Abstract
Background
The purpose of this systematic review and meta-analysis was to compile existing evidence on the significance of the NLR in predicting endometriosis in order to aid clinical decision-making and outcomes.
Methods
We searched ProQuest, Web of Science, and PubMed for related studies published before January 2, 2023. Standardized mean difference (SMD) with a 95% confidence interval (CI) was reported for each outcome. Because a significant level of heterogeneity was found, we used the random-effects model to calculate pooled effects. We used Newcastle-Ottawa Scale (NOS) for quality assessment.
Results
Overall, 18 article with were included in the analysis. A random-effect model revealed that patients with endometriosis had elevated levels of NLR compared to healthy controls (SMD = 0.79, 95% CI = 0.33 to 1.25, P < 0.001). Patients with endometriosis had elevated levels of NLR compared to those with other benign tumors (SMD = 0.85, 95% CI = 0.17 to 1.53, P = 0.014). In addition, NLR level of patients with stage III and IV endometriosis was not different from that of patients with stage I and II endometrioma (SMD = 0.30, 95% CI = -0.14 to 0.74, P = 0.18). However, NLR level was not different between endometriosis patients with and without peritoneal lesions (SMD = -0.12, 95% CI = -0.34to 0.10, P = 0.28), between patients with and without endometrioma (SMD = 0.20, 95% CI = -0.15 to 0.55, P = 0.26) and between endometriosis patients with and without deep lesions (SMD = 0.04, 95% CI = -0.20 to 0.28, P = 0.72). The pooled sensitivity of NLR was 0.67 (95% CI = 0.60–0.73), and the pooled specificity was 0.68 (95% CI, 0.62–0.73).
Conclusions
NLR might be utilized in clinics as a possible predictor to help clinicians diagnose endometriosis in affected women.
Similar content being viewed by others
Background
The existence of endometrial tissue outside the uterine cavity is known as endometriosis. In the general population, endometriosis is thought to affect 10 to 15% of people, and it may affect up to 70% of women who have chronic pain in the pelvic region [1,2,3]. Endometriosis patients often have infertility and dysmenorrhea, drastically reducing their quality of life [2]. Yet, there is not a uniform approach in dealing with these symptoms, and the illness can recur even after undergoing appropriate surgical procedures or using medications [4, 5]. Notably, surgery can be conceptualized as a cytoreductive approach aimed at eradicating the condition, yet endometriosis recurrence remains plausible. Conversely, medical treatment works by suppressing endometriosis. In a similar yet distinct manner, if medical treatment is stopped, the illness might become active again [6].
However, even when assisted reproductive technology (ART) enables a pregnancy, the profound emotional distress associated with infertility persists, particularly when considering the challenging hormonal therapies women undergo [7, 8]. Gynecological ailments like endometriosis might contribute to the emergence of anxiety and depression in these women [9]. Nonetheless, the comprehensive ART route can amplify substantial psychological distress for both genders, particularly in scenarios marked by iterative disappointments [10]. The particular medical conditions that hinder the occurrence of spontaneous pregnancy can serve as targeted psychological risk elements, shaping the paths of individual and couple development. These challenges encompass issues like anxiety and depressive disorders, and tendencies toward self-blame [11, 12]. Additionally, the sexual life of women is adversely affected [13].
There is significant patient diversity regarding illness phenotype and related symptom severity. Although abnormally high levels of estrogen and chronic inflammation are prominent symptoms of endometriosis, the underlying cause of the illness remains unclear [1]. This is due to the disease's multifactorial and complex character, which has already been linked to hormonal, genetic, immunological, and environmental variables [14]. Understanding the pathogenesis of endometriosis and attempting to avoid it, is one of the primary issues of contemporary gynecology. The most generally acknowledged explanation of endometrial lesion development to date is that while menstruation, cells and tissues of endometrium retract into the fallopian tubes and attach to the structures of the pelvic, resulting in discomfort, fibrosis, and also an inflammatory response [15,16,17,18]. Numerous inflammatory indicators, such as interleukins, neutrophils, and neutrophil to lymphocyte ratio (NLR), are raised in severe endometriosis because of the chronic inflammatory course of the disease [19,20,21]. In particular, the NLR has been suggested as a straightforward and practical prognostic and diagnostic biomarker for several illnesses [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. Without early management and a precise diagnosis, endometriosis may become an emerging gynecological problem and cause infertility and dysmenorrhea.
As new studies on NLR's utility in endometriosis accumulate, a systematic review to assist clinical decision-making is necessary. The goal is to comprehend what an increased ratio means for a patient with endometriosis in order to implement early therapies and enhance outcomes. As far as we know, there are no systematic reviews on using NLR in this setting in the available literature. The purpose of this systematic review and meta-analysis was to compile existing evidence on the significance of the NLR in predicting endometriosis in order to aid clinical decision-making and outcomes.
Materials and methods
Search strategy, eligibility criteria, and study selection
The keywords "endometriosis," "NLR," and "neutrophil to lymphocyte ratio" were used in combination to perform a thorough search of articles in online databases like Web of Science, PubMed, and ProQuest from their establishment before January 2, 2023. Two researchers independently evaluated the relevancy of abstracts. Then, they separately reviewed the full texts of the relevant articles. The following were the requirements for eligibility: (1) evaluation of NLR; (2) comparison of endometriosis-affected and unaffected human participants; (3) cross-sectional or case–control design; and (4) full-text publications.
The references of the retrieved publications and reviews were also examined to discover further related articles. A third researcher arbitrated any disagreements that arose between the reviewers. To rate the quality of each research, we employed the Newcastle–Ottawa scale (NOS). The NOS assessed the following elements: selection of the cohort, and comparability of groups.
Statistical analysis
Standardized mean differences (SMDs) were employed to compare NLR levels between healthy controls and patients with endometriosis and also to create forest plots of continuous data. Statistical significance was defined as p < 0.05, and 95% confidence intervals (CIs) were reported. The mean and standard deviation values were extrapolated from the median and IQR/range values in three studies, as previously explained [40].
The Q statistic was used to assess the heterogeneity of SMD across studies (significance level at p < 0.10). Additionally, the I2 statistic, a quantitative indicator of study inconsistency, was calculated. I2 values below 25%, between 25 and 50%, between 50 and 75%, and above 75% indicated no heterogeneity, moderate, high, and extreme heterogeneity, respectively. Since there was substantial heterogeneity, the pooled SMD and corresponding 95% confidence intervals were calculated using a random-effects model.
The command "metandi" was used to calculate the diagnostic odds ratio (DOR), pooled specificity, specificity, positive likelihood ratio, and negative likelihood ratio. A summary receiver operating characteristic (SROC) curve was also developed.
To assess the existence of possible publication bias, the relationships between the size of the study and the magnitude of effect were assessed using Egger's regression asymmetry test at the p < 0.05 level of significance. Stata 14 was used for statistical analysis (STATA Corp., College Station, TX, USA). Last but not least, our research complied completely with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results
Search results and included studies
In the initial search, we found a total of 272 results, and among them, 18 papers were included after multiple stags of screening [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39], shown in Fig. 1.
