Abstract
Background
Timely initiation of modern contraceptive use is vital to prevent unintended pregnancy and its related morbidities and mortalities. However, there is a scarcity of evidence about the duration of time elapsing from childbirth to initiating modern contraceptive use following childbirth and its associated factors in the study area for evidence-based interventions. Therefore, we aimed to assess the time to initiation of modern contraceptive method use and its predictors in Hossana town, southern Ethiopia.
Methods
A retrospective follow-up study was conducted at public health facilities in Hosanna town. A total of 503 study participants were included in the study using a systematic random sampling technique. The Box and Whisker plot was used to estimate the time to initiation of modern contraceptive use. A Weibull regression model was applied to identify predictors of time to initiation of modern contraceptive use. Adjusted Hazard Ratio (AHR) with a 95% confidence interval (CI) was used to interpret the strength of the association.
Results
The median time to initiation of modern contraceptive use was 6 months, with an interquartile range of 3 months. Husband/partner attending higher education [AHR = 1.64, 95% CI: 1.04, 2.57], women who had parity of more than two [AHR = 1.93, 95% CI: 1.01, 3.67], and women who had communicated with their husband/partner about modern contraceptive methods [AHR = 3.03, 95% CI: 1.41, 6.67] were more likely to initiate modern contraceptive method use within six months after childbirth. In contrast, women with an older age of greater than or equal to 30 years [AHR = 0.32, 95% CI: 0.13, 0.82] and who did not resume sexual intercourse after childbirth [AHR = 0.02, 95% CI: 0.01, 0.03] were less likely to initiate modern contraceptive method use within six months after childbirth.
Conclusions
The median time to initiation of modern contraceptive method use after childbirth in the postpartum period was delayed from the World Health Organization recommendation of at most 6 weeks. Emphasis should be given to older women, women with lower parity, and men’s participation in contraceptive communication to improve timing for initiation of modern contraceptive use after childbirth and to curb the five-month lag periods.
Similar content being viewed by others
Background
The time elapsed from childbirth until initiation of modern contraceptive use is crucial to prevent unintended pregnancy and its consequences, such as unsafe abortion, hemorrhage, sepsis, and maternal death [1]. Timely initiation of postpartum modern contraceptive use (in the first month of childbirth) plays an important role in strategies to achieve adequate intervals between pregnancies (at least 2 years) [2]. More than 30% of maternal deaths and 10% of child deaths can be prevented by spacing pregnancy for at least 2 years using modern contraceptive methods. Thus, timely initiation of modern contraceptive method use after childbirth saves the lives of mothers and children [3].
Globally, in 2019, the proportion of family planning requirements met by modern methods was 75.7%. However, demographic and health survey data analysis from 27 countries shows that 95% of women who are 0–12 months postpartum want to avoid a pregnancy in the next 2 years, but 70% of them are not using contraception [4]. A significant proportion of women, particularly in developing countries, have sexual intercourse after childbirth without any form of contraception [5]. Empirical studies revealed that women in low and middle income countries including Ethiopia, less utilize modern methods often due to lack of decision-making autonomy, perceived social norms (approval of or conformability to others), fear of side effects, myths and misconceptions [6, 7]. In Sub-Saharan Africa, nearly one-third of postpartum women are at risk of becoming pregnant from unprotected sex within the first two years of delivery [8].
In Ethiopia, even in contraceptive-accessible areas like urban areas, a sizable proportion (50%) of women did not use any form of modern method. Still, 22% of women have an unmet need for modern contraception (13% for spacing and 9% for limiting) [9]. Many postpartum women in Ethiopia resumed sexual intercourse without contraception. For instance, a study in Ethiopia found that 78.3% of postpartum women resumed intercourse after giving birth, with a median time of 6 weeks with a late start to contraception [10]. According to the studies in Gondar city and Gozamen district, the median time to use modern contraceptives among women during the extended postpartum period was 6 and 3.2 months, respectively [11, 12]. In Ethiopia, it is common for women to have too many children who are too close in age. As a result, the country’s population has increased significantly, but economic growth has not kept pace. An unbalanced population will inevitably have a negative impact on the nation’s well-being. Modern contraception is one of the strategies that is proving to be effective in addressing these issues [12].
