Abstract
Background
A considerable proportion of cervical cancer diagnoses in high-income countries are due to lack of timely follow-up of an abnormal screening result. We estimated colposcopy non-attendance, examined the potential factors associated and described non-attendance reasons in a population-based screening study.
Methods
Data from the MARZY prospective cohort study were analysed. Co-test screen-positive women (atypical squamous cells of undetermined significance or worse [ASC-US+] or high-risk human papillomavirus [hrHPV] positive) aged 30 to 65 years were referred to colposcopy within two screening rounds (3-year interval). Women were surveyed for sociodemographic, HPV-related and other data, and interviewed for non-attendance reasons. Logistic regression was used to examine potential associations with colposcopy attendance.
Results
At baseline, 2,627 women were screened (screen-positive = 8.7%), and 2,093 again at follow-up (screen-positive = 5.1%; median 2.7 years later). All screen-positives were referred to colposcopy, however 28.9% did not attend despite active recall. Among co-test positives (ASC-US+ and hrHPV) and only hrHPV positives, 19.6% were non-attendees. Half of only ASC-US+ screenees attended colposcopy. Middle age (adjusted odds ratio [aOR] = 1.55, 95% CI 1.02, 4.96) and hrHPV positive result (aOR = 3.04, 95% CI 1.49, 7.22) were associated with attendance. Non-attendance was associated with having ≥ 3 children (aOR = 0.32, 95% CI 0.10, 0.86). Major reasons for non-attendance were lack of time, barriers such as travel time, need for childcare arrangements and the advice against colposcopy given by the gynaecologist who conducted screening.
Conclusions
Follow-up rates of abnormal screening results needs improvement. A systematic recall system integrating enhanced communication and addressing follow-up barriers may improve screening effectiveness.
Similar content being viewed by others
Background
Cervical cancer (CC) is preventable with effective primary and secondary prevention measures such as human papillomavirus (HPV) vaccination and screening. Cervical cancer screening (CCS) includes cytological assessment, viral detection of HPV or both (co-testing) [1]. However, following an abnormal screening result where risk of progression to CC is elevated, colposcopy is an important step to guide management [2]. Colposcopy involves magnified visual inspection of the cervix and biopsy extraction where necessary by trained and experienced colposcopists. Non-adherence to follow-up of abnormal screening results, i.e. colposcopy non-attendance, may lead to undiagnosed precancer (cervical intraepithelial neoplasia, CIN) and preventable CC [3], undermining screening effectiveness [4].
Until 2020, Germany offered free opportunistic Pap screening annually to women from age 20, but quality assurance measures were not systematically monitored [5]. Despite reasonable coverage [6] and declines in incidence, up to half of invasive CC cases were diagnosed in women screened frequently in the preceding 10 years [7]. Over two thirds of diagnoses had preceding negative screening results [8]. Failure of CCS to detect disease include sample collection issues to detect abnormal cells, but also lack of follow-up after an abnormal screening result [9]. The latter is not unique to Germany. For example in the US, 8% of CC diagnoses were attributed to colposcopy non-attendance [10] and a meta-analysis attributed 12% of CC to poor follow-up care [11]. Follow-up failures can be minimised if referrals are part of a failsafe recall system, via systemic tracking, call-and-recall invitations and reminders [2, 12]. In 2020, HPV testing was adopted as a co-test in women 35 years of age and older in Germany [5]. Therefore, it is important to identify sub-groups likely to be non-adherent with follow-up, particularly with the addition of HPV screening.
Several studies have examined potential factors associated with colposcopy non-attendance [3, 10, 13,14,15,16,17,18,19,20,21,22,23]. However, most lack individual socio-demographic information [10, 13, 16, 17, 20], or are based on underserved populations such as migrants [13, 14]. The role of HPV status on follow-up attendance was explored only recently in a small pilot study [24]. Additionally, small qualitative studies have examined reasons for colposcopy non-attendance [25, 26]. We estimated colposcopy non-attendance among screen-positive women from a population-based, real-world screening study involving co-testing and examined the potential factors associated with attendance. Additionally, we described non-attendance reasons.
Methods
Participants and data collection
The data stem from randomly recruited participants from the general population (n = 2,627) who were screened within the randomised trial and prospective cohort MARZY study, described previously [27, 28]. Briefly, women eligible from the general population (aged 30 to 65 years, with no history of hysterectomy or CC and not pregnant) were screened by office-based gynaecologists at study baseline (R1, 2005–2007) with routine Pap smear, plus an additional MARZY study swab (liquid-based cytology, ThinPrep, Cytyc/Hologic including subsequent HPV testing, Hybrid Capture®2). HPV co-testing was investigated [27]. Participants were administered a questionnaire (Q1) relating to sociodemographic and other factors.