Characteristics of the population and quality assessment
In total, 18 articles were included in the analysis [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39], including 2507 patients with endometriosis and 2179 healthy controls. Seventeen of the included studies compared patients with endometriosis with healthy controls [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36, 38, 39], five of them compared patients with endometriosis and those with other benign tumors [25, 26, 29, 34, 38], three of them compared endometriosis patients with and without deep lesions [30, 31, 37], two of them compared endometriosis patients with and without peritoneal lesions [31, 37], four study compared endometriosis patients with and without endometrioma [30, 31, 37, 39], and four studies compared patients with stage III and IV endometriosis with those with stage I and II endometrioma [31, 32, 36, 37]. Six studies conducted receiver operating characteristic (ROC) curve analysis [25, 26, 32, 35, 36, 38]. Four of them were prospective [28, 29, 31, 32] and others were retrospective. Five of them were on East Asian patients [23,24,25, 29, 38] and others were on Caucasian patients. Check out Table 1 for overall characteristics and quality scores of the included articles. Table 2 shows the exclusion criteria of included studies.
Differences in NLR Level between patients with endometriosis and healthy controls
Patients with endometriosis had elevated levels of NLR compared to healthy controls (SMD = 0.79, 95% CI = 0.33 to 1.25, P < 0.001, Fig. 2).
In the subgroup analysis according to study design, we found that patients with endometriosis had elevated levels of NLR compared to healthy controls in retrospective studies (SMD = 0.75, 95% CI = 0.20 to 1.31, P = 0.007), but not in prospective studies (SMD = 0.90, 95% CI = -0.21 to 2.00, P = 0.11, Fig. 3).
In the subgroup analysis according to ethnicity, we found that NLR is higher in patients with endometriosis compared to healthy controls among either East Asian (SMD = 1.61, 95% CI = 0.31 to 2.91, P = 0.015) or Caucasian (SMD = 0.39, 95% CI = 0.19 to 0.59, P < 0.001) ethnicity (Fig. 4).
Differences in NLR Level between patients with endometriosis and other benign tumors
Patients with endometriosis had elevated levels of NLR compared to those with other benign tumors (SMD = 0.85, 95% CI = 0.17 to 1.53, P = 0.014, Fig. 5).
In the subgroup analysis according to study design, we found that patients with endometriosis had elevated levels of NLR compared to those with other benign tumors in prospective study (SMD = 1.72, 95% CI = 1.35 to 2.09, P < 0.001), but not in retrospective studies (SMD = 0.64, 95% CI = -0.15 to 1.42, P = 0.11, Fig. 6).
In the subgroup analysis according to ethnicity, we found that NLR is higher in patients with endometriosis compared to those with other benign tumors among East Asian ethnicity (SMD = 1.44, 95% CI = 1.01 to 1.87, P < 0.001), but not among Caucasian (SMD = -0.10, 95% CI = -1.88 to 1.68, P = 0.91) ethnicity (Fig. 7).
Differences in NLR Level between patients with different types of endometriosis
There were not any differences in NLR levels between endometriosis patients with and without deep lesions (SMD = 0.04, 95% CI = -0.20 to 0.28, P = 0.72, Fig. 8).
NLR level was not different between endometriosis patients with and without peritoneal lesions (SMD = -0.12, 95% CI = -0.34to 0.10, P = 0.28, Fig. 9).
NLR level was not different between endometriosis patients with and without endometrioma (SMD = 0.20, 95% CI = -0.15 to 0.55, P = 0.26, Fig. 10).
Differences in NLR Level between patients with different stages of endometriosis
NLR level of patients with stage III and IV endometriosis was not different from that of patients with stage I and II endometrioma (SMD = 0.30, 95% CI = -0.14 to 0.74, P = 0.18, Fig. 11).
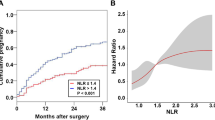
Diagnostic value of NLR in endometriosis
The pooled sensitivity was 0.67 (95% CI = 0.60–0.73), and the pooled specificity was 0.68 (95% CI, 0.62–0.73). The pooled positive likelihood ratio, negative likelihood ratio, diagnostic odds ratio (DOR) of NLR were 2.13(95%CI = 1.67–2.73),0.47 (95%CI = 0.37–0.61), and 2.09 (95%CI = 1.63–2.68), respectively (Fig. 12).
Publication bias
There was no significant publication bias among studies on either differences in NLR levels between patients with endometriosis and heathy controls (Egger test P = 0.38, Fig. 13A) or differences in NLR levels between patients with endometriosis and those with other benign tumors (Egger test P = 0.42, Fig. 13B).
Discussion
Three key conclusions emerged from our investigation. First, endometriosis patients had significantly higher NLR levels compared to healthy controls. Second, endometriosis patients of Caucasian and East Asian ethnicity exhibited higher NLR levels than healthy controls. Third, patients with endometriosis exhibited higher levels of NLR than those with other benign tumors. Appreciating the dynamic functions that neutrophils and lymphocytes play in the context of endometriosis is crucial to fully grasp the relevance of their relative proportions. A higher NLR has been reported in endometriosis patients compared to controls because of an elevation in neutrophil count and a reduction in lymphocyte count.
Infertility, pelvic discomfort, and other symptoms experienced by endometriosis patients have a negative impact on their quality of life [41, 42]. Endometriosis is a highly intricate condition that has a substantial effect on the psychological well-being, quality of life, and interpersonal connections of affected women [43, 44]. The symptoms of endometriosis gradually hinder a woman's capability to perform certain daily tasks, leading to a perception of deteriorating overall health status and well-being [45]. The repercussions of these symptoms have been incompletely explored, and additional research and clinical expertise are required to gain a comprehensive understanding of the scope of this condition. Studies have indicated that endometriosis is linked to significant direct and indirect expenses, on par with major chronic diseases like diabetes [45]. Furthermore, symptoms related to endometriosis significantly disrupt the employment of affected women, often leading to missed workdays in numerous cases [45]. New data indicates that approximately half of women who experience infertility may be affected by endometriosis [44]. The illness can impact fertility by modifying gamete transport, tuba-ovarian function, endometrial receptivity, and triggering inflammatory characteristics in peritoneal fluid, which in turn leads to changes in function and quality of sperms [46,47,48,49,50]. Research on oocyte donation indicates a negative impact on oocytes rather than endometrial receptivity [51]. Alongside the qualitative influence on oocytes, a quantitative decline in ovarian reserve is also a concern for women afflicted with endometriosis [52].
Significant reductions in ovarian reserve lead to unfavorable reproductive outcomes following in vitro fertilization (IVF) [53,54,55]. The current therapeutic approaches are far from being curative [10, 11]. Fertility preservation (FP) provides women at risk of age-related fertility decline with the opportunity of bearing children in the future using their own gametes [56]. A recent comprehensive study, the largest of its kind, presents successful outcomes achieved through oocyte vitrification for both elective FP and FP in cancer patients, while also identifying factors contributing to success [57]. Endometriosis indeed contributes to diminishing the ovarian reserve, thereby making women diagnosed with the condition increasingly eligible candidates for FP [58,59,60]. Currently, oocyte vitrification stands as an effective choice for elective FP in reproductive-aged women [61, 62]. In cases involving women diagnosed with endometriosis, this method additionally boasts the advantage of being relatively minimally invasive and lacking detrimental effects on ovarian reserve [59, 60].
