Abstract
Background
San Huang Shel Shin Tang (SHSST) is a traditional herbal decoction used as a hepato-protective agent and is composed of Rheum officinale Baill, Scutellaria baicalnsis Geprgi and Coptis chinensis Franch (2:1:1 w/w). Beta-cyclodextrin (β-CD) modification may potentially increase the solubility and spectral properties of SHSST.
Methods
In this research, the hepato-protective effects of unmodified SHSST, β-CD modified SHSST complex (SHSSTc) and silymarin were evaluated in carbon tetrachloride (CCl4) induced acute hepatotoxicity in rats.
Results
SHHSTc (40 mg/kg/day) and silymarin (100 mg/kg/day) both decreased the CCl4-induced cirrhosis pathway-related transforming growth factor beta (TGF-β) and apoptosis pathway-related caspase-8 protein expressions, but SHSST (40 mg/kg/day) did not reduce TGF-β and caspase-8 significantly . Moreover, SHHSTc (40 mg/kg/day) enhanced the activation of insulin-like growth factor 1 receptor (IGF1R) mediated survival pathway than the silymarin (100 mg/kg/day) to protect the liver from damage induced by CCl4.
Conclusions
β-CD modification promotes hepato-protective effects of SHSST and reduces the required-dosage of the SHSST.
Similar content being viewed by others
Background
Hepatic fibrosis is one of the most critical pathological features of chronic liver disease. Liver fibrosis is associated with the inflammatory and reparative phase of hepatic fibrosis by activated hepatic stellate cells (HSC) and can be characterized by an excessive deposition of extracellular matrix (ECM) components in the liver parenchyma [1]. Liver fibrosis is known to be a serious chronic disease and it is difficult to treat with an aggressive treatment due to possible cirrhosis outcomes. This makes it necessary to develop a new complex or cocktail of more efficient drugs with sufficiently low dosages to prevent side effects.
SHSST is a cocktail of traditional herbal decoction, with reported bioactivities such as hypotension, antioxidation, anti-inflammation and cardio-protective effects [2]. Rheum was discovered to have a hepato-protective effect and can be used to treat carbon tetrachloride (CCl4)-induced liver injury in rats [3, 4]. Scutellaria and Coptis were also reported to elicit similar liver protection against acute hepatotoxicity [5–7]. The similar liver protection effects of Rheum officinale, Scutellaria baicalnsis and Coptis chinensis are due to the similarity in the constituent bioactive compounds such as baicalein, which is a flavonoid [8–10].
In our previous study, the tumor necrosis factor ligand superfamily member 6 (FAS) was activated in the course of CCl4-induced liver failure, with down stream apoptotic protein caspase-8 on Fas-associated protein with death domain (FADD) released to cytosol, causing cleavage of caspase 3 and progression of cellular apoptosis [11, 12]. CCl4 induced liver failure occurs through an oxidation process when CCl4 is transported through the vascular system to the liver and by catalysis by mixed function oxidase (MFO) such as P450, changes into methane chloride or radicals. These radicals cause protein metabolic obstruction and inflammation in the liver, producing CCl4 induced acute liver injury [13, 14]. Silymarin can provide an anti-oxidation function to block the CCl4 catalyzing process and protect the liver from CCl4 induced acute liver injury but not through the P450 inhibition [15]. Many flavonoid compounds play the same role with their anti-oxidative function. Baicalein in SHSST can also enhance cell survival ability through PI3K-Akt pathway activation. The active Akt can keep the Bcl-2-associated death promoter (Bad) protein in phosphorylated type and prevent cell apoptosis [16]. Here, the liver protection function of SHSST was tested and compared with silymarin.
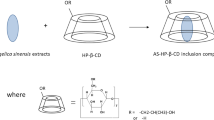
In our previous research, beta- cyclodextrin (β-CD) increased the solubility and spectral properties of guest molecules, especially the hydrophobic drugs, without changing their intrinsic property to permeate the cell membranes [17–19]. Thus, β-CD complex synthesis with the indicated compound or herbal decoction can enhance the solubility, stability and bioavailability of drugs [20, 21]. This research evaluated the liver protection effects of the β-CD modified SHSST complex (SHSSTc), SHSST and silymarin in CCl4 induced acute hepato-toxicity in rats.
