Abstract
Background
Despite legislation and intervention programmes, the rates of maternal and child mortality in Nigeria remain high. Sustainable development goals on mother and child mortality would be a mirage if this continues. The study investigated the autonomy of women (women’s decision-making autonomy) and the use of maternal health-care services in Nigeria.
Methods
Secondary data obtained from the Nigeria Demographic and Health Survey, 2018 were used in this investigation. Women who indicated they gave birth in the five-year before the surveys were considered in the study. The association between autonomy of women and maternal health-care utilization was studied using binary logistic regression models.
Results
In total, about one-fifth of the women (19.6%) indicated they had at least eight ANC visits for their most recent birth. Overall, 40.5% of the women gave birth in a health institution, and 20.1% went for postnatal checkups. The use of health-care services was significantly related to the autonomy of women. Women’s and husbands/partners’ educational levels, residency and ethnicity were socio-demographic characteristics that influenced women’s healthcare service consumption.
Conclusions
For most recent childbirth, most women did not utilise the health-care services in Nigeria. To enhance the autonomy of women and, as a result, maternal health-care services use in Nigeria, effective interventions, policies, and programmes are required.
Similar content being viewed by others
Background
Every year, over 287,000 women in their childbearing age die around the world due to complications during pregnancy and childbirth [1,2,3]. Despite local, national, regional, and international efforts, programmes, and other policies to curtail maternal and child mortality, nearly all maternal deaths due to complications during pregnancy and childbirth occur in less developed countries [3], with more than two-thirds (about 66%) occurring in sub-Saharan African countries [4]. Maternal mortality has increased in many sub-Saharan African nations [5]. Maternal mortality accounts for about 59,000 deaths annually [5]. Globally, India is ranked first and Nigeria ranked second in maternal incident rate [5, 6]. Nigeria has about 545 prevalence of maternal mortality for every 100, 000 births [5, 7].
Increased usage of health-care services by women and their children is critical for improving women’s health and reducing mother and child morbidity and mortality [8]. In Nigeria, the high rate of women’s death is related to the non-use or poor use of maternal health services [8]. Maternal health-care that is timely, regular, and adequate can help to improve maternal well-being and reduce the risk of negative pregnancy outcomes.
Complications of pregnancy, as well as the mortality associated with them, can be decreased by efforts that increase healthcare delivery, maternal nutrition, and rapid utilization of healthcare facilities whenever there is a need for urgent obstetric care [9]. After a child is born, postnatal health-care services can help to prevent postpartum and life-threatening complications. Without concerted efforts to reduce maternal and child mortality, attaining the Sustainable Development Goals on women and child health would be a mirage [10].
The autonomy of women refers to the power and liberty of women to make decisions about matters that impact them and their families on their own or in collaboration with their partners [8]. They are involved in family decision-making, have access to funds or resources, and partake in resource management and decision-making [11,12,13]. The roles of women in decision-making have been linked to access and the usage of health-care services [14,15,16]. Furthermore, women’s status has an impact on women’s and child health [11, 17].
In Nigeria, this study looked into the relationship between the autonomy of women and maternal health-care services utilization (antenatal care (ANC) visitations, delivery at health facility, and postnatal health services) using the most recent Nigeria Demographic and Health Survey dataset. Men in Nigeria have a greater social rank than women. Most family heads, breadwinners, and older partners are men [18]. The patriarchal nature of most Nigerian households, which is reinforced by religion, may have an impact on the autonomy of women and the use of healthcare services, as well as maternal and childhood illness and death. Studies have explored socio-demographic and behavioural issues regarding maternal health-care services utilization. Socio-demographic and behavioural factors such as wealth status, maternal occupation, parity, media exposure were found to be associated with maternal health-care services utilization. Other factors found to be associated with maternal health-care services utilization were complications during pregnancy and antenatal checkups by skilled birth attendants [19,20,21,22]. Also, studies abound on timing of first ANC visits, early initiation of ANC visits, inequalities in early ANC visits and factors associated with them. Education, occupation, residence, parity, distance, wealth status and knowledge of the timing of ANC were found to be associated with early initiation of ANC [23,24,25,26]. Despite the previous study on the autonomy of women and maternal health-care service utilisation in Nigeria [10, 27,28,29,30,31,32,33,34,35], the association between maternal health-care services use and the autonomy of women needs further exploration [36]. The high level of maternal morbidity and mortality in Nigeria is an indication of the need for more evidence-based research on maternal health-care services utilization [37]. Studies have been carried out using a composite index of 4 or more ANC visits [38,39,40], delivery at the health facility, and postnatal care among childbearing women [39, 41]. World Health Organisation recommended a minimum of 8 antenatal care visits for positive pregnancy outcome and to promote the health of mothers [42]. Compliance with the recommended standard of minimum of 8 ANC contacts could improve the indicators of maternal and child health [37]. This study considered a composite index of 8 or more ANC visits, delivery at the health facility, and postnatal care among childbearing women in Nigeria.
