Abstract
Background
Spermacoce princeae (K. Schum) has been used in the treatment of bacterial skin infections in Uganda. Pharmacological studies revealed that extracts of S. princeae exhibited antibacterial, antioxidant, and sun protection potential. This study aimed at isolating and identifying pure compounds from the extracts based on comprehensive analytical characterization by multiple analytical techniques.
Methods
The plant samples were extracted by sequential maceration using n-hexane, ethyl acetate, methanol, and distilled water. The compounds were isolated using a combination of chromatographic techniques and their structures were elucidated by multiple spectroscopic techniques. The antibacterial and antifungal activity determination of the isolated compounds was carried out using an agar well diffusion and potato dextrose assay against Pseudomonas aeruginosa, Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, Candida albicans, and Aspergillus flavus while the antioxidant activity was screened with the 2,2-diphenyl-2-picryl-hydrazyl (DPPH) radical scavenging assay. The sun protection factor was determined using a Shimadzu Ultra Violet-visible (UV–VIS) double beam spectrophotometer between 290 to 320 nm.
Results
Eleven compounds; quercetin (1), kaempferol-3-O-rutinoside (2), rutin (3, 12), myo-inositol (4), asperulosidic acid (5), hexadecanoic acid (6), β-sitosterol (7), stigmasterol (8), campesterol (9), ursolic acid (10), and β-sitosterol glucoside (11) were identified in the S. princeae extracts. Compound 2 had good antifungal activity against C. albicans (zone of inhibition, 23.0 ± 0.1 mm). Compound 10 showed antibacterial and antifungal activity against S. aureus, P. aeruginosa, C. albicans, and A. flavus. Compound 2 had a good percentage radical scavenging effect (IC50 = 64.81 µg/ml) and a good sun protection factor (SPF = 26.83).
Conclusion
This study reports the first-time isolation and identification of compounds 1 to 11 from S. princeae, which contribute to its antimicrobial, antioxidant, and sun protection potential.
Similar content being viewed by others
Introduction
Spermacoce princeae from the genus Spermacoce is an annual flowering herb endemic to tropical Asia, Africa, and East India [1, 2]. Spermacoce is a genus of the family Rubiaceae comprising about 275 species. The plants have fimbriate stipules connected to the petioles, with white flowers at maturity arranged in compact lateral inflorescences [3,4,5]. Species from the genus have been reported to possess medicinal properties. For example; the seeds of Spermacoce hispida in India alleviate liver and kidney damage associated with oxidative stress [6], S. princeae in Kenya and Cameroon has been used to treat bacterial infection [3]. S. princeae is locally known as “Ekaiza nkoju” in the Kiswahili language [7]. In Uganda, the plant is known as either “musanvuma/enkokoma enkazi” in Luganda or “Kisakimu” in the Rutoro dialect [8]. Aqueous extracts from leaves and roots are used for the management and treatment of malaria, cancer, wounds, eye and skin diseases, among others [3, 7, 9]. Water extracts of S. princeae fresh leaves are taken orally by pregnant women to induce labor during childbirth or are applied on skin cuts to treat wounds. In Central and Eastern Uganda, dry leaves are pounded, mixed with oil, and smeared on the skin to treat skin infections [10]. Previous phytochemical screening of S. princeae extracts revealeds the presence of saponins, alkaloids, glycosides, tannins, flavonoids, and terpenoids [1, 2]. Our previous pharmacological study showed that S. princeae extracts (MeOH and water) were active against S. aureus, K. pneumoniae, and P. aeruginosa. The same study revealed that the methanol and aqueous extracts exhibited good antioxidant activity [11]. Some species of the genera Spermacoce have been studied and more than 60 compounds from different compound classes have been isolated. For example; stigmasterol, benzo-isoquinoline, and sitostenone among others have been isolated from S. exilis, S. verticillate, and S. articularis [12, 13]. There is no report on the active compounds from S. princeae (K. Schum) and their isolation. The purpose of this paper is to isolate and determine active compounds from S. princeae extracts and to study their antibacterial, antifungal, antioxidant, and sun protection activities.
Materials and methods
Sample collection and preparation
Plant collection and extraction were carried out as previously reported [11]. After identification and authentication (Mr. Rwaburindore Portase, Makerere University Herbarium, Department of Botany), the leaves of S. princeace were collected along the shores of Ndura water stream, 2 km from the Makerere University Biological field station, Fort portal. The plant sample was collected with the assistance of local leaders and indigenous people after obtaining permission from National Forestry Authority. A Voucher specimen number, 002 in account number 50892, has been deposited at the Makerere University Herbarium, College of Natural Sciences, Department of Plant Science, Microbiology, and Biotechnology for future reference. The samples were air-dried at room temperature for 28 days. The dry samples were then ground into a fine powder. The powders were then sealed in air-tight polythene bags and stored in a cool dry place. The powdered sample (1.0 kg) was extracted sequentially by maceration using n-hexane, ethyl acetate, methanol, and distilled water. The extraction was carried out five times using 3 L of solvent at each time. The extracts were filtered through cotton fabric followed by Whatman No.1 filter paper and concentrated using a rotary evaporator (Buchi, R300) at 40 °C to dryness. The dried extracts were transferred to sample bottles which were placed in a desiccator containing anhydrous sodium sulphate to remove any traces of water. The dried extracts were later put in tightly stoppered sample bottles and stored in a refrigerator. Figure 1 shows the flow chart of the experimental procedures of the study. Sequential extraction allows a set of phytochemicals to be extracted according to polarity, starting with apolar substances, such as essentiaol oils, going to polar compounds such as flavonoids [14].
Isolation and purification of compounds from extracts
The methanol extract (16.2 g) was subjected to column chromatography using a gradient solvent system of n-hexane/ethyl acetate (EtOAc) and EtOAc/methanol (MeOH) affording 12 fractions (M1-12), after monitoring separation using analytical thin layer chromatography (TLC) on aluminum plates precoated with silica gel. The TLC plates were used to develop the solvent system used in the purification of the compounds [15,16,17]. Fraction M3 (0.313 g) was subjected to column chromatography using a gradient solvent system of n-hexane/EtOAc (from 7:3 to 1:1, v/v), and EtOAc/MeOH (95:5, v/v) to obtain 16 sub-fractions (C1-16). Sub-fraction C16 was purified on Sephadex LH-20 with CHCl3/MeOH (1:1, v/v) to obtain compound 1 (12 mg). Fraction M9 (1.693 g) was subjected to column chromatography on silica gel with n-hexane/EtOAc to obtain 13 subfractions (P1-13). Sub-fraction P8 was purified on silica gel using n-hexane/EtOAc (75:25, v/v) to obtain compound 2 (14.2 mg). Fraction M10 (5.398 g) was subjected to column chromatography using a gradient solvent system of EtOAc/MeOH to yield 9 subfractions (J1-9). Subfraction J4 was purified on a silica gel column using EtOAc/tert butanol/H2O (65:25:9, v/v/v) to obtain compound 3 (15 mg) [18]. Compound 4 (5 mg) which crystallized out of subfraction J7, was filtered off, and washed with pure MeOH. Fraction M11 (2.921 g) was purified on silica gel with EtOAc/MeOH/H2O (20:3:2, v/v/v) to obtain 14 subfractions (N1-14). Subfraction N7 was subjected to repeated column chromatography with EtOAc/MeOH/H2O (20: 3: 2 v/v/v) to yield compound 5 (5 mg) [19].
The EtOAc extract (20.253 g) was subjected to silica gel column chromatography with n-hexane/EtOAc and EtOAc/MeOH affording 21 fractions (E1-21) [20, 21]. Fraction E5 was subjected to repeated column chromatography on silica gel with n-hexane/CH2Cl2 (1:1, v/v) to obtain compound 6 (15.1 mg) and fraction E6 (0.343 g) with n-hexane/CH2Cl2 (4:1, v/v) to obtain 24 subfractions (E6(1–24)). Subfraction E-6–3 precipitated needle-like crystals, which were washed with pure hexane to obtain a mixture of compounds 7, 8, and 9 (10.0 mg). Fraction E13 (1.021 g) was washed with pure EtOAc followed by pure MeOH. The MeOH filtrate (E13m) was subjected to silica gel column chromatography using acetonitrile (MeCN) to obtain compound 10 (23 mg). Fraction E18 (0.803 g) was subjected to repeated column chromatography on silica gel using n-hexane/EtOAc (100:30, v/v) to obtain compound 11 (5.7 mg).
