Abstract
Objective
Suicide is a complex and multifactorial public health problem. Understanding and addressing the various factors associated with suicide is crucial for prevention and intervention efforts. Machine learning (ML) could enhance the prediction of suicide attempts.
Method
A systematic review was performed using PubMed, Scopus, Web of Science and SID databases. We aim to evaluate the performance of ML algorithms and summarize their effects, gather relevant and reliable information to synthesize existing evidence, identify knowledge gaps, and provide a comprehensive list of the suicide risk factors using mixed method approach.
Results
Forty-one studies published between 2011 and 2022, which matched inclusion criteria, were chosen as suitable. We included studies aimed at predicting the suicide risk by machine learning algorithms except natural language processing (NLP) and image processing.
The neural network (NN) algorithm exhibited the lowest accuracy at 0.70, whereas the random forest demonstrated the highest accuracy, reaching 0.94. The study assessed the COX and random forest models and observed a minimum area under the curve (AUC) value of 0.54. In contrast, the XGBoost classifier yielded the highest AUC value, reaching 0.97. These specific AUC values emphasize the algorithm-specific performance in capturing the trade-off between sensitivity and specificity for suicide risk prediction.
Furthermore, our investigation identified several common suicide risk factors, including age, gender, substance abuse, depression, anxiety, alcohol consumption, marital status, income, education, and occupation. This comprehensive analysis contributes valuable insights into the multifaceted nature of suicide risk, providing a foundation for targeted preventive strategies and intervention efforts.
Conclusions
The effectiveness of ML algorithms and their application in predicting suicide risk has been controversial. There is a need for more studies on these algorithms in clinical settings, and the related ethical concerns require further clarification.
Highlights
• Understanding various factors associated with suicide is crucial for prevention and intervention efforts.
• Machine learning (ML) could enhance the prediction of suicide attempts.
• The neural network (NN) algorithm exhibited the lowest accuracy of 0.70.
• The random forest demonstrated the highest accuracy for suicide prediction.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Suicide is a global concern recognized by the World Health Organization (WHO), with a life lost to suicide every 40 s, making suicide prevention a pressing priority worldwide [1]. This form of violent death not only brings personal tragedy but also poses a significant threat to communities’ socio-psychological well-being and stability [2]. While suicide is a complex phenomenon influenced by multiple factors, behavioral, lifestyle, and clinical, can significantly contribute to an elevated risk of suicide [3]. For example, substance use can be considered a significant factor for suicide within the behavioral category [4]. Job and financial problems serve as important examples of lifestyle-related suicide risk [5]. Additionally, mental disorders are crucial clinical factors associated with suicide risk [6]. Early identification of risk factors is crucial in predicting suicide [7, 8]. The prevalence of suicide is exceptionally high among adolescents and young adults, specifically those aged 15 to 44, it is not a universal phenomenon [9]. Research indicates that, in some countries the lower risk of suicide among older individuals may be due to their enhanced resilience and greater capacity to cope with adversity, potentially reducing the likelihood of suicidal behavior [10, 11]. The other common factor can be gender. Some studies have revealed that gender differences in suicide rates indicate that men are more likely to die by suicide. However, this remains controversial because each gender is influenced by many other biological and environmental factors [12]. Suicide imposes financial burden on the healthcare system. For example, in Canada, New Zealand, and Ireland, the estimated direct and indirect costs of each suicide are approximately 443,000, 1.1 million, and 1.4 million pounds, respectively [13,14,15]. A comprehensive review of the works by these authors leads us to the conclusion that suicide is a global issue. Consequently, it is imperative for countries worldwide to collaborate in addressing this concern [1]. There is a growing interest in utilizing machine learning (ML) techniques for predicting suicide risk to address the issue. ML is a combination of statistical and computational models that can learn from data and improve through experience [16]. It is categorized into two main types: supervised and unsupervised. In supervised learning, the model is trained on labelled databases; however, in unsupervised learning, the model relies on unlabeled databases [17]. Both supervised and unsupervised algorithms can be utilized for suicide prediction depending on the type of database and the nature of the prediction.
Research by Walsh, Ribeiro, and Franklin (2017) demonstrated the superior performance of ML over conventional methods in accurately identifying suicide attempts [9]. ML methods have gained prominence due to their ability to extract valuable insights from diverse datasets and organize data efficiently [10, 11]. While ML shows promise in predicting suicide events, it is vital to consider the varied outcomes produced by different ML algorithms. The study conducted by various researchers suggests that while there have been notable scientific advancements in leveraging digital technologies, such as ML algorithms to prevent suicide attempts and identify at-risk individuals, there are still limitations in terms of training, knowledge, and the integration of databases [18,19,20]. Current suicide risk assessment methods heavily rely on subjective questioning, limiting their accuracy and predictive value [21]. As such, this study aims to systematically review previous research that has applied ML methods to predict suicide attempts and identify patients at high risk of suicide. The primary objectives are to evaluate the performance of various ML algorithms and summarize their effects on suicide. Additionally, the study aims to identify significant variables that serve as more effective suicide risk factors.
Materials and methods
Search strategy and study selection
We adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to systematically identify, select, and assess relevant studies for inclusion in our review. Our search strategy focused on PubMed, Scopus, Web of Science and SID databases, and there were no limitations on the publication date, ensuring comprehensive coverage of the literature. The project was initiated on June 1, 2022, and concluded on August 8, 2023, with a focus on two domains: machine learning (ML) and suicide.
To capture relevant studies, our search strategy incorporated keywords such as “self-harm”, “self-injury”, “self-destruction”, “self-poisoning”, “self-mutilation”, “self-cutting”, “self-burning”, “suicid*”. Additionally, we explored using artificial intelligence and ML techniques to predict suicidal attempts by employing “AND” and “OR” operators. The management of literature was facilitated through Endnote X7.