Methods
Preparation of SHSST and SHSST-β-CD complex
The SHSST was purchased from PaiAn pharmacy (Taichung, Taiwan). The SHSST-β-CD complex was prepared by coprecipitation. β-CD (70.0 g) was dissolved in distilled water (85 ml) at 70 °C in a water bath for 1 h. SHSST (10.0 g) in ethanol (15 mL) was slowly added to the β-CD solution with continuous agitation and stirred continuously for 6 h. Following that, 40 mL of ethanol was added drop wise to regulate the solubility of the hydrophobic solute in β-CD solution. The solution was then refrigerated overnight at 4 °C. The precipitated SHSSTc (SHSST-β-CD complex, SHSST: β-CD = 1: 9 in weight) was recovered by filtration and washed with ethanol to remove unencapsulated SHSST. This residue was dried in a vacuum oven at −20 °C for 48 h. The final powder was stored at 4 °C until use.
Animal model
The animal experimental protocol was approved by the Institutional Animal Care and Use Committee (IACUC) of China Medical University (No.100-3-B, date 2010-9-1). There were 30 SD rats (300 g in body weight, aged 10 weeks) purchased from BioLASCO Taiwan Co., Ltd and were divided into 5 groups (n = 6 each). The groups were designated as control, CCl4 (Sgma-Aldrich, Taipei, Taiwan) intraperitoneal injection treatment, CCl4 intraperitoneal injection combined with SHSSTc (40 mg/kg/day) oral treatment, CCl4 intraperitoneal injection combined with SHSST oral treatment (40 mg/kg/day), CCl4 intraperitoneal injection combined with silymarin (Sigma-Aldrich, Taipei, Taiwan) oral treatment. CCl4 intraperitoneal injection (100 mg/kg/day) treatment was performed on the 7th day following 6 days of pretreatment with the test materials. After 24 h CCl4 intraperitoneal injection, all the rats were killed by decapitation and samples were collected immediately.
Blood biochemical analysis
Blood was collected from rat in each group during the while decapitation and measured using the blood routine examination protocol at China Medical University Hospital. The following parameters were analyzed: TC (total cholesterol), cholesterol, AST (aspartate transaminase), ALT (alanine transaminase), BUN (blood urea nitrogen), CK (creatine kinase).
Hemotoxyline and eosin staining
Livers from rats in each group were soaked in 10 % formalin, dehydrated through graded alcohols and embedded in paraffin wax. Following that, 2 μm thick paraffin sections were cut from these paraffin-embedded tissue blocks. The tissue sections were deparaffinized by immersion in xylene and rehydrated. Sections were stained with hematoxylin and eosin (H&E), immersed in graded alcohols followed by xylene and mounted in mounting medium kit (Surgipath, Leica Biosystems, Instrument Co., Richmond, USA). Photomicrographs were obtained using Zeiss Axiophot microscopes (Taiwan Instrument Co., Taipei, Taiwan).
Masson’s trichrome staining
Rat livers from each group were soaked in 10 % formalin, dehydrated through graded alcohols and embedded in paraffin wax. Following that, 2 μm thick paraffin sections were cut from these paraffin-embedded tissue blocks. The tissue sections were deparaffinized by immersion in xylene and rehydrated. Samples were then stained with Masson’s trichrome (MT) using HT15 Sigma Trichrome stain (Masson) kit (HT1079, Sigma-Aldrich, Taipei, Taiwan) and the procedure was according to the protocol of the kit. MT satin was used to investigate liver histological and fibrotic changes and photomicrographs were obtained using Zeiss Axiophot microscopes (Taiwan Instrument Co., Taipei, Taiwan).