The aqueous extract (76 g) was partitioned in CH2Cl2/H2O (1:1, v/v) in a separating funnel [18, 22]. The mixture was shaken for 10 min and left for phase separation. The organic layer was collected and evaporated on a rotary evaporator at 40 0C up to dryness. The organic extract (70.5 mg) was subjected to silica gel column chromatography using n-hexane/EtOAc (1:1, v/v) affording 6 subfractions (AO1-6). Subfraction AO6 (10 mg) was purified using preparative TLC with a solvent system of EtOAc/tert-butanol/H2O/acetic acid (20:3:1:1, v/v/v/v) to obtain compound 12 (4.9 mg).
Spectroscopic analysis of the isolated compounds
The Fourier transform infrared (FT-IR) and UV/VIS spectra of isolated compounds were recorded on a PerkinElmer FT-IR and double-beam UV/VIS Frontier spectrophotometer respectively [23]. All nuclear magnetic resonance (NMR) spectra were recorded on a Bruker Avance II 400 MHz instrument (resonance frequencies 400.13 MHz for 1H and 100.61 MHz for 13C) equipped with a 5 mm N2-cooled broadband cryo-probe-head (Prodigy) with z–gradients at room temperature with standard Bruker pulse programs. The samples were dissolved in 0.6 ml of either CDCl3, DMSO-d6, MeO-d4, or D2O (all Eurisotop, Saint-Aubin, France). Chemical shifts are given in ppm, referenced to residual solvent signals (CDCl3: δH/δC 7.26 / 77.0 ppm, DMSO-d6: δH/δC 2.49 / 39.6 ppm, MeO-d4: δH/δC 3.31 / 49.0 ppm) or in the case of D2O by addition of one drop of acetone δH/δC 2.22 / 30.9 ppm) [24]. Ultra-Performance Convergence Chromatography Quadrupole Time-of-Flight Mass Spectrometry (UPC2-QTof-MS) was used to support the structural assignment of the compounds [25, 26]. The structures of the compounds were identified by interpretation of their spectral data and by comparison with those reported in the literature.
GC–MS/FID analysis
Gas Chromatography (Agilent Technologies 5975C) coupled to mass spectrometry (MSD inert XL TAD) and a flame ionization detector (FID) were used to analyze subfraction E-6–3 from which the MS of compounds 7, 8, and 9 were recorded. The MS detector was operated in the electron-impact (EI) mode at 70 eV using a temperature of 280 °C. The mass scanning range was set to 29–1050 amu (atomic mass unit), and the solvent cutting time was 4 min. The FID was operated at 400 °C, with H2 flow of 30 mL/ min, air flow of 400 mL/ min, and makeup flow (combined) of 25 mL/ min. The GC device was fitted with a UltiMetal VF-5ht capillary column (30 m × 250 µm × 0.10 µm, Agilent J&W). The column temperature program was set as follows: initial T = 65 °C isothermal for 5 min, ramp to 380 °C (rate, 10 °C/ min), and maintain at 380 °C for 8 min. Helium was used as a carrier gas, with a gas flow of 2.5 mL/ min. Injection (1.0 μL) was performed by an autosampler in a cold multimode inlet (MMI), which was kept at 65 °C for 6 s, increased to 380 °C at 500 °C/ min, and then held for 5 min (cold split injection). The split ratio was set to 15:1 (split flow, 37.5 mL/ min). The total analysis time was 44.50 min. Compounds were analyzed with GC as their trimethylsilyl derivatives. 200 μL of silylating agent composed of 9:1, v/v of N,N-bis(trimethylsilyl)-trifluoroacetamide (BSTFA, ≥ 99%, Sigma-Aldrich) and trimethylchlorosilane (TMCS, ≥ 99%, Sigma-Aldrich) respectively were added to each vial, which contained 5 mg of homogenized sample [27,28,29,30]. Five drops of hydrous pyridine (99.8%, Sigma-Aldrich) were also added to each vial before the vortex. All spectra were analyzed with Enhanced ChemStation (MSD ChemStation F.01.01.2317), deconvoluted, and then evaluated using the Mass Hunter Workstation software. The compounds were identified by comparison with Wiley10 and the National Institute of Standard and Technology (NIST17) mass spectral library.
Spectroscopic data of the isolated compounds
Quercetin (1) [31, 32]: yellow powder: FT-IR: 3214, 2924, 1652, 1598, 1504, 1441, 1366, 1259, 1163, 1089 and 1008 cm−1: UV λmax MeOH (nm); 255 and 370: 1H-NMR (400 MHz, CD3OD), δH 7.73 (H-2’, d, J = 2.1 Hz, 1H), 7.63 (H-6’, dd, J = 2.1, 8.5 Hz, 1H), 6.88 (H-5’, d, J = 8.5 Hz, 1H), 6.39 (H-8, d, J = 2.0 Hz, 1H) and 6.18, (H-6, d, J = 2.0 Hz, 1H); 13C-NMR (100 MHz, CD3OD): δC 177.4 (C-4), 165.7 (C-7), 162.6 (C-5), 158.3 (C-9), 148.8 (C-4’), 148.1 (C-2), 146.3 (C-3’), 137.2 (C-3), 124.3 (C-1’), 121.7 (C-6’), 116.3 (C-5’), 115.9 (C-2’), 104.5 (C-10), 99.2 (C-6) and 94.3 (C-8): UPC2-QTof-MS (positive mode) m/z 341.0058 [M + K]+, C15H10O7.
Kaempferol-3-O-rutinoside (2) [33, 34]: yellow powder: FT-IR: 3285, 2916, 1652, 1598, 1498, 1359, 1179 and 1065 cm−1: UV λmax MeOH (nm); 266 and 349: 1H-NMR (400 MHz, CD3OD), δH 8.07 (H-2’/6’, d, J = 8.9 Hz, 2H), 6.89 (H-3’/5’, d, J = 8.9 Hz, 2H), 6.42 (H-8, d, J = 2.0 Hz, 1H), 6.21 (H-6, d, J = 2.0 Hz, 1H), 5.12 (H-1’’, d, J = 7.6 Hz, 1H), 4.51 (H-1’’’, d, J = 1.5 Hz, 1H), 3.81 (H-6 ‘‘a, d, J = 10.5 Hz, 1H), 3.63 (H-2 ‘‘‘, dd, J = 3.3, 1.5 Hz, 1H), 3.52 (H-3 ‘‘‘, dd, J = 9.4, 3.3 Hz, 1H), 3.45 (H-5 ‘‘‘, m, 1H), 3.44 (H-2 ‘‘, m, 1H), 3.41 (H-3 ‘‘, m, 1H), 3.37 (H-6 ‘‘b, m, 1H), 3.33 (H-5 ‘‘, m, 1H), 3.28 (H-4 ‘‘‘, m, 1H), 3.25 (H-4 ‘‘, m, 1H), and 1.12 (H-6 ‘‘‘, d, J = 6.2 Hz, 3H); 13C-NMR (100 MHz, CD3OD), δC 179.4 (C-4), 166.2 (C-7), 163.1 (C-5), 161.5 (C-4’),159.6 (C-2), 158.5 (C-9), 135.6 (C-3), 132.4 (C-2’/6 ‘) 122.7 (C-1’), 116.2 (C-3’/5 ‘), 105.6 (C-10), 104.7 (C-1’’), 102.4 (C-1’’’), 100.1 (C-6), 95.0 (C-8), 78.1 (C-3’’), 77.2 (C-5’’), 75.7 (C-2’’), 74.0 (C-4’’’), 72.4 (C-3’’’), 72.2 (C-2’’’), 71.4 (C-4’’), 69.7 (C-5’’’), 68.5 (C-6’’), 18.0 (C-6’’’): UPC2-QTof-MS (negative mode) m/z 593.1529 [M-H]−, C27H30O15.