The study encompassed two primary outcomes: first, identifying the most effective ML algorithms based on their outcome measures, and second, identifying influential risk factors for predicting suicide. These outcomes were instrumental in achieving a comprehensive understanding of the field and informing our research objectives.
Inclusion & exclusion criteria
Inclusion criteria were applied to identify relevant studies for our review. The following criteria were considered:
-
1.
Population: Studies that included participants from various age groups, including pediatrics, geriatrics, and all-age populations, were included.
-
2.
Language: Only studies published in the English language were included.
-
3.
Methods: Studies employing ML methods to predict suicide were included.
-
4.
Publication format: Studies published as journal articles, theses, and dissertations were included.
-
5.
Study design: Various study designs, including prospective, retrospective, retrospective cohort, case-cohort, case-control, cohort, diagnostic/prognostic, longitudinal, longitudinal cohort, longitudinal prospective, prognostic, prospective cohort, retrospective, retrospective cohort, and randomized control trial studies, were considered for inclusion.
Exclusion criteria were applied to select relevant studies for our analysis. Studies were excluded if they met the following criteria:
-
1.
Population: Studies focusing specifically on military personnel and veterans were excluded. Including military personnel and veterans in our analysis could introduce unique variables and considerations related to their distinct healthcare needs, access to services, and experiences. For example, military personnel and veterans often have specific healthcare requirements stemming from their service-related experiences. These may encompass a range of issues, including physical injuries sustained during deployment, exposure to hazardous environments leading to unique health challenges, and complex medical histories shaped by their military service.
Moreover, their access to healthcare services can differ significantly from that of the general population. To maintain the homogeneity of our study population and to ensure the relevance and applicability of our findings to the specific context of hospitals, we have opted to exclude this subgroup.
-
2.
Social media-based studies: Studies aiming to predict suicide attempts using ML among adults who posted or searched content related to suicide on internet platforms such as Twitter, Instagram, and Google were excluded.
-
3.
Natural language processing (NLP) and image processing methods: Studies utilizing NLP and image processing techniques for predicting suicide attempts were excluded.
-
4.
Publication type: Conference papers, reviews, letters to editors, book chapters, and commentary papers were excluded from the analysis.
By applying these inclusion and exclusion criteria, we aimed to select studies that align with the objectives and focus of our research.
Data collection process
Data extraction was conducted using Microsoft Excel 2016 spreadsheet. The following information was extracted from each included study:
-
1.
Study title: The title of the research article.
-
2.
Authors: The names of the authors involved in the study.
-
3.
Year of publication: The year in which the study was published.
-
4.
Country of study: The geographical location where the study was conducted.
-
5.
Population: The target population or participants involved in the study.
-
6.
Type of study: The research design employed in the study.
-
7.
Sample size: The number of participants included in the study.
-
8.
Study objective: The main objective or aim of the study.
-
9.
Suicide risk factors: Factors or variables considered in predicting suicide risk.
-
10.
ML models: The specific ML models used in the study.
-
11.
Outcome measures: Various performance metrics used to evaluate the models, including area under the curve (AUC), sensitivity, specificity, accuracy, false negative rate, false positive rate, true positive rate, negative predictive value, positive predictive value, precision, and recall.
Quality assessment
The quality of the included articles was assessed using the Mixed Methods Appraisal Tool (MMAT 2018) following the search process. We adopted MMAT’s five sets of criteria to evaluate the quality of each type of study included in our analysis, namely qualitative, randomized controlled, nonrandomized, quantitative descriptive, and mixed methods studies [8]. This rigorous assessment process allowed us to evaluate the included studies’ methodological quality and ensure our findings’ reliability and validity.
Data analysis methods
During the quantitative phase, the extracted data were analyzed using STATA 14.1 statistical software to conduct meta-analytic procedures. We applied the Freeman-Tukey double arcsine transformation to estimate the pooled prevalence of study outcomes and their corresponding 95% confidence intervals (CI). This transformation was also utilized to stabilize variances when generating the CIs. A random-effects model based on DerSimonian and Laird’s method was employed in the pooled data collection to account for between-study variability. This model incorporated the variability using the inverse-variance fixed-effect model [22, 23].
In the qualitative phase, the extracted data was imported into MAXQDA 20 software to facilitate meta-synthesis procedures. This critical stage involved coding the suicide risk factors from our final studies based on various themes or categories, such as demographic (demographic factors, such as age, gender, marital status), clinical and behavioral (certain behaviors, like impulsivity, self-harm, or aggression, and clinical factors involve mental health diagnoses and conditions), lifestyle (encompass aspects of an individual’s daily life, including habits and routines), laboratory and biomarkers (these could include genetic markers, hormonal imbalances), and questionnaires (the use of standardized scales and questionnaires helps quantify and measure psychological factors associated with suicide risk). Through this process, we aggregated the coded data to identify common suicide risk factors across all the studies, allowing for a comprehensive understanding of the topic.
Publication bias
We researched various languages and databases to address study, citation and database biases. We enhanced our search strategy, resulting in the identification of 7529 publications. This abundance of sources highlights the prevalence of multiple-citation publications within our dataset. Given the common occurrence of publishing study results in similar or consecutive articles, we utilized EndNote software to identify duplicates and mitigate the risk of multiple publications and bias.