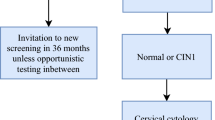
Positive screening results were defined as atypical squamous cells of undetermined significance or worse (ASC-US+) or high-risk HPV positive (hrHPV). Screen-positives were contacted by postal letter, which included HPV information and referred to the study colposcopy clinic (University Medical Center, Mainz; Fig. 1). These letters contained additional information on HPV infection and explained the colposcopy procedure in simple terms. Active telephone recall efforts were carried out by female study personnel to improve colposcopy attendance rates among women who did not arrange an appointment at the study clinic within 3 months of referral. Personnel also interviewed non-attendees for their reasons on non-attendance.
Screening was conducted again 3 years later (R2, 2008–2010) among women who participated in R1 and were still eligible (no hysterectomy or CC diagnoses since R1 and not pregnant). Lifestyle exposures such as smoking status were updated in a second questionnaire (Q2). Active recalls were again conducted by female study personnel if screen-positive participants had not attended colposcopy within 3 months following referral to the designated study clinic (University Medical Center, Mainz and St. Vincenz and Elisabeth Hospital, Mainz).
After R2 concluded (2010), an additional questionnaire with HPV-related questions (Q3) was administered to all hrHPV positive women, investigating perception and communication of HPV results, and HPV knowledge. As the MARZY screenings were conducted with a 3-year interval but routine Pap screenings were offered opportunistically and annually in the study region, any screenings conducted outside the study between the two MARZY rounds were retrospectively documented.
Colposcopy -attendance
We classified colposcopy attendance status using medical records from the designated colposcopy clinics. The primary outcome was non-attendance after referral to colposcopy within a 4 month time-frame, calculated as number of non-attendees among all referrals. This definition is based on the study referral threshold (ASC-US+ or hrHPV or both positive). At the time of study conduct, the 2008 European guidelines suggested colposcopies be conducted following ASC-US+ and hrHPV positive results [9]. The German CCS guideline in effect at the time advised women with low-grade squamous intraepithelial lesions or worse (LSIL+) who were also hrHPV positive to undergo colposcopy [29]. Attendance was estimated for both thresholds (ASC-US+ and hrHPV positive; LSIL+ and hrHPV positive).
Variables of interest
Sociodemographic variables obtained included age, region of residency, nationality, highest education level attained (lower secondary; upper secondary and further), employment situation, net monthly household income (low income ≤ 1500€; higher income > 1500€), marital status, parity (≤ 2 children; ≥ 3 children) and health insurance status. Smoking status, oral contraception use and hormone replacement therapy (HRT) were dichotomised (ever vs. never). Self-reported frequency of CCS attendance was grouped (regularly every 1–2 years; irregularly every 3 years or less or never). Screen-positive was defined as ASC-US+ only, hrHPV only or both ASC-US+ and hrHPV positive, and also LSIL+ only or both LSIL and hrHPV positive.
At the time of the Q3 survey, no validated HPV knowledge scale was available for use but the questionnaire items were based on extensive review of the qualitative body of evidence published. Perceived experience during and after the screening examination and concerns about infectivity or impact on sexual relationships were based on the Psychosocial Effects of Abnormal PAP Smears Questionnaire (PEAPS-Q) [30] and Cervical Dysplasia Distress Questionnaire (CDDQ) [31]. The items of interest were sub-categorised by 5-point Likert scale or binary “yes/no” answers as (i) Perception: negative screening experience (dichotomised), degree of negative reaction and understanding regarding the positive hrHPV result such as anxiety or insecurity, and (ii) HPV knowledge: as determined by the ability to identify at least 2 areas of HPV infection (virus, persistence consequences, vaccination; dichotomised), level of HPV understanding (none to good), and prior HPV knowledge to the study. Communication (iii) that occurred between the gynaecologists and participant (dichotomised), comprehensiveness of the counselling (dedicated time, provided background information and support), trust in the physician and discussion of result between the participant and friends or family members were also analysed. Concerns (iv) regarding cancer, infertility and infectivity were captured.