Rutin (3, 12) [35, 36]: yellow powder: FT-IR; 3332, 2941, 2537, 1646, 1593, 1497, 1452, 1356, 1284, 1202, 1059, 999, 965 and 941 cm−1: UV λmax (nm); 257 and 358 nm: 1H-NMR (400 MHz, CD3OD), δH 7.66 (H-2’, d, J = 2.1 Hz, 1H), 7.63 (H-6’, dd, J = 8.4, 2.1 Hz, 1H), 6.87 (H-5’, d, J = 8.4 Hz, 1H), 6.40 (H-8, d, J = 2.0 Hz, 1H), 6.21 (H-6, d, J = 2.0 Hz, 1H), 5.11 (H-1’’, d, J = 7.6 Hz, 1H), 4.52 (H-1’’’, d, J = 1.5 Hz, 1H), 3.81 (H-6 ‘‘a, dd, J = 10.9, 1.2 Hz, 1H), 3.63 (H-2 ‘‘‘, dd, J = 3.4, 1.7 Hz, 1H), 3.53 (H-3 ‘‘‘, dd, J = 9.5, 3.4 Hz, 1H), 3.46 (H-2 ‘‘, m, 1H), 3.45 (H-5 ‘‘‘, m, 1H), 3.41 (H-3 ‘‘, m, 1H), 3.39 (H-6 ‘‘b, m, 1H), 3.32 (H-5 ‘‘, m, 1H), 3.28 (H-4 ‘‘‘, m, 1H), 3.26 (H-4 ‘‘, m, 1H), 1.12 (H-6 ‘‘‘, d, J = 6.2 Hz, 3H). 13C-NMR (100 MHz, CD3OD); δC 179.4 (C-4), 166.1 (C-7), 163.0 (C-5), 159.3 (C-2), 158.5 (C-9), 149.8 (C-4’), 145.8 (C-3’), 135.6 (C-3), 123.5 (C-6’), 123.1 (C-1’), 117.7 (C-2’), 116.1 (C-5’), 105.6 (C-10), 104.7 (C-1’’), 102.4 (C-1’’’), 99.9 (C-6), 94.8 (C-8), 78.3 (C-3’’), 77.2 (C-5’’), 75.7 (C-2’’), 73.9 (C-4’’’), 72.2 (C-3’’’), 72.1 (C-2’’’), 71.4 (C-4’’), 69.6 (C-5’’’), 68.5 (C-6’’), 17.9 (C-6’’’): UPC2-QTof-MS (positive mode) m/z 633.1426 [M + Na]+, C27H30O16.
Myo-inositol (4) [37]: white crystalline solid: FT-IR: 3304, 1634, 1408 and 1050 cm−1: 1H-NMR (400 MHz, D2O), δH 4.04 (H-4, t, J = 2.8 Hz 1H), 3.61 (H-2/6, dd, J = 10.0, 9.4 Hz, 2H), 3.52 (H-3/5, dd, J = 10.0, 2.8 Hz, 2H), 3.26 (H-1, t, J = 9.4 Hz, 1H); 13C-NMR (100 MHz, CD3OD): δC 75.0 (C-1), 73.0 (C-2,6), 72.8 (C-4), 71.8 (C-3,5): UPC2-QTof-MS (positive mode) m/z 203.0526 [M + Na]+, C6H12O6.
Asperulosidic acid (5) [38]: white solid: FT-IR: 3339, 2902, 1578, 1410, 1250, 1075, 1029 and 931 cm−1: UV λmax MeOH (nm); 252: 1H-NMR (400 MHz, CD3OD), 7.42 (H-3, s, 1H), 5.98 (H-7, s, 1H), 4.97 (H-1, d, J = 8.8 Hz, 1H), 4.94 (H-10a, d, J = 15 Hz, 1H), 4.89 (H-6, m, 1H), 4.81 (H-10b, d, J = 15 Hz, 1H), 4.71 (H-1’, d, J = 7.8 Hz, 1H), 3.84 (H-6’a, dd, J = 12.3, 1.6 Hz, 2H), 3.62 (H-6’b, dd, J = 12.3, 6.0 Hz, 1H), 3.38 (H-3’, m, 1H), 3.26 (H-4’,H-5’ m, 2H), 3.23 (H-2’, dd, J = 9.1, 7.8 Hz, 1H), 3.05 (H-5, br.t, J = 3.1, 1H), 2.59 (H-9, pseudo-t, J = 8.2 Hz, 1H), 2.09 (H-12, s, 3H); 13C-NMR (100 MHz, CD3OD): δC 172.6 (C-11), 170.2 (C-13), 151.6 (C-3), 146.2 (C-8), 131.8 (C-7), 113.7 (C-4), 100.7 (C-1), 100.4 (C-1 ‘), 78.6 (C-5’), 78.0 (C-3’), 76.0 (C-6), 75.1 (C-2’), 71.8 (C-3’), 64.1 (C-10), 63.1 (C-6’), 47.0 (C-9), 43.7 (C-5), 20.9 (C-12). UPC2-QTof-MS (negative mode) m/z 431.1186 [M-H]−, C18H24O12.
Hexadecanoic acid (6) [39]: oily liquid: FTIR: 3380, 2955, 2915, 2848, 1698, 1464, 1464, 1292 and 940 cm−1: 1H NMR (400 MHz, CDCl3), δH 2.34 (H-2, t, 2H), 1.62 (H-3, p, 2H), 1.28 (H-15, m, 2H), 1.25 (H-4,5,6,7,8,9,10,11,12, m, 2H) and 0.88 (3H, t, H-16); 13C NMR (100 MHz, CDCl3): δC 180.0 (C-1), 34.2 (C-2), 32.2 (C-14), 29.9 (C-10–13), 29.8 (C-5/6), 29.6 (C-4), 29.5 (C-8), 29.4 (C-9), 29.2 (C-7), 24.9 (C-3), 22.9 (C-15), and 14.3 (C-16): UPC2-QTof-MS (negative mode) m/z 255.2329 [M-H]−; C16H32O2.
β-Sitosterol (7) [21, 40]: white needle-like crystals: FT-IR: 3329, 2933, 2866, 1689, 1456, 1374, 1192, 1052, 960 and 838 cm−1: 1H-NMR (400 MHz, CDCl3), δH 5.35 (H-6, m, 1H), 3.52 (H-3, m, 1H), 2.30 (H-4a, ddd, J = 13.1, 5.1, 1.9 Hz), 2.25 (H-4b, dm, J = 13.1 Hz), 2.01 (H-12a, m, 1H), 1.98 (H-7a, m, 1H), 1.85 (H-1a, m, 1H), 1.84 (H-2a, H-16a, m, 2H), 1.67 (H-25, m, 1H), 1.58 (H-15a, m, 1H,), 1.54 (H-7b, m, 1H), 1.51 (H-2b, m, 1H), 1.50 (H-11a, m, 1H), 1.46 (H-11b, m, 1H), 1.45 (H-8, m, 1H), 1.36 (H-20, m, 1H), 1.33 (H-22a, m, 1H), 1.27 (H-16b, m, 1H), 1.25 (H-241, m 2H,), 1.17 (H-23, m, 1H), 1.16 (H-12b, m, 1H), 1.12 (H-17, m, 1H), 1.08 (H-1b, m, 1H), 1.07 (H-15b, m, 1H), 1.02 (H-22b, m, 1H), 1.01 (H-19, s, 3H), 1.00 (H-14, m, 1H), 0.93 (H-9, H-24, m, 2H), 0.92 (H-21, d, J = 6.7 Hz, 3H), 0.85 (H-242, t, J = 7.4 Hz, 3H), 0.84 (H-27, d, J = 7.5 Hz, 3H), 0.82 (H-26, d, J = 6.9 Hz, 3H), 0.68 (H-18, s, 3H);
13C-NMR (CDCl3) 140.8 (C-5), 121.7 (C-6), 71.8 (C-3), 56.8 (C-14), 56.1 (C-17), 50.2 (C-9), 45.9 (C-24), 42.3 (C-4, C-13), 39.8 (C-12), 37.3 (C-1), 36.5 (C-10), 36.2 (C-20), 34.0 (C-22), 31.93 (C-8), 31.91 (C-7), 31.7 (C-2), 29.2 (C-25), 28.2 (C-16), 26.1 (C-23), 24.3 (C-15), 23.1 (C-241), 21.1 (C-11), 19.8 (C-27), 19.4 (C-19), 19.0 (C-26), 18.3 (C-21), 12.0 (C-242), 11.9 (C-18): GC–MS molecular mass 413 \({[\mathrm{M}]}^{+.}\),calculated for C29H49O.