Few studies have been conducted recently on autonomy of women and maternal health-care services utilization in Nigeria [10, 34, 35]. Available studies have not fully examined the relationship between the autonomy of women and maternal health-care services utilization in Nigeria particularly the use of a composite index of 8 or more ANC visits along with delivery at the health facility, and postnatal care services [10]. Examination of the link between the autonomy of women and maternal health-care services utilization using a recent dataset is important to address issues of maternal and child needs in Nigeria. As a result, the purpose of this study is to investigate the relationship between the autonomy of women and the use of maternal health-care services in Nigeria. This is required because mother and child mortality are high, and maternal health-care resources are underutilized [43]. The findings of this study will enhance understanding of the relationship between the autonomy of women and the use of maternal health-care services, as well as the factors that influence these relationships. It will also drive policies and intervention programs on the usage of maternal health services, potentially lowering the country’s mother and child morbidity and death rates.
Methods
Source of data
Data from the Nigeria Demographic and Health Survey (NDHS), a cross-sectional, national, and representative sample survey, were used in the study. The information was acquired under the supervision of the National Population Commission, which oversees such matters. The survey’s goal was to gather current and trustworthy information on family planning, fertility, HIV/AIDS knowledge, domestic violence, nutritional status of children, maternal health, child health and health-care services utilization. The Nigeria Population Commission and the ICF Macro Institutional Review Board in Calverton, Maryland, USA, both accepted the study’s protocol. There is no need for independent ethical approval because the dataset is freely available on the official DHS website [44].
Study participants
The survey included married women of age group 15–49 who indicated they gave birth in the five years prior to the survey (n = 19,764). Detailed information on the questionnaire and methods used to conduct the survey can be found somewhere [7].
Outcome variable
The outcome variable is maternal health-care services utilization (a composite index of 8 or more ANC visits [42], delivery at health facility, and postnatal care of a recent or current child born within the five-year before the survey). ANC visits was coded as one if a respondent reported eight or more ANC visits for the latest childbirth, otherwise zero. Health facility delivery was coded as one if a respondent used health facility at childbirth for the latest childbirth, otherwise zero. Postnatal care was coded as one if a respondent went for postnatal care services for the latest childbirth, otherwise zero.
Independent variables
The autonomy of women was one of the independent variables studied (the composite index of decision-making on health-care services for respondents, huge household purchases and visitations to relatives or family) [8]. Other covariates included education (no formal education, primary education, and post or higher secondary education), ethnicity (Yoruba, Igbo, Hausa/Fulani and others), children ever born, respondents’ age (<25, 25–34, and 35+), partners’ age (<25, 25–34, and 35–44, and 45+), level of education of partners or spouses (no formal form education, primary education, and post or higher secondary education), wealth index (rich, middle and poor), residence (urban and rural) and religion (Islam and Christianity). To account for sampling variability, sample weight was used [8].
Data analysis
The study employed three types of analyses: univariate, bivariate, and multivariate. The frequency and percentage distributions of variables were explored in the univariate analysis. Using the Chi-square test, the bivariate analysis looked at the relationship between a dependent (maternal health-care services utilization - antenatal care (ANC) visitations, delivery at health facility, and postnatal health services) and independent variables (autonomy of women, education, and age of respondent and partner, wealth status, residence, religion, ethnicity, and children ever born). In addition, a test of correlation was performed among explanatory variables to account for multicollinearity. The results of the test demonstrated that the multicollinearity assumptions were not violated. More than 0.10 was the tolerance value [45]. The multivariate analysis explored the influence of the autonomy of women on maternal health-care use using logistic regression models.
