Abstract
Background
The women-friendly care approach focuses on women’s rights to have access to quality care for themselves as individuals, as mothers, and for their infants. However, access to quality health services is not guaranteed for many women, particularly in low and middle-income countries. Hence, this study aimed to assess the level of women-friendly care provision and associated factors among mothers in the immediate post-partum period at public hospitals of Bale Zone, Southeast Ethiopia 2021.
Methods
An institutional-based cross-sectional survey was employed among mothers in the immediate post-partum period in public hospitals of Bale Zone from March 1–30, 2021. A total of 363 mothers were recruited by systematic random sampling technique in this study. Data was collected through pre-tested structured questionnaires. A 21-verified questionnaire was used to measure the outcome variable. The data were entered into Epi Data version 4.6.2.0 and exported to the statistical package of social science version 26.0 for analysis. A variable with a P value of less than 0.25 in the bi-variable binary logistic regression model was transferred to a multivariable binary logistics regression model. Hosmer and Lemeshow’s goodness of fit model was checked. Adjusted odds ratio with 95% confidence intervals were used to estimate the strength of association between the outcome variable and independent variables. A p-value less than 0.05 was considered as significantly associated.
Results
The level of women-friendly care provision among mothers in immediate post-partum at public hospitals of Bale Zone was found to be 61% [95% confidence interval (55.73–66.04)]. Being prim para mother [Adjusted odds ratio = 1.88(1.07–3.33)], having planned pregnancy [Adjusted odds ratio = 1.94(1.04–3.63)] and staying at a health facility after delivery [Adjusted odds ratio = 4.8(1.71–13.39)] were found to be statistically significant predictors of level of women-friendly care provision.
Conclusion
The women-friendly care provision among mothers in the immediate post-partum period in this study area was found to be low against most of the pre-existing findings. Strong counseling on planned pregnancy and staying at a health facility after delivery is recommended.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Every year more than 289,000 women die during pregnancy or childbirth due to severe maternal complications over the globe due to different reasons including substandard care provision in health facilities [1]. Evidence report that the less change in maternal mortality trend and fatality rates documented for obstetric complications indicate the lack of improvement in the quality of maternal health care provision [2].The main barriers that contribute to the low quality of women's health services include the lack of compliance of services with defined standards, the shortage of supplies, infrastructure problems, deficiency in detection and management of complications or emergency cases, and poor client-provider interaction [3].
According to Windau-Melmer, service providers must ensure that every woman seeking care is a person of value and has the right to be treated with respect and consideration [4]. However, still, access to quality health services is not guaranteed for many women, particularly in low and middle-income countries (LMICs) [5]. As a result, women were suffered from significant mistreatment in health facilities. Study in Ghana said, 83% of women suffered from at least one form of mistreatment during facility childbirth [6]. Other quantitative studies reported a prevalence of mistreatment in facility-based childbirth ranging from 15 to 98%, with most studies measuring mistreatment prevalence ranging from 12 to 20% in Tanzania, Kenya, and India [7]. Because of services paid, little attention to their needs, and showed little sensitivity towards local culture, women in Peru were reluctant to utilize Emergency Obstetrics Care(EmOC) facilities [8].
Ethiopia has one of the highest maternal mortality ratios (MMR) that is 401 maternal deaths per 100,000 live births in 2019 [9] and studies showed that the lack of women-friendly care during facility-based childbirth is continuing as a problem. For instance, in Ethiopian public health facilities, at least one form of mistreatment of women was committed in 36% of the observation in which 38% in health centers and 32% in hospitals [10]. Specifically, the study conducted in Jimma, Bahir Dar, Arba Minch revealed that (29%), (43%) and (98.9%) of women were did not receive women-friendly care services during facility-based childbirth respectively [11,12,13].
Poorly perceived quality of women-friendly care in facility-based childbirth often acts as a deterrent to current and/or future utilization of facility-based childbirth services. A recent assessment in Ethiopia showed that from 103 of the women interviewed, 85% of them reported that their service experience influenced their decision on where to deliver in the future [14]. Providing good-quality care is one of the most effective ways of ensuring that maternal health services are used and can be achieved through improving the women-friendly care health services which focuses on the rights of women to have access to quality care for themselves as individuals and as mothers, and for their infants [3].