According to the World Health Organization medical eligibility criteria for contraceptive use, women should be offered contraceptives within the first month of postpartum [13]. As all nations also share, the Ethiopian government has an ambition to reduce current maternal mortality (412 per 100,000 live births) to at least 70 per 100,000 live births at the end of 2030 [14]. To achieve this sustainable development goal, timely initiation of modern contraceptive method use is one of the key strategies, globally [15].
Therefore, we aimed to assess the duration of time to initiate modern contraceptive use and its predictors among postpartum women visiting public health facilities for child immunization in Hossana town, southern Ethiopia. The finding will contribute to improving maternal and child health by reducing unintended pregnancies and related morbidities and mortalities at local and national levels.
Methods
Study design and setting
A health facility-based retrospective follow-up study was applied to this study. The study was conducted in Hossana town, which is found in Hadiya Zone, southern Ethiopia. Hossana town is located 232 km from the capital city, Addis Ababa, and 294 km from its regional capital city, Hawassa. There is one comprehensive specialized hospital and three health centers (Hosanna, Lichamba, and Bobicho) that offer maternal and child health care services [Hadiya Zone Health Department, unpublished report]. The study was conducted in these health facilities from May 25 to July 25, 2021.
Participants
For this study, women in an extended postpartum period with a one-year-old child who were attending public health facilities for their child’s vaccination during the study period (May 25 to July 25, 2021) were included and retrospectively followed to get data.
Variables and measurements
The dependent variable was the time spent from childbirth to initiation of modern contraceptive use in completed months. A follow-up period was defined as the number of months between a childbirth and the initiation of modern contraceptive use. The event was the initiation of modern contraceptive use in the first six months, whereas the censored was not initiating modern contraceptive use within six months of childbirth. The independent variables were defined as follows: Residence: refers to where the women usually live, categorized as urban or rural.
Education status: refers to the level of education that an individual attended, categorized as no formal education (no grade), primary (1-8th grade), secondary (9-12th grade), higher (attending colleges and Universities).
Occupation: refers to the main job that an individual works.
Parity: the number of times that a woman has given birth, irrespective of outcome.
Family planning council during ANC visits: refers to whether a woman received advice about modern contraceptive use after delivery or not, categorized as “yes” if received or “no” otherwise.
Future reproductive plan: refers to whether the couples have a plan to have additional children or not in the future, categorized as wanting no more children, wanting children within two years, wanting children at and after two years, and undecided.
Communication with partner about modern contraceptive methods: refers to whether a woman has had any discussion about modern contraceptive method use after delivery with her husband or not, categorized as “yes” or “no.“
Husband approval: refers to whether the husband agree or support his wife to use modern contraceptive methods or not, responded as “yes” if agreed and “no” otherwise.
Decision-maker for contraceptive use: measured by asking a woman that who would make a decision to use modern contraceptive methods when needed, categorized as “wife alone,“ “jointly,“ or “husband.“
Return of menses: whether a woman has seen her menses before initiating contraceptive use or not, responded as “yes” or “no”.
Resumption of sexual intercourse: refers to whether the couples, after recent childbirth, have had initiated sexual intercourse or not before using contraceptive methods, responded as “yes” or “no”.
Sample size and sampling procedure
The sample size was determined using Epi info version 7 for proportional hazard regression model by taking 80% power, 5% level of significance, 0.5 standard deviation, 95% confidence interval (CI), and %outcome in the unexposed group of 22.83, %outcome in the exposed group of 35%, and AHR of 1.53. [16]. Finally, the total sample size with 10% non-response rate was 513.