Late diagnosis and high recurrence rates are characteristics of endometriosis [63, 64]. Although laparoscopy is the gold standard for diagnosing endometriosis, it is probably missed in cases with severe pelvic adhesions and atypical, extraperitoneal, minor lesions. Furthermore, laparoscopy has a significant risk of complications and is an expensive procedure [65]. Therefore, identifying suitable early non-invasive diagnostic markers and minimizing needless intervention methods are of significant clinical importance, and this is where NLR steps in to help.
NLR, SII, platelet-to-lymphocyte ratio (PLR), and monocyte-to-lymphocyte ratio (MLR) have been shown to correlate with endometriosis so that they might be employed as hematological markers for endometriosis diagnosis [66,67,68]. While using NLR for endometriosis diagnosis, the variations of this biomarker in menstrual period should be taken into account. Menstruation exhibits many features of an inflammatory process [69] and NLR as a marker of inflammation can be increased in these circumstances. In this investigation, we discovered that NLR was higher in patients with endometriosis than in healthy controls, which may properly represent the inflammatory state in endometriosis patients.
Endometriosis has been linked to a greater incidence of autoimmune inflammatory disorders (like asthma and allergy) and increased inflammatory activity [70]. This disease may develop due to high quantities of inflammatory chemokines, cytokines, and prostaglandins in the peritoneal microenvironment of endometriosis-affected women [70]. There is increasing proof that women with endometriosis have altered levels of specific subtypes of white blood cells and alternations in peritoneal fluid, endometrial and peripheral blood [71, 72]. Tokmak et al. discovered WBC alterations in endometriosis patients, including an increased neutrophil and a reduced lymphocyte count, and they validated the existence of a chronic inflammatory state in these patients [35].
These results revealed that inflammation could play a role in the development of endometriosis. TNF-alpha was one of several inflammatory cytokines that many researchers investigated. Scholl et al. [73] discovered that TNF-alpha contributes to endometriosis, and another study indicated that TNF-alpha expression was elevated in the endometriosis patients' tissues [74]. TNF-alpha may thus have a significant role in the inflammatory component of endometriosis. By starting or maintaining inflammatory reactions in the peritoneal cavity, IL-16 may also contribute to the pathogenesis of endometriosis [75]. In both luteal and proliferative biopsies, endometriosis-affected women had higher levels of chemotactic activity in macrophages, neutrophils, and inflammatory cells compared to healthy women [76]. Anti-inflammatory drugs have been evaluated as the significance of inflammation in endometriosis became clear. Mariani et al. [77] discovered that elocalcitol, a selective agonist of the vitamin D receptor, may slow the development of endometriosis in an animal model. LXA4 may inhibit the development of endometriosis in the mouse model by reducing inflammation [78].
Since inflammation is involved in endometriosis and it is acknowledged that NLR is an indicator of systemic inflammation, it may be appropriate to employ this inflammatory ratio as a diagnostic biomarker for endometriosis. However, understanding the functions of neutrophils and lymphocytes in endometriosis is necessary to offer a thorough justification for using NLR as a prognostic biomarker.
One of the important parts of innate immunity are neutrophils, which release pro-inflammatory cytokines like IL-8, vascular endothelial growth factor (VEGF), and CXCL10, which could contribute to disease progression [79,80,81]. Neutrophils are involved in almost all inflammatory disorders, ranging from autoimmune, acute, chronic, infectious, and non-infectious diseases [82]. Numerous investigations have revealed that neutrophils have a role in endometriosis pathogenesis [79, 83]. Regarding endometriosis, higher numbers of neutrophils have been identified in patients compared to those without the condition [84, 85]. This is most likely the consequence of elevated levels of chemotactic elements such as IL-8, human neutrophil peptide (HNP1-3), and epithelial neutrophil-activating peptide (ENA-78) [86]. It is interesting to note that estrogens have been demonstrated to affect neutrophil function [87]. It has not been confirmed yet if this characteristic plays a part in endometriosis pathogenesis. In an animal model's early phases of endometriosis, the dominancy of neutrophil infiltration into ectopic uterine tissue was observed [88, 89]. These cells' primary function is to cause inflammation by releasing IL-17A, which can promote the migration of neutrophils or other pro-inflammatory mediators such as VEGF, IL-8, and CXCL10 [83]. Recent animal research on endometriosis mice revealed that depleting neutrophils using an anti-Gr-1 antibody decreased lesion formation [90]. In this investigation, neutrophil depletion decreased the formation of the lesion in the early but not late stages of disease progression, indicating that neutrophils are required for the initial endometriosis formation [90].
T and B lymphocytes are crucial adaptative immune subsets involved in the proliferation and survival of endometrial cells. Furthermore, endometriosis is characterized by a decrease in the function of cytotoxic T lymphocytes and in the secretion of cytokines by T helper cells, and also synthesis of autoantibodies by B cells [91, 92]. Here we will discuss the role of each type of lymphocyte in endometriosis one by one.
There are several studies on the role of cellular response in endometriosis, and various features are noteworthy. Since endometriosis patients had higher quantities of cytokines indicative of Th2 lymphocytes in their peritoneal fluid and plasma, the illness was described as polarizing towards this specific cellular response [93, 94]. The normal Th2 response, which is biologically linked to healing and fibrosis, has not been thoroughly studied in the context of endometriosis [95]. The relative preponderance of Th1 cells in peripheral blood makes it difficult to interpret investigations. The CD4/CD8 ratio and the quantity of each type of cell were shown to be greater in the peritoneal fluid of affected women [96]. T-cell counts in endometrial lesions were higher than in eutopic endometrium; however, the CD4/CD8 ratio was similar.
Peripheral blood revealed no alterations [97, 98]. In contrast, Abramiuk et al.'s research showed no significant differences in the overall number of lymphocytes but a decline in the proportion of CD8 + T cells in peripheral blood [79]. Moreover, it has been discovered that the proportion of Th17 cells in a patient's peritoneal fluid increases with the illness stage [99]. It has also been shown that the endometriotic environment has higher quantities of IL-17. By promoting the generation of cytokines that cause inflammation and angiogenesis, this interleukin could accelerate the progression of endometriosis [100, 101]. Regulatory T cells, a subset of lymphocytes engaged in the cellular response, also have a crucial role in endometriosis. Although their part in the emergence of endometriosis is yet unknown, they theoretically serve a regulatory role and are implicated in the tolerance of immune cells. According to the authors of new research, there are more regulatory T cells in the patient's peritoneal fluid, which may be related to local immunosuppression that prevents the removal of ectopic endometrial cells [79]. Hanada et al. discovered a larger proportion of Treg in patients' peritoneal fluid while finding no differences in peripheral blood compared to controls [97]. Olkowska-Truchanowicz et al. provided similar findings, evaluating the percentages of CD25 + CD4 + Foxp3 + T cells in peripheral blood, which were identical to Takamura et al. [102, 103]. Another study also showed no variations in the proportion of regulatory T cells with the CD25 + CD4 + Foxp3 + phenotype in peripheral blood, indicating that their involvement is restricted to a local impact [79].