Statistical analyses
Any screen-positives leading to a referral at either round between 2005 and 2010 were included. If women were referred at both rounds, we designated questionnaire and interview data from the first referral only for regression analyses. All variables of interest were analysed using R (version 4.0.5, R Foundation for Statistical Computing, Vienna, Austria). Potential associations between attendance and individual factors were examined by univariable regression modelling and collinearity between variables were assessed. For multivariable regression, we applied multiple imputation methods to obtain model averaged estimates for missing data and computed bootstrap resampled 95% confidence intervals (CI; bootstraps = 500) using the MAMI package for R [32]. Missing data in regression models were treated as available case analyses and the adjusted odds ratios (aOR) controlled for all available confounders (age, region of residency, nationality, highest education level attained, employment situation, income, marital status, parity, smoking status, OC use, HRT use, screening frequency, screening result and insurance status), as these were previously reported to be associated with attendance [3, 10, 13,14,15,16,17,18,19,20,21,22,23]. Education, employment and screening result were dichotomised for regression. Non-attendee interview responses from both rounds were described together. In the case where women were non-attendees at both rounds, we designated the interview data from the first interview only. We also descriptively assessed the longitudinal outcomes (screening results, colposcopy attendance) of R1 referrals who did not attend colposcopy then but who were screened again at R2.
Informed consent was provided by all study participants prior to screening at study baseline. The MARZY study was approved by the ethical committee of the state of Rhineland-Palatinate (Landesärztekammer Rheinland-Pfalz: 837.438.03 (4100)) and the state government data protection office.
Results
Colposcopy attendance status
Of 2,627 women screened at R1, 228 (8.7%) were screen-positive, 222 (8.5%) were referred to colposcopy while 6 were not invited due to pre-planned hysterectomy elsewhere (Fig. 1). Initially, 106 of these 222 screen-positive women did not attend colposcopy within 3 months following referral. With active recall efforts, 96 could be reached and 28 (29.2%) attended afterwards. One woman who was not reached by telephone eventually attended colposcopy. Finally, 145 women (65.3%) attended colposcopy within 4 months, while 77 (34.7%) did not.
At R2, 2,093 (79.7%) women were screened at a median of 2.7 years later. Of the 107 screen-positive women referred to colposcopy, 32 initially did not attend after referral and 28 were reached via active recall (Fig. 1). Ten (31.3%) women were motivated to attend. Finally, 23 (21.5%) were non-attendees and 84 attended colposcopy (78.5%; Additional file 1: Table S1).
Twenty-one women were referred at both rounds where half were referred due to only hrHPV positive results (Additional file 1: Table S2). A total of 222 women (R1) and 86 women (R2) were referred to colposcopy (n = 308) in the entire study.
Overall, among 308 total referrals, attendance was recorded in 219 (71.1%) women and non-attendance in 89 (28.9%). Mean age in both groups were similar: 45.8 years (SD = 9.1) and 45.7 years (SD = 10.1) respectively. Among both ASC-US+ and hrHPV co-test positives, 9 (19.6%) did not attend (Fig. 2A). Among LSIL+ and hrHPV positives, 6 (17.1%) did not attend colposcopy (Fig. 2B). Approximately half of only cytology-positives attended colposcopy; the majority had ASC-US (Additional file 1: Table S3). By R2, 32 women had positive routine Pap results detected between study rounds. Non-attendance rates were similar (~ 20%) after excluding these cases (Additional file 1: Figure S1).
Proportion of overall referrals who attended or did not attend colposcopy by screening result at ASC-US+ threshold (A) and at LSIL+ (B). ASC-US+: Atypical squamous cells of undetermined significance or worse; hrHPV: high-risk human Papillomavirus; LSIL+: low grade squamous intraepithelial lesion or worse
Sociodemographic and other factors
Compared to younger women (30–39 years), 40–49 year old women were more likely to attend colposcopy (75% vs. 69%; aOR = 1.55, 95% CI 1.02, 4.96) (Table 1). Women who resided in the urban area were less likely to attend, albeit not statistically significant (65% vs. 76%; aOR = 0.63, 95% CI 0.30, 1.00). Among women from low income households, 87% were attendees while 68% of the women from higher income households (net monthly income >1500€) attended colposcopy. Women with higher household income or who had birthed ≥ 3 children were 67% (aOR = 0.33, 95% CI 0.11, 0.92) and 68% (aOR = 0.32, 95% CI 0.10, 0.86) less likely to attend colposcopy respectively. Smoking status, oral contraceptive use and HRT were not significantly associated with attendance. Sixty percent who attended screening irregularly (every 3 years or less) or not at all, attended colposcopy versus 73% of regular participants. A positive hrHPV screening result increased likelihood of attending by threefold (aOR = 3.04, 95% CI 1.49, 7.22; Table 1).