Results
Table 1 presents the descriptive features of the participants. The study included a weighted sample of 19,764 married participants who gave birth in five-year preceding the survey. Almost two-fifths of respondents (38.6%) indicated they were not involved in decisions that affected their lives and households. Approximately 25% of the mothers were under the age of twenty-five, and almost two-fifth of the mothers (38.2%) was between the ages of 25 and 34. More than one-third of the women (47.3%) and their spouses (38.2%) reported no formal form of education, and more than a quarter of the women (29.6%) and their spouses (32.9%) had secondary education. Muslim women made up a higher number of married women (64.6%), while 62.0% of married women lived in rural regions. The Hausa/Fulani ethnic group accounted for 49.8% of the total population. A higher percentage of those polled had given birth to four or more children.
Respondents’ utilization of maternal health-care services is presented in Table 2. In the five-year preceding the survey, less than one-fifth of the mothers (19.6%) who had a child had 8 or more prenatal care visits. About 40.5% of the mothers had their last child in a health institution, and about one-fifth of the women (20.1%) claimed they went for postnatal care. In the five-year prior to the study, less than 41.0% of the mothers used all three services for their previous live birth (8 or more ANC checkups, health facility delivery as at last birth, and postnatal visits).
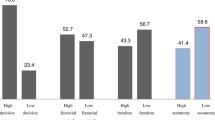
Table 3 shows the background and other selected variables by maternal health-care services utilization for the most recent or current live birth in the five-year prior to the survey. When compared to women who claimed they did not have autonomy in decision-making, mothers (7.8%) who indicated they did had autonomy in decision-making used more maternal health-care services (ANC visits, 26.2%; health facility delivery, 50.3% and postnatal care services, 24.9%). In comparison to mothers under the age of 25, mothers above the age of 25 used maternal healthcare services more frequently. The utilization of maternal health-care services rose with an increase in education; respondents with at least a secondary level of education used maternal health-care services more than respondents with only a primary level of education. Christian women accessed maternity health-care more frequently than Muslim women. Respondents from wealthy households, those who lived in cities, and those who belonged to the Yoruba tribe and had one child used maternal healthcare services more frequently. The usage of maternal health-care services by women increases with the education of husbands/partners. In comparison to males in other age groups, wives of men in the 35–44 age group used maternal health-care services more. As presented in Table 3, the autonomy of women and all the background features (age, education, religion, wealth index, residence, region, children ever born (CEB) and ethnicity) of women were statistically associated with maternal health-care services utilization.
Table 4 summarizes the findings from the analysis of the autonomy of women and maternal health-care services utilization using logistic regression models. There was a positive association between maternal healthcare services utilization and the autonomy of women. When compared to women who did not participate in family decision-making, those who participated in household or family decision-making were more than two times more likely to use maternal health-care services.
Having adjusted for socio-demographic and other selected variables in Table 5, the autonomy of women ((ANC visits (OR 1.24; 95% CI 1.06–1.44)), (health facility delivery (OR 1.19; 95% CI 1.08–1.31)) and (postnatal services (OR 1.49; 95% CI 1.32–1.68))) maintained a positive association with the utilization of maternal health-care services. When compared to women who did not participate in household or family decision-making, women who participated in household or family decision-making were more likely to use maternal health-care services. In addition, model 5 revealed that mothers with primary education ((ANC visits (OR 1.56; 95% CI 1.29–1.90)), (health facility delivery (OR 1.34; 95% CI 1.16–1.54)) and (postnatal services (OR 1.29; 95% CI 1.10–1.51))) and secondary education ((ANC visits (OR 1.80; 95% CI 1.48–2.20)) and (health facility delivery (OR 1.77; 95% CI 1.51–2.07)) and (postnatal services (OR 1.30; 95% CI 1.10–1.54))) were more likely to use maternal health-care services than mothers with no formal form of education. When compared to mothers in urban regions, the likelihood of maternal health-care services utilization was shown to be lower in rural areas ((ANC visits (OR 0.68; 95% CI 0.59–0.78)), (health facility delivery (OR 0.74; 95% CI 0.64–0.86)) and (postnatal services (OR 0.81; 95% CI 0.71–0.93))). When compared to mothers of Hausa/Fulani descent, mothers of the Igbo tribe ((ANC visits (OR 3.70; 95% CI 0.2.81–4.86)), (health facility delivery (OR 6.29; 95% CI 4.85–8.15)) and (postnatal services (OR 2.39; 95% CI 1.91–3.01))) and mothers of the Yoruba tribe ((ANC visits (OR 9.66; 95% CI 7.55–12.37)), (health facility delivery (OR 5.84; 95% CI 4.55–7.49)) and (postnatal services (OR 1.95; 95% CI 1.57–2.42))) reported higher odds of maternity health-care services utilization. In addition, the higher the level of educational attainment, the higher the use of maternal health-care services. Women who claimed their husbands/partners had secondary education (ANC visits (OR 1.34; 95% CI 1.07–1.68)), (health facility delivery (OR 1.81; 95% CI 1.55–2.11)) and (postnatal services (OR 1.85; 95% CI 1.55–2.20))), and post-secondary education (ANC visits (OR 1.65; 95% CI 1.25–2.19)), (health facility delivery (OR 2.48; 95% CI 2.04–3.02)) and (postnatal services (OR 2.23; 95% CI 1.83–2.72))) had a higher likelihood of maternal health-care services usage than husbands/partners of mothers with no formal form education.