Endometriosis has long been assumed to be an autoimmune disease. Several studies demonstrated the existence of anti-endometriosis antibodies in the peritoneal fluid and serum of individuals with the condition [104, 105]. Although autoantibodies are hypothesized to promote the progression of endometriosis by sustaining inflammation and activating the immune system, there is no solid proof to back up this theory [79]. The presence of autoantibodies in patients with endometriosis is further exacerbated by comorbidities. The emergence of autoimmune and immunological disorders like psoriasis, rheumatoid arthritis, and allergies are related to endometriosis [106, 107]. The existence of autoantibodies led researchers to look into the function of B lymphocytes in the endometriosis pathophysiology [79]. Most investigations in a meta-analysis on this matter imply a connection between endometriosis and elevated percentages or stimulation of B lymphocytes. There were no variations in the numbers of B cells between patients and controls in 7 of the 22 included publications [108]. B cells also secrete cytokines like IL-6 and IL-17, which have been demonstrated to influence immunological cells like CD4 + T cells and sustain chronic inflammation [108]. Endometriosis is also related to these cytokines [86, 109, 110]. Therefore, in endometriosis, B lymphocytes may contribute to local and systemic cytokine production and inflame their microenvironment [79]. Therefore, further research is required to completely comprehend the role of B lymphocytes and their interactions with other immune cells in endometriosis disease.
The NK cell provides a connection between the adaptive and innate immune responses. Oosterlynck et al. were the first to define the role of natural killer (NK) cells in the pathophysiology of endometriosis by demonstrating that NK cell cytotoxic effect was decreased when faced with ectopic endometrial cells. This association correlated with advanced phases of the illness [89, 109, 111]. The reason behind the decreased function of NK cells in endometriosis is not fully understood. Numerous inhibitory and activating receptors were found to be abnormally expressed on their surface when compared to these cells in normal women [112,113,114,115]. This may be explained by the enhanced expression of KIR (killer cell immunoglobulin-like receptors) that has been detected in the peritumoral NK cells [116]. Chronic inflammation caused by the disease may lead to the aberrant function of NK cells [117, 118]. By removing cells that exhibit autoantigens, NK cells help maintain the balance of immunological tolerance. As a result, their decreased activity in endometriosis may account for the higher frequency of autoimmunity witnessed in the condition [119]. It has been shown that the presence of IL-6 and TGF-β in the peritoneal fluid of endometriosis-affected women decreases the cytolytic ability of NK cells [120, 121]. Furthermore, it has been shown that IL-15, which is significantly produced on endometrial stromal cells at the ectopic site, inhibits NK cell activity in vitro [122]. It was discovered that macrophages and endometrial cells interacted to lessen NK cell cytotoxicity, possibly by releasing more IL-10 and TGF-β [123].
Strength and limitations
There are multiple features to the current meta-analysis. First, this is the first meta-analysis of the association between NLR levels and endometriosis. We discovered that patients with endometriosis had significantly higher NLR levels than healthy controls according to the pooled analysis. Furthermore, the results of subgroup analyses were mainly consistent with the main results of the study, indicating that our findings were plausible. Second, when pooling effect estimates, we employed the random-effects model, a more conservative strategy that improved the accuracy of our meta-analysis findings. Third, the publication date and language constraints were not limited for the literature search, reducing the possibility of publication bias in the findings of our study. Fourth, the majority of the included studies excluded patients with coexisting lesions, such as endometrial hyperplasia, endometrial polyp, adenomyosis, myoma uteri, gynecological, and it could strength our results. In addition, it has been reported that the level of inflammatory markers may rise in some systemic disorders and it could affect the findings. However, the majority of the included articles excluded the patients with diseases affecting inflammatory markers, including hematological disorders, acute or chronic infectious, hepatic insufficiency, renal dysfunction, steroid therapy, inflammatory diseases, or malignancies. Obviously, this exclusion criterion among included studies could increase the validity our results substantially.
There are some limitations that should be addressed. The majority of the patients are from Asia, and this could be a bias. In other words, the sample was almost representative of the Asian population but would tend to miss people from other continents. Further studies are needed to determine the association between NLR and endometriosis in other continents. Although we found that there was no association between NLR and grade and degree of migration of endometriosis, these results need to interpreted with caution because of limited number of included studies. More research on this topic needs to be undertaken before the relationship between NLR and grade and degree of migration of endometriosis is more clearly understood. In addition, we could not compare the NLR level before and after treatment of endometriosis, due to the lack of original studies on this context. further studies, which take these variables into account, will need to be undertaken.
Conclusion
The results of this systematic review and meta-analysis demonstrate the significantly higher levels of NLR in patients with endometriosis compared to healthy controls. As a result, NLR might be utilized in clinics as a possible predictor to help clinicians diagnose endometriosis in women. Additional research is required to carry out a meta-analysis with a greater number of included publications in order to obtain more precise findings.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
- NLR:
-
Neutrophil to lymphocyte ratio
- NOS:
-
Newcastle-Ottawa scale
- DOR:
-
Diagnostic odds ratio
- SROC:
-
Summary receiver operating characteristic
- ROC:
-
Receiver operating characteristic
- PLR:
-
Platelet-to-lymphocyte ratio
- MLR:
-
Monocyte-to-lymphocyte ratio
- VEGF:
-
Vascular endothelial growth factor
- HNP1-3:
-
Human neutrophil peptide
- ENA-78:
-
Epithelial neutrophil-activating peptide
- NK:
-
Natural killer
- KIR:
-
Killer cell immunoglobulin-like receptors
References
Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364(9447):1789–99.
Parasar P, Ozcan P, Terry KL. Endometriosis: epidemiology, diagnosis and clinical management. Curr Obstet Gynecol Rep. 2017;6(1):34–41.
Smycz-Kubańska M, Kondera-Anasz Z, Sikora J, Wendlocha D, Królewska-Daszczyńska P, Englisz A, et al. The role of selected chemokines in the peritoneal fluid of women with endometriosis—participation in the pathogenesis of the disease. Processes. 2021;9(12):2229.
D’Alterio MN, Saponara S, D’Ancona G, Russo M, Laganà AS, Sorrentino F, et al. Role of surgical treatment in endometriosis. Minerva Obstet Gynecol. 2021;73(3):317–32.
Laganà AS, La Rosa VL. Multidisciplinary management of endometriosis: current strategies and future challenges. Minerva Med. 2019;111(1):18–20.
Habib N, Buzzaccarini G, Centini G, Moawad G, Ceccaldi P-F, Gitas G, et al. Impact of lifestyle and diet on endometriosis: a fresh look to a busy corner. Menopause Review/Prz Menopauzalny. 2022;21(2):124–32.