Results
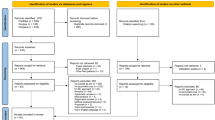
Figure 1 presents the PRISMA flow chart, which provides a concise review process overview. The initial search yielded 7,529 published studies. After removing 569 duplicate records, we screened the titles and abstracts of the remaining 6,624 papers. Based on this screening, 5,624 papers were excluded as they did not meet the inclusion criteria. Subsequently, the full texts of the remaining 369 studies were thoroughly assessed to determine their eligibility for inclusion in the analysis. Among these, 328 studies were deemed ineligible as they did not meet the predetermined criteria. Ultimately, 41 studies were selected for the meta-analysis and meta-synthesis, meeting the quality assessment criteria. Overall, the selected studies demonstrated satisfactory quality.
The included studies had sample sizes ranging from 159 to 13,980,570, as reported in previous research [24, 25]. The mean sample size of (Mean = 549,944.51) refers to the average number of participants across the studies included in our analysis. This value is important as it indicates the generalizability of the findings. Larger sample sizes contribute to more robust and reliable results, allowing for broader applicability of our conclusions.
Standard deviation of (SD = 2,242,858.719), reflects the variability in sample sizes observed across the individual studies. Some studies may have significantly larger or smaller sample sizes compared to the mean, resulting in a wide dispersion of values. This variability influences the heterogeneity of the overall findings and underscores the need to consider the diversity in sample sizes when interpreting the results. The median of sample size, representing the central value, is 13,420. Most of these studies were conducted in the United States and South Korea, with cohort and case-control designs being the most employed study designs. The participants in these studies predominantly represented the general population. The outcome measurement criteria of the data collection process and its results are presented below.
Pooled prevalence of ML outcomes
Additional details of the studies included can be found in Table 1 (after reference section). Note that the statistical analysis revealed that the negative predictive value and the false positive rate did not show a significant difference, with a p-value greater than 0.05. To identify single study influence on the overall meta-analysis, a sensitivity analysis was performed using a random-effects model and the result showed there was no evidence for the effect of single study influence on the overall meta-analysis.
Accuracy
Accuracy refers to the ability of ML models to differentiate between health and patient groups [56] correctly. Out of the 41 final studies, 13 studies reported information on accuracy. The reported accuracy rates varied across the studies as indicated in Panel A of Fig. 2, with the lowest being 0.70 for NN in the study conducted in [30], and the highest being 0.94 for the random forest in the study conducted in [32]. The overall pooled prevalence of accuracy was 0.78 ((\({I}^{2}=56.32\%\); 95% CI: 0.73, 0.84), Table 2.
AUC
The area under the curve (AUC) as a metric used in this study to compare the performance of multiple classifiers [26]. In our analysis, a total of thirty-two studies reported AUC values as indicated in Fig. 3, Panel B. Balbuena et al.’s (2022) study reported the lowest AUC of 0.54, based on the COX and random forest models. On the other hand, Choi et al.’s (2021) reported the highest AUC of 0.97, using the XGBoost classifier. The pooled prevalence of AUC across the studies was estimated to be 0.77 (\({I}^{2}=\) 95.86%; 95% CI: 0.74, 0.80), Table 2.
Precision
Precision is a measure that determines the number of true positives divided by the sum of true positives and false positives [27]. In our analysis, three studies reported precision values as depicted in Fig. 4, Panel C. Two studies reported the highest precision rate of 0.93. The first study, conducted by Choi et al., utilized the XGBoost classifier, and the second study, by Kim et al. (2021), employed a random forest model. On the other hand, the lowest precision rate of 0.86 was documented in the Delgado-Gomez et al. (2016) study, which used a decision tree model. The pooled prevalence of positive predictive value was estimated to be 0.91 (\({I}^{2}=\) 0.001%; 95% CI: 0.85, 0.98), Table 2.
Positive predictive value
Positive predictive value (PPV) represents the proportion of true positive cases among all positive predictions [27]. Among the studies included in our analysis, six studies reported PPV values as depicted in Fig. 5, Panel D. The PPV varied across the studies, ranging from 0.01 in Cho et al.’s study conducted in 2020 and 2021, which utilized a random forest model, to 0.62 in Navarro’s (2021) study, also employing a random forest model. The pooled prevalence of PPV was estimated to be 0.10 (\({I}^{2}=\) 97.02%; 95% CI: 0.03, 0.21), Table 2.
True positive rate
The true positive rate (TPR), also known as sensitivity, represents the proportion of actual positive cases correctly identified by the model [27]. In our analysis, only one study conducted by Ballester et al. (2021), utilized the gradient tree boosting model, reported the TPR as depicted in Fig. 6, Panel E. The pooled prevalence of TPR in this study was estimated to be 0.77 (95% CI: 0.40, 1.34), Table 2.
Sensitivity
Sensitivity, also known as the true positive rate, measures the proportion of actual positive cases correctly identified by the model (specified patient cases) [28]. In our analysis, fifteen studies provided data on sensitivity as illustrated in Fig. 7, Panel F. The sensitivity ranged from 0.43 in Navarro’s (2021) random forest study to 0.87 in Delgado-Gomez et al.’s (2016) decision tree study. The pooled prevalence of sensitivity was estimated to be 0.69 (\({I}^{2}=\) 95.94%; 95% CI: 0.60, 0.78), Table 2.
Specificity
Specificity is a measure that identifies the proportion of actual negative cases correctly identified by the model [28]. In our analysis, fifteen studies reported specificity rates as illustrated in Fig. 8, Panel G. The specificity ranged from 0.63 in Melhem et al.’s (2019) study using logistic regression, to 0.90 in Barak-Corren et al.’s (2017) study using Naive Bayesian classifier. The pooled prevalence of specificity was estimated to be 0.81 (\({I}^{2}= 80.31\%;\)95% CI: 0.77, 0.86), Table 2.