Tissue protein extraction
Liver tissue extracts from 6 rats in each group were obtained by homogenizing in a lysis buffer (0.05 M Tris–HCl, pH 7.4, 0.15 M NaCl, 0.25 % deoxycholic acid, 1 % NP-40, 1 mM EDTA) at a ratio of 100 mg tissue/1 ml buffer. The homogenates were placed on ice and then centrifuged at 13,000 rpm for 40 min. The supernatants were collected and stored at −80 °C for further experiments.
Western blot assay
Liver tissue extract protein concentrations were determined using the Lowry protein assay. Protein samples were separated in a 12 % SDS polyacrylamide gel electrophoresis (SDS-PAGE) with a constant voltage of 75 V for 120 min. Proteins were then transferred to Hybond-C membranes (GE healthcare UK limited., Buckinghamshire, UK) using 50 volt for 3 h. PVDF membranes were incubated in 3 % bovine serum albumin (BSA) in Tris-buffered solution (TBS). Primary antibodies (Santa Cruz Biotechnology, CA, USA) were added into the membranes to recognize the respective proteins. After washing 3 times, horseradish peroxidase-labeled antibodies were then used. Last, after 3 times washed and pictures were taken with Fujifilm LAS-3000 (GE healthcare UK limited, Buckinghamshire, UK).
Statistical analysis
The results shown are the means ± SD of three independent experiments. Statistical analysis was performed using one-way analysis of variants. The Student’s t-test was used for paired samples.
Results
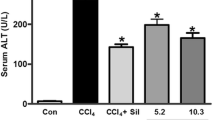
After 24 h CCl4 intraperitoneal injection treatment, the parameters of TG and TC did not show any significant change. AST and ALT were significantly expressed after CCl4-IP treatment within 24 (Table 1). However, 7 days pretreatments of SHSSTc and silymarin reduced the cholesterol after CCl4 intraperitoneal injection. ALT expression was especially reduced in SHSST, SHSSTc and silymarin treatment groups while AST expression was reduced only in the SHSSTc treatment group.
Further, H&E staining showed abnormal lipid accumulation within the hepatocytes around the small vascular of the liver 24 h after CCl4 treatment and these abnormal morphology imply the presence of fat cells with vacuolated cytoplasm which is an indication of hepatic steatosis. The SHSSTc and silymarin efficiently protected the hepatocytes and decreased the abnormality around the small vascular (Fig. 1). MT staining confirmed the fibrosis area through the collagen accumulation in CCl4 induced damaged liver and showed similar results in the SHSSTc and silymarin treated rat livers. SHSSTc and silymarin treatment inhibited the fibrosis and reduced the collagen accumulation in CCl4 induced damaged rat livers.
Hematoxylin and eosin stain (H&E) and Massion’s trichrome stain (MT) of liver slides. H&E stain show the CCl4 induce damaged group rat livers caused the lipid accumulation around the capillary and indicated by black arrows. SHSST and silymarin treatments provided a slight reduction in lipid accumulation. But SHSSTc treatment protected the liver and prevented the cell death. MT stain shows a serious liver fibrosis in CCl4-damaged rat liver group and are indicated by white arrows. After the silymarin, SHSST and SHSSTc treatments all can provide a great anti-fibrosis effect in CCl4 induced damaged rat livers. (The nuclei of the cells are stained with blue color, and others are stained by pink color by H&E staining assay. The fibrosis cells are indicated by blue color and normal cells are indicated by pink color in MT staining assay)
TGF-β pathway activation is necessary for fibroblast collagen secretion in the fibrosis process. CCl4 intraperitoneal injection treated groups rats showed highly expressed TGF-β pathway proteins, such as p-Samd and CTGF (Fig. 2a). The TGF-β pathway protein expression showed a decrease in the SHSSTc and silymarin treated groups similar to the control group. The unmodified SHSST treated group did not show a significant reduction in TGF-β pathway protein expression. After further calculation, the SHSSTc treatment decreased TGF-β and p-Smad more efficiently than other treatments (Fig. 2b, c) however, silymarin also provided efficient reduction of CTGF in CCl4 induced liver fibrosis (Fig. 2d).