Burgio S, Polizzi C, Buzzaccarini G, Laganà AS, Gullo G, Perricone G, et al. Psychological variables in medically assisted reproduction: a systematic review. Menopause Review/Prz Menopauzalny. 2022;21(1):47–63.
Peterson BD, Sejbaek CS, Pirritano M, Schmidt L. Are severe depressive symptoms associated with infertility-related distress in individuals and their partners? Hum Reprod. 2014;29(1):76–82.
Reis S, Xavier MR, Coelho R, Montenegro N. Psychological impact of single and multiple courses of assisted reproductive treatments in couples: a comparative study. Eur J Obstet Gynecol Reprod Biol. 2013;171(1):61–6.
Vitale SG, La Rosa VL, Rapisarda AMC, Lagana AS. Psychology of infertility and assisted reproductive treatment: the Italian situation. J Psychosom Obstet Gynecol. 2017;38(1):1–3.
Laganà A, La Rosa V, Rapisarda A, Vitale S. Reflections about the impact of infertility on female sexual function. Kathmandu Univ Med J. 2016;14(56):299–300.
Frederiksen Y, Farver-Vestergaard I, Skovgård NG, Ingerslev HJ, Zachariae R. Efficacy of psychosocial interventions for psychological and pregnancy outcomes in infertile women and men: a systematic review and meta-analysis. BMJ Open. 2015;5(1):e006592.
Udry-Jørgensen L, Darwiche J, Germond M, Wunder D, Vial Y. Anxiety, depression, and attachment before and after the first-trimester screening for Down syndrome: comparing couples who undergo ART with those who conceive spontaneously. Prenat Diagn. 2015;35(13):1287–93.
Parazzini F, Esposito G, Tozzi L, Noli S, Bianchi S. Epidemiology of endometriosis and its comorbidities. Eur J Obstet Gynecol Reprod Biol. 2017;209:3–7.
Sampson J. Endometriosis peritoneal debida a la diseminación menstrual del tejido endometrial hacia la cavidad peritoneal. Rev Am Obstet Ginecol. 1927;14:422–69.
Tavoli Z, Asgari Z, Afshari F, Tabatabaei F, Montazeri A. Recurrence rate of endometrioma after laparoscopic bilateral cystectomy and unilateral cystectomy and drainage in opposite side. Iran J Obstet Gynecol Infertil. 2020;23(3):19–25.
Asgari Z, Tavoli Z, Hosseini R, Nataj M, Tabatabaei F, Dehghanizadeh F, et al. A comparative study between transcutaneous electrical nerve stimulation and fentanyl to relieve shoulder pain during laparoscopic gynecologic surgery under spinal anesthesia: a randomized clinical trail. Pain Res Manag. 2018;2018:9715142.
Zahraasgari FT, Hosseini R, Tavoli Z, Moini A, Zebardast J, Montazeri A. Ovarian reserve after laparoscopic salpingectomy compared with laparoscopic Salpingotomy in patients with tubal ectopic pregnancy. Acta Medica. 2019;35:967.
Jiang L, Yan Y, Liu Z, Wang Y. Inflammation and endometriosis. Front Biosci Landmark. 2016;21(5):941–8.
Kokot I, Piwowar A, Jędryka M, Sołkiewicz K, Kratz EM. Diagnostic significance of selected serum inflammatory markers in women with advanced endometriosis. Int J Mol Sci. 2021;22(5):2295.
Tavoli Z, Tabatabaei F, Zebardast J, Montazeri A. Are measuring CA-125 and RDW in stage III and IV endometriosis helpful for operative planning. Med Sci. 2019;23(99):694–9.
Biyik I, Keskin F, Nagihan S. The role of monocyte to high-density lipoprotein cholesterol ratio in prediction of increased systemic inflammation and the risk of cardiovascular disease in endometriosis. J Exp Clin Med. 2021;38(2):106–10.
Chen T, Wei JL, Leng T, Gao F, Hou SY. The diagnostic value of the combination of hemoglobin, CA199, CA125, and HE4 in endometriosis. J Clin Lab Anal. 2021;35(9):e23947.
Chen Z-Y, Zhang L-F, Zhang Y-Q, Zhou Y, Li X-Y, Huang X-F. Blood tests for prediction of deep endometriosis: a case-control study. World J Clin Cases. 2021;9(35):10805.
Cho S, Cho H, Nam A, Kim HY, Choi YS, Park KH, et al. Neutrophil-to-lymphocyte ratio as an adjunct to CA-125 for the diagnosis of endometriosis. Fertil Steril. 2008;90(6):2073–9.
Kalem Z, Şimşir Ç, Bakırarar B, Kalem MN. The additional diagnostic value of NLR and PLR for CA-125 in the differential diagnosis of endometrioma and benign ovarian cysts in women of reproductive age: a retrospective case-control study. Eur Res J. 2020;6(2):111–9.
Karadadas E, Hortu I, Ak H, Ergenoglu AM, Karadadas N, Aydin HH. Evaluation of complement system proteins C3a, C5a and C6 in patients of endometriosis. Clin Biochem. 2020;81:15–9.
Kedzia M, Osinski M, Mantaj U, Wender-Ozegowska E. Endometriosis is associated with an increased whole-blood thrombogenicity detected by a novel automated microchip flow-chamber system (T-TAS®). Ginekol Pol. 2023;94(4):291–7.
Li G, Yu Z, Li K. The value of FS, NLR, and CA-125 in the diagnosis of endometriosis. Int J Clin Exp Med. 2016;9(4):7309–13.
Moini A, Ghanaat M, Hosseini R, Rastad H, Hosseini L. Evaluating hematological parameters in women with endometriosis. J Obstet Gynaecol. 2021;41(7):1151–6.
Ottolina J, Bartiromo L, Dolci C, Salmeri N, Schimberni M, Villanacci R, et al. Assessment of coagulation parameters in women affected by endometriosis: validation study and systematic review of the literature. Diagnostics. 2020;10(8):567.
Sayan CD, Özakşit MG, Sarikaya E, Eryilmaz ÖG, Mollamahmutoğlu L, Deveer R. Serum interleukin-8, CA-125 levels, neutrophil-to-lymphocyte ratios, and combined markers in the diagnosis of endometriosis. Turkish J Med Sci. 2013;43(3):417–23.
Seckin B, Ates MC, Kirbas A, Yesilyurt H. Usefulness of hematological parameters for differential diagnosis of endometriomas in adolescents/young adults and older women. Int J Adolesc Med Health. 2021;33(2). https://doi.org/10.1515/ijamh-2018-0078.
Tas M. The value of the neutrophil to lymphocyte ratio, platelet to lymphocyte ratio and ca-125 in differential diagnosis of ovarian endometriosis. Medicine. 2019;8(4):782–5.
Tokmak A, Yildirim G, Öztaş E, Akar S, Erkenekli K, Gülşen P, et al. Use of neutrophil-to-lymphocyte ratio combined with CA-125 to distinguish endometriomas from other benign ovarian cysts. Reprod Sci. 2016;23(6):795–802.