Discussions
The purpose of this study was to investigate the influence of the autonomy of women on maternal health-care services utilization in Nigeria. Maternal health-care services utilization is a composite index of 8 or more ANC visitations, delivery at the health facility, and postnatal care for a current or recent childbirth in the five-year preceding the current Nigeria Demographic and Health Survey. The composite index of women’s decision-making autonomy on health-care for respondents, large household purchases, and visits to relatives or family were used to measure women’s autonomy. A weighted sample of 19,764 married women who gave birth in the five-year preceding the survey was used [8]. The findings, as corroborated by other studies [10, 46], revealed the autonomy of women had a significant influence on maternal healthcare services utilization in Nigeria. The findings also revealed low maternal health-care services utilization [16, 47]. In Nigeria, the potential consequence of low usage of healthcare services among women might be high maternal and child mortality [10].
This highlights the importance of intervention programmes and policies that will increase the autonomy of women to improve the utilization of maternal health-care services in Nigeria. Women of high autonomy are more likely to use health-care facilities during pregnancies, deliveries and postnatal care periods compared to women of low autonomy [8]. There is a link between the autonomy of women and maternal health-care services utilization. Higher women’s autonomy in decision-making on health-care services will increase the use of maternal health-care services and consequently reduce pregnancy risks, complications, and childhood and maternal mortality. It will lead to better pregnancy outcomes, welfare of children and mothers [8, 48].
The findings also revealed that women’s education was related to their use of maternal health-care [46, 47, 49]. As women’s education levels rise, so does their use of maternal healthcare services. Education improves women’s access to healthcare facilities [8] as well as their ability to participate in family decision-making [50]. School also empowers and boosts women’s self-esteem [50]. The level of education of husbands/partners yielded similar results. Women with educated spouses were more likely to use maternal healthcare services than their counterparts. Educated men will appreciate women more and understand why they should be involved in family decisions.
Muslims used maternal healthcare services less frequently than Christians. This could be related to the fact that Christianity is more open to western education, which encourages women’s autonomy and the use of maternal health-care services. Household wealth influenced the use of maternal healthcare services in Nigeria, according to the study. Women from wealthy households used maternal health-care services more frequently [46, 49]. Many women’s inability may be due to a lack of financial resources.
Furthermore, women in urban areas used maternal healthcare services more than women in rural areas [47]. Women in cities have access to more health and education services. In comparison to rural women, they are more empowered and liberal. Women in urban areas may be more likely to use maternal health facilities because of this. The study discovered disparities in maternal healthcare service utilization among Nigeria’s three major ethnic groups. In Nigeria, the Yoruba tribe is the most educated and sociable, followed by the Igbo tribe. Hence, more use of maternal health-care services by the Yoruba and Igbo tribes compared to the Hausas.
Furthermore, as the number of children increased, the usage of maternal healthcare services declined. As the number of children grows, so does the cost of their care. This could explain why women with fewer children use maternal healthcare services more frequently.
Conclusion
In Nigeria, maternal health-care services utilization is linked to women’s autonomy. As a result, women’s autonomy as a predictor should be examined alongside many other determinants to encourage and enhance the utilization of maternal health services. Increased utilization of maternal health services in Nigeria could be aided by effective policies, programmes, and interventions concentrating on increasing the autonomy of women.