The TGF-β regulated fibrosis pathway protein expressions analysis. The protein sample of each group was analyzed by western blotting assay. a TGF-β/p-Smad/CTGF protein expressions increased in CCl4-induced acute hepato-toxicity group and reduced in SHSSTc treatment group. b The protein expression folds of TGF-β. c The protein expression folds of p-Smad. d The protein expression folds of CTGF. (* = P <0.05, ** = P <0.01, *** = P <0.001, compared with control group.)
FAS ligand and FAS complex are known to lead to the formation of death inducing signal complex starting with recruitment of the FAS associated death domain (FADD) adaptor protein. FADD recruits and aggregates the pro-form of caspase-8, leading to caspase-8 activation and triggering the progression of apoptosis. The liver protein analysis shows the FAS/ FADD/caspase-8 pathway activation in CCl4 treatment group within 24 h (Fig. 3a). Silymarin and SHSST treatment did not reduce FAS and FADD proteins by any significant level (Fig. 3b, c). However, downstream caspase-8 activation was indeed blocked by SHSSTc and silymarin treatments (Fig. 3d)
The FAS regulated apoptosis pathway protein expressions analysis. The protein sample of each group was analysis by western blotting assay. a FAS/FADD/Caspase 8 protein expressions increased in CCl4-induced acute hepatotoxicity group and decreased in SHSSTc treatment group. b The protein expression folds of FAS. c The protein expression folds of FADD. d The protein expression folds of Caspase 8. (* = P <0.05, ** = P <0.01, *** = P <0.001, compared with control group.)
The most important cell survival signaling pathway is through the activation of PI3K/Akt. In SHSSTc treatment, the p-PI3K and p-Akt were activated highly and maintained downstream Bad-phosphorylated (Fig. 4a). Finally, SHSSTc blocked caspase-3 cleavage stronger than SHSST and silymarin treatment. Both the SHSST and SHSSTc were effective than the silymarin in enhancing IGF receptor phosphorylation (Fig. 4b), and its downstream p-PI3K/p-Akt/p-Bad (Fig. 4c, d, e). The Caspase-3 expression was also partly reduced by SHSST and silymarin treatments, but was totally blocked by SHSSTc treatment (Fig. 4f).
The PI3K regulated survival pathway protein expressions analysis. The protein sample of each group was analysis by western blotting assay. a p-IGF1R/p-PI3K/p-Akt/p-Bad protein expressions decreased in CCl4-induced acute hepatotoxicity group and increased in SHSSTc treatment group. Apoptotic protein Caspase 3 was increased in CCl4-induced acute hepatotoxicity group and decreased in SHSSTc treatment group. b The protein expression folds of p-IGF1R. c The protein expression folds of p-PI3K. d The protein expression folds of p-Akt. e The protein expression folds of p-Bad. f The protein expression folds of Caspase 3. (* = P <0.05, ** = P <0.01, *** = P <0.001, compared with control group, # = P <0.05, ## = P <0.01, ### = P <0.001, compared with CCl4 treatment group.)
Discussion
CCl4 can be changed into CHCl3 through oxidation in the liver [22]. However, the products after CCl4 oxidation also include free radicals, such as trichloromethyl free radical (CCl3•) and trichloromethylperoxyl free radical (CCl3OO•), these free radical compounds will react with the lipoprotein in hepatocytes causing cholesterol accumulation because of the problems in lipid metabolism [23]. Silymarin can provide an anti-oxidant function and reduce the amount of free radicals in the liver, providing liver protection [24]. The flavonoids rich SHSST might also present a similar function, but the result shown the liver protection effect of SHSST was still very week (Table 1, Fig. 1). SHSSTc treatment acts better than SHSST even silymarin owing to the modulations in its bioavailability for being modified with the β-CD complex.