Recall
Recall is a measure that determines the proportion of true positive cases correctly identified by the model [27]. In our analysis, three studies reported recall rates as depicted in Fig. 9, Panel H, ranging from 0.11 in McKernan et al.’s (2019) study using bootstrapped L-1 penalized regression to 0.95 in Kim et al.’s (2021) study using random forest. The pooled prevalence of recall was estimated to be 0.58 (\({I}^{2}= 98.43\%;\)95% CI: 0.15, 1.29), Table 2.
False negative rate
False negative rate represents the proportion of actual negative cases incorrectly identified by the model [29]. Two studies provided data on false negative rates, with rates that were similar to each other as shown in Fig. 10, Panel I. These studies utilized the random forest and binary logistic regression models. The pooled prevalence of the false negative rate was estimated to be 0.26 (\({I}^{2}= 0.001\%;\)95% CI: 0.24, 0.28), Table 2.
Suicide risk factors
In our meta-synthesis analysis, we studied 41 studies in which we identified 261 suicide risk factors. We implemented a rigorous extraction process to identify the most significant risk factors. While some studies presented vast datasets with over 2500 entries of potential risk factors, the focus was on extracting those factors consistently cited as common and important indicators of suicide risk across multiple studies [30, 31]. To ensure robustness, we excluded risk factors reported less than three times, resulting in the compilation of 55 frequently occurring risk factors. We aimed to focus on more prevalent risk factors in the database to enhance the generalizability of the findings to the broader population. Some factors with lower frequencies can introduce noise in the analysis, making it more challenging to identify true patterns. The minimum threshold helped us filter out less relevant factors. This decision was based on a focus group session that included two psychiatrists and one emergency physician. The focus group selected the most common variables that were repeated more than three times based on their scientific knowledge and experience. These factors were categorized into five distinct categories in our study, as outlined in Table 3.
Discussion
This study employed a systematic review, meta-analysis, and meta-synthesis approach to examine the pooled prevalence of ML outcomes for predicting suicide and provide a comprehensive list of suicide risk factors. The intricate nature of suicide as a behavior is underscored by a diverse array of risk factors, spanning clinical variables to lifestyle influences [32]. Our study adopted a comprehensive approach, employing both qualitative and quantitative methods. Additionally, the study was limited to studies with prospective, retrospective, retrospective cohort, case cohort, case-control, cohort, diagnostic/prognostic, longitudinal, longitudinal cohort, longitudinal prospective, prognostic, prospective cohort, retrospective, retrospective cohort, and randomized control trial designs due to the large number of studies in the final stage, and to ensure methodological rigor. Ultimately, 41 studies were selected for the meta-analysis and meta-synthesis, meeting the quality assessment criteria. Results revealed the neural network (NN) algorithm with the lowest accuracy at 0.70, contrasting with the random forest exhibiting the highest accuracy at 0.94. Furthermore, the XGBoost classifier demonstrated the highest Area Under the Curve (AUC) value, reaching an impressive 0.97. These findings not only contribute to our understanding of suicide risk factors but also highlight the significance of methodological considerations and algorithmic performance in predictive models.
The findings of this study are consistent with previous research conducted by [33, 34] which suggested that ML algorithms and the identification of innovative indicators play a valuable role in predicting suicide and detecting mental health issues. However, these findings contradict the results of [35], which indicated insufficient evidence to support the superior performance of ML over logistic regression in clinical prediction models. The studies included in the analysis that used ML techniques to predict suicidal attempts demonstrated overall good performance on the most commonly used algorithms, namely XGBoost. For example, the AUC values reported in these studies were consistently high, ranging approximately between 0.65 and 0.97. An AUC value of 0.5 indicates a random prediction, while a value of 1 represents a perfect prediction. The AUC values in the range of 0.97 for XGBoost model suggest that the ML models had a high degree of accuracy in classifying individuals with respect to their risk of suicidal attempts. The findings of this study are consistent with previous research conducted by [36] which confirmed acceptable performance of XGBoost algorithm in cognition of patients with major depressive disorder. This result may be due to the fact that XGBoost is an ensemble model that constructs various models to reduce classification errors on each iteration. According to [37], certain ML algorithms, such as support vector machines (SVM) and decision trees (DT), are preferred over others due to their superior performance in predicting suicide risk. Furthermore [38], confirmed that the application of ML techniques to analyze large databases holds great potential for facilitating the prediction of suicide, offering promising avenues for future research. The results of this study align with the findings of [39], which highlighted the ability of ML to enhance suicide prediction models by incorporating a larger number of suicide risk factors. Applicability of these methods in specific patient groups is invaluable. For example [40], indicated that predicting whether a person has a mental illness itself poses a significant challenge. Therefore, if machine learning can offer a new avenue of hope for clinicians, it is commendable. However [41], discovered that although these models have demonstrated accuracy in the overall classification, their ability to predict future events remains limited in the context of suicide prediction models.
Consequently, it is important to note that the performance of ML algorithms can vary depending on various factors, including the quality and size of the dataset, the specific features used as input, the preprocessing steps applied, and the hyperparameters selected for the algorithms. Therefore, the overall performance of these algorithms in predicting suicide showed strong discriminatory power in distinguishing between individuals who are at risk of suicidal attempts and those who are not. Future research should continue exploring and refining ML approaches for suicide prediction, considering these factors to improve the accuracy and reliability of predictions.
The findings of our study revealed that various factors, such as age, sex, substance abuse, depression, anxiety, alcohol consumption, marital status, income, education, low-density lipoprotein (LDL) and occupation, were identified as the most prevalent risk factors based on the analysis of included studies. Age plays a complex role in suicide, with several studies indicating a higher incidence of suicide among middle-aged and older adults. However, it is important to note that age is not the sole factor contributing to suicidal behavior [42, 43]. The prevalence of suicide is exceptionally high among young adults, specifically those aged 15 to 19 as it is a fourth cause of death in the world [44]. Sex is a significant risk factor for suicide. In general, men are more likely to die by suicide than women, but women attempt suicide more often than men. This may be because men are more likely to use lethal methods [42, 45, 46].