Strengths and limitations
The survey is nationally representative, allowing the findings to be generalized across Nigeria. The study, however, had some flaws. Few household’s decision-making indexes may not adequately capture women’s autonomy [8]. The cause-effect linkages cannot be deduced due to the cross-sectional character of the survey, hence interpretations of findings should be done with caution. Due to the self-reported nature of the data, the survey may suffer from recall bias and social desirability [18, 51].
Data and materials availability
Data were sourced from Demographic and Health survey (DHS) and are available here: http://dhsprogram.com/data/available-datasets.cfm.
References
Maternal. deaths halved in 20 years, but faster progress needed [Internet]. PRWeb. [cited 2022 Apr 26]. Available from: https://www.prweb.com/releases/2012/5/prweb9511744.htm
Gogoi M. Women Empowerment and Maternal Health Care Utilisation in North-East India.:12.
Dickson KS. Women Empowerment and Skilled Birth Attendants among Women in Rural Ghana.BioMed Research International. 2021 Dec 24;2021:e9914027.
trends-in-maternal-. mortality-1990-to-2015.pdf [Internet]. [cited 2022 Apr 26]. Available from: https://www.afro.who.int/sites/default/files/2017-05/trends-in-maternal-mortality-1990-to-2015.pdf
Olonade O, Olawande TI, Alabi OJ, Imhonopi D. Maternal mortality and maternal Health Care in Nigeria: implications for Socio-Economic Development. Open Access Maced J Med Sci. 2019 Mar;14(5):849–55.
Sageer R, Kongnyuy E, Adebimpe WO, Omosehin O, Ogunsola EA, Sanni B. Causes and contributory factors of maternal mortality: evidence from maternal and perinatal death surveillance and response in Ogun state, Southwest Nigeria. BMC Pregnancy Childbirth. 2019 Feb;11(1):63.
Nigeria. - Demographic and Health Survey – 2019 [Internet]. Reproductive Health Supplies Coalition. [cited 2021 Nov 8]. Available from: https://www.rhsupplies.org/activities-resources/publications/nigeria-demographic-and-health-survey-2019-8194/
Adhikari R. Effect of Women’s autonomy on maternal health service utilization in Nepal: a cross sectional study.BMC Women’s Health. 2016 May13;16(1):26.
Antenatal care in. developing countries: promises, achievements and missed opportunities. - Free Online Library [Internet]. [cited 2022 Apr 26]. Available from: https://www.thefreelibrary.com/Antenatal+care+in+developing+countries%3a+promises%2c+achievements+and… a0118687898
Obasohan PE, Gana P, Mustapha MA, Umar AE, Makada A, Obasohan DN. Decision making autonomy and maternal Healthcare utilization among nigerian women. Int J MCH AIDS. 2019 Mar;20(1):11–8.
Adhikari R, Sawangdee Y. Influence of women’s autonomy on infant mortality in Nepal. Reproductive Health. 2011;8:7.
Culture. the status of women and demographic behaviour: illustrated with the case of India (Library resource) [Internet]. Europos lyčių lygybės institutas. [cited 2022 Apr 26]. Available from: https://eige.europa.eu/lt/library/resource/kvinnsam.4627020
Kishor S, Subaiya L. Understanding women’s empowerment: a comparative analysis of demographic and health surveys (DHS) data. 2008 Oct 1 [cited 2022 Apr 26]; Available from: https://preview.dhsprogram.com/publications/publication-cr20-comparative-reports.cfm
Balk D. Individual and community aspects of women’s Status and Fertility in Rural Bangladesh. Popul Stud. 1994 Mar;48(1):21–45.
Beegle K, Frankenberg E, Thomas D. Bargaining power within couples and use of prenatal and delivery care in Indonesia. Stud Fam Plann. 2001 Jun;32(2):130–46.
Sado L, Spaho A, Hotchkiss DR. The influence of women’s empowerment on maternal health care utilization: evidence from Albania. Soc Sci Med. 2014 Aug;114:169–77.
Castle SE. Intra-household differentials in women’s status: household function and focus as determinants of children’s illness management and care in rural Mali. Health Transit Rev. 1993 Oct;3(2):137–57.
Odusina EK, Ayotunde T, Kunnuji M, Ononokpono DN, Bishwajit G, Yaya S. Fertility preferences among couples in Nigeria: a cross sectional study. Reprod Health. 2020 Dec;17(1):92.