It is a key intervention to improve the quality and bring unreached women to health facilities for maternity care services, although, full attention was not given to the level of women-friendly care provision and factors associated. As far as we know, in the study area, there is lack of evidences on the level of women-friendly care provision at public health facilities. Hence, this study aimed to assess the level of women-friendly care provision and its associated factors among mothers in the immediate post-partum period at public hospitals of southeast Ethiopia.
Methods
Study setting, design, and period
An institutional-based cross-sectional study was conducted at public hospitals of Bale Zone, from March 1–30, 2021. Bale zone is located in Southeast Ethiopia. Robe, the Zone city, is located 435 km far from the capital town of Ethiopia; Addis Ababa. Based on the report of Bale Zonal health department, the Zone has a total population of 1,269,951 from which women of childbearing age is around 281,040. The estimated number of pregnant women in the zone is around 44,067. Currently, the zone has five hospitals namely, Goba Referral Hospital, Delo Mena General Hospital, Madda Walabu General Hospital, Goro Hospital, and Robe General Hospital which is under robe town administration. Among five public hospitals, only Goba Referral Hospital, Delo Mena General Hospital, and Madda Walabu General Hospital were providing labor and delivery services during the data collection period. Robe General Hospital served as the center for COVID19 and Goro General Hospital was non-functional (Bale zone health department report, 2021).
Study population
All mothers who gave birth in public hospitals of Bale Zone and in the immediate post-partum period were the source population, whereas randomly selected mothers who were in the immediate post-partum period were the study population. In this study, mothers with severe complications of birth were excluded.
Sample size determination
The sample size was calculated using the single population proportion formula, assuming 71% proportion of women-friendly care provision from an institutional-based cross-sectional study conducted in public Hospitals of Jimma Zone, Ethiopia [11], 95% confidence interval (CI), and 5% margin of error. n = (1.96)2 0.71(0.29)/ (0.05)2 = 316. After adding a 15% non-response rate, the final sample size was found to be 363.
Sampling procedure
According to the report from the zonal health department, the total number of delivery for the last three months was 1990, 289, and 137 in Goba Referral Hospital, Delo Mena General Hospital, and Madda Walabu General Hospital respectively. The monthly average number of delivery for these three hospitals was 663, 96, and 46 respectively. Further allocation of the sample was done for these hospitals proportionally based on the average number of clients who have received childbirth services in the last three months. So, the final sample size was 299, 43, and 21 for respective hospitals. Individual participants in each of the hospitals were selected by systematic sampling technique every K of 2 using a list of a mother who gave birth and recorded on postnatal registration book for the last three months as the sampling frame.
Data collection tool and data collection procedure
A structured questionnaire which was adapted from different works of literature and consists of 36 questions and 21 verification criteria [3, 11, 15] is used in this study to assess the level of women-friendly care provision. It was made up of four sections, the first section was used to assess socio-demographic characteristics of the mother with 13 items, the second section was used to assess obstetric characteristics of participants with 13 items, the third section was used to assess facilities services use and providers related characteristics with 10 items, the fourth section was used to measure the level of women-friendly care provision experienced by mothers during facility childbirth which measured by 21 verified questions. The value 1 is given for those who answered ‘yes’ and 0 for those who answered ‘no’ and coded. The opposite questions were recoded. Then values were computed and a score of at least mean and above was taken as a good level of women-friendly care provision. In this study, four data collectors and four supervisors were assigned to facilitate the data collection. Data were collected during the immediate post-partum period in post-natal ward through interviews administered questions prepared by local language.
Study variables, outcome variable, and operational definitions
Socio-demographic, provider, facility-related, and obstetrics variables were study variables whereas the level of women-friendly care provision was outcome variable.
A series of 21 questions related to the level of women-friendly care provision were asked. Study participants who scored at least score of 50% towards women-friendly care provision questions were categorized as getting a "good level of women-friendly provision" and else were categorized as getting poor women-friendly care provision.
Severe birth complications were complications like postpartum convulsion due to eclampsia and severe birth canal injury secondary to instrumental deliveries.
Data quality assurance
An adopted questionnaire prepared in English was translated to Afan Oromo and then translated back to English by another language expert to check and maintain its consistency. Pretest was done to improve clarity, understandability, and simplicity of the messages of the tools before actual data collection. After pretest, modification on minutes needed for interviewing was corrected from 5–10 min to 10–15 min and some words was re-write as per suggestions from data collectors to make it simply understandable and clear tool which helps to meet the objective of the study. Data collectors and supervisors were trained for two days on the objective, method, sampling technique, ethical issues, data collection instrument, and data collection procedure before data collection. All of the questionnaires were checked for completeness and accuracy during and after the period of data collection.