Silymarin is reported to provide protection against liver cirrhosis and it reduces the levels of hepatic fibrosis markers including serum TGF-β1, especially in the CCl4 induced liver injury model [25]. TGF-β1/p-Smad signaling expression can enhance collagen synthesis in fibroblasts [26]. The MT staining assay showed collagen accumulation in the CCl4 induced liver fibrosis group and TGF-β1/p-Smad signaling over expression within 24 h (Figs. 1, 2). In 1 week pretreatment with silymarin and SHSSTc, TGF-β1/p-Smad signaling and collagen accumulation were blocked (Fig. 1, 3). The experimental data suggests that SHSSTc and silymarin have similar anti- cirrhosis effects.
SHSSTc treatment efficiently protects the hepatocytes in CCl4 induced liver injury. The possible protection mechanism is through FAS/FADD/caspase-8 apoptosis pathway inhibition and IGF1R/PI3K/Akt survival pathway activation [27, 28] (Fig. 4). Here, silymarin could only inhibit apoptosis through caspase-8 suppression but not through IGF1R pathway activation. This may be the difference between SHSSTc and silymarin in liver protection which makes SHSSTc protect the liver better than silymarin in this CCl4 induced liver injury animal model.
The bioactive compounds of SHSST represent anthraquinones, such as emodin, aloe-emodin, chrysophanol, and flavones such as baicalin, baicalein, wogonoside, wogonin, and alkaloids such as berberine, palmatine, coptisine [29]. The components from silymarin are flavonols such as silybin, isosilybin, silydianin, and silychristin [30]. The chemical structures of all of these components are shown in Fig. 5. The structures of bioactive compounds from SHSST belong to the flavone and flavonol groups. Although the bioavailability of flavonol is greater than for flavones, the large functional groups in silymarin derivatives might decrease the original benefits of flavonol. The small molecular weight of the bioactive compounds from SHSST might enhance the diffusion ability. Thus, the β-CD modification can increase the water solubility of hydrophobic flavone compounds and improve the hepatoprotective effects. The SHSSTc was formed by SHSST and β-CD at the ratio of 1:9 by weight and the water solubility, stability and bioavailability were promoted better than by SHSST. Actually, both the anti-cirrhosis and liver protection effects of SHSSTc treatment were better than the other groups in the CCl4 induced acute liver injury animal model.
Conclusions
SHSST modification with β-CD complex to SHSSTc enhances the liver protection effects of SHSST. SHSSTc shows similar inhibitory effects with silymarin in the FAS/FADD/caspase-8 apoptosis pathway and TGF-β fibrosis pathway. However, SHSSTc augmented the IGF1R/PI3K/Akt survival pathway more than silymarin and displayed stronger protection against CCl4 induced liver injury.
Abbreviations
ALT, alanine transaminase; AST, aspartate transaminase; Bad: Bcl-2-associated death promoter; BUN, blood urea nitrogen; CCl4, carbon tetrachloride; CK, creatine kinase; ECM, extracellular matrix; FADD, Fas-associated protein with death domain; FAS, tumor necrosis factor ligand superfamily member 6; HSC, hepatic stellate cells; MFO, mixed function oxidase; SHSST, San Huang Shel Shin Tang; SHSSTc, β-CD modified SHSST complex; TC, total cholesterol; TGF-β, transforming growth factor beta; β-CD, Beta-cyclodextrin
References
Parsons CJ, Takashima M, Rippe RA. Molecular mechanisms of hepatic fibro genesis. J Gastroenterol Hepatol. 2007;22:S79–84.
Cheng WY, Wu SL, Hsiang CY, Li CC, Lai TY, Lo HY, Shen WS, Lee CH, Chen JC, Wu HC, Ho TY. San-Huang-Xie-Xin-Tang and its herbal components on the gene expression profiles in HepG2 cells. Am J Chin Med. 2008;36:783–97.
Wang JB, Zhao HP, Zhao YL, Jin C, Liu DJ, Kong WJ, Fang F, Zhang L, Wang HJ, Xiao XH. Hepatotoxicity or hepatoprotection? Pattern recognition for the paradoxical effect of the Chinese herb Rheum palmatum L. in treating rat liver injury. PLoS One. 2011;6:e24498.