Turgut A, Hocaoğlu M, Özdamar OI, Akın U, Günay T, Akdeniz E. Could hematologic parameters be useful biomarkers for the diagnosis of endometriosis? 2019.
Viganò P, Ottolina J, Sarais V, Rebonato G, Somigliana E, Candiani M. Coagulation status in women with endometriosis. Reprod Sci. 2018;25(4):559–65.
Yang H, Lang JH, Zhu L, Wang S, Sha GH, Zhang Y. Diagnostic value of the neutrophil-to-lymphocyte ratio and the combination of serum CA-125 for stages III and IV endometriosis. Chin Med J. 2013;126(11):2011–4.
Yavuzcan A, Çağlar M, Üstün Y, Dilbaz S, Özdemir İ, Yıldız E, et al. Evaluation of mean platelet volume, neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in advanced stage endometriosis with endometrioma. J Turk Ger Gynecolog Assoc. 2013;14(4):210.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:1–13.
D’Hooghe T, Hummelshoj L. Multi-disciplinary centres/networks of excellence for endometriosis management and research: a proposal. Hum Reprod. 2006;21(11):2743–8.
Yun BH, Lee YS, Chon SJ, Jung YS, Yim SY, Kim HY, et al. Evaluation of elevated urinary enolase I levels in patients with endometriosis. Biomarkers. 2014;19(1):16–21.
Vitale SG, La Rosa VL, Rapisarda AMC, Laganà AS. Impact of endometriosis on quality of life and psychological well-being. J Psychosom Obstet Gynecol. 2017;38(4):317–9.
La Rosa VL, Barra F, Chiofalo B, Platania A, Di Guardo F, Conway F, et al. An overview on the relationship between endometriosis and infertility: the impact on sexuality and psychological well-being. J Psychosom Obstet Gynecol. 2020;41(2):93–7.
La Rosa VL, De Franciscis P, Barra F, Schiattarella A, Török P, Shah M, et al. Quality of life in women with endometriosis: a narrative overview. Minerva Med. 2019;111(1):68–78.
Gupta S, Agarwal A, Agarwal R, de Mola JRL. Impact of ovarian endometrioma on assisted reproduction outcomes. Reprod Biomed Online. 2006;13(3):349–60.
Mansour G, Aziz N, Sharma R, Falcone T, Goldberg J, Agarwal A. The impact of peritoneal fluid from healthy women and from women with endometriosis on sperm DNA and its relationship to the sperm deformity index. Fertil Steril. 2009;92(1):61–7.
Matsuzaki S, Schubert B. Oxidative stress status in normal ovarian cortex surrounding ovarian endometriosis. Fertil Steril. 2010;93(7):2431–2.
Yoshida S, Harada T, Iwabe T, Taniguchi F, Mitsunari M, Yamauchi N, et al. A combination of interleukin-6 and its soluble receptor impairs sperm motility: implications in infertility associated with endometriosis. Hum Reprod. 2004;19(8):1821–5.
Young VJ, Brown JK, Saunders PT, Horne AW. The role of the peritoneum in the pathogenesis of endometriosis. Hum Reprod Update. 2013;19(5):558–69.
Simon C, Gutiérrez A, Vidal A, de los Santos MJ, Tarín JJ, Remohí J, et al. Outcome of patients with endometriosis in assisted reproduction: results from in-vitro fertilization and oocyte donation. Hum Reprod. 1994;9(4):725–9.
Seyhan A, Ata B, Uncu G, editors. The impact of endometriosis and its treatment on ovarian reserve. Seminars in reproductive medicine; Thieme Medical Publishers. 2015. https://pubmed.ncbi.nlm.nih.gov/26594869/, https://europepmc.org/article/med/26594869.
Lemos NA, Arbo E, Scalco R, Weiler E, Rosa V, Cunha-Filho JS. Decreased anti-Müllerian hormone and altered ovarian follicular cohort in infertile patients with mild/minimal endometriosis. Fertil Steril. 2008;89(5):1064–8.
Barnett R, Banks N, Decherney AH. Endometriosis and Fertility Preservation. Clin Obstet Gynecol. 2017;60(3):517–23.
Hamdan M, Dunselman G, Li T, Cheong Y. The impact of endometrioma on IVF/ICSI outcomes: a systematic review and meta-analysis. Hum Reprod Update. 2015;21(6):809–25.
Cobo A, García-Velasco JA. Why all women should freeze their eggs. Curr Opin Obstet Gynecol. 2016;28(3):206–10.
Cobo A, García-Velasco J, Domingo J, Pellicer A, Remohí J. Elective and onco-fertility preservation: factors related to IVF outcomes. Hum Reprod. 2018;33(12):2222–31.
Somigliana E, Viganò P, Filippi F, Papaleo E, Benaglia L, Candiani M, et al. Fertility preservation in women with endometriosis: for all, for some, for none? Hum Reprod. 2015;30(6):1280–6.
Carrillo L, Seidman D, Cittadini E, Meirow D. The role of fertility preservation in patients with endometriosis. J Assist Reprod Genet. 2016;33:317–23.
Streuli I, Benard J, Hugon-Rodin J, Chapron C, Santulli P, Pluchino N. Shedding light on the fertility preservation debate in women with endometriosis: a swot analysis. Eur J Obstet Gynecol Reprod Biol. 2018;229:172–8.
Gullo G, Perino A, Cucinella G. Open vs. closed vitrification system: which one is safer? Eur Rev Med Pharmacol Sci. 2022;26(4):1065–7.
Cobo A, Giles J, Paolelli S, Pellicer A, Remohí J, García-Velasco JA. Oocyte vitrification for fertility preservation in women with endometriosis: an observational study. Fertil Steril. 2020;113(4):836–44.
Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil Steril. 2006;86(5):1296–301.
Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, et al. The social and psychological impact of endometriosis on women’s lives: a critical narrative review. Hum Reprod Update. 2013;19(6):625–39.
Walter AJ, Hentz JG, Magtibay PM, Cornella JL, Magrina JF. Endometriosis: correlation between histologic and visual findings at laparoscopy. Am J Obstet Gynecol. 2001;184(7):1407–13.
Bullon P, Manuel NJ. Inflammasome as a key pathogenic mechanism in endometriosis. Curr Drug Targets. 2017;18(9):997–1002.
Jing X, Li C, Sun J, Peng J, Dou Y, Xu X, et al. Systemic inflammatory response markers associated with infertility and endometrioma or uterine leiomyoma in endometriosis. Ther Clin Risk Manag. 2020;16:403.
Kim HS, Choi H-Y, Lee M, Suh DH, Kim K, No JH, et al. Systemic inflammatory response markers and CA-125 levels in ovarian clear cell carcinoma: a two center cohort study. Cancer Res Treat. 2016;48(1):250–8.
Evans J, Salamonsen LA. Inflammation, leukocytes and menstruation. Rev Endocr Metab Disord. 2012;13:277–88.