Data processing and analysis
The data were entered into Epi Data 4.6.2.0 and were coded. After that, it was exported to SPSS version 26.0 and cleaned before analysis. Descriptive statistics were calculated for the variables. Statistical significance and strength of the association between independent variables and outcome variables were analyzed by using the logistic regression model. A variable with a P value of less than 0.25 in the bi-variable binary logistic regression model was transferred to a multivariable binary logistics regression model to adjust the confounder’s effects. The enter method was used to run the model. Hosmer and Lemeshow’s goodness of fit model was checked and the data fitted the model well (p = 0.92). Crude and adjusted odds ratios with their 95% confidence intervals were calculated. Adjusted odds ratio with 95% confidence intervals were used to estimate the strength of association between the outcome variable and independent variables. A p-value less than 0.05 was considered as significantly associated. Finally, the result of the study was presented using tables, chart, and texts based on the data obtained.
Result
In this study a total of 363 study participants participated, yielding a response rate of 98.9%, whereas the remaining 1.1% non-response rate was due to incomplete data not due to the sensitivity of the questionnaires.
Socio-demographic characteristics of the study participants
Most of the participants 281(78.3%) were Oromo in ethnicity followed by Amhara 64(17.8%). The mean age of participants was 28.34 years with a standard deviation of ± 5.51SD and a range from age of 17 to 42 years. The majority 334(93.0%) of the participants were married and 175(48.3%) of them were Muslim followers whereas 11(3.1%) were Waqeffatta. Of total the participants, 92(25.6%) had a primary level of education while 244(68.0%) participants’ means of transportation to health facility was public transport which took 30 min in 173(48.2%) of the participants (Table 1).
Obstetric history of the participants
Regarding deliveries, 279(77.7%) participants had more than one number of deliveries, and 285(79.4%) last pregnancy was planned. Among participants who had ANC follow-up, only 155(53.7%) had four and more times of follow up while 38(10.6%) participants did not have ANC follow up at all. Considering the type of mode of delivery 208(57.9%) participants gave birth through vaginal delivery followed by cesarean Sect. 80(22.3%). Of the total respondents, 267(74.4%) received postnatal care in the immediate postpartum period. During the last delivery, 116(32.3%) participants had experienced birth complications in which 44(12.3%) developed postpartum hemorrhage and 9(2.5%) developed inversion of the uterus (Table 2).
Facility services use and providers related characters
Most of the participants 204 (56.8%) reported average waiting time to see a provider during a visit was less than 30 min. Of the total respondents, 19(5.3%) paid money during the care provision even if maternity care was free of charge in Ethiopia. Regarding the sex of the main providers assisting the participants during delivery, 234(65.2%) participants were assisted by a midwife, and the main 232 (64.5%) sex of care provider was male. And among the participants, 28(7.8%) were treated badly in which 12(3.3%) of them were treated badly by the doctor followed by midwife 10(2.8%) and the main type of abuse reported by study participants was psychological abuse which was shouting at them in 12(3.3%) participants (Table 3).
Provision of women-friendly care
A total of 21 questions were used to measure the provision of women-friendly care among the participants. The value 1 is given for those who answered ‘yes’ and 0 for those who answered ‘no’ and coded. The opposite questions were recoded. The sum of these questions was calculated to range from 0 to 21 with a mean women-friendly care provision of 12.24 and SD of 3.68.
As indicated in the table below, 337(93.7%), 322(89.7%), 320(89.1%) and 257(71.6%) respondents answered ‘yes’ to the question that asked if received care from the skilled birth attendant, if health facility provides them with the continuous availability of basic supplies, equipment or drugs, if they satisfied with waiting time in a health facility during health services provisions and if the language spoken by the health worker was easy to understand respectively. In another case, 217(60.3%), 272(75.8%) and 331(92.2%) respondents answered “no” to the questions if health facility provides them access to the ambulance to reach health institutions, if health care facility provides them with clean bathroom, toilet & water and if health care facility charge for services, drugs, and supplies respectively (Table 4).