Reasons for non-attendance
Overall, 83 respondents provided reasons on non-compliance (response rate R1: 68/77 (88.3%); R2: 18/23 (78.3%) (Fig. 3). Over half indicated lack of time (56%), almost half (48%) mentioned barriers such as long travel time, travel cost, childcare challenges and 29% cited lack of choice of colposcopy clinic (Fig. 3A). A fifth of the women reported to have forgotten the appointment, while 15–16% feared the procedure itself or the outcome of the examination (Fig. 3A).
A Reasons for non-attendance over both rounds and B characteristics of the participants who were advised against attending the study colposcopy. ASC-US+: Atypical squamous cells of undetermined significance or worse; hrHPV: high-risk human Papillomavirus; LSIL+ low grade squamous intraepithelial lesion or worse
Forty-four percent mentioned that their office-based gynaecologist who conducted screening advised against colposcopy at the study clinic (Fig. 3B). Thirty-six percent of these women resided in the urban region, 40% were aged 40–49 years, 8% had a positive co-test at the guideline threshold LSIL+ , 12% reported irregular or no screening history and 80% reported having a repeat test since the MARZY screening round (Figs. 3B.1–B.5). Among 9 co-test screen-positives (ASC-US+ and hrHPV positive) who did not attend at either round (Table 1), only one cited the advice of the screening gynaecologist as the main reason for non-attendance; the remainder reported other barriers or concerns (Additional file 1: Table S4).
HPV: Perception, knowledge, communication and concerns
Among women who reported negative experiences during screening, 78% attended colposcopy compared to 87% of attendees who did not report a negative screening experience and 78% who reported moderate to high levels of negative reaction to their HPV result attended compared to 84% of attendees with little to no negative reaction (Table 2). Likelihood of attending colposcopy was lowered if screening was associated with a negative experience (OR = 0.49, 95% CI 0.21, 1.09) or reaction (OR = 0.64, 95% CI 0.27, 1.41), but not statistically significant. Approximately 79% of women reporting to have HPV knowledge attended compared to 82% with no HPV knowledge. Better levels of HPV knowledge were markedly lower among attendees (75%) than those reporting poor or no HPV knowledge who also attended colposcopy (82%). Level of understanding of the HPV result was not significantly associated with attendance (OR = 1.15, 95% CI 0.42, 2.82).
For communication, 85% of attendees reported direct communication of the HPV result by their gynaecologist compared to 76% of colposcopy attendees who were not directly informed by the gynaecologist. Direct communication increased the likelihood of attending but was not statistically significant (OR = 1.34, 95% CI 0.39, 5.03). Higher proportions of attendees also reported comprehensive counselling (83% vs. 80%), and discussed their result with a friend or family member (84% vs. 74%) than those who did not report these discussions. Eighty-five percent of women who reported lack of trust in their gynaecologist went to colposcopy compared to 81% who reported trust. Approximately 77% of all hrHPV positive women who responded in Q3 were concerned about cancer.
Longitudinal outcomes
At baseline R1, 77 referrals to colposcopy at R1 did not attend. Of these, 44 were lost to follow-up and not subsequently screened at R2. Respectively, baseline data and retrospective documentation of outcomes among these women indicated that 25 women (57%) were at least hrHPV positive (hrHPV positive only or both ASC-US+ and hrHPV positive) and a total of 4 women were scheduled to later undergo hysterectomies outside of the study (Additional file 1: Table S5). Three of the 4 women who underwent hysterectomies had a positive screening result within routine screening after R1 of MARZY.
Among the 33 referrals who did not attend colposcopy at R1 and were re-screened at R2, the majority (92%) were screened routinely between study rounds with negative screening results (Table 3). Only 2 non-attendees from R1 were screen-positive upon routine screening after study baseline. At R2, 4 women (12%) were hrHPV positive only, 2 (6%) were co-test positive to both cytology and hrHPV, while 27 (82%) were screen-negative. Among the 6 women referred again to colposcopy at R2, 5 (83%) did not attend, despite all 5 having a hrHPV positive result detected at R2 screening. Two of these women also had a concurrent cytological abnormality and via retrospective data linkage, it was found that they later underwent hysterectomies due to severe cervical intraepithelial neoplasia or worse (CIN3+ ; Additional file 1: Table S6).