Stigmasterol (8) [41]: white needle-like crystals: FT-IR (see FT-IR of compound 7): 1H-NMR (400 MHz, CDCl3), δH 5.35 (H-6, m, 1H), 5.16 (H-22, dd, J = 15.2, 8.5 Hz, 1H), 5.02 (H-23, dd, J = 15.2, 8.5 Hz, 1H), 3.52 (H-3, m, 1H), 2.30 (H-4a, ddd, J = 13.1, 5.1, 1.9 Hz), 2.25 (H-4b, dm, J = 13.1 Hz), 2.05 (H-20, m, 1H), 2.01 (H-12a, m, 1H), 1.98 (H-7a, m, 1H), 1.85 (H-1a, m, 1H), 1.84 (H-2a, H-16a, m, 2H), 1.67 (H-25, m, 1H), 1.58 (H-15a, m, 1H), 1.54 (H-7b, H-24, m, 2H), 1.51 (H-2b, m, 1H), 1.50 (H-11a, m, 1H), 1.46 (H-11b, m, 1H), 1.45 (H-8, m, 1H), 1.27 (H-16b, m, 1H), 1.25 (H-241, m 2H,), 1.16 (H-12b, m, 1H), 1.12 (H-17, m, 1H), 1.08 (H-1b, m, 1H), 1.07 (H-15b, m, 1H), 1.02 (H-21, d, J = 6.5 Hz, 3H), 1.01 (H-19, s, 3H), 1.00 (H-14, m, 1H), 0.93 (H-9, H-24, m, 2H), 0.85 (H-242, t, J = 7.4 Hz, 3H), 0.84 (H-27, d, J = 7.5 Hz, 3H), 0.82 (H-26, d, J = 6.9 Hz, 3H), 0.68 (H-18, s, 3H);
13C-NMR (CDCl3) 140.8 (C-5), 138.3 (C-22), 129.3 (C-23), 121.7 (C-6), 71.8 (C-3), 56.8 (C-14), 56.1 (C-17), 51.2 (C-24), 50.2 (C-9), 42.3 (C-4, C-13), 40.5 (C-20), 39.8 (C-12), 37.3 (C-1), 36.5 (C-10), 31.93 (C-8), 31.91 (C-7), 31.7 (C-2), 29.2 (C-25), 28.2 (C-16), 24.3 (C-15), 23.1 (C-241), 21.1 (C-11), 21.2 (C-21), 19.8 (C-27), 19.4 (C-19), 19.0 (C-26), 12.0 (C-242), 11.9 (C-18); GC–MS molecular mass 411 \({[\mathrm{M}]}^{+.}\), calculated for C29H47O.
Campesterol (9): white need-like crystals: FT-IR (see FT-IR of compound 7): RT, 27.2 min: GC–MS molecular mass 399 \({[\mathrm{M}]}^{+.}\), calculated for C28H47O.
Ursolic acid (10) [42, 43]: white solids: FT-IR: 3379, 2919, 1687, 1454, 1372, 1162, 1035 and 800 cm−1: 1H -NMR (400 MHz, DMSO-d6), δH 5.10 (br.t, J = 3.3, H-12), 2.98 (dd, J = 10.2, 5.6, H-3), 2.10 (d, J = 11.3, H-18), 1.90 (m, H-16a), 1.83 (m, H-11a + b), 1.82 (m, H-15a), 1.52 (m, H-22a + b), 1.51 (m, H-1a, H-16b), 1.46 (m, H-6a), 1.44 (m, H2a + b, H-9), 1.42 (m, H-7a, H-21a), 1.29 (m, H-6b, H-19), 1.26 (m, H-21b), 1.25 (m, H-7b), 1.02 (s, H-27), 0.97 (m, H-15b), 0.92 (m, H-20), 0.90 (m, H-1b), 0.89 (d, J = 6.6, H-29), 0.88 (s, H-23), 0.85 (s, H-25), 0.80 (d, J = 6.4, H-30), 0.74 (s, H-26), 0–66 (m, H-5), 0.66 (s, H-24); 13C -NMR (100 MHz, DMSO-d6), δc 178.4 (C-28), 138.3 (C-13), 124.4 (C-12), 76.8 (C-3), 54.8 (C-5), 52.4 (C-18), 47.0 (C- 9), 46.8 (C-17), 41.8 (C-14), 39.2 (C-8), 38.62 (C-20), 38.56 (C-19), 38.5 (C-4), 38.2 (C-1), 36.6 (C-22), 36.5 (C-10), 32.7 (C-7), 30.2 (C-21), 28.2 (C-23), 27.5 (C-15), 27.0 (C-2), 23.8 (C-16), 23.2 (C-27), 22.8 (C-11), 21.1 (C-29), 18.0 (C-6), 17.14 (C-30), 17.06 (C-26), 16.0 (C-24), 15.2 (C-25); UPC2-QTof-MS m/z 455.3518 [M-H]+, C30H48O3.
β-Sitosterol glucoside (11) [20, 44]: white solids: FT-IR: 3380, 2935, 2868, 1454, 1372, 1254, 1162, 1035, 925 and 799 cm−1: 1H -NMR (400 MHz, DMSO-d6), δH 5.31 (m, H-6), 4.89 (d, J = 4.8, 3’-OH), 4.87 (d, J = 4.8, 2’-OH), 4.86 (d, J = 4.7, 4’-OH), 4.43 (t, J = 6.0, 6’-OH), 4.20 (d, J = 7.7, H-1’), 3.63 (dd, J = 11.7, 5.5, H-6’a), 3.39 (m, H-6’b), 3.45 (m, H-3), 3.10 (m, H-3’), 3.08 (m, H-5’), 3.00 (m, H-4’), 2.88 (ddd, J = 8.6, 7.7, 4.8, H-2’), 2.35 (br.dd, J = 13.6, 3.4, H-4a), 2.11 (pseudo-t, J = 13.6, H-4b), 1.95 (m, H-12a), 1.91 (m, H-7a), 1.80 (m, H-2a), 1.78 (m, H-1a, H-16a), 1.62 (m, H-25), 1.53 (m, H-15a), 1.49 (m, H-7b), 1.47 (m, H-2b), 1.46 (m, H-11a), 1.39 (m, H-11b), 1.38 (m, H-8), 1.32 (m, H-20), 1.29 (m, H-22a), 1.22 (m, H-16b, H-28a + b), 1.13 (m, H-12b, H-23a + b), 1.09 (m, H-17), 1.03 (m, H-15b), 0.99 (m, H-22b), 0.97 (m, H-1b, H-14), 0.94 (s, H-19), 0.90 (m, H-9, H-24), 0.89 (d, J = 6.6, H-21), 0.81 (t, J = 7.1, H-29), 0.80 (d, J = 6.7, H-27), 0.78 (d, J = 6.7, H-26), 0.64 (s, H-18); 13C -NMR (100 MHz, DMSO-d6), δc 140.4 (C-5), 121.2 (C-6), 100.9 (C-1’), 77.0 (C-3), 76.9 (C-3’, C-5’), 73.6 (C-2′9, 70.2 (C-4’), 61.2 (C-6’), 56.2 (C-14), 55.4 (C-17), 49.6 (C- 9), 45.1 (C-24), 41.8 (C-13), 39.3 (C-12), 38.3 (C-4), 36.8 (C-1), 36.2 (C-10), 35.5 (C-20), 33.3 (C-22), 31.53 (C-8), 31.48 (C-7), 29.3 (C-2), 28.7 (C-25), 27.8 (C-16), 25.4 (C-23), 23.9 (C-15), 22.6 (C-28), 20.6 (C-11), 19.7 (C-27), 19.1 (C-19), 18.9 (C-26), 18.6 (C-21), 11.8 (C-29), 11.7 (C-18).