To select the study participants, a systematic random sampling technique was applied in each health center and hospital. The last six-month immunization services for children in each health facility were considered to estimate the number of postpartum women visiting the health facilities (sample frame) and calculate the sample fraction. The total sample size (513) was proportionally allocated to each health facility (Hossana health center = 181, Wachemo University Nigist Eleni Mohammed Memorial hospital = 127, Lichamba health center = 110, and Bobicho health center = 95). Based on the calculated sample fraction of each health facility (k = 8), the study participants were included in the study. The first participant was selected using a simple random sampling technique (lottery method).
Data collection tools and procedures
Data were collected using structured interviewer administered questionnaire adapted from previously done similar researches and modified according to the local context by the investigators. The questionnaire was prepared in English, then translated into Amharic and back into English by experts in both languages to check its consistency. The pre-test was carried out on 5% of the sample size prior to the actual data collection time in Homecho Hospital to make necessary adjustments after obtaining informed consent. The questionnaire was checked for its clarity, understanding ability, uniformity, and completeness of the questions. Necessary amendments, such as skipping and changing the order of questions, were made based on the pre-test result.
A structured interview questionnaire and chart review were used to obtain background information or potential predictors affecting time to modern contraceptive use, such as sociodemographic and economic factors, pregnancy history, reproductive characteristics, access to service & health information related and decision-making, Data collectors (four BSc midwives) who are familiar with the local language and supervisors (four public health professionals) participated in data collection after receiving two days of training by the principal investigator about the data collection instrument, ethical considerations, and objectives of the study.
Data processing and analysis
Data were coded and entered into Epi-data version 7 software and exported to Stata version 14 for the analysis. Before the analysis, the data were checked for missing values and outliers. For quantitative variables means, median and standard deviations were calculated. Continuous variables were categorized using Ethiopian demographic and health survey reports and recoding was done when the cells are few in number. For categorical variables, descriptive statistics such as frequencies and percentages were calculated. The Box and Whisker plot was used to compute the median survival time (time to initiation of modern contraceptive use in months). A cox-proportional hazard assumption was checked using a Schenofeld residual test (global test), and the proportionality assumption was violated. As a result, a parametric model was used as an option, and a parametric distribution that fits the data reasonably better (the Weibull distribution) was selected using a log-likelihood in the null model. In the bivariable Weibull regression model, variables that have shown a significant association with time to initiation of modern contraceptive method use at P < 0.25 were included in the multivariable model. In the multivariable Weibull regression model, variables with a 95% CI for the adjusted hazard ratio that did not include 1 and a P < 0.05 were declared as predictors of time to initiation of modern contraceptive method use.
Data quality control measures
Data quality was assured before, during, and after the data collection process. Before data collection: structured questionnaire was developed from different literature conducted to collect data. It was translated from English to Amharic and back to English to assure consistency. In addition, questionnaire was pre-tested, and training was given for data collectors and supervisors. During data collection, there was close day-to-day supervision. The collected data were checked for completeness and consistency by the supervisors and principal investigator. Adequate time (until they respond) was given for the participants to remember the date variables (age, time of contraceptive use, resumption of sexual intercourse, return of menses) to minimize recall bias. After data collection, the supervisors and the principal investigator together rechecked the completeness and consistency before transferring it into computer software. Non-overlapping numerical codes were given for each question, and then coded data was entered into Epi-data version 7.
Results
Socio-demographic and other characteristics
Of 513 women with one-year-old children who came to the immunization unit, 503 were successfully interviewed, yielding a response rate of 98.05%. The mean age of the study participants was 29.8 ± 5.6 years. The ages range from 17 to 44 years. Three hundred sixty five (72.6%) of the women were protestant religion follower (Table 1).
Time to initiation of modern contraceptive use
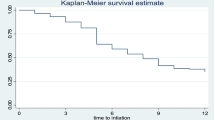
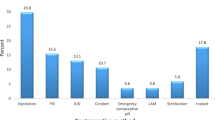
The median survival time to initiate modern contraceptive method use among postpartum women was 6 months, with an interquartile range of 3 months. The proportion of “events” (women who initiated modern contraceptive method use within six months) was 217 (43.1%), and the proportion of “censored” (women who did not initiate using the modern contraceptive methods within 6 months) was 286 (56.9%). Of 217 women who had initiated modern contraceptive methods, 10 (4.6%) pill (progestin only pill), 114 (52.7%) injectable, 90 (41.4%) implants, and 3 (1.3%) male condom users. The cumulative probability of surviving (not initiating modern contraceptive method use) was decreasing as months in the postpartum period increased: 88% within the first month, 80% at the third month, and 57% at the sixth month (Fig. 1).