Amin R, Shah NM, Becker S. Socioeconomic factors differentiating maternal and child health-seeking behavior in rural Bangladesh: A cross-sectional analysis. Int J Equity Health. 2010 Apr3;9:9.
Islam N, Islam MT, Yoshimura Y. Practices and determinants of delivery by skilled birth attendants in Bangladesh. Reprod Health. 2014 Dec;11:11:86.
Deo KK, Paudel YR, Khatri RB, Bhaskar RK, Paudel R, Mehata S, et al. Barriers to utilization of Antenatal Care Services in Eastern Nepal. Front Public Health. 2015;3:197.
Akeju DO, Oladapo OT, Vidler M, Akinmade AA, Sawchuck D, Qureshi R et al. Determinants of health care seeking behaviour during pregnancy in Ogun State, Nigeria.Reproductive Health. 2016 Jun8;13(1):32.
Paudel Y, Jha T, Mehata S. Timing of First Antenatal Care (ANC) and Inequalities in Early Initiation of ANC in Nepal. Frontiers in Public Health. 2017 Sep 1;5:242.
Seidu AA. Factors associated with early antenatal care attendance among women in Papua New Guinea: a population-based cross-sectional study. Archives of Public Health. 2021 May6;79(1):70.
Geta MB, Yallew WW. Early Initiation of Antenatal Care and Factors Associated with Early Antenatal Care Initiation at Health Facilities in Southern Ethiopia.Advances in Public Health. 2017 Sep18;2017:e1624245.
Alemu Y, Aragaw A. Early initiations of first antenatal care visit and associated factor among mothers who gave birth in the last six months preceding birth in Bahir Dar Zuria Woreda North West Ethiopia. Reproductive Health. 2018 Dec 12;15(1):203.
Ononokpono DN, Azfredrick EC. Intimate partner violence and the utilization of maternal health care services in Nigeria. Health Care Women Int. 2014;35(7–9):973–89.
Fagbamigbe AF, Idemudia ES. Wealth and antenatal care utilization in Nigeria: Policy implications.Health Care for Women International. 2017 Jan2;38(1):17–37.
Adewuyi EO, Auta A, Khanal V, Bamidele OD, Akuoko CP, Adefemi K et al. Prevalence and factors associated with underutilization of antenatal care services in Nigeria: A comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. PLoS ONE. 2018 Jan 1;13(5):e0197324.
Akinyemi JO, Afolabi RF, Awolude OA. Patterns and determinants of dropout from maternity care continuum in Nigeria. BMC Pregnancy Childbirth. 2016 Sep27;16(1):282.
Kuuire VZ, Kangmennaang J, Atuoye KN, Antabe R, Boamah SA, Vercillo S, et al. Timing and utilisation of antenatal care service in Nigeria and Malawi. Glob Public Health. 2017 Jun;12(6):711–27.
Omer K, Afi NJ, Baba MC, Adamu M, Malami SA, Oyo-Ita A, et al. Seeking evidence to support efforts to increase use of antenatal care: a cross-sectional study in two states of Nigeria. BMC Pregnancy Childbirth. 2014 Nov;20:14:380.
Jo A, Ea B. O A. Trends in neonatal mortality in Nigeria and effects of bio-demographic and maternal characteristics. BMC pediatrics [Internet]. 2015 Sep 4 [cited 2022 Oct 7];15. Available from: https://pubmed.ncbi.nlm.nih.gov/25886566/
Ahuru RR. The influence of women empowerment on maternal and childcare use in Nigeria.International Journal of Healthcare Management. 2021 Jul3;14(3):690–9.
F AA, Chima V. A AO. Women autonomy and maternal healthcare services utilization among young ever-married women in Nigeria. IJNM. 2018 Jun30;10(6):62–73.
Dalal K, Shabnam J, Andrews-Chavez J, Mårtensson LB, Timpka T. Economic empowerment of women and utilization of maternal delivery care in bangladesh. Int J Prev Med. 2012 Sep;3(9):628–36.
Fagbamigbe AF, Olaseinde O, Setlhare V. Sub-national analysis and determinants of numbers of antenatal care contacts in Nigeria: assessing the compliance with the WHO recommended standard guidelines. BMC Pregnancy Childbirth. 2021 May;25(1):402.