Antibacterial and antifungal screening of the isolated compounds
The antibacterial activity of the isolated compounds was investigated according to the agar well diffusion method [45, 46]. Muller-Hinton agar was used for bacterial growth. The inoculum was a culture of each bacterial species in 10 ml of Muller Hinton agar diluted in the same medium to a final concentration of 1 × 103 CFU/ml (0.5 NTU – McFarland scale). Wells were made using a 6 mm diameter of sterile cork borer. For antibacterial screening, the tested compound (10 mg/ml), ciprofloxacin (100 μl), and DMSO as negative control were added to each well separately. The plates were incubated at 37 °C for 24 h. Antifungal tests were carried out using 100 µl of suspension containing a culture of fungi on potato dextrose agar (PDA) incubated at room temperature for 72 h. The antimicrobial activity of the compounds was determined by measuring the diameter of the clear zone around the well. Three replicates were carried out for each experiment [47].
Antioxidant activity of the isolated compounds
The antioxidant activity of the isolated compounds was determined by a 2,2-diphenyl-1-picryl-hydrazyl (DPPH) assay [48]. A 0.5 mM DPPH solution was prepared by dissolving 19.7 mg of DPPH in 100 ml of distilled methanol and kept in the dark for 45 min at room temperature. Methanoic solution of the isolated compounds and of ascorbic acid as a standard were prepared (2.0 mg/ml each) and diluted to lower concentrations (1000, 500, 250, 125, 62.5 µg/ml). The prepared solutions and DPPH (2000 µl each) were mixed in a cuvette and kept in the dark for 15 min to stabilize. The absorbance of the mixture was measured at 517 nm on a Shimadzu UV–VIS double-beam spectrophotometer against a blank. The concentration of the compound (antioxidant) required to decrease the initial DPPH concentration by 50% (IC50) was calculated using Logit regression analysis. A lower IC50 value corresponded to a larger scavenging power. All experiments were performed in triplicate and values were expressed as mean ± standard deviation (SD).
Sun protection potential of the isolated compounds
The sun protection factor was determined according to a modified method reported by Dutra et al. (2004). The compounds were dissolved in methanol without ultra-sonication to a concentration 2 mg/ml. The absorption data of each sample was measured on a JENWAY UV–VIS single beam spectrophotometer between 290 to 320 nm every 5 nm, and methanol as a blank. Para amino-benzoic acid was used as a standard sunscreen. Four measurements were averaged and the sun protection factor was determined using the Mansur equation [49].
Data analysis
All data were analyzed using descriptive statistics as implemented by Microsoft Excel. The results were generally expressed as mean ± standard deviation (SD).
Results
Eleven bioactive compounds were isolated from the extracts (Fig. 2), namely; quercetin (1), kaempferol-3-O-rutinoside (2), rutin (3), myo-inositol (4), asperulosidic acid (5), hexadecanoic acid (6), β-sitosterol (7), stigmasterol (8), campesterol (9), ursolic acid (10), and β-sitosterol glucoside (11). All compounds were comprehensively analytically characterized and the data compared to literature values. Compounds 1, 2, 3, 4, and 5 were isolated from the methanolic extract. Compounds 6, 7, 8, 9, 10, and 11 from the ethyl acetate extract and compound 12 from the aqueous extract. Figure 2 shows the flow chart of the isolation and bioactivity of the identified compounds. Some of these compounds have been reported previously to occur in plants of the same genus, such as S. verticillate, S. articularis, S. exilis, and S. hispida [6, 12, 13].
GC–MS analysis of subfraction E-6–3 led to the identification of compound 9, campesterol. The GC–MS data were compared with Wiley10 and the National Institute of Standards and Technology (NIST17) mass spectral libraries. The GC–MS spectrum of subfraction E-6–3 showed three peaks at RT (min); 27.21, 27.45, and 27.86 (Fig. 3). Analysis of the peak signals showed a molecular ion at; m/z 472 for campesterol (9) at 27.20 min, m/z 484 for stigmasterol (8) at 27.45 min, and m/z 486 for β-sitosterol (7). Characteristic fragment ions at m/z 382 for campesterol were observed (Fig. 4) while fragment ions at m/z 394 and 396, typical of stigmasterol and β-sitosterol respectively, were linked to the peaks at 27.45 and 27.86 min. All the peaks showed a molecular ion peak at m/z 129 which is a characteristic fragment of this phytosterol group [50].
Antibacterial and antifungal activity of the isolated compounds
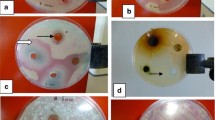
The antibacterial and antifungal activity of isolated compounds 2, 3, 7, 8, 9, 10, and 11 were examined against bacterial (S. aureus, E. coli, K. pneumoniae, and P. aeruginosa) and fungal (C. albicans and A. flavus) strains as shown in Fig. 5. Compound 10 showed activity against S. aureus (20.0 ± 0.1 mm), P. aeruginosa (18.0 ± 0.1 mm), C. albicans (12.0 ± 0.1 mm), and A. flavus (20.5 ± 0.3 mm). Compound 2 showed activity against C. albicans (23.0 ± 0.1 mm). The data indicated that compound 10 displayed a wide degree of antibacterial and antifungal activity on the different tested micro-organisms. The other tested compounds did not show any activity against the tested bacterial and fungal strains. The quantity of compounds 1, 4, 5, and 6 was only sufficient for spectroscopic analysis, but not for bioactivity testing.
Antioxidant activity of the isolated compounds by DPPH (free radical scavenging) activity
Compounds 2 and 3 showed a good radical scavenging activity of 83.87 and 58.58% respectively. Compound 2 showed the highest radical scavenging activity among the extracted compounds tested (IC50 = 64.81 µg/ml). Ascorbic acid (IC50 = 2.59 × 10–16 µg/ml) was used as a positive control to determine the effectiveness of the extract in scavenging the free radicals. Compounds 7, 8, 9, 10, and 11 were only used for antimicrobial analysis.
Sun protection potential of isolated compounds 2, 3, and 7—11
The sun protection potential of the isolated compounds is as shown in Fig. 6. Para-aminobenzoic acid (standard) was used to determine the effectiveness of the extract in protecting the skin against UV light. Compounds 2 (26.83 ± 0.27) and 3 (24.92 ± 0.31) showed a good ability to protect the skin against ultraviolet (UV) light.
Discussion
Phytochemical analysis of the MeOH extract of S. princeae yielded three flavonoids (1–3), a monoterpene (4), an iridoid (5) characteristic of the family Rubiaceae [51], and an essential oil (6). Flavonoids (2, 3) were the phytochemicals identified also in the aqueous extract. Triterpenoids (7–11) were the major phytochemicals in the EtOAc extract [1]. Figure 7 shows the chemical structures of the isolated compounds. This is the first report of the isolated active compounds from the aerial parts S. princeae. From Fig. 5, compounds 2 and 10 showed potential as antibacterial and antifungal agents. This agrees with a previous report, in which compound (10) from Sambucus australis has been reported to exhibit antibacterial activity against S. aureus, and P. aeruginosa [22, 43]. According to Namukobe et al. (2021), the EtOAc extract of S. princeae did not have any antibacterial potential. In this study, it was noticed that compound 10 which showed a good antibacterial and antifungal activity was isolated from the EtOAc extract.