Predictors of time to initiation of modern contraceptive use
The Cox proportional hazard assumption was checked for the covariates using a Schoenfeld residual test, and the proportionality assumption was violated (Global test chi-square = 45.08, df = 13, and Prob > chi2 = 0.0000) (Additional file 1). Thus, fitting a suitable parametric survival model that provides a hazard ratio (distributions that report log relative hazard) for better interpretation was chosen. Accordingly, we compared three parametric distributions (Exponential, Gompertz, and Weibull) using a log-likelihood in the null model to select a distribution that fit the data reasonably better. The Weibull distribution found to provide a higher log-likelihood (-362.94) than Exponential (-390.95), and Gompertz (-379.53), and selected as better distribution for our data.
In a bivariable Weibull regression model, maternal age, residence, maternal education, husband’s education, parity, number of alive children, family planning counseling during the recent antenatal care, the future reproductive plan, communication between partners, husband approval, decision-making about contraception, return of menses, and resumption of sexual intercourse were significantly associated with time to initiation of modern contraceptive method use at P < 0.25.
In multivariable Weibull regression model, maternal age ≥30 years, husband’s attending a higher education, parity of more than two, communication with husband about modern contraceptive methods, and resumption of sexual intercourse were found to be statistically significant predictors of time to initiation of modern contraceptive method use, with a 95% confidence level and P < 0.05. Women attending secondary education (9-12th grade) and return of menses were marginally significant predictors.
Accordingly, women who were 30 years and older were 68% [AHR = 0.32, 95% CI: 0.13, 0.82] less likely to initiate modern contraceptive methods within six months after childbirth than women who were 17–24 years old. Husband/partner who attended a higher education were nearly twice [AHR = 1.64, 95% CI: 1.04, 2.57] more likely to initiate modern contraceptive methods within six months than those attending a primary and lower education. Women who had parity of more than two were nearly twice [AHR = 1.93, 95% CI: 1.01, 3.67] more likely to initiate modern contraceptive methods within six months than para two and lower. Women who have communicated about modern contraceptive methods with their husband/partner were three times [AHR = 3.03, 95% CI: 1.41, 6.67] more likely to initiate modern contraceptive methods within six months as compared to their counterparts. Women who had not resumed sexual intercourse after the recent childbirth were 98% [AHR = 0.02, 95% CI: 0.01, 0.03] less likely to initiate modern contraceptive methods within six months than those who had resumed sexual intercourse (Table 2).
Discussions
This study aimed to assess the median time to initiation of modern contraceptive method use after childbirth and its predictors among postpartum women. Accordingly, the median time to initiation of modern contraceptive method use was six months, which is associated with maternal age, husband/partner education, parity, communication with husband/partner about contraceptive methods, and resumption of sexual intercourse after childbirth.
In this study, the median time to initiation of modern contraceptive method use after childbirth was six months. The finding of this study suggests that there is a greater delay in initiating contraceptive use after childbirth than recommended by the World Health Organization, which is six weeks [13]. Women in this period could be prone to unintended pregnancy and its consequences, especially when their menses has returned. In Sub-Saharan Africa, including Ethiopia, the rate of mistimed pregnancies is becoming a problem [17,18,19,20]. Approximately half of all pregnancies reported to have come soon, which could have been prevented with increased access to effective utilization of modern postpartum contraceptive methods in a timely manner [17]. The finding of this study was consistent with that of Gondar City, Northwest Ethiopia, which was 6 months [11], and Ambo Town, Central Ethiopia, which was 6 months [21]. The finding was a bit higher than the finding from the national report of four months [22], but lower than the median time reported from Uganda, 19 months [23]. The differences could be due to variation in awareness, access, and availability of modern contraceptive methods, desire for the number of children, decision-making autonomy for contraceptive methods, sample size, the study population considered, and other socio-cultural issues among the countries or study settings.
