains a significant dearth of quantitative evidence in the SEIPS model with regard to IPC-related problems.
Previous studies have not adequately addressed the evidence of nurses’ preference for IPC interventions. Nurses play a pivotal role in implementing IPC as the largest group of practitioners, and their high-level compliance with IPC behaviors is crucial in preventing the spread of HCAI, with the significant differences in the nature and social structure of nursing work compared to medicine and allied health professions [20]. Meanwhile, researchers can analyze how individuals’ preferences differ for each attribute and how the interaction of various elements affects their decision-making using discrete choice experiment (DCE). Within the context of enhancing IPC, this study aimed to utilize DCE to capture nurses’ preferences for interventions targeted at improving their IPC behaviors based on the SEIPS model. Obtaining such insight can provide effective support for interventions in the perspective of IPC system, while the further application of latent class analysis may facilitate the understanding of any variations that exist across different groups in their preferences to promote IPC behaviors among nurses.
Methods
Participants
The participants in this study were front-line nurses who were recruited from a tertiary hospital located in Ganzhou City, Jiangxi Province. The hospital is equipped with approximately 3,000 beds and ranks in the top three in performance assessments among similar hospitals in Jiangxi Province. We conducted a cross-sectional face-to-face questionnaire survey by convenience sampling from July 5th to 10th, 2021, among nurses who were on active duty and willing to participate.
The inclusion criteria included ① front-line nurses working in the clinic, ②having a minimum of one year of clinical work experience. The exclusion criteria encompassed ①interns, ②training staff. The sample size required was determined based on the number of choice tasks (t), the number of alternatives (a), and the largest number of levels for the attributes (c) using the equation N > 500c / (t × a) [21].According to the equation, the sample size of this study should be greater than 31.25.
Attributes and levels
DCE is a method that involves hypothetical scenarios to systematically investigate nurses’ preferences for interventions. To identify factors that influence IPC behaviors based on the SEIPS model, we conducted a literature review. Subsequently, we conducted a qualitative interview involving 18 expert healthcare workers (11 nurses, 5 doctors, and 2 infection preventionists) to confirm the attributes and levels based on the perspectives of stakeholders. The literature review and qualitative interviews informed the determination of the attributes and levels of the intervention based on the SEIPS model [22]. Six attributes were determined: person, organization, tools and technology, tasks, internal environment, and external environment. Overall. all attributes had two levels, except for IPC tasks, which had three levels (Table 1).
Questionnaire design and quality control
The D-efficiency design is the most efficient and widely used partial factorial design nowadays, which can ensure that each attribute is independent, and the different levels of each attribute appear at the same frequency. In this study, D-efficiency was designed by Ngene software generating 24 combinations in 2 blocks, with 12 combinations for each version. The survey was structured as follows (supplementary file): the aim and description of the research, a practice question with explanation, discrete choice questions (Table 2) and socio-demographic character: gender, age, work year, degree, title and department.
In terms of quality control in the data collection, this study implemented several measures. Firstly, a repeated design of a selection set was adopted to test the consistency of respondents’ answers. The questionnaire included 13 combination sets, with the 5th combination set repeated as the 13th combination set for validation purposes. Additionally, to ensure the survey’s clarity and ease of understanding for nurses, it underwent a pilot test with 20 clinical nurses. Based on their feedback, any inappropriate or confusing information was revised to enhance comprehension and interpretation. Furthermore, to ensure that respondents carefully read the scenarios, the questionnaire was administered in the presence of trained investigators.
Data analysis
Descriptive statistics were used to describe the characteristics of participants. We used a conditional logit model, which is a commonly-used DCE model derived by McFadden based on economic theory, to determine the average utility assigned to the attribute level compared to the reference level in the preference among nurses. Since the conditional logit model ignores preference heterogeneity, we employed a latent class logit model to further explore the potential classes in preference, as the latent class of preference is commonly seen. The latent analysis can examine both the homogeneous preferences within classes and heterogeneous preferences across classes [23]. The number of the latent classes was determined by comparing the model fitness in the model with 2, 3, 4, 5 and 6 classes. All levels were treated as categorical variables with the level of no measure taken as the reference, while dummy coding was applied for three attribute levels in the model. We considered p < 0.05 as the threshold for statistical significance, indicating that an attribute level is significantly different from that of the reference level. A positive coefficient indicates that an attribute level is preferred over the reference level in the intervention scenario. All the analyses were performed using Stata 15.0 (StataCorp LP, College Station, TX, USA).