Compounds 2, and 10 demonstrated efficacy against C. albicans, S. aureus and P. aeruginosa strains. Thus, they could be used as antibacterial and antifungal agents. Antimicrobial flavonoids have multiple cellular targets and form complexes with proteins through nonspecific forces such as hydrogen bonding, hydrophobic effects, and covalent bond formation [52]. Thus, their mode of action (Table 1) may be related to their ability to inactivate microbial adhesins, enzymes, and cell envelope transport proteins [53, 54].
The identified compounds could explain the use of the plant in the treatment of skin infections and adjuvant effects in other diseases such as cancer or diabetes. From Table 2, both compounds 2 and 3 showed good antioxidant activity (IC50 = 64.81 and 666.85 µg/ml) indicating that the antioxidant activity of S. princeae methanol extract with IC50 = 61.26 µg/ml [11] was due to the presence of these compounds. By their antioxidant activity, the compounds could serve radical scavengers [63]. The antioxidant activity of flavonoids depends on the arrangement of functional groups in the aromatic structure. The configuration, substitution pattern, and total number of hydroxyl groups substantially influence the antioxidant activity. The B ring hydroxyl configuration is the most significant determinant of antioxidant activity because it can donate hydrogen and an electron to hydroxyl, peroxyl, and peroxynitrite radicals, in turn giving rise to a relatively stable flavonoid radical [52, 64].
Sunscreens are chemicals that absorb UV rays protecting the skin from damaging solar radiation. [65]. In Fig. 6, compounds 2 and 3 showed high a level of against UV light compared to the standard para-aminobenzoic acid. The other compounds only exhibited a low level of protection against UV light. The recorded sun protection potential of the isolated compounds was better than that of crude methanolic and aqueous extract of S. princeae [11]. Solar ultraviolet radiation is made up of UV-C (200–280 nm), UV-B (280–320 nm), and UV-A (320–400 nm) [65]. UV-C is filtered out by the ozone layer and the most biologically damaging radiation, UV-B, and UV-A radiation are responsible for inducing skin cancer. The use of skin care products supplemented with several effective sunscreen agents may be an effective approach for reducing UV-B generated reactive oxygen spices as well as mediated photo-aging [66].
Some of the isolated compounds have been previously reported to possess variable biological activities with different mode of action as summaries in Table 1. Compounds 1, 2, and 3 have antibacterial, antifungal, antioxidant, and sun protection potential [52, 67,68,69]. Compound 5 has been reported to exhibit antioxidant activity, one of the studied has reported a good renal interstitial fibrosis effects, characterized by the accumulation of excess extracellular matrix and renal tissue damage in the kidney [57, 70]. However, its antibacterial potential is still lacking. Similar compounds such as asperulosidic acid methyl ester, have been reported to possess good antifungal activity against C. albicans (8.33 mm zone of inhibition diameter) [71]. Compound 4 is a major form through which plants store phosphorus [72, 73] and has been reported as a metabolic mediator during the transcription of stimuli-responsive genes in stress response and hormones. It is used in treating mood disorders but no studies have been carried out to investigate its antioxidant, sun protection and antibacterial potential [56, 74]. Compounds 7, 8, 9 and 11 have antibacterial and antioxidant activity [75,76,77].
Conclusion
This study provides the scientific basis for the ethnopharmacological use of S. princeae for the treatment of skin infections, with 11 bioactive compounds having been isolated from the extracts and unambiguously identified. Compound 2, kaempferol-3-O-rutinoside has antifungal activity against C. albicans. Compound 10, ursolic acid shows various antibacterial and antifungal activities against S. aureus, P. aeruginosa, C. albicans and A. flavus. Therefore, these compounds explain the effects observed and used in traditional medicine. They should be considered in drug formulations and be further evaluated for their cytotoxicity, to establish their mode of action, sensitivity, and selectivity. In future work, we will address further in-dept analysis of the compounds contained in the n-hexane and aqueous extracts of Spermacoce princeae.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request and Mendeley data repository DOI.10.17632/x2y89bdcj8.1
Abbreviations
- DCM:
-
Dichloromethane
- EtOAc:
-
Ethyl acetate
- MeOH:
-
Methanol
- Hex:
-
n-Hexane
- DMSO:
-
Dimethyl sulfoxide
- UV:
-
Ultra Violet
- VIS:
-
Visible
- NMR:
-
Nuclear Magnetic Resonance
- Q-ToF:
-
Quadrupole time- of-flight
- MS:
-
Mass spectroscopy
- GC:
-
Gas chromatography
- FID:
-
Flame Ionization Detector
- MHz:
-
Megahertz
References
Nyaboke JO, Onyancha MJ, Odhiambo, JacksnOnyukaMemba JO, Ogembo GP, Wambugy MC. Phytochemical Studies of Acmella Caulirhiza and Spermacoce Princeae Used By Postpartum Mothers in Nyamira. Int J Sci Reserach Publ. 2017;7(8):591–9.
Wong KY, Vikram P, Chiruvella KK, Mohammed A. Phytochemical screening and antimicrobial potentials of Borreria sps (Rubiaceae). J King Saud Univ - Sci. 2015;27(4):302–11.
Ntemafack A, Gatsing D, Chegaing Fodouop SP, Magnifouet HN. Toxicological evaluation of the aqueous leaf extract of Spermacoce princeae (rubiaceae): A traditional antibacterial preparation. Int J Toxicol Pharmacol Res. 2015;7(3):123–9.
Dessein S, Robbrecht E, Smets E. A new heterophyllous Spermacoce species (Rubiaceae) from the Marungu highlands, Democratic Republic of the Congo. . Novon. 2006;16(2):231–4.
Vaes E, Vrijdaghs A, Smets EF, Dessein S. Elaborate petals in Australian Spermacoce (Rubiaceae) species: Morphology, ontogeny and function. Ann Bot. 2006;98(6):1167–78.
Kaviarasan K, Pugalendi KV. Influence of flavonoid-rich fraction from spermacoce hispida seed on ppar-alpha gene expression, antioxidant redox status, protein metabolism and marker enzymes in high-fat-diet fed stz diabetic rats. J Basic Clin Physiol Pharmacol. 2009;20(2):141–58.
Ramadhani SON, Denis Z, Mainen JM, Paul E, Samuel W, Moses NN, Vincent PKT, Abdul WK, Pax JM. Ethnobotanical survey and in vitro antiplasmodial activity of medicinal plants used to treat malaria in Kagera and Lindi regions Tanzania. J Med Plants Res. 2015;9(6):179–92.
Namukobe J, Kasenene JM, Kiremire BT, Byamukama R, Kamatenesi-Mugisha M, Krief S, et al. Traditional plants used for medicinal purposes by local communities around the Northern sector of Kibale National Park. Uganda J Ethnopharmacol. 2011;136(1):236–45.
Ochwangi DO, Kimwele CN, Oduma JA, Gathumbi PK, Mbaria JM, Kiama SG. Medicinal plants used in treatment and management of cancer in Kakamega County. Kenya J Ethnopharmacol. 2014;151(3):1040–55.
Kamatenesi-Mugisha M, Oryem-Origa H. Medicinal plants used to induce labour during childbirth in western Uganda. J Ethnopharmacol. 2007;109(1):1–9.
Namukobe J, Sekandi P, Byamukama R, Murungi M, Nambooze J, Ekyibetenga Y, et al. Antibacterial, antioxidant, and sun protection potential of selected ethno medicinal plants used for skin infections in Uganda. Trop Med Health. 2021;49(49):1–10.
Keat NB, Umar RU, Lajis NH, Chen TY, Li TY, Rahmani M, et al. Chemical constituents from two weed species of spermacoce (Rubiaceae). Malaysian J Anal Sci. 2010;14(1):6–11.
Ferreira Júnior JC, Lyra Lemos RP, Conserva LM. Chemical constituents from Spermacoce verticillata (Rubiaceae). Biochem Syst Ecol. 2012;44:208–11.