Characteristics of the non-attendees who presented again at R2 show that 67% were women aged 50 years and above and 61% resided in an urban area (Additional file 1: Table S7). Twenty-one percent had 3 or more children and 28% did not attend screening regularly. Sixty-four percent of non-attendees from R1 reported no time as a reason for non-attendance at R1 and 50% reported a barrier. Among the 5 referrals who did not attend colposcopy at either R1 or R2, common reasons were lack of time, concerns and obstacles to arranging the appointment (Additional file 1: Table S6).
Discussion
In a population-based cohort study with both cytological and HPV testing (co-testing), the overall proportion of colposcopy non-attendance in screen-positive women was 29%. In referrals with ASC-US+ and hrHPV positive results, 20% did not attend despite active recall efforts. Attendance was associated with having a positive HPV status. Lack of time, barriers including childcare arrangements, travel time as well as lack of clinic choice and the advice given by the gynaecologist who conducted screening were cited as major reasons for non-attendance.
We observed higher non-attendance than in Europe (6–10%) [13, 16, 33]. In North America where CCS is offered opportunistically, non-attendance was observed in 28% of screened women [17], and up to 44% in underserved populations [34]. Low proportions of non-attendance appear to stem from organised screening contexts with active referral to colposcopy. This most likely explains the higher non-attendance rate observed in our study, since screening in Germany until 2020 was opportunistic. Historically, expert colposcopy was also not routinely performed, partly due to the annual screening interval, lack of certified dysplasia centres [35] and gynaecologists conducting repeat smears instead. This is evident in the high proportion of women in our study who were advised by their gynaecologist not to attend colposcopy and instead underwent repeat screening. Additionally, the guideline in effect at the time, when HPV screening was not offered, did not include recommendations for positive HPV or co-test results. The discrepancy between guideline and study protocol could explain this advice.
High non-adherence rates also arise from the lack of a screening registry to systematically contact non-attendees and lack of personnel to conduct recalls in non-organised programmes [36]. Randomised trials and community programs have demonstrated written reminders, preclinic calls and communication with patients significantly increase adherence to follow-up care [20, 23]. In our study, we were able to motivate a third of non-attending women to attend colposcopy by active call-recall. However, this may pose logistical challenges as the communication of results and referral is the responsibility of the screening physician, both in the previous and current screening program in Germany [5]. Management gaps between screening physicians and dysplasia centres where colposcopies are conducted also exist [35]. Enhanced patient communication conducted by clinic staff, streamlined management between gynaecological care providers and integration within a standardised call-recall system need to be introduced to reduce anxiety and improve attendance. Similar to other countries with organised screening, a programme target of less than 15% non-attendance should also be set [12].
Almost half (48%) of referrals with cytological abnormalities did not attend colposcopy, probably due to the annual screening interval. Congruent to a recent pilot study [24], a positive hrHPV result significantly increased attendance in our study by three times. We screened participants with HPV testing in addition to cytology, which at the time was not part of routine CCS in Germany. As the majority of hrHPV referrals reported concerns about cancer in our study, additional HPV testing may have caused anxiety or concern [37], which might have led to better attendance. However, in a randomised trial to reduce anxiety by educating participants on HPV before colposcopy, knowledge significantly increased but anxiety did not decrease [38]. Balanced risk communication must be addressed in a programme that offers HPV screening, and could be differential for subgroups such as younger and older women [39]. Furthermore, attendance rates could be improved if engaging information on colposcopy and particular attention for the emotional experience are provided [25, 26]. This is important since concerns and barriers were noted as reasons for non-attendance in a small group of women that did not attend colposcopy, despite being referred in both rounds.
Women with several children were less likely to attend colposcopy. Indeed, the major reasons cited for non-attendance were lack of time and barriers including lack of childcare arrangements, transport times and general lack of clinic choice (hospitals only). Additionally, our active recall efforts may not have mitigated such barriers, rather that it was more effective among women with hesitations. Moreover, we observed better attendance among women who were communicated their positive hrHPV result by the screening gynaecologist, in alignment with previous findings [23]. In a meta-analysis, even after HPV self-sampling kits are offered as a method to address barriers, follow-up non-adherence remains around 19% [40]. These observations underscore the necessity to diversify follow-up alternatives (self-sampling) and the importance of an established relationship including trust between the patient and physician. As recall appears largely to be left to the responsibility of the provider [5], encouraging information packs, educational support for screening physicians in counselling patients backed by a systematic screening registry for call-recall should be provided [12].