Fang F, Wang JB, Zhao YL, Jin C, Kong WJ, Zhao HP, Wang HJ, Xiao XH. A comparative study on the tissue distributions of rhubarb anthraquinones in normal and CCl4-injured rats orally administered rhubarb extract. J Ethnopharmacol. 2011;137:1492–7.
Chien CF, Wu YT, Tsai TH. Biological analysis of herbal medicines used for the treatment of liver diseases. Biomed Chromatogr. 2011;25:21–38.
Nan JX, Park EJ, Kim YC, Ko G, Sohn DH. Scutellaria baicalensis inhibits liver fibrosis induced by bile duct ligation or carbon tetrachloride in rats. J Pharm Pharmacol. 2002;54:555–63.
Ye X, Feng Y, Tong Y, Ng KM, Tsao S, Lau GK, Sze C, Zhang Y, Tang J, Shen J, Kobayashi S. Hepatoprotective effects of Coptidis rhizoma aqueous extract on carbon tetrachloride-induced acute liver hepatotoxicity in rats. J Ethnopharmacol. 2009;124:130–6.
Püssa T, Raudsepp P, Kuzina K, Raal A. Polyphenolic composition of roots and petioles of Rheum rhaponticum L. Phytochem Anal. 2009;20:98–103.
Wang CZ, Calway TD, Wen XD, Smith J, Yu C, Wang Y, Mehendale SR, Yuan CS. Hydrophobic flavonoids from Scutellaria baicalensis induce colorectal cancer cell apoptosis through a mitochondrial-mediated pathway. Int J Oncol. 2013;42:1018–26.
Liu L, Chen Z. Analysis of four alkaloids of Coptis chinensis in rat plasma by high performance liquid chromatography with electrochemical detection. Anal Chim Acta. 2012;737:99–104.
Huang CY, Yang AL, Lin YM, Wu FN, Lin JA, Chan YS, Tsai FJ, Tsai CH, Kuo CH, Lee SD. Anti-apoptotic and pro-survival effects of exercise training on hypertensive hearts. J Appl Physiol (1985). 2012;112:883–91.
Lee SD, Shyu WC, Cheng IS, Kuo CH, Chan YS, Lin YM, Tasi CY, Tsai CH, Ho TJ, Huang CY. Effects of exercise training on cardiac apoptosis in obese rats. Nutr Metab Cardiovasc Dis. 2013;23:566–73.
Chaudhury S, Mehendale HM. Amplification of CCl4 toxicity by chlordecone: destruction of rat hepatic microsomal cytochrome P-450 subpopulation. J Toxicol Environ Health. 1991;32:277–94.
Klingensmith JS, Mehendale HM. Destruction of hepatic mixed-function oxygenase parameters by CCl4 in rats following acute treatment with chlordecone, Mirex, and phenobarbital. Life Sci. 1983;33:2339–48.
Kim HJ, Chun YJ, Park JD, Kim SI, Roh JK, Jeong TC. Protection of rat liver microsomes against carbon tetrachloride-induced lipid peroxidation by red ginseng saponin through cytochrome P450 inhibition. Planta Med. 1997;63:415–8.
Zhang HB, Lu P, Guo QY, Zhang ZH, Meng XY. Baicalein induces apoptosis in esophageal squamous cell carcinoma cells through modulation of the PI3K/Akt pathway. Oncol Lett. 2013;5:722–8.
Tsai Y, Tsai HH, Wu CP, Tsai FJ. Preparation, characterisation and activity of the inclusion complex of paeonol with b-cyclodextrin. Food Chem. 2010;120:837–41.
Yuan C, Jin Z, Xu X, Zhuang H, Shen W. Preparation and stability of the inclusion complex of astaxanthin with hydroxypropyl-b-cyclodextrin. Food Chem. 2008;109:264–8.