Kettle A, Scientific TF, Sunnyvale C. Natural products extraction using accelerated solvent extraction. Thermo Fish Sci Brand. 2016;70632:1–6.
Böhmdorfer ST, Oberlerchner J, Rosenau T, Potthast A. Thin Layer Chromatography and the Analysis of Wood Derived Biomass. Curr Chromatogr. 2016;3(2):75–85.
Adia MM, Emami SN, Byamukama R, Faye I, Borg-Karlson AK. Antiplasmodial activity and phytochemical analysis of extracts from selected Ugandan medicinal plants. J Ethnopharmacol. 2016;186:14–9.
Byamukama R, Barbara G, Namukobe J, Heydenreich M, Kiremire B. Bioactive compounds in the stem bark of Albizia coriaria (Welw. ex Oliver). Int J Biol Chem Sci. 2015;9(2):1013.
Reich E, Schibli A, Pharm M. High-Performance Thin-Layer Chromatography for the Analysis of Medicinal Plants. 2006.
Kamurthy H, Dontha S, Duggi S, Sudhakar M. Phytochemical Screening on Pentas lanceolata Leaves-Isolation of Saponin and Anthracene Glycosides and Alkaloids. Am J Ethnomed. 2014;1(4):206–15.
Arora M, Kalia AN, Mishra R, Siddqui AA. Isolation and characterization of stigmasterol and β -sitosterol-D-glycoside from ethanolic extract of the stems of Salvadora persica Linn. Int J Pharm Pharm Sci. 2013;5(1):245–9.
Sekandi P, Namukobe J, Byamukama R, Akala HM, Yeda RA, Heydenreich M. Bioactive secondary metabolites from the leaves of Secamone africana (Olive.). Int J Biol Chem Sci. 2020;14(5):1820–30.
Huong PTT, Van TN, Diep CN, Thao NP, Cuong NT, Cuong NX, et al. Antimicrobial Compounds From Rhizophora Stylosa. J Sci Technol. 2015;53(2):205–10.
Awwad AM, Salem NM, Abdeen AO. Green synthesis of silver nanoparticles using carob leaf extract and its antibacterial activity. Int J Ind Chem. 2013;4(1):1–6.
Jacobsen NE. NMR Spectroscopy Explained. NMR Spectroscopy Explained. 2007.
Siller M, Amer H, Bacher M, Roggenstein W, Rosenau T, Potthast A. Effects of periodate oxidation on cellulose polymorphs. Cellulose. 2015;22(4):2245–61.
Barbini S, Sriranganadane D, Espanã Orozco S, Kabrelian A, Karlström K, Rosenau T, et al. Tools for Bark Biorefineries: Studies toward Improved Characterization of Lipophilic Lignocellulosic Extractives by Combining Supercritical Fluid and Gas Chromatography. ACS Sustain Chem Eng. 2021;9(3):1323–32.
Barbini S, Jaxel J, Karlström K, Rosenau T, Potthast A. Multistage fractionation of pine bark by liquid and supercritical carbon dioxide. Bioresour Technol. 2021;341(8):341.
Nagawa CB, Böhmdorfer S, Rosenau T. Chemical composition of volatiles extracted from indigenous tree species of Uganda: Composition of bark extracts from Psorospermum febrifugum and Milicia excels. Holzforschung. 2015;69(6):815–21.
Becker M, Zweckmair T, Forneck A, Rosenau T, Potthast A, Liebner F. Evaluation of different derivatisation approaches for gas chromatographic-mass spectrometric analysis of carbohydrates in complex matrices of biological and synthetic origin. J Chromatogr A. 2013;1281:115–26.
Becker M, Liebner F, Rosenau T, Potthast A. Ethoximation-silylation approach for mono- and disaccharide analysis and characterization of their identification parameters by GC/MS. Talanta. 2013;115:642–51.
Ma XM, Liu Y, Shi YP. Phenolic derivatives with free-radical-scavenging activities from Ixeridium gracile (DC.) SHIH. Chem Biodivers. 2007;4(9):2172–81.
Leena PN, Aleykutty NA. Isolation and spectral identification of quercetin from the alcoholic root extract of Clerodendrum paniculatum Linn. Int J Pharma Sci Res. 2016;7(1):47–50.
Jang YS, Wang Z, Lee JM, Lee JY, Lim SS. Screening of Korean natural products for anti-adipogenesis properties and isolation of kaempferol-3-o-rutinoside as a potent anti-adipogenetic compound from Solidago virgaurea. Molecules. 2016;21(2):1–11.
Wang Y, Tang C, Zhang H. Hepatoprotective effects of kaempferol 3-O-rutinoside and kaempferol 3-O-glucoside from Carthamus tinctorius L. on CCl4-induced oxidative liver injury in mice. J Food Drug Anal. 2015;23(2):310–7.
Lin LJ, Huang XB, Lv ZC. Isolation and identification of flavonoids components from Pteris vittata L. Springerplus. 2016;5(1):5–7.
Sheng Z, Zheng-Ming T, Yi Z, Guo-Wei SZ-WQ. Chemical Constituents from the Stems and Leaves of Elaeocarpus glabripetalus. Adv Polar SciSPJ. 2010;2018(1):21–4.
Rebecca OPS, Boyce AN, Somasundram C. Isolation and identification of Myo-inositol crystals from dragon fruit (Hylocereus polyrhizus). Molecules. 2012;17(4):4583–94.
Kamiya K, Hamabe W, Harada S, Murakami R, Tokuyama S, Satake T. Chemical constituents of Morinda citrifolia roots exhibit hypoglycemic effects in streptozotocin-induced diabetic mice. Biol Pharm Bull. 2008;31(5):935–8.
Chowdhury SK, Dutta T, Chattopadhyay AP, Ghosh NN, Chowdhury S, Mandal V. Isolation of antimicrobial tridecanoic acid from Bacillus sp. LBF-01 and its potentialization through silver nanoparticles synthesis: a combined experimental and theoretical studies. J Nanostructure Chem. 2021;11(4):573–87.
Chaturvedula VSP, Prakash I. Isolation of Stigmasterol and Beta-Sitosterol from the dichloromethane extract of Rubus suavissimus. Int Curr Pharm J. 2012;1(9):239–42.
Kamboj A, Saluja AK. Isolation of stigmasterol and β-sitosterol from petroleum ether extract of aerial parts of Ageratum conyzoides (Asteraceae). Int J Pharm Pharm Sci. 2011;94–6.
Girma B. Isolation of ursolic acid from the leaves of Ocimum lamiifolium collected from Addis Ababa Area, Ethiopia. African J Biotechnol. 2020;19(2):65–70.
Do Nascimento PGG, Lemos TLG, Bizerra AMC, Arriaga AMC, Ferreira DA, Santiago GMP, et al. Antibacterial and antioxidant activities of ursolic acid and derivatives. Molecules. 2014;19(1):1317–27.
Khan NM, Hossain MS. Scopoletin and β-sitosterol glucoside from roots of Ipomoea digitata. J Pharmacogn Phytochem. 2015;4(2):05–7.
Ibrahim HA, Elgindi MR, Ibrahim RR, El-Hosari DG. Antibacterial activities of triterpenoidal compounds isolated from Calothamnus quadrifidus leaves. BMC Complement Altern Med. 2019;19(102):1–6.
Bbosa GS, Kyegombe DB, Ogwal-Okeng J, Bukenya-Ziraba R, Odyek O, Waako P. Antibacterial activity of Mangifera indica (L.). Afr J Ecol. 2007;45(1):13–6.
Bariş Ö, Güllüce M, Şahin F, Özer H, Kiliç H, Özkan H, et al. Biological activities of the essential oil and methanol extract of Achillea biebersteinii Afan. (Asteraceae). Turkish J Biol. 2006;30(2):65–73.
Krishnaiah D, Sarbatly R, Nithyanandam R. A review of the antioxidant potential of medicinal plant species. Food Bioprod Proc. 2011;89(3):217–33.