Limitations
We defined non-attendees as screen-positive to either cytology or HPV testing, rather than both cytology and HPV test positive. This may overestimate non-attendance as many who are screen-positive to one test only would normally undergo repeat Pap smear 3, 6 or 12 months later according to the guidelines in effect at the time in Germany [29]. However after restricting non-attendance to positive co-test results (ASC-US+ or LSIL+ and hrHPV positive), we found similar attendance rates. The sample size may have also restricted our analyses, particularly for the HPV-related items in Q3. However, only 18% of hrHPV positive cases were Q3 non-respondents. Additional assessment between Q3 respondents and non-respondents revealed some differences in nationality and socioeconomic status (Additional file 1: Table S8). These differences highlight potential external validity limitations of our results to un(der)screened women. Some non-attendees whom were unreachable may have sought colposcopy elsewhere, but the numbers are small.
Conclusion
Our population-based screening study offers important insight into colposcopy non-attendance, particularly as HPV testing is being integrated into screening in many countries. We quantitatively and qualitatively described the major reasons for non-attendance, which is important to maximise screening effectiveness. A considerable proportion of women did not attend colposcopy after abnormal screening results, and this persisted even in some women who were referred twice. Certain subgroups of women could be targeted by personalised measures within a failsafe recall system, especially since HPV testing is new. Continued educational support of screening gynaecologists should also be integrated. An optimised screening management continuum can reduce loss to follow up, minimise preventable CC diagnoses and improve the overall effectiveness of cancer screening.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASC-US:
-
Atypical squamous cells of undetermined significance
- CC:
-
Cervical cancer
- CCS:
-
Cervical cancer screening
- CIN:
-
Cervical intraepithelial neoplasia
- HC2:
-
Hybrid Capture®2
- HPV:
-
Human papillomavirus
- hrHPV:
-
High-risk HPV
- LSIL:
-
Low-grade squamous intraepithelial lesion
References
Maver PJ, Poljak M. Primary HPV-based cervical cancer screening in Europe: implementation status, challenges, and future plans. Clin Microbiol Infect. 2020;26(5):579–83.
Prendiville W, Sankaranarayana R. Colposcopy and Treatment of Cervical Precancer. IARC Technical Publication No. 45. Lyon, France: International Agency for Research on Cancer. 2017. Available from: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Technical-Publications/Colposcopy-And-Treatment-Of-Cervical-Precancer-2017.
Leyden WA, Manos MM, Geiger AM, Weinmann S, Mouchawar J, Bischoff K, et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst. 2005;97(9):675–83.
Doubeni CA, Gabler NB, Wheeler CM, McCarthy AM, Castle PE, Halm EA, et al. Timely follow-up of positive cancer screening results: a systematic review and recommendations from the PROSPR Consortium. CA Cancer J Clin. 2018;68(3):199–216.
Hillemanns P, Iftner T. New secondary prevention of cervical cancer in Germany starting in 2020. Onkologe. 2020;26(7):591–7.
Klug SJ, Taylor KJ, Scheidemann-Wesp U, Lautz D, Guther B, Potthoff P, et al. Participation in cervical cancer screening in Germany. Prev Med. 2010;51(5):431–2.
Tanaka LF, Schriefer D, Radde K, Schauberger G, Klug SJ. Impact of opportunistic screening on squamous cell and adenocarcinoma of the cervix in Germany: A population-based case-control study. PLoS ONE. 2021;16(7): e0253801.
Marquardt K, Buttner HH, Broschewitz U, Barten M, Schneider V. Persistent carcinoma in cervical cancer screening: non-participation is the most significant cause. Acta Cytol. 2011;55(5):433–7.
Jordan J, Arbyn M, Martin-Hirsch P, Schenck U, Baldauf JJ, Da Silva D, et al. European guidelines for quality assurance in cervical cancer screening: recommendations for clinical management of abnormal cervical cytology, part 1. Cytopathology. 2008;19(6):342–54.
Landy R, Mathews C, Robertson M, Wiggins CL, McDonald YJ, Goldberg DW, et al. A state-wide population-based evaluation of cervical cancers arising during opportunistic screening in the United States. Gynecol Oncol. 2020;159(2):344–53.
Spence AR, Goggin P, Franco EL. Process of care failures in invasive cervical cancer: systematic review and meta-analysis. Prev Med. 2007;45(2):93–106.
Murphy J, Varela NP, Elit L, Lytwyn A, Yudin M, Shier M, et al. The organization of colposcopy services in Ontario: recommended framework. Curr Oncol. 2015;22(4):287–96.