Results
Participants’ characteristics
The response rate was 93.36%, with 301 questionnaires distributed and 281 valid questionnaires obtained. Finally, 259 questionnaires were included in the analysis, and 22 were excluded because of failing to pass logical consistency. Among the 259 survey respondents, most were women (256, 98.94%). The vast majority of nurses were younger than 45 years old (245, 94.59%), worked for less than 20 years (229, 88.42%), held intermediate or lower professional titles (232, 89.58%), and most had bachelor’s degrees (252, 97.30%) (Table 3).
Discrete choice experiment results: conditional logit model
From the results of the conditional logit model, person factor was the most valued in the attribute of IPC intervention. Nurses preferred interventions featured better IPC knowledge and awareness training (β = 0.797, P < 0.001) compared to interventions with no measures adopted. In addition, interventions were preferred when improvement of IPC organization and management (β = 0.318, P < 0.001), improvement of the availability and comfort of protective equipment (β = 0.475, P < 0.001), improvement of IPC workflow (β = 0.382, P < 0.001), reduced workload (β = 0.337, P < 0.001) and improvement of the physical (β = 0.450, P < 0.001) and external environment (β = 0.614, P < 0.001) were adopted (Table 4).
Discrete choice experiment results: latent class logit model
The results of the latent class logit model suggest that three classes are best suited to capture the preferences of nurses regarding IPC interventions based on the model parsimony and model fit. The largest proportion, comprising 41.9% of nurses, belonged to class one, which is referred to as the multifaceted-aspect-preferred class. Nurses in class one preferred the intervention that focused on better IPC knowledge and awareness training (β = 1.071, P < 0.001), IPC organization improvement (β = 0.799, P < 0.001), improvement of the availability and comfort of protective equipment (β = 0.955, P < 0.001), IPC workflow improvement (β = 0.804, P < 0.001), reduced workload (β = 0.326, P = 0.015), IPC physical environment improvement (β = 0.735, P < 0.001) and IPC external environment improvement (β = 0.603, P < 0.001). In general, nurses in class one preferred to address multiple aspects of IPC practice to create a comprehensive and effective intervention (Table 5).
The results of the latent class logit model indicate that 19.7% of nurses were in class two, which is referred to as the person-preferred class. This class had a strong preference for IPC knowledge and awareness training, with the coefficient of the person factor (better IPC knowledge and awareness training) being highly significant (β = 3.767, P < 0.001) while the coefficients for other factors were not significant. This suggests that nurses in this class place a great emphasis on the importance of training as a means to improve IPC behaviors.
According to the results of the latent class logit model, 36.4% of nurses fell into class three, which is referred to as the environment-preferred class. Nurses in this class placed high value on interventions that characterized as improvement of the availability and comfort of protective equipment (β = 0.268, P = 0.001), IPC workflow improvement (β = 0.252, P = 0.030), reduced workload (β = 0.600, P < 0.001), IPC physical environment improvement (β = 0.415, P < 0.001) and IPC external environment improvement (β = 0.962, P < 0.001). However, unlike the characteristics above, person (better IPC knowledge and awareness training) (β=-0.056, P = 0.509) and organization (IPC organization improvement) (β = 0.044, P = 0.853) had little influence on nurses’ willingness to choose interventions. Nurses in this class tended to adopt the intervention with external environment improvement mostly (Fig. 1).
Discussion
This study explored nurses’ preferences for the intervention designed to improve IPC behaviors based on the SEIPS model. Our results suggested the heterogeneity among nurses in the preferences of interventions for IPC behaviors. In addition to the multifaceted-aspect-preferred class, nurses can also be categorized into person-preferred class and environment-preferred class.
The latent class logit model used in this study demonstrated superior fitness to the data, handling preference heterogeneity and information richness more effectively than the conditional logit models. The analysis revealed three distinct classes of nurses with different preferences for IPC behavior interventions.