Evsen M, Soydinc H, Sak M, Ozler A, Turgut A, Celik Y, et al. Increased platelet count in severe peritoneal endometriosis. Clin Exp Obstet Gynecol. 2014;41(4):423–5.
D’Hooghe TM, Nugent NP, Cuneo S, Chai DC, Deer F, Debrock S, et al. Recombinant human TNFRSF1A (r-hTBP1) inhibits the development of endometriosis in baboons: a prospective, randomized, placebo-and drug-controlled study. Biol Reprod. 2006;74(1):131–6.
Hooghe T, Hill J, Oosterlynck D, Koninckx P, Bambra C. Endometriosis: Effect of endometriosis on white blood cell subpopulations in peripheral blood and peritoneal fluid of baboons. Hum Reprod. 1996;11(8):1736–40.
Scholl B, Bersinger NA, Kuhn A, Mueller MD. Correlation between symptoms of pain and peritoneal fluid inflammatory cytokine concentrations in endometriosis. Gynecol Endocrinol. 2009;25(11):701–6.
Kuteken FS, Lancellotti CLP, Ribeiro HSAA, Aldrighi JM, Ribeiro PAAG. Expressão de mediadores neurotróficos e pró-inflamatórios na endometriose de reto e sigmoide. Rev Bras Ginecol Obstet. 2012;34:568–74.
Koga K, Osuga Y, Yoshino O, Hirota Y, Yano T, Tsutsumi O, et al. Elevated interleukin-16 levels in the peritoneal fluid of women with endometriosis may be a mechanism for inflammatory reactions associated with endometriosis. Fertil Steril. 2005;83(4):878–82.
Leiva MC, Hasty LA, Lyttle CR. Inflammatory changes of the endometrium in patients with minimal-to-moderate endometriosis. Fertil Steril. 1994;62(5):967–72.
Mariani M, Vigano P, Gentilini D, Camisa B, Caporizzo E, Di Lucia P, et al. The selective vitamin D receptor agonist, elocalcitol, reduces endometriosis development in a mouse model by inhibiting peritoneal inflammation. Hum Reprod. 2012;27(7):2010–9.
Xu Z, Zhao F, Lin F, Chen J, Huang Y. Lipoxin A 4 Inhibits the Development of Endometriosis in Mice: The Role of Anti-Inflammation and Anti-Angiogenesis. Am J Reprod Immunol. 2012;67(6):491–7.
Abramiuk M, Grywalska E, Małkowska P, Sierawska O, Hrynkiewicz R, Niedźwiedzka-Rystwej P. The role of the Immune System in the Development of Endometriosis. Cells. 2022;11(13):2028.
Kim JY, Lee DH, Joo JK, Jin JO, Wang JW, Hong YS, et al. Effects of Peritoneal Fluid from Endometriosis Patients on Interferon-γ-Induced Protein-10 (CXCL10) and Interleukin-8 (CXCL8) Released by Neutrophils and CD4+ T Cells. Am J Reprod Immunol. 2009;62(3):128–38.
Na Y-J, Yang S-H, Baek D-W, Lee D-H, Kim K-H, Choi Y-M, et al. Effects of peritoneal fluid from endometriosis patients on the release of vascular endothelial growth factor by neutrophils and monocytes. Hum Reprod. 2006;21(7):1846–55.
Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13(3):159–75.
Izumi G, Koga K, Takamura M, Makabe T, Satake E, Takeuchi A, et al. Involvement of immune cells in the pathogenesis of endometriosis. J Obstet Gynaecol Res. 2018;44(2):191–8.
Milewski Ł, Dziunycz P, Barcz E, Radomski D, Roszkowski PI, Korczak-Kowalska G, et al. Increased levels of human neutrophil peptides 1, 2, and 3 in peritoneal fluid of patients with endometriosis: association with neutrophils, T cells and IL-8. J Reprod Immunol. 2011;91(1–2):64–70.
Symons LK, Miller JE, Kay VR, Marks RM, Liblik K, Koti M, et al. The immunopathophysiology of endometriosis. Trends Mol Med. 2018;24(9):748–62.
Farland LV, Eliassen AH, Tamimi RM, Spiegelman D, Michels KB, Missmer SA. History of breast feeding and risk of incident endometriosis: prospective cohort study. BMJ. 2017;358:j3778.
Chung HH, Or YZ, Shrestha S, Loh JT, Lim CL, Ong Z, et al. Estrogen reprograms the activity of neutrophils to foster protumoral microenvironment during mammary involution. Sci Rep. 2017;7(1):1–13.
Králíčková M, Fiala L, Losan P, Tomes P, Vetvicka V. Altered immunity in endometriosis: what came first? Immunol Invest. 2018;47(6):569–82.
Riccio LDGC, Santulli P, Marcellin L, Abrão MS, Batteux F, Chapron C. Immunology of endometriosis. Best Pract Res Clin Obstet Gynaecol. 2018;50:39–49.
Takamura M, Koga K, Izumi G, Urata Y, Nagai M, Hasegawa A, et al. Neutrophil depletion reduces endometriotic lesion formation in mice. Am J Reprod Immunol. 2016;76(3):193–8.
Králíčková M, Vetvicka V. Immunological aspects of endometriosis: a review. Ann Transla Med. 2015;3(11):153.
Osuga Y, Koga K, Hirota Y, Hirata T, Yoshino O, Taketani Y. Lymphocytes in endometriosis. Am J Reprod Immunol. 2011;65(1):1–10.
Davis AC, Goldberg JM, editors. Extrapelvic endometriosis. Seminars in reproductive medicine; Thieme Medical Publishers. 2017. https://pubmed.ncbi.nlm.nih.gov/27992931/.
Troncon JK, Zani ACT, Vieira ADD, Poli-Neto OB, Nogueira AA, Rosa-e-Silva JC. Endometriosis in a patient with mayer-rokitansky-küster-hauser syndrome. Case Rep Obstet Gynecol. 2014;2014:376231.
Mechsner S, Weichbrodt M, Riedlinger W, Bartley J, Kaufmann A, Schneider A, et al. Estrogen and progestogen receptor positive endometriotic lesions and disseminated cells in pelvic sentinel lymph nodes of patients with deep infiltrating rectovaginal endometriosis: a pilot study. Hum Reprod. 2008;23(10):2202–9.
Trabert B, Peters U, De Roos AJ, Scholes D, Holt VL. Diet and risk of endometriosis in a population-based case–control study. Br J Nutr. 2011;105(3):459–67.
Hanada T, Tsuji S, Nakayama M, Wakinoue S, Kasahara K, Kimura F, et al. Suppressive regulatory T cells and latent transforming growth factor-β-expressing macrophages are altered in the peritoneal fluid of patients with endometriosis. Reprod Biol Endocrinol. 2018;16(1):1–8.
Zondervan KT, Cardon LR, Kennedy SH. What makes a good case–control study? Design issues for complex traits such as endometriosis. Hum Reprod. 2002;17(6):1415–23.