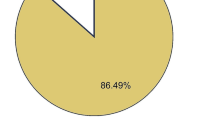
As the below figure shows, more than half 219(61%) of participants got the good provision of women-friendly care which is greater or equal to the mean value, and 140(39%) participants got the poor provision of women-friendly care (Fig. 1).
Factors associated with provision of women-friendly care
In this study, the association of different background factors of the study participants with a level of women-friendly care provision was investigated using bivariate and multivariable binary logistic regression analysis. On bivariate binary logistic regression analysis; residence, mother’s level of education, family monthly income, parity, last pregnancy planned, stay at a health facility after delivery, and paid for services were found to be statistically significant.
Variables found statistically significant on bivariate binary logistic regression analysis and had predetermined p-value less than 0.25 were entered into multivariable binary logistic regression. During multivariable binary logistic regression; parity, last pregnancy planned, and stay at a health facility after delivery were found to be statistically significant predictors of women-friendly care provision.
Primi para mother had almost 2 times more likely to have good women friendly care provision than multi mother [AOR = 1.88(1.07–3.33)]. In addition, participants who did plan their last pregnancy were 2 times more likely to have good women friendly care provision than those who did not plan [AOR = 1.94(1.04–3.63)], whereas participants who stayed at a health facility after delivery were found to be almost 5 times more likely to have good women friendly care provision than those who did not stay at a health facility after delivery [AOR = 4.8(1.71–13.39)] (Table 5).
Discussion
This study assessed women-friendly care provision and associated factors among mothers in the immediate post-partum period at public hospitals of southeast Ethiopia. The finding showed that the women-friendly care provision was (61%) [95%CI (55.73–66.04)] in the study area. The finding of this study was in line with a study conducted in Tanzania 63% [16], however, higher than related study conducted in Western (25.2%), Eastern (38.4%) Ethiopia [17, 18], and Bahir Dar (57%) [12], but lower than the study conducted in Jimma (71%), Gamo Gofa (79.1%), Harar Hospitals (85%) and Amhara region hospital (88%) [11, 19,20,21].
The possible reason for the discrepancies may be due to adherence to health facilities with women-friendly care amenities and different characteristics of health care providers in these different health facilities which affect the care provision. In these different places, there may be different capacity building in training techniques for health care providers result in different levels of women-friendly care provision. In addition, the possible reason may be particularly participant’s level of understanding about the services, service quality, and perception of normalizing some mistreatments.
Evidence report that disrespect and abuse of women during maternity care are problems that have been masked by a veil of silence and they can expressively impact women’s readiness to seek life-saving maternity care [4]. According to this study, of the total participants (7.8%) were disrespected during facility-based childbirth. This finding was lower than studies conducted in Egypt [22], Bahir Dar [12], and Arba Minch, Ethiopia [13]. The difference may be due to differences in health policy regarding maternity care across the countries and the level of applying that policy in the right ways in different administrations of the countries. This finding shows that still significant number of mothers are disrespected during post-delivery services while they bring newborns into this world. This type of activity may hinder women from seeking maternity care. If not resolved the lack of women-friendly care in facility-based childbirth often acts as a deterrent to future utilization of facility-based childbirth services [14]. Therefore, attention should be given to delivering quality-based maternity services during the immediate post-partum period, the crucial period after labor pain.
As the study revealed prim para mothers had almost 2 times more likely to have good women-friendly care provision than multipara mothers. The possible reason may be primipara mothers may be strange for the environment and assume the care provided by health facility as it is perfect whereas multipara mothers knew the care provided by health facility in a good manner from the experience and graded the health facilities service from the experience. However, the result disagreed with the previous related study conducted [23].
In addition, participants who did plan their last pregnancy were 2 times more likely to have good women-friendly care provision than those who did not plan. Similarly, last pregnancy was associated with women-friendly care in the study conducted in Eastern part of Ethiopia [18]. The possible reason may be, as pregnancy intentional, wanted and planned; utilization of maternal health services increased that help the mothers to be familiarized with friendly care health services, with health care providers that reduced sense of mistreated and increase the women’s attitude to perceive the care as friendly and respectful.
Correspondingly, in this study participants who stayed at a health facility after delivery were found to be almost 5 times more likely to have good women-friendly care provision than those who did not stay at a health facility after delivery. The finding was agreed with the related study conducted at Harar Hospitals [20]. The probable reason may be as long as the women stayed at health facilities they may perceive that they got good women-friendly care provision. The other reason may be as they stayed at health facilities they may familiarized with the environment and request good services.