Ftwi M, Gebretsadik GG, egziabher, Berhe H, Haftu M, Gebremariam G, Tesfau YB. Coverage of completion of four ANC visits based on recommended time schedule in Northern Ethiopia: A community-based cross-sectional study design. PLOS ONE. 2020 Aug 18;15(8):e0236965.
Mr K, An I, D Y, Kb M. M B. Assessing the association between an early and recommended number of focused antenatal care visits and the number of prenatal care content received before delivery in Ethiopia. PloS one [Internet]. 2023 Mar 3 [cited 2023 Mar 15];18(3). Available from: https://pubmed.ncbi.nlm.nih.gov/36867632/
Kumar G, Choudhary TS, Srivastava A, Upadhyay RP, Taneja S, Bahl R, et al. Utilisation, equity and determinants of full antenatal care in India: analysis from the National Family Health Survey 4. BMC Pregnancy Childbirth. 2019 Sep;5(1):327.
Mwebesa E, Kagaayi J, Ssebagereka A, Nakafeero M, Ssenkusu JM, Guwatudde D, et al. Effect of four or more antenatal care visits on facility delivery and early postnatal care services utilization in Uganda: a propensity score matched analysis. BMC Pregnancy Childbirth. 2022 Jan;3:22:7.
WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience [Internet]. Geneva: World Health Organization. ; 2016 [cited 2022 Oct 7]. (WHO Guidelines Approved by the Guidelines Review Committee). Available from: http://www.ncbi.nlm.nih.gov/books/NBK409108/
Srivastava A, Mahmood S, Mishra P, Shrotriya V. Correlates of maternal health care utilization in rohilkhand region, India. Ann Med Health Sci Res. 2014 May;4(3):417–25.
Measure DHS. demographic and health surveys. http://www.measuredhs.com/what-we-do/survey/survey-display-356.cfm - Search [Internet]. [cited 2022 Apr 26]. Available from: https://www.bing.com/search?q=Measure+DHS%3A+demographic+and+health+surveys.+http%3A%2F%2Fwww.measuredhs.+com%2Fwhat-we-do%2Fsurvey%2Fsurvey-display-356.cfm&cvid=2372c3113a0c4b8b9e9751f66c9bed7e&aqs=edge.69i57.2085j0j1&pglt=41&FORM=ANNTA1&PC=U531
Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Boston: Pearson/Allyn & Bacon; 2007. xxviii, 980 p.
Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 ethiopian demographic and Health Survey. BMC Pregnancy Childbirth. 2014 May;7:14:161.
Dimensions of women’s autonomy and the influence on maternal. health care utilization in a North Indian city | Demography | Duke University Press [Internet]. [cited 2022 Mar 14]. Available from: https://read.dukeupress.edu/demography/article/38/1/67/170420/Dimensions-of-women-s-autonomy-and-the-influence
Dyson T, Moore M. On Kinship structure, female autonomy, and demographic behavior in India. Popul Dev Rev. 1983;9(1):35–60.
Effects of women’s autonomy on maternal healthcare utilization. Bangladesh: evidence from a national survey. Sex Reproductive Healthc. 2017 Dec;1:14:40–7.
Women’s. Education, Autonomy, and Reproductive Behaviour: experience from developing countries. Oxford, New York: Oxford University Press; 1996. p. 328.
Yaya S, Odusina EK, Bishwajit G. Prevalence of child marriage and its impact on fertility outcomes in 34 sub-saharan african countries. BMC Int Health Hum Rights. 2019 Dec;19(1):33.
Acknowledgements
The authors acknowledged the MEASURE DHS project for their support and free access to the original data.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
EKO contributed to the study design and conceptualization. EKO reviewed the literature. OSO and EKO performed the analysis. All authors provided technical support and critically reviewed the manuscript for its intellectual content. EKO had final responsibility to submit for publication. All authors read drafts of the paper and approved the final version.
Corresponding author
Ethics declarations
Consent for publication
This is not applicable to this study.
Ethics approval and consent to participate
Ethics approval was not required; data are secondary and are available in the public domain. More information on DHS data and ethical standards is available at: http://goo.gl/ny8T6X.
Competing interests
No competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Odusina, E.K., Oladele, O.S. Is there a link between the autonomy of women and maternal healthcare utilization in Nigeria? A cross-sectional survey. BMC Women's Health 23, 167 (2023). https://doi.org/10.1186/s12905-023-02317-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-023-02317-z