Vyas A, Saraf S, Saraf S. Cyclodextrin based novel drug delivery systems. J Incl Phenom Macro. 2008;62:23–42.
Uekama K, Hirayama F, Irie T. Cyclodextrin Drug Carrier Systems. Chem Rev. 1998;98:2045–76.
Kang J, Kumar V, Yang D, Chowdhury PR, Hohl RJ. Cyclodextrin complexation: Influence on the solubility, stability, and cytotoxicity of camptothecin, an antineoplastic agent. Eur J Pharm Sci. 2002;15:163–70.
Raymond P, Plaa GL. Effect of dosing vehicle on the hepatotoxicity of CCl4 and nephrotoxicity of CHCl3 in rats. J Toxicol Environ Health. 1997;51:463–76.
Weber LW, Boll M, Stampfl A. Hepatotoxicity and mechanism of action of haloalkanes: carbon tetrachloride as a toxicological model. Crit Rev Toxicol. 2003;33:105–36.
Velussi M, Cernigoi AM, De Monte A, Dapas F, Caffau C, Zilli M. Long-term (12 months) treatment with an anti-oxidant drug (silymarin) is effective on hyperinsulinemia, exogenous insulin need and malondialdehyde levels in cirrhotic diabetic patients. J Hepatol. 1997;26:871–9.
Wei F, Liu SK, Liu XY, Li ZJ, Li B, Zhou YL, Zhang HY, Li YW. Meta-analysis: silymarin and its combination therapy for the treatment of chronic hepatitis B. Eur J Clin Microbiol Infect Dis. 2013;32:657–69.
Xue W, Yunliang Q, Rong J, Yan W, Jun C, Chen W, Danru W. Effects of TRAP-1-Like Protein (TLP) Gene on Collagen Synthesis Induced by TGF-b/Smad Signaling in Human Dermal Fibroblasts. Plos One. 2013;8:e55899.
Hsieh SR, Cheng WC, Su YM, Chiu CH, Liou YM. Molecular targets for anti-oxidative protection of green tea polyphenols against myocardial ischemic injury. BioMedicine. 2014;4:7–16.
Wang CH, Lin WD, Bau DT, Chou IC, Tsai CH, Tsai FJ. Appearance of acanthosis nigricans may precede obesity: An involvement of the insulin/IGF receptor signaling pathway. BioMedicine. 2013;3:82–7.
Li CY, Hou YC, Lee Chao PD, Shia CS, Hsu IC, Fang SH. Potential ex vivo immunomodulatory effects of San-Huang-Xie-Xin-Tang and its component herbs on mice and humans. J Ethnopharmacol. 2010;127:292–8.
Parveen R, Baboota S, Ali J, Ahuja A, Vasudev SS, Ahmad S. Effects of silymarin nanoemulsion against carbon tetrachloride-induced hepatic damage. Arch Pharm Res. 2011;34:767–74.
Acknowledgment
Not applicable.
Funding
This study is supported in part by Taiwan and from Taiwan Ministry of Health and Welfare Clinical Trial and Research Centre of Excellence (MOHW105-TDU-B-212-133019).
Availability of data and materials
We have presented all our data in the form of figures and tables. The datasets supporting the conclusions of this article are included within the article.
Authors’ contribution
YLY, WJT, WWK, HHH and CYS contributed conception, design and acquisition of data. YML, CHC and VVP contributed the analysis and interpretation of data. YT drafted the manuscript and CYH revised and gave final approval of the version to be published. All authors were read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The animal experimental protocol used in this study was approved by the Institutional Animal Care and Use Committee (IACUC) of China Medical University (No.100-3-B, date 2010-9-1).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yeh, YL., Ting, WJ., Kuo, WW. et al. San Huang Shel Shin Tang beta-cyclodextrin complex augmented the hepatoprotective effects against carbon tetrachloride-induced acute hepatotoxicity in rats. BMC Complement Altern Med 16, 150 (2016). https://doi.org/10.1186/s12906-016-1127-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-016-1127-8