According to the meta-synthesis results, there appears to be a significant correlation between substance abuse and depression with suicide. This correlation may be because substance abuse can impair judgment and increase impulsivity. On the other hand, a person who is depressed may experience feelings of hopelessness, helplessness, and despair, which can lead to suicidal thoughts or behaviors. These findings align with the study conducted by [47, 48]. Anxiety as a mental health condition can lead to various negative outcomes, including an increased risk of suicide [49]. Alcohol use can increase impulsivity and decrease inhibitions, leading to risky behaviors such as self-harm or suicide attempts [50, 51]. found that the consumption of alcohol while feeling sad or depressed could indicate suicidal behavior in adolescents who had not previously reported having thoughts of suicide before attempting it.
Marital status is a common suicide risk factor. Researchers have found that married individuals have lower suicide rates than their unmarried counterparts. This trend is observed in both men and women across different age groups and cultures [52]. Low income has been associated with an increased risk of suicide. The reasons for this link are complex and multifactorial, but some possible explanations include limited access to healthcare and mental health services, financial strain, and social isolation [53]. Lower education levels are also associated with higher suicide rates. This may be because lower education-level individuals have fewer job opportunities and may experience more financial stress [53]. In addition to the clinical and demographic factors discussed, it is crucial to recognize the significant role that certain biomarkers and laboratory factors play in the vulnerability to suicide. One notable example is the impact of low serum cholesterol levels, which have been found to significantly heighten the risk of suicide [54]. Some studies have shown that LDL level is an important factor in the incidence of suicide [55]. Moreover, some studies have indicated that individuals who have committed suicide had higher levels of LDL compared to non-attempters [56].
Machine learning (ML) techniques are suitable for predicting suicide risk, overcoming the constraints of traditional methods. However, ML requires sufficient and relevant data to train and validate the early identification of risk factors and suicide prediction. We acknowledge the importance of anticipating and addressing immediate concerns related to suicide in a clinical setting. Due to this, some studies have focused on utilizing certain scales in psychiatric outpatients [57]. However, reliance solely on these scales may instill an unwarranted sense of assurance among healthcare providers. Hence, it is crucial to factor in data availability and the computational demands of handling extensive datasets and intricate models. Our evaluation underscores the proficiency of ML algorithms in uncovering concealed relationships and delivering precise predictions of suicide risk, contingent upon the judicious selection and meticulous evaluation of algorithms. This underscores the indispensable role of ML algorithms in exhaustively analyzing data and pinpointing crucial risk factors, thereby advocating for further exploration in the field. This methodological breadth mirrors the multifaceted nature of suicide risk prediction, enhancing the generalizability of our findings. However, our study may be susceptible to limitations arising from the included studies and the meta-analysis methodology. Additionally, reliance on published literature may introduce publication bias, favoring studies with statistically significant results and potentially skewing overall findings. Furthermore, it is suggested to report τ² and the Q-statistic in future studies to assess heterogeneity. Despite these challenges, our study offers valuable insights into the role of machine learning algorithms in predicting suicide risk and sheds light on important risk factors associated with suicidal behavior. Future research endeavors will continue to tackle these methodological hurdles, striving for enhanced standardization and transparency in study reporting to fortify the reliability and reproducibility of findings in this crucial domain of inquiry.
Ethical considerations in the use of ML for suicide prediction
Machine learning (ML) for suicide prediction requires the implementation of ethical considerations as the well-being and rights of individuals and the privacy and confidentiality of individuals’ data are crucial. Participants should be fully informed about the study’s purpose, potential risks, and benefits and have the right to withdraw their consent at any time. Understanding and interpreting the factors and variables that contribute to the predictions is important. This transparency is required to gain the trust of both individuals at risk and healthcare professionals. Ensuring that ML algorithms cannot be replaced by human intervention and clinical judgment is important. Human oversight is critical in interpreting and acting upon the predictions made by the algorithms. Healthcare professionals should make informed decisions based on ML predictions, considering the individual’s unique circumstances and context [58].
Conclusion
Suicide is a complex and multifaceted public health issue with significant implications for individuals and communities. Our study examined the application of ML techniques for predicting suicide risk. Our research findings highlight the diverse performance of ML algorithms in predicting suicide, indicating the need for further investigation and refinement.
Our analysis identified several general risk factors contributing to an individual’s heightened risk of suicide. These factors include age, sex, substance abuse, depression, anxiety, alcohol consumption, marital status, income, education, and occupation. Recognizing that these risk factors interact in complex ways is important, and their presence does not guarantee suicidal behaviour. Nonetheless, understanding and addressing these risk factors can aid in developing targeted prevention and intervention strategies.
While ML algorithms have shown promise in predicting suicide risk, their performance can vary depending on the specific dataset and risk factors being considered. Further studies are warranted to explore using ML algorithms across diverse databases encompassing various risk factors. This would allow for a more comprehensive understanding of the predictive capabilities of ML in different contexts and populations.
Moreover, future research should focus on enhancing the interpretability and explainability of ML models in suicide prediction. Understanding the underlying mechanisms and variables contributing to predictions is essential for effective intervention and decision-making. Additionally, rigorous validation and evaluation of ML algorithms should be conducted to assess their accuracy, generalizability, and potential biases.