Campari C, Fedato C, Iossa A, Petrelli A, Zorzi M, Anghinoni E, et al. Cervical cancer screening in immigrant women in Italy: a survey on participation, cytology and histology results. Eur J Cancer Prev. 2016;25(4):321–8.
Carrillo T, Montealegre JR, Bracamontes CG, Scheurer ME, Follen M, Mulla ZD. Predictors of timely diagnostic follow-up after an abnormal Pap test among Hispanic women seeking care in El Paso, Texas. BMC Womens Health. 2021;21(1):11.
Collier R, Quinlivan JA. Domestic violence is a leading risk factor in default from colposcopy services. J Obstet Gynaecol Res. 2014;40(6):1785–90.
Douglas E, Wardle J, Massat NJ, Waller J. Colposcopy attendance and deprivation: a retrospective analysis of 27,193 women in the NHS Cervical Screening Programme. Br J Cancer. 2015;113(1):119–22.
Elit L, Krzyzanowska M, Saskin R, Barbera L, Razzaq A, Lofters A, et al. Sociodemographic factors associated with cervical cancer screening and follow-up of abnormal results. Can Fam Physician. 2012;58(1):e22-31.
Green LI, Mathews CS, Waller J, Kitchener H, Rebolj M, Committee THPS. Attendance at early recall and colposcopy in routine cervical screening with human papillomavirus testing. Int J Cancer. 2021;148(8):1850–7.
Miller SM, Tagai EK, Wen KY, Lee M, Hui SA, Kurtz D, et al. Predictors of adherence to follow-up recommendations after an abnormal Pap smear among underserved inner-city women. Patient Educ Couns. 2017;100(7):1353–9.
Ogilvie GS, Shaw EA, Lusk SP, Zazulak J, Kaczorowski JA. Access to colposcopy services for high-risk Canadian women: can we do better? Can J Public Health. 2004;95(5):346–51.
Sharp L, Cotton S, Thornton A, Gray N, Cruickshank M, Whynes D, et al. Who defaults from colposcopy? A multi-centre, population-based, prospective cohort study of predictors of non-attendance for follow-up among women with low-grade abnormal cervical cytology. Eur J Obstet Gynecol Reprod Biol. 2012;165(2):318–25.
Fish LJ, Moorman PG, Wordlaw-Stintson L, Vidal A, Smith JS, Hoyo C. Factors associated with adherence to follow-up colposcopy. Am J Health Educ. 2013;44(6):293–8.
Eggleston KS, Coker AL, Das IP, Cordray ST, Luchok KJ. Understanding barriers for adherence to follow-up care for abnormal pap tests. J Womens Health. 2007;16(3):311–30.
Buick C, Murphy KJ, Howell D, Metcalfe K. Understanding the role of oncogenic human papillomavirus (HPV) status on adherence behaviors among women with abnormal cervical cytology. BMC Womens Health. 2021;21(1):29.
Swancutt DR, Greenfield SM, Luesley DM, Wilson S. Women’s experience of colposcopy: a qualitative investigation. BMC Womens Health. 2011;11:11.
Young A, Cotton S, Cruickshank ME. Information needs of young women vaccinated against HPV attending colposcopy: a qualitative study. BMC Womens Health. 2018;18(1):200.
Liang LA, Einzmann T, Franzen A, Schwarzer K, Schauberger G, Schriefer D, et al. Cervical cancer screening: comparison of conventional Pap smear test, liquid-based cytology, and human papillomavirus testing as stand-alone or cotesting strategies. Cancer Epidemiol Biomark Prev. 2021;30(3):474–84.
Radde K, Gottschalk A, Bussas U, Schülein S, Schriefer D, Seifert U, et al. Invitation to cervical cancer screening does increase participation in Germany: results from the MARZY study. Int J Cancer. 2016;139(5):1018–30.
Deutschen Gesellschaft für Gynäkologie und Geburtshilfe e. V. (DGGG). Interdisziplinäre S2k-Leitlinie für die Prävention, Diagnostik und Therapie der HPV-Infektion und präinvasiver Läsionen des weiblichen Genitale. AWMF-Leitlinien-Register. 2008 July 2008. Report No.: AWMF 015/027. [Accessed on 24 June 2021]. Available from: https://www.ag-cpc.de/wp-content/uploads/2018/07/015-027_S2_IDA_Praevention__Diagnostik_und_Therapie_der_HPV-Infektion_und_praeinvasiver_Laesionen_des_weiblichen_Genitale_06-2008_09-2012.pdf.