The majority of nurses, belonging to multifaceted-aspect-preferred class, preferred interventions that comprehensively improve person, organization, technology and tools, task, internal environment, and external environment factors in the SEIPS model, which are consistent with previous studies [24,25,26]. The key attributes of the intervention strategy involving several aspects of the IPC work system in the SEIPS model, such as person, organization, tool and technology, task, internal environment and external environment factors, have been highlighted in previous studies as essential components in successful interventions. For example, Gould et al. identified the importance of interventions that improve the internal environment, such as increasing the availability of hand hygiene consumption, training through different types of education, and organizational support [9], while McAteer et al. emphasize the significance of the improvement of IPC tasks by providing designated time for IPC tasks and appropriate assignment of IPC tasks based on qualitative research [27]. Personal factors such as capacity, knowledge, and attitude play a crucial role in successful IPC practices, while organizational factors such as safety atmosphere, organizational commitment, and leadership are essential in promoting a culture of infection prevention [28]. Improving technology and tools, such as hand hygiene equipment, and the comfort of personal protective equipment also contribute to better adherence to IPC practices [26]. Finally, the design of tasks [5], and the internal and external environment of clinical settings also impact the effectiveness of IPC practices [25, 29]. The results of this study add to the existing literature by providing further evidence that the intervention approach in line with the SEIPS model can be a successful strategy for improving IPC behaviors among nurses. By addressing multiple aspects of the IPC work system, the intervention that addresses the needs and preferences of different nurses can effectively encourage the compliance to IPC practices, and ultimately improve patient outcomes.
Class two (person-preferred class), comprising the smallest number of nurses, demonstrates a strong inclination towards IPC behavior training as a means to enhance their infection prevention and control practices. The fact that this class had no preference in other attribute indicates that they may not prioritize other attributes of intervention as much as training. This finding corresponds to previous studies where some nurses believed that their poor IPC behaviors attribute to lack of knowledge about their significance and the consequences of not following them [4]. Furthermore, due to limited knowledge about IPC among many nurses, training may be the primary approach to enhance their knowledge and attitudes towards IPC that they can readily acknowledge. Consequently, there is a tendency for nurses to prioritize this attribute when making choices.
The findings of this study suggest that approximately one-third of nurses (class three), belonging to environment-preferred class, have no differences in the preference of interventions that focus on IPC knowledge and awareness training or IPC organization improvement. These nurses instead prioritize external factors, such as tools and technology, task, internal environment and external environment. This preference is in accordance with the principles of the human factors approach, which emphasizes the importance of considering the system as a whole rather than attributing errors solely to individuals [30]. In addition, the non-selection of training and management in nurses may be explained by the excessive workload and demands on their time due to the training [31]. Frequent or complex training and examinations can often lead to fatigue among nurses, posing as an obstacle to improving IPC behaviors. Healthcare organizations should strive to provide appropriate training and management to support nurses in their IPC practices. Meanwhile, by addressing the external factors, healthcare organizations can ensure that nurses have the resources and tools needed to carry out effective IPC practices.
Implication
This study used DCE to quantify the preferences of nurses for IPC behavior improvement strategies and provide a useful reference for hospital managers and policymakers in designing and implementing effective IPC behavior improvement strategies. The classification of nurses into different classes suggests that adjustments need to be made based on the differing preferences when devising intervention strategies. To better address the needs of nurses, intervention strategies should comprehensively consider factors related to the SEIPS model. These factors include enhancing IPC knowledge and awareness through training, improving IPC organization, ensuring the availability and comfort of protective equipment, optimizing IPC workflow, reducing workload, enhancing the physical environment for IPC, and addressing external environmental factors. Furthermore, in cases where interventions may not yield optimal results, it is important to incorporate preference-based measures tailored to this population of nurses. Measures such as targeted IPC training, reducing training and examination pressures, or enhancing the training or work environment can be explored to ensure the effectiveness of interventions. In the future, it would be valuable to further explore the characteristics and influencing factors of latent classes among nurses.
Limitations
Although we tried our best to investigate nurses who were on duty to ensure the data are representative, participants in this study were recruited from one tertiary hospital, which potentially could limit the generalizability and application of the study’s findings to other healthcare settings. In the future, this model can be further evaluated among primary medical staff to ensure that it is generalizable across different healthcare contexts.
Conclusions
The study’s findings identified three classes of nurses with different preferences for IPC behavior interventions. Most nurses exhibited a preference for comprehensive interventions that considered various factors related to the SEIPS model. Apart from multifaceted-aspect-preferred class, nurses can also be divided into person-preferred class and environment-preferred class. It is, therefore, essential to perform preference-based measures in different classes to ensure the acceptability and effectiveness of the intervention. This approach can help tailor the IPC intervention strategies to the specific needs of each class of nurses, thereby ensuring its effectiveness and sustainability.
Data availability
The data that support the findings of this study are available from surveyed local institutions but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of surveyed local institutions.