To advance the field of suicide prediction using ML, collaboration between researchers, clinicians, and policymakers is crucial. This interdisciplinary approach can foster the development of comprehensive and ethical frameworks for implementing ML algorithms in suicide prevention efforts. Ensuring that ML techniques are used responsibly, prioritizing patient well-being, privacy, and equitable outcomes is imperative.
In conclusion, our study sheds light on the potential of ML algorithms in predicting suicide risk. However, further research is needed to refine and validate these algorithms across different datasets and risk factors. By understanding the complexities of suicide and leveraging the power of ML, we can work towards more effective strategies for suicide prevention and intervention.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Organization WH. Live life: preventing suicide: implementation. World Health Organization; 2022.
Furqatovich UF, Sattorovich EZ. Suicide–as a global problem facing humanity. Web Scientist: Int Sci Res J. 2022;3(02):349–54.
Reddy M. Suicide incidence and epidemiology. New Delhi, India: SAGE Publications Sage India; 2010. pp. 77–82.
Diefenbach GJ, et al. Uncovering the role of substance use in suicide attempts using a mixed-methods approach. Suicide Life-Threatening Behav. 2024;54(1):70–82.
Cao Z, et al. Healthy lifestyle and the risk of depression recurrence requiring hospitalisation and mortality among adults with pre-existing depression: a prospective cohort study. BMJ Mental Health. 2024;27(1):e300915.
Brådvik L. Suicide risk and Mental disorders. Int J Environ Res Public Health. 2018;15(9):2028.
Fonseka TM, Bhat V, Kennedy SH. The utility of artificial intelligence in suicide risk prediction and the management of suicidal behaviors. Aust N Z J Psychiatry. 2019;53(10):954–64.
Pluye P, Cargo RE, Bartlett M, O’Cathain G, Griffiths A. F. A Mixed Methods Appraisal Tool for systematic mixed studies reviews 2011. November 15, 2013]; http://mixedmethodsappraisaltoolpublic.pbworks.com.
Amini P, et al. Evaluating the high risk groups for suicide: a comparison of logistic regression, support vector machine, decision Tree and Artificial neural network. Iran J Public Health. 2016;45(9):1179–87.
Lindesay J. Suicide in the elderly. Int J Geriatr Psychiatry. 1991;6(6):355–61. https://doi.org/10.1002/gps.930060605.
Ormiston CK, et al. Trends in adolescent suicide by Method in the US, 1999–2020. JAMA Netw Open. 2024;7(3):e244427–244427.
Schunk DH, Meece JL. Self-efficacy development in adolescence. Self-efficacy Beliefs Adolescents. 2006;5(1):71–96.
O’Dea D, Tucker S. The cost of suicide to society. Wellington: Ministry of Health; 2005.
Clayton D, Barceló A. The cost of suicide mortality in New Brunswick, 1996. Chronic Dis Injuries Can. 1999;20(2):89.
Kennelly B. The economic cost of suicide in Ireland. Crisis. 2007;28(2):89–94.
Kayikci S, Khoshgoftaar TM. Blockchain meets machine learning: a survey. J Big Data. 2024;11(1):9.
Love BC. Comparing supervised and unsupervised category learning. Psychon Bull Rev. 2002;9(4):829–35.
Mendes-Santos C, et al. Understanding mental health professionals’ perspectives and practices regarding the implementation of digital mental health: qualitative study. Volume 6. JMIR formative research; 2022. p. e32558. 4.
Bucci S, Schwannauer M, Berry N. The digital revolution and its impact on mental health care. Psychol Psychotherapy: Theory Res Pract. 2019;92(2):277–97.
Bucci S, Berry N, Morris R, Berry K, Haddock G, Lewis S, Edge D. They are not hard-to-reach clients. We have just got hard-to-reach services. Staff views of digital health tools in specialist mental health services. Front Psychiatr. 2019;10:344. https://doi.org/10.3389/fpsyt.2019.00344.
Fonseka TM, Bhat V, Kennedy SH. The utility of artificial intelligence in suicide risk prediction and the management of suicidal behaviors. Australian New Z J Psychiatry. 2019;53(10):954–64.
Freeman MF, Tukey JW. Transformations related to the angular and the Square Root. Ann Math Stat. 1950;21(4):607–11.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Bai S, et al. Potential biomarkers for diagnosing major depressive disorder patients with suicidal ideation. J Inflamm Res. 2021;14:495–503.
Coley RY, et al. Racial/Ethnic disparities in the performance of Prediction models for death by suicide after Mental Health visits. JAMA Psychiatry. 2021;78(7):726–34.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36.
Ting KM. Precision and Recall. Encyclopedia of machine learning. Boston, MA: Springer US; 2010. pp. 781–781. C. Sammut and G.I. Webb, Editors.
Baratloo A, Hosseini M, Negida A, El Ashal G. Part 1: simple definition and calculation of accuracy, sensitivity and specificity. Emerg (Tehran). 2015 Spring;3(2):48–9.
Riffenburgh RH. Statistics in medicine. Academic; 2012.
Jiang T, et al. Suicide prediction among men and women with depression: a population-based study. J Psychiatr Res. 2021;142:275–82.
Edgcomb JB, et al. Machine learning to differentiate risk of suicide attempt and self-harm after General Medical hospitalization of Women with Mental Illness. Med Care. 2021;59:S58–64.
de Beurs D, et al. A network perspective on suicidal behavior: understanding suicidality as a complex system. Suicide Life-Threatening Behav. 2021;51(1):115–26.
Burke TA, Ammerman BA, Jacobucci R. The use of machine learning in the study of suicidal and non-suicidal self-injurious thoughts and behaviors: a systematic review. J Affect Disord. 2019;245:869–84.