In this study, women with an older age of 30 or more years were less likely to initiate modern contraceptive method use after childbirth than those with an age of 17 to 24 months. The finding highlights a need for attention for those older women. As women ages goes to older and older (such as ≥30 years), fertility usually decline, and women might have few reproductive times to reach desired number of children [24]. As a result, they might be less likely to use modern contraceptive methods. On the other side, they might have experience of using traditional methods, particularly if they have a regular cycle, so that they less intend to utilize the modern methods [25]. The finding was supported by the findings from Ambo Town and Myanmar, which revealed that older women were less likely to initiate the modern contraceptive method use than those with younger ages [21, 26, 27].
Women with a parity of more than two were more likely to initiate modern contraceptive method use than those with a parity of one to two. Those women with parity of more than two might have reached the desired number of children sooner than those with lower parity. Hence, they may want to space or limit the number of children by using modern contraceptive methods. A study from Ambo Town reported the contrary finding that women with higher parity were less likely to initiate modern contraceptive use following childbirth than those with lower parity [21]. This could be due to socio-cultural variation in the desired number of children in different parts of the country. In some societies, a number of children believed to be an asset for family, as they believed to support parents/families in different circumstances such as income generation, sense of security or protection of family, including females, ease of labour, etc. [28].
This study found that husband/partner with higher education were more likely to initiate modern contraceptive use than those with primary or lower educational attainment. This indicates that an educated husband/partner might have supported or encouraged his wife to use modern contraceptive methods after childbirth. Higher educated husband/partner might have a better access to health care information, and greater ability to use health care services, increases their discussion about the methods than those who had lower education level [29, 30].
Communication of contraceptive issues with their husband/partner significantly associated with timing of modern contraceptives method initiation. The finding suggests the importance of men’s involvement in maternal health care service utilization, such as modern contraceptive use. Communication between couples might have improved the confidence of women to utilize contraceptive services in time. The finding was supported by the study done in northern Ethiopia, Senegal, and Niger that showed couples’ communication about modern contraception was significantly associated with improved utilization of modern contraceptive methods [31,32,33].
Resumption of sexual intercourse after childbirth was found to be an inducing factor to initiate modern contraceptive method use. This could be due to the couple’s awareness of the risk of getting pregnant, possibly an unintended pregnancy, and other related issues such as poor maternal and child health status due to inadequate spacing. The finding was supported by the other studies [34, 35].
Despite the attempts made to reduce bias, this study might have limitations: the study relied on the ability to recall the time of initiation of modern contraceptive method use, and the first sexual initiation, which were difficult to remember accurately. Moreover, this study relied on women bringing a one-year-old child to health facilities for vaccination, and some women who did not bring their children for vaccination were not included in the sample. Furthermore, some women who had a one-year-old child but are pregnant might not have been included in the study, as they might not have visited vaccination clinics. As a result, selection bias might have occurred to some extent. Despite the limitations, the findings can be generalized for population with similar contexts.
Conclusions
The median time to initiation of modern contraceptive method use after childbirth in the postpartum period was delayed from the World Health Organization recommendation of at most 6 weeks. Emphasis should be given for older women, women with lower parity, and men participation in contraceptive communication to improve time to initiation of modern contraceptive use after childbirth, and to curb down the five month lag periods. Improving clients’ awareness of the advantages of timely initiation of modern contraceptive methods, such as the prevention of unintended pregnancies, reducing the risk of abortion, preventing pregnancy-breastfeeding overlaps, preventing maternal nutritional depletion, preventing low birth weight, etc., is crucial.
Data Availability
The raw materials that support the conclusions of this research will be available to researchers, who need the data to use for non-commercial purposes through requesting the corresponding author.
References
Mehare T et al. Postpartum contraceptive use and its determinants in Ethiopia: a systematic review and meta-analysis. International journal of reproductive medicine. 2020;2020.