Gogacz M, Winkler I, Bojarska-Junak A, Tabarkiewicz J, Semczuk A, Rechberger T, et al. Increased percentage of Th17 cells in peritoneal fluid is associated with severity of endometriosis. J Reprod Immunol. 2016;117:39–44.
Ahn SH, Edwards AK, Singh SS, Young SL, Lessey BA, Tayade C. IL-17A contributes to the pathogenesis of endometriosis by triggering proinflammatory cytokines and angiogenic growth factors. J Immunol. 2015;195(6):2591–600.
Hirata T, Osuga Y, Takamura M, Saito A, Hasegawa A, Koga K, et al. Interleukin-17F increases the secretion of interleukin-8 and the expression of cyclooxygenase 2 in endometriosis. Fertil Steril. 2011;96(1):113–7.
Takamura M, Koga K, Izumi G, Hirata T, Harada M, Hirota Y, et al. Simultaneous Detection and Evaluation of Four Subsets of CD4+ T Lymphocyte in Lesions and Peripheral Blood in Endometriosis. Am J Reprod Immunol. 2015;74(6):480–6.
Okimura H, Tanaka Y, Fujii M, Shimura K, Maeda E, Ito F, et al. Changes in the proportion of regulatory T cell subpopulations during menstrual cycle and early pregnancy. Am J Reprod Immunol. 2022;88(6):e13636.
Montagna P, Capellino S, Villaggio B, Remorgida V, Ragni N, Cutolo M, et al. Peritoneal fluid macrophages in endometriosis: correlation between the expression of estrogen receptors and inflammation. Fertil Steril. 2008;90(1):156–64.
Lousse J-C, Van Langendonckt A, González-Ramos R, Defrère S, Renkin E, Donnez J. Increased activation of nuclear factor-kappa B (NF-κB) in isolated peritoneal macrophages of patients with endometriosis. Fertil Steril. 2008;90(1):217–20.
Duignan N, Jordan J, Coughlan B, Logan-Edwards R. One thousand consecutive cases of diagnostic laparoscopy. Int J Obstet Gynaecol. 1972;79(11):1016–24.
Tran LVP, Tokushige N, Berbic M, Markham R, Fraser IS. Macrophages and nerve fibres in peritoneal endometriosis. Hum Reprod. 2009;24(4):835–41.
Greaves E, Temp J, Esnal-Zufiurre A, Mechsner S, Horne AW, Saunders PT. Estradiol is a critical mediator of macrophage-nerve cross talk in peritoneal endometriosis. Am J Pathol. 2015;185(8):2286–97.
Oosterlynck DJ, Meuleman C, Waer M, Koninckx PR, Vandeputte M. Immunosuppressive activity of peritoneal fluid in women with endometriosis. Obstet Gynecol. 1993;82(2):206–12.
Sillem M, Prifti S, Monga B, Buvari P, Shamia U, Runnebaum B. Soluble urokinase-type plasminogen activator receptor is over-expressed in uterine endometrium from women with endometriosis. Mol Hum Reprod. 1997;3(12):1101–5.
Shi F-D, Ljunggren H-G, La Cava A, Van Kaer L. Organ-specific features of natural killer cells. Nat Rev Immunol. 2011;11(10):658–71.
Ohara J, Paul WE. Up-regulation of interleukin 4/B-cell stimulatory factor 1 receptor expression. Proc Natl Acad Sci. 1988;85(21):8221–5.
Hu-Li J, Shevach E, Mizuguchi J, Ohara J, Mosmann T, Paul W. B cell stimulatory factor 1 (interleukin 4) is a potent costimulant for normal resting T lymphocytes. J Exp Med. 1987;165(1):157–72.
Seder RA, Paul WE, Davis MM, de FazekasSt Groth B. The presence of interleukin 4 during in vitro priming determines the lymphokine-producing potential of CD4+ T cells from T cell receptor transgenic mice. J Exp Med. 1992;176(4):1091–8.
Hsieh C-S, Heimberger AB, Gold JS, O’Garra A, Murphy KM. Differential regulation of T helper phenotype development by interleukins 4 and 10 in an alpha beta T-cell-receptor transgenic system. Proc Natl Acad Sci. 1992;89(13):6065–9.
Wu M-Y, Yang J-H, Chao K-H, Hwang J-L, Yang Y-S, Ho H-N. Increase in the expression of killer cell inhibitory receptors on peritoneal natural killer cells in women with endometriosis. Fertil Steril. 2000;74(6):1187–91.
McCANN SE, Freudenheim J, Darrow SL, Batt RE, Zielezny MA. Endometriosis and body fat distribution. Obstet Gynecol. 1993;82(4 Pt 1):545–9.
Shah DK, Correia KF, Vitonis AF, Missmer SA. Body size and endometriosis: results from 20 years of follow-up within the Nurses’ Health Study II prospective cohort. Hum Reprod. 2013;28(7):1783–92.
Dunselman G, Vermeulen N, Becker C, Calhaz-Jorge C, D’Hooghe T, De Bie B, et al. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014;29(3):400–12.
Guo S-W, Du Y, Liu X. Platelet-derived TGF-β1 mediates the down-modulation of NKG2D expression and may be responsible for impaired natural killer (NK) cytotoxicity in women with endometriosis. Hum Reprod. 2016;31(7):1462–74.
Kang Y-J, Jeung IC, Park A, Park Y-J, Jung H, Kim T-D, et al. An increased level of IL-6 suppresses NK cell activity in peritoneal fluid of patients with endometriosis via regulation of SHP-2 expression. Hum Reprod. 2014;29(10):2176–89.
Yu J-J, Sun H-T, Zhang Z-F, Shi R-X, Liu L-B, Shang W-Q, et al. IL15 promotes growth and invasion of endometrial stromal cells and inhibits killing activity of NK cells in endometriosis. Reproduction. 2016;152(2):151–60.
Yang H-L, Zhou W-J, Chang K-K, Mei J, Huang L-Q, Wang M-Y, et al. The crosstalk between endometrial stromal cells and macrophages impairs cytotoxicity of NK cells in endometriosis by secreting IL-10 and TGF-β. Reproduction. 2017;154(6):815–25.
Acknowledgements
Not applicable.
Funding
This systematic review and meta-analysis was not funded in any way.
Author information
Authors and Affiliations
Contributions
F.T. designed the study, designed data collection, collected data, carried out the initial analyses, drafted the initial manuscript and revised the manuscript. Sh.Kh. supervised data collection and statistical analyses and critically reviewed the manuscript. A.B. collected data and conducted the initial analyses. A.Gh. and Sh.Kh. conceptualised and designed the study, designed data collection and reviewed the manuscript. H.T helped in the revision process and conducted the further analyses requested by reviewers. All authors read and approved the final manuscript and are responsible for data review.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tabatabaei, F., Tahernia, H., Ghaedi, A. et al. Diagnostic significance of neutrophil to lymphocyte ratio in endometriosis: a systematic review and meta-analysis. BMC Women's Health 23, 576 (2023). https://doi.org/10.1186/s12905-023-02692-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02692-7