Bennetts A, Irwig L, Oldenburg B, Simpson JM, Mock P, Boyes A, et al. PEAPS-Q: a questionnaire to measure the psychosocial effects of having an abnormal pap smear. Psychosocial effects of abnormal Pap smears questionnaire. J Clin Epidemiol. 1995;48(10):1235–43.
Shinn E, Basen-Engquist K, Le T, Hansis-Diarte A, Bostic DS, Martinez-Cross J, et al. Distress after an abnormal Pap smear result: scale development and psychometric validation. Prev Med. 2004;39(2):404–12.
Schomaker M, Heumann C. Model selection and model averaging after multiple imputation. Comput Stat Data Anal. 2014. https://doi.org/10.1016/j.csda.2013.02.017.
Rebolj M, Lynge E. Incomplete follow-up of positive HPV tests: overview of randomised controlled trials on primary cervical screening. Br J Cancer. 2010;103(3):310–4.
Benard VB, Lawson HW, Eheman CR, Anderson C, Helsel W. Adherence to guidelines for follow-up of low-grade cytologic abnormalities among medically underserved women. Obstet Gynecol. 2005;105(6):1323–8.
Beckmann MW, Quaas J, Bischofberger A, Kämmerle A, Lux MP, Wesselmann S. Establishment of the certification system “gynaecological dysplasia” in Germany. Geburtshilfe Frauenheilkd. 2014;74(9):860–7.
Wordlaw-Stinson L, Jones S, Little S, Fish L, Vidal A, Smith JS, et al. Challenges and recommendations to recruiting women who do not adhere to follow-up gynecological care. Open J Prev Med. 2014;4(3):123–8.
McBride E, Marlow LAV, Forster AS, Ridout D, Kitchener H, Patnick J, et al. Anxiety and distress following receipt of results from routine HPV primary testing in cervical screening: the psychological impact of primary screening (PIPS) study. Int J Cancer. 2020;146:2113–21.
de Bie R, Massuger L, Lenselink C, Derksen Y, Prins J, Bekkers R. The role of individually targeted information to reduce anxiety before colposcopy: a randomised controlled trial. BJOG. 2011;118(8):945–50.
O’Connor M, O’Leary E, Waller J, Gallagher P, Martin CM, O’Leary JJ, et al. Socio-economic variations in anticipated adverse reactions to testing HPV positive: implications for the introduction of primary HPV-based cervical screening. Prev Med. 2018;115:90–6.
Arbyn M, Smith SB, Temin S, Sultana F, Castle P. Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: updated meta-analyses. BMJ. 2018;363: k4823.
Acknowledgements
We thank all participating office-based gynaecologists, the staff at the colposcopy clinic of the University Medical Center Mainz and St Vincenz hospital, the MARZY study team at the Institute of Medical Biostatistics, Epidemiology and Informatics, University Medical Center Mainz, and all women participating in the MARZY study.
Funding
Open Access funding enabled and organized by Projekt DEAL. The MARZY study was funded by the German Cancer Aid (Deutsche Krebshilfe [DKH], No. 105827, 106619, 107247, 108047, and 107159). The funding agency did not interfere with the study results.
Author information
Authors and Affiliations
Contributions
Study conception and design: SJK, MB. Data collection and patient management: SRZ, KR, SF, HI. Study co-ordination: KR, SJK. Data analysis and interpretation: LAL, GS, SM, SJK. Drafting of the manuscript: LAL, SJK. Revision and final manuscript review: all co-authors. Supervision of the findings: SJK. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent to participate in the MARZY prospective cohort study was provided in written form by all study participants prior to screening at study baseline. The MARZY study was approved by the ethical committee of the state of Rhineland-Palatinate (Landesärztekammer Rheinland-Pfalz: 837.438.03 (4100)) and the state government data protection office. All recruitment, data collection and analyses were performed in accordance to Good Epidemiological Practice guidelines and the Declaration of Helsinki.
Consent for publication
Not Applicable (NA).
Competing interests
HI reports co-ownership of a laboratory for cytology and molecular diagnostics. All other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. The following file contains further analyses and insight (tables S1–S8 and figure S1) to complement the main analyses of our study
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liang, L.A., Zeissig, S.R., Schauberger, G. et al. Colposcopy non-attendance following an abnormal cervical cancer screening result: a prospective population-based cohort study. BMC Women's Health 22, 285 (2022). https://doi.org/10.1186/s12905-022-01851-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01851-6