Dutra EA, Gonçalves DA, Costa E, Oliveira DA, Rosa E, Kedor-Hackmann M, Rocha MI, Santoro M, et al. Determination of sun protection factor (SPF) of sunscreens by ultraviolet spectrophotometry. Revista Brasileira de Ciências Farmacêuticas Br J Pharm. 2004;40(3):381–5.
Phillips KM, Ruggio DM, Ashraf-Khorassani M. Analysis of steryl glucosides in foods and dietary supplements by solid-phase extraction and gas chromatography. J Food Lipids. 2005;12(2):124–40.
Schripsema J, Caprini GP, Van Der Heijden R, Bino R, De Vos R, Dagnino D. Iridoids from Pentas lanceolata. J Nat Prod. 2007;70(9):1495–8.
Kumar S, Pandey AK. Chemistry and biological activities of flavonoids: An overview. Sci World J ScientificWorld Ltd. 2013;3:1–16.
Oloya B, Namukobe J, Heydenreich M, Ssengooba W, Schmidt B, Byamukama R. Antimycobacterial Activity of the Extract and Isolated Compounds From the Stem Bark of Zanthoxylum leprieurii Guill and Perr. Nat Prod Commun. 2021;16(8):2–9.
Nishino C, Enoki N, Tawata S, Mori A, Kobayashi K, Fukushima M. Antibacterial activity of flavonoids against staphylococcus epidermidis, a skin bacterium. Agric Biol Chem. 1987;51(1):139–43.
Cushnie TPT, Lamb AJ. Antimicrobial activity of flavonoids. Int J Antimicrob Agents. 2005;26(5):343–56.
Valluru R, Van den Ende W. Myo-inositol and beyond - Emerging networks under stress. Plant Sci. 2011;181:387–400.
Xianyuan L, Wei Z, Yaqian D, Dan Z, Xueli T, Zhanglu D, et al. Anti-renal fibrosis effect of asperulosidic acid via TGF-β1/smad2/smad3 and NF-κB signaling pathways in a rat model of unilateral ureteral obstruction. Phytomedicine. 2019;53:274–85.
Chen DF, Li X, Xu Z, Liu X, Du SH, Li H, et al. Hexadecanoic acid from buzhong yiqi decoction induced proliferation of bone marrow mesenchymal stem cells. J Med Food. 2010;13(4):967–75.
Loizou S, Lekakis I, Chrousos GP, Moutsatsou P. Sitosterol exhibits anti-inflammatory activity in human aortic endothelial.pdf. Mol Nutr Food Res. 2010;54:551–8.
Morgan LV, Petry F, Scatolin M, de Oliveira PV, Alves BO, Zilli GAL, et al. Investigation of the anti-inflammatory effects of stigmasterol in mice: insight into its mechanism of action. Behav Pharmacol. 2021;32(8):640–51.
Awad AB, Fink CS. Phytosterols as anticancer dietary components: Evidence and mechanism of action. J Nutr. 2000;130(9):2127–30.
Katashima CK, Silva VR, Gomes TL, Pichard C, Pimentel GD. Ursolic acid and mechanisms of actions on adipose and muscle tissue: a systematic review. Obes Rev. 2017;18(6):700–11.
Medini F, Fellah H, Ksouri R, Abdelly C. Total phenolic, flavonoid and tannin contents and antioxidant and antimicrobial activities of organic extracts of shoots of the plant Limonium delicatulum. J Taibah Univ Sci. 2014;8(3):216–24.
Heim KE, Tagliaferro AR, Bobilya DJ. Flavonoid antioxidants : chemistry, metabolism and structure-activity relationships. J Nutr Biochem. 2002;13:572–84.
Kaur CD, Saraf S. In vitro sun protection factor determination of herbal oils used in cosmetics. Pharmacognosy Res. 2010;2(1):22–5.
Jain SK, Jain NK. Multiparticulate carriers for sun-screening agents. Int J Cosmet Sci. 2010;32:89–98.
Srinivasan R, Natarajan D, Shivakumar MS. Antioxidant Compound Quercetin-3-O-α-L-rhamnoside(1→6)- β-D-glucose (Rutin) isolated from ethyl acetate leaf extracts of Memecylon edule Roxb (Melastamataceae). Free Radicals Antioxidants. 2015;5(1):35–42.
Smith AJ, Oertle J, Warren D, Prato D. Quercetin: a promising flavonoid with a dynamic ability to treat various diseases, infections, and cancers. J Cancer Ther. 2016;07(02):83–95.
Choquenet B, Couteau C, Paparis E, Coiffard LJM. Quercetin and rutin as potential sunscreen agents: Determination of efficacy by an in vitro method. J Nat Prod. 2008;71(6):1117–8.
Yang D, Zhang C, Liu XX, Zhang Y, Wang K, Cheng ZQ. Chemical Constituents and Antioxidant Activity of Lasianthus hartii. Chem Nat Compd. 2017;53(2):390–3.
Toktas U, Sarikahya NB, Parlak C, Ozturk I, Kayalar H. A new iridoid skeleton from Galium asparagifolium and biological activity studies. J Mol Struct. 2022;1250(131693):1–5.
Moldoveanu SC, Davis MF. Analysis of quinic acid and of myo-inositol in tobacco. Beitrage zur Tab Int. 2012;25(4):498–506.
Ariza A, Moroz OV, Blagova EV, Turkenburg JP, Waterman J, Roberts SM, et al. Degradation of Phytate by the 6-Phytase from Hafnia alvei: A Combined Structural and Solution Study. PLoS ONE. 2013;8(5):1–13.
Harwood AJ. Lithium and bipolar mood disorder: The inositol-depletion hypothesis revisited. Mol Psychiatry. 2005;10:117–26.
Gupta R, Sharma AK, Dobhal MP, Sharma MC, Gupta RS. Antidiabetic and antioxidant potential of β-sitosterol in streptozotocin-induced experimental hyperglycemia. J Diabetes. 2011;3(1):29–37.
Sarkar S, Pal A, Chouni A, Paul S. A novel compound β-sitosterol-3-o-β-d-glucoside isolated from azadirachta indica effectively induces apoptosis in leukemic cells by targeting g0/g1 populations. Indian J Biochem Biophys. 2020;57(1):27–32.
Yoshida Y, Niki E. Antioxidant effects of phytosterol and its components. J Nutr Sci Vitaminol (Tokyo). 2003;49(4):277–80.
Acknowledgements
The authors acknowledge the AESA-RISE support grant for the financial support, the Institute of Chemistry of Renewable Resources, Department of Chemistry, University of Natural Resources and Life Science, Vienna, for the technical support in the identification of compounds, Joel Mukwaya and Caroline Nakirijja from College of Veterinary medicine Makerere University for carrying out the antimicrobial assay, and taxonomist Mr. Protase Rwaburindore for identifying the plant. The county of Lower Austria is acknowledged for support through the Austrian Biorefinery Center Tulln (ABCT).
Funding
This work was supported through the AESA-RISE postdoctoral fellowship (ARPDF-18–06) implemented by the African Academy of Sciences (AAS) through funding from the Carnegie Corporation of New York. The statements made and views expressed in this work are solely the responsibility of the authors.
Author information
Authors and Affiliations
Contributions
Jane Namukobe conceptualized the research study. Peter Sekandi collected data, analyzed it, and wrote the main manuscript text. Markus Bacher; analysis of NMR data during the structural elucidation of compounds, Stefano Barbini and Stefan Böhmdorfer; MS analysis of isolated compounds, Robert Byamukama, Christine Betty Nagawa, and Thomas Rosenau: data analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experimental research and field studies were performed in accordance to the WHO guidelines (2003) on good agricultural and collection practices for medicinal plants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sekandi, P., Namukobe, J., Byamukama, R. et al. Antimicrobial, antioxidant, and sun protection potential of the isolated compounds from Spermacoce princeae (K. Schum). BMC Complement Med Ther 23, 201 (2023). https://doi.org/10.1186/s12906-023-04026-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-023-04026-4