Chahar R, Dubey AK, Narang SK. A review and meta-analysis of machine intelligence approaches for mental health issues and depression detection. Int J Adv Technol Eng Explor. 2021;8(83):1279.
Christodoulou E, et al. A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. J Clin Epidemiol. 2019;110:12–22.
Zheng S, et al. Can cognition help predict suicide risk in patients with major depressive disorder? A machine learning study. BMC Psychiatry. 2022;22(1):580.
Castillo-Sánchez G, et al. Suicide risk Assessment using machine learning and Social Networks: a scoping review. J Med Syst. 2020;44(12):205.
Bernert RA, Hilberg AM, Melia R, Kim JP, Shah NH, Abnousi F. Artificial intelligence and suicide prevention: A systematic review of machine learning investigations. Int J Environ Res Public Health. 2020;17(16):5929. https://doi.org/10.3390/ijerph17165929.
Corke M, et al. Meta-analysis of the strength of exploratory suicide prediction models; from clinicians to computers. BJPsych Open. 2021;7(1):e26.
Kumar P, Chauhan R, Stephan T, Shankar A, Thakur S. A Machine learning implementation for mental health care. Application: Smart Watch for depression detection. 2021 11th international conference on cloud computing, data science & engineering (Confluence), Noida, India, 2021. p. 568–574. https://doi.org/10.1109/Confluence51648.2021.9377199.
Belsher BE, et al. Prediction models for suicide attempts and deaths: a systematic review and Simulation. JAMA Psychiatry. 2019;76(6):642–51.
Cho S-E, Geem ZW, Na K-S. Development of a suicide prediction model for the Elderly using Health Screening Data. Int J Environ Res Public Health. 2021;18(19):10150.
Edgcomb JB, et al. Predicting suicidal behavior and self-harm after general hospitalization of adults with serious mental illness. J Psychiatr Res. 2021;136:515–21.
Hughes JL, et al. Suicide in young people: screening, risk assessment, and intervention. BMJ. 2023;381:e070630.
Fradera M, et al. Can routine primary Care records help in detecting suicide risk? A Population-based case-control study in Barcelona. Archives Suicide Res. 2022;26(3):1395–409.
Choi SB, et al. Ten-year prediction of suicide death using Cox regression and machine learning in a nationwide retrospective cohort study in South Korea. J Affect Disord. 2018;231:8–14.
Chattopadhyay S, Daneshgar F. A study on suicidal risks in psychiatric adults. Int J BioMed Eng Technol. 2011;5(4):390–408.
Chang HB, et al. The role of substance use, smoking, and inflammation in risk for suicidal behavior. J Affect Disord. 2019;243:33–41.
Sareen J, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: a Population-based longitudinal study of adults. Arch Gen Psychiatry. 2005;62(11):1249–57.
Choi J, Cho S, Ko I, Han S. Identification of risk factors for suicidal ideation and attempt based on machine learning algorithms: A longitudinal survey in Korea (2007-2019). Int J Environ Res Public Health. 2021;18(23):12772. https://doi.org/10.3390/ijerph182312772.
Schilling EA, et al. Adolescent alcohol use, suicidal ideation, and suicide attempts. J Adolesc Health. 2009;44(4):335–41.
Smith JC, Mercy JA, Conn JM. Marital status and the risk of suicide. Am J Public Health. 1988;78(1):78–80.
Berkelmans G, et al. Identifying socio-demographic risk factors for suicide using data on an individual level. BMC Public Health. 2021;21(1):1702.
Troisi A. Cholesterol in coronary heart disease and psychiatric disorders: same or opposite effects on morbidity risk? Neurosci Biobehavioral Reviews. 2009;33(2):125–32.
Loas G, et al. Relationships between Anhedonia, alexithymia, impulsivity, suicidal ideation, recent suicide attempt, C-reactive protein and serum lipid levels among 122 inpatients with mood or anxious disorders. Psychiatry Res. 2016;246:296–302.
Ma YJ, Zhou YJ, Wang DF, Li Y, Wang DM, Liu TQ, Zhang XY. Association of lipid profile and suicide attempts in a large sample of first episode drug-naive patients with major depressive disorder. Front Psychiatr. 2020;11:543632. https://doi.org/10.3389/fpsyt.2020.543632.
Barzilay S, et al. Determinants and predictive value of Clinician Assessment of short-term suicide risk. Suicide Life-Threatening Behav. 2019;49(2):614–26.
Castillo-Sánchez G, Acosta MJ, Garcia-Zapirain B, De la Torre I, Franco-Martín M. Application of machine learning techniques to help in the feature selection related to hospital readmissions of suicidal behavior. Int J Ment Health Addict. 2022;18:1–22. https://doi.org/10.1007/s11469-022-00868-0. Epub ahead of print.
Alexopoulos GS, et al. Modifiable predictors of suicidal ideation during psychotherapy for late-life major depression. A machine learning approach. Translational Psychiatry. 2021;11(1):536.
Balbuena LD, et al. Identifying long-term and imminent suicide predictors in a general population and a clinical sample with machine learning. BMC Psychiatry. 2022;22(1):120.
Ballester PL, et al. 5-year incidence of suicide-risk in youth: a gradient tree boosting and SHAP study. J Affect Disord. 2021;295:1049–56.
Barak-Corren Y, et al. Predicting suicidal behavior from longitudinal electronic health records. Am J Psychiatry. 2017;174(2):154–62.
Bhak Y, et al. Depression and suicide risk prediction models using blood-derived multi-omics data. Translational Psychiatry. 2019;9(1):262.
Cho S-E, Geem ZW, Na K-S. Prediction of suicide among 372,813 individuals under medical check-up. J Psychiatr Res. 2020;131:9–14.