World Health Organization. WHO recommendations on postnatal care of the mother and newborn. World Health Organization; 2014.
World Health Organization. Programming strategies for postpartum family planning 2013.
Kantorová V, et al. Estimating progress towards meeting women’s contraceptive needs in 185 countries: a bayesian hierarchical modelling study. PLoS Med. 2020;17(2):e1003026.
Marcolino C, Galastro EP. Males’ and females’ views on women’s and men’s participation in family planning. Rev Latinoam Enferm. 2001;9(3):77–82.
Moreira LR, et al. Reasons for nonuse of contraceptive methods by women with demand for contraception not satisfied: an assessment of low and middle-income countries using demographic and health surveys. Reproductive Health. 2019;16:1–5.
Dingeta T, et al. Low contraceptive utilization among young married women is associated with perceived social norms and belief in contraceptive myths in rural Ethiopia. PLoS ONE. 2021;16(2):e0247484.
Clements S, Madise N. Who is being served least by family planning providers? A study of modern contraceptive use in Ghana, Tanzania and Zimbabwe. African journal of reproductive health. Aug. 2004;1:124–36.
Central Statistical Agency - CSA/Ethiopia. and ICF. Ethiopia Demographic and Health Survey 2016. 2017, CSA and ICF: Addis Ababa, Ethiopia.
Tesfay F, Mesfin E, Gedefaw A. Resumption of Postpartum sexual intercourse and use of modern contraceptive among In-Union women in Addis Ababa: Cross Sectional Study. Ethiop J Reproductive Health. 2018;10(1):13.
Mekonnen BD, Gelagay AA, Lakew AM. Time to use modern contraceptives and associated factors among women in extended postpartum period in Gondar City, Northwest Ethiopia. Fam Med Med Sci Res. 2020;9(243):10–2147.
Gizaw W, et al. Extended postpartum modern contraceptive utilization and associated factors among women in Gozamen district, East Gojam Zone, northwest Ethiopia, 2014. Insights Reprod Med. 2017;1(2):8.
World Health Organization. Medical eligibility criteria for contraceptive use. World Health Organization; 2010.
Lee BX, et al. Transforming our world: implementing the 2030 agenda through sustainable development goal indicators. J Public Health Policy. 2016;37:13–31.
Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Global Health: Science and Practice. 2016;4(2):191–210.
Dona A, et al. Timely initiation of postpartum contraceptive utilization and associated factors among women of child bearing age in Aroressa District, Southern Ethiopia: a community based cross-sectional study. BMC Public Health. 2018;18(1):1–9.
Vernon R. Meeting the family planning needs of postpartum women. Stud Fam Plann. 2009;40(3):235–45.
Bearak et al. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a bayesian hierarchical model. Lancet Glob Health 2018 April; 6(4): e380–9.
Exavery, et al. Predictors of mistimed, and unwanted pregnancies among women of childbearing age in Rufiji, Kilombero, and Ulanga districts of Tanzania. Reproductive Health. 2014;11:63.
Ahinkorah BO. Individual and contextual factors associated with mistimed and unwanted pregnancies among adolescent girls and young women in selected high fertility countries in sub-saharan Africa: a multilevel mixed effects analysis. PLoS ONE. 2020;15(10):e0241050.
Bekele GG, et al. Time to initiate postpartum modern contraceptives among pregnant women in Ambo Town, Central Ethiopia; Cox-proportional hazard regression analysis. Contracept Reproductive Med. 2022;7(1):26.
Ahmed M, Seid A. Survival time to modern contraceptive uses from the resumption of sexual intercourse among postpartum women in Ethiopia. Int J Women’s Health 2020 Aug 19:641–7.
Wamala R, Kabagenyi A, Kasasa S. Predictors of time-to-contraceptive use from resumption of sexual intercourse after birth among women in Uganda International Journal of Population Research, 2017. 2017.
The American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. Female age-related Fertility Decline Fertility and Sterility. 2014;101(3):633–4.