Abbreviations
- SEIPS:
-
Systems Engineering Initiative to Patient Safety
- IPC:
-
infection prevention and control
- HCAI:
-
healthcare-associated infections
- DCE:
-
Discrete Choice Experiment
References
Weiner-Lastinger LM, Abner SEJ, Kallen AJ, Karlsson M, Magill SS, Pollock D, See I, Soe MM, Walters MS, Dudeck MA. Antimicrobial-resistant pathogens associated with adult healthcare-associated Infections: Summary of data reported to the National Healthcare Safety Network, 2015–2017. Infect Control Hosp Epidemiol. 2020;41:1–18. https://doi.org/10.1017/ice.2019.296.
Liu X, Spencer A, Long Y, Greenhalgh C, Steeg S, Verma A. A systematic review and meta-analysis of Disease burden of healthcare-associated Infections in China: an economic burden perspective from general hospitals. J Hosp Infect. 2022;123:1–11. https://doi.org/10.1016/j.jhin.2022.02.005.
Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schunemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–87. https://doi.org/10.1016/S0140-6736(20)31142-9.
Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of Healthcare-Associated Infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32:101–14. https://doi.org/10.1086/657912.
Ataiyero Y, Dyson J, Graham M. Barriers to hand hygiene practices among health care workers in sub-saharan African countries: a narrative review. Am J Infect Control. 2019;47:565–73. https://doi.org/10.1016/j.ajic.2018.09.014.
Srigley JA, Corace K, Hargadon DP, Yu D, MacDonald T, Fabrigar L, Garber G. Applying psychological frameworks of behaviour change to improve healthcare worker hand hygiene a systematic review. J Hosp Infect. 2015;91:202–10. https://doi.org/10.1016/j.jhin.2015.06.019.
Jeong SY, Kim KM. Influencing factors on hand hygiene behavior of nursing students based on theory of planned behavior: a descriptive survey study. Nurse Educ Today. 2016;36:159–64. https://doi.org/10.1016/j.nedt.2015.09.014.
Bae S. The ways in which healthcare interior environments are associated with perception of safety from infectious Diseases and coping behaviours. J Hosp Infect. 2020;106:107–14. https://doi.org/10.1016/j.jhin.2020.06.022.
Gould DJ, Moralejo D, Drey N, Chudleigh JH, Taljaard M. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev 2017 9.https://doi.org/10.1002/14651858.CD005186.pub4.
Allegranzi B, Sax H, Pittet D. Hand hygiene and healthcare system change within multi-modal promotion: a narrative review. J Hosp Infect. 2013;83:3–S. https://doi.org/10.1016/S0195-6701(13)60003-1.
Bail K, Willis E, Henderson J, Blackman I, Verrall C, Roderick A. Missed Infection control care and healthcare associated Infections: a qualitative study. Collegian. 2021;28:393–9. https://doi.org/10.1016/j.colegn.2020.11.007.
Agreli H, Barry F, Burton A, Creedon S, Drennan J, Gould D, May CR, Smiddy MP, Murphy M, Murphy S, et al. Ethnographic study using normalization process theory to understand the implementation process of Infection prevention and control guidelines in Ireland. BMJ Open. 2019;9e029514. https://doi.org/10.1136/bmjopen-2019-029514.
Hooker C, Hor S, Wyer M, Gilbert G, Jorm C, Iedema R. Trajectories of hospital Infection control: using non-representational theory to understand and improve Infection prevention and control. Soc Sci Med. 2020;256:113023. https://doi.org/10.1016/j.socscimed.2020.113023.
Smiddy MP, O’ Connell R, Creedon SA. Systematic qualitative literature review of health care workers’ compliance with hand hygiene guidelines. Am J Infect Control. 2015;43:269–74. https://doi.org/10.1016/j.ajic.2014.11.007.
Carayon P, Schoofs Hundt A, Karsh BT, Gurses AP, Alvarado CJ, Smith M, Flatley Brennan P. Work system design for patient safety: the SEIPS mode. Qual Saf Health Care. 2006;Suppl 1i50–58. https://doi.org/10.1136/qshc.2005.015842.
Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56:1669–86. https://doi.org/10.1080/00140139.2013.838643.
Carayon P, Wooldridge A, Hoonakker P, Hundt AS, Kelly MM. SEIPS 3.0: human-centered design of the patient journey for patient safety. Appl Ergon. 2020. https://doi.org/10.1016/j.apergo.2019.103033.
Backman C, Marck PB, Krogman N, Taylor G, Sales A, Bonten MJ, Gigengack-Baars AC. Barriers and bridges to Infection prevention and control: results of a qualitative case study of a Netherlands’ surgical unit. BMJ Open. 2012. https://doi.org/10.1136/bmjopen-2011-000511.