It can be concluded that good women-friendly care provision at the health facilities level has multidirectional benefits at large and is clinically important to decreasing maternal and neonatal mortality rates. It should be provided regardless of circumstances, because all women have the right of to be well-treated. Irrespective of the variables associated with good woman-friendly care, all women who give birth in a health facility should be treated equally. The finding implies that there is still substandard postpartum care in developing countries like Ethiopia. As a result, there is a need to improve immediate postpartum care at the clinical level in each health facility.
Even if the study follows scientific procedural approach carefully, however, it had the following limitations. The firs one is, since the data were collected in the health facility there may be social desirability bias and fear of reporting mistreatment. To decrease this bias, the participant’s privacy was kept through using screen as a shelter for the mothers during data collection. The second one is, since the data was collected in the immediate post-delivery period it was difficult for the women to respond to the questions. The third one is, since the nature of the study design was cross-sectional, the study may difficult to ascertain the causal relationship between the study variables.
Conclusion
In general, compared to most of the other findings, the level of women-friendly care provision in public hospitals of Southeast Ethiopia was found to be low. Variables like parity, last pregnancy planned, and stay at a health facility after delivery were found to be statistically significant predictors of women-friendly care provision.
Since providing good women-friendly care is measure of quality care for health facilities, health care providers should be trained well to provide good women-friendly. Providing good women-friendly care is clinically important to increase health professional’s job satisfaction and helps to tackle maternal mortality rate.
The management of hospitals should work on better infrastructures, to provide better health care services and regularly evaluate the condition of women-friendly care services in the postnatal ward and should take correction measures.
Besides, that all supportive staff should be cooperative in providing good women-friendly care including cleaners and others. Furthermore, strong counseling on planned pregnancy and staying at health facilities after delivery is recommended. At the last, but not the least, researchers recommended working more in the areas by using a mixed study design.
Availability of data and materials
The data set analyzed during the current study are not publicly available due to consent for publication was not taken from the participants, but are available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Ante Natal Care
- CEmOC:
-
Comprehensive Emergency Obstetric care
- MMR:
-
Maternal Mortality Rate
- SPSS:
-
Statistical Package of Social Science
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- AOR:
-
Adjusted odds ratio
- SD:
-
Standard Deviation
- MWU:
-
Madda Walabu University
- LMICs:
-
Low and middle-income countries
References
USAID. Ending Preventable Maternal Mortality : USAID Maternal Health Vision for Action. 2014;
Abdella A. Maternal Mortality Trend in Ethiopia. EthiopJHealth Dev. 2010;(24 Special Issue I):110–20.
WHO/UNICEF/UNFPA. ‘Women friendly Health services Experiences in maternal care: report of a WHO/ UNICEF/ UNFPA workshop. Mexico City. 2008;
Windau-Melmer T. A Guide for Advocating for Respectful Maternity Care. Washington, DC: Futures Group, Health Policy Project; 2013.
Estimates by WHO, UNICEF, UNFPA WBG and the UNPD. Trends in Maternal Mortality : 1990 to 2015. 2015;
Krampah JKG and E. Mistreatment of Women in Health Facilities by Midwives during Childbirth in Ghana: Prevalence and Associated Factors. IntechOpen. 2018;
Hill DB and K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth Report of a Landscape Analysis. USAID. 2010;1–57.
Impact T, Health M. The Impact of Maternal Health in Peru :A Case study. Jessica Wunderlich/CARE. 2008;
WHO, UNICEF, UNFPA WBG and TUNPD. Trends in Maternal Mortality 2000 to 2017 Excutive summary. 2019;
Sheferaw ED, Bazant E, Gibson H, Fenta HB, Ayalew F, Belay TB, et al. Respectful maternity care in Ethiopian public health facilities. Reprod Health. 2017;14(1):60.
Hurissa BF, Getinet T. Assessment of Provision of Women Friendly Care and Associated Factors among Postnatal Mothers at Three Public Hospitals of Jimma Zone, Oromia Region, Ethiopia, 2016. J Biomed Sci. 2017;6(3):26.
Biresaw Wassihun SZ. Compassionate and respectful maternity care during facility based child birth and women ’ s intent to use maternity service in Bahir Dar,Ethiopia. BMC Pregnancy Childbirth. 2018;18(294).