Ajayi AI, Adeniyi OV, Akpan W. Use of traditional and modern contraceptives among childbearing women: findings from a mixed methods study in two southwestern Nigerian states. BMC Public Health. 2018;18:1–9.
Oumer M, Manaye A, Mengistu Z. Modern contraceptive method utilization and associated factors among women of reproductive age in Gondar City, Northwest Ethiopia. Open Access Journal of Contraception 2020 Jun 24:53–67.
Wai MM, Bjertness E, Htay TT, Liabsuetrakul T, Myint AN, Stigum H, Sundby J. Dynamics of contraceptive use among married women in North and South Yangon, Myanmar: findings from a cross-sectional household survey. Contraception: X. 2020;2:100015.
Ayele DG. Determinants of fertility in Ethiopia. Afr Health Sci. 2015;15(2):546–51.
Tsegaw M, Mulat B, Shitu K. Modern contraceptive utilization and Associated factors among Married women in Liberia: evidence from the 2019 Liberia Demographic and Health Survey. Open Access Journal of Contraception 2022 Feb 15:17–28.
Gubhaju B. The influence of wives’ and husbands’ education levels on contraceptive method choice in Nepal, 1996–2006. International Perspectives on Sexual and Reproductive Health. 2009 Dec 1:176 – 85.
Gebrehiwot SW, Azeze GA, Robles CC, Adinew YM. Utilization of dual contraception method among reproductive age women on antiretroviral therapy in selected public hospitals of Northern Ethiopia. Reproductive Health. 2017;14(1):1–9.
Grabert BK, et al. Couple communication and contraception use in urban Senegal. SAGE Open Medicine. 2021;9:20503121211023378.
Challa S, Shakya HB, Carter N, Boyce SC, Brooks MI, Aliou S, Silverman JG. Associations of spousal communication with contraceptive method use among adolescent wives and their husbands in Niger. PLoS ONE. 2020;15(8):e0237512.
Gejo NG, Anshebo AA, Dinsa LH. Postpartum modern contraceptive use and associated factors in Hossana town. PLoS ONE. 2019;14(5):e0217167.
Abraha TH, Teferra AS, Gelagay AA. Postpartum modern contraceptive use in northern Ethiopia: prevalence and associated factors. Epidemiol Health. 2017;39:e2017012.
Council for International Organizations of Medical Sciences. International ethical guidelines for biomedical research involving human subjects. Bull Med Ethics. 2002;(182):17–23.
Acknowledgements
We are very much thankful to study participants, data collectors, and supervisors for their participation.
Funding
This study was sponsored by Wachemo University. The funders had no any contribution in collecting, analyzing or writing the paper except the financial support.
Author information
Authors and Affiliations
Contributions
EA.M,DE.M,TA.L, BH.J and EA.T: initiate the study. EA.M,DE.M,TA.L, BH.J and EA.T: involved in designing the study, organizing data collection process, analysis and writing of the draft manuscript. All authors read and approved the final manuscript and have equal contribution.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted after the confirmation of national and international ethical guidelines for biomedical research involving human subjects [36]. Ethical approval was obtained from the Institutional Research Ethics Review Committee of Wachemo University. A formal letter was submitted to the Hadiya Zone Health Department, and permission was obtained from each health institution to conduct the study. A verbal, informed consent was obtained from the participants before the interview. The verbal, informed consent was approved by the Institutional Research Ethics Review Committee (IRERC) of Wachemo University (Hossana, Ethiopia) (Permission Number: 163/2015). The study participants were informed that their participation was on a voluntary basis and that they could withdraw from the interview at any time. They have also been informed that their withdrawal will not result in any harm or prohibit them from using the service at any time. The confidentiality was maintained at every step of the research by keeping anonymity; using codes rather than personal identifiers like names. All methods were carried out in accordance to the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mugoro, E.A., Mekango, D.E., Lule, T.A. et al. Time to initiation of modern contraceptive method use after childbirth and its predictors in Southern Ethiopia: a retrospective follow-up study. BMC Women's Health 23, 658 (2023). https://doi.org/10.1186/s12905-023-02809-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02809-y