Patel PR, Kallen AJ. Human factors and Systems Engineering: the future of Infection Prevention? Infect Control Hosp Epidemiol. 2018;39:849–51. https://doi.org/10.1017/ice.2018.122.
Dekker M, Jongerden IP, van Mansfeld R, Ket JCF, van der Werff SD, Vandenbroucke-Grauls CMJE, de Bruijne MC. Infection control link nurses in acute care hospitals: a scoping review. Antimicrob Resist Infect Control. 2019;8. https://doi.org/10.1186/s13756-019-0476-8.
de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA. Sample size requirements for Discrete-Choice experiments in Healthcare: a practical guide. Patient. 2015;8:373–84. https://doi.org/10.1007/s40271-015-0118-z.
Zhou Q. Influencing mechanism of Infection Prevention and Control Behaviors in Medical Staff based on systems Engineering Initiative to Patient Safety Model. Huazhong University of Science and Technology; 2022.
Karim S, Craig BM, Vass C, Groothuis-Oudshoorn CGM. Current practices for Accounting for Preference heterogeneity in Health-Related Discrete Choice experiments: a systematic review. PharmacoEconomics. 2022;40:943–56. https://doi.org/10.1007/s40273-022-01178-y.
Lydon S, Greally C, Tujjar O, Reddy K, Lambe K, Madden C, Walsh C, Fox S, O’Connor P. Psychometric evaluation of a measure of factors influencing hand hygiene behaviour to inform intervention. J Hosp Infect. 2019;102:407–12. https://doi.org/10.1016/j.jhin.2019.02.003.
Lai X, Wang X, Yang Q, Xu X, Tang Y, Liu C, Tan L, Lai R, Wang H, Zhang X, et al. Will healthcare workers improve Infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob Resist Infect Control. 2020;983. https://doi.org/10.1186/s13756-020-00746-1.
De Leeuw JA, Woltjer H, Kool RB. Identification of Factors Influencing the Adoption of Health Information Technology by nurses who are digitally lagging: In-Depth interview study. J Med Internet Res. 2020;22:e15630. https://doi.org/10.2196/15630.
McAteer J, Stone S, Fuller C, Michie S. Using psychological theory to understand the challenges facing staff delivering a ward-led intervention to increase hand hygiene behavior: a qualitative study. Am J Infect Control. 2014;42:495–9. https://doi.org/10.1016/j.ajic.2013.12.022.
Chen W, Tseng CL. What are healthcare workers’ preferences for hand hygiene interventions? A discrete choice experiment. BMJ Open. 2021;11. https://doi.org/10.1136/bmjopen-2021-052195.
Kelly D, Kutney-Lee A, Lake ET, Aiken LH. The critical care work environment and nurse-reported health care-associated Infections. Am J Crit Care. 2013;22:482–8. https://doi.org/10.4037/ajcc2013298.
Bail K, Grealish L. Failure to maintain’: a theoretical proposition for a new quality indicator of nurse care rationing for complex older people in hospital. Int J Nurs Stud Adv. 2016;63:146–61. https://doi.org/10.1016/j.ijnurstu.2016.08.001.
CDC COVID-19 Response Team. Characteristics of Health Care Personnel with COVID-19 — United States, February 12–April 9. MMWR Morb Mortal Wkly Rep. 2020;64:477–81. https://doi.org/10.15585/mmwr.mm6915e6.
Acknowledgements
The authors would also like to acknowledge Wang Ying, Wang Yongyi, and Yu Tiantian in data collection.
Funding
This research was funded by 2021 Wuhan Medical Research Project, grant number WG21D05 and 2022 Clinical research program of Wuhan Children’s Hospital, grant number 2022FE019.
Author information
Authors and Affiliations
Contributions
X.P.Z. and Q.Z. conceived and designed the study. H.L. and L.T. collected the data. Q.Z. and X.P.Z. performed the statistical analysis. X.P.Z., J.J.L., F.Y.Z., Q.N.W. and W.J.L. contributed to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG: IORG0003571). Written informed consent was obtained from the respondents, and any information that could identify participants was guaranteed confidentiality. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, Q., Liu, J., Zheng, F. et al. Nurses’ preferences for interventions to improve infection prevention and control behaviors based on systems engineering initiative to patient safety model: a discrete choice experiment. BMC Nurs 23, 29 (2024). https://doi.org/10.1186/s12912-024-01701-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-01701-w