Gebresilasea Gendisha MK, WG. Disrespect and abuse of women during childbirth in public health facilities in Arba Minch town, south Ethiopia – a cross-sectional study. PLoS ONE. 2019;14(4):1–17.
Bill & Melinda Gates Foundation U and U. News from the last Ten Kilometers :Improving Acess and Quality of BEmONC Services. Vol. 2. 2014. 1–4 p.
Kongnyuy EJ, Mlava G, Van Den BN. Criteria-based audit to improve women-friendly care in maternity units in Malawi. 2009;35(3):483–9.
Marya Plotkin, Gauiosa Tibaijuka, christina Lulu SC and ML. Quality of Care for Prevention and Management of Common Maternal and Newborn Complications: A study of 12 region in Tanzania. USAID, Matern Child Heal Integr Program,maisha. 2011;
Firew Tekle, Habtamu Kebede, Belachew Etana MW and TR. Disrespect and abuse during childbirth in Western Ethiopia : Should women continue to tolerate ? PLoS One. 2019;14(6):1–15.
Bante A, Teji K, Seyoum B, Mersha A. Respectful maternity care and associated factors among women who delivered at Harar hospitals, eastern Ethiopia : a cross- sectional study. BMC Pregnancy Childbirth. 2020;20(86):1–9.
Tesfaye R, Worku A, Godana W, Lindtjorn B. Client Satisfaction with Delivery Care Service and Associated Factors in the Public Health Facilities of Gamo Gofa Zone , Southwest Ethiopia : In a Resource Limited Setting. Hindawi Obstet Gynecol Int. 2016;1–7.
Getenet AB, Roba KT, Endale BS, Mamo AM, Darghawth R. Women ’ s satisfaction with intrapartum care and its predictors at Harar hospitals, Eastern Ethiopia : a cross-sectional study. Dovepress Nurs Res Rev. 2019;9:1–11.
Asres GD. Satisfaction of maternal care among women delivered at Asrade Zewude Memorial Primary Hospital, Bure, West Gojjam, Amhara, Ethiopia : A cross sectional study. J Public Heal Epidemiol. 2018;10(5):147–54.
Mousa O, Turingan OM. Quality of care in the delivery room : Focusing on respectful maternal care practices. J Nurs Educ Pract. 2019;9(1):1–5.
Asha Panth PK. Maternal Satisfaction on Delivery Service among Postnatal Mothers in a Government Hospital , Mid-Western Nepal. Hindawi Obstet Gynecol Int. 2018;11.
Acknowledgements
The authors would like to thank study participants, data collectors, and supervisors for all their support. The authors would like to thank Madda Walabu University for funding.
Funding
Madda Walabu University funded this work which is evidenced by the letter reference number RMU/14/92/667.
Author information
Authors and Affiliations
Contributions
Chala Kene designed the study, involved in data collection, data analysis, interpretation of the results, and preparation of all versions of the manuscript. Yohannes Tekalegn, Diriba Dibaba, Mujib Abdella, Genet Fikadu, Daniel Atlaw, Degefa Gomora, Girma Geta, Sintayehu Hailu, Kenbon Seyoum, Neway Ejigu, Biniyam Sahiledengle, and Alelign Tasew participated in proposal development, supervise during data collection, assisted during analysis and interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from MWU Research and Ethical committee with a letter of reference number RDD/0093/13. Then supporting and permission letter was obtained from the management of each public hospital. After explaining the objectives of the study in detail, written informed consent was obtained from each study participant. The right was given to the study participant to refuse, stop or withdraw from participation at the time of data collection. Privacy and confidentiality of the information and their responses were guaranteed by using screen during interview and throughout the entire study period and information was provided for any misconception at the end of the interview as deemed necessary. Since all participants were eighteen years old and above, written consent was taken from all of the study participants. In this study, all methods were performed in accordance with the relevant guidelines and regulations. All protocols were approved by Madda Walabu University’s research ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests in this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kene, C., Tekalegn, Y., Dibaba, D. et al. Level of women-friendly care provision among mothers in immediate post-partum period at public hospitals of Southeast Ethiopia: a cross-sectional study. BMC Women's Health 22, 475 (2022). https://doi.org/10.1186/s12905-022-02061-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-02061-w