Choi KS, et al. Deep graph neural network-based prediction of acute suicidal ideation in young adults. Sci Rep. 2021;11(1):1–11.
Etter DJ, et al. Suicide screening in primary care: use of an electronic screener to assess suicidality and improve Provider Follow-Up for adolescents. J Adolesc Health. 2018;62(2):191–7.
Ge F, Jiang J, Wang Y, Yuan C, Zhang W. Identifying suicidal ideation among Chinese patients with major depressive disorder: Evidence from a real-world hospital-based study in China. Neuropsychiatr Dis Treat. 2020;16:665–72. https://doi.org/10.2147/NDT.S238286.
Hill RM, Oosterhoff B, Do C. Using machine learning to identify suicide risk: a classification tree approach to prospectively identify adolescent suicide attempters. Archives Suicide Res. 2020;24(2):218–35.
Kim S, Lee H-K, Lee K. Detecting suicidal risk using MMPI-2 based on machine learning algorithm. Sci Rep. 2021;11(1):15310.
Haroz EE, et al. Comparing the predictive value of screening to the use of electronic health record data for detecting future suicidal thoughts and behavior in an urban pediatric emergency department: a preliminary analysis. Volume 51. Suicide and Life-Threatening Behavior; 2021. pp. 1189–202. 6.
Melhem NM, et al. Severity and variability of depression symptoms Predicting suicide attempt in high-risk individuals. JAMA Psychiatry. 2019;76(6):603–13.
Machado CdS, et al. Prediction of suicide attempts in a prospective cohort study with a nationally representative sample of the US population. Psychol Med. 2021;52(14):2985–96.
Miranda O, et al. DeepBiomarker: identifying important lab tests from Electronic Medical Records for the prediction of suicide-related events among PTSD patients. J Personalized Med. 2022;12(4):524.
Zheng L, et al. Development of an early-warning system for high-risk patients for suicide attempt using deep learning and electronic health records. Translational Psychiatry. 2020;10(1):72.
Zhu R, et al. Discriminating suicide attempters and Predicting suicide risk using altered frontolimbic resting-state functional connectivity in patients with bipolar II disorder. Front Psychiatry. 2020;11:597770.
Setoyama D, et al. Plasma metabolites predict severity of depression and suicidal ideation in psychiatric patients-a multicenter pilot analysis. PLoS ONE. 2016;11(12):e0165267.
van Mens K, et al. Predicting future suicidal behaviour in young adults, with different machine learning techniques: a population-based longitudinal study. J Affect Disord. 2020;271:169–77.
Su C, et al. Machine learning for suicide risk prediction in children and adolescents with electronic health records. Translational Psychiatry. 2020;10(1):413.
Forkmann T, et al. Interpersonal theory of suicide: prospective examination. BJPsych Open. 2020;6(5):e113.
Adams RS, et al. Sex-specific risk profiles for suicide among persons with Substance Use disorders in Denmark. Addiction. 2021;116(10):2882–92.
Barak-Corren Y, et al. Validation of an Electronic Health record–based suicide risk prediction modeling Approach across multiple Health Care systems. JAMA Netw Open. 2020;3(3):e201262–201262.
Barros J, et al. Suicide detection in Chile: proposing a predictive model for suicide risk in a clinical sample of patients with mood disorders. Brazilian J Psychiatry. 2016;39:1–11.
Delgado-Gomez D, et al. Computerized adaptive test vs. decision trees: development of a support decision system to identify suicidal behavior. J Affect Disord. 2016;206:204–9.
Delgado-Gomez D, et al. Improving the accuracy of suicide attempter classification. Artif Intell Med. 2011;52(3):165–8.
Delgado-Gomez D, et al. Suicide attempters classification: toward predictive models of suicidal behavior. Neurocomputing. 2012;92:3–8.
DelPozo-Banos M, et al. Using neural networks with routine health records to identify suicide risk: feasibility study. JMIR Mental Health. 2018;5(2):e10144.
Gradus JL, et al. Predicting Sex-specific nonfatal suicide attempt risk using machine learning and data from Danish National registries. Am J Epidemiol. 2021;190(12):2517–27.
Harman G, et al. Prediction of suicidal ideation and attempt in 9 and 10 year-old children using transdiagnostic risk features. PLoS ONE. 2021;16(5):e0252114.
Navarro MC, et al. Machine Learning Assessment of Early Life Factors Predicting Suicide Attempt in adolescence or young adulthood. JAMA Netw Open. 2021;4(3):e211450–211450.
McKernan LC, et al. Outpatient Engagement and predicted risk of suicide attempts in Fibromyalgia. Arthritis Care Res. 2019;71(9):1255–63.
Acknowledgements
The authors would like to thank Mohammad Hossein Mehrolhassani for his collaboration in this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Houriyeh Ehtemam: Conceptualization, Investigation, Methodology, Writing – original draft, Data management, Visualization, Meta-analysis & Meta-synthesis. Shabnam Sadeghi Esfahlani: Writing – review & editing. Alireza Sanaei: Meta-analysis. Mohammad Mehdi Ghaemi: Supervision. Sadrieh Hajesmaeel-Gohari: Writing – review & editing. Rohaneh Rahimisadegh: Writing – review & editing, Validation. Kambiz Bahaadinbeigy: Supervision. Fahimeh Ghasemian: editing. Hassan Shirvani: Review, Editing and Supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ehtemam, H., Sadeghi Esfahlani, S., Sanaei, A. et al. Role of machine learning algorithms in suicide risk prediction: a systematic review-meta analysis of clinical studies. BMC Med Inform Decis Mak 24, 138 (2024). https://doi.org/10.1186/s12911-024-02524-